- 1Department of Health Promotion and Behavior, College of Public Health, The University of Georgia, Athens, GA, USA
- 2Department of Health Promotion and Community Health Sciences, Texas A&M Health Science Center, School of Public Health, College Station, TX, USA
- 3Division of Health Systems Management and Policy, School of Public Health, The University of Memphis, Memphis, TN, USA
- 4National Council on Aging, Washington, DC, USA
- 5Department of Epidemiology and Biostatistics, Texas A&M Health Science Center, School of Public Health, College Station, TX, USA
- 6Department of Medicine, Stanford Patient Education Research Center, Stanford School of Medicine, Palo Alto, CA, USA
With a near 20-year developmental history as an evidence-based program, the suite of Chronic Disease Self-Management Education (CDSME) programs were selected in 2010 for grand-scale dissemination in a federally supported initiative to improve the health of older Americans. The primary charge of this national effort was to establish a sustainable program delivery system for empowering American adults with one or more chronic conditions to better manage their health. The current study focused on a series of dissemination and implementation science research questions to: (1) examine the geographic distribution of participation in this initiative across the Unites States; (2) describe workshop characteristics engaged to reach program participants in various settings; and (3) describe personal characteristics of the first 100,000 participants. Each subsequent entering cohort was descriptively examined to indicate whether there was constancy or change in delivery sites and populations reached over time. Findings show a strengthening of the workshop delivery infrastructure in that it took 9.4 months to reach the first 25,000 participants in 853 counties compared to 5.4 months to reach the last 25,000 participants in 1,109 counties. The workshop delivery characteristics and participant characteristics remained relatively consistent across increments of 25,000 participants reached, although general trends were observed for some variables. For example, after reaching the first 25,000 participants, subsequent groups of 25,000 participants were reached more quickly. Additionally, workshops were increasingly delivered in ZIP Codes with higher percentages of families residing below the federal poverty line. As more participants were reached, more participants with chronic conditions were enrolled. This national translational study illustrates the rapid expansion of CDSME programs throughout the United States and capability to reach diverse populations in a variety of settings.
Introduction
Seen as a critical part of primary care for the past 20 years (1, 2), disease self-management programs have been associated with a plethora of positive health outcomes among middle-aged and older adults in the United States (3). While the healthcare system is increasingly expected to provide chronic care (1), chronic disease self-management initiatives outside of the physician’s office are now widely recognized as an effective complement to improve health indicators and quality of life while reducing overall health-related complications and associated costs (4). One of the most extensively tested programs, the Stanford Chronic Disease Self-Management Program (CDSMP), is a 6-week program (5) that has strong evidence demonstrating its ability to improve participants’ health status, modify their health behaviors, and reduce their healthcare utilization and associated costs (6–9). The interactive workshop sessions are designed to enhance three types of skills necessary for the everyday management of chronic conditions: medical management, emotional management, and social role management (6). While CDSMP remains the flagship program, Stanford has translated it to be delivered online, in multiple languages, and for specific diseases/conditions (e.g., diabetes, arthritis, chronic pain, HIV) (5). This collection of interventions (including CDSMP) comprises the suite of Chronic Disease Self-Management Education (CDSME) programs.
Building on a nascent evidence-based prevention initiative supported by the U.S. Administration on Aging (AoA) beginning in 2003 (10), funding was provided as part of the American Recovery and Reinvestment Act of 2009 (ARRA) to disseminate CDSME programs in 45 states, Puerto Rico, and the District of Columbia between 2010 and 2012 (11). Given the solid evidence base behind CDSMP, this jointly administered initiative of the AoA, the Centers for Disease Control and Prevention (CDC), and the Centers for Medicare and Medicaid Services (CMS) sought to bring these evidence-based programs to scale for the important goal of addressing the rapidly rising number of older adults struggling to manage their chronic conditions. The national goal of this ARRA-funded initiative was to reach at least 50,000 program completers (i.e., attend four or more of the six workshops sessions). Each participating state and entity was assigned a target goal for program completers based on the size of its population of older Americans. There was an expectation that certain delivery site types would be utilized (e.g., senior centers, healthcare organizations, residential facilities, educational institutions, faith-based organizations, and tribal centers), and special emphasis was placed on recruiting and enrolling racial/minority and other underserved populations.
