Commentary: The Role of Dentists and Primary Care Physicians in the Care of Patients With Sleep-Related Breathing Disorders
- 1Dental Sleep Medicine of Indiana, Indianapolis, IN, United States
- 2Department of Health Promotion and Behavior, College of Public Health, The University of Georgia, Athens, GA, United States
- 3Department of Health Promotion and Community Health Sciences, School of Public Health, Texas A&M University, College Station, TX, United States
Obesity is a global epidemic that is well rooted in the United States and Western cultures (1–4). Recent attention of the magnitude of the epidemic warrants new approaches to health promotion, including expanded attention to obesity prevention by all health professions and disciplines. Driven by a combination of behavioral (e.g., unhealthy diets, physical inactivity) and environmental factors (e.g., food costs, community walkability, fast food establishment prevalence), obesity impacts individuals across the life-course and is responsible for morbidity, premature mortality, and escalating healthcare costs (5–8). The ramifications of obesity are pronounced among certain subpopulations, with disproportionate disparity and burden observed among racial/ethnic minorities, those of lower socioeconomic status, and those living in rural areas (9–13).
While the direct linkage of obesity to conditions such as diabetes, metabolic syndrome, and cardiovascular disease is well known (14, 15), these diseases may take years to manifest and be diagnosed. As such, there is growing recognition about more proximal risks associated with obesity, such as sleep-related breathing disorders (SRBD), including obstructive sleep apnea (16–19). When an individual struggles to breathe while sleeping, or actually stops breathing during sleep, additional stress is being placed on their heart, which can lead to health risks, including cardiovascular disease, pulmonary hypertension, enlarged heart, and stroke (20, 21).
Focusing on the signs and symptoms of obesity beyond body mass index (BMI) represents a health promotion approach with potential to prevent disease-related consequences by facilitating early screening and diagnosis. Such an approach may require new or slightly modified roles for existing healthcare professionals who are in regular contact with patients. While disease diagnoses are traditionally driven by physicians and nurse practitioners, opportunity exists for addressing the continuum of SRBD care within other disciplines during ongoing provider–patient interactions. Complementing specialized medicine efforts with additional professional expertise in SRBD can attenuate situations where patients go undiagnosed for long durations and experience exacerbated consequences once diagnosed because of advanced disease progression. Within this context, this article proposes a model that integrates dentists into multidisciplinary medical teams to collaboratively screen, refer, diagnose, and treat SRBD (see Figure 1).
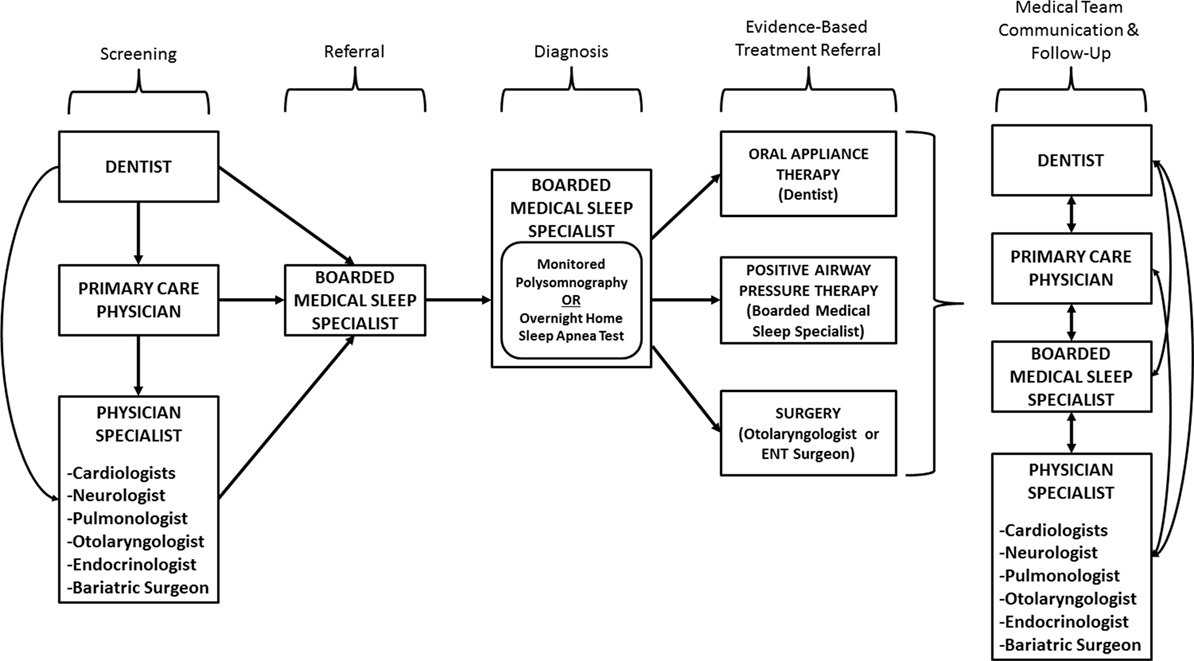
Figure 1. Involvement of a multidisciplinary medical team in the screening, referral, diagnosis, and treatment processes.
