
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health, 07 July 2021
Sec. Public Mental Health
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.613321
This article is part of the Research TopicBioethics Amidst the COVID-19 PandemicView all 24 articles
Background: The rapid spread and uncertain outcome of the 2019 novel coronavirus disease (COVID-19) around the world have caused worry, fear, and stress among the general population. Nevertheless, the prevalence of depression among college students in China during lockdown, following the COVID-19 pandemic, and their coping strategies have not been quantitatively assessed.
Objective: We aimed to evaluate the prevalence of depression among college students in China during the lockdown due to the COVID-19 pandemic and assess their coping strategies.
Methods: Systematic review and meta-analysis were conducted to assess the prevalence of depression among college students in China and their coping strategies.
Results: The results indicated that, during lockdown in the COVID-19 pandemic, the prevalence rates of college students in China suffering from mild, moderate, and severe depression were 25% (95% CI = 17–33%), 7% (95% CI = 2–14%), and 2% (95% CI = 1–5%), respectively. Besides, the proportion of college students who use WeChat and Weibo to acquire COVID-19 knowledge was 39% (95% CI = 13–68%), whereas the proportion of college students using mental health application services (APPs) to deal with depression was 59% (95% CI = 41–73%).
Conclusions: The prevalence of depression among college students in China was high during the lockdown in the COVID-19 pandemic. Thus, considering the adverse outcomes of depression, it is imperative to screen college students in China for depression during the CIVID-19 pandemic and provide them with necessary psychological interventions to control and prevent depression. Social media platforms, such as WeChat and Weibo, and mental health APPs could provide an opportunity for psychological health information dissemination for college students. However, their effectiveness in reducing depression will have to be assessed.
Coronavirus disease (COVID-19) started in Wuhan, one of the biggest cities in China, in 2019 and quickly spread to almost every human settlement on the planet. The outbreak has been particularly severe in the United States, India, and Brazil such that each had more than 2 million cases. According to a report of the World Health Organization (WHO), there were nearly 20 million COVID-19 patients all over the world, and about three-quarters of a million people died from this disease. Although millions of patients have recovered from the disease, their quality of life has been severely affected by different side effects (1). Furthermore, public health measures including social restrictions and quarantines have been adopted by countries to control the spread of COVID-19, and these have also seriously affected the lives of billions of people (2). Some studies have indicated that the outbreak of COVID-19 and the social isolation policies adopted by countries could lead to serious mental health problems in the general population (3, 4).
Specifically, college students in China were seriously affected by the outbreak of COVID-19 in that most of them were confined to the same place during lockdowns, and emerging data have suggested that the COVID-19 pandemic has brought unbearable psychological pressure to many people (5), including college students (6). For example, some studies have confirmed that COVID-19 has caused an increase in anxiety and depression among medical staff (7), while other studies have found that socially isolated college students have higher rates of unhealthy behaviors, such as longer cell phone use (8) and smoking and drinking (9, 10). However, these studies did not quantitatively evaluate the mental health problems of college students amidst the COVID-19 pandemic and the related prevention and control measures. Therefore, quantitative studies, such as meta-analysis, that can provide more valuable information for the improvement of mental health services in colleges are warranted.
Clinically, depression can be classified into mild, moderate, and severe according to the symptoms of the patients, and different levels of depression should receive different mental health services (11, 12). Reasonable treatment measures can effectively alleviate the symptoms of depression; otherwise, lack of appropriate treatment may worsen the patient's state (13). In our previous research (14), we found that many Chinese college students did not have an ideal mental health literacy, and these students could not correctly judge depression and were reluctant to seek professional psychological help.
Students with severe depression should receive timely treatment to reduce their depressive symptoms; otherwise, some of them may decide to commit suicide (15). Some recent studies have suggested that the impact of the epidemic are profound and lasting, possibly leading to higher suicide rates among the population (16, 17), and a survey has shown that the suicide intention of the Chinese population is higher than that in normal times; especially, people aged 18–24 years (college students are in this age range) have a much higher suicide intention during the epidemic (18).
