
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 06 September 2019
Sec. Children and Health
Volume 7 - 2019 | https://doi.org/10.3389/fpubh.2019.00250
This article is part of the Research Topic Assessment of Psychological Functioning and Risk in Healthcare Settings View all 11 articles
The aim of this paper was to assess strengths and fragilities in children aged 6 to 10 who suffered one or more hospitalizations. State and trait anxiety, coping abilities, and cognitive and affective functioning through play were assessed using a triangulation approach. Fifty hospitalized children aged 6–10 were compared to 50 non-hospitalized children, and children at first admission were compared with children with more than one hospitalization experience. The State-Trait Anxiety Scales Inventory for Children was administered for assessing trait and state anxiety, and the Children's Coping Strategies Checklist (Revision 1) was administered to assess coping dimensions. The Affect in Play Scale - Preschool - Brief (Extended version) was used to assess cognitive and affective dimensions of play. No significant differences were found for trait anxiety between hospitalized vs. non-hospitalized children. Instead, as expected, state anxiety was significantly higher in hospitalized childen than in the non-hospitalized children. Hospitalized children reported higher scores than non-hospitalized children in support-seeking strategies. As for pretend play, hospitalized children showed significantly higher cognitive scores than non-hospitalized children. However, hospitalized children appeared significantly more restricted in their affect expressions. No significant differences were found for play and anxiety scores between children admitted for the first time in the hospital ward and children with more than one admission. However, children at first admission scored higher in coping and positive cognitive restructuring and in avoidance-coping strategies than children with more than one admission. The initial assessment of the interplay of key variables such as anxiety, coping and play can inform healthcare professionals by serving as a guide in order to determine a child's risk for negative psychological outcomes due to hospitalization, to plan appropriate interventions and to provide substantial assistance to hospitalized children in the future.
Hospitalization for children means leaving their home and their caregivers and siblings and an interruption of their daily activities and routines. Moreover, hospital wards are often associated with staying in a “cold and medical” setting, facing fear of medical examinations, pain, uncertainty, and loss of control and safeness [e.g., (1, 2)]. This is particularly true for elementary school children who are involved in mental, emotional, and social adjustment developmental tasks. Literature about hospitalization during childhood underscores how, in the short term, extreme distress may compromise the completion of a required medical procedure, while in the long term it may lead to difficulties in future intakes that discourage the use of medical treatments (3–6). Moreover, anxiety-provoking experiences (such as hospitalizations) can affect children physical growth, personality, or emotional development (7). Burns-Nader and Hernandez-Reif (2) stressed that to determine children's needs in the medical setting, specialists have to carry out a psychological assessment in order to detect potential stress, anxiety, coping abilities, and play skills to provide age-appropriate interventions.
Usually, children feel anxious before encountering medical professionals, as well as experiencing a hospitalization (7). Empirical studies suggest that children express anxiety through regression in behaviors, aggression, lack of cooperation, withdrawal, and difficulty recovering from procedures (8, 9). Literature shows that children involved in psychological programs were more able to contain anxiety, showing lower levels of anxiety assessed before surgery, and reporting less postoperative anxiety (10). Previous studies supported the importance of specific clinical measures to assess children's anxiety in medical settings (11). Indications provided by tailored tools, might be helpful to support children in approaching medical situations with a sense of comfort, achievement, and control. Few empirical studies have been carried out on levels of trait and state anxiety in hospitalized children (12). Trait anxiety follows the child in everyday experiences including hospitalization and as such, if elevated, has to be recognized as a vulnerability for the child. State anxiety could originate from the hospital experience. The literature shows that among children aged 5–11, it vanishes from hospital admission to discharge (13). Trait vs. state anxiety is not often assessed, and subsequently undertreated (14). Trait anxiety plays an important role in the child's response to hospitalization (9, 15). The higher a child's trait anxiety, the higher his or her perception of hospitalization as a stressful experience will be and the less effective will be his or her ability to cope (15, 16).
Burns-Nader and Hernandez-Reif (2) suggested it is fundamental to foster effective coping to minimize anxiety in children experiencing a medical situation. Coping in children can be defined as a collection of conscious and purposeful efforts that are directed at the regulation of aspects of the self (emotion, cognition, behavior, and physiology) and the environment in contexts involving stress [e.g., (17–19)]. Adaptive coping strategies could fail under stressful conditions (20–22). Effective coping behaviors provide resilience to mitigate the likelihood of adverse outcomes and potentially enhance growth (23–26). Effective coping promotes adjustment to stressful life events, well-being, competence and resilience during childhood and adolescence (27). Blount et al. (28) highlighted the importance to consider coping a multidimensional construct. Specifically, Skinner et al. (21) suggested that five categories of coping are clearly crucial across ages and have been empirically supported in children and adolescents (17, 29–32): problem-solving, positive cognitive restructuring (active coping), support seeking, avoidance, and distraction. Research findings suggested that psychological outcomes related to hospitalization are linked to children's coping styles (33). Avoidant coping is mainly used during the acute phase of health care or hospitalization, whereas active coping is prominent in the recovery phase (7). Avoidant coping strategies are characterized by restricted thoughts on an upcoming event, denial of worries, and disconnection from stressful stimuli. They seem to be less effective in reducing the stress connected to hospitalization (12). With regard to the link between previous hospitalization and anxiety/coping, conclusions are not well-established. Some research has found that previous hospitalization is not related to a child's anxiety or coping (12, 34). However, children with no previous hospitalization, as well as those with fewer previous surgeries, showed higher anxiety than the ones who were already familiar with the medical setting (13, 35).