Screening
Dentists and primary care physicians (PCP) are often the first line of detection and treatment for the public. Dentists potentially see their patients much more frequently than physicians, especially those who adhere to the recommended cleaning every 6 months. In addition, PCP potentially see their patients more frequently than do physician specialists (e.g., cardiologist, neurologist, pulmonologist, otolaryngologist), especially those who adhere to recommended annual checkups. Both dentists and PCP have the opportunity to discuss a variety of concerns that affect their patient’s quality of life, general well-being, and potential health risks. Since a great number of patients with undetected and untreated sleep disorders (such as obstructive sleep apnea) pass through the dental and PCP offices each day, it is necessary that these practitioners are educated about these conditions through trainings and continuing education courses so that they understand how best to embed practical assessments and referrals into routine care. Furthermore, their efforts can be twofold. The first is working with a referral system to link the patient to the proper specialist for diagnosis and to the proper professional for treatment. The second is to educate and consult the patient about healthy lifestyle choices that reduce risk factors for obesity and SRBD.
During a routine examination, the dentist can physically examine the patient’s teeth and perform an oral cancer screening that involves the tongue and the tissue in the back of the oral cavity. With minimum addition of time, these routine examinations can identify potential risk factors for SRBD such as sleep apnea. A dentist who has been educated about sleep apnea can also evaluate the patency of the airway, the size and position of the tongue, the size of the uvula, and the length of the soft palate tissue and tonsillar tissue. Following an examination of the oral tissues and noting the crowding of the oropharynx, dentists can weigh their patients and measure their height to determine their BMI, which can be used to facilitate discussions about obesity, its causes, and options for healthy eating and physical activity. Additionally, dentists could measure the neck circumference of their patients to assess SRBD risk (i.e., women with a 15-inch neck or greater and men with a 17-inch neck or greater are more likely to have sleep apnea) (22, 23). Further, dentists could take the patient’s blood pressure.
During routine office encounters, dentists and PCP can also collect subjective information from patients to assess their risk for sleep apnea. The most telling surrounds snoring. Loud snoring is caused by the tongue falling back into the airway and crowding with the uvula and soft palate and tonsils, if present. This crowding condition causes vibration of the tissue as patients breathe, and this vibration is heard as snoring. The crowding of the airway causing snoring can lead to a condition called upper airway resistance syndrome in which the struggling to breathe is more severe than snoring alone. Next on the continuum is mild sleep apnea, followed by moderate sleep apnea and then severe sleep apnea, which are all determined by the number of times per hour a patient completely or partially stops breathing. While everyone who snores does not necessarily have apnea, everyone with apnea snores. For this reason, snoring and apnea cannot be separated and both must be assessed/diagnosed. To assess snoring, patients should be asked: Do you snore? If yes, how would your ‘bed partner’ describe your snoring? Because apnea indicates that patients are not getting quality, restorative sleep during the night, follow-up questions include: When you wake up in the morning, do you feel refreshed? Are you tired or sleepy through the day? Do you have low energy throughout the day? Is it difficult to pay attention or remember things? Additional questions can be asked about the patient waking up through the night, going to the bathroom, having low libido, and experiencing diminished cognitive skills such as memory and concentration.
