
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health , 02 July 2015
Sec. Epidemiology
Volume 3 - 2015 | https://doi.org/10.3389/fpubh.2015.00169
This article is part of the Research Topic Health disparities: An important public health policy concern View all 8 articles
The relationship between residential segregation and overweight/obesity among African-American adults remains unclear. Elucidating that relationship is relevant to efforts to prevent and to reduce racial disparities in obesity. This article provides a critical review of the 11 empirical studies of segregation and overweight/obesity among African-American adults. Results revealed that most studies did not use a valid measure of segregation, many did not use a valid measure of overweight/obesity, and many did not control for neighborhood poverty. Only four (36% of the) studies used valid measures of both segregation and overweight/obesity and also controlled for area-poverty. Those four studies suggest that segregation contributes to overweight and obesity among African-American adults, but that conclusion cannot be drawn with certainty in light of the considerable methodologic problems in this area of research. Suggestions for improving research on this topic are provided.
The prevalence of overweight and obesity is high among all Americans, and among African-Americans in particular (1–3). For example, rates of overweight/obesity among African-American women are 44% higher than among White women (1–5). Racial disparities in socioeconomic status (SES) (3, 5) and in health behaviors (e.g., diet, physical activity) contribute to racial disparities in body weight (5, 6), and African-American cultural variables such as religiosity (7, 8) and acculturation level (9) contribute as well, but these individual-level factors do not fully explain the disparities (5).
Recent research has highlighted the neighborhood context as an additional determinant of obesity and obesity disparities (5, 10–15). Such studies have identified obesogenic environments as contributors, i.e., neighborhoods that facilitate overweight/obesity via their paucity of parks and recreational facilities, prevalence of fast food outlets, dearth of healthy food options, and dangerousness that discourages outdoor activities (10–15). Low-SES neighborhoods have been demonstrated to be obesogenic environments that contribute to overweight and to obesity among their residents irrespective of resident race-ethnicity (11–15). Racially segregated African-American neighborhoods also meet the criteria for obesogenic environments (16) in terms of their food choices (17–20) and recreational resources (21–23). Thus, residing in a segregated, African-American neighborhood might contribute to overweight and obesity among African-Americans, and might in part explain the racial disparities in body weight that transcend low-SES (10, 16). The relationship between residential segregation and overweight/obesity, however, remains unclear (10, 16). This paper reviews the empirical studies on residential racial segregation and body weight among African-American adults in an effort to elucidate the segregation–obesity relationship.
First, we define racial residential segregation in the U.S. and highlight the various ways in which it is measured. Then, we review and compare studies of segregation and weight among African-American adults to ascertain the nature and strength of that relationship, and highlight its implications for preventing and reducing racial disparities in obesity.
Residential segregation refers to the geographic separation of Whites from minorities (African-Americans in this case) in residential areas (24, 25). It can be measured at any geographic-level (e.g., census tracts, zip codes, counties, Metropolitan Statistical Areas/MSAs) and usually is measured at the level of census tracts or MSAs in health research (25–29). Irrespective of area-level used, segregation can be measured in several ways, including Isolation, Dissimilarity, Concentration, Clustering, Centralization, and Hypersegregation (26, 28, 29). These terms are defined in Table 1. Each of these standard, valid measures of segregation is computed by the U.S. Census Bureau, and ranges from 0 to 1, with ≥0.60 regarded as high segregation (25–29).
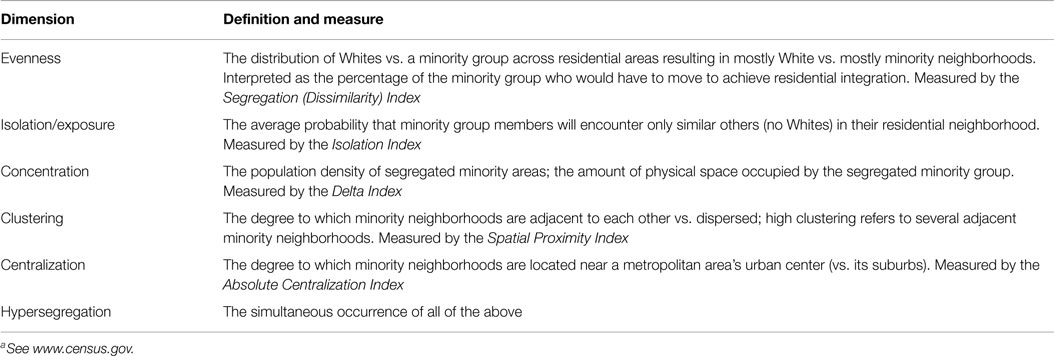
TABLE 1. Dimensions and measures of residential segregationa (29).