Therefore, this study conducted a meta-analysis of the incidence of depression among college students during the COVID-19 pandemic in China. In this regard, the proportions of mild, moderate, and severe depression among college students were calculated to help authorities provide targeted interventions to college students with different degrees of depression. In addition, a quantitative assessment of the coping styles of college students with depression was conducted, and the role of new information platforms, such as Weibo and mobile application services (APPs), in disseminating knowledge about the prevention and control of the COVID-19 pandemic as well as mental health among college students was evaluated.
Six electronic databases (Web of Science, PubMed, Embase, WanFang, CNKI, and WeiPu) were searched for related studies published not later than July 2020. Furthermore, studies published only in English or Chinese were considered. The search terms included “COVID” OR “COVID19” OR “Coronavirus” OR “SARSCOV2” AND “college students” OR “university students” AND “depression” in the title and/or abstract.
The included studies met the following criteria: (1) they investigated Chinese college students; (2) they were conducted during the COVID-19 outbreak; (3) they examined the emotional or psychological changes in college students; (4) they used valid diagnostic criteria for depression symptoms; (5) they were written in Chinese or English language; (6) they contained the necessary research outcomes needed for this study; (7) depression in this study refers to individuals showing obvious negative emotions such as decreased interest, hopelessness, inferiority, etc. These negative emotions can be evaluated using professional scales.
The following data from eligible studies were independently extracted by two authors: first author, year of publication, study design, research location, sample size, number of college students with varying degrees of depression, assessment tools for depression, coping styles of depressed college students, number of college students who obtained relevant information through electronic social media platforms, and other information.
The main outcome variable for this study was the prevalence of mild, moderate, and severe depression among Chinese college students during the COVID-19 pandemic.
Mild depression was defined as not being interested in many things. In this case, negative emotions do not affect normal work and study. These symptoms last no more than 2 weeks and can be alleviated by talking to family or friends (11, 12).
Moderate depression was defined as negative emotions such as pessimism, low productivity, and inability to fully engage in work and study. These symptoms last more than 2 weeks.
Severe depression was defined as a chronic lack of sleep, suicidal tendencies, and inability to work or study properly. For the classification of depression, this study referred to the International Classification of Diseases (ICD-10); relevant literatures were also reviewed, and the classification was consistent (11, 12).
The secondary objective of this study was to assess the role of new information platforms, such as Weibo and mobile APPs, in disseminating knowledge about the prevention and control of the COVID-19 pandemic as well as mental health among college students.
A mobile APP in this study refers to any mental health APP supported by iPhone and Android systems. Weibo is also called as Microblog, which is a platform based on user relationship information sharing, dissemination, and acquisition; users can form personal communities through various clients, such as Web.
The risk of bias was assessed according to the guidelines of the Cochrane reviews (19). Two authors evaluated the following information: representativeness of sample, consistency of the survey tools, and information integrity. The included studies were graded according to the Newcastle Ottawa Scale, with respect to the above information.
The untransformed proportions (PRAW), log transformation (PLN), logit transformation (PLOGIT), arcsine transformation (PAS), and the Freeman–Tukey double arcsine transformation (PFT) were used to evaluate whether the distribution of the main outcome (rate of depression) conforms to a normal distribution (20). The index that was closest to the normal distribution was selected to perform rate merging. The rate of depression and the corresponding 95% confidence intervals (CIs) were calculated. Heterogeneity was assessed using the I2-test. Accordingly, an I2 > 50% indicated the existence of heterogeneity, and in this case a random model was adopted, whereas an I2 <50% implied low heterogeneity and, hence, a fixed model is adopted (21). In addition, publication bias was evaluated by a funnel plot and confirmed using Egger's test. All statistical analyses were conducted using R version 3.4.4 (R Project for Statistical Computing, Vienna, Austria). Statistical tests were considered significant when P < 0.05.
We first obtained 86 related studies from six electronic databases (Web of Science, PubMed, Embase, WanFang, CNKI, and WeiPu). Of these, 17 were duplicates and so were removed. After screening the titles and abstracts of the remaining studies, 31 were excluded. Furthermore, among the 38 full-text studies left, 27 were ruled out because they did not have the outcomes of interest for this study. Finally, a total of 11 studies (22–32) with 25,020 Chinese college students were included in the present study. The flowchart is schematically shown in Figure 1.
