
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 07 January 2021
Sec. Clinical Diabetes
Volume 8 - 2020 | https://doi.org/10.3389/fpubh.2020.568832
This article is part of the Research Topic Achieving Effective Management and Treatment of Diabetes Mellitus in Future Primary Care View all 11 articles
 Olivia McCarthy1*
Olivia McCarthy1* Rachel Deere2
Rachel Deere2 Max L. Eckstein3,4
Max L. Eckstein3,4 Jason Pitt1
Jason Pitt1 Ben Wellman1
Ben Wellman1 Stephen C. Bain5
Stephen C. Bain5 Othmar Moser3,4
Othmar Moser3,4 Richard M. Bracken1
Richard M. Bracken1Aim: To explore the influence of clinical exercise trial participation on glycaemia and insulin therapy use in adults with type 1 diabetes (T1D).
Research Design and Methods: This study involved a secondary analysis of data collected from 16 individuals with T1D who completed a randomized clinical trial consisting of 23-h in-patient phases with a 45-min evening bout of moderate intensity continuous exercise. Participants were switched from their usual basal-bolus therapy to ultra-long acting insulin degludec and rapid-acting insulin aspart as well as provided with unblinded interstitial flash-glucose monitoring systems. To assess the impact of clinical trial participation, weekly data obtained at the screening visit (pre-study involvement) were compared against those collated on the last experimental visit (post-study involvement). Interstitial glucose [iG] data were split into distinct glycaemic ranges and stratified into day (06:00–23:59) and night (00:00–05:59) time periods. A p-value of ≤ 0.05 was accepted for significance.
Results: Following study completion, there were significant decreases in both the mean nocturnal iG concentration (Δ-0.9 ± 4.5 mmol.L−1, p < 0.001) and the time spent in severe hyperglycaemia (Δ-7.2 ± 9.8%, p = 0.028) during the night-time period. The total daily (Δ-7.3 ± 8.4 IU, p = 0.003) and basal only (Δ-2.3 ± 3.8 IU, p = 0.033) insulin dose requirements were reduced over the course of study involvement.
Conclusions: Participation in clinical research may foster improved nocturnal glycaemia and reduced insulin therapy use in people with T1D. Recognition of these outcomes may help encourage volunteers to partake in clinical research opportunities for improved diabetes-related health outcomes.
Clinical Trial Registration: DRKS.de; DRKS00013509.
Volunteering as a research participant displays altruism and a willingness to help advance medical science. However, research trial participation often requires unaccustomed adjustments to routine care, as well as considerable time commitments for those involved. As such, patient enrollment, and indeed retention, represent long-standing obstacles in the conduction of clinical research (1–3). Nevertheless, research participation can provide patients access opportunities to novel pharmacological therapies and/or technological devices, as well as intense and frequent interactions with clinical research teams who provide educational support. For individuals with type 1 diabetes (T1D), pharmaceutical developments in modern ultra-long acting basal insulins with refined pharmacokinetic and pharmacodynamic profiles have led to improved glycaemic outcomes (4–10). Furthermore, recent advances in interstitial glucose (iG) monitoring systems have challenged the sole dependency on self-monitoring of blood glucose, and proven useful in aiding patient adherence to frequent glycaemic assessment (11–14). In addition, interactive opportunities with health care professionals who offer medical information and support can foster positive psychosocial and glycaemic outcomes (15–17). These pharmaceutical, technological, and physiological aids are complemented by lifestyle factors, including both diet and physical activity. Though exercise is endorsed by several international consensus panels as an integral component of the treatment plan of those with T1D (18–21), participation rates remain low, with fears around loss of glycaemic control and uncertainty in how to appropriately adjust exogenous insulin therapy cited as leading factors dissuading regular engagement (22). The heightened bioenergetic demands of exercising muscle can induce increases in intramuscular glucose uptake by up to 50-fold that of basal rates (23, 24). When combined with an inability to lower exogenous insulin concentrations as well as an often blunted glucoregulatory rescue system (25), the maintenance of normoglycaemia during exercise is challenging for those with T1D. Though acutely apparent, the metabolic challenges evoked by physical exercise may persist for several hours subsequent to its cessation (26–29). This often extends the risk of dysglycaemia leading into and throughout the nocturnal period, at a time when self-monitoring of blood glucose is inherently difficult. As such, glycaemic management strategies that seek to address these concerns are integral in encouraging safe exercise performance whilst minimizing the extent of glycaemic fluctuations. The ideal therapeutic care of those with T1D involves a multimodal approach including access to current pharmacological, technological, and support opportunities that collectively help to cultivate optimal self-management. Thus, research trials that include any of these elements may have clinically relevant outcomes beyond the those solely pertinent to answering the primary outcome.
