
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 16 March 2021
Sec. Health Economics
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.654822
This article is part of the Research TopicAge-related Diseases Through the Lens of Health EconomicsView all 13 articles
 Erwei Zheng1†
Erwei Zheng1† Jiao Xu1†
Jiao Xu1† Juan Xu2†
Juan Xu2† Xueyun Zeng2
Xueyun Zeng2 Wan Jie Tan3
Wan Jie Tan3 Jinmei Li4
Jinmei Li4 Miaomiao Zhao5
Miaomiao Zhao5 Bo Liu2
Bo Liu2 Rui Liu2
Rui Liu2 Mingjie Sui2
Mingjie Sui2 Zhong Zhang2
Zhong Zhang2 Yang Li1
Yang Li1 Hongbin Yang6
Hongbin Yang6 Hongjuan Yu1,7
Hongjuan Yu1,7 Yongqing Wang2,8*
Yongqing Wang2,8* Qunhong Wu2*
Qunhong Wu2* Weidong Huang2*
Weidong Huang2*Objective: Hypertension is one of the most common public health issues worldwide. However, few existing studies examining health-related quality of life (HRQoL) were conducted on elderly patients with hypertension in China. Hence, this study aimed to assess the HRQoL of elderly patients with hypertension and its influencing factors using EuroQol five-dimensional-three-level (EQ-5D-3L) in China.
Methods: Data were obtained from the 6th National Health Service Survey in Heilongjiang province from June to July 2018, with a stratified multistage random cluster sampling method. All eligible participants were interviewed using a standardized questionnaire, which included the EQ-5D-3L, socio-demographics characteristics, clinical and lifestyle characteristics. The mean EQ-5D index scores for the different subgroups were evaluated using ANOVA. A Tobit regression model was also employed to analyze the potential factors influencing HRQoL.
Results: A total of 705 elderly patients with hypertension were included in this study. The mean EQ-5D utility score was 0.79 [standard deviation (SD) = 0.23]. The proportion of participants reporting pain/discomfort problems was the highest (57.0%), while problems in self-care was the lowest (17.2%). Influencing factors of HRQoL for elderly patients with hypertension included gender, age, income, education level, physical activity, health examination and coexisting diseases. Specifically, the female gender, being above 80 years old, having a lower education and/or higher income, and the presence of coexisting diseases were associated with lower utility index. In contrast, regular physical activity and medical examination had a positive impact on the HRQoL of elderly hypertension patients.
Conclusion: Overall, elderly patients with hypertension in China have a lower HRQoL than the general population. To improve the HRQoL of elderly patients with hypertension, it is imperative that better public health education is provided to enhance the knowledge of hypertension, encourage the adoption of healthy habits such as regular physical activity and medical examination, and improve the management of coexisting diseases. More care should also be directed to males with hypertension who are above 80 years old.
Hypertension is amongst the most common non-infectious chronic diseases. It has been identified as the leading risk factor for mortality, and is ranked third as a cause of disability-adjusted life years (DALYs) worldwide (1–3). It is estimated that up to 9.4 million pre-mature deaths and 92 million DALYs were attributable to hypertension each year (1), and is predicted that by the year 2025, there will be 1.56 billion people with hypertension (4). Likewise, hypertension as a public health challenge is similarly observed in China. A recent large population survey in China revealed that in 2019, ~245 million Chinese adults have hypertension (5). Moreover, hypertension tends to occur more frequently among older adults, where after the age of 69, the prevalence of hypertension rises to one in two individuals (6).
