
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 18 March 2021
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.664971
This article is part of the Research Topic Infection and Control of Vector-Borne Diseases View all 34 articles
 Lili Wang1
Lili Wang1 Jianhai Yin2*
Jianhai Yin2* Canjun Zheng3*
Canjun Zheng3* Samuel Juana Smith4
Samuel Juana Smith4 Esther Ngegba1
Esther Ngegba1 Xiaoxia Huang5
Xiaoxia Huang5 Anitta Kamara4
Anitta Kamara4 Xia Chen6
Xia Chen6 Xu Wang2
Xu Wang2 Wei Luo7
Wei Luo7 Biao Kan6
Biao Kan6Sierra Leone is a highly endemic area for malaria, and the implementation of the National Malaria Strategic Plan (2016–2020) has reached its midpoint in 2018. To provide more specific guidance for interventions in the future, a household-based cross-sectional survey was conducted to elucidate the knowledge, awareness and practices regarding malaria and malarial control measures among the general public. Three communities (Grafton, Jui, and Kossoh) in the Western Area Rural District that were in close proximity to Sierra Leone's capital city of Freetown were included. Households were randomly selected and interviewed with a structured questionnaire covering malaria infection, diagnosis, treatment and prevention, as well as knowledge of malaria prevention. As a result, a total of 262 qualified questionnaires were included. The average cost for meals per day is ~30,000 Leones in each household. The rate of awareness, indicated by reporting having heard of malaria, was 98.1% (257/262), and 86.6% (227/262) of the respondents knew that mosquito bites are the main route of transmission. In addition, 80.9% (212/262) of the respondents sought health advice or treatment for the illness, and a similar percentage of respondents had been tested for malaria, mostly with rapid diagnostic tests (RDTs). A high demand for long-lasting insecticidal nets (72.1%) matched the serious shortage (61.8%, 162/262), and of the households that reported a lack of nets, 66 had children younger than 5 years old. In conclusion, public awareness of malaria prevention is high, based on this survey, although there was a limited use of preventive measures in these three communities and the malaria burden was still high. Therefore, the public's knowledge of malaria should be sustained and reinforced, and the distribution and use of malaria prevention measures should be promoted to supprt the achievement of the planned objectives.
Malaria is endemic in Sierra Leone; the entire population is at risk of exposure because Sierra Leone is an area of stable malarial endemicity, and almost cases were infected with Plasmodium falciparum (1). Sierra Leone's high malaria disease burden accounted for ~48% of outpatient morbidity and ~38% of mortality in children younger than 5 years according to the national Malaria Indicator Survey conducted in 2016 (2). Although significant progress with regard to reducing mortality has been made, it is still a major public health concern. The control of malaria remains a priority in the national health agenda of Sierra Leone.
A multipronged strategy to control malaria, including vector control interventions, diagnostic testing, treatment with quality-assured artemisinin-based combination therapies, and standardized case management training manuals for community and facility treatment providers, has been developed and implemented in Sierra Leone based on the World Health Organization (WHO) recommendations (3). The goals are for 80% of the population to have appropriate levels of knowledge and uptake/practice of malaria prevention and management strategies, all the at-risk population to have access to the appropriate preventive interventions, 80% of individuals with suspected malaria cases to have access to confirmatory diagnostic testing, and all individuals with malaria to receive effective treatment by 2018, according to the current Sierra Leone National Malaria Strategic Plan (2016–2020) (SL-NMSP) (3).
The awareness of malaria symptoms, transmission, prevention and treatments is closely related to the implementations of malaria control programs (4–6). A knowledge, awareness and practices (KAP) survey about malaria could help policy makers better understand the current situation and guide malaria control strategies. Therefore, this study is conducted to determine the knowledge, awareness and practices regarding malaria and its control measures in the general public through a household-based survey at the midpoint of the implementation of the SL-NMSP.
Three communities (Grafton, Jui, and Kossoh) in Western Area Rural District within close proximity to Sierra Leone's capital city Freetown were included in this household-based survey on malaria. This district is home to a very religiously and ethnically diverse population. Grafton is a trade center. Jui and Kossoh are neighborhood towns. Kossoh town is surrounded by a large forest reserve, and its major industries are farming and coal mining.
A total of 300 households in the three designated communities were randomly selected as survey respondents using a cluster sampling design. One adult member from each selected household was interviewed with a structured questionnaire covering demographic information, economic status, basic knowledge of malaria, and malaria prevention and control practices. When medicines were discussed, packages of various drugs were displayed to the participants.