Among others, play is considered a coping method for children who experience a hospitalization, because play activity allows to express and elaborate affects and to show problem-solving abilities (36, 37). Play allows children to convey their feelings and control stressful experience because through it children can recreate and transform their life events (2, 38, 39). In a study in which outcome measures were not assessed, hospitalized children stated that they used play to manage stressful experiences more frequently than non-hospitalized children (2, 40). For such a purpose, symbolic play, or pretend play, represents an important integration opportunity of cognitive, affective, and interpersonal competencies. Play facilitates representation of the world and helps children to express their feelings, make choices, transform stories, use imagination, focus on stressful or unfamiliar themes, and develop skills (41–44). A growing amount of research has supported the validity and reliability of the Affect in Play Scale [APS, (43)], a measure to assess pretend play with children. Both the original and the brief version, which does not include video-recording, showed good psychometric properties in school and preschool-based samples of typically developing children in the United States and in Italy (45–52). The existing literature underlines the importance of providing children with play sessions in the hospital playroom, at the bedside, or even in waiting rooms of hospital wards (2). Li et al. (53) highlighted the role of play intervention in reducing distress and anxiety in children that are hospitalized. Although, O'Connor (54) indicated pretend play as a natural mediator with hospitalized children, there is a paucity of valid and reliable tools devoted to it (55). So, the assessment of cognitive and affective abilities in pretend play during hospitalization of children, should be seen as beneficial for researchers and clinicians (56, 57).
The aim of the current paper was to assess the strengths and fragilities of hospitalized children aged 6 to 10 who suffered one or more hospitalization, comparing them to a community sample of non-hospitalized children. More specifically, the purposes of the current paper were twofold: to compare the level of state and trait anxiety, coping, and pretend play in (a) hospitalized vs. non-hospitalized children and (b) children at first admission vs. children with more than one hospitalization experience. In order to accomplish these goals, state and trait anxiety, coping abilities, and cognitive and affective functioning through play were assessed using a triangulation approach, which refers to the application and combination of several research methods in the study of the same phenomenon (58–60). In this study different information about the hospitalized children was collected using quantitative mixed methods (questionnaires and play tasks) gathered by the children themselves and compared with the same tools gathered by non-hospitalized children.
Attention was given to tools with adequate psychometric properties that can inform about a child's life by serving as a guide for initial assessments in pediatric wards where often a qualitative assessment is preferred. We hypothesized no significant differences in trait anxiety between hospitalized and non-hospitalized children, because it accompanies the child in everyday experience. Instead, state anxiety was expected to be higher.
The administration was carried out in compliance with the ethical standards for research outlined in the Ethical Principles of Psychologists and Code of Conduct (61). The study was approved by the ethics committee of the hospital including the pediatric unit and by the ethics committee for psychological research of Padova University (2017/num 2310). Each participant was met individually in a place where he or she could comfortably play and complete the questionnaires. During each session, participants were first engaged in the play task to assess cognitive and affective pretend play processes and later the two questionnaires were administered. No reward was offered for participation.
Power analysis to estimate the sample size was carried out using G*Power 3.1 (62). The sample size was inferred by considering three factors: a significance level of 0.05 (one tail); a medium effect size based on previous studies (53); and a power of 0.80. Power analysis indicated that there was an 80% chance of correctly rejecting the null hypothesis of no difference between hospitalized and non-hospitalized children, with a total sample of 100 (50 + 50) participants.
Thus, 50 hospitalized children (22 boys and 28 girls) aged 6–10 were recruited from a pediatric clinic in Northern Italy and 50 non-hospitalized children (22 boys and 28 girls) were recruited from elementary schools in Northern Italy.