To explore the influence of clinical exercise trial participation on glycaemic and insulin therapy outcomes in adults with type 1 diabetes (T1D).
This study was a secondary analysis of data collected from a single-centered, randomized, open-label, four-period, cross-over clinical trial (DRKS.de; DRKS00013509) consisting of four 23-h in-patient phases with a 45-min evening bout of semi-recumbent cycling at 60 ± 6% VO2max. The study was performed in accordance with good clinical practice and the Declaration of Helsinki (https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/). Approval was granted by both the national research ethics committee (16/WA/0394) and the local health authority (EudraCT number: 2017-004774-34; UTN: U1111-1174-6676). The primary outcome was to detail the extent and prevalence of post-exercise and nocturnal hypoglycaemia following peri-exercise bolus insulin dose adjustments in individuals with T1D using multiple daily injections of insulins aspart (IAsp) and degludec (IDeg). As part of a secondary, retrospective analysis, the present study sought to explore the influence of clinical exercise trial participation on glycaemia and insulin therapy use in adults with T1D.
Ahead of trial inclusion, participants were screened for anthropometric, cardiovascular, and T1D specific markers prior to the performance of a cardio-pulmonary exercise test on a semi-recumbent cycle ergometer (Corival Recumbent, Lode, NL) (30). Main inclusion criteria were: diagnosis of T1D for ≥12 months; age 18–65 years (both inclusive); body mass index of 18.0–29.4 kg.m2; use of multiple daily injections of insulin for ≥12 months; body mass-specific peak oxygen uptake of ≥20 mL.kg−1.min−1, and a status of being physically active as assessed by the International Physical Activity Questionnaire Short Form. All participants were considered hypoglycaemic aware, having avoided recurrent severe hypoglycaemia (defined as >1 severe hypoglycaemia event during the previous 12 months) and demonstrated a sound understanding of the symptomatic traits of hypoglycaemia to the investigator. After successful completion against the reference inclusion criteria, participants were switched from their usual basal/bolus insulin therapies (n = 8; glargineU100/IAsp, n = 1; glargineU300/IAsp, n = 1; IDeg/IAsp, n = 6; detemir/IAsp) to ultra-long-acting IDeg (Tresiba®, NovoNordisk, Denmark) in 3 mL pre-filled investigational pens (PDS290) and rapid-acting IAsp (NovoRapid® NovoNordisk, Denmark) in 3 mL pre-filled investigational pens (FlexPen®). Therapy with IDeg began on the morning following trial inclusion with a starting dosage of 70–80% of total daily basal insulin dose (TDBD) calculated by means of a titration algorithm. Participants were required to achieve a mean overnight-fasted morning blood glucose (BG) value of 4.4–7.2 mmol.L−1 over 3 consecutive days within 4 weeks of the first basal insulin dose. If glycaemic instability persisted for ≥3 days following titration, a dose adjustment alteration was made until criteria was met. A run-in period of >7 days was required to assure optimal adaptation to IDeg prior to the experimental period.
Unblinded flash glucose monitoring readers and sensors (Freestyle® Libre, Abbott, Lake Bluff, Illinois, USA) were provided by the study site for the duration of the trial. The sensor was inserted into the posterior aspect of the upper arm and measured interstitial glucose (iG) in 15-minute intervals. Participants were trained in use of the system and asked to change the sensor at least 48 h before each trial visit to avoid sensor expiration during the research period. With the exception of one individual, all participants were new to use of interstitial glucose monitoring, having previously used a range of point of care self-blood glucose monitoring systems. Though familiar with carbohydrate counting and insulin: carbohydrate dosing ratios, participants were guided through how to accurately record dietary information and shown insulin dose adjustment algorithms by the research team. This included the calculation of their individualized carbohydrate ([CarbF] = 5.7*kg/total daily dose of insulin [TDD]) and correction ([CorrF] = 109 mmol/l/TDD) factors as previously described (31). For the remainder of their involvement, participants were monitored by the study personnel to ensure glycaemic stability prior to each experimental visit. Stability was assessed via inspection of their iG patterns with particular scrutiny in the avoidance of hypoglycaemia (≤3.9 mmol.L−1) prior to laboratory attendance. As to control for any potential influence of extraneous variables on experimental trial day activities, participants were asked to replicate their habitual diet, physical activity, and insulin dosing strategies in the 24 h prior to each laboratory visit. Participants were contacted frequently by the research team to provide details of any adjustments.