The survey was conducted in collaboration with the National Malaria Control Program of the Ministry of Health and Sanitation, Sierra Leone, in December 2018, at the midpoint of the SL-NMSP (3). Local staff from Sierra Leone-China Friendship Biological Safety Laboratory (7) were trained in prior to their involvement in the administration of the survey.
Data was input and cross-checked by EpiData version 3.1 (8, 9). Then, descriptive statistics and percentages were presented using Microsoft Excel 2010 software. Differences in distribution among three communities were evaluated using the chi-square (χ2) test or Fisher's exact test by SPSS software version 20.0 (IBM, USA) and P < 0.05 was considered statistically significant.
A total of 300 households were investigated, and 262 qualified questionnaires from 108, 47, and 107 households in Grafton, Jui, and Kossoh communities, respectively, were finally included in the analysis after checking for questionnaire completion and logic. The survey covered 1,645 residents, with ~6 persons per family. The average cost of meals per day was ~30,000 Leones in each household (one US dollar was equal to 8,000 Leones in December 2018).
A total of 929 persons in 202 households reported having had a fever in 2018. Among them, 406 persons from 97 households, 228 persons from 46 households, and 295 persons from 89 households in Grafton, Jui, and Kossoh communities, respectively, reported having suffered malaria. Moreover, 129 persons from 64 households reported having suffered malaria once, and 146 persons from 66 households reported having suffered malaria being twice, and 61 persons from 26 households being three times, and 275 persons from 91 households being more than three times, respectively.
Moreover, ~80.9% (212/262) of the respondents reported seeking professional advice or treatment for the illness from any source (P < 0.001, Fisher's exact test) (Table 1). Additionally, 72.2% (153/212) of the respondents reported preferring to seek advice and treatment from the public medical sector (including government hospital, government health center, mobile clinic, community health worker, other public sector) only (P = 0.001, Fisher's exact test). And 20.3% (43/212) and 7.1% (15/212) were found to seek assistance from the private sector (including private hospital, private clinic, mission/faith-based hospital, mission/faith-based clinic, pharmacy, mobile clinic, other private medical sector) only or any sector (Tables 1, 2).
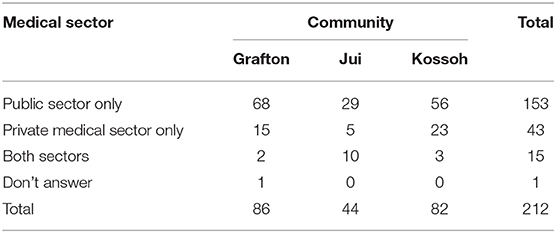
Table 1. The distribution of medical sectors people seeking health advice or treatment in the three communities in the Western Area Rural District, Sierra Leone, 2018.
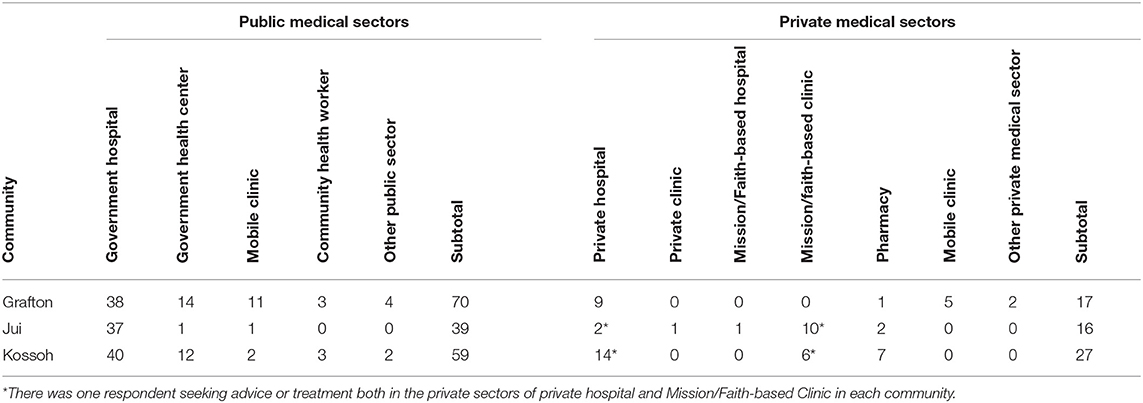
Table 2. The detail of public or private medical sectors people selected for health care seeking in the three communities in the Western Area Rural District, Sierra Leone, 2018.
