
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 13 July 2021
Sec. Public Health Policy
Volume 9 - 2021 | https://doi.org/10.3389/fpubh.2021.580585
This article is part of the Research Topic Strengthening Health System and Community Responses to Confront COVID-19 Pandemic in Resource-Scare Settings View all 27 articles
Introduction: Hypoxia is the main cause of morbidity and mortality in COVID-19. During the COVID-19 pandemic, some countries have reduced access to supplemental oxygen, whereas other nations have maintained and even improved access to supplemental oxygen. We examined whether variation in the nationally determined oxygen guidelines had any association with national mortality rates in COVID-19.
Methods: Three independent investigators searched for, identified, and extracted the nationally recommended target oxygen levels for the commencement of oxygen in COVID-19 pneumonia from the 29 worst affected countries. Mortality estimates were calculated from three independent sources. We then applied both parametric (Pearson's R) and non-parametric (Kendall's Tau B) tests of bivariate association to determine the relationship between case fatality rate (CFR) and target SpO2, and also between potential confounders and CFR.
Results: Of the 26 nations included, 15 had employed conservative oxygen strategies to manage COVID-19 pneumonia. Of them, Belgium, France, USA, Canada, China, Germany, Mexico, Spain, Sweden, and the UK guidelines advised commencing oxygen when oxygen saturations (SpO2) fell to 91% or less. A statistically significant correlation was found between SpO2 and CFR both parametrically (R = −0.53, P < 0.01) and non-parametrically (−0.474, P < 0.01).
Conclusion: Our study highlights the disparity in oxygen provision for COVID-19 patients between the nations analysed. In those nations that pursued a conservative oxygen strategy, there was an association with higher national mortality rates. We discuss the potential reasons for such an association.
SARS-CoV2 causes COVID-19 (Coronavirus Disease 2019). As of May 2020, the total reported cases of COVID-19 were over 5 million, with 350,000 deaths over 5 months (1). More than half these deaths have occurred in the last month. Whilst there has been a slight reduction in the rate of growth for new infections globally, this is most likely due to strict infection control policies (e.g., case isolation, social distancing, and “lockdown”) (2). With the seroprevalence of SARS-CoV2 being reported as between <1 and 22% (3), it is most likely the majority of infections are yet to come, and the rate of infections will once again increase as infection control measures are balanced with economic pressures.
The true COVID-19 mortality rate is difficult to ascertain during the outbreak. Background infections, asymptomatic infections, testing criteria, reporting of fatalities, and the time lag between new cases and outcome are all potential confounders (4). This makes measuring the effects of national interventions difficult. It is reasonable, however, to expect that a nation's COVID-19 mortality rate will depend on access to healthcare and likely will also depend on the type of healthcare offered. The need for effective healthcare can be reasonably inferred from the marked disparity between mortality rates during a surge of cases vs. mortality post-surge (5).
Oxygen is a cornerstone of treatment for patients with COVID-19 pneumonia. Indeed, the major mechanism for injury and death in COVID-19 relates to hypoxia (6). It has been established that a delay in identifying and correcting hypoxia in pneumonia leads to increased disease severity, increased rate of mechanical ventilation, and increased mortality (7, 8). Whilst there are no controlled studies in COVID-19 specifically examining duration spent hypoxic and subsequent disease burden and mortality, Sun et al. have reported a reduction in the need for mechanical ventilation where hypoxia was detected and corrected early in patients with COVID-19 (9).
In relation to conservative oxygen strategies generally, there are four key mortality studies. The IOTA meta-analysis published in 2018 examined conservative vs. liberal oxygen strategies across a range of studies. None of the studies analysed related to pneumonia, and the majority of studies examined oxygen as a treatment not as a means to correct hypoxia. The authors suggest that optimal target oxygen saturations (SpO2) for all acute medical patients “might” be 94–96% (10).