Following preliminary testing (visit 1) and a run-in period for adjustment to IDeg, visits 2, 3, 4, and 5 were experimental visits that involved 23-h of in-patient monitoring with an overnight stay in a clinical research facility. After a standardized day-time period (08:00–15:59), participants undertook a bout of evening (17:00) cycling exercise at 60 ± 6 % O2max One hour prior to, and following exercise, participants administered either a full (100%) or reduced (50%) dose (100%; 5.1 ± 2.4 vs. 50%; 2.6 ± 1.2 IU, p < 0.001) of individualized IAsp alongside the consumption identical low-glycaemic index carbohydrate (CHO) rich meals (1.0 g.CHO.kg−1). An unaltered and regular dose of IDeg was kept consisted across each experimental visit. Trial day glycaemia was determined via capillary (08:00–15:59), venous (16:00–07:00), and interstitial (08:00–07:00) glucose monitoring over the 23-h in-patient stays.
Over the course of the study it became apparent that many individuals were perceiving their participation experience as beneficial to aspects of their diabetes related care outside of the experimental periods. Thus, as part of a retrospective, observational, secondary analysis we investigated weekly data taken from a “pre-study” period and compared them against data taken in the final week of their enrolment i.e., “post-study.” The pre-study period was classified as the 6-days after the screening visit but before any experimental trial visits (between visits 1 and 2), whilst the post-study period was classified as the 6-days prior to the final experimental trial visit immediately ahead of study completion (between visits 4 and 5). A 6-, rather than 7-day average was taken to avoid any potential interference of trial-related activities on habitual behaviors. Figure 1 provides a schematic overview of the study design with reference to the primary interventional manipulations and experimental visit schedule.
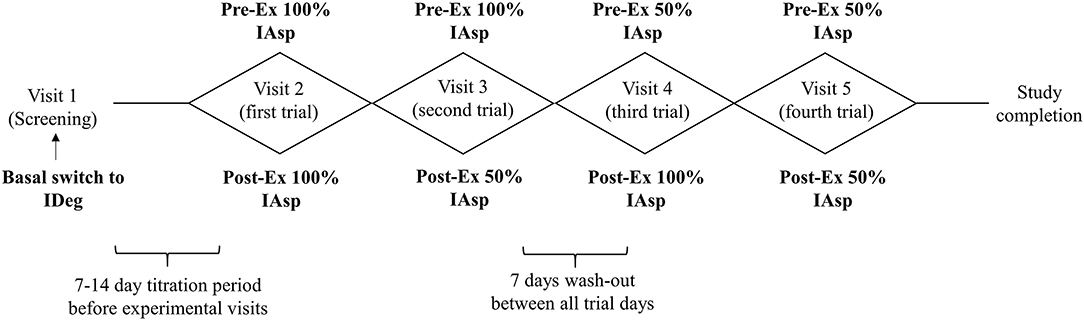
Figure 1. Schematic overview of the trial design with reference to the four interventional cross over arms involving peri-exercise adjustments to bolus insulin aspart on a stable background of insulin degludec. IAsp, insulin aspart; IDeg, insulin degludec.
On trial days, participants intake weighed whilst fasted and asked to report their previous 6-day average basal and bolus insulin doses, CHO intake and physical activity patterns (International Physical Activity Questionnaire). iG data were stratified into time spent within glycaemic thresholds i.e., time in range (TIR), time below range (TBR) and time above range (TAR). The targets are further bracketed into levels 1 and 2 to detail the severity of both hypo-and hyper-glycaemia; TBR 2 (<3.0 mmol.L−1), TBR 1 (≥3.0– <3.9 mmol.L−1), TIR (≥3.9– ≤ 10.0 mmol.L−1), TAR 1 (≥10.1– ≤ 13.9 mmol.L−1), TAR 2 (>13.9 mmol.L−1) (32). iG data were also split into day (06:00–23:59) and night (00:00–05:59) time periods. Due to a significant loss of data points, four participants were excluded from iG analysis. The significance of change in measurements from pre- to post-study was assessed via paired student's t-test or non-parametric equivalents used when necessary. SPSS (version 26.0) was used for all data analyses and reporting. P values of a p ≤ 0.05 (two-sided) accepted as statistically significant.
Baseline characteristics of study participants are included in Table 1. The average length of time for trial participation was 55 ± 29 days.