Furthermore, 84.4% (221/262) of the respondents reported that they and their family members always visited a health care worker or doctor when they suspected they had contracted malaria (P = 0.071, Fisher's exact test). Among the individuals who went to see a health care worker or doctor, they reported visiting a professional every time (43.4%, 96/221) or most of the times (37.1%, 82/221) they suspected they had contracted malaria (χ2 = 37.219, P < 0.000) (Table 3).
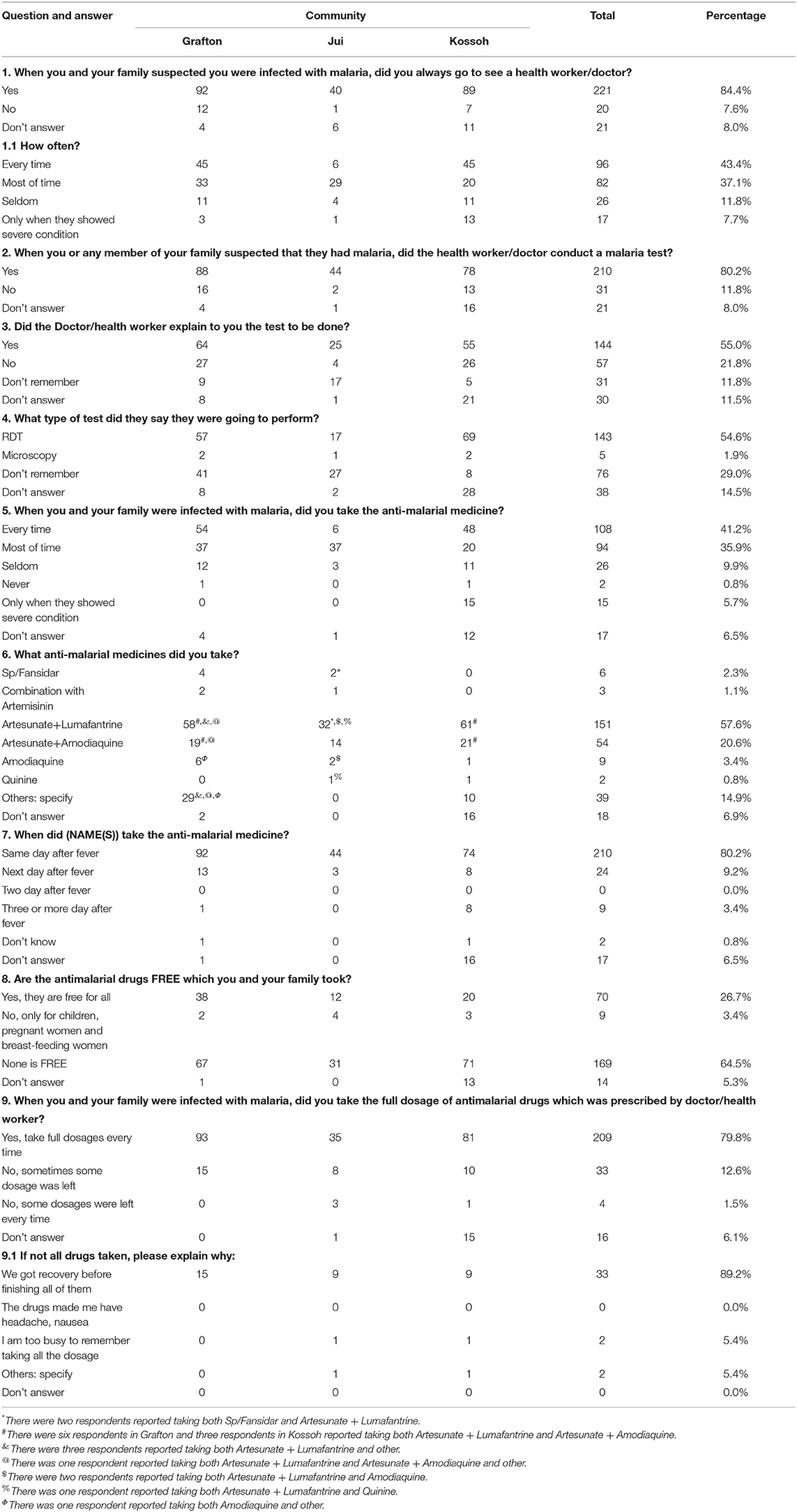
Table 3. Malaria diagnosis and anti-malarial medicine taking in the three communities in the Western Area Rural District, Sierra Leone, 2018.
