- 1University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA, United States
- 2University of Pittsburgh Medical Center, Pittsburgh, PA, United States
- 3University of Maryland School of Medicine, Baltimore, MD, United States
Background: Telemedicine, or healthcare delivery from a distance, has evolved over the past 50 years and helped alter health care delivery to patients around the globe. Its integration into numerous domains has permitted high quality care that transcends obstacles of geographic distance, lack of access to health care providers, and cost. Ultrasound is an effective diagnostic tool and its application within telemedicine (“tele-ultrasound”) has advanced substantially in recent years, particularly in high-income settings. However, the utility of tele-ultrasound in resource-limited settings is less firmly established.
Objective: To determine whether remote tele-ultrasound is a feasible, accurate, and care-altering imaging tool in resource-limited settings.
Data Sources: PubMed, MEDLINE, and Embase.
Study Eligibility Criteria: Twelve original articles met the following eligibility criteria: full manuscript available, written in English, including a direct patient-care intervention, performed in a resource-limited setting, images sent to a remote expert reader for interpretation and feedback, contained objective data on the impact of tele-ultrasound.
Study Appraisal and Synthesis Methods: Abstracts were independently screened by two authors against inclusion criteria for full-text review. Any discrepancies were settled by a senior author. Data was extracted from each study using a modified Cochrane Consumers and Communication Review Group's data extraction template. Study bias was evaluated using the ROBINS-I tool.
Results: The study results reflect the diverse applications of tele-ultrasound in low-resource settings. Africa was the most common study location. The specialties of cardiology and obstetrics comprised most studies. Two studies primarily relied on smartphones for image recording and transmission. Real-time, rather than asynchronous, tele-ultrasound image interpretation occurred in five of the 12 studies. The most common outcome measures were image quality, telemedicine system requirements, diagnostic accuracy, and changes in clinical management.
Limitations: The studies included were of poor quality with a dearth of randomized control trials and with significant between study heterogeneity which resulted in incomplete data and made cross study comparison difficult.
Conclusions and Implications of Key Findings: Low-quality evidence suggests that ultrasound images acquired in resource-limited settings and transmitted using a telemedical platform to an expert interpreter are of satisfactory quality and value for clinical diagnosis and management.
Introduction
Background and Rationale
Global health encompasses both research and action aimed at promoting health for all persons, independent of national boundaries (1). Common barriers to global health initiatives include lack of healthcare access and lack of resources (2). Telemedicine (also called mHealth, telehealth, e-health), or literally “healing at a distance,” is a tool well-suited to reduce these barriers (3). The term telemedicine specifically refers to care provided by a physician whereas telehealth is a more global term that encapsulates care provided by all healthcare professionals (e.g., pharmacists, nurses) (4). While its manifestation and implementation can vary across different medical specialties, telemedicine universally attempts to utilize technology to provide clinical support to patients across geographical barriers in an effort to improve patient health outcomes (2). Telemedicine, therefore, functionally expands patient access to care by mitigating geographic barrier to healthcare (5).
The history of telemedicine dates back more than a century. An article published in the Lancet in 1879 describes the use of the telephone to reduce patient office visits (6). In the 1900's there were there are reports about physicians using the radio to make a medical diagnosis. In 1906, a paper was published by Willem Einthoven, the inventor of the electrocardiogram, about the use of tele-cardiogram. Einthoven used the telephone cable to transmit a signal from the hospital to his laboratory, 1.5 km away. He subsequently utilized telecardiogram to remotely analyze clinical EKGs from patients in the hospital. By the 1920's, telemedicine provided medical consultation from medical centers in Italy, Norway and France to patients aboard ships and on remote islands (6, 7). By the 1950's, the transmission of radiographic images began in the United States and occurred shortly thereafter in Canada (8). The United States National Aeronautics and Space Administration's (NASA) adopted telemedicine in the 1960's in an effort to ensure safety in space flight. What began as remote monitoring of biometric data in the 1960s gradually escalated to ensure that astronauts could receive an accurate diagnosis by onboard crewmates in the event of a medical emergency. NASA ultimately developed a terrestrial parallel program called Space Technology Applied to Rural Papago Health Care (STARPAHC) (9). In collaboration with the Tohono O'odham tribe of Southern Arizona and the Indian Health Service, NASA used rudimentary telemedicine technology to successfully connect patients in resource-limited areas with physicians at hospitals elsewhere in the state via mobile support units (10). Since then, the field of telemedicine has evolved rapidly, propelled by major technological advances including email, mobile phones, the internet, ultrasound technologies, videoconferencing, and smartphones.
As telemedicine evolved, the field of ultrasonography matured in parallel. By the 1990s, ultrasound technology had developed into a bedside tool that physicians, particularly emergency physicians, were routinely utilizing (11). Ultrasound is a safe (non-ionizing) and portable tool capable of being used in a diagnostic or interventional capacity. Ultrasound has both 2D and 3D capabilities, can be analyzed in real-time, and is a comparatively low-cost imaging modality (12). Moreover, a growing body of evidence demonstrates that bedside ultrasound is more accurate than conventional physical exam for cardiovascular diagnoses (13). In low- and middle-income countries (LMICs), ultrasound and plain radiographs are often the only available imaging modalities (14). As ultrasound machines became increasingly portable and as technologies to support data transmission became commercially available, adequate infrastructure could support the emergence of tele-ultrasound. The tele-ultrasound paradigm involves performing bedside ultrasound at one location with images transmitted and interpreted by a provider located in a geographically distant location. This process can be conducted either in a synchronous, or real-time manner, or in an asynchronous manner. Asynchronous tele-ultrasound utilizes a store-and-forward technique in which images are captured, stored, and later transmitted for image interpretation. Tele-ultrasound offered a seamless solution for skeptics of telemedicine who questioned the ability to ascertain a meaningful physical examination from afar.
Studies based in high-income countries suggest that tele-ultrasound is clinically valuable. Tele-ultrasound has been successfully used in diverse settings, including telecardiology consultation for neonatal units in Northern Ireland, airplanes in flight, Antarctic research stations, even at the International Space Station (15–18). Furthermore, studies have clearly demonstrated that images can be reliably transmitted between geographically distinct locations without loss of clinically important image quality via commercially available two-way audiovisual technology (19–21). Instrumental to the evolution and global utilization of tele-ultrasound was the finding that minimally trained sonographers can acquire high quality images using real-time guidance from experts afar, an infrastructure called remote tele-mentored ultrasound (RTMUS) (20, 22). RTMUS utilizes a single centrally-located physician trained in bedside ultrasound who guides a geographically-removed bedside provider in image acquisition and performs image interpretation from afar. Early work in high-income countries demonstrated that remote tele-mentored ultrasound was feasible and accurate in cardiac, trauma, and critical care applications (22–25).