The goal of having over 50,000 adults complete CDSME program workshops was accomplished within the first 24 months of this initiative across more than 1,000 United States counties (12). This accomplishment demonstrates the feasibility of a coordinated effort with the aging services network, the public health, and healthcare sectors. This study examined participant accrual of the first 100,000 participants enrolled in this national CDSME program roll out in four blocks (i.e., each representing 25,000 participants). Using this frame of progressing accrual blocks, the purposes of this study were to: (1) examine the geographic distribution of participation in this initiative across the Unites States; (2) describe workshop characteristics engaged to reach program participants in various settings; and (3) describe personal characteristics of the first 100,000 participants. Each subsequent entering cohort was descriptively examined to indicate whether there was constancy or change in delivery sites and populations reached over time.
Materials and Methods
Chronic Disease Self-Management Education (CDSME) Programs
As described previously, CDSMP falls within a suite of CDSME programs that have been widely disseminated in the U.S. as a method to empower patients with self-management skills to deal with their chronic conditions (12, 13). Drawing upon Social Learning Theory (14), CDSMP is an evidence-based, peer-led intervention consisting of six highly participative classes held for 2.5 h each, once a week, for six consecutive weeks (13). Additional details about the theory behind CDSME programs and their implementation can be found elsewhere (15).
Data Source and Study Population
This study reports findings based on cross-sectional data collected from the first 100,000 participants enrolled in the nationwide delivery of CDSME programs as part of the American Recovery and Reinvestment Act of 2009 (i.e., Recovery Act) Communities Putting Prevention to Work: Chronic Disease Self-Management Program initiative (12). Workshops were delivered in 45 states, Puerto Rico, and the District of Columbia (11). With support from AoA, a centralized online data system was developed by the National Council on Aging to collect data from participating organizations (15). Each state identified several database users at the state- and/or regional-level who were responsible for entering workshop and participant data.
Measures
In recognition of the importance of minimizing assessment burden, the data collection effort was limited to a short informational sheet about the delivery organization to be filled out by the delivery sites; a brief set of items describing participant characteristics such as age, sex, race/ethnicity, number and type of self-reported chronic conditions, living arrangements and ZIP Code (for participant residence and delivery site location); and attendance logs to document the specific sessions attended by each participant. While the expectation was that each organization would collect all the data referenced above, due to privacy and other concerns at some locations, all of the data elements were not collected at all of the sites (15). Further, because the completion of the participant questionnaire was not a pre-requisite for attending the workshop, some delivery sites chose not to collect all data points and some participants elected not to complete the questionnaire. However, to be counted as a “successful” completer (i.e., attending four of the six offered workshop sessions), the workshop information sheet and attendance roster was required.
Analyses
Statistical analyses for this study were performed using SPSS (version 21). Workshop and participant characteristics were compared between the first, second, third, and fourth group of 25,000 participants reached. Additionally, maps were generated to illustrate the cumulative geospatial distribution and accruement of CDSME program participants and workshops for the first 25,000 participants, 50,000 participants, 75,000 participants, and all 100,000 participants. Plots indicate workshop locations. Shading indicates the number of participants reached in each state (i.e., darker shade represents more participants reached). Hash markings represent the first year in which funding was received by state.
Results
National CDSME Program Uptake
Figure 1 depicts the cumulative geospatial distribution of the first 100,000 CDSME program enrollees by increments of 25,000 participants. As can be seen, the first 25,000 participants were reached by 2,226 workshops in 1,705 unique implementation sites over a 9.4-month period across 853 counties. At this stage in the intervention, only a few states had reached over 1,000 participants. Comparatively, the last 25,000 participants were reached by 2,154 workshops in 1,769 unique implementation sites over a 5.4-month period across 1,109 counties. At this stage in the intervention, only a few states had not reached over 1,000 participants.