Health-related quality of life (HRQoL) is a concept commonly used in the subjective evaluation of a patient's health status, reflecting the patient's physical, psychological, social and emotional well-being (7, 8). As the HRQoL comprehensively examines the impact of the disease on the patient's life, as well as factors corresponding to their physical and mental health, a growing number of clinicians and policymakers are applying HRQoL in clinical treatment, drug research, preventive health care, health decision-making and health economic evaluation (9, 10). HRQoL can be measured using multi-attribute utility instruments (MAUI), which are divided into two categories: generic instruments and specific disease instruments (8, 11, 12). EuroQol five-dimension (EQ-5D) is one of the most commonly used generic instruments in the world. It has been translated into more than 170 languages and is used to measure the HRQoL of the general population and several patient populations (13). As a preference-based tool, EQ-5D can measure the health state utility (HSU) of the population to estimate the quality-adjusted life years (QALYs) (14). The three-level version of the EQ-5D (EQ-5D-3L) was introduced in 1990 (15). It has demonstrated validity and reliability (16–18), and has been widely used to measure the HRQoL of several medical conditions including hypertensive patients in China (16–25).
Previous studies have examined the relationship between HRQoL and hypertension in elder populations (26, 27). For example, a study in China reported that elderly patients with hypertension have low HRQoL (28). Another study in Vietnam found that advanced age and comorbidity were negatively associated with HRQoL (29). However, most of the studies conducted with Chinese elder population have measured HRQoL using generic instruments comprising of many items, such as the Medical Outcomes 36-Item Short Form Health Survey (SF-36) (30, 31). To date, few studies have evaluated the HRQoL of elderly patients with hypertension in China using well-validated MAUI, such as the EQ-5D.
Therefore, the current study aimed to: (1) estimate the HRQoL of elderly patients with self-reported diagnosis of hypertension, and (2) identify factors of the HRQoL that are associated with hypertension.
Data was extracted from the 6th National Health Services Survey (NHSS) conducted in Heilongjiang, a province located in northeastern China with a population of 38.7 million and a middle-income economy in terms of its gross domestic product per capita (32).
NHSS is a cross-sectional household questionnaire survey conducted in China once every 5 years, and is overseen by the Center for Health Statistics Information. The 6th NHSS was conducted from June to July 2018.
In the 6th NHSS, a multi-stage stratified cluster random sampling method was adopted, involving 6,627 individuals from 3,000 households in five counties/districts, comprising of 25 towns/sub-districts and 50 villages/residential committees. Well-trained interviewers used standardized questionnaires installed on tablets to collect information. Each field site had a survey supervisor who revisited 5% of the participating households to validate the information that was collected (33).
The questionnaire included items on demographic (e.g., age, sex, and ethnicity) and socioeconomic (e.g., residency, marital status, educational attainment, employment, income, housing, and health insurance) data, clinical status (e.g., chronic conditions), and lifestyle (e.g., smoking, alcohol consumption, health examination, and physical activity) of the participants (34). Inclusion criteria for the participants were: (1) having answered “Yes” to the question “Have you been diagnosed with hypertension by a doctor?,” and (2) being 60 years old and above. This resulted in a final sample of 705 participants for the purpose of this study.
The EQ-5D-3L was used as a tool to measure the HRQoL of elderly patients with hypertension in the present study (15). The EQ-5D-3L contains a short health description system questionnaire (EQ-5D descriptive system) and a visual analog scale (EQ-VAS). EQ-VAS is used for respondent's own global rating of their overall health, on a scale from 0 (worst possible health) to 100 (best health possible). The description system of the EQ-5D-3L consists of five health dimensions: “Mobility,” “Self-care,” “Usual Activities,” “Pain/Discomfort,” and “Anxiety/Depression.” Each dimension has three response categories: “no problems,” “some problems,” and “extreme problems.” Thus, the EQ-5D-3L defines a total of 243 (35) health states, with the best heath state indicated by the response “11111” and the worst health state indicated by the response “33333.” In the current study, EQ-5D-3L health states were (33) converted into a single healthy utility index score using a scoring algorithm that is based on the public preferences of the Chinese population (35).