Participants were a convenient sample of children admitted at the Pediatric Clinic of the University of Padova, during a 13-month period. In this period, 50 pediatric patients met the criteria selected for the present research. Inclusion criteria included children diagnosed by a physician as affected by middle (e.g., rheumatologic, cardiac, and metabolic pathologies) or transient pathologies (e.g., appendicitis or tonsillitis) or both. Moreover, children with psychiatric symptoms, severe cognitive impairment, and maladjustment were excluded. This information was collected in an anamnestic form fulfilled by parents, who signed written consent. Forty-two percent of selected children (n = 21) were at their first admission into the ward, and 58% (n = 29) had more than one admission to the hospital ward. Among the latter, 11% (n = 5) were admitted for different reasons, whereas 49% (n = 24) were admitted for the same reason. The admission period lasted between 5 and 10 days. Measures were administered in a quiet room, after a warm-up meeting with the examiner. The administration was scheduled in order not to interfere with the daily medical routine.
Non-hospitalized children were selected randomly from a larger sample matched by gender and age with the hospitalized children. Children with psychiatric symptoms, severe cognitive impairment, and maladjustment were excluded. Consent forms were sent home to parents. Children were allowed to participate in the study after parents provided written consent. A brief questionnaire about the children's physical health was sent to parents for the assessment of possible hospitalization. Each participant was met individually during school hours in a room where the children could comfortably play and complete the questionnaires. Some familiarity with the examiner was established before task administration. During each session, participants were first engaged in the play task to assess cognitive and affective pretend play processes and later the two questionnaires were administered.
State-Trait Anxiety Inventory for Children [STAI-C; (63, 64)] is a self-report measure developmentally adequate for assessing anxiety symptoms in children aged 9–12 years, but it can be used with younger children with average or above average reading abilities. It includes two separate scales for measuring two anxiety concepts: state and trait anxiety. The state scale, a measure of transitory anxiety states, consists of 20 statements that ask children how they feel at a particular moment in time. The items all start with the stem “I feel” and next to each stem respondents have to choose among three responses the one that best describes their state (e.g., very calm, calm, or not calm). The trait scale consists of 20 statements that ask children how they generally feel. It measures relatively stable individual differences in anxiety proneness. The items are rated on a 3-point scale with responses: hardly-ever, sometimes, and often. STAI-C showed adequate psychometric features in both international and national samples [e.g., (65, 66)]. Cronbach's alpha for the state scale was 0.79 for hospitalized and 0.71 for non-hospitalized children; alphas for the trait scale were 0.77 and 0.76 for hospitalized and non-hospitalized children, respectively.
Children's Coping Strategies Checklist-Revision 1 [CCSC-R1; (67)] includes 54 statements. Each statement starts with “If I have a problem” and is followed, for example, by “I tell others how I would like to solve it.” Children have to indicate how frequently they usually adopted the coping strategies described in the item on a 4-point Likert scale: 1 = never, 2 = sometimes, 3 = often, and 4 = always. CCSC-R1 is composed of 13 subscales and five dimensions: problem focused, coping and positive cognitive restructuring, distraction coping strategies, avoidance coping strategies, and support-seeking strategies. Examples of items are as follow: problem focused (“You thought about what you needed to know before”); coping and positive cognitive restructuring (“You told yourself you could handle whatever happens”); distraction coping strategies (“You watched TV”); avoidance coping strategies (“You tried to stay away from things that made you feel upset”); support-seeking strategies (“You talked to someone who could help you solve the problem”). Thus, CCSC-R1 includes two dimensions of active coping (problem-focused coping and positive cognitive restructuring), two dimensions connected with avoidance (distraction and avoidance coping strategies), and finally one dimension connected with support-seeking strategies. In this paper, each scale was made of the sum of the items. In the Italian validation, all dimensions yielded adequate reliability (68). Cronbach's alphas for the current study ranged from 0.67 to 0.87 for hospitalized children and from 0.55 to 0.77 for non-hospitalized ones.
The extended version of the Affect in Play Scale-Preschool Brief Version [APS-P-BR; (43, 46–50)] is a structured individually administered 5 min play task that allows evaluation of the affective and cognitive aspects (affect, imagination, organization, and comfort) in child's play using a standardized and empirically validated administration procedure and in vivo scoring attribution (43). Children are asked to play with a set of plastic and stuffed toys [for further detail see (49)]. Six primary scores (four cognitive and two affective) are assigned using a detailed scoring manual (43). The four cognitive scores are organization, elaboration, imagination, and comfort, coded on a 4-point Likert scale. Two main scores concerning affects are frequency of affect and tone [see (49)]. Psychometric characteristics of APS-P-BR Extended version showed satisfactory results (49).
Student's one-tailed t-tests for independent samples was performed on the APS-P-BR Extended version, state and trait STAI-C, and CCSC-R1 scores to compare hospitalized vs. non-hospitalized children. Moreover, a Student's one-tailed t-test for independent samples on all variables was performed to compare means of children who were admitted in the hospital ward for the first time vs. children who were admitted more than one time. A one-tailed test was considered appropriate because the aim was to check if the estimated value may depart from the reference value in only one direction.