Objective
Tele-ultrasound is increasingly used to provide global health care. Even in high-income countries, patient care is frequently limited by a lack of access to trained clinicians. This supply-demand mismatch is further exaggerated in resource-limited settings where a dearth of subspecialty and procedurally-trained physicians often exists and the resources available to those physicians may be limited by economic constraints. The use of tele-ultrasound in resource-limited countries is, therefore, a rapidly burgeoning field. Due to the topic's clinical significance, a need exists to aggregate the various studies on the topic of tele-ultrasound in resource-limited settings. The goal of this paper is to systematically review the literature to determine whether remote tele-ultrasound is a feasible and accurate imaging modality that alters the care provided to patients in resource-limited settings compared to the standard of care. To our knowledge, no prior systematic review has been conducted on this topic.
Methods
Design and Study Selection
We performed a review of all published reports of tele-ultrasound in resource-limited settings. This review follows the PRISMA guidance for systematic reviews (26). We included full manuscripts written in the English language and we excluded non-human studies, studies using exclusively 1D ultrasound, review articles, abstracts, case reports, and editorials. Inclusion criteria required: (1) a direct patient-care intervention; (2) performance in a resource-limited setting; (3) patient ultrasound images sent to a remote, expert reader for interpretation and feedback; and (4) objective data on the clinical impact of tele-ultrasound. In this study, we defined resource-limited settings as low-resource areas in LMICs. We excluded studies conducted in remote areas of resource-abundant countries. Studies that involved images collected by robotic arm or under the aide of virtual reality technologies were excluded. Only studies published before January 1, 2019 were included.
Search Strategy
The literature search was conducted under the direction of the University of Maryland Health Sciences and Human Services Library Systematic Review Consultation Service (Baltimore, MD, USA). Databases searched include PubMed, MEDLINE, and Embase. Search terms included “ultrasound” AND “telemedicine” AND “resource-limited” present in the title or abstract, as well as common synonyms, including sonography, eHealth, developing world, and more (detailed electronic search strategy including relevant MESH terms for PubMed and MEDLINE and Emtree/exploded terms for Embase in Supplementary Materials 1.1 and 1.2, respectively). Relevant MESH and Emtree/exploded terms were also included. The database searches were completed on February 1, 2019 with all manuscripts published prior to January 1, 2019 evaluated for eligibility for inclusion in this review. Next, we searched the references of included papers to identify additional studies meeting inclusion criteria.
Two authors independently screened abstracts and selected candidate articles for full text review. If either author wanted to include a study for full text review, the full text was reviewed in its entirety. Full text review of remaining studies based on inclusion and exclusion criteria identified the final group of studies. A senior author settled any discrepancy in article selection between the two initial authors.
Data Extraction and Analysis
Data extracted from each study included: study type, study location, publication year, tele-ultrasound method (real-time vs. asynchronous), sample size, patient demographics, organ system assessed, available cost data, ultrasound performer training level, interpreter training level and location, ultrasound type, telemedicine platform, and clinical outcomes. Descriptive statistics were used to report trends in the performer training level, specialty, and outcome measured.
Bias Assessment
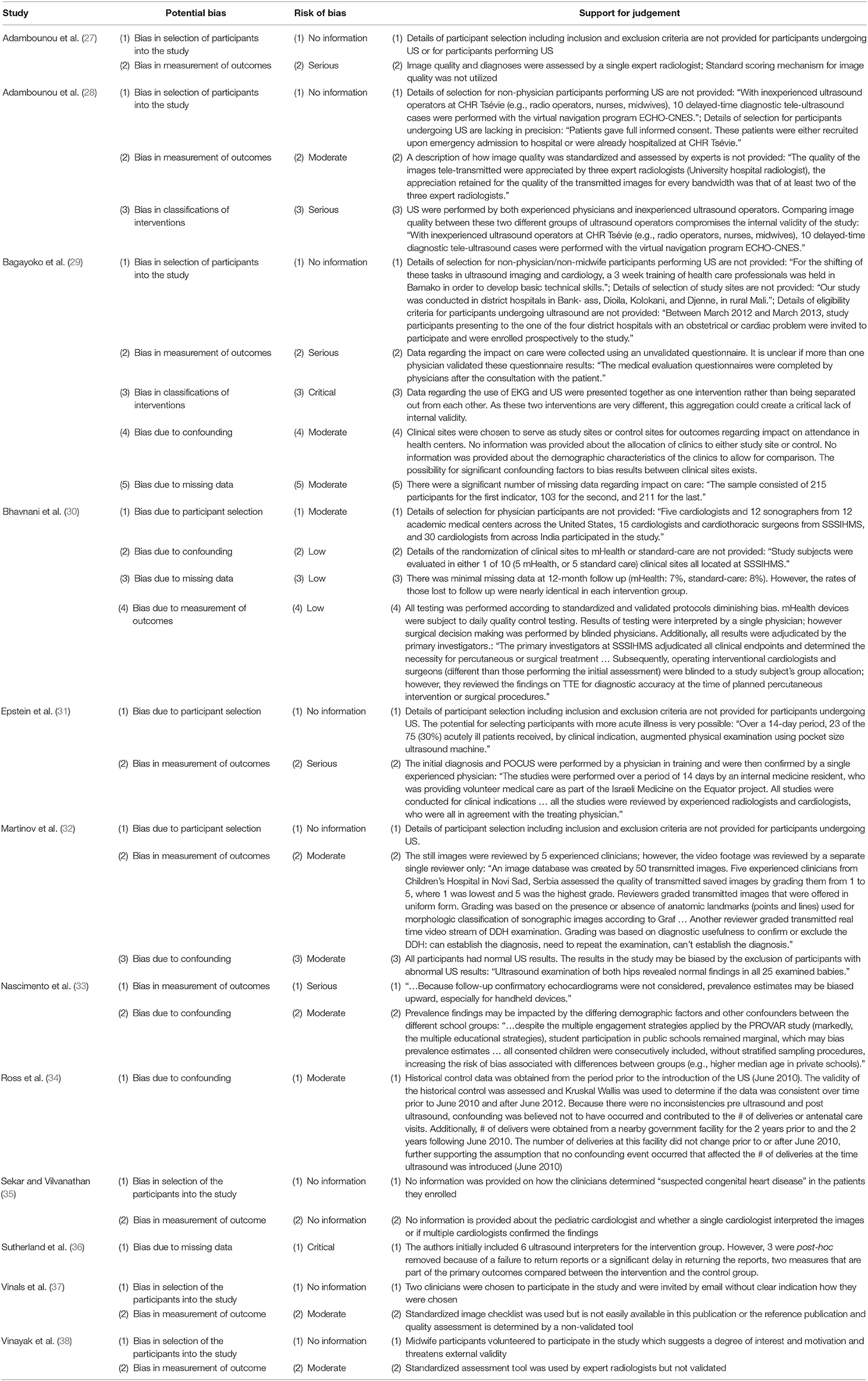
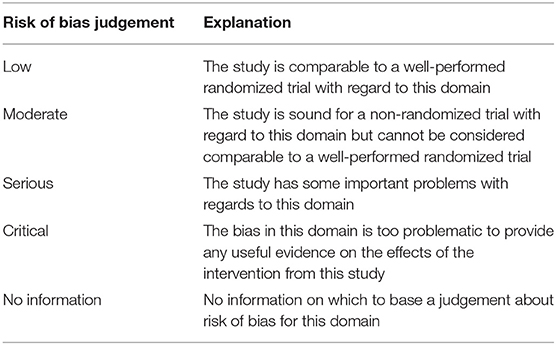
We utilized a tool adapted from the ROBINS-I from the Cochrane collaboration in order to evaluate bias at an individual study level (Table 1) (39). The quality of the studies included in this systematic review was poor which precluded any further quantitative data analysis.