As recalled by the respondents, the health care worker or doctor performed a malaria test when they visited because they suspected that they had contracted malaria (80.2%, 210/262) (χ2 = 15.854, P = 0.003), and the malaria rapid diagnostic tests (RDT) was the most commonly used test (54.6%, 143/262); however, approximately half of the respondents (55.0%, 144/262) reported that the doctors or health care workers did not explain the test to them (Table 3).
Most respondents took anti-malarial medicine every time (41.2%, 108/262) or almost every time (35.9%, 94/262) they were diagnosed with malaria, and ~79.8% (209/262) of them took the full course of treatment every time as prescribed by the doctor or health care worker. Artesunate and lumefantrine (57.6%, 151/262) and artesunate and amodiaquine (20.6%, 54/262) were the top two choices of combination therapy. The most common reason given for the early termination of a course of treatment was having recovered prior to finishing all the doses (89.2%, 33/37). Moreover, ~80.2% (210/262) of the respondents reported starting anti-malarial medicine on the same day that they noted the fever, and ~64.5% (169/262) of them responded that the anti-malarial medicine were not free (Table 3).
In this survey, 188 households had long-lasting insecticidal nets (LLINs) (χ2 = 2.282, P = 0.340), but more nets were required because 189 respondents said that they did not have enough LLINs in their households (P = 0.102, Fisher's exact test), so resulting in children under the age of 5 years in 66 households not having LLINs to sleep under (P = 0.120, Fisher's exact test). Only 146 respondents had slept under nets the night before the survey (P = 0.073, Fisher's exact test). Furthermore, some members in 162 households with nets did not sleep under LLINs (χ2 = 18.179, P = 0.001), which could lead to cross-infection. Half of the LLINs were distributed by the governmental hospital/health centers (49.6%, 130/262) and community health centers (15.3%, 40/262) (Table 4).