We compared the utility scores of the FCs with those of the local general population norm which were available from a representative sample of the local population in Heilongjiang as part of the fourth National Health Services Survey, involving 15,875 individuals (from 5,530 households) in 13 cities and counties (33). To explore the factors associated with the HRQoL, health utility score of the patient were compared between the different socio-demographic groups (gender, age, area, level of education, marital status, medical insurance, annual household income, and employment status), which have been commonly used in studies on HRQoL of patients with hypertension (21, 26, 36). Consistent with other studies on HRQoL of patients with hypertension (20, 22, 37), comorbidity and lifestyle characteristics, such as smoking status, alcohol consumption, health examination, and physical activity, were also included as these are potential factors associated with HRQoL.
All data analyses were performed using STATA 15.0 software. Statistical significance was defined as p < 0.05. Descriptive statistics were calculated for the basic demographic variables of HRQoL. Mean and standard deviations (SD) were calculated for continuous variables, while frequencies and percentages were calculated for categorical variables. Student t-tests (for two groups) and one-way ANOVA tests (for multiple groups) were used to examine how EQ-5D utility scores may differ on different levels of each variable. All variables tested by the ANOVA-test were entered into the Tobit regression model. Previous studies recommend Tobit regression to deal with data of such a censored nature (38, 39), because they have theoretical advantages over the ordinary least squares estimator (40). In the present study, 34.1% of the respondents had the highest possible score of 1.0. As the EQ-5D utility data was censored, a Tobit regression model was hence employed to identify associated factors of HRQoL among elderly patients with hypertension.
The majority of the elderly patients with hypertension in the sample had the following characteristics: female (54%), rural residents (53.5%), primary school education level (42.35%), covered by medical insurance (95.7%), married (76.6%), and unemployed (47.9%). Respondents were less likely to smoke (74.8%), drink (79.7%), and take a health examination (51.9%). Furthermore, 57.2% of the respondents regularly participate in physical activities (Table 1).
The dimension of the EQ-5D-3L with the highest proportion of elderly patients reporting “no problem” was “self-care” at 82.8%, followed by “anxiety/depression” at 76.9%. As for the dimensions of “usual activities” and “mobility,” the proportion of respondents rating “no problem” were 71.1 and 60.2%, respectively. In contrast, the “Pain/Discomfort” dimension exhibited the lowest proportion of “no problem” responses (43.0%). Overall, a total of 241 participants (34.1%) reported “no problems” in any of the five dimensions (Table 2).
Figure 1 depicts the comparison of the EQ-5D-3L utility scores between elderly patients with hypertension and the general population in Heilongjiang, China. Patients had a significantly lower utility score than the general population (0.79 vs. 0.96, p < 0.001). When classified by gender, the utility score of the patients were also significantly lower than those of their respective counterparts in the general population (p < 0.001).
Lower healthy utility index scores were found among respondents who were older (p < 0.001), lived in urban areas (p = 0.016), had a lower education level (p < 0.001), or were unemployed (p < 0.001). In contrast, higher utility scores were found in hypertensive respondents who drunk (p < 0.001), exercised regularly (p < 0.001), had no comorbidity (p < 0.001), and had a lower income level (p = 0.002). The index scores are described in Table 3.