Detailed information about the included studies is shown in Table 1. Ten of the included studies were published in Chinese journals and one in an English journal. In terms of the diagnostic criteria, six studies used the SCL-90 (Symptom Checklist 90) while four studies used PHQ-9 (Patient Health Questionnaire 9) to assess depression symptoms. Samples were selected from different regions of China. Furthermore, the quality of the included literatures is shown in Table 1. In this regard, according to the Newcastle Ottawa Scale, four papers were evaluated to have four points and seven papers have three points.
According to the diagnostic criteria for depression, college students with depression during the COVID-19 pandemic were classified as having mild, moderate, and severe depression (11). Additionally, 10 studies provided information on college students who suffered from mild depression during the COVID-19 pandemic, and the normality test indicated that logit conversion of the original rate was the closest to the normal distribution, so logit conversion was performed on the original rate before merging the rates. The result of heterogeneity indicated that there was significant heterogeneity in this result, so the random model was selected. During the COVID-19 pandemic, about 25% (95% CI = 17–33%) of college students suffered from mild depression (Figure 2). Based on the information in the included literature, the incidence of depression between the sexes was explored, and the results indicated that there was no significant difference between genders [relative risk (RR) = 0.94, 95% CI = 0.82–1.07]. Figure 3 shows the details.
Eight included studies described the prevalence of moderate depression among college students during the COVID-19 pandemic, and this involved 5,000 subjects. The combined results, using a random model, showed that the proportion of college students suffering from moderate depression during the COVID-19 pandemic was 7% (95% CI = 2–14%) (Figure 4).
Furthermore, 10 different studies involving 24,234 college students found that 590 had major depression. The normality test indicated the use of the PFT to perform rate merging; due to significant heterogeneity, the random model was applied. During the COVID-19 pandemic, the combined incidence of severe depression among Chinese college students was 2% (95% CI = 1–5%). Figure 5 shows the details.
The proportion of college students who use WeChat and Weibo to acquire COVID-19 knowledge was 39% (95% CI = 13–68%). Social software (including mobile APPs and public accounts) also played an important role in spreading knowledge of the prevention and control of the pandemic. Our research results showed that about 28% (95% CI = 10–51%) of the college students acquired COVID-19 prevention and control knowledge through the foregoing channel. This proportion is slightly lower than that for social platform users, but higher than that for traditional communication channel users (Figure 6).
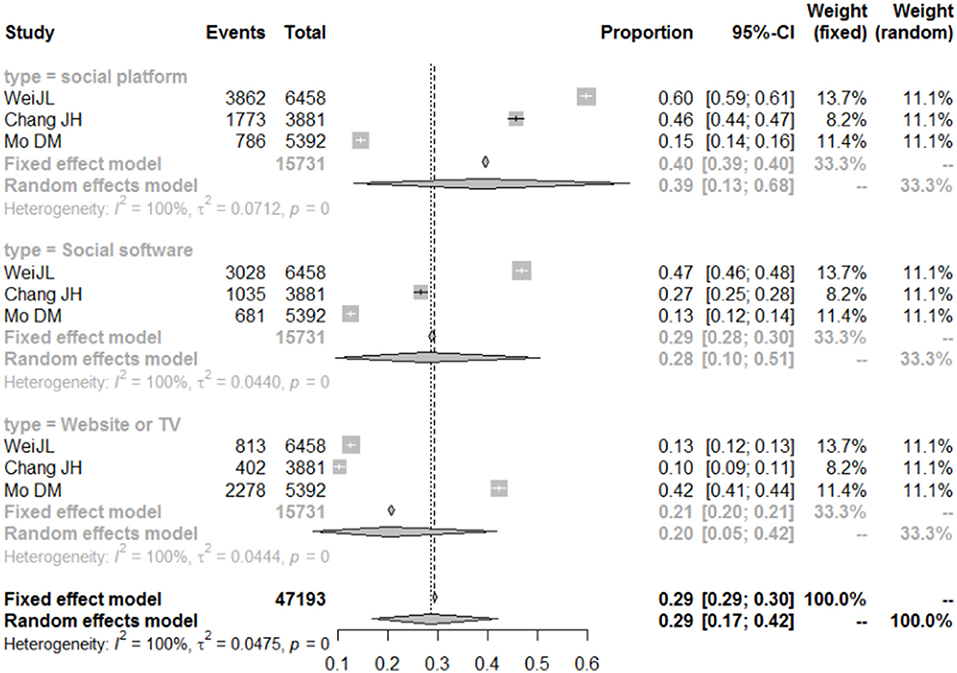
Figure 6. Forest plot of the importance of different information platforms in disseminating COVID-19 knowledge.