Since the IOTA study, there have been three clinical studies, two of which were randomised controlled trials (RCTs), examining the mortality effect of conservative oxygen strategies. The ICU-ROX trial suggests that there may be no mortality effect at the higher target levels of SpO2 (actual mean SpO2 96–97% vs. 95–96%) in mechanically ventilated patients from any cause (n = 1,000) (11). Another, a retrospective analysis, published in March 2020 examined over 35,000 intensive care patients and found the optimum SpO2 target of 94–98%. The authors note that patients who were in the optimal range for only 40% of the time had nearly twice the mortality of those who spent 80% of the time within the optimal target, even after correction for disease severity (12).
The most recent RCT, and the most well-controlled study of true conservative oxygen strategies to date (and the most relevant to COVID-19), examined 204 patients with acute respiratory distress syndrome (ARDS). Patients were randomised to either a conservative arm (actual SpO2 of 92–93%) vs. a liberal arm (SpO2 of 95–97%) and then followed up for 90 days. The study was halted early due to excessive deaths in the conservative oxygen group. In those patients with ARDS who were managed with a conservative oxygen strategy, there was a 27% increase in intensive care deaths and a 50% increase in 90-day mortality (13).
Despite the critical nature of oxygen therapy in COVID-19 pneumonia, there remains a marked variation between national guidelines for when to offer supplemental oxygen. Many nations seem to have implemented conservative oxygen strategies during the pandemic, effectively limiting the access of patients to supplemental oxygen. Others seem to have actively increased their capacity to offer supplemental oxygen for patients with COVID-19 pneumonia. Here, we examine the national guidelines from 29 nations to ascertain whether the national decision to promote a “conservative” oxygen strategy has any relationship to that nation's case fatality rate (CFR).
We followed the advice for global reporting on health estimates as per the GATHER statement (14). All countries with more than 20,000 cases as of May 18, 2020, were assessed. Three investigators (DG, AK, and HD) independently identified the specific national recommendations for the target SpO2 to commence oxygen in patients with COVID-19. Two investigators (AK and HD) were blinded as to the reason for the study. Each nation's ministry of health, national guideline bodies, respiratory medicine bodies, and national health service were searched for relevant COVID-19 clinical guidelines. The European Society of Respiratory Medicine (15) was a useful resource with direct links to a number of COVID-19-specific clinical guidelines from across the world. Literature databases were also used as a means of identifying links to national guidelines. If guidelines were not available in one of the languages spoken by the investigators, online translation services were utilised, specifically for guidelines on “supplemental oxygen” or “oxygen therapy”—the entire guideline was not translated. Note, only guidelines applicable to the majority of the population were extracted, and guidelines for patients with underlying conditions such as chronic obstructive airways disease were not recorded.
If guidelines were unclear, instruction was to disregard the country from further analysis. Where there was more than one recommendation, the investigator made a determination as to the most likely guideline to be followed (Figure 1). Where there was divergence between the three investigators, the consensus value was used. Results were tabulated and compared.