Device coverage was ≥89% over the 6-day data capture in both the pre- and post-study phases (pre; 91 ± 19 vs. post; 89 ± 14%, p = 0.716). Overall and stratified iG are presented in Table 2. Analysis revealed significant decreases in both the mean nocturnal iG concentration (Δ-0.9 ± 4.5 mmol.L−1, p < 0.001) and the TAR2 (Δ-7.2 ± 9.8%, p = 0.028) during the night-time hours.
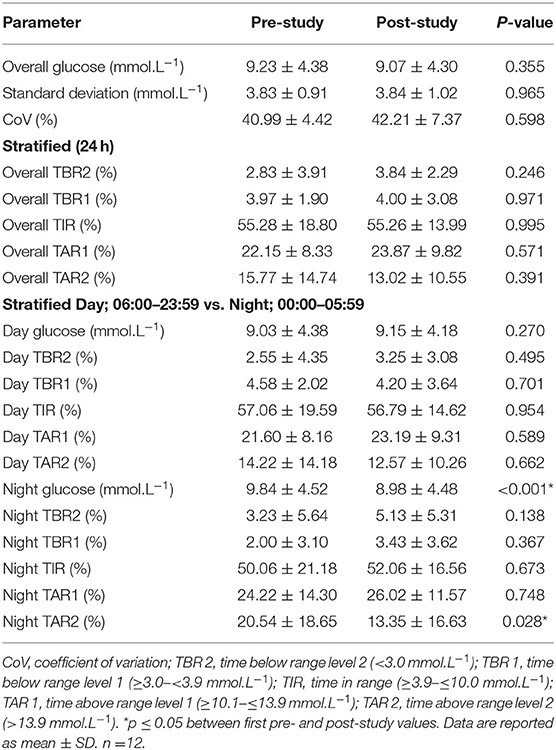
Table 2. Time spent in each glycaemic range as part of a 6-day analysis from the first to last experimental trial visits.
There were significant reductions in both the total daily (Δ-7.3 ± 8.4 IU, p = 0.003) and basal only (Δ-2.3 ± 3.8 IU, p = 0.033) insulin dose requirements from pre-to-post-study involvement (Table 3). There were no changes in any of the anthropometric, dietary CHO or physical activity metrics.
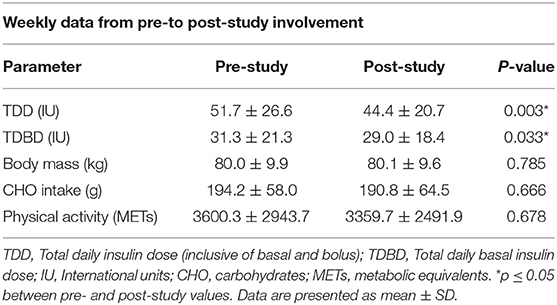
Table 3. Participant insulin regime, anthropometric data, and physical activity patterns on the first vs. last trial visits.
This exploratory study investigated the wider glycaemic impact of participation in a clinical exercise trial involving a therapeutic switch to ultra-long acting insulin degludec as well as the introduction to, and ad-hoc education support with, an interstitial glucose monitoring system in individuals with T1D.
Comparative analysis of interstitial glucose (iG) data obtained over a 6-day period taken before vs. after clinical trial participation revealed significant reductions in both the mean nocturnal glucose concentration and the amount of time spent in severe hyperglycaemia during the night-time hours. Additionally, upon trial completion, substantial reductions in both total daily, and basal only, insulin dose requirements were noted in the absence of changes in any anthropometric, dietary, and physical activity factors.
The reduction in insulin dosing requirements in the present study aligns with previous investigations that have demonstrated the efficacy of IDeg therapy in maintaining glycaemic outcomes at significantly lower dosing amounts (33, 34). The end of study IDeg dosing quantities used in this study are similar to those reported in recent work by Heise et al. (9) (Heise; 0.38 ± 0.23 IU.kg−1 vs. Our data; 0.34 ± 0.20 IU.kg−1), which reaffirms the safe integration of IDeg as a stable basal therapy at clinically relevant dosing levels. These dose reductions occurred in the absence of any changes in body mass, carbohydrate intake and physical activity patterns. Though we cannot out rule the possibility that great diligence to dietary tracking may have triggered individuals to select healthier food options, including lower glycaemic index carbohydrates, which may have contributed to drop in insulin dose, in light of the potential obesogenic implications associated with an over reliance on exogenous insulin administration (35), the dose reductions observed in this study carry important clinical undertones that stretch beyond those relating to dysglycaemia. Furthermore, 14/15 (93%) participants opted for continued use of IDeg as their basal analog and applied locally for continued Freestyle Libre provision upon study completion, perhaps emphasizing the value of these therapeutics in terms of patient satisfaction.