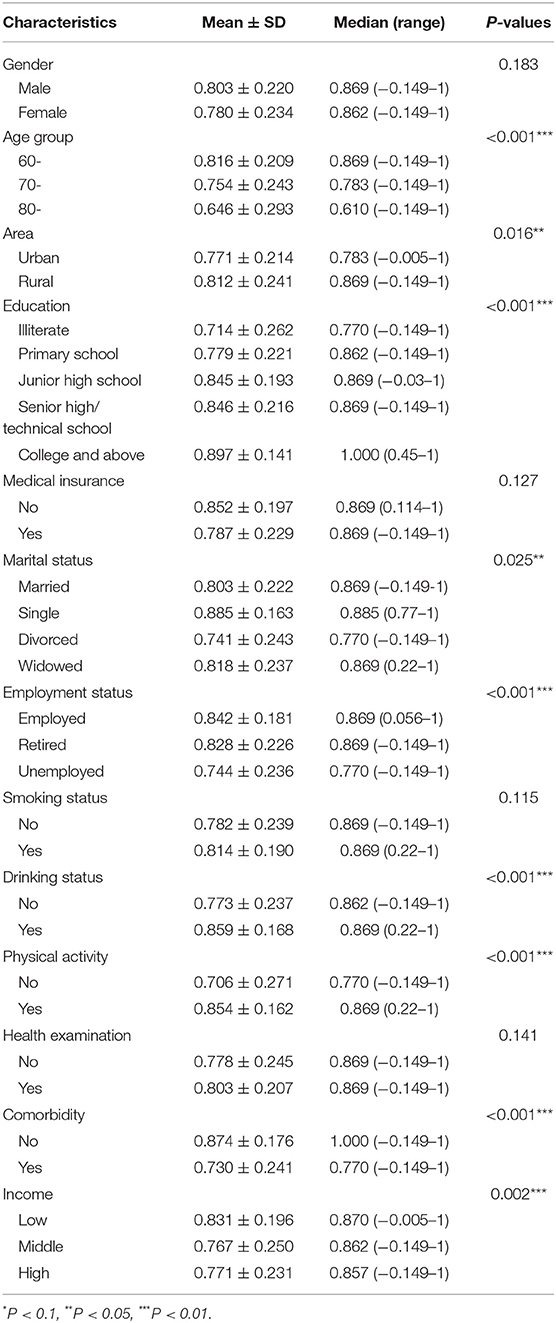
Table 3. EQ-5D-3L health utility index scores on each characteristic of elderly patients with hypertension.
Findings from the Tobit regression model further confirmed that gender, age, education level, physical activity, health examination, comorbidity, and income level were associated with the HRQoL of elderly patients with hypertension (Table 4).
The present study quantified the utility scores of elderly patients with self-reported diagnosis of hypertension, and identified factors that influenced HRQoL using the EQ-5D-3L. To the best of our knowledge, this makes the present study the first of its kind in Heilongjiang province, China.
Findings showed that older adults with hypertension reported significantly more problems in each of the EQ-5D domains and have a lower health utility index than the local general population (33). This indicates that hypertension has an adverse effect on older mainland Chinese. Similar to previous studies, the present study found that the utility score was lower for respondents with hypertension than those without (19–21). Nonetheless, it is important to note that in previous studies, the mean utility score of the respondents with a diagnosis of hypertension were lower [i.e., 0.96 in Yao et al.'s (20), 0.92 in Zhang et al.'s (21), and 0.85 in Liang et al.'s (19) studies] than in the present study. Moreover, current respondents reported more problemsin all five dimensions of the EQ-5D-3L than reported in other studies (20, 21). This may be mainly due to differences in age. Participants in the current study were elderly patients aged 60 years and older, while previous studies included all adults over 18 years old. Moreover, the present study found that the HRQoL of those aged 60 years and above with hypertension gradually decreased with age. It is possible that hypertension is a chronic disease which progresses with age and increasingly affects health (41). The functions and immunity of the body gradually decline with age, and especially in the northeast of China where the winters are cold and long, the elderly people spend less time outside and have lesser physical activity (42). In addition, it is difficult for the elderly with high blood pressure to acquire knowledge on the management of hypertension, especially when information is largely obtained through the Internet in recent times (43).
Likewise, the HRQoL of elderly females with hypertension was also lower compared to their male counterparts in the present study. Similar gender differences in HRQOL of patients with hypertension have been found in Japan and South Korea populations (44, 45). This may be due to variances in social position and opportunities between males and females in different societies. In China, there are the gender inequities in areas such as socioeconomic status (20), education (21), and health (19). Hence, a low HRQoL among elderly females with hypertension would be expected.
The present study also found that patients with higher education levels demonstrated better HRQoL. This is consistent with the findings reported by Andrade et al. (46), Zhang et al. (21) and Saleem et al. (47). A possible explanation for this is that people with higher educational levels tend to have higher levels of health literacy, such as reducing salt intake, quitting smoking, restricting alcohol, and complying with medical advice, which are considered helpful for improving HRQoL (48).