During the COVID-19 pandemic, college students in China were in social isolation. Research on college students' coping or seeking help for depression during the isolation period is beneficial for improving the quality of the mental health service system. The results indicated that 70% (95% CI = 51–85%) of the college students sought help from family members when they were depressed.
Moreover, 59% (95% CI = 41–73%) of depressed college students often used mobile phone mental health APPs for help in dealing with depression. Figure 7 shows the details.
The funnel plot is shown in Figure 8. The results of the Eggers test indicated that there was no significant publication bias (t = 0.51, p = 0.616, bias = 1.56, se.bias = 3.06, slope = 0.51), thus justifying the validity and credibility of this meta-analysis.
College students are in a special period of transition from teenagers to adults and have poor ability to adjust and cope with emergencies. Major public events can have negative effects on the psychology of young people, such as SARS in 2003 (33) and the Wenchuan earthquake in 2008 (34). Recently, the COVID-19 pandemic has lasted longer than the preceding events, and social isolation measures have been stricter than those for SARS in 2003 (35). Public health emergencies are strongly stressful situations for individuals; under such circumstances, people will show a lot of abnormal psychology and behavior, such as anxiety, depression, sleep disorders, and physical discomfort (16). Social supports based on social networks can effectively mitigate the impact of the epidemic on affected people. However, due to the restrictions of relevant policies, the function of social networks has been weakened; thus, during the COVID-19 pandemic, some people may commit suicide because they could not stand the strict social isolation policies or due to other reasons (32). A recent study indicated that people aged 18–24 years may have a higher risk of depression and a higher rate of suicidal thoughts than on normal days (18).
The COVID-19 outbreak in China came at a time when college students were in the Spring Festival holiday, and they had to isolate themselves at home for the next 6 months after the outbreak. Previous studies found that the strict social segregation policy may have a negative impact on children's psychology (36), suggesting that revising the policy so as to include psychological intervention measures was necessary.
This study explored the psychological state of college students during lockdown in the COVID-19 pandemic. The results indicated that college students suffered from depression at a higher rate than in normal circumstances, which was consistent with the concerns of some scholars (34, 37).
Specifically, the results of the meta-analysis showed that the proportion of college students with mild depression was 25% (95% CI = 17–33%), those with moderate depression was 7% (95% CI = 2–14%), and those with severe depression was 2% (95% CI = 1–5%). There was no significant gender difference in the incidence of mild depression (RR = 0.94, 95% CI = 0.82–1.07); however, this result may be related to the samples of the included literatures, in which gender parity was not considered when conducting the surveys.
Due to the non-uniform assessment criteria for depression used in the included literatures (there were four assessment criteria, including two questionnaires and two international depression assessment scales), the confidence intervals of the data obtained in this study were relatively wide. However, the results indicated that the COVID-19 pandemic has had a significant negative impact on the mental state of college students. Therefore, in order to reduce the impact of COVID-19 on the mental health of college students, colleges and universities should provide effective mental health services to their students during the COVID-19 pandemic.
Some scholars have conducted studies on the impact of COVID-19 on people's mental state, which recommended that adolescents, including university students, should be provided with effective mental health services to reduce the impact of the epidemic on them (38, 39).
In this study, college students with depression were classified as having mild, moderate, and severe depression according to the diagnostic criteria for depression, suggesting that different interventions should be developed according to the degree of depression in students in order to prevent the aggravation of depressive symptoms.
Thus, although previous studies showed that the COVID-19 pandemic negatively impacted on the healthcare systems in many countries, including mental health services1, it is imperative for college administrators to pay more attention to the mental health of their students in the same way as they do when protecting them from COVID-19.