The significant decreases in both mean iG concentrations and the amount of TAR2 during nocturnal hours are meaningful from both a practitioner and patient point of view. Given the lack of endogenous autoregulation in the synthesis and secretion of insulin, the prevalence of the dawn phenomenon is a common feature of T1D which continues to represent a serious clinical concern (36). Combined with the inherent difficulties of performing regular self-monitoring of blood glucose during sleep, dysglycaemia during the night-time constitutes a major worry not only for those with T1D, but also for those who take an active role in their care (37–39). These fears are perhaps magnified following evening exercise, which, due to its long-lasting insulin-sensitizing effects, can disrupt glycaemia for the many hours subsequent to its performance (29, 40–42). Several international panels of diabetes specialists have convened to outline the merits of utilizing iG metrics to support decision making in clinical care (32, 43). The improvements in nocturnal glycaemia observed in this study may be the result of the introductory provision of an iG monitoring device, which allowed for the assessment of glycaemic patterns throughout the night-time period and hence, the ability to act accordingly to prevent glycaemic excursions. These results offer encouragement for the integration of modern ultra-long acting insulin analogs alongside iG monitoring systems in aiding glucose management around physical exercise in those with T1D. An important caveat is that our study cohort had a relatively long diabetes duration (~14 years), thus may have had greater experience in glycaemic management around physical exercise than those with a newer diagnosis.
For those with T1D, the fear of hypoglycaemia around exercise prevails as the main barrier to regular engagement, whilst a greater knowledge of insulin pharmacokinetics and/or using appropriate approaches to minimize exercise-related hypoglycaemia are associated with fewer perceived hurdles (22). The volatility in blood glucose levels around exercise may be one of the reasons that >60% of individuals with T1D currently fail to meet physical activity guidelines (44). To that end it is encouraging to learn of the potential value interactions with health care professionals and exercise physiologists throughout trial participation may have on the individuals involved, who's willingness to participate in clinical trials help advance our research efforts.
Due to the provision of two therapeutic aids alongside access to clinical diabetes care and support, it is difficult to discern the exact source of the observed improvements. Rather, we put forth these findings as part of a multi-faceted analysis, that, irrespective of being able to irrefutably demonstrate a clear cause and effect relationship, highlights the beneficial effects of research participation in a mutually reciprocal manner. Recognition of these outcomes may help incite volunteers to partake in clinical trials as well as encourage scientists to explore hypotheses outside of the primary objective.
Participation in clinical research may foster improved nocturnal glycaemia and reduced insulin therapy use in people with T1D. Beyond pursuing the primary outcomes of a research hypothesis, these data provide a basis for exploring the wider, clinically relevant health outcomes that may be associated with research trial participation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the national research ethics committee (16/WA/0394) and the local health authority (EudraCT number: 2017-004774-34, UTN: U1111-1174-6676). The patients/participants provided their written informed consent to participate in this study.
OMc, OMo, RD, ME, JP, and RB were responsible for data collection. OMc, JP, BW, and RB were responsible for data interpretation and statistical analyses. OMc, JP, and RB wrote the manuscript. SB and RB were the chief and principle investigators of the study. SB provided medical oversight for the study. RB wrote and secured funding for the study. All authors contributed to feedback and revisions for the final manuscript.
This study was funded by Novo Nordisk as part of an investigator sponsored study.
The authors declare that this study was funded by Novo Nordisk A/S as part of an investigator sponsored study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. OMc* has received a Zienkiewcz scholarship and travel grants from Novo Nordisk. OMo has received lecture fees from Medtronic, travel grants from Novo Nordisk A/S, Novo Nordisk AT, Novo Nordisk UK and Medtronic AT, research grants from Sêr Cymru II COFUND fellowship/European Union, Sanofi-Aventis, Novo Nordisk A/S, Novo Nordisk AT, Dexcom Inc., as well as material funding from Abbott Diabetes Care. ME has received a KESS2/European Social Fund scholarship and travel grants from Novo Nordisk A/S and Sanofi-Aventis. SB has received research grants (includes principal investigator, collaborator or consultant and pending grants as well as grants already received) from Health care and Research Wales (Welsh Government) and Novo Nordisk. He has received other research support from Healthcare and Research Wales (Welsh Government), honoraria from Novo Nordisk, Sanofi, Lilly, Boehringer Ingelheim and Merck, and has an ownership interest in Glycosmedia (diabetes on-line news service). RB reports having received honoraria, travel, and educational grant support from Boehringer-Ingelheim, Eli Lilly and Company, Novo Nordisk, and Sanofi-Aventis.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We would like to thank the participants for their significant time commitments and adherence to the study protocol. We would also like to thank the clinical care team and research facility for their considerable service and support throughout the project.