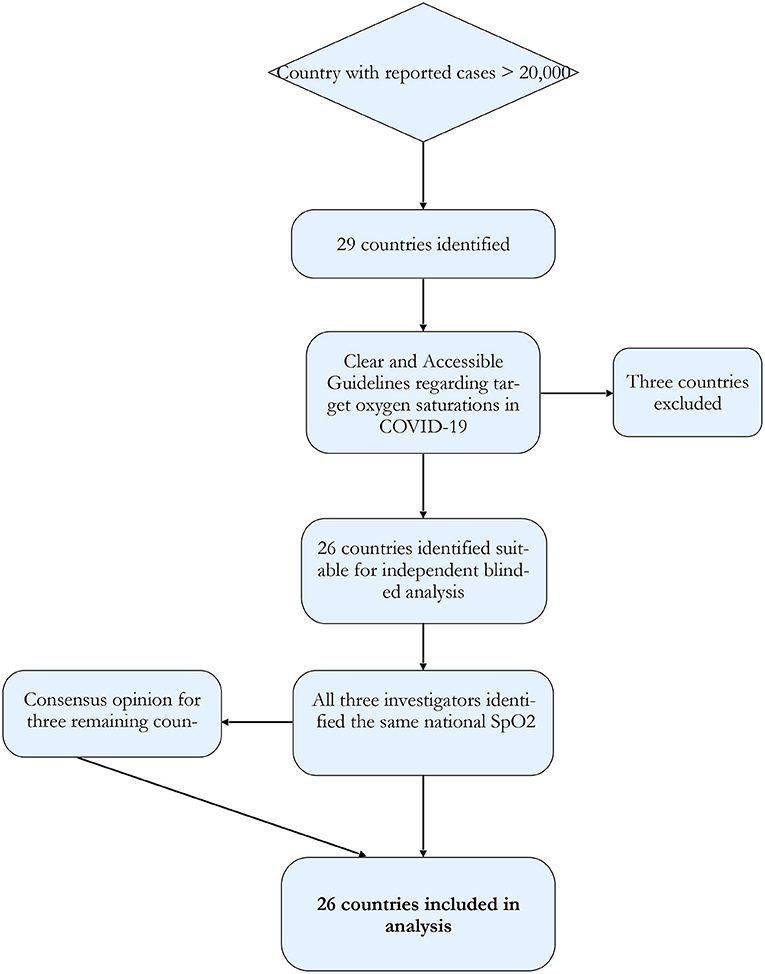
Figure 1. Study protocol flowchart. Using the WHO situation report countries with case numbers over 20,000 were selected. These countries were subjected to analysis via three different, independent investigators for the ascertainment of nationally recommended target oxygen saturations.
CFR is the percentage ratio of deaths to total cases. It is a crude figure privy to a number of potential confounders. For most nations, it is likely to be numerically incorrect (4). CFR, however, is likely to maintain a relationship to actual infection mortality rate (IFR) (3, 4) and as such was used in this study. CFR was calculated and cross-referenced from three different sources—The WHO, John Hopkins University, and Worldometer. There was no significant difference between the calculated CFR across the three sources.
All statistics were performed using SPSS. Both parametric (Pearson's R) and non-parametric (Kendall's Tau B) tests of bivariate association were performed to identify and characterised a potential trend between CFR and target SpO2, as given the small sample size it was not clear whether the assumptions of linearity, homoscedasticity, and normality of variables were met. Kendall's Tau B was used as the test of non-parametric bivariate association as there were ties in both CFR and SpO2, which are problematic for Spearman's Rho.
Scatter plots with linear regression lines of best fit are also given, as well as the y-intercept and gradient of these lines reported. Means and standard errors of CFR, SpO2, and confounding variables are given.
In total, there were 29 countries with a total case number over 20,000 on May 18, 2020. Of those, 26 countries had accessible clinical guidelines referring to target oxygen levels for the commencement of supplemental oxygen in COVID-19. UAE (United Arab Emirates) was excluded from further analysis as the national guidelines advised (at page 9) admitting all patients with COVID-19 to hospital, and commencing oxygen when “needed” (16). The Netherlands and Belarus were also excluded due to all three investigators failing to find clear national guidelines regarding oxygen targets.
Of the remaining 26 countries, there was concordance between all three investigators identifying the same national target oxygen levels in 23 countries. Of the remaining three countries (UK, Pakistan, and Qatar), determination of national target SpO2 in COVID-19 was made by consensus. For links to national guidelines, see Supplementary Material.
Of the 26 nations analysed, six recommended commencing oxygen if SpO2 fell to below 95% (Singapore, Peru, Switzerland, Ireland, Qatar, and Pakistan), five made recommendation for below 94% (Saudi Arabia, Chile, Brazil, India, and Russia), five for below 93% (Portugal, Iran, Turkey, Bangladesh and Italy), six for below 92% (Canada, Belgium, France, UK, USA, and China), and four for below 91% (Germany, Mexico, Spain, and Sweden). CFR ranged from 0.06% (Qatar) to 16.4% (Belgium). A statistically significant correlation was found between SpO2 and CFR both parametrically (R = −0.53, P < 0.01) and non-parametrically (−0.474, P < 0.01), and no statistically significant correlation was found with the potential confounders analysed here. A scatter graph with the linear best-fit line is shown in Figures 2, 3A.