Summary Measures and Synthesis of Results
No summary measures were utilized in this narrative systematic review. The heterogeneity and quality of the studies prevented data from being combined or any formal measures of data consistency to be performed. Furthermore, due to the data quality, no meta-analysis was performed and there is no plan for a follow up meta-analysis.
Results
Search Results
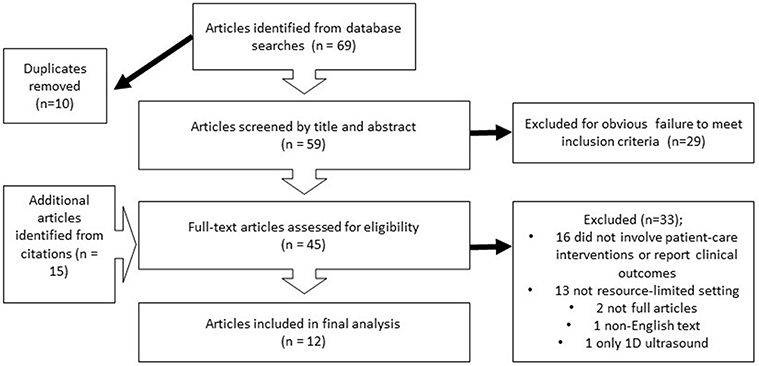
A literature search conducted in PubMed, MEDLINE, and Embase resulted in 69 articles with filters for English language and human subjects applied. Ten duplicates were removed for a total of 59 unique articles. After title and abstract review, 29 articles were removed due to failure to meet inclusion criteria. Fifteen additional articles were identified from citations. Of the remaining 45 articles that underwent full text evaluation, 16 were removed for either not involving a patient-care intervention or not reporting clinical outcomes, 13 were eliminated for failing to meet criteria for a resource-limited setting, and two abstracts without accompanying manuscripts were removed (one had an English title and abstract but foreign language full text; one utilized only 1D ultrasound). A total of 12 studies were included in the final analysis (27–38). A schematic of the study search and selection process is shown in Figure 1.
Risk of Bias
We utilized the ROBINS-I tool provided by the Cochrane Collaboration to assess for bias within each individual study. The majority of the studies evaluated were non-randomized control trials, making the ROBINS-I tool most appropriate. The results of the bias evaluation are shown in Table 1. Explanation of the risk judgement categories are shown in Table 2. The heterogeneity of the studies and the lack of principal summary measures in the majority of the studies made any evaluation of between study bias using a tool such as GRADE meaningless (40).
Synthesized Findings
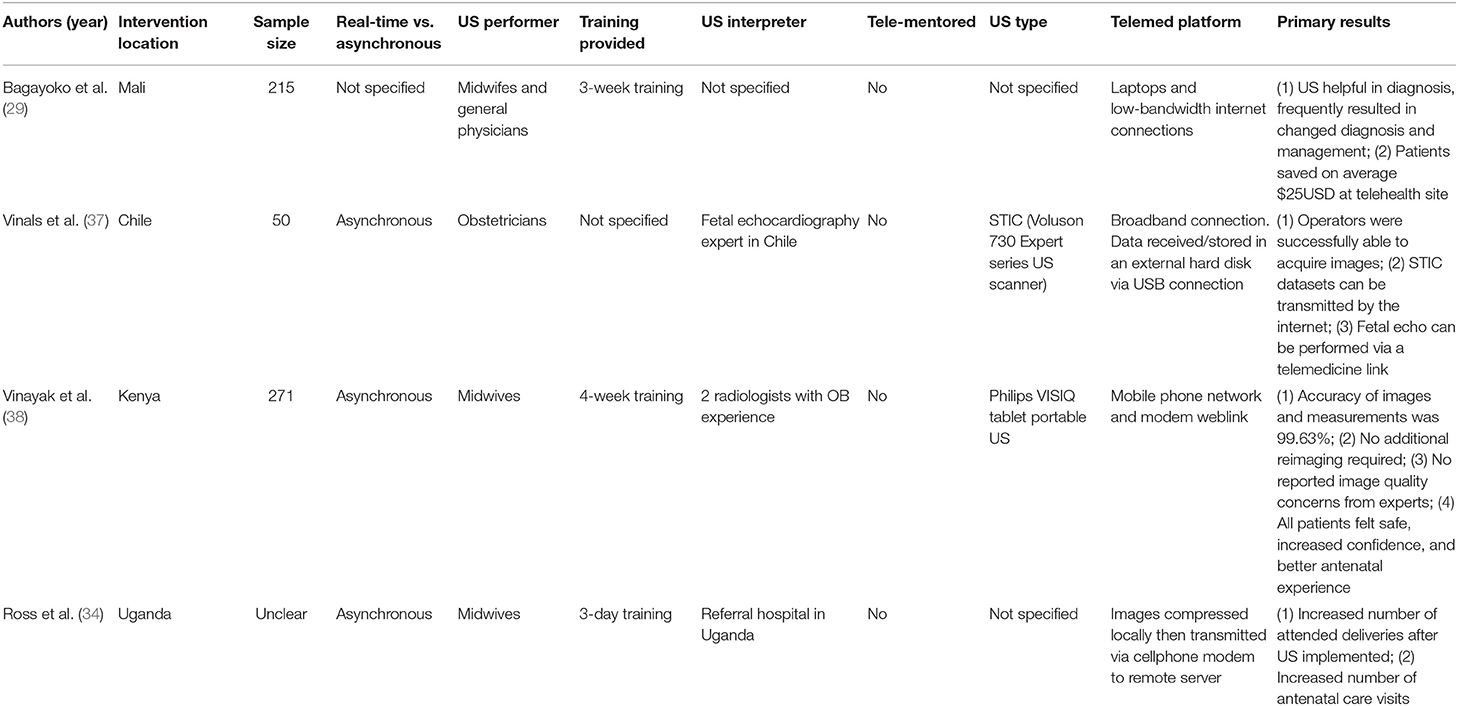
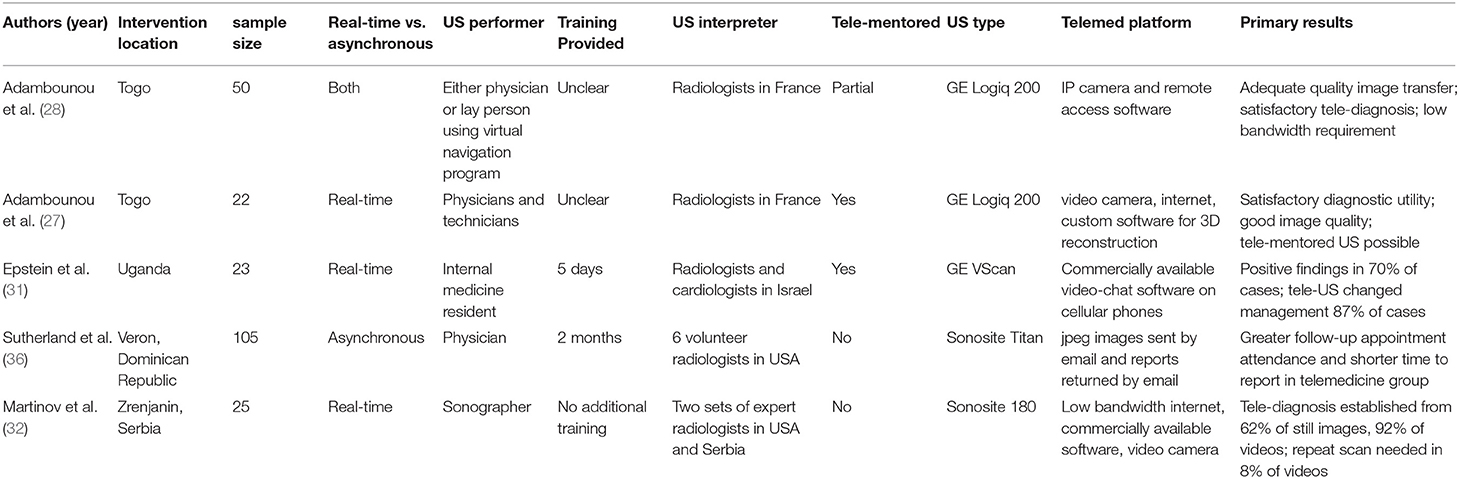
The results of the included studies are summarized in Tables 3–5. The studies were conducted over diverse geographic locations. Of the twelve studies, six were in Africa (two in Togo, one in Mali, two in Uganda, one in Kenya), two in South Asia (India), two in South America (Chile and Brazil), one in Europe (Serbia), and one in the Caribbean (Dominican Republic). The study size ranged from 22 subjects to 12,048. Four of the studies were pilot or feasibility studies and two were single-site randomized trials with patients enrolled into either an experimental arm (telemedicine) or control (standard care that did not include telemedicine) arm.
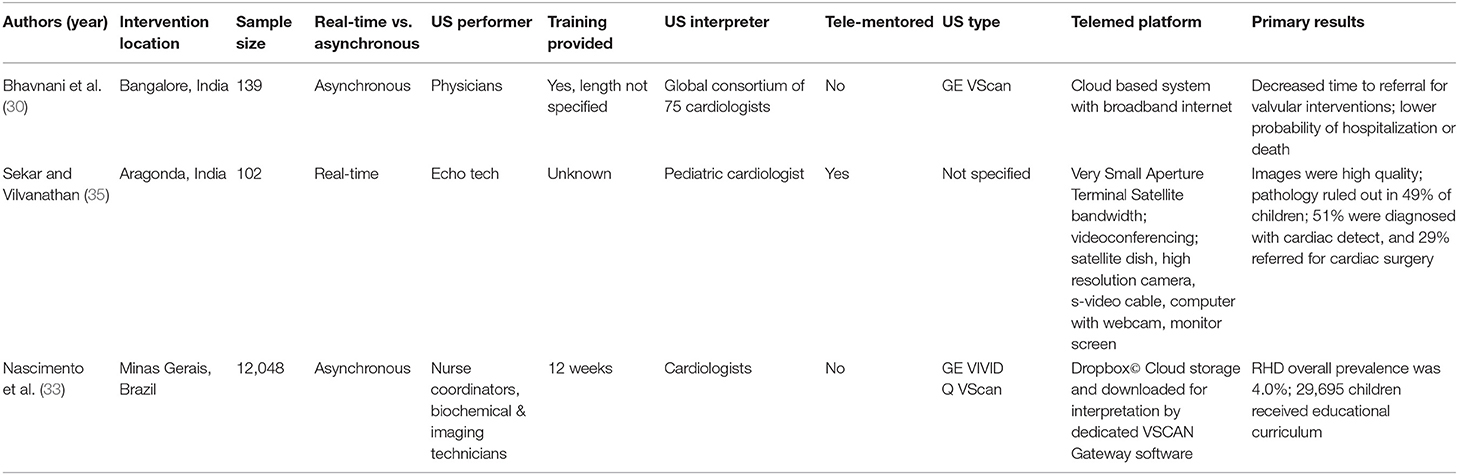