s1. Wittes RE, Friedman MA. Accrual to clinical trials. J Natl Cancer Inst. (1988) 80:884–5. doi: 10.1093/jnci/80.12.884
2. Ross S, Grant A, Counsell C, Gillespie W, Russell I, Prescott R. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol. (1999) 52:1143–56. doi: 10.1016/S0895-4356(99)00141-9
3. Hunninghake DB, Darby CA, Probstfield JL. Recruitment experience in clinical trials: literature summary and annotated bibliography. Control Clin Trials. (1987) 8(4 Suppl. 1):6–30. doi: 10.1016/0197-2456(87)90004-3
4. Mathieu C, Hollander P, Miranda-Palma B, Cooper J, Franek E, Russell-Jones D, et al. Efficacy and safety of insulin degludec in a flexible dosing regimen vs insulin glargine in patients with type 1 diabetes (BEGIN: Flex T1): a 26-week randomized, treat-to-target trial with a 26-week extension. J Clin Endocrinol Metab. (2013) 98:1154–62. doi: 10.1210/jc.2012-3249
5. Meneghini L, Atkin SL, Gough SCL, Raz I, Blonde L, Shestakova M, et al. The efficacy and safety of insulin degludec given in variable once-daily dosing intervals compared with insulin glargine and insulin degludec dosed at the same time daily: a 26-week, randomized, open-label, parallel-group, treat-to-target trial in individuals with type 2 diabetes. Diabetes Care. (2013) 36:858–64. doi: 10.2337/dc12-1668
6. Heise T, Meneghini L. Insulin stacking versus therapeutic accumulation: understanding the differences. Endocr Pract. (2014) 20:75–83. doi: 10.4158/EP13090.RA
7. Haahr H, Heise T. A review of the pharmacological properties of insulin degludec and their clinical relevance. Clin Pharmacokinet. (2014) 53:787–800. doi: 10.1007/s40262-014-0165-y
8. Korsatko S, Deller S, Mader JK, Glettler K, Koehler G, Treiber G, et al. Ultra-long pharmacokinetic properties of insulin degludec are comparable in elderly subjects and younger adults with type 1 diabetes mellitus. Drugs Aging. (2014) 31:47–53. doi: 10.1007/s40266-013-0138-0
9. Heise T, Hermanski L, Nosek L, Feldman A, Rasmussen S, Haahr H. Insulin degludec: four times lower pharmacodynamic variability than insulin glargine under steady-state conditions in type 1 diabetes. Diabetes Obes Metab. (2012) 14:859–64. doi: 10.1111/j.1463-1326.2012.01627.x
10. Josse RG, Woo V. Flexibly timed once-daily dosing with degludec: a new ultra-long-acting basal insulin. Diabetes Obes Metab. (2013) 15:1077–84. doi: 10.1111/dom.12114
11. Battelino T, Phillip M, Bratina N, Nimri R, Oskarsson P, Bolinder J. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care. (2011) 34:795–800. doi: 10.2337/dc10-1989
12. Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet. (2016) 388:2254–63. doi: 10.1016/S0140-6736(16)31535-5
13. Dover AR, Stimson RH, Zammitt NN, Gibb FW. Flash glucose monitoring improves outcomes in a type 1 diabetes clinic. J Diabetes Sci Technol. (2017) 11:442–3. doi: 10.1177/1932296816661560
14. Edelman SV, Argento NB, Pettus J, Hirsch IB. Clinical implications of real-time and intermittently scanned continuous glucose monitoring. Diabetes Care. (2018) 41:2265–74. doi: 10.2337/dc18-1150
15. Scavone G, Manto A, Pitocco D, Gagliardi L, Caputo S, Mancini L, et al. Effect of carbohydrate counting and medical nutritional therapy on glycaemic control in Type 1 diabetic subjects: a pilot study. Diabet Med. (2010) 27:477–9. doi: 10.1111/j.1464-5491.2010.02963.x
16. Knight BA, Hickman IJ, Gibbons K, Taylor J, McIntyre HD. Psychosocial outcomes in adults with type 1 diabetes following a novel ‘short course’ structured flexible MDI therapy self-management programme. Pract Diabetes. (2017) 34:235–39a. doi: 10.1002/pdi.2126
17. DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ. (2002) 325:746. doi: 10.1136/bmj.325.7367.746
18. Riddell MC, Gallen IW, Smart CE, Taplin CE, Adolfsson P, Lumb AN, et al. Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol. (2017) 5:377–90. doi: 10.1016/S2213-8587(17)30014-1
19. Moser O, Eckstein ML, West DJ, Goswami N, Sourij H, Hofmann P. Type 1 diabetes and physical exercise: moving (forward) as an adjuvant therapy. Curr Pharm Des. (2020) 29:946–57. doi: 10.2174/1381612826666200108113002
20. Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: a position statement of the American diabetes association. Diabetes Care. (2016) 39:2065–79. doi: 10.2337/dc16-1728
21. Adolfsson P, Riddell MC, Taplin CE, Davis EA, Fournier PA, Annan F, et al. ISPAD clinical practice consensus guidelines 2018: exercise in children and adolescents with diabetes. Pediatr Diabetes. (2018) 19(Suppl. 27):205–26. doi: 10.1111/pedi.12755
22. Brazeau A-S, Rabasa-Lhoret R, Strychar I, Mircescu H. Barriers to physical activity among patients with type 1 diabetes. Diabetes Care. (2008) 31:2108–9. doi: 10.2337/dc08-0720
23. Rose AJ, Richter EA. Skeletal muscle glucose uptake during exercise: How is it regulated? Physiology. (2005) 20:260–70. doi: 10.1152/physiol.00012.2005
24. Moser O, Yardley J, Bracken R. Interstitial glucose and physical exercise in type 1 diabetes: integrative physiology, technology, and the gap in-between. Nutrients. (2018) 10:93. doi: 10.3390/nu10010093
25. Petersen KF, Price TB, Bergeron R. Regulation of net hepatic glycogenolysis and gluconeogenesis during exercise: impact of type 1 diabetes. J Clin Endocrinol Metab. (2004) 89:4656–64. doi: 10.1210/jc.2004-0408
26. Yardley JE, Zaharieva DP, Jarvis C, Riddell MC. The “Ups” and “Downs” of a bike race in people with type 1 diabetes: dramatic differences in strategies and blood glucose responses in the paris-to-ancaster spring classic. Can J Diabetes. (2015) 39:105–10. doi: 10.1016/j.jcjd.2014.09.003
27. McMahon SK, Ferreira LD, Ratnam N, Davey RJ, Youngs LM, Davis EA, et al. Glucose requirements to maintain euglycemia after moderate-intensity afternoon exercise in adolescents with type 1 diabetes are increased in a biphasic manner. J Clin Endocrinol Metab. (2007) 92:963–8. doi: 10.1210/jc.2006-2263
28. Hansen PA, Nolte LA, Chen MM, Holloszy JO. Increased GLUT-4 translocation mediates enhanced insulin sensitivity of muscle glucose transport after exercise. J Appl Physiol. (1998) 85:1218–22. doi: 10.1152/jappl.1998.85.4.1218
29. Tsalikian E, Mauras N, Beck RW, Tamborlane WV, Janz KF, Chase HP, et al. Impact of exercise on overnight glycemic control in children with type 1 diabetes mellitus. J Pediatr. (2005) 147:528–34. doi: 10.1016/j.jpeds.2005.04.065
30. Hofmann P, Tschakert G. Special needs to prescribe exercise intensity for scientific studies. Cardiol Res Pract. (2011) 2011:209302. doi: 10.4061/2011/209302
31. Walsh J, Roberts R, Bailey T. Guidelines for optimal bolus calculator settings in adults. J Diabetes Sci Technol. (2011) 5:129–35. doi: 10.1177/193229681100500118
32. Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. (2019) 42:1593–603. doi: 10.2337/dci19-0028
33. Nakamura T, Sakaguchi K, So A, Nakajima S, Takabe M, Komada H, et al. Effects of insulin degludec and insulin glargine on day-to-day fasting plasma glucose variability in individuals with type 1 diabetes: a multicentre, randomised, crossover study. Diabetologia. (2015) 58:2013–9. doi: 10.1007/s00125-015-3648-y
34. Ponzani P, Berra C, Di Lelio A, Del Sindaco P, Di Loreto C, Reggiani F, et al. Switching patients with type 1 diabetes to insulin degludec from other basal insulins: real-world data of effectiveness and safety. Diabetes Ther. (2019) 11:97–105. doi: 10.1007/s13300-019-00722-y