Means and standard deviations for all variables for hospitalized and non-hospitalized children are reported in Table 1.
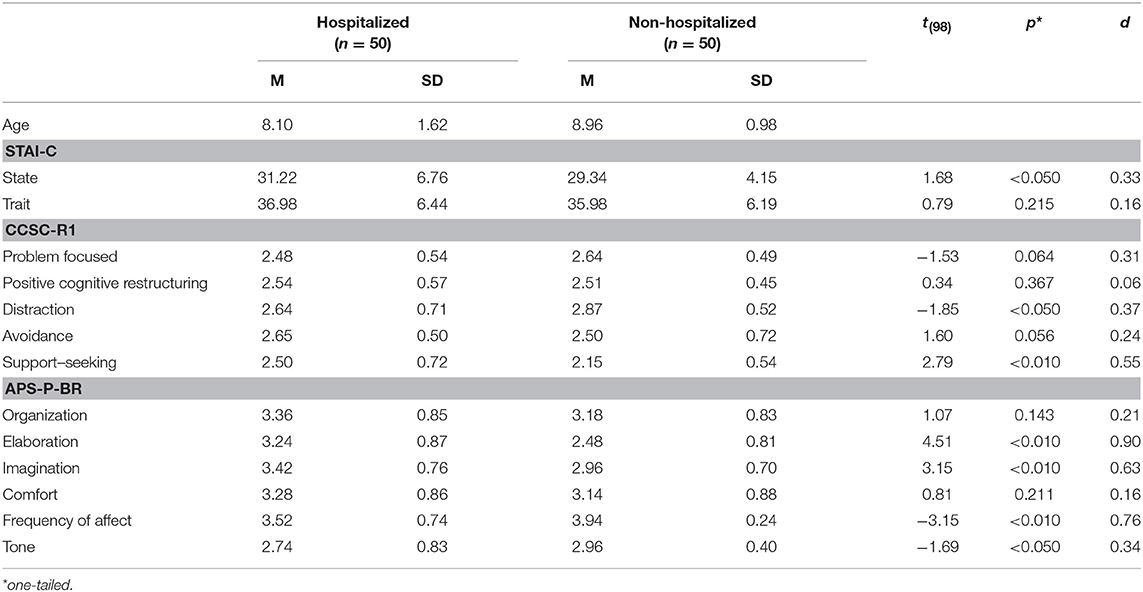
Table 1. Means, standard deviations and Student's t-test for hospitalized and non-hospitalized children.
Student's t-test value for independent samples was calculated for all tools administered to compare hospitalized vs. non-hospitalized children. Results are shown in Table 1.
Regarding anxiety, as expected no significant differences were found for trait anxiety. However, hospitalized children showed a higher level of state anxiety with a medium effect size. Focusing on coping strategies, support-seeking strategies showed hospitalized children reporting higher scores than non-hospitalized ones, with medium effect size. In regards to distraction, hospitalized children reported lower distraction scores. No other differences were found concerning this measure. As for pretend play, hospitalized children showed significantly higher elaboration and imagination than non-hospitalized children, with high and medium effect size, respectively. However, they appeared significantly more restricted in their affect expressions and with lower scores on tone, with high and medium effect size.
Means and standard deviations for children admitted for the first time in the hospital ward and children with more than one admission as well as Student's t-test for independent samples are reported in Table 2.
No significant differences were found for play and anxiety scores. For coping strategies, children at first admission scored higher in coping and positive cognitive restructuring and in avoidance-coping strategies than children with more than one admission. Effect sizes of these differences were medium.