Hospitalized patients were enrolled in five studies, outpatients in clinics were enrolled in six studies, and patients in both schools and clinics were enrolled in one study. The medical scope of the studies varied widely. Four studies primarily involved obstetrics (Table 3), three studies focused on cardiology (Table 4), and five studies focused on general practice or other specialties (Table 5). Five studies were designed as screening programs accomplished by tele-ultrasound.
Pocket and other portable ultrasound machines were the most commonly used ultrasound devices. In five studies, video images were captured via the ultrasound machine. Still images were captured in two studies, but the type of image capture was not specified in four studies. All studies required internet access. Four studies were designed to operate using low-bandwidth connections. Four studies used cameras to record images from the screen of the ultrasound machine, while the remaining eight studies sent ultrasound images without the use of camera recordings. Two studies relied on smartphones for image recording and transmission, and two studies utilized satellite for internet connectivity.
Substantial study diversity existed regarding who functioned as the bedside ultrasonographer and the level of expertise of the image interpreter. Physicians and midwives scanned patients in nine of the twelve studies. Scans were also obtained by trained sonographers, technicians, and non-healthcare professionals. Remote interpreters were dispersed around the globe. When the ultrasonographer and interpreter were in the same country, the interpreter was generally found at a large academic or major referral center. All image interpreters were trained radiologists or cardiologists. Tele-ultrasound was performed synchronously in four studies and asynchronously in six studies. Both methods were used in one study, and it was not specified which method was used in a final study. Remote tele-mentored ultrasonography was used in four of the twelve studies.
The most commonly reported outcome in the twelve studies was diagnostic utility of tele-ultrasound (eight studies), followed by assessment of image quality (six studies). Other reported outcomes include management impact of tele-ultrasound (four studies), telemedicine system requirements (four studies), impact on follow-up (four studies), data transmission reliability and quality (three studies), effectiveness of education program for ultrasound examiner (two studies), patient cost savings (two studies), time to referral or follow-up (two studies), likelihood of hospitalization or adverse outcome (one study), and patient satisfaction with tele-ultrasound (one study). All the studies showed generally positive results for the primary outcome measures that were assessed.