Regular physical exercise is one of the important influencers of HRQoL in elderly people with hypertension, which is consistent with the conclusion of a previous study that utilized the SF-36 (49). Moreover, the HRQoL of patients with hypertension who underwent health examinations in the past year was significantly higher than that of patients who did not. These findings are consistent with the results in a previous study (20). Health management, such as regular physical exercise and medical examination, is beneficial in preventing and treating hypertension. For example, regular physical exercise could promote blood circulation and metabolism, reduce blood pressure, increase fat burning, and body shape maintenance (50). As for regular health examinations, it can help to detect chronic diseases including hypertension at an early stage, and help patients be mindful of their own health, improve their living habits, and pay attention to the prevention and treatment of hypertension and other comorbidities (20).
The present research also confirmed that elderly patients with hypertension and other comorbidities tended to have lower HRQoL, which is consistent with findings of previous studies (19, 20, 28, 51). Patients with hypertension are susceptible to a range of comorbidities, such as myocardial infarction, angina pectoris, stroke, and kidney failure, which is considered as one of main risk factors that reduce HRQoL (52). A previous study found that nearly 20% of the HRQoL scores could be caused by comorbidity, while only 2% of that are due to hypertension (53). It could be postulated that this variance of HRQoL is more serious in elderly patients with hypertension. Therefore, it is essential to consider commodity when evaluating HRQoL among elderly patients with hypertension, and prevent and treat comorbidity that may further decrease HRQoL.
We acknowledge that the current research has the following limitations. First, although the study sample is a regionally representation, findings from the present study may not be generalizable to other geographic areas in China. Second, as the present study utilized a cross-sectional design, it is difficult to ascertain the causal relationship between HRQoL and associated factors. Third, the cases of hypertension included in this study are restricted to those 60 years and above with a self-reported diagnosis of hypertension by a doctor, hence accuracy may be affected.
Overall, elderly patients with hypertension in China have a lower HRQoL than the general population. To improve the HRQoL of elderly patients with hypertension, it is imperative that better public health education is provided to enhance the knowledge of hypertension, encourage the adoption of healthy habits such as regular physical activity and health examination, and improve the management of coexisting diseases. More care should also be directed to females with hypertension who are above 80 years old.
The data analyzed in this study is subject to the following licenses/restrictions: The data and code are available from the corresponding author upon reasonable request. Requests to access these datasets should be directed to weidong218@126.com.
YW, QW, and WH contributed to the conception and design of the study. EZ, JiX, JuX, JL, MZ, BL, RL, MS, ZZ, YL, HYa, and HYu conducted the data reduction and analyses. XZ and WH wrote the manuscript. YW, QW, WH, and WT reviewed the manuscript. All authors read and approved the manuscript before submission.
This research was funded by the National Social Science Foundation of China (Grant No. 71974048, 71603066, and 72004104) and the China Medical Board (CMB-19-308).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/S0140-6736(12)61766-8
2. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
3. Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. (2019) 124:1045–60. doi: 10.1161/CIRCRESAHA.118.313236