The percentage of African-Americans in an area often is used as a measure of segregation as well (25–29). This crude measure lacks validity and is unrelated to the valid measures of segregation (26, 28, 29). As shown by the 10 census tracts in Table 2 for example, the percentage of African-Americans in an area can range from 32 to 55% yet the census tract might not be highly segregated, i.e., the Isolation Index can be lower than 0.60. This is because, unlike the percentage of African-Americans, valid measures of segregation take into account relative population sizes and their distribution across an area. We highlight this because (as will be shown) many studies used percent African-Americans as their measure of segregation.
PubMed and PsychINFO were searched using these search terms: African-Americans, Blacks, residential segregation, racial segregation, racial composition (first set of terms), and adult obesity, adult body mass index (BMI), and adult body weight (second terms). This initial search returned 58 publications. Their abstracts then were examined by all authors; publications that were theoretical, dissertations, commentaries, did not measure segregation, focused on other racial-ethnic groups and did not contain African-Americans, or focused on children and did not include adults were excluded. Only articles that were empirical studies of adult body weight, measured segregation, and included U.S. African-American adults were retained. The final set of articles consisted of 11 publications that met all inclusion criteria.
The 11 full-length articles (10, 16, 30–38) were examined independently by the authors, each of whom completed a table detailing these article-variables: author and publication year; database (national vs. local); in-person vs. telephone interview methodology; sample size, gender, and age; definition and measurement of overweight and obesity; measure of segregation and definition of high segregation; control for neighborhood low-SES, and whether the best measure of that (i.e., percent below the federal poverty line [see Ref. (29)]) was used; and their results. Inconsistencies among the tables were discussed and articles re-analyzed until 100% agreement among the authors was reached. The 11 articles are shown in Table 3 with details on the above article-variables.
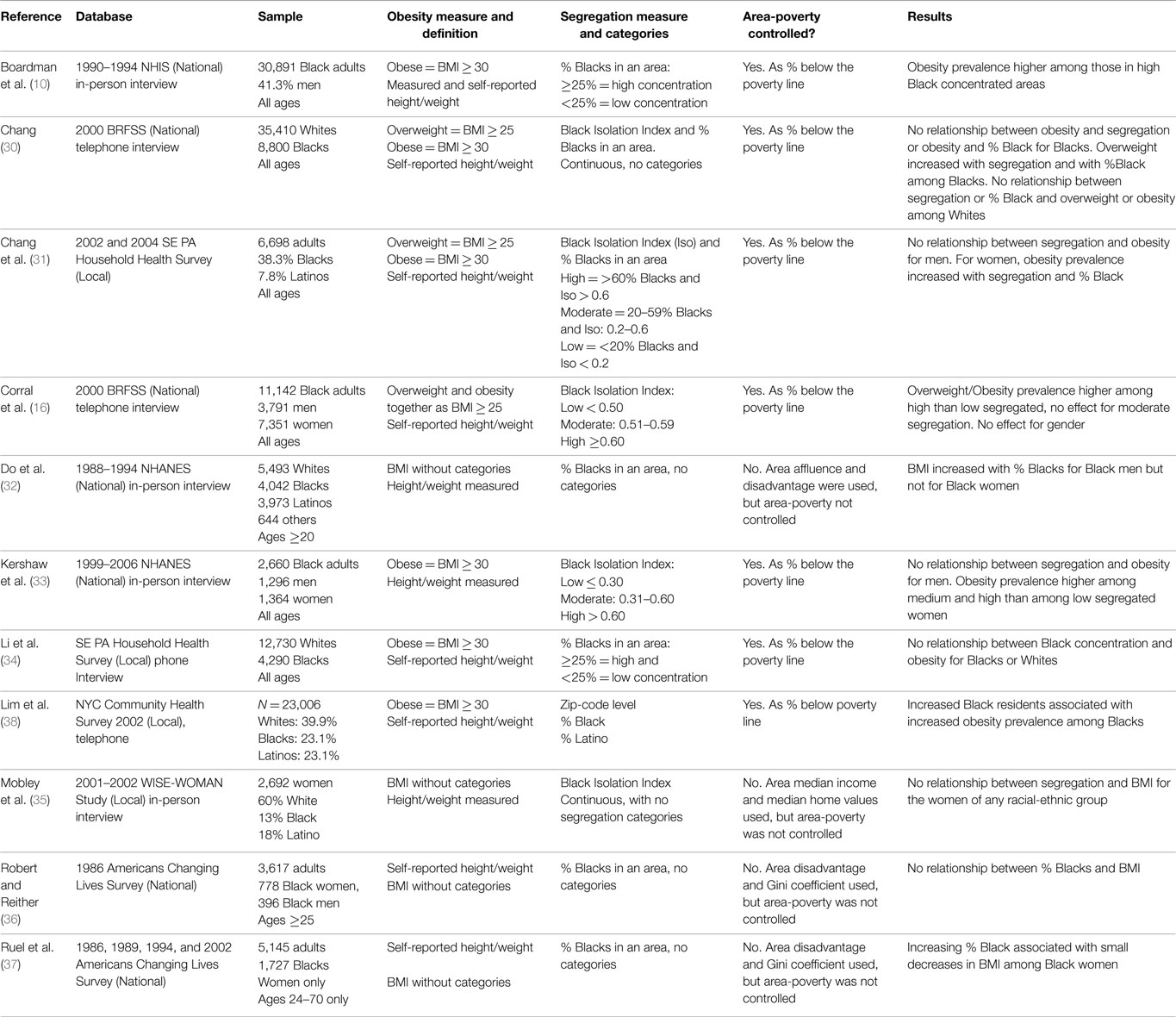
Table 3. Eleven empirical studies of segregation and overweight/obesity among African-American adults.
Articles were compared on their (1) definition and measurement of overweight and obesity; (2) measure of segregation and definition of high segregation; (3) measurement and control for neighborhood low-SES; (4) report of gender-specific analyses; (5) use of a local vs. national database and sample; and (6) their findings.
Eight of the 11 studies (73%) reported a positive relationship between segregation and BMI/obesity/overweight; increases in segregation were associated with increases in BMI or in overweight or obesity prevalence in those studies.