Cost was a commonly addressed concern throughout the included studies, with an emphasis on the need for affordable tele-ultrasound platforms to make its use feasible in low-resource settings. Several of the studies built telemedicine platforms using open-source or low-cost, commercially available software, over-the-counter hardware, and low-cost portable ultrasound machines in an effort to minimize costs. Two studies explored cost from the patients' perspective and found that the introduction of tele-ultrasound was associated with lower out-of-pocket costs for the patient, generally due to minimizing need for travel to larger medical centers with formal imaging capacity.
Our formal analysis of bias using the ROBINS-I tool identified significant potential risks of bias in most of the studies. The majority of the studies had both a risk of bias in measurement of outcomes (ten studies) and in the selection of participants into the study (nine studies). Due to inconsistencies in study outcomes reported, the lack of principal summary measures, and the low quality of the studies included which primarily encompassed technical feasibility and observational studies with few randomized control trials, no meta-analysis was performed.
Discussion
Summary of Main Findings
This systematic review suggests that tele-ultrasound performed in resource-limited settings can reliably produce satisfactory images with diagnostic utility that guide clinical management. According to the World Health Organization (WHO), imaging is needed for diagnosis in 20–30% of clinical cases and ultrasound and/or plain radiographs are sufficient for 80–90% of those cases. Yet, two-thirds of the world's population remains without access to medical imaging (14). Ultrasound, integrated into a telemedicine platform expands access to a safe, accessible, and affordable diagnostic imaging modality to populations in resource-limited settings.
Globally, ultrasound is a burgeoning diagnostic tool that often offers more insight into patient pathophysiology than the stethoscope. Thoracic ultrasound, as compared to chest radiography, has a high sensitivity and specificity for diagnosing cardiogenic pulmonary edema, pneumonia, COPD, pneumothorax, and pulmonary embolism in both the intensive care unit and the emergency department (41, 42). In fact, lung ultrasound is superior to chest radiograph in diagnosing pneumonia in the emergency department (43). In resource-limited settings, lung ultrasound was more sensitive and specific than chest radiograph to diagnose pneumonia (44). Furthermore, point-of-care ultrasound can be incorporated into a telemedicine platform and performed with relatively little training by non-physicians located at the bedside under the real-time guidance from ultrasound experts (20, 21, 45, 46). Thus, the use of RTMUS obviates the need for a bedside ultrasound expert to acquire images or a local expert to interpret them. RTMUS is particularly relevant in resource-limited settings in LMICs, where a scarcity of physicians often exists with expertise in ultrasound or with training in ultrasound-heavy subspecialties such as cardiology or obstetrics. Task-shifting ultrasound performance away from formally-trained sonographers and physicians to non-experts, while maintaining high quality imaging, helps establish a sustainable and cost-effective telemedicine program (47). This task-shifting also dramatically expands patient access to otherwise inaccessible subspecialists.
The studies included in this systematic review reinforce the concept that adequate ultrasound acquisition techniques can be taught in a remote tele-mentored manner. In cardiac ultrasound (Table 4), the high success rates for visualization of anatomic structures by non-experts allows for changes in medical management in the absence of a bedside physician. These changes include earlier treatment and appropriate escalation of care to tertiary centers (37). By utilizing non-experts as ultrasonographers, a larger population of patients gains access to ultrasonography as a diagnostic tool and to cardiology expertise. In this review, non-experts included physicians unfamiliar with a designated ultrasound approach, nurse research coordinators, a biomedical technician, and an imaging technician. Additional studies that did not meet the requirements for this review included custodians and medical interpreters as the non-experts performing the ultrasound (20). Collectively, these studies inform the conclusion that the quality of the ultrasound images obtained by non-experts are sufficient for interpretation by experts remotely.
Our literature review indicates that tele-ultrasound was frequently used in the field of cardiology (Table 4). Tele-ultrasound has demonstrated success in producing high quality, diagnostically significant images which alter management, decrease time to treatment, and provide more cost-effective care, especially when coupled with supporting data such as electrocardiogram, chest radiography, laboratory results, and clinical history (29, 30, 33, 35, 37, 48). In Aragonda, India, the use of remote tele-mentored echocardiography allowed for the diagnosis of pediatric cardiovascular pathology, resulting in a 29% referral for cardiac surgery based on those findings (35). In Bangladore, India, tele-ultrasound was used to assess times to treatment and long-term outcomes among children with structural heart disease. Images were collected in asynchronously and interpreted by a global consortium of cardiologists. Tele-ultrasound reduced the time to referral for valvular interventions and reduced the likelihood of both hospitalization and death (30). Though uncommon in high-income countries and likely underreported in low-income ones, rheumatic heart disease (RHD) is a major source of morbidity and mortality in LMICs (49). In the PROVAR study from Brazil, non-expert ultrasonographers successfully screened schoolchildren for RHD and images were interpreted by geographically-removed experts (33). Collectively, cardiology-based tele-ultrasound studies demonstrate the transformative potential of utilizing this imaging modality in a resource-limited setting as a tool to better understand the epidemiological impact of a disease and to improve disease management and outcomes.
Obstetrics is an additional medical specialty in which ultrasound is heavily utilized around the globe (50). Unfortunately, supply of ultrasound machines, sonographers, and radiologists in LMICs is very low. For example, only two radiologists work in Liberia (51). In an attempt to overcome such challenges, ultrasound training programs have taught non-experts either to independently perform obstetric ultrasounds to screen for high-risk pregnancies (52–55) or to utilize tele-ultrasound (29, 34, 37, 38). Of the multiple studies addressing the role of tele-ultrasound in resource-limited countries, the four included in this review focus on the obstetrics tele-ultrasound evaluation (Table 3). Ultrasonographers included physicians and midwives without prior obstetrics ultrasound training, but none of the obstetrics studies utilized RTMUS. Collectively, these studies concluded that ultrasound acquired accurate fetal structural views, allowed for the modification of perinatal care, and helped facilitate transfer to specialty centers when needed. Tele-ultrasound performed by a novice ultrasonographer prevented the need for additional re-imaging and yielded results available to the patient within 15 min. Image acquisition can be taught from a distance via the internet and a telemedicine platform is reliably able to transmit high quality images (29, 34, 37, 38).
Most of the studies included in this review implemented a brief training program for novice bedside ultrasonographers, regardless of the use of remote tele-mentored, real-time instruction. The training courses offered ranged from 3 days to 3 months. No correlation existed between the ultrasonographer's length of training and ability to adequately perform bedside ultrasound. Based on research not included in this systematic review, synchronous RTMUS can be successfully performed with <60 min of training (20, 21, 45, 46).