4. World Health Organization (WHO). Global Summary of Hypertension. World Health Organization. (2013). Available online at: https://www.who.int/zh/
5. National Cardiovascular Disease Center. Annual report on cardiovascular health and diseases in China 2019. J Cardiovasc Pulm Dis. (2020) 39:14–9. doi: 10.3969/j.issn.1007-5062.2020.10.001
6. Forette A-SRaB. Hypertension in older adults. J Gerontol Med Sci. (2001) 56A:M217–M25. doi: 10.1093/gerona/56.4.M217
7. Carr AJ, Gibson B, Robinson PG. Measuring quality of life is quality of life determined by expectations or experience? BMJ. (2001) 322:1240–3. doi: 10.1136/bmj.322.7296.1240
8. Brazier JE, Yang Y, Tsuchiya A, Rowen DL. A review of studies mapping (or cross walking) non-preference based measures of health to generic preference-based measures. Eur J Health Econ. (2010) 11:215–25. doi: 10.1007/s10198-009-0168-z
9. Pietersma S, van den Akker-van Marle ME, de Vries M. Generic quality of life utility measures in health-care research: conceptual issues highlighted for the most commonly used utility measures. Int J Wellbeing. (2013) 3:173–81. doi: 10.5502/ijw.v3i2.4
10. Efficace F, Osoba D, Gotay C, Sprangers M, Coens C, Bottomley A. Has the quality of health-related quality of life reporting in cancer clinical trials improved over time? Towards bridging the gap with clinical decision making. Ann Oncol. (2007) 18:775–81. doi: 10.1093/annonc/mdl494
11. Devlin NJ, Brooks R. EQ-5D and the EuroQol Group: past, present and future. Appl Health Econ Health Policy. (2017) 15:127–37. doi: 10.1007/s40258-017-0310-5
13. Charro RRaFd. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. (2001) 33:337–43. doi: 10.3109/07853890109002087
14. Payakachat N, Ali MM, Tilford JM. Can The EQ-5D detect meaningful change? A systematic review. Pharmacoeconomics. (2015) 33:1137–54. doi: 10.1007/s40273-015-0295-6
15. Group TE. EuroQol*–a new facility for the measurement of health-related quality of life. Health Policy. (1990) 16:199–208. doi: 10.1016/0168-8510(90)90421-9
16. Zeng X, Sui M, Liu B, Yang H, Liu R, Tan RL, et al. Measurement properties of the EQ-5D-5L and EQ-5D-3L in six commonly diagnosed cancers. Patient. (2021) 14:209–22. doi: 10.1007/s40271-020-00466-z
17. Li L, Liu C, Cai X, Yu H, Zeng X, Sui M, et al. Validity and reliability of the EQ-5D-5 L in family caregivers of leukemia patients. BMC Cancer. (2019) 19:522. doi: 10.1186/s12885-019-5721-2
18. Yu H, Zeng X, Sui M, Liu R, Tan RL, Yang J, et al. A head-to-head comparison of measurement properties of the EQ-5D-3L and EQ-5D-5L in acute myeloid leukemia patients. Qual Life Res. (2020). doi: 10.1007/s11136-020-02644-w
19. Liang Z, Zhang T, Lin T, Liu L, Wang B, Fu AZ, et al. Health-related quality of life among rural men and women with hypertension: assessment by the EQ-5D-5L in Jiangsu, China. Qual Life Res. (2019) 28:2069–80. doi: 10.1007/s11136-019-02139-3
20. Yao Q, Liu C, Zhang Y, Xu L. Health-related quality of life of people with self-reported hypertension: a national cross-sectional survey in China. Int J Environ Res Public Health. (2019) 16:1721. doi: 10.3390/ijerph16101721
21. Zhang L, Guo X, Zhang J, Chen X, Zhou C, Ge D, et al. Health-related quality of life among adults with and without hypertension: a population-based survey using EQ-5D in Shandong, China. Sci Rep. (2017) 7:14960. doi: 10.1038/s41598-017-15083-4
22. Zhang Y, Zhou Z, Gao J, Wang D, Zhang Q, Zhou Z, et al. Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province, China. BMC Health Serv Res. (2016) 16:277. doi: 10.1186/s12913-016-1536-x
23. Huang W, Yang J, Liu Y, Liu C, Zhang X, Fu W, et al. Assessing health-related quality of life of patients with colorectal cancer using EQ-5D-5L: a cross-sectional study in Heilongjiang of China. BMJ Open. (2018) 8:e022711. doi: 10.1136/bmjopen-2018-022711