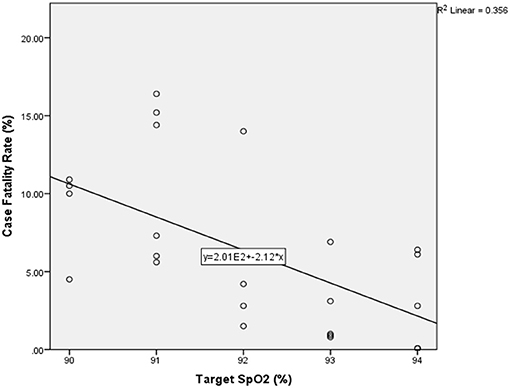
Figure 2. Scatter graph of national target oxygen saturations vs. national case fatality rate with best fit linear line (n = 26). SpO2–oxygen saturations.
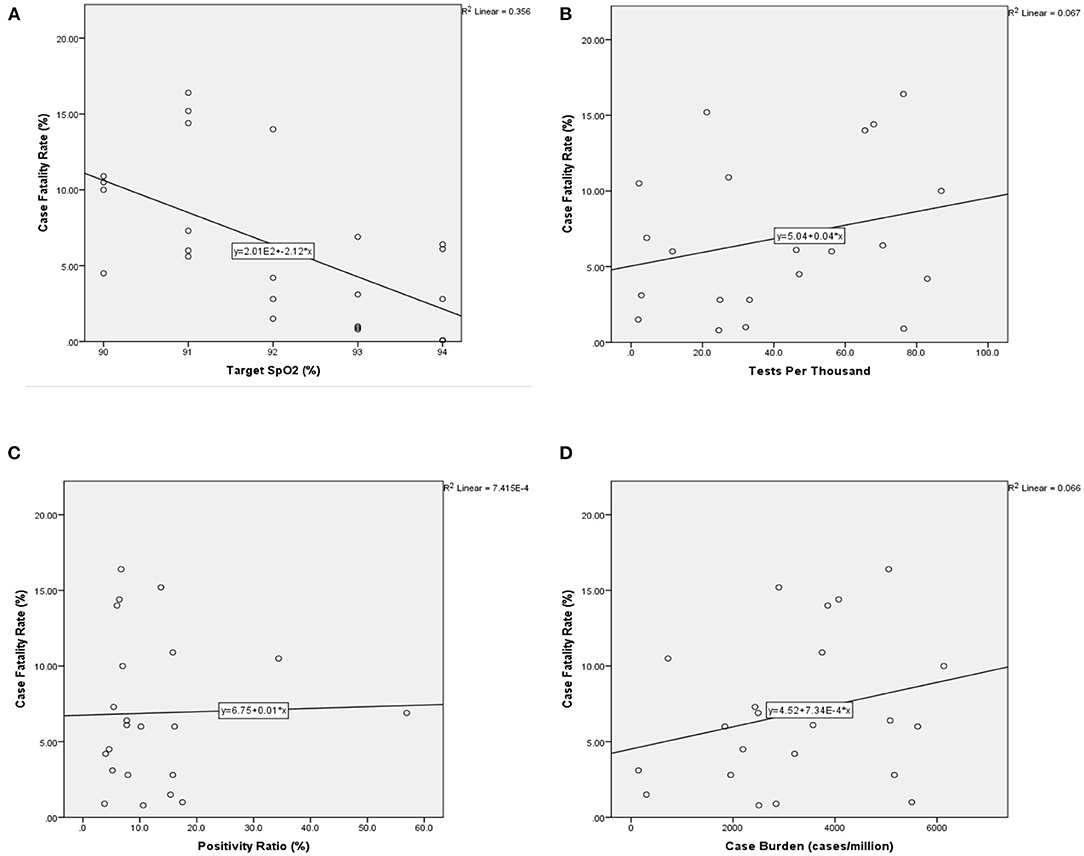
Figure 3. Scatter graphs with best-fit line for primary measure and confounders vs. CFR (N = 26). CFR is along the vertical axis in each and measured as percentage ratio. (A) Comparison of national CFR vs. nationally recommended target SpO2 (%) in COVID-19. (B) CFR vs. burden of cases measured by total number of cases per million inhabitants. (C) CFR vs. Testing Rate measured by total number of tests undertaken per thousand inhabitants (tests/thousand). (D) CFR vs. the overall positivity ratio (%), measured as the percentage ratio of positive tests to total tests. CFR, case fatality rate; SpO2, oxygen saturations. CFR, case fatality rate; SpO2, oxygen saturations.