To date, we are unaware of any studies directly comparing synchronous to asynchronous telemedicine or tele-ultrasound. However, we believe an implicit benefit exists with using synchronous tele-ultrasound. Real-time image acquisition is well-suited to be combined with remote tele-mentoring to establish a hub-and-spoke paradigm whereby a single trained ultrasonographer can mentor numerous geographically removed ultrasound-naïve bedside providers to maximize the global reach of tele-ultrasound. By capitalizing on the concept of task-shifting inherent to RTMUS, any person located at the patient's bedside can function as the bedside ultrasonographer. Furthermore, real-time image acquisition and interpretation reduces delays in patient care and the need to return for follow up images, which may occur in an asynchronous point-and-store model of tele-ultrasound. Synchronous image acquisition also allows for real-time image quality control. As technology improves, wireless network and mobile phone access become more globally reliable, and commercially-available real-time audiovisual software (e.g., Skype, FaceTime) develop HIPAA-compliant platforms, the use of synchronous, RTMUS systems will be universally within reach.
The potential impacts of tele-ultrasound in LMICs are substantial with regard to the scope and breadth of both the numerous clinical areas (e.g., respiratory failure, hemodynamic compromise, procedural guidance) and the stakeholders (e.g., patients, providers, health systems) affected. The results of this systematic review, however, should be interpreted within the pre-established boundaries defined by the question we sought to answer using existing relevant studies. Specifically, this review addresses the feasibility of tele-ultrasound in LMICs and its clinical benefit to patients. Though certainly relevant to public health, this review was not intended to analyze the potential economic or workflow impacts of this technology on the health care providers or the health care system within each country. As public policy lies at the intersection of economic analysis and patient benefit, this systematic review cannot independently support changes to public policy but instead serves to further highlight the important clinical impact on patients.
Limitations
Several limitations and biases impacted this review. It is possible that some articles were not assessed for eligibility due to the constraints of English language-only texts or articles not indexed on PubMed, MEDLINE, or Embase. Our goal was to capture those studies that utilized tele-ultrasound in resource-limited settings that involved direct patient care investigations and reported those outcomes accordingly. Excluding remote areas of high-income countries from our definition of resource-limited settings changed the available group of studies. While many important investigations have examined tele-ultrasound in remote settings of high-income countries (15, 16, 56), we chose to examine LMICs specifically in this review due to the fundamental differences in financial resources, healthcare personnel training and availability, health systems, and infrastructure that separate high-income countries from LMICs. Similar reasoning explains the exclusion of studies using robotic arm and virtual reality technologies. Several studies on the topic of tele-ultrasound in resource-limited settings were not included because they did not report a patient care intervention or meaningful clinical outcomes (20, 57–60). These studies were excluded because the goal of this review was to highlight those studies most germane to clinical practice, and studies in non-clinical environments that do not collect results relating to patient care are less easily clinically applicable.
The breadth of tele-ultrasound utilization was reflected in the marked heterogeneity of study designs. These varied designs led to different goals, outcomes, and reported data; moreover, their differences resulted in incomplete data when comparing studies. Many of the reported outcomes are related to technical feasibility or image quality interpretation and this evaluation is entirely subjective without the use of any standardized or validated measurement. This was compounded by the reality that the articles themselves were generally low quality and deemed as having a moderate to severe risk for bias, ranging from the selection of patients to be included in the study to bias regarding the selection of outcomes evaluated (Table 1). The high risk of bias in the majority of the included studies does limit the internal validity of the included studies. The missingness of reported data among the studies including the study design, patient selection, and participant selection limited the comparison of outcomes between studies. Control groups and randomization were rare. Nearly one-third of the studies were either pilot or feasibility studies. Collectively, this prevented substantial quantitative analysis of these studies and would certainly preclude any quantitative synthesis of the results into a meta-analysis. While all the articles reflected the promise of tele-ultrasound in resource-limited settings, the need for higher quality evidence in the future is obvious.
Conclusions
The global burden of disease in resource-limited countries often outpaces the access to diagnostic modalities needed to identify disease and the availability of trained clinicians to treat disease. This supply-demand mismatch makes ultrasound a precious tool in resource-limited countries. Ultrasound is a low-cost, reliable, diagnostic tool which can be performed by minimally-trained bedside providers. Over the last quarter century, numerous advances have precipitated the feasibility and success of remote tele-ultrasound in resource-limited settings. Technologically speaking, ultrasound machines have become smaller, more portable and durable, and the relative cost has decreased dramatically. Smartphones are becoming more commonplace and seamlessly operate numerous software options which are capable of functioning as affordable handheld telemedicine platforms. Lastly, global connectivity is increasing, particularly wireless cellular and internet access. These advances, in concert, have made tele-ultrasound feasible and invaluable in resource-limited settings.
Author Contributions
MAM performed initial systematic review and first draft of manuscript. SS helped with initial review and with manuscript edits. AS contributed to initial manuscript review of manuscripts included in systematic review and initial drafting of manuscript. AL edited manuscript and contributed to bias analysis. MTM oversaw project, involved in systematic review, and involved in drafting and revising the manuscript. NB performed bias analysis, revised paper to include bias analysis, and performed manuscript edits for second and third submission of paper.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank the University of Maryland Health Sciences and Human Services Library Systematic Review Consultation Service (Baltimore, MD, USA) for their guidance with the literature search.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2019.00244/full#supplementary-material
References
1. Beaglehole R, Bonita R. What is global health? Glob Health Action. (2010) 3:5142. doi: 10.3402/gha.v3i0.5142
2. WHO. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth. Geneva: World Health Organization (2011).
3. Strehle EM, Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics? Arch Dis Child. (2006) 91:956–9. doi: 10.1136/adc.2006.099622
4. Federal Communications Commission. Telehealth, Telemedicine and Telecare: What's What? (2014). Available online at: https://www.fcc.gov/general/telehealth-telemedicine-and-telecare-whats-what (accessed April 1, 2019).
5. Lugn NE. Global health care—bridging the gap. J Telemed Telecare. (2006) 12:109–10. doi: 10.1258/135763306776738576
6. Board on Health Care Services. The Evolution of Telehealth: Where Have We Been and Where Are We Going? Washington, DC: National Academies Press, Institute of Medicine (2012). doi: 10.1093/oxfordhb/9780199603329.013.0049
7. Moukabary T. Willem Einthoven (1860–1927): father of electrocardiography. Cardiol J. (2007) 14:316–7.
8. Ryu S. History of telemedicine: evolution, context, and transformation. Healthc Inform Res. (2010) 16:65. doi: 10.4258/hir.2010.16.1.65
9. Perednia DA, Allen A. Telemedicine technology and clinical applications. JAMA. (1995) 273:483–8. doi: 10.1001/jama.273.6.483
10. Freiburger G, Holcomb M, Piper D. The STARPAHC collection: part of an archive of the history of telemedicine. J Telemed Telecare. (2007) 13:221–3. doi: 10.1258/135763307781458949
12. Baran JM, Webster JG. Design of low-cost portable ultrasound systems: review. In: 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society (Minneapolis, MN) (2009). p. 792–5. doi: 10.1109/IEMBS.2009.5332754
13. Kobal SL, Trento L, Baharami S, Tolstrup K, Naqvi TZ, Cercek B, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. (2005) 96:1002–6. doi: 10.1016/j.amjcard.2005.05.060
14. WHO Department of Essential Health Technologies. Essential Diagnostic Imaging. www.who.int/eht. World Health Organization (2018). Available online at: https://web.archive.org/web/20121023154427/http://www.who.int/eht/en/DiagnosticImaging.pdf (accessed March 1, 2019).