This triangulation study evaluated state and trait anxiety, coping, and pretend play in a sample of hospitalized school-age Italian children compared with a control group of children of the same age never hospitalized. Trait anxiety did not differentiate significantly hospitalized vs. not hospitalized children, meaning that anxiety levels that typically accompany children during their everyday life experiences did not seem to be affected by the hospitalization. Trait anxiety did not differentiate significantly children at their first admission vs. children who already experienced hospitalization, meaning that the structural level of anxiety, so-called trait anxiety, was maintained at a normative level and was not undermined by the hospitalization experience (9, 15). As expected, state anxiety that was influenced by stressful transient experiences, such as the hospitalization, was higher in hospitalized children, with no difference in one-admission or multiple-admission subgroups (53). Referring to coping, hospitalized children reported a higher level of support seeking but lower score on distraction. As expected, children in the hospital ward are looking for more support by parents, nurses, or volunteers, but they are forced to reduce distraction strategies, such as sport or watching TV. No significant differences were found between hospitalized and non-hospitalized children for the two dimensions of active coping—problem-focused and positive cognitive restructuring. Literature suggested that an increase in problem-solving strategies is typical of this stage of development (27), showing that school age children are involved in a gradual shift from behavioral actions to more cognitive-based coping (69, 70). This pattern seemed to be valid independently from hospitalization experience. However, when looking at the two subsamples of hospitalized children, positive cognitive structuring and avoidance appeared significantly higher for children in their first admission. As Wilcox (33) suggested, the effectiveness of coping strategies are affected by recurrence and length of admissions. Children with more than one hospitalization are less prone in avoiding the stress of the situation and in recalling positive thoughts. Despite the unpleasant experience of hospitalization, hospitalized children in this study were able to maintain an organized pretend play and appeared comfortable in play at the same level as non-hospitalized children. Moreover, they used a higher amount of variety and complexity of embellishment in the story themes (elaboration) and a higher amount of fantasy and number of transformations (e.g., using one thing as another) in the play (imagination). Their more sophisticated elaboration of the scenario and the more prominent use of transformation in their storytelling might represent a useful way to deal with the distressing, unfamiliar, and painful reality of the hospitalization experience [e.g., (54)]. However, hospitalized children were more restricted in their expressions of affections in play, maybe for fear of being overwhelmed by a great variety and amount of affects that hospitalization could activate. It is interesting that the trend was maintained both for children at first hospitalization as well as for children with more than one hospitalization. Repeated hospitalizations do not seem to influence cognitive or affective components of play. Altogether, in this study the results showed that hospitalized children were able to organize a pretend play and trait anxiety did not differ from not clinical children. Moreover, they expressed active coping, but they also try to use avoidance defenses and they recognized their need for support.
However, this research has several limitations. This study was exploratory in nature. First, the sample was small and was made up of children affected by different kinds of diseases. Moreover, the generalizability of the results might be biased by the sampling method used for the collection of hospitalized children. Even though the sample size was supported by the power analysis, the number of participants was also affected by the recruitment in a hospital ward and by the restricted time schedule of the agreement with the hospital itself. Research and clinical literature showed the use of play in hospital, but often introduced and interpreted in a qualitative way: the use of the APS-P-BR Extended version would give the experts a way to assess in a more empirical way how the hospitalized children would be able to organize or not a pretend play in a distressful period of their lives.
There is a paucity of research on quantitative assessment with a triangulation method, mostly used to combine qualitative and quantitative approaches. The present paper aimed to propose the use of three validated measures to highlight children functioning in the experience of hospitalization. Even though anxiety, coping, and play are singular important aspects, their interplay might shed more light on the way children face a stressful experience, capturing the different dimensions of the same phenomenon. Referring to Lewick (7), beginning a health care assessment as it was proposed in this study stressing children's resources and labilities means to recognize and support patients' resilience, or strengths, and contributes in understanding the way in which a child patient can manage struggles in his or her life. In this way, a medical professional helps the patient to focus on and bring out his or her internal resources in order to deal with and overcome his or her concerns about the medical problems. Both strengths and difficulties should be relevant for—and emphasized by—medical professionals. In addition, starting from the resources and reframing negative talk around the child, a health care provider can decrease a child's anxiety and maladaptive trauma responses, regardless of the specific reasons for medical treatment. At last, the advice given to medical professionals to speak aloud a child's positive qualities during the first assessment (as well as whenever possible) is of crucial importance because it may be the only time in a day a child hears about them.
The datasets for this manuscript are not publicly available because Data available upon request. Requests to access the datasets should be directed to ZWxpc2EuZGVsdmVjY2hpb0B1bmlwZy5pdA==.
This study was carried out in accordance with the recommendations of the Ethical Principles of Psychologists and Code of Conduct (61) with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Ethic committee of the hospital including the pediatric unit and by the Ethic committee for psychological research of Padova University (#2310).
AL, DD, ED, and SS contributed conception and design of the study. AG organized the database and performed the statistical analysis. AL wrote the first draft of the manuscript. DD, ED, and SS wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Many thanks to the hospital professionals and staff, to the children and their families, and to Dr. C. Alberti, who collaborated for data collection.