Referral and Diagnosis
Routinely gathering physical and subjective screening information during office visits can arm dentists and PCP with information necessary to identify patients with increased SRBD risk and make referrals to other medical team members. Screening and referrals are among the most important roles dentists and PCP have because they routinely see a large number of patients (of all demographics) each year and can identify probable sleep apnea cases. Once identified, dentists and PCP can refer patients to boarded medical sleep specialists (i.e., board-certified by the American Academy of Sleep Medicine), who can then consult with the patient and order an overnight sleep test called a polysomnography (PSG) or an overnight home sleep apnea test (HSAT). The PSG is monitored by a sleep technologist at a sleep center, while the HSAT is self-conducted at the patient’s home and not directly monitored by a professional. Both methods are used by physicians to diagnose sleep apnea. These tests are used to objectively diagnose SRBD, including sleep apnea.
Evidence-Based Treatment Referral
After sleep apnea is diagnosed by PSG or HSAT, the boarded medical sleep specialist can recommend multiple treatments. Possible treatments include weight loss, positional therapy (the best positions in which to sleep), continuous positive airway pressure (CPAP), surgery, and oral appliance therapy (OAT). Combination therapy is also common (e.g., CPAP/OAT, surgery/OAT, surgery/CPAP/OAT). The clinician or health professional responsible for overseeing each evidence-based treatment is different. Pending proper training and credentialing, dentists can effectively treat patients with sleep apnea using OAT (24–27). Regardless of the treatment or health professional overseeing that treatment option, patients should receive ongoing reinforcement about healthy behaviors during routine office visits.
Communication and Follow-Up
Despite the treatment prescribed, ongoing communication among members of the multidisciplinary medical team is essential for success. A patient does not encounter just one healthcare professional; rather, they encounter a variety of professionals for different purposes at different times. As such, to establish an effective medical home for the patient, all healthcare professionals caring for the patient should be aware of (and involved with to some degree) the treatment decisions and related outcomes for that patient. By communicating treatment results with all medical team members, common and unified recommendations can be offered to the patient in terms of lifestyle modification, screening practices, and treatment adherence. Having multiple healthcare professionals repeatedly reinforce recommendations to the patient is preferable to less-effective unilateral messaging, which can be conflicting and cause confusion/misinterpretation.
Given the prevalence of obesity and associated disparities among subpopulations, additional efforts are needed to prevent its occurrence, delay the onset of associated conditions, and treat existing diseases caused by its presence. To complement the abundance of community-driven interventions to address obesity by modifying diet and physical activity (28–30), additional initiatives are needed in the clinical setting. While the costs to the healthcare system and society place emphasis on diseases such as diabetes and cardiovascular disease (31, 32), efforts to identify more proximal signs and symptoms of obesity-related conditions should not be overlooked. As such, dentists and PCP are uniquely positioned to screen patients for SRBD and sleep apnea because they are among the most frequently seen clinicians by the American population. In a ‘no wrong door’ to healthcare scenario, they can be the first encounter in a subsequent chain of healthcare interactions to prevent disease and improve health status. Dentists and PCP can be trained to perform physical and subjective screenings to identify sleep apnea risk and make referrals to boarded medical sleep specialists. Dentists can also guide and be included in sleep apnea treatments involving OAT. Regardless of the treatment received, dentists and PCP are valuable members of the medical team when caring for SRBD patients.