15. Mulholland HC, Casey F, Brown D, Corrigan N, Quinn M, McCord B, et al. Application of a low cost telemedicine link to the diagnosis of neonatal congenital heart defects by remote consultation. Heart. (1999) 82:217–21. doi: 10.1136/hrt.82.2.217
16. McBeth PB, Crawford I, Blaivas M, Hamilton T, Musselwhite K, Panebianco N, et al. Simple, almost anywhere, with almost anyone: remote low-cost telementored resuscitative lung ultrasound. J Trauma. (2011) 71:1528–35. doi: 10.1097/TA.0b013e318232cca7
17. Garcia KM, Harrison MF, Sargsyan AE, Ebert D, Dulchavsky SA. Real-time ultrasound assessment of astronaut spinal anatomy and disorders on the international space station. J Ultrasound Med. (2018) 37:987–99. doi: 10.1002/jum.14438
18. Otto C, Shemenski R, Scott JM, Hartshorn J, Bishop S, Viegas S. Evaluation of tele-ultrasound as a tool in remote diagnosis and clinical management at the Amundsen-Scott South Pole Station and the McMurdo Research Station. Telemed J E Health. (2013) 19:186–91. doi: 10.1089/tmj.2012.0111
19. Zennaro F, Neri E, Nappi F, Grosso D, Triunfo R, Cabras F, et al. Real-time tele-mentored low cost “Point-of-Care US” in the hands of paediatricians in the emergency department: diagnostic accuracy compared to expert radiologists. PLoS ONE. (2016) 11:e0164539. doi: 10.1371/journal.pone.0164539
20. Robertson TE, Levine AR, Verceles AC, Buchner JA, Lantry JH 3rd, Papali A, et al. Remote tele-mentored ultrasound for non-physician learners using FaceTime: A feasibility study in a low-income country. J Crit Care. (2017) 40:145–8. doi: 10.1016/j.jcrc.2017.03.028
21. Levine AR, Buchner JA, Verceles AC, Zubrow MT, Mallemat HA, Papali A, et al. Ultrasound images transmitted via FaceTime are non-inferior to images on the ultrasound machine. J Crit Care. (2016) 33:51–5. doi: 10.1016/j.jcrc.2016.02.019
22. Afset JE, Lunde P, Rasmussen K. Accuracy of routine echocardiographic measurements made by an inexperienced examiner through tele-instruction. J Telemed Telecare. (1996) 2:148–54. doi: 10.1258/1357633961929970
23. Boniface KS, Shokoohi H, Smith ER, Scantlebury K. Tele-ultrasound and paramedics: real-time remote physician guidance of the Focused Assessment With Sonography for Trauma examination. Am J Emerg Med. (2011) 29:477–81. doi: 10.1016/j.ajem.2009.12.001
24. Dyer D, Cusden J, Turner C, Boyd J, Hall R, Lautner D, et al. The clinical and technical evaluation of a remote telementored telesonography system during the acute resuscitation and transfer of the injured patient. J Trauma. (2008) 65:1209–16. doi: 10.1097/TA.0b013e3181878052
25. Olivieri PP, Verceles AC, Hurley JM, Zubrow MT, Jeudy J, McCurdy MT. A pilot study of Ultrasonography-Naïve Operators' ability to use tele-ultrasonography to assess the heart and lung. J Intensive Care Med. (2018). doi: 10.1177/0885066618777187. [Epub ahead of print].
26. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
27. Adambounou K, Farin F, Boucher A, Adjenou KV, Gbeassor M, N'dakena K, et al. Preliminary experience with tele-sonography and tele-mammography in Togo. Diagn Interv Imaging. (2012) 93:639–42. doi: 10.1016/j.diii.2012.03.020
28. Adambounou K, Adjenou V, Salam AP, Farin F, N'Dakena KG, Gbeassor M, et al. A low-cost tele-imaging platform for developing countries. Front Public Health. (2014) 2:135. doi: 10.3389/fpubh.2014.00135
29. Bagayoko CO, Traoré D, Thevoz L, Diabaté S, Pecoul D, Niang M, et al. Medical and economic benefits of telehealth in low- and middle-income countries: results of a study in four district hospitals in Mali. BMC Health Serv Res. (2014) 14 (Suppl. 1):S9. doi: 10.1186/1472-6963-14-S1-S9
30. Bhavnani SP, Sola S, Adams D, Venkateshvaran A, Dash PK, Sengupta PP, et al. A randomized trial of pocket-echocardiography integrated mobile health device assessments in modern structural heart disease clinics. JACC Cardiovasc Imaging. (2018) 11:546–57. doi: 10.1016/j.jcmg.2017.06.019
31. Epstein D, Petersiel N, Klein E, Marcusohn E, Aviran E, Harel R, et al. Pocket-size point-of-care ultrasound in rural Uganda—A unique opportunity “to see”, where no imaging facilities are available. Travel Med Infect Dis. (2018) 23:87–93. doi: 10.1016/j.tmaid.2018.01.001
32. Martinov D, Ignjatov Z, Markovic D. Low cost telesonography model for DDH exam. Int J Video Image Process Netw Secur. (2010) 10:14–20.