National guidelines for target saturations were relatively clear for most countries. Together with the high rate of consensus amongst investigators, it seems unlikely that investigator bias was a significant factor. The main confounders are more likely to stem from the many variables associated with CFR.
We found no correlation between CFR and cases/million inhabitants (Figure 3B), or tests/thousand inhabitants (Figure 3C), or overall positivity rate (Figure 3D), suggesting that the testing strategy between the countries examined did not have a significant visible relationship with our mortality measure, CFR (Table 1). We could not examine the potential impact of national-level reporting bias on the CFR from the data available.
National guidelines for when to commence supplemental oxygen in patients with COVID-19 varied significantly between the countries examined. Combined, the target SpO2 for the commencement of oxygen and target SpO2 for ongoing treatment varied from 90% to 98%. There are a number of potential reasons for the variation in oxygen policies between countries and the association with mortality.
Based on the design of the study, a causal relationship between national oxygen targets and national CFR cannot be determined. However, our analysis did reveal an association between national target oxygen saturations and national CFR—the lower the national target oxygen saturations, the higher the national CFR. One possible explanation for the identified relationship is that the national guidelines have been followed and implemented, and it is the lower oxygen levels during COVID-19 pneumonia that has led to an increased mortality.
Based on our current understanding of the effects of hypoxia on inflammation (17) and coagulation (18), there is good scientific basis for the increased mortality associated with suboptimal oxygen strategies and/or a delay in correcting hypoxia. There are direct effects of hypoxia leading to increased mortality, such as cardiac arrhythmias and ischemia-related pathologies [as identified in the aforementioned ARDS study (13)]. It is also quite plausible, indeed quite likely, given that hypoxia is pro-inflammatory, the delay in correcting hypoxia leads to more severe disease. This of course raises the possibility that rationing, or a conservative oxygen approach, or a failure to provide access to supplemental oxygen in COVID-19 pneumonia, actually increases healthcare burden and resource consumption (19).
The presence of “silent hypoxia”—low oxygen levels without respiratory distress—is likely to compound the mortality effect of reduced access to supplemental oxygen. A fall below normal SpO2 (95% or less) indicates progression of COVID-19 to pneumonia or pneumonitis. If sent home at this stage despite evidence for disease progression, around one-third of patients will be unaware of their own deterioration and therefore will either fail to re-present and demise at home, or will present even later (20). This will almost certainly add greater pressure on ICU facilities and increase morbidity and mortality. Conservative oxygen strategies are questionable at the best of times (19); with COVID-19, such strategies likely carry even greater harm. Optimal oxygen strategies have the additional benefit of identifying and observing these at-risk “silent hypoxia” patients.
An alternative explanation for the relationship between national oxygen targets and mortality is that the recommendation to conserve oxygen simply reflects the resource limitations of the nation, and it is this resource limitation that causes an increase in mortality. For example, the UK directive to ration oxygen supply in April 2020 reduced the normal national target for the commencement of oxygen from SpO2 of 94% to a new value of 91%. The reason for rationing was related to the surge of infections and subsequent concern over the supply of oxygen (21). If such practises are common in other nations, the relationship between national guidelines' SpO2 and national CFR identified here may be a representation of the demands on healthcare during a surge of COVID-19 cases.
There are a number of reasons why mortality increases during a surge of infections. Patients are less likely to attend hospital or seek medical care, for fear of either contracting COVID-19 or overburdening their health service (22). Triage systems during a surge can be set with high thresholds for onward referrals (23). Another mortality factor is a potential lack of resources both staff and consumables. The overall delay to treatment that ensues prevents early correction of hypoxia, implementation of VTE (venous thromboembolism) prophylaxis, readjustment of medications (e.g., nephrotoxics) and the detection of secondary bacterial infection, and thus a likely increased mortality (24).