1. Koukourikos K, Tzeha L, Pantelidou P, Tsaloglidou A. The importance of play during hospitalization of children. Mater Sociomed. (2015) 27:438–41. doi: 10.5455/msm.2015.27.438-441
2. Burns-Nader S, Hernandez-Reif M. Facilitating play for hospitalized children through child life services. Children's Health Care. (2016) 45:1–21. doi: 10.1080/02739615.2014.948161
3. Du S, Jaaniste T, Champion GD, Yap CS. Theories of fear acquisition: the development of needle phobia in children. Ped Pain Letter-Comm. (2008) 10:13–7. Retrieved from: http://childpain.org/ppl/issues/v10n2_2008/v10n2_yap.pdf
4. Kennedy RM, Luhmann J, Zempsky WT. Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics. (2008) 122 (Suppl 3):S130–3. doi: 10.1542/peds.2008-1055e
5. Noel M, McMurtry CM, Chambers CT, McGrath PJ. Children's memory for painful procedures: The relationship of pain intensity, anxiety, and adult behaviors to subsequent recall. J Ped Psych. (2010) 35:626–36. doi: 10.1093/jpepsy/jsp096
6. Ersig AL, Kleiber C, McCarty AM, Hanrahan K. Validation of a clinically useful measure of children's state anxiety before medical procedures. J Spec Ped Nurs. (2013) 18:311–9. doi: 10.1111/jspn.12042
7. Lerwick JL. Minimizing pediatric healthcare-induced anxiety and trauma. World J Clin Pediatr. (2016) 8 5:143–50. doi: 10.5409/wjcp.v5.i2.143
8. Favara-Scacco C, Smirne G, Schiliro G, Di Cataldo A. Art therapy as support for children with leukemia during painful procedures. Med and Ped Oncol. (2001) 36:474–80. doi: 10.1002/mpo.1112
9. Hart D, Bossert E. Self-reported fears of hospitalized school-aged children. J Ped Nurs. (1994) 9:83–90.
10. Yun-ping L, Zhen-hua H, Finley GA, Yun-xia Z. Effects of the combination of mask preconditioning with idazolam pretreatment on anxiety and mask acceptance during pediatric inhalational induction and postoperative. Chin Med J. (2012) 125:1908–14. doi: 10.3760/cma.j.issn.0366-6999.2012.11.013
11. Stephens BK, Barkey ME, Hall HR. Techniques to comfort children during stressful procedures. Accid. Emerg. Nurs. (1999) 7:226–36. doi: 10.1016/S0965-2302(99)80055-1
12. Koller D. (2008). Child Life Council Evidence-Based Practice Statement: Therapeutic Play in Pediatric Health Care: The Essence of Child Life Practice. Retrieved from: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.517.4281&rep=rep1&type=pdf (accessed August 20, 2019).
13. Tiedeman ME, Clatworthy S. Anxiety responses of 5- to 11-year-old children during and after hospitalization. J Ped Nurs. (1990) 5:334–43.
14. Crandall MRN, Lammers C, Senders C, Savedra M, Braun JV. Initial validation of a numeric zero to ten scale to measure children's state anxiety. Anes Analg. (2007) 105:1250–3. doi: 10.1213/01.ane.0000284700.59088.8b
15. Bossert E. Factors influencing the coping of hospitalized school-age children. J Ped Nurs. (1994) 9:299–306.
16. Bossert E. Stress appraisals of hospitalized school-age children. Children's Health Care. (1994) 23:33–49. doi: 10.1207/s15326888chc2301_3
17. Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psych Bull. (2001) 127:87–127. doi: 10.1037/0033-2909.127.1.87
18. Eisenberg N, Fabes RA, Guthrie IK. Coping with stress: the roles of regulation and development. In: Wolchik SA, Sandler I, editors. Handbook of Children's Coping: Linking Theory and Intervention. NewYork, NY: Plenum (1997). doi: 10.1007/978-1-4757-2677-0_2
19. Skinner E, Edge K. Reflections on coping and development across the lifespan. Intern J Behav Dev. (1998) 22:357–66. doi: 10.1080/016502598384414
20. Skinner EA, Wellborn JG. Coping during childhood and adolescence: a motivational perspective. In: Featherman DL, Lerner RM, Perlmutter M. editors. Life-Span Development and Behavior. Life-Span Development and Behavior. Vol. 12 (Hillsdale, NJ: Lawrence Erlbaum. (1994). p. 91–133. doi: 10.4324/9781315789255-3
21. Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psych Bull. (2003) 129:216–69. doi: 10.1037/0033-2909.129.2.216
22. Skinner EA, Zimmer-Gembeck MJ. The development of coping. Ann Rev Psych. (2007) 58:119–44. doi: 10.1146/annurev.psych.58.110405.085705
23. Blount RL, Bunke VL, Zaff JF. Bridging the gap between explicative and treatment research: a model and practical implications. J Clin Psych in Med Sett. (2000) 7:79–90. doi: 10.1023/A:1009501604652
24. Carrey N, Ungar M. Resilience theory and the diagnostic and statistical manual: incompatible bed fellows? Child Adol Psych Clin of North Am. (2007) 16:497–513. doi: 10.1016/j.chc.2006.12.007
25. Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. J Cons Clin Psych. (1997) 65:453–63. doi: 10.1037/0022-006X.65.3.453