33. Nascimento BR, Sable C, Nunes MCP, Diamantino AC, Oliveira KKB, Oliveira CM, et al. Comparison between different strategies of rheumatic heart disease echocardiographic screening in brazil: data from the PROVAR (Rheumatic Valve Disease Screening Program) study. J Am Heart Assoc. (2018) 7:8039. doi: 10.1161/JAHA.117.008039
34. Ross AB, DeStigter KK, Rielly M, Souza S, Morey GE, Nelson M, et al. A low-cost ultrasound program leads to increased antenatal clinic visits and attended deliveries at a health care clinic in rural Uganda. PLoS ONE. (2013) 8:e78450. doi: 10.1371/journal.pone.0078450
35. Sekar P, Vilvanathan V. Telecardiology: effective means of delivering cardiac care to rural children. Asian Cardiovasc Thorac Ann. (2007) 15:320–3. doi: 10.1177/021849230701500411
36. Sutherland JE, Sutphin HD, Rawlins F, Redican K, Burton J. A comparison of telesonography with standard ultrasound care in a rural Dominican clinic. J Telemed Telecare. (2009) 15:191–5. doi: 10.1258/jtt.2009.080909
37. Vinals F, Mandujano L, Vargas G, Giuliano A. Prenatal diagnosis of congenital heart disease using four-dimensional spatio-temporal image correlation (STIC) telemedicine via an Internet link: a pilot study. Ultrasound Obstet Gynecol. (2005) 25:25–31. doi: 10.1002/uog.1796
38. Vinayak S, Sande J, Nisenbaum H, Nolsøe CP. Training midwives to perform basic obstetric point-of-care ultrasound in rural areas using a tablet platform and mobile phone transmission technology—A WFUMB COE project. Ultrasound Med Biol. (2017) 43:2125–32. doi: 10.1016/j.ultrasmedbio.2017.05.024
39. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
40. Schünemann H, Brozek J, Guyatt G, Oxman A. Grade Handbook: Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach. Grading of Recommendations, Assessment, Development and Evaluation (GRADE) Working Group (2018). Available online at: https://gdt.gradepro.org/app/handbook/handbook.html#h.hnedbo8gqjqk
41. Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. (2008) 134:117–25. doi: 10.1378/chest.07-2800
42. Bekgoz B, Kilicaslan I, Bildik F, Keles A, Demircan A, Hakoglu O, et al. BLUE protocol ultrasonography in Emergency Department patients presenting with acute dyspnea. Am J Emerg Med. (2019) 2019:28. doi: 10.1016/j.ajem.2019.02.028
43. Bourcier J-E, Paquet J, Seinger M, Gallard E, Redonnet J-P, Cheddadi F, et al. Performance comparison of lung ultrasound and chest x-ray for the diagnosis of pneumonia in the ED. Am J Emerg Med. (2014) 32:115–8. doi: 10.1016/j.ajem.2013.10.003
44. Amatya Y, Rupp J, Russell FM, Saunders J, Bales B, House DR. Diagnostic use of lung ultrasound compared to chest radiograph for suspected pneumonia in a resource-limited setting. Int J Emerg Med. (2018) 11:8. doi: 10.1186/s12245-018-0170-2
45. Levine AR, McCurdy MT, Zubrow MT, Papali A, Mallemat HA, Verceles AC. Tele-intensivists can instruct non-physicians to acquire high-quality ultrasound images. J Crit Care. (2015) 30:871–5. doi: 10.1016/j.jcrc.2015.05.030
46. Douglas TM, Levine AR, Olivieri PP, McCurdy MT, Papali A, Zubrow MT, et al. Brief training increases nurses' comfort using tele-ultrasound: A feasibility study. Intens Crit Care Nurs. (2019) 51:45–9. doi: 10.1016/j.iccn.2018.11.004
47. Nascimento BR, Nunes MCP, Lopes ELV, Rezende VMLR, Landay T, Ribeiro ALP, et al. Rheumatic heart disease echocardiographic screening: approaching practical and affordable solutions. Heart. (2016) 102:658–64. doi: 10.1136/heartjnl-2015-308635
48. Nascimento BR, Beaton AZ, Nunes MCP, Diamantino AC, Carmo GAL, Oliveira KKB, et al. Echocardiographic prevalence of rheumatic heart disease in Brazilian schoolchildren: Data from the PROVAR study. Int J Cardiol. (2016) 219:439–45. doi: 10.1016/j.ijcard.2016.06.088
49. Zühlke LJ, Steer AC. Estimates of the global burden of rheumatic heart disease. Glob Heart. (2013) 8:189–95. doi: 10.1016/j.gheart.2013.08.008
50. WHO. Trends in Maternal Mortality: 1990 to 2015. (2015). Available online at: https://apps.who.int/iris/bitstream/handle/10665/193994/WHO_RHR_15.23_eng.pdf?sequence=1
51. Ali FS, Harrington SG. Diagnostic Radiology in Liberia: a country report. J Global Radiol. (2015) 1:1020. doi: 10.7191/jgr.2015.1020
52. Swanson JO, Kawooya MG, Swanson DL, Hippe DS, Dungu-Matovu P, Nathan R. The diagnostic impact of limited, screening obstetric ultrasound when performed by midwives in rural Uganda. J Perinatol. (2014) 34:508–12. doi: 10.1038/jp.2014.54
53. Sanchez O, Baker J, Vaughan J, Steller JG, Toohey JS. The rural obstetrical ultrasound triage exam (ROUTE): teaching health care workers in international settings [392]. Obstetrics Gynecol. (2015) 125:122S. doi: 10.1097/01.AOG.0000463214.16868.eb
54. Swanson JO, Plotner D, Franklin HL, Swanson DL, Lokomba Bolamba V, Lokangaka A, et al. Web-based quality assurance process drives improvements in obstetric ultrasound in 5 low- and middle-income countries. Glob Health Sci Pract. (2016) 4:675–83. doi: 10.9745/GHSP-D-16-00156
55. Martinez B, Hall-Clifford R, Coyote E, Stroux L, Valderrama CE, Aaron C, et al. Agile development of a smartphone app for perinatal monitoring in a resource-constrained setting. J Health Inform Dev Ctries. (2017) 11:212.
56. Yoo SK, Kim DK, Jung SM, Kim E-K, Lim JS, Kim JH. Performance of a web-based, realtime, tele-ultrasound consultation system over high-speed commercial telecommunication lines. J Telemed Telecare. (2004) 10:175–9. doi: 10.1258/135763304323070841
57. Cone SW, Hummel R, León J, Merrell RC. Implementation and evaluation of a low-cost telemedicine station in the remote Ecuadorian rainforest. J Telemed Telecare. (2007) 13:31–4. doi: 10.1258/135763307779701220
58. DeStigter KK, Morey GE, Garra BS, Rielly MR, Anderson ME, Kawooya MG, et al. Low-cost teleradiology for rural ultrasound. In: 2011 IEEE Global Humanitarian Technology Conference (Seattle, WA) (2011). p. 290–5. Available online at: ieeexplore.ieee.org
59. Ferrer J, Chaumont T, Trujillo L, Fernandez I, Guerrero J, Stewart P, et al. New tele-diagnostic model using volume sweep imaging for rural areas. Conf Proc IEEE Eng Med Biol Soc. (2017) 2017:2622–5. doi: 10.1109/EMBC.2017.8037395
Keywords: telemedicine, eHealth, ultrasound, resource-limited, tele-ultrasound, LMIC, tele-radiology, global health
Citation: Britton N, Miller MA, Safadi S, Siegel A, Levine AR and McCurdy MT (2019) Tele-Ultrasound in Resource-Limited Settings: A Systematic Review. Front. Public Health 7:244. doi: 10.3389/fpubh.2019.00244
Received: 01 April 2019; Accepted: 13 August 2019;
Published: 04 September 2019.
Edited by:
Laurent Bonnardot, Université Paris Descartes, FranceReviewed by:
Margo Bergman, University of Washington Tacoma, United StatesMario Ettore Giardini, University of Strathclyde, United Kingdom
Copyright © 2019 Britton, Miller, Safadi, Siegel, Levine and McCurdy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael T. McCurdy, ZHJtY2N1cmR5JiN4MDAwNDA7Z21haWwuY29t
†Co-first authorship
 Noel Britton1
Noel Britton1 Michael A. Miller
Michael A. Miller Sami Safadi
Sami Safadi Ariel Siegel
Ariel Siegel Michael T. McCurdy
Michael T. McCurdy