So then, the association between target SpO2 and CFR identified here may be more related to target SpO2 being an indicator of an overwhelmed healthcare service.
The issuing of national guidelines recommending lower target oxygen saturations than would be typical for viral pneumonias (25) may relate more to the overall approach of a national response to COVID-19, and as such, it is this “national approach” that relates to mortality rate.
All three investigators noted the quite different approaches between nations, as set out in their national guidelines. Some followed a “stay home” approach, whereas others defaulted to clinical assessment of patients either with COVID-19 or with any risk factor associated with it. For example, Singapore guidelines default to clinical assessment (26), whereas a country with a similar prevalence burden, the UK, has much higher thresholds for referral onward for assessment (27) (Table 2).
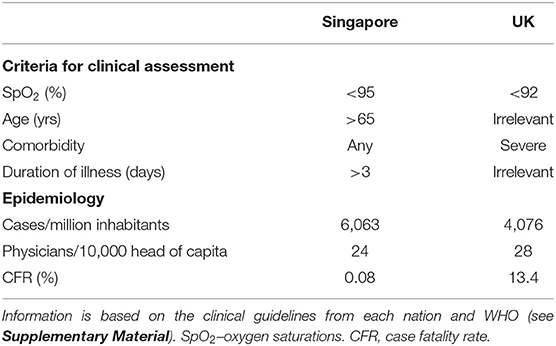
Table 2. Comparison of the criteria for assessment in suspected or confirmed COVID-19 between Singapore and the UK.
In this situation, where the national guideline target SpO2 is part of an overall strategy of avoiding admissions, then whilst it does remain possible that conservative oxygen approaches do contribute to higher mortality, it may be the contribution of other policies to avoid admissions that leads to an increased CFR. In the UK vs. Singapore example, a target SpO2 of <92% is likely to be harmful, but equally, failing to account for age of the patient or duration of fever may also be harmful. As such, the relationship identified here between CFR and target SpO2 may be more a relationship between CFR and national strategy; target SpO2 may be more of an indicator of national policy.
This study highlights the variation in national guidelines for when to commence supplemental oxygen in patients with COVID-19. In of itself, this raises important questions as to the optimal response to COVID-19. Attempting to delineate the interventions and strategies that are potentially beneficial between nations is difficult without using a mortality estimation, which carries inherent confounders. CFR depends on many factors, not least of which is the accurate reporting of COVID-19-related deaths. Whilst we found no correlation between CFR and rates of testing or crude case burden, we could not account for disparities in reporting of deaths, nor did we analyse for differences in the age of the population, nor the socioeconomic status of the infected population.
We undertook an analysis of the national guidelines using three independent investigators. The consensus amongst the investigators supports the accuracy of the target SpO2 extracted. The possibility remains that localities within a country, or individual doctors and nurses, chose not to follow their national guidelines. Even if such local differences were significant, the national guidelines permit not implementing oxygen therapy until the target oxygen level is reached; therefore, triage systems, nurses, and physicians can avoid admissions and thus limit access to supplemental oxygen. Despite the prospect of local variations in following the guidelines, the presence of the guidelines will shape and likely reflect practise nationally.
Utilising patient-specific data from cohorts from the nations analysed here would provide greater insight into whether target oxygen saturation guidelines are both being followed and having a direct impact on mortality. A further follow-up study utilising patient-specific data could help determine whether the relationship identified here is in fact causal. It would also be useful to undertake further analysis into the cost-effectiveness of increasing access to supplemental oxygen vs. expanding intensive care facilities—could more lives be saved by treating more cases earlier and with optimum oxygen targets?
There is clear disparity between national guidelines for target oxygen saturations (SpO2) in COVID-19 across the countries analysed here. Those nations that implemented a lower target oxygen level for when to commence oxygen in patients with COVID-19 had a significantly higher CFR. Whilst there are multiple confounders to the CFR, the overall relationship between increasing CFR with a decreasing target SpO2 warrants further investigation.