Although the valid, biomedical definitions are overweight = BMI ≥ 25 and obesity = BMI ≥ 30, four studies (36%) did not use these BMI categories in data analyses. Instead, they used continuous BMI scores. Of these four, two (50%) found no relationship between continuous BMI and segregation, and two found a positive relationship for men or for women only. In the remaining seven studies, six defined obesity as a BMI ≥ 30 and one used BMI ≥ 25 to define the combined variable overweight/obesity. Six of these seven studies (86%) found a positive relationship between segregation and BMI-categorical overweight and/or obesity. Eight of the 11 studies used self-reported height and weight, and six of those eight (75%) found a positive relationship between segregation and overweight or obesity. Three studies measured height and weight, and two of those (67%) found a similar positive relationship.
Only five of the 11 studies (45%) used a valid measure of residential segregation (e.g., the Isolation Index, see Table 1); a positive relationship was found in four (80%) of those studies. Six (55%) of 11 studies used the percentage of African-Americans in an area as their measure of segregation, with a positive relationship found in four of those studies (67%). Most studies (8 of 11 or 73%) did not define high segregation using standard, valid categories shown in Table 1. Two of the five that used Isolation Index scores used continuous scores. Only three studies that used the Isolation Index defined high segregation as scores ≥0.60; two of these found a positive relationship between segregation and overweight/obesity for women only. The six studies that used percent African-Americans as their measure of segregation either did not define the percentage that constitutes high segregation (four of the six studies), or defined high segregation as ≥25% African-Americans in a census tract or zip code.
Seven of the 11 studies (64%) used percent of area residents below the federal poverty line as their measure of low-SES neighborhoods, and then controlled for area-poverty in their analyses. Six of those studies (86%) found a positive relationship between segregation and overweight/obesity. Of the four studies that used measures of neighborhood SES (e.g., income inequality, median home values) that are less sensitive to area-SES health disparities, two found a positive relationship and two found no effect.
Two studies had women-only samples. Both used invalid measures of segregation and used continuous BMI. Only one found increases in BMI with increases in segregation. Four studies reported gender-specific analyses; all four used valid measures, and all found a positive relationship between segregation and overweight/obesity. Two found this for women only, one found this for men only, and one found no effect for gender.