26. Blount RL, Bunke VL, Zaff JF. The integration of basic research, treatment research, and clinical practice in pediatric psychology. In: Drotar D, editors. Handbook of Research in Pediatric and Child Clinical Psychology: Practical Strategies and Methods. NewYork, NY: Kluwer Academic/Plenum Publishers. (2000). p. 491–510. doi: 10.1007/978-1-4615-4165-3_23
27. Zimmer-Gembeck MJ, Skinner EA. Review: the development of coping across childhood and adolescence: an integrative review and critique of research. Inter J Beh Dev. (2011) 35:1–17. doi: 10.1177/0165025410384923
28. Blount RL, Simons LE, Devine KA, Jaaniste T, Cohen LL, Chambers CT, et al. Evidence-based assessment of coping and stress in pediatric psychology. J Ped Psych. (2008) 33:1021–45. doi: 10.1093/jpepsy/jsm071
29. Ayers TS, Sandler IN, West SG, Roosa MW. A dispositional and situational assessment of children's coping: testing alternative models of coping. J Pers. (1996) 64:923–58. doi: 10.1111/j.1467-6494.1996.tb00949.x
30. Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary responses to stress. J Cons Clin Psych. (2000) 68:976–92. doi: 10.1037/0022-006X.68.6.976
31. Tobin DL, Holroyd KA, Reynolds RV, Wigal JK. The hierarchical factor structure of the coping strategies inventory. Cogn Ther Res. (1989) 13:343–61. doi: 10.1007/BF01173478
32. Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the pain response inventory for children. Psych Assess. (1997) 9:392–405. doi: 10.1037/1040-3590.9.4.392
33. Wilcox LN. Exploring Coping Skills of Hospitalized Children: A Children's Book Proposal. (2018). Retrieved from: https://pdfs.semanticscholar.org/e3a4/d3b7d6d96564d496305aac9d09ea62440c59.pdf (accessed August 20, 2019).
34. Thompson LM. Information-seeking coping and anxiety in school-age children anticipating surgery. Children's Health Care. (1994) 23:87–97. doi: 10.1207/s15326888chc2302_2
35. Wells RD, Schwebel AI. Chronically ill children and their mothers: Predictors of resilience and vulnerability to hospitalization and surgical stress. Devel Behav Ped. (1987) 8:83–9. doi: 10.1097/00004703-198704000-00004
37. Bjorklund DF, Green BL. The adaptive nature of cognitive immaturity. Am Psych. 47:46. doi: 10.1037//0003-066X.47.1.46
38. Moore ER, Bennett KL, Dietrich MS, Wells N. The effect of directed medical play on young children's pain and distress during burn wound care. J Ped Health Care. (2015) 29:265–73. doi: 10.1016/j.pedhc.2014.12.006
39. Nabors L, Bartz J, Kichler J, Sievers R, Elkins R, Pangallo J. Play as a mechanism for working through medical trauma for children with medical illnesses and their siblings. Issues Compr Ped Nurs. (2013) 36:212–24. doi: 10.3109/01460862.2013.812692
40. Salmela M, Salantera S, Ruotsalainen T, Aronen E. Coping strategies for hospital-related fears in pre-school-aged children. J Ped Child Health. (2010) 46:108–14. doi: 10.1111/j.1440-1754.2009.01647.x
41. Vygotsky LS. Play and its role in the mental development of the child. Sov Psych. (1967) 5:6–18. doi: 10.2753/RPO1061-040505036
43. Russ SW. Play in Child Development and Psychotherapy: Toward Empirically Supported Practice. Mahwah, NJ: Lawrence Erlbaum (2004).
44. Singer DG, Golinkoff RM, Hirsh-Pasek K. Play: How Play Motivates and Enhances Children's Cognitive and Social-Emotional Growth. New York, NY: Oxford University Press (2006).
45. Cordiano TJ, Russ SW, Short EJ. Development and validation of the affect in play scale-brief rating version (APS-BR). J Pers Ass. (2008) 90:52–60. doi: 10.1080/00223890701693744
46. Delvecchio E, Di Riso D, Li J-B, Lis A, Mazzeschi C. Affect in play scale preschool-version: validation on a sample of school age italian children. J Child Fam Stud. (2016) 25:3523–36. doi: 10.1007/s10826-016-0504-8
47. Delvecchio E, Mabilia D, Li J, Di Riso D. Pretend play in Italian children: validation of the affect in play scale-preschool version. J Child Fam Stud. (2016) 25:86–95. doi: 10.1007/s10826-015-0208-5
48. Delvecchio E, Li JB, Pazzagli C, Lis A, Mazzeschi C. How do you play? a comparison among children aged 4-10. Front Psych. (2016) 17:1833. doi: 10.3389/fpsyg.2016.01833
49. Di Riso D, Salcuni S, Lis A, Delvecchio E. From research to clinical settings: validation of the affect in play scale – preschool brief version in a sample of preschool and school aged Italian children. Front Psych. (2017) 12:728. doi: 10.3389/fpsyg.2017.00728
50. Fehr K, Russ SW. Assessment of pretend play in preschool-aged children: validation and factor analysis of the affect in play scale-preschool versions. J Pers Ass. (2014) 96:350–7. doi: 10.1080/00223891.2013.838171
51. Kaugars AS. Assessment of pretend play. In: Russ SW and Niec LN, editors. Play in Clinical Practice: Evidence Based Approaches. New York, NY: Guilford (2011). p. 51–82.