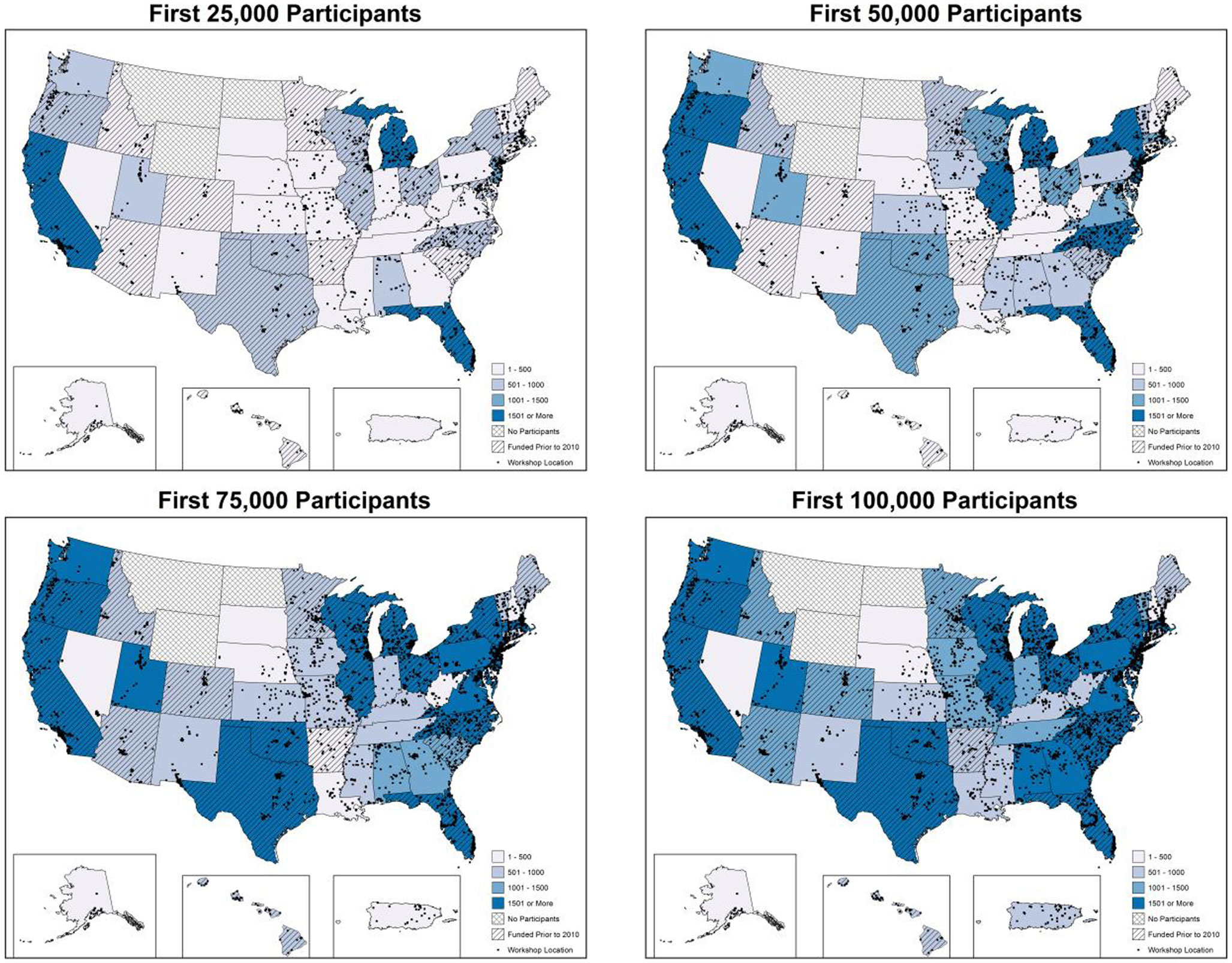
Figure 1. Geospatial distribution of CDSMP workshops and participants by increments of 25,000 participants.