As it stands currently, our results support the position that managing COVID-19 pneumonia should not differ from the management of other pneumonias (24), insomuch as access to supplemental oxygen delivered optimally is necessary to prevent excessive mortality.
Publicly available datasets were analysed in this study. This data can be found at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200518-covid-19-sitrep-119.pdf?sfvrsn=4bd9de25_4.
DG and FM initially conceived of the study. HD, AK, JN, and SB contributed further to the conception and/or design of the study and contributed to the manuscript. DG, HD, and AK conducted the analysis of the national guidelines. Statistical analysis was undertaken primarily by JN. FM and DG wrote the majority of the manuscript. All contributors reviewed the final manuscript before submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.580585/full#supplementary-material
1. WHO Situation Report 119. (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200518-covid-19-sitrep-119.pdf?sfvrsn=4bd9de25_4 (accessed May 20, 2020).
2. Okell LC, Verity R, Watson OJ, Mishra S, Walker P, Whittaker C, et al. Have deaths from COVID-19 in Europe plateaued due to herd immunity? Lancet. (2020). 395:e110–1. doi: 10.1016/S0140-6736(20)31357-X
3. Ioannidis J. The infection fatality rate of COVID-19 inferred from seroprevalence data. medRxiv. (2020) 99:19–33F. doi: 10.1101/2020.05.13.20101253
4. Battegay M, Kuehl R, Tschudin-Sutter S, Hirsch HH, Widmer AF, Neher RA. 2019-novel Coronavirus (2019-nCoV): estimating the case fatality rate—a word of caution. Swiss Med Wkly. (2020) 150:w20203. doi: 10.4414/smw.2020.20203
5. Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. (2020) 8:e480. doi: 10.1016/S2214-109X(20)30068-1
6. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1038. doi: 10.1016/S0140-6736(20)30566-3
7. Hu WP, Zhang FY, Zhang J, Hang J-Q, Zeng Y-Y, Du C-L, et al. Initial diagnosis and management of adult community-acquired pneumonia: a 5-day prospective study in Shanghai. J Thorac Dis. (2020) 12:1417–26. doi: 10.21037/jtd.2020.03.02
8. Blot SI, Rodriguez A, Solé-Violán J, Blanquer J, Almirall J, Rello J, et al. Effects of delayed oxygenation assessment on time to antibiotic delivery and mortality in patients with severe community-acquired pneumonia. Crit Care Med. (2007) 35:2509–14. doi: 10.1097/01.CCM.0000287587.43801.9C
9. Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care. (2020) 10:33. doi: 10.1186/s13613-020-00650-2
10. O'Driscoll BR, Howard LS, Earis J, Mak V. British Thoracic Society Emergency Oxygen Guideline Group; BTS Emergency Oxygen Guideline Development Group. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax. (2017) 72(Suppl 1):ii1–ii90. doi: 10.1136/thoraxjnl-2016-209729
11. Chu DK, Kim LH, Young PJ, Zamiri N, Almenawer SA, Jaeschke R, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. (2018). 391:1693–705. doi: 10.1016/S0140-6736(18)30479-3
12. Van den Boom W, Hoy M, Sankaran J, Liu M, Chahed H, Feng M, et al. The search for optimal oxygen saturation targets in critically ill patients: observational data from large ICU databases. Chest. (2020) 157:566–73. doi: 10.1016/j.chest.2019.09.015
13. Barrot L, Asfar P, Mauny F, Winiszewski H, Montini F, Badie J, et al. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. (2020) 382:999–1008. doi: 10.1056/NEJMoa1916431
14. Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. (2016) 388:e19–23. doi: 10.1016/S0140-6736(16)30388-9
15. European Society of Respiratory Medicine. COVID-19: Guidelines and recommendations directory. Available online at: https://www.ersnet.org/covid-19/covid-19-guidelines-and-recommendations-directory/ (accessed on May 30, 2020).
16. United Arab Emirates Ministry of Health and Prevention. National Guidelines for Clinical Management and Treatment of COVID-19. April 3rd. (2020). Version 2. Available online at: https://www.dha.gov.ae/en/HealthRegulation/Documents/COVID%20National%20Guidelines%20FINAL%2018%20March.pdf (accessed May 14, 2020).