24. Wang L, Shi J-F, Zhu J, Huang H-Y, Bai Y-N, Liu G-X, et al. Health-related quality of life and utility scores of patients with breast neoplasms in China: a multicenter cross-sectional survey. Breast. (2018) 39:53–62. doi: 10.1016/j.breast.2018.03.004
25. Wang H, Pan Y, Guo C, Li F, Xu R, Liu M, et al. Health-related quality of life among rural residents aged 45–69 years in Hua County, Henan Province, China: results of ESECC trial for esophageal cancer screening with endoscopy. Chin J Cancer Res. (2018) 30:240–53. doi: 10.21147/j.issn.1000-9604.2018.02.07
26. Wong ELY, Xu RH, Cheung AWL. Health-related quality of life in elderly people with hypertension and the estimation of minimally important difference using EQ-5D-5L in Hong Kong SAR, China. Eur J Health Econ. (2020) 21:869–79. doi: 10.1007/s10198-020-01178-9
27. Liu HY, Tsai WC, Chiu MJ, Tang LY, Lee HJ, Shyu YL. Mild cognitive impairment in combination with comorbid diabetes mellitus and hypertension is negatively associated with health-related quality of life among older persons in Taiwan. Qual Life Res. (2019) 28:1281–91. doi: 10.1007/s11136-019-02101-3
28. Wang R, Zhao Y, He X, Ma X, Yan X, Sun Y, et al. Impact of hypertension on health-related quality of life in a population-based study in Shanghai, China. Public Health. (2009) 123:534–9. doi: 10.1016/j.puhe.2009.06.009
29. Huong NT, Ha LTH, Tien TQ. Determinants of health-related quality of life among elderly: evidence from Chi Linh Town, Vietnam. Asia Pac J Public Health. (2017) 29:84S−93S. doi: 10.1177/1010539517704041
30. Wu M, Yang Y, Zhang D, Zhao X, Sun Y, Xie H, et al. Association between social support and health-related quality of life among Chinese rural elders in nursing homes: the mediating role of resilience. Qual Life Res. (2018) 27:783–92. doi: 10.1007/s11136-017-1730-2
31. Wang HCK, Zhou B, Wang JF. Study on social determinants and health-related quality of life among the ‘empty nest' (lonely) elderly Chinese people. Zhonghua Liu Xing Bing Xue Za Zhi. (2010) 31:400–4.
32. Heilongjiang Bureau of Statistics. The 6th National Health Services Survey Plan. (2018). Available online at: http://tjj.hlj.gov.cn/
33. Huang W, Yu H, Liu C, Liu G, Wu Q, Zhou J, et al. Assessing health-related quality of life of Chinese adults in Heilongjiang using EQ-5D-3L. Int J Environ Res Public Health. (2017) 14:224. doi: 10.3390/ijerph14030224
34. National Health Commission of the People's Republic of China. The 6th National Health Services Survey Plan. (2018). Available online at: http://www.nhc.gov.cn/mohwsbwstjxxzx/qgdlcws/lcdc.shtml
35. Liu GG, Wu H, Li M, Gao C, Luo N. Chinese time trade-off values for EQ-5D health states. Value Health. (2014) 17:597–604. doi: 10.1016/j.jval.2014.05.007
36. Saleem F, Hassali MA, Akmal Shafie A, Atif M. Noman ul Haq, Aljadhey H. Disease related knowledge and quality of life: a descriptive study focusing on hypertensive population in Pakistan. Sout Med Rev. (2012) 1:47–52.
37. Theodorou M, Kaitelidou D, Galanis P, Middleton N, Theodorou P, Stafylas P, et al. Quality of life measurement in patients with hypertension in Cyprus. Hellenic J Cardiol. (2011) 52:407–15.
38. Yu H, Zhang H, Yang J, Liu C, Lu C, Yang H, et al. Health utility scores of family caregivers for leukemia patients measured by EQ-5D-3L: a cross-sectional survey in China. BMC Cancer. (2018) 18:950. doi: 10.1186/s12885-018-4855-y
39. Sullivan PW, Ghushchyan VH. EQ-5D scores for diabetes-related comorbidities. Value Health. (2016) 19:1002–8. doi: 10.1016/j.jval.2016.05.018
40. Powell JL. Least absolute deviations estimation for the censored regression model. J Econ. (1984) 25:303–25. doi: 10.1016/0304-4076(84)90004-6
41. Anderson GH Jr. Effect of age on hypertension: analysis of over 4,800 referred hypertensive patients. Saudi J Kidney Dis Transplant. (1999) 10:286–97.