CDSME Program Workshop Characteristics
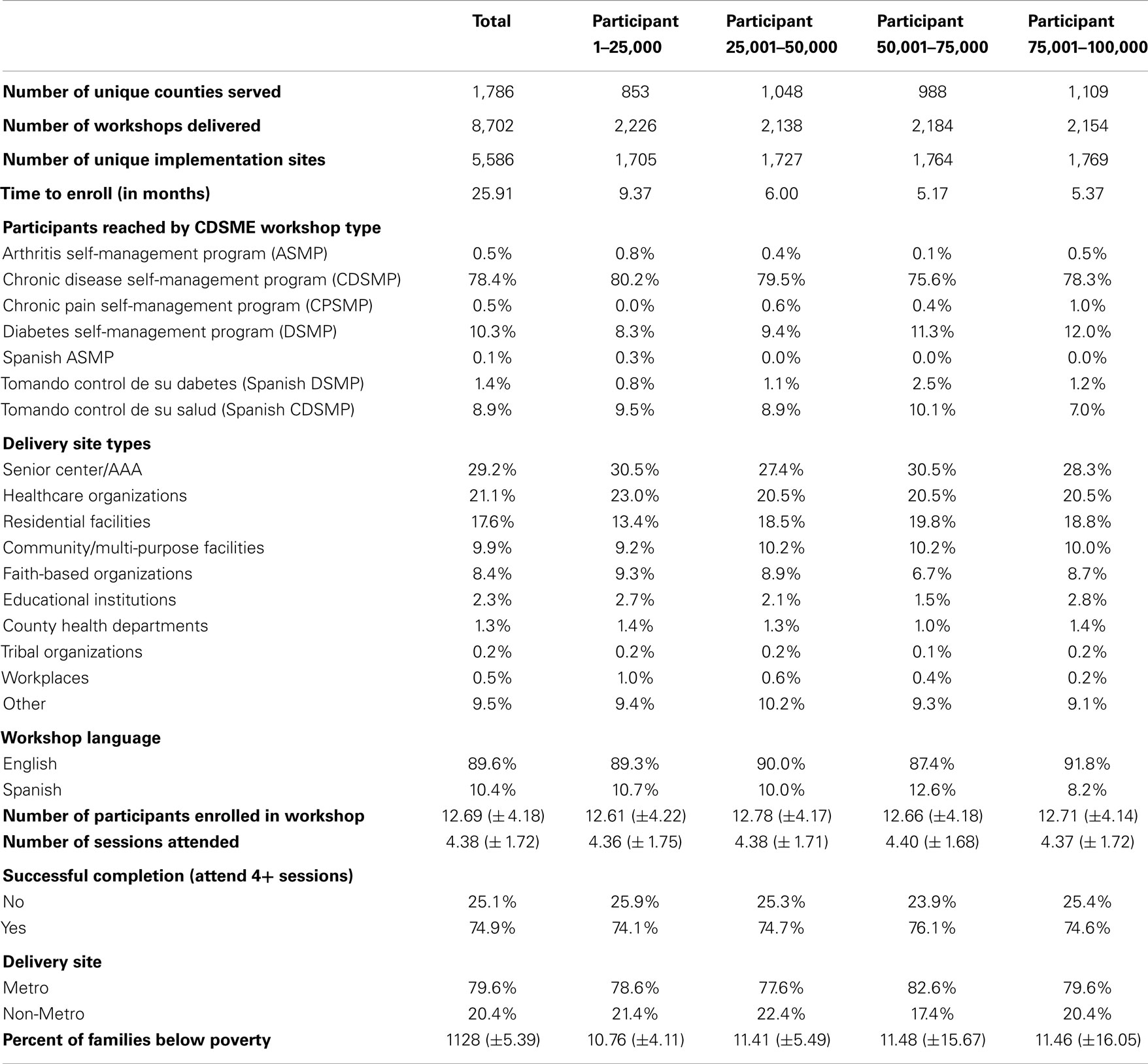
Table 1 presents workshop characteristics for the first 100,000 CDSME program participants enrolled in the intervention. These 100,000 participants were reached by 8,702 workshops in 5,586 unique implementation sites over a 25.9 month period across 1,786 counties. The majority of participants enrolled in CDSMP workshops (78.4%), followed by Diabetes Self-Management Program (DSMP) workshops (10.3%) and Tomando Control de su Salud (Spanish CDSMP) workshops (8.9%). The largest proportion of participants attended workshops at senior centers or area agencies on aging (29.2%), followed by healthcare organizations (21.1%), residential facilities (17.6%), community/multi-purpose facilities (9.9%), faith-based organizations (8.4%), and other settings (e.g., correctional facilities malls, RV parks, fire departments, county administration buildings, private residences, casinos, career centers). The majority of participants attended workshops delivered in English (89.6%) and in metro settings (79.6%). On average, workshops included 12.69 (±4.18) participants, and participants attended 4.38 (±1.72) sessions. The workshop completion rate was 74.9%.