Seven studies (64%) used national databases, such as the National Health Interview Survey (NHIS), National Health and Nutrition Examination Survey (NHANES), or Behavioral Risk Factor Surveillance System (BRFSS), and used large, random, national samples; six of these (86%) found a positive relationship. Of the four studies that used local (smaller) databases, half found a positive relationship and half found no effect.
Of 11 studies of segregation and overweight/obesity, 73% reported that increased segregation or high segregation was associated with increased obesity/overweight prevalence or increased BMI among African-Americans adults. The conclusion that segregation is associated with overweight/obesity cannot be drawn from that finding, however, because of the considerable problems in the measures and data-analytic strategies of the studies. Most (55% of) studies did not use a valid measure of segregation. Instead, they defined segregation as the percentage of African-Americans in an area (e.g., ≥25% of area residents), a measure known to lack validity. Others used the Isolation Index (a valid measure) but treated it as a continuous variable, without defining Isolation ≥ 0.6 as high segregation. Overall, 73% of the studies did not define high segregation using valid research categories. Moreover, only 64% used BMI categories to define obesity and overweight, only 64% included adequate controls for neighborhood-poverty in their analyses, and only 36% reported gender-specific analyses despite well-known gender differences in obesity (1–3).
Nonetheless, the 11 studies provide insights into the relationship between segregation and overweight/obesity, and highlight ways to improve this area of research. Specifically, 86% of the studies that used BMI categories to define overweight/obesity (i.e., valid measures) found a positive relationship to segregation, compared to only 50% of those that did not use BMI categories. Likewise, 80% of the studies that used valid measures of segregation found a positive relationship compared to 66% of those that used invalid measures. Similarly, 86% of the studies that used adequate controls for neighborhood poverty found a positive segregation–body weight relationship vs. 50% of those without such controls. Moreover, 86% of studies that used national databases found a positive segregation–body weight relationship compared to only 50% of those using local datasets.
Such findings suggest that inconsistencies in study results by and large reflect inconsistencies in their measures and their control of neighborhood-SES; studies tended to find a positive relationship if they used valid measures of segregation and of overweight/obesity, and also controlled for area poverty. Indeed, 100% of the studies that used valid measures of overweight/obesity and of segregation and also controlled for area-poverty found a positive segregation–obesity/overweight relationship [i.e., Ref. (16, 30, 31, 33)], but there were only four such studies. Those four lead to the tentative conclusion that residential segregation indeed may be associated with overweight/obesity among African-American adults (women in particular), but more studies with similar robust measures and controls are needed to draw that conclusion. A more firm conclusion about the segregation–overweight/obesity relationship cannot be drawn because only 45% of studies used a valid measure of segregation. However, if segregation is associated with overweight/obesity among African-American adults, then efforts to prevent and to reduce racial disparities in overweight/obesity can be improved by targeting (not African-American people but) African-American places – i.e., segregated African-American neighborhoods and their obesogenic features. These tentative conclusions must be considered in the context of the limitations of this study.
One important limitation is that we included only studies in which residential segregation was measured, irrespective of the validity of that measure. Hence, relevant studies that did not measure segregation were excluded. Two such studies (39, 40) examined racial disparities in obesity (defined as BMI ≥ 30) in racially integrated census tracts and found no African-American–White differences in obesity prevalence in integrated neighborhoods among women (39) or men (40). These two studies indirectly support the tentative conclusion that segregated African-American neighborhoods contribute to racial disparities in obesity. A second limitation is the methods sections of the 11 studies reviewed here. Details of the methods and measures (and even the sample sizes) were not provided in some articles, and hence our summary (Table 3) of their methods and measures (of neighborhood-SES in particular) might be somewhat less than accurate. In addition, we excluded studies of children from this review because the definition of overweight/obesity in children (percentile rank relative to age- and sex-matched peers) differs from the definition for adults, and a single definition was preferred. Studies of segregation and overweight/obesity among children may or may not be similar to those of adults in methodological shortcomings and findings. Despite these limitations, this review is the first of its kind, and highlights serious flaws in this area of research – use of invalid measures of segregation and of obesity foremost among those. Hence, we encourage future studies to use valid measures of segregation and of overweight/obesity to clarify the relationship between them and potentially enhance prevention efforts.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA (2012) 307(5):491–7. doi: 10.1001/jama.2012.39
2. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA (2010) 303:235–41. doi:10.1001/jama.2009.2014
3. Wang Y, Beydoun MA. The obesity epidemic in the United States – gender, age, socioeconomic, racial/ethnic, and geographic characteristics. Epidemiol Rev (2007) 29:6–28. doi:10.1093/epirev/mxm007
4. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Taback CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA (2006) 295(13):1549–55. doi:10.1001/jama.295.13.1549
5. Kumanyika SK, Whitt-Glover MC, Gary TL, Prewitt TE, Odoms-Young AM, Banks-Wallace J, et al. Expanding the obesity research paradigm to reach African-American communities. Prev Chronic Dis (2007) 4(4):A112–33.