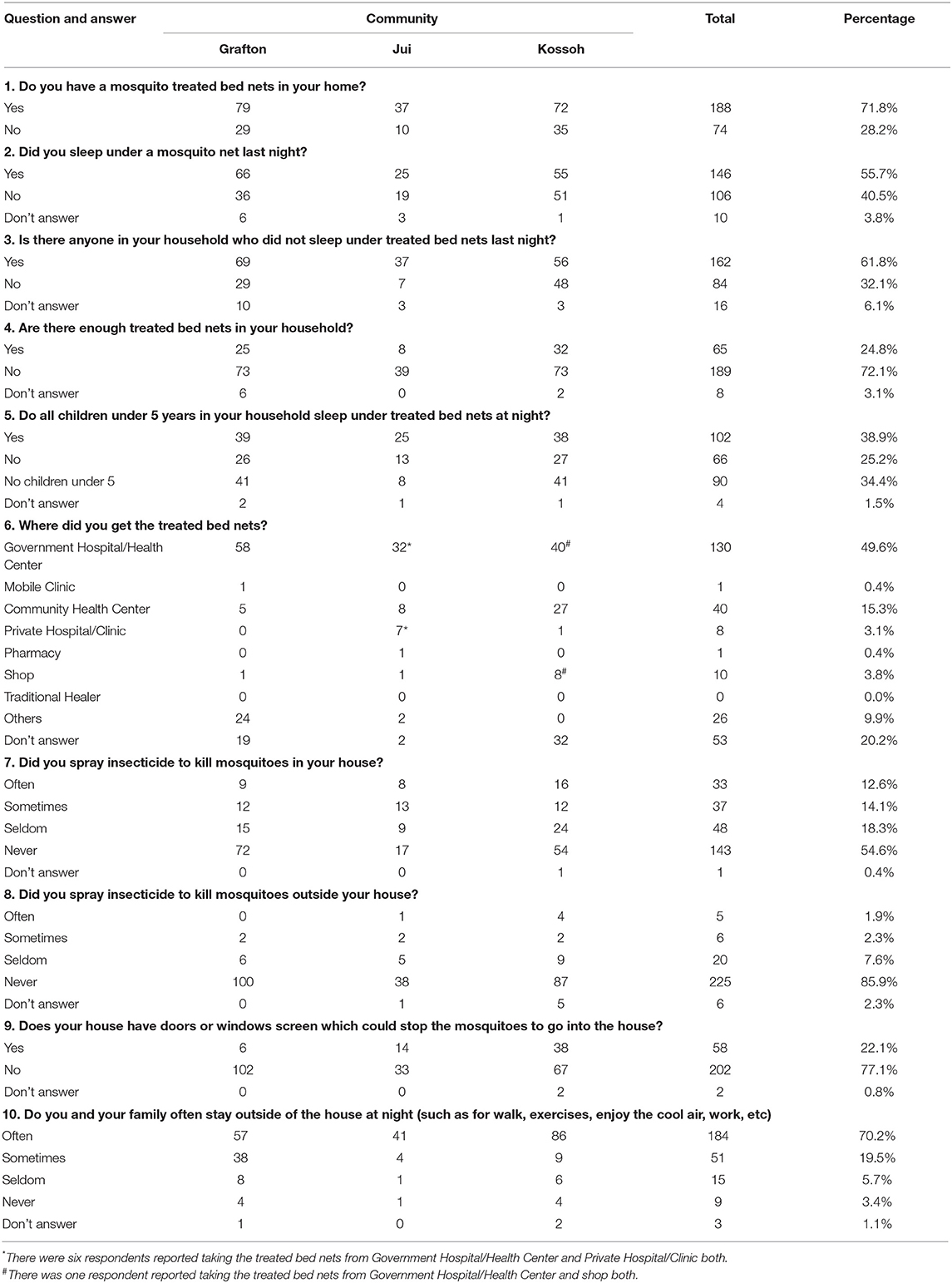
Table 4. Malaria prevention practices in the three communities in the Western Area Rural District, Sierra Leone, 2018.
In addition, a total of 143 households never sprayed insecticide indoors to kill mosquitoes (χ2 = 19.945, P = 0.007), and 225 households never sprayed insecticide outside (P = 0.073, Fisher's exact test). Furthermore, more than three quarters of the respondents (77.1%, 202/262) reported that they did not have a door or window screen to prevent mosquitoes from entering their houses (P < 0.001, Fisher's exact test). Additionally, most families (89.7%, 235/262) reported staying outside of the house at night (P < 0.001, Fisher's exact test) (Table 4).
In this survey, almost all the respondents had heard about malaria (98.1%, 257/262) (P = 0.214, Fisher's exact test) and knew that the main route of transmission was through mosquito biting (86.6%, 227/262) (χ2 = 5.045, P = 0.081). Fever (44.3%, 116/262) (χ2 = 4.845, P = 0.092), body aches or joint pain (38.9%, 102/262) (χ2 = 1.189, P = 0.566), and loss of appetite (36.6%, 96/262) (χ2 = 2.928, P = 0.237) were the top three clinical manifestations they reported. A total of 173 respondents reported that they would always go to see a doctor or health care worker when they suspected they had malaria (χ2 = 1.323, P = 0.530), while 48 interviewees said they would take some of the anti-malarial medicine kept in their houses first (χ2 = 15.322, P < 0.001). The expensive costs (mentioned by 176 respondents) was the main factor preventing people from visiting the doctor or health care worker (χ2 = 0.059, P = 0.969). Sleeping under LLINs (198) (χ2 = 1.432, P = 0.499) and keeping their surrounding clean (84) (χ2 = 5.982, P = 0.051) were the most common methods of malaria prevention employed (Table 5).