Conclusion
The long-standing collaboration between dentists and physicians can help manage the obesity epidemic (and its related health conditions) by addressing SRBD through screening, diagnosis (by a physician), treatment, and referrals. Working together, dentists and physicians can fight the ramifications of sleep apnea and obesity to improve the health of individual patients and communities. This opinion indicates an ideal model of inter-professional care. However, challenges implementing such recommendations remain because of competing training demands, limited patient appointment times, and current reimbursement constraints. Thus, we call for additional efforts to increase awareness about this important public health and clinical issue. Studies are also warranted to examine the benefits and practicalities of implementing such a model in diverse settings. Ongoing efforts are needed to build upon the existing support given to the fields of medical and dental sleep medicine by organizations such as the American Medical Association, the American Dental Association, and insurance companies throughout the United States.
Author Contributions
HS and MS conceptualized, drafted, and reviewed the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to acknowledge the leadership and support of the American Academy of Dental Sleep Medicine (AADSM) and the American Academy of Sleep Medicine (AASM) to establish and promote polices and practice standards, which have defined the valuable role of dentists (and mandated the need for their inclusion) on medical teams in their communities. Together, dentists and physicians working within their respective scopes of practice will protect the public through a continuum of care to treat patients with sleep-related breathing disorders.
References
1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (2014) 384(9945):766–81. doi: 10.1016/S0140-6736(14)60460-8
2. Popkin BM, Doak CM. The obesity epidemic is a worldwide phenomenon. Nutr Rev (1998) 56(4):106–14. doi:10.1111/j.1753-4887.1998.tb01722.x
3. Goryakin Y, Lobstein T, James WP, Suhrcke M. The impact of economic, political and social globalization on overweight and obesity in the 56 low and middle income countries. Soc Sci Med (2015) 133:67–76. doi:10.1016/j.socscimed.2015.03.030
4. Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol (2013) 9(1):13–27. doi:10.1038/nrendo.2012.199
5. Dee A, Kearns K, O’Neill C, Sharp L, Staines A, O’Dwyer V, et al. The direct and indirect costs of both overweight and obesity: a systematic review. BMC Res Notes (2014) 7(1):1. doi:10.1186/1756-0500-7-242
6. Lehnert T, Sonntag D, Konnopka A, Riedel-Heller S, König HH. Economic costs of overweight and obesity. Best Pract Res Clin Endocrinol Metab (2013) 27(2):105–15. doi:10.1016/j.beem.2013.01.002
7. Masters RK, Reither EN, Powers DA, Yang YC, Burger AE, Link BG. The impact of obesity on US mortality levels: the importance of age and cohort factors in population estimates. Am J Public Health (2013) 103(10):1895–901. doi:10.2105/AJPH.2013.301379
8. Masters RK, Powers DA, Link BG. Obesity and US mortality risk over the adult life course. Am J Epidemiol (2013) 177(5):431–42. doi:10.1093/aje/kws325
9. Robinson WR, Gordon-Larsen P, Kaufman JS, Suchindran CM, Stevens J. The female-male disparity in obesity prevalence among black American young adults: contributions of sociodemographic characteristics of the childhood family. Am J Clin Nutr (2009) 89(4):1204–12. doi:10.3945/ajcn.2007.25751
10. Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008). J Rural Health (2012) 28(4):392–7. doi:10.1111/j.1748-0361.2012.00411.x
11. Ogden CL. Disparities in obesity prevalence in the United States: black women at risk. Am J Clin Nutr (2009) 89(4):1001–2. doi:10.3945/ajcn.2009.27592
12. Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev (2007) 29(1):6–28. doi:10.1093/epirev/mxm007
13. Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab (2004) 89(6):2590–4. doi:10.1210/jc.2004-0339