6. Wang Y, Chen X. How much of racial/ethnic disparities in dietary intakes, exercise, and weight status can be explained by nutrition- and health-related psychosocial factors and socioeconomic status among U.S. adults? J Am Diet Assoc (2011) 111(12):1904–11. doi:10.1016/j.jada.2011.09.036
7. Holt CL, Haire-Joshu DL, Lukwago SN, Lewellyn LA, Kreuter MW. The role of religiosity in dietary beliefs and behaviors among urban, African-American women. Cancer Control (2005) 12(S2):84–90.
8. Kennedy BM, Ard JD, Harrison L, Conish BK, Kennedy E, Levy EJ, et al. Cultural characteristics of African Americans: implications for the design of trials that target behavior and health promotion programs. Ethn Dis (2007) 17(3):548–54.
9. Ard JD, Skinner CS, Chen C, Aickin M, Svetkey LP. Informing cancer prevention strategies for African-Americans. J Behav Med (2005) 28(3):239–47. doi:10.1007/s10865-005-4660-3
10. Boardman JD, Saint Onge JM, Rogers RG, Denney JT. Race differentials in obesity: the impact of place. J Health Soc Behav (2005) 46:229–43. doi:10.1177/002214650504600302
11. Glass TA, Rasmussen MD, Schwartz BA. Neighborhoods and obesity in older adults. Am J Prev Med (2006) 31:455–63. doi:10.1016/j.amepre.2006.07.028
12. Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics (2006) 117:417–24.
13. Wang MC, Soowan K, Gonzalez AA, MacLeod KE, Winkleby MA. Socioeconomic and food-related physical characteristics of the neighborhood environment are associated with body mass index. J Epidemiol Community Health (2006) 61:491–8. doi:10.1136/jech.2006.051680
14. Nelson NM, Woods CB. Obesogenic environments: are neighborhood environments that limit physical activity obesogenic? Health Place (2009) 15(4):917–24. doi:10.1016/j.healthplace.2009.02.001
15. Reidpath DD, Burns C, Gerrard J, Mahoney M, Townsend M. An ecological study of the relationship between social and environmental determinants of obesity. Health Place (2002) 8:141–5.
16. Corral I, Landrine H, Zhao L, Hao Y, Mellerson J, Cooper D. Residential segregation, health behavior, and overweight/obesity among a national sample of black adults. J Health Psychol (2012) 17:371–8. doi:10.1177/1359105311417191
17. Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med (2007) 44:189–95. doi:10.1016/j.ypmed.2006.08.008
18. Powell LM, Chaloupka FJ, Bao Y. The availability of fast food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med (2007) 33(4 Suppl):S240–5. doi:10.1016/j.amepre.2007.07.005
19. Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy goods and their effects on environmental justice. Am J Public Health (2012) 102(9):1644–54. doi:10.2105/AJPH.2012.300865
20. Bower KM, Thorpe RJ, Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the US. Prev Med (2014) 58:33–9. doi:10.1016/j.ypmed.2013.10.010
21. Powell LM, Slater S, Chaloupka FJ, Harper BA. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics. Am J Public Health (2006) 96(9):1676–80. doi:10.2105/AJPH.2005.065573
22. Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med (2008) 34(1):16–22. doi:10.1016/j.amepre.2007.09.021
23. Duncan DT, Kawachi I, White K, Williams DR. The geography of recreational open space: influence of neighborhood racial composition and neighborhood poverty. J Urban Health (2013) 90(4):618–31. doi:10.1007/s11524-012-9770-y
24. Iceland J, Weinberg DH, Steinmetz E. Racial and Ethnic Segregation in the United States, 1980-2000. Washington, DC: U.S. Government Printing Office, U.S. Census Bureau (2002).