52. Kaugars AS, Russ SW. Assessing preschool children's pretend play: preliminary validation of the affect in play scale–preschool version. Early Educ De. (2009) 20:733–55. doi: 10.1080/10409280802545388
53. Li WHC, Chung JOK, Ho KY, Kwok BMC. Play interventions to reduce anxiety and negative emotions in hospitalized children. BMC Pediatr. (2016) 11:16–36. doi: 10.1186/s12887-016-0570-5
54. O'Connor K. Addressing diversity issues in play therapy. Profess Psych: Res Prac. (2005) 36:566–73. doi: 10.1037/0735-7028.36.5.566
55. Moore M, Russ SW. Pretend play as a resource for children: Implications for pediatricians and health professionals. J Dev Behav Pediatr. (2006) 27:237–48. doi: 10.1097/00004703-200606000-00011
56. Kazdin AE. Evidence-based assessment for children and adolescents: Issues in measurement development and clinical applications. J Clin Child Adol Psych. (2005) 34:548–58. doi: 10.1207/s15374424jccp3403_10
57. Mash EJ, Hunsley J. Evidence-based assessment of child and adolescent disorders: issues and challenges. J Clin Child Adol Psych. (2005) 34:362–79. doi: 10.1207/s15374424jccp3403_1
58. Altrichter H, Feldman A, Posch P, Somekh B. Teachers Investigate Their Work: An Introduction to Action Research Across the Professions, 2nd ed. London and NewYork, NY: Routledge (2008).
59. Bogdan R, Biklen SK. Qualitative Research for Education: An Introduction to Theories and Methods. Needham, MA: Allyn and Bacon (2006).
60. Cohen L, Manion L. Research Methods in Education, 5th ed. London and New-York, NY: Routledge (2000).
61. American Psychological Association. Publication Manual of the American Psychological Association, 6th ed. Washington, DC: American Psychological Association (2010).
62. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Meth. (2009) 41:1149–60. doi: 10.3758/BRM.41.4.1149
63. Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire). Palo Alto, CA: Consulting Psychologists Press (1970).
64. Spielberger CD, Edwards CD, Lushene RE, Montuori J, Platzek D. State-Trait Anxiety Inventory for Children – STAIC: Professional manual. Redwood City, CA: Mind Garden, Inc (1973).
65. Almerigogna J. Vérification de la structure factorielle d'une traduction française de l'Inventaire de l'Anxiété État-Trait pour Enfants. [Verifying the factorial structure of a French translation of the State-Trait Anxiety Inventory for Children]. Ann Méd Psychol. (2011) 169:345–47. doi: 10.1016/j.amp.2010.01.009
66. Delvecchio E, Cavallina C, Di Riso D, Mazzeschi C. Early evidence of the Italian validation of the trait anxiety scale of the state-trait anxiety inventory for children. Eur J of Dev Psych. (2017) 15:214–23. doi: 10.1080/17405629.2017.1297227
67. Ayers TS, Sandler IN. Manual for the Children's Coping Strategies Checklist & How I Coped Under Pressure Scale. (1999). Retrieved from: http://www.asu.edu/clas/asuprc/ (accessed June 10, 2006).
68. Camisasca E, Caravita SCS, Milani L, Di Blasio P. The Children's Coping Strategies Checklist-revision 1: A validation study in the Italian population. TPM. (2012) 19:197–218. doi: 10.4473/TPM19.3.4
69. Losoya S, Eisenberg N, Fabes RA. Developmental issues in the study of coping. Intern J Behav Dev. (1998) 22:287–313. doi: 10.1080/016502598384388
Keywords: anxiety, coping, symbolic play, hospitalized child, assessment
Citation: Delvecchio E, Salcuni S, Lis A, Germani A and Di Riso D (2019) Hospitalized Children: Anxiety, Coping Strategies, and Pretend Play. Front. Public Health 7:250. doi: 10.3389/fpubh.2019.00250
Received: 11 February 2019; Accepted: 20 August 2019;
Published: 06 September 2019.
Edited by:
Marie Leiner, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, United StatesReviewed by:
Prashanth GP, Oman Medical College, OmanCopyright © 2019 Delvecchio, Salcuni, Lis, Germani and Di Riso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniela Di Riso, ZGFuaWVsYS5kaXJpc29AdW5pcGQuaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.