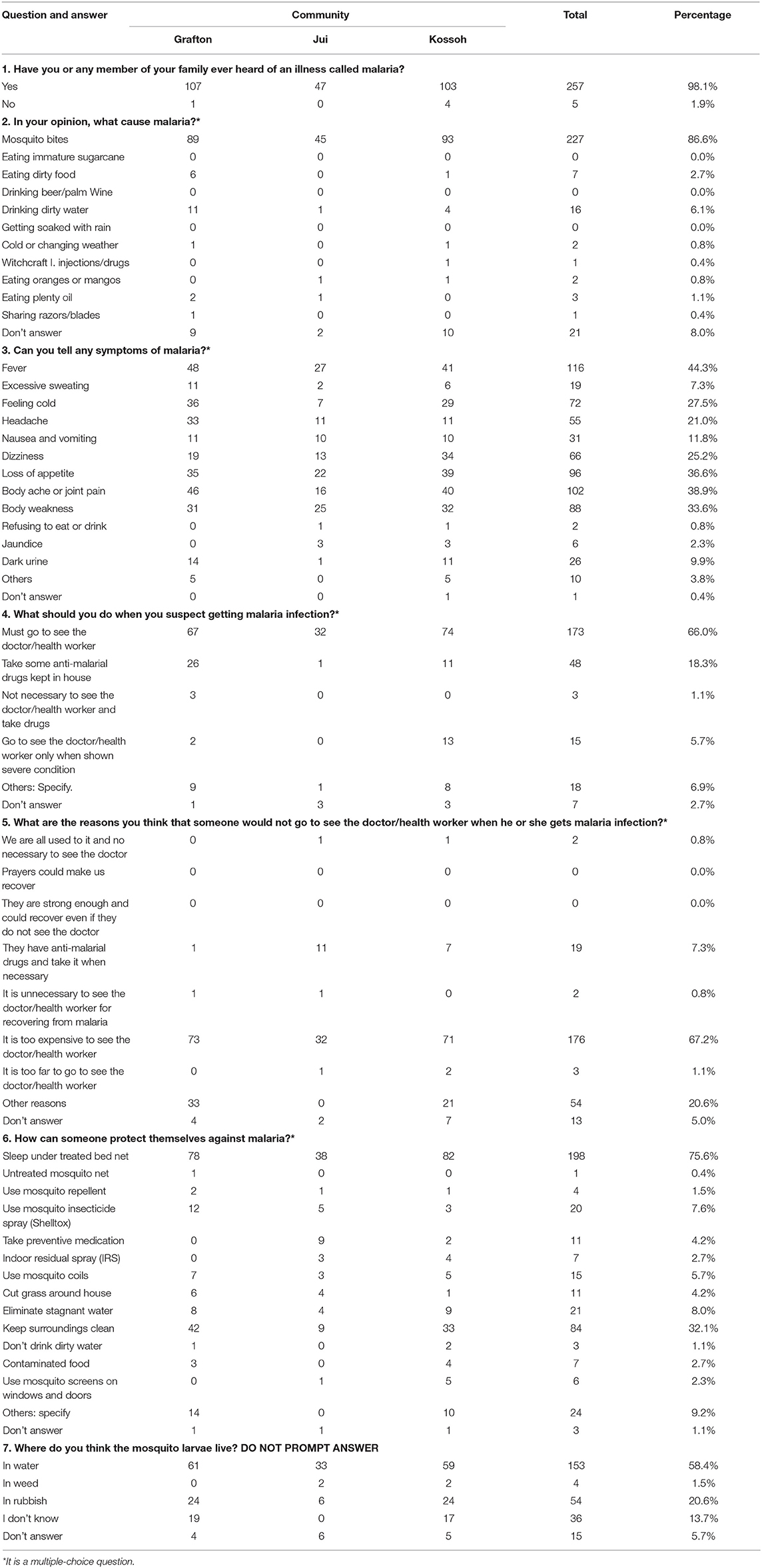
Table 5. Knowledge of malaria transmission, symptom and prevention in the three communities in the Western Area Rural District, Sierra Leone, 2018.
Malaria remains one of the most serious public health issues and is responsible for high proportions of morbidity and mortality in Sierra Leone. In the present study, overall high levels of knowledge regarding the causes of malaria, prevention mechanisms and symptoms, and active seeking of treatment for malaria from health care providers were found among Sierra Leoneans, similar to the results in the MIS 2013 and 2016 (2, 10); these results with regards to knowledge and practices support malaria control (11–13).
Globally, vector control is the most commonly accomplished through the use of LLINs and indoor residual spraying (IRS), with the aim of reducing the transmission by preventing human–vector contact and killing vector mosquitoes (14, 15). The goal was for the entire at-risk population to employ preventive measures, including the use of LLINs, IRS and larval source management, by 2017 in Sierra Leone. However, 72.1% of the respondents required more nets, which may explain the high percentage (61.8%, 162/262) of households and the high proportion of children under 5 years old who did not sleep under the nets at night according to this survey. This indicates a large gap in obtaining and using nets by the most vulnerable groups who are not benefiting as much as hoped from preventive malaria interventions. Moreover, screens for doors and windows that are cost-effective to install and maintain are a supplementary public health intervention to prevent humans from being bitten by mosquito vectors indoors, thereby significantly reducing the transmission of malaria. However, screens seem to have been neglected in the regular malaria control campaigns (16, 17), resulting in fewer than 25% of households having door or window screen in this survey, and a general low awareness of the role of screens. In addition, a low level of implementation of IRS and outside spraying and a high level of engagement in activities outside of the house at night were found, despite the presence of many mosquitoes. Therefore, how to improve residents' outdoor protection, or reduce outdoor activities at night, as well as to further improve the awareness and correct use of protective measures, can become an important content of the future malaria campaign.