35. Purnell JQ, John EH, Cleary PA, Nathan DM, Lachin JM, Zinman B, et al. The effect of excess weight gain with intensive diabetes mellitus treatment on cardiovascular disease risk factors and atherosclerosis in type 1 diabetes mellitus: results from the diabetes control and complications trial/epidemiology of diabetes interventions and complications study (DCCT/EDIC) study. Circulation. (2013) 127:180–7. doi: 10.1161/CIRCULATIONAHA.111.077487
36. Ostrovski I, Lovblom Le, Scarr D, Weisman A, Orszag A, D'aoust E, et al. Analysis of prevalence, magnitude, and timing of the dawn phenomenon in type 1 diabetes—descriptive analysis of two insulin pump trials. Diabetes. (2018) 67(Suppl. 1):10-OR. doi: 10.2337/db18-10-OR
37. Sherr JL, Cengiz E, Palerm CC, Clark B, Kurtz N, Roy A, et al. Reduced hypoglycemia and increased time in target using closed-loop insulin delivery during nights with or without antecedent afternoon exercise in type 1 diabetes. Diabetes Care. (2013) 36:2909–14. doi: 10.2337/dc13-0010
38. Barnard K, Thomas S, Royle P, Noyes K, Waugh N. Fear of hypoglycaemia in parents of young children with type 1 diabetes: a systematic review. BMC Pediatr. (2010) 10:50. doi: 10.1186/1471-2431-10-50
39. Gonder-Frederick L, Nyer M, Shepard JA, Vajda K, Clarke W. Assessing fear of hypoglycemia in children with type 1 diabetes and their parents. Diabetes Manag. (2011) 1:627–39. doi: 10.2217/dmt.11.60
40. Moser O, Eckstein Ml, Mccarthy O, Riddell M, Fontana Fy, Skroce K, et al. 66-LB: greater time spent in hypoglycemia during night compared with day during intensified training in professional cyclists with type 1 diabetes—a prospective observational study. Diabetes. (2019) 68(Suppl. 1):66-LB. doi: 10.2337/db19-66-LB
41. Iscoe KE, Riddell MC. Continuous moderate-intensity exercise with or without intermittent high-intensity work: effects on acute and late glycaemia in athletes with type1 diabetes mellitus. Diabet Med. (2011) 28:824–32. doi: 10.1111/j.1464-5491.2011.03274.x
42. Younk LM, Mikeladze M, Tate D, Davis SN. Exercise-related hypoglycemia in diabetes mellitus. Expert Rev Endocrinol Metab. (2011) 6:93–108. doi: 10.1586/eem.10.78
43. Bergenstal RM, Ahmann AJ, Bailey T, Beck RW, Bissen J, Buckingham B, et al. Recommendations for standardizing glucose reporting and analysis to optimize clinical decision making in diabetes: THE AMBULATORY GLUCOSE PROFILe (AGP). In: Diabetes Technology and Therapeutics. New Rochelle, NY: Mary Ann Liebert, Inc (2013). p. 198–211. doi: 10.1089/dia.2013.0051
44. Bohn B, Herbst A, Pfeifer M, Krakow D, Zimny S, Kopp F, et al. Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care. (2015) 38:1536–43. doi: 10.2337/dc15-0030
Keywords: type 1 diabetes (T1D), exercise, insulin, glycaemia, research participant experience
Citation: McCarthy O, Deere R, Eckstein ML, Pitt J, Wellman B, Bain SC, Moser O and Bracken RM (2021) Improved Nocturnal Glycaemia and Reduced Insulin Use Following Clinical Exercise Trial Participation in Individuals With Type 1 Diabetes. Front. Public Health 8:568832. doi: 10.3389/fpubh.2020.568832
Received: 02 June 2020; Accepted: 25 November 2020;
Published: 07 January 2021.
Edited by:
Boon-How Chew, Putra Malaysia University, MalaysiaReviewed by:
Marco Infante, University of Miami, United StatesCopyright © 2021 McCarthy, Deere, Eckstein, Pitt, Wellman, Bain, Moser and Bracken. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Olivia McCarthy, b2xpdmlhLm1jY2FydGh5QHN3YW5zZWEuYWMudWs=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.