Workshop delivery characteristics remained relatively consistent across increments of 25,000 participants reached, although general trends were observed for some variables. For example, after reaching the first 25,000 participants, it took shorter amounts of time to reach subsequent groups of 25,000 participants (i.e., 9.37 months to reach the first 25,000 participants and 5.37 months to reach the last 25,000 participants). As more participants were reached, larger proportions participated in DSMP workshops (i.e., 8.3% for the first 25,000 participants and 12.0% for the last 25,000 participants) and fewer participated in Spanish-language workshops (i.e., 10.7% for the first 25,000 participants and 8.2% for the last 25,000 participants). Additionally, workshops were increasingly delivered in ZIP Codes with higher percentages of families residing below the federal poverty line (i.e., an average of 10.76 families below poverty for the first 25,000 participants and 11.46 for the last 25,000 participants).
CDSME Program Participant Characteristics
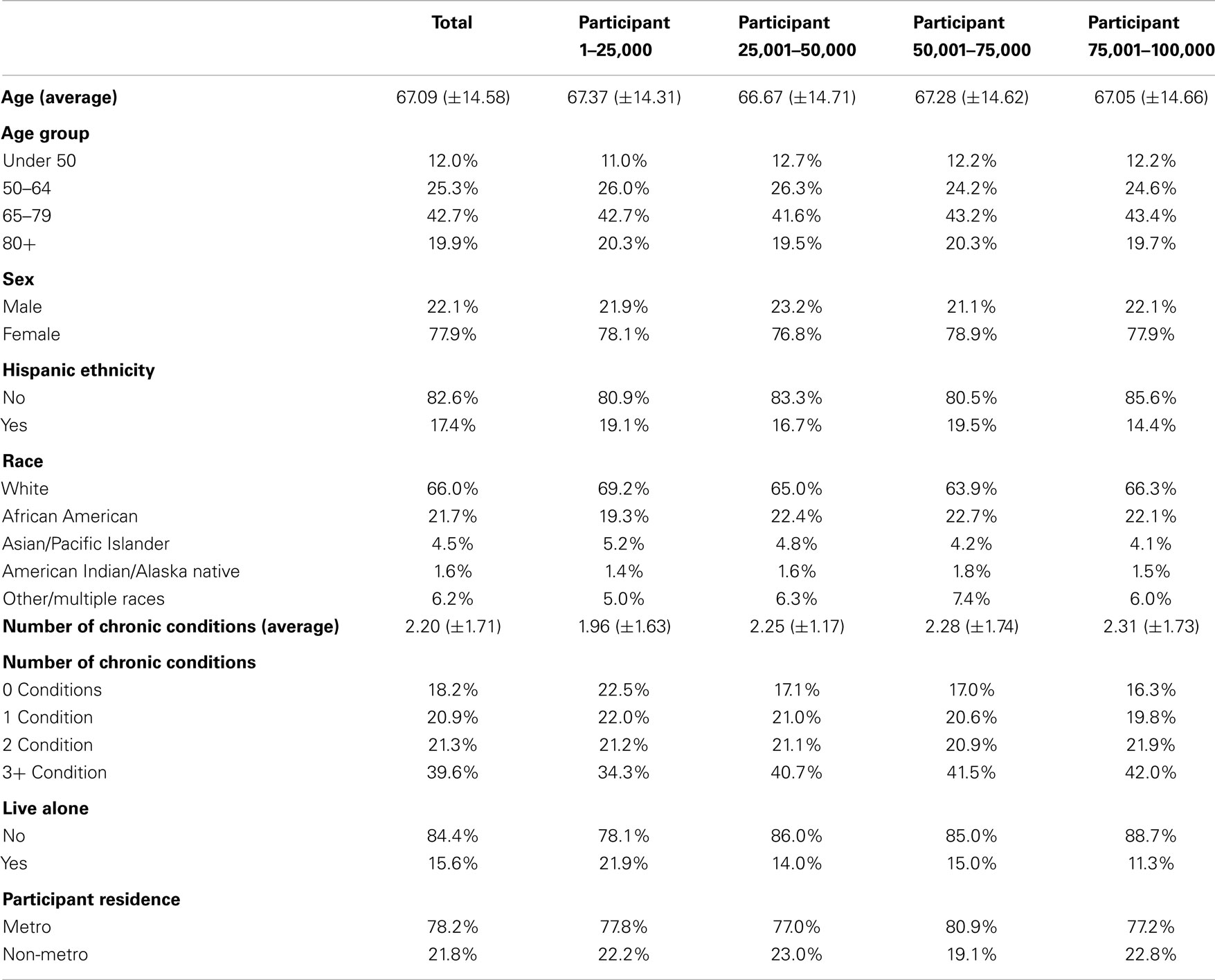
Table 2 presents participant characteristics of the first 100,000 CDSME program participants enrolled in the intervention. On average, the first 100,000 CDSME program participants were 67.09 (±14.58) years of age; 12.0% were under age 50 years, 42.7% were aged 65–79 years, and 19.9% were aged 80 years and older. The majority of participants was female (77.9%), non-Hispanic (82.6%), and white (66.0%). Approximately 22% of participants were African American, 4.5% were Asian or Pacific Islander, 1.6% American Indian or Native Alaskan, and 6.2% “other” or multiple races. The majority of participants resided with other individuals (84.4%) and lived in metro areas (78.2%). On average, participants self-reported 2.20 (±1.71) chronic conditions; 39.6% reported three or more co-morbidities.