14. Ritchie S, Connell JM. The link between abdominal obesity, metabolic syndrome and cardiovascular disease. Nutr Metab Cardiovasc Dis (2007) 17(4):319–26. doi:10.1016/j.numecd.2006.07.005
15. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health (2009) 9(1):1. doi:10.1186/1471-2458-9-88
16. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol (2013) 177(9):1006–14. doi:10.1093/aje/kws342
17. Chen X, Wang R, Lutsey PL, Zee PC, Javaheri S, Alcántara C, et al. Racial/ethnic differences in the associations between obesity measures and severity of sleep-disordered breathing: the Multi-Ethnic Study of Atherosclerosis. Sleep Med (2016) 26:46–53. doi:10.1016/j.sleep.2015.06.003
18. Horvath C, Jossen J, Brill AK, Nett P, Baty F, Ott S. Sleep disordered breathing in morbidly obese patients prior to bariatric surgery – a retrospective analysis. Eur Respir J (2016) 48(Suppl 60):PA347. doi:10.1183/13993003.congress-2016.PA347
19. Smith ML, Smith HA, Wilson KL, Ahn S, Pulczinski JC, Ory MG. Obesity and perceived severity of obstructive sleep apnea-related conditions. Fam Community Health (2014) 37(4):258–70. doi:10.1097/FCH.0000000000000042
20. Marshall NS, Wong KK, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study cohort. J Clin Sleep Med (2014) 10(4):355–62. doi:10.5664/jcsm.3600
21. Kendzerska T, Leung R, Gershon A, Hawker G, Tomlinson G. Obstructive sleep apnea in risk for first cardiovascular event and all-cause mortality: a competing risks approach. Sleep Med (2013) 14:e27–8. doi:10.1016/j.sleep.2013.11.028
22. Onat A, Hergenç G, Yüksel H, Can G, Ayhan E, Kaya Z, et al. Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin Nutr (2009) 28(1):46–51. doi:10.1016/j.clnu.2008.10.006
23. Cowan DC, Allardice G, MacFarlane D, Ramsay D, Ambler H, Banham S, et al. Predicting sleep disordered breathing in outpatients with suspected OSA. BMJ Open (2014) 4(4):e004519. doi:10.1136/bmjopen-2013-004519
24. Phillips CL, Grunstein RR, Darendeliler MA, Mihailidou AS, Srinivasan VK, Yee BJ, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med (2013) 187(8):879–87. doi:10.1164/rccm.201212-2223OC
25. Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F, Kushida CA, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med (2014) 10(2):215–27. doi:10.5664/jcsm.3460
26. Andrén A, Hedberg P, Walker-Engström ML, Wahlén P, Tegelberg Å. Effects of treatment with oral appliance on 24-h blood pressure in patients with obstructive sleep apnea and hypertension: a randomized clinical trial. Sleep Breath (2013) 17(2):705–12. doi:10.1007/s11325-012-0746-7
27. Doff MH, Hoekema A, Wijkstra PJ, van der Hoeven JH, Huddleston Slater JJ, de Bont LG, et al. Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: a 2-year follow-up. Sleep (2013) 36(9):1289–96. doi:10.5665/sleep.2948
28. Dietz WH. The response of the US Centers for Disease Control and Prevention to the obesity epidemic. Annu Rev Public Health (2015) 36:575–96. doi:10.1146/annurev-publhealth-031914-122415
29. Miller WC, Koceja DM, Hamilton EJ. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Int J Obes (1997) 21(10):941–7. doi:10.1038/sj.ijo.0800499
30. Nestle M, Jacobson MF. Halting the obesity epidemic: a public health policy approach. Public Health Rep (2000) 115(1):12. doi:10.1093/phr/115.1.12
31. Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States a policy statement from the American Heart Association. Circulation (2011) 123(8):933–44. doi:10.1161/CIR.0b013e31820a55f5
Keywords: sleep apnea, disordered breathing, dental, primary care, medical team, disparities
Citation: Smith HA and Smith ML (2017) The Role of Dentists and Primary Care Physicians in the Care of Patients with Sleep-Related Breathing Disorders. Front. Public Health 5:137. doi: 10.3389/fpubh.2017.00137
Received: 26 December 2016; Accepted: 30 May 2017;
Published: 15 June 2017
Edited by:
Allen C. Meadors, The Global Leadership Group, United StatesReviewed by:
Warren G. McDonald, Methodist University, United StatesCopyright: © 2017 Smith and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthew Lee Smith, health@uga.edu
 Harold A. Smith1
Harold A. Smith1 Matthew Lee Smith
Matthew Lee Smith