With regard to help seeking for depression, the results of this study indicated that most depressed students sought help from their families, suggesting that social support, such as family, can play an important role in alleviating depression. Furthermore, about 59% of the depressed college students used mobile phone APPs of mental health category for help in dealing with bad emotions, indicating that these APPs also play an important role in helping depressed college students to cope with their bad emotions. However, the antidepressant effects of these mobile phone APPs were not evaluated in this study. Thus, an evaluation of the effectiveness of these mobile phone APPs in providing mental health services to Chinese college students should be conducted precisely because, although previous studies have confirmed that these APPs may play a role in providing mental health services for early depression, they also have some shortfalls (40). For example, some studies found that some psychological intervention APPs have disadvantages such as excessive disclosure of personal privacy, inappropriate use, and lack of professional psychological intervention content (40). Also, a study examining the effectiveness of a smartphone APP in treating depression found that the exact contribution of the APP in decreasing the depression scores was unclear (41).
In addition, concerning the sources of knowledge for the COVID-19 pandemic, this study found that Weibo, official accounts, and other social media platforms were not only the most important sources of knowledge about the COVID-19 pandemic accessed by Chinese college students but they also played an important role in communication. These results are consistent with the results of related previous studies.
Some limitations should be noted in this study. Firstly, most of the included studies investigated Chinese college students, which may preclude generalizing these results to other non-Chinese college students. Secondly, symptoms of depression were not a predefined outcome, hence may not have been accurately evaluated. Besides, among the included studies, there were different evaluation scales for depression, including PHQ-9, SCL-90, and the National Health Commission questionnaire, which may account for the heterogeneity in the results. Despite the preceding limitations, the present study provides valuable information for psychological interventions aimed at effectively improving the depression symptoms of college students.
The prevalence of depression among college students in China was high during the lockdown in the COVID-19 pandemic. Thus, considering the adverse outcomes of depression, it is imperative that college administrators frequently screen college students in China for depression during the CIVID-19 pandemic and provide them with necessary psychological interventions to control and prevent depression. Social media platforms, such as WeChat and Weibo, and mental health APPs could provide an opportunity for psychological health information dissemination for college students in China. However, their effectiveness in reducing depression will have to be assessed.
SG and JX conceived and designed the analysis and performed the analysis. SG, JX, and AK wrote the paper. All authors contributed to the article and approved the submitted version.
This work was supported by the Education fund of Hunan Province (number: 18B409; http://jyt.hunan.gov.cn/sjyt/xxgk/tzgg/201903/t20190318_5297301.html).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
COVID-19, 2019 novel coronavirus disease; APPs, application service; PHQ-9, Patient Health Questionnaire 9; SCL-90, Symptom Checklist 90.
1. ^Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1
1. Wu C, Hu X, Song J, Yang D, Xu J, Cheng K, et al. Mental health status and related influencing factors of COVID-19 survivors in Wuhan, China. Clin Transl Med. (2020) 10:e52. doi: 10.1002/ctm2.52
2. Usher K, Marriott R, Smallwood R, Walker R, Shepherd C, Hopkins K, et al. COVID-19 and social restrictions: the potential mental health impact of social distancing and isolation for young Indigenous Australians. Austral Psychiatry. (2020) 28:599–600. doi: 10.1177/1039856220943018
3. Kim HHS, Laurence J. COVID-19 restrictions and mental distress among American adults: evidence from Corona Impact Survey (W1 and W2). J. Public Health. (2020) 42:704–11. doi: 10.1093/pubmed/fdaa148