Generally, participant characteristics remained consistent across increments of 25,000 participants reached; however, trends were observed for some variables. For example, as more participants were reached by CDSME programs, more participants with chronic conditions were enrolled, with the number of participants enrolling with three or more chronic conditions increasing from 34.3% for the first 25,000 participants to 42.0% for the last 25,000 participants (i.e., participant 75,001–100,000). Additionally, as more participants were reached, the program enrolled smaller proportions of participants who lived alone (i.e., decreasing from 21.9% for the first 25,000 participants to 11.3% for the last 25,000 participants).
Discussion
Self-management education has been recognized as a critical factor in empowering adults to improve their health and functioning (3). This study provides valuable dissemination and implementation insights into the nature and progression of the largest ever national roll out of CDSME programs (i.e., highly effective evidence-based programs designed to help middle-aged and older adults more effectively manage their chronic conditions). The aging services sector, in partnership with other healthcare, public health, community, and faith-based organizations, proved to be a coordinated, efficient, and diverse delivery system capable of rapidly reaching large numbers of older adults across the country. Exceeding programmatic goals of having 50,000 participants complete CDSME program workshops (12), over 100,000 participants were reached more quickly than in previous efforts (16). Further, with the exception of a predominant female participant population typically served with health promotion programs (16–18), participants were representative of the U.S. population and not just easy-to-reach subgroups.