42. Pinto E. Blood pressure and ageing. Postgrad Med J. (2007) 83:109–14. doi: 10.1136/pgmj.2006.048371
43. Jin Y, Jing M, Zhang L, Song S, Ma X. Internet access and hypertension management among the elderly population: a nationally representative cross-sectional survey in China. J Med Internet Res. (2019) 21:e11280. doi: 10.2196/11280
44. Fujikawa A, Suzue T, Jitsunari F, Hirao T. Evaluation of health-related quality of life using EQ-5D in Takamatsu, Japan. Environ Health Prev Med. (2011) 16:25–35. doi: 10.1007/s12199-010-0162-1
45. Lee MH, So ES. Impact of hypertension-related comorbidity on health-related quality of life: a population-based survey in South Korea. Asia Pac J Public Health. (2012) 24:753–63. doi: 10.1177/1010539511431822
46. Andrade JM, Rios LR, Teixeira LS, Vieira FS, Mendes DC, Vieira MA, et al. Influence of socioeconomic factors on the quality of life of elderly hypertensive individuals. Cien Saude Colet. (2014) 19:3497–504. doi: 10.1590/1413-81232014198.19952013
47. Saleem F, Hassali MA, Shafie AA. A cross-sectional assessment of health-related quality of life (HRQoL) among hypertensive patients in Pakistan. Health Expect. (2014) 17:388–95. doi: 10.1111/j.1369-7625.2012.00765.x
48. Trevisol DJ, Moreira LB, Kerkhoff A, Fuchs SC, Fuchs FD. Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens. (2011) 29:179–88. doi: 10.1097/HJH.0b013e328340d76f
49. Martin CK, Church TS, Thompson AM, Earnest CP, Blair SN. Exercise dose and quality of life. Arch Intern Med. (2009) 169:269–78. doi: 10.1001/archinternmed.2008.545
50. Papademetriou V, Kokkinos PF. Exercise training and blood pressure control in patients with hypertension. J Clin Hypertens (Greenwich). (1999)1:95–105.
51. Chin YR, Lee IS, Lee HY. Effects of hypertension, diabetes, and/or cardiovascular disease on health-related quality of life in elderly Korean individuals: a population-based cross-sectional survey. Asian Nurs Res (Korean Soc Nurs Sci). (2014) 8:267–73. doi: 10.1016/j.anr.2014.10.002
52. Bardage C, Isacson DG. Hypertension and health-related quality of life: an epidemiological study in Sweden. J Clin Epidemiol. (2001) 54:172–81. doi: 10.1016/S0895-4356(00)00293-6
Keywords: hypertension, elderly patients, health-related quality of life, EQ-5D-3L, utility score
Citation: Zheng E, Xu J, Xu J, Zeng X, Tan WJ, Li J, Zhao M, Liu B, Liu R, Sui M, Zhang Z, Li Y, Yang H, Yu H, Wang Y, Wu Q and Huang W (2021) Health-Related Quality of Life and Its Influencing Factors for Elderly Patients With Hypertension: Evidence From Heilongjiang Province, China. Front. Public Health 9:654822. doi: 10.3389/fpubh.2021.654822
Received: 19 January 2021; Accepted: 12 February 2021;
Published: 16 March 2021.
Edited by:
Mingsheng Chen, Nanjing Medical University, ChinaReviewed by:
Haipeng Wang, Shandong University, ChinaCopyright © 2021 Zheng, Xu, Xu, Zeng, Tan, Li, Zhao, Liu, Liu, Sui, Zhang, Li, Yang, Yu, Wang, Wu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongqing Wang, wyq.nefu@263.net; Qunhong Wu, wuqunhon@163.com; Weidong Huang, weidong218@126.com
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.