4. Tanne JH. Covid-19: mental health and economic problems are worse in US than in other rich nations. BMJ. (2020) 370:m3110. doi: 10.1136/bmj.m3110
5. Kola L. Global mental health and COVID-19. Lancet Psychiatry. (2020) 7:655–7. doi: 10.1016/S2215-0366(20)30235-2
6. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolescent Health. (2020) 4:421. doi: 10.1016/S2352-4642(20)30109-7
7. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Chin J Ind Hygiene Occup Dis. (2020) 38:E001. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDZHYX&filename=ZHLD202003006&v=SzeRjQZul1%25mmd2FIyOvyH7Khbmd%25mmd2F6nR18dj
8. Yehudai M, Bender S, Gritsenko V, Konstantinov V, Reznik A, Isralowitz R. COVID-19 fear, mental health, and substance misuse conditions among university social work students in Israel and Russia. Int J Mental Health Addict. (2020) 1–8. doi: 10.1007/s11469-020-00360-7
9. Nascimento MDM. Covid-19: U3A students' report on the impacts of social isolation on physical and mental health and access to information about the virus during the pandemic. Educ. Gerontol. (2020) 46:1–13. doi: 10.1080/03601277.2020.1795371
10. Zhang ZH, Nurius P, Sefidgar Y, Morris M, Balasubramanian S, Brown J, et al. How does COVID-19 impact Students with disabilities/health concerns? arXiv (2020). Available online at: https://arxiv.org/ftp/arxiv/papers/2005/2005.05438.pdf
11. Jing L, Xiao-Ling Y. A comparative study of diagnostic criteria of CCMD-3 and DSM-IV on childhood autism. Chin Mental Health J. (2006) 1032:560–70. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2006&filename=ZXWS200609001&v=cdDlzovbDRa5Jb%25mmd2B5ZbxX2JIhZioe2AA%25mmd2BytAb8J2xkIoVrk47Hl%25mmd2FhmZa8Ib8y7o6M
12. Huang SH, Lependu P, Iyer SV, Tai-Seale M, Carrell D, Shah NH. Toward personalizing treatment for depression: predicting diagnosis and severity. J Am Med Informatics Assoc. (2014) 21:1069–75. doi: 10.1136/amiajnl-2014-002733
13. Hallensleben N, Glaesmer H, Forkmann T, Rath D, Strauss M, Kersting A, et al. Predicting suicidal ideation by interpersonal variables, hopelessness and depression in realtime. An ecological momentary assessment study in psychiatric inpatients with depression. Euro Psychiatry. (2019) 56:43–50. doi: 10.1016/j.eurpsy.2018.11.003
14. Guo S, Yang Y, Liu F, Li F. The awareness rate of mental health knowledge Among Chinese adolescent: a systematic review and meta-analysis. Medicine. (2020) 99:e19148. doi: 10.1097/MD.0000000000019148
15. Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: differences in psychosocial functioning. J Consult Clin Psychol. (1995) 63:90. doi: 10.1037/0022-006X.63.1.90
16. Xu H. Meta analysis on antibody positive conversion rate of domestic and imported mumps vaccines. Disease Surv. (2013) 28:288–93. doi: 10.3784/j.issn.1003-9961.2013.4.011
17. Klomek AB. Suicide prevention during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:390. doi: 10.1016/S2215-0366(20)30142-5
18. Shi L, Que J, Lu Z, Gong Y, Liu L, Wang Y, et al. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur Psychiatry. (2021) 64:e18. doi: 10.1192/j.eurpsy.2021.5
19. Abdelsattar M, Krauth D, Anglemyer A, Bero L. Risk of bias meta-analysis data. Dryad. (2015) 11. doi: 10.5061/dryad.4c2bj
20. Wei JL. Psychological Problems of College Students and their Response to COVID-19 epidemic. J Multimedia Netw Teach China. (2020) 7:217–9.
21. Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stats Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
22. Yujie Z, Mengjie LI. Analysis on the mental health status of College Students in Wuhan during the CoVID-19 epidemic. Modern Commerce Trade Industry. (2020) 41:52–3.
23. Minjiang D, Chunfu H. Study on the influence of COVID-19 epidemic on college students' psychological behavior. J Huaihai Inst Technol. (2020) 18:129–40. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2020&filename=HHGX202002017&v=hlnnj7822w94h6qjJRgw3z5BfIzaJmaPryRIg1%25mmd2FFBuDjO09RXdS%25mmd2FTRtz8pKHXSqu
24. Wei JL. Psychological Problems of College Students and their Response to COVID-19 epidemic. J Multimedia Netw Teach China. (2020) 7:217–9. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2020&filename=DMWJ202007084&v=3lwqNCZmxSWZX4hFhdYhtdbu32llt5VGET09%25mmd2BzX53YUQbwh955i1iwjMPGUrG2ul
25. Ma L, Wang X, Liao QY. Effects of COVID-19 stress events on college students' mental health. Health Res. (2020) 40:258–60.