The early diagnosis and prompt treatment of malaria reduces the transmission of the disease and prevents deaths. It is critical for people to seek diagnosis and care as soon as they experience any symptoms of malaria. It is encouraging that more than 80% of the respondents reported that they visited the doctor in a timely manner, and a similar percentage of respondents reported being tested for malaria, usually with RDTs not microscopy, which is the standard method for malaria diagnosis. However, approximately three-quarters of the respondents said that the doctors did not interpret the test results for the patients. Therefore, a good opportunity to provide health education and promote malaria control and prevention is being missed. A home-based RDT that could be performed by trained family members rather than at a healthcare facility may improve the timeliness of the diagnosis of malaria (18–20). Moreover, the reported adherence to completing the course of antimalarial treatment was close to 80% at the clinic or if self-administration at home. Reasons for the lack of adherence were reported to be sickness after the first dose, insufficient food to take the medicine, forgetting to take the medicine, and poor instructions provided by the community health center (CHC) (21). In addition, the cost of medical treatment and the distance from the hospital must also be considered.
However, there were some limitations of this study. First, this was a small-sample cross-sectional study conducted in three communities, and the findings are not yet nationally representative. Second, the collected data were based on respondent recall, and the data may be biased. Therefore, the results of the study highlight the need for more extensive investigations of the KAP regarding malaria in Sierra Leone.
In conclusion, in these three communities, public awareness of malaria prevention measures was relatively high in this survey, but the malaria burden was still higher than because the limited use of preventive measures against malaria potentially. Thus, the existing knowledge of malaria should be sustained and reinforced, and the availability and use of malaria prevention measures should be promoted to achieve the goals of the SL-NMSP.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Sierra Leone Ethics and Scientific Review Committee. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
JY and CZ conceived the study, developed questionnaire, and conducted fieldwork. LW and JY analyzed data and wrote the manuscript. SS and BK contributed to the study design. EN and AK conducted fieldwork and supervised fieldwork. XH, XC, XW, and WL contributed to data collation and cross-checking. All authors read and approved the final draft.
This study was supported by Sierra Leone-China Second Phase of the Fixed Biological Safety Laboratory Technical Cooperation Project and the National Science and Technology Major Program of China (No. 2018ZX10101002–002).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We appreciate the Sierra Leonean staff for their wonderful work in the Sierra Leone-China Friendship Biological Safety Laboratory.
2. Sierra Leone Malaria Indicator Survey. Freetown, Sierra Leone: NMCP, SSL, CRS, and ICF International (2016).
3. Sierra Leone Malaria Control Strategic Plan (2016-2020). Freetown, Sierra Leone: National Malaria Control Programme (2015).
4. Naing PA, Maung TM, Tripathy JP, Oo T, Wai KT, Thi A. Awareness of malaria and treatment-seeking behaviour among persons with acute undifferentiated fever in the endemic regions of Myanmar. Trop Med Health. (2017) 45:31. doi: 10.1186/s41182-017-0070-9
5. Mathania MM, Kimera SI, Silayo RS. Knowledge and awareness of malaria and mosquito biting behaviour in selected sites within Morogoro and Dodoma regions Tanzania. Malar J. (2016) 15:287. doi: 10.1186/s12936-016-1332-4
6. Alelign A, Petros B. Knowledge, attitudes and practices of malaria transmission and preventive measures in Woreta town, Northwest Ethiopia. BMC Res Notes. (2018) 11:491. doi: 10.1186/s13104-018-3607-z
7. Wang LL, Wang XC, Pang MF, Hu XQ, Qi XP, Dong XP. The practice of the public health cooperation in the republic of sierra leone: contributions and experiences. China CDC Weekly. (2020) 2:28–31. doi: 10.46234/ccdcw2020.007
8. Lauritsen JM, Bruus M. EpiData (Version 3). A Comprehensive Tool for Validated Entry and Documentation of Data. Odense, Denmark: The EpiData Association (2003–2008).