17. Fröhlich S, Boylan J, McLoughlin P. Hypoxia-induced inflammation in the lung: a potential therapeutic target in acute lung injury? Am J Respir Cell Mol Biol. (2013) 48:271–9. doi: 10.1165/rcmb.2012-0137TR
18. Børvik T, Evensen LH, Morelli VM, Melbye H, Brækkan SK, Hansen JB. Impact of respiratory symptoms and oxygen saturation on the risk of incident venous thromboembolism-the Tromsø study. Res Pract Thromb Haemost. (2020) 4:255–62. doi: 10.1002/rth2.12299
19. Goyal DK, Mansab F, Bhatti S. Room to breathe: the impact of oxygen rationing on health outcomes in SARS-CoV2. Front Med. (2021) 7:573037. doi: 10.3389/fmed.2020.573037
20. Brouqui P, Amrane S, Million M, Cortaredona S, Parola P, Lagier J-C, et al. Asymptomatic hypoxia in COVID-19 is associated with poor outcome. Int J Infect Dis. (2020) 102:233–8. doi: 10.1016/j.ijid.2020.10.067
21. NHS England. Clinical guide for the optimal use of Oxygen therapy during the coronavirus pandemic. (2020). Version 1. Available online at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0256-specialty-guide-oxygen-therapy-and-coronavirus-9-april-2020.pdf (accessed May 14, 2020).
22. Lee SA, Mathis AA, Jobe MC, Pappalardo EA. Clinically significant fear and anxiety of COVID-19: a psychometric examination of the coronavirus anxiety scale. Psychiatry Res. (2020) 290:113112. doi: 10.1016/j.psychres.2020.113112
23. Steinberg E, Balakrishna A, Habboushe J, Shawl A, Lee J. Calculated decisions: COVID-19 calculators during extreme resource-limited situations. Emerg Med Pract. (2020) 22 (4 Suppl):CD1–5.
24. Goyal DK, Mansab F, Iqbal A, Bhatti S. Early intervention likely improves mortality in COVID-19 infection. Clin Med. (2020) 20:248–50. doi: 10.7861/clinmed.2020-0214
25. British Thoracic Society (2015) —Annotated BTS Guideline for the management of CAP in adults. (2009). Available online at: https://www.brit-thoracic.org.uk/quality-improvement/guidelines/pneumonia-adults/ (accessed May 14, 2020).
26. National Centre for Infectious Diseases (Singapore). Interim Treatment Guidelines for COVID-19 (Version 1.0, April 2, 2020). Available online at: https://www.ncid.sg/Health-Professionals/Diseases-and-Conditions/Documents/Treatment%20Guidelines%20for%20COVID-19%20%282%20Apr%202020%29%20-final.pdf (accessed May 14, 2020).
27. NICE (UK) guideline [NG165] COVID-19 rapid guideline: managing suspected or confirmed pneumonia in adults in the community (April 3 2020). Available online at: https://www.nice.org.uk/guidance/ng165 (accessed May 14, 2020).
Keywords: COVID-19, SARS-CoV2, oxygen, mortality, treatment, early intervention, rationing, target oxygen saturation
Citation: Mansab F, Donnelly H, Kussner A, Neil J, Bhatti S and Goyal DK (2021) Oxygen and Mortality in COVID-19 Pneumonia: A Comparative Analysis of Supplemental Oxygen Policies and Health Outcomes Across 26 Countries. Front. Public Health 9:580585. doi: 10.3389/fpubh.2021.580585
Received: 19 July 2020; Accepted: 06 May 2021;
Published: 13 July 2021.
Edited by:
Thi H. Do, Nguyen Tat Thanh University, VietnamReviewed by:
Joseph Friedman, UCLA David Geffen School of Medicine, United StatesCopyright © 2021 Mansab, Donnelly, Kussner, Neil, Bhatti and Goyal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel K. Goyal, ZGFuaWVsLmdveWFsQGdoYS5naQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.