26. Liu Dan. Investigation on mental health status of vocational college students under COVID-19 epidemic and research on countermeasures – a case study of 553 students in a Vocational College. Psychol Monthly. (2020) 15:51–5. doi: 10.19738/j.cnki.psy.2020.17.016
27. Wang DX, Cai YN, Wang LN, Zhou YQ, Zhang H. Investigation on psychological distress and psychological help of home-based college students in the context of COVID-19 epidemic and analysis on psychological adjustment strategies. Psychol Monthly. (2020) 15:37–9. doi: 10.19738/j.cnki.psy.2020.17.011
28. Chang JH, Yuan YX, Wang D. Analysis on the college students under the coVID-19 epidemic. J South Med Univ. (2020) 40:171–6. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2020&filename=DYJD202002007&v=qRb6AzusgQkcHRj6NFA%25mmd2BqKVGFPPZGVzjBhVgbjjsSNc2rMmr3sgEk%25mmd2B6cPArq0S%25mmd2BX
29. Ma L, Wang X, Liao QY. Effects of COVID-19 stress events on college students' mental health. Health Res. (2020) 40:258–60.
30. Cao W, Fang Z, Hou G, Han M, Xu XR, Deng JX, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
31. Daming M, Junwei Y, Xin L. Prevalence rate and related influencing factors of anxiety disorder in children and adolescents during the outbreak of COVID-19. Sichuan Mental Health. (2020) 33:202–6. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2020&filename=WANT202003003&v=IxjK2WkV%25mmd2F%25mmd2Bh4%25mmd2FjThiZDhqQepLb8UiMxF1gpD%25mmd2BeoNbXzL1GMFNKUGVrOCo3wVzuWC
32. Tagupa H. Social isolation, loneliness, and hearing loss during COVID-19. Hear J. (2020) 73:46–7. doi: 10.1097/01.HJ.0000666456.65020.b9
33. Sufang L, Jiandong M, Ping W. The Mental State of Medical College Student during the Period of SARS Diffusion. Heath Psychol J. (2004) 2:117–20.
34. Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students mental health in the US: interview-survey study. J Med Internet Res. (2020) 22:e21279. doi: 10.2196/21279
35. Wan NC, Tan CW, Foo R, Kang AEZ, Wang LF. Serological differentiation between COVID-19 and SARS infections. Emerg Microbes Infect. (2020) 9:1–23. doi: 10.1080/22221751.2020.1780951
36. Miranda DMD, Athanasio BDS, Oliveira ACS, Simoes-E-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disas Risk Reduct. (2020) 2:10945–7. doi: 10.1016/J.IJDRR.2020.101845
37. Seidel EJ, Mohlman J, Basch CH, Fera J, Ethan D. Communicating mental health support to college students during COVID-19: an exploration of website messaging. J Community Health. (2020) 43:1259–62. doi: 10.1007/s10900-020-00905-w
38. Restauri N, Sheridanmd AD. Burnout and PTSD in the COVID-19 Pandemic: Intersection, Impact and Interventions. J Am College Radiol. (2020) 17:921–6. doi: 10.1016/j.jacr.2020.05.021
39. Ríos-Barnés M, Lanaspa M, Noguera-Julian A, Baleta L, Fumadó V. The spectrum of COVID-19 disease in adolescents. Arch Bronconeumol. (2020) 57:84–5. doi: 10.1016/j.arbres.2020.08.016
40. Kenny R, Dooley B, Fitzgerald A. Developing mental health mobile APPs: exploring adolescents' perspectives. Health Informatics J. (2014) 22:265–75. doi: 10.1177/1460458214555041
Keywords: COVID-19, depression, college students, meta-analysis, mental health apps
Citation: Guo S, Kaminga AC and Xiong J (2021) Depression and Coping Styles of College Students in China During COVID-19 Pandemic: A Systemic Review and Meta-Analysis. Front. Public Health 9:613321. doi: 10.3389/fpubh.2021.613321
Received: 02 October 2020; Accepted: 17 May 2021;
Published: 07 July 2021.
Edited by:
Asem H. Mansour, King Hussein Cancer Center, JordanReviewed by:
Richa Tripathi, All India Institute of Medical Sciences Gorakhpur, IndiaCopyright © 2021 Guo, Kaminga and Xiong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Xiong, em5keHhobEAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.