9. Lauritsen JM, Bruus M, Myatt MA. EpiData (Version 1.0-1.5). A Tool for Validated Entry and Documentation of Data. County of Funen Denmark and Brixton Health UK (2001).
10. Sierra Leone Malaria Indicator Survey. Freetown, Sierra Leone: NMCP, SSL, CRS, and ICF International (2013).
11. Yasuoka J, Kikuchi K, Nanishi K, Ly P, Thavrin B, Omatsu T, et al. Malaria knowledge, preventive actions, and treatment-seeking behavior among ethnic minorities in Ratanakiri Province, Cambodia: a community-based cross-sectional survey. BMC Public Health. (2018) 18:1206. doi: 10.1186/s12889-018-6123-0
12. Balami AD, Said SM, Zulkefli NAM, Norsa'adah B, Audu B. Knowledge, motivation, self-efficacy, and their association with insecticidal net use among pregnant women in a secondary health centre in Maiduguri, Nigeria. Malar J. (2018) 17:359. doi: 10.1186/s12936-018-2518-8
13. Moscibrodzki P, Dobelle M, Stone J, Kalumuna C, Chiu YM, Hennig N. Free versus purchased mosquito net ownership and use in Budondo sub-county, Uganda. Malar J. (2018) 17:363. doi: 10.1186/s12936-018-2515-y
14. Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. (2015) 526:207–11. doi: 10.1038/nature15535
15. Killeen GF, Smith TA, Ferguson HM, Mshinda H, Abdulla S, Lengeler C, et al. Preventing childhood malaria in Africa by protecting adults from mosquitoes with insecticide-treated nets. PLoS Med. (2007) 4:e229. doi: 10.1371/journal.pmed.0040229
16. Kirby MJ, Ameh D, Bottomley C, Green C, Jawara M, Milligan PJ, et al. Effect of two different house screening interventions on exposure to malaria vectors and on anaemia in children in The Gambia: a randomised controlled trial. Lancet. (2009) 374:998–1009. doi: 10.1016/S0140-6736(09)60871-0
17. Killeen GF, Masalu JP, Chinula D, Fotakis EA, Kavishe DR, Malone D, et al. Control of malaria vector mosquitoes by insecticide-treated combinations of window screens and eave baffles. Emerg Infect Dis. (2017) 23:782–9. doi: 10.3201/eid2305.160662
18. Elmardi KA, Malik EM, Abdelgadir T, Ali SH, Elsyed AH, Mudather MA, et al. Feasibility and acceptability of home-based management of malaria strategy adapted to Sudan's conditions using artemisinin-based combination therapy and rapid diagnostic test. Malar J. (2009) 8:39. doi: 10.1186/1475-2875-8-39
19. Thiam S, Thwing J, Diallo I, Fall FB, Diouf MB, Perry R, et al. Scale-up of home-based management of malaria based on rapid diagnostic tests and artemisinin-based combination therapy in a resource-poor country: results in Senegal. Malar J. (2012) 11:334. doi: 10.1186/1475-2875-11-334
20. Ranasinghe S, Ansumana R, Lamin JM, Bockarie AS, Bangura U, Buanie JA, et al. Attitudes toward home-based malaria testing in rural and urban Sierra Leone. Malar J. (2015) 14:80. doi: 10.1186/s12936-015-0582-x
Keywords: malaria, KAP survey, Western Area Rural District, Sierra Leone, national malaria strategic plan
Citation: Wang L, Yin J, Zheng C, Smith SJ, Ngegba E, Huang X, Kamara A, Chen X, Wang X, Luo W and Kan B (2021) A Household-Based Cross-Sectional Survey of Knowledge, Awareness and Practice Regarding Malaria in Western Area Rural District, Sierra Leone. Front. Public Health 9:664971. doi: 10.3389/fpubh.2021.664971
Received: 06 February 2021; Accepted: 25 February 2021;
Published: 18 March 2021.
Edited by:
Tianmu Chen, Xiamen University, ChinaReviewed by:
Hui Liu, Yunnan Institute of Parasitic Diseases, ChinaCopyright © 2021 Wang, Yin, Zheng, Smith, Ngegba, Huang, Kamara, Chen, Wang, Luo and Kan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianhai Yin, eWluamhAbmlwZC5jaGluYWNkYy5jbg==; Canjun Zheng, emhlbmdjakBjaGluYWNkYy5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.