25. Johnston R, Poulsen M, Forrest J. Ethnic and racial segregation in U.S. metropolitan areas, 1980-2000. Urban Aff Rev Thousand Oaks Calif (2007) 42(4):479–504. doi:10.1177/1078087406292701
26. Brown LA, Chung SY. Spatial segregation, segregation indices and the geographical perspective. Popul Space Place (2006) 12(2):125–43. doi:10.1002/psp.403
27. Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and black-white disparities in hypertension. Am J Epidemiol (2011) 174(5):537–45. doi:10.1093/aje/kwr116
28. Kramer MR, Cooper HL, Drews-Botsch CD, Waller LA, Hogue CR. Do measures matter? Comparing surface-density-derived and census-tract-derived measures of racial residential segregation. Int J Health Geogr (2010) 3:3–21. doi:10.1186/1476-072X-9-29
29. Landrine H, Corral I. Advancing research on racial-ethnic health disparities: improving measurement equivalence in studies with diverse samples. Front Public Health (2014) 2:282. doi:10.3389/fpub.2014.00215
30. Chang VW. Racial residential segregation and weight status among U.S. adults. Soc Sci Med (2006) 63:1289–303. doi:10.1016/j.socscimed.2006.03.049
31. Chang VW, Hillier AE, Mehta NK. Neighborhood racial isolation, disorder and obesity. Soc Forces (2009) 87:2063–92. doi:10.1353/sof.0.0188
32. Do DP, Dubowitz T, Bird CE, Lurie N, Escarce JJ, Finch BK. Neighborhood context and ethnicity differences in body mass index: a multilevel analysis using NHANES III survey (1988-1994). Econ Hum Biol (2007) 5(2):179–203. doi:10.1016/j.ehb.2007.03.006
33. Kershaw KN, Albrecht SS, Carnethon MR. Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among Blacks and Mexican Americans. Am J Epidemiol (2013) 177(4):299–309. doi:10.1093/aje/kws372
34. Li K, Wen M, Henry KA. Residential racial composition and black-white obesity risks. Int J Environ Res Public Health (2014) 11:626–42. doi:10.3390/ijerph110100626
35. Mobley LR, Root ED, Finkelstein EA, Khavjou O, Farris RP, Will JC. Environment, obesity, and cardiovascular disease in low-income women. Am J Prev Med (2006) 30(4):327–32. doi:10.1016/j.amepre.2005.12.001
36. Robert SA, Reither EN. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Soc Sci Med (2004) 59:2421–34. doi:10.1016/j.socscimed.2004.03.034
37. Ruel E, Reither EN, Robert SA, Lantz PM. Neighborhood effects on BMI trends: examining BMI trajectories for black and white women. Health Place (2010) 16:191–8. doi:10.1016/j.healthplace.2009.09.009
38. Lim S, Harris TG. Neighborhood contributions to racial and ethnic disparities in obesity among New York city adults. Am J Public Health (2015) 105(1):159–65. doi:10.2105/AJPH.2013.301782
39. Bleich SN, Thorpe RJ, Sharif-Harris H, Fesahazion R, LaVeist TA. Social context explains race disparities in obesity among women. J Epidemiol Community Health (2010) 64(5):465–9. doi:10.1136/jech.2009.096297
Keywords: residential segregation, Blacks, African-Americans, obesity, overweight
Citation: Corral I, Landrine H, Hall MB, Bess JJ, Mills KR and Efird JT (2015) Residential segregation and overweight/obesity among African-American adults: a critical review. Front. Public Health 3:169. doi: 10.3389/fpubh.2015.00169
Received: 14 April 2015; Accepted: 17 June 2015;
Published: 02 July 2015
Edited by:
Haichang Xin, University of Alabama at Birmingham, USAReviewed by:
Mildred Audrey Pointer, North Carolina Central University, USACopyright: © 2015 Corral, Landrine, Hall, Bess, Mills and Efird. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hope Landrine, Center for Health Disparities, Brody School of Medicine, East Carolina University, 1800 W 5th Street, Medical Pavilion 6, Greenville, NC 27834, USA,bGFuZHJpbmVoQGVjdS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.