The ability of this initiative to quickly reach 100,000 participants can be attributed to many factors. First, having each state set ambitious yet feasible and attainable goals (19) can help stimulate them to think differently about program planning, participant recruitment, and partnership development. Second, the stimulus money utilized in this initiative was essential for reaching this recruitment goal, but it was also leveraged by funds from other organizations with some non-traditional partners (e.g., healthcare partners), which fostered growth by adopting and promoting CDSME programs as an integral care practice. Third, capitalizing on the existing program delivery infrastructure established by previous AoA initiatives, the broad network of delivery and funding partners has resulted in widespread financing of CDSME programs by other government organizations. Fourth, workshops were available in many local communities largely because of the cooperation of the program developers to utilize and expand their training infrastructure (5). As seen in this initiative, the culmination of leveraging opportunities led to the rapid dissemination of CDSME programs by creating a highly collaborative community structure that accelerated the speed of scalability across the country to meet the needs of an increasingly diverse group of participants.
Past reports have shown CDSME programs have capacity to serve large numbers of heterogeneous adults via a growing network of delivery sites (8, 12, 20, 21). Success can be attributed, in part, to a community-driven delivery system that employed existing networks for recruiting participants of varied ages, race/ethnicity; disease status; geographic region; and socio-economic status (22). However, additional efforts are needed to help CDSME programs gain major penetration among the over 35 million older Americans estimated to have at least one chronic condition (23). As such, this study suggests several actions that can help make the dissemination of CDSME programs part of routine care.
First, we must further examine and strengthen referral systems to CDSME programs and the interconnectedness of the healthcare, public health, and aging services networks. Multi-institute funding initiatives that highly encourage/mandate multi-sectorial partnerships can set the stage for bridging such connections (11). Second, we need to embrace the paradigm shift in provider-patient communications that emphasizes the value of “informed and activated” patients working collaboratively with their prepared practice team (1). This theme, initially articulated in Wagner’s chronic care model, is being revisited with the recent movement toward patient-centered care (24). Third, we need to be aware of the constraints facing today’s healthcare providers in terms of shortened office visits and greater expectations for administrative paperwork (25). Thus, we recommend easy-to-employ methods and mechanisms (e.g., automated systems) to help health care providers know where evidence-based programs like CDSMP are offered. Also, guidelines are needed for identifying the types of patients who are best suited for specific programs (e.g., information about the pros and cons of generic self-care programs versus disease-specific programs). While clinicians and other allied health providers should be trained about these guidelines and referral processes, it is also important that program participants report back to their healthcare providers about their experiences and progress in such programs. Fourth, we must recognize that programmatic scalability needs to be paired with plans for achieving sustainability over time. Thus, we recommend that national, state, and local roll outs of evidence-based programs include sustainability planning as a core element. Successful sustainability plans are those that build upon and leverage existing resources, often employing champions for recognizing and promoting new models of care (26).
There are study limitations that must be acknowledged. While this national effort afforded large numbers of participants, specific data points were limited due to community concerns regarding burden. Additionally some data was missing due to local/regional constraints, and not necessarily individual refusal. Study data represented a “snapshot” of an ongoing evolving evaluation process at a particular time point. Underserved populations (e.g., African Americans) were overrepresented in this study because of the focus of the larger initiative to serve this subgroup of Americans. However, males were underrepresented in this study, as they traditionally are in evidence-based programs delivered through the aging services network (16–18). Despite these limitations inherent when using administrative records, we nevertheless believe this study represents a unique examination about how a national evidence-based dissemination rolls out over time, what infrastructure facilitates this type of grand-scale roll out, and what types of participants are reached.
Findings from this study capture the spread of CDSME programs during a national, government-funded roll out and show the ability of this intervention to rapidly reach a diverse set of participants using a well-coordinated delivery system. As of August 2014, over 196,700 participants reached by CDSME programs through 17,500 workshops in 1,200 counties across the United States. While this initiative capitalized and built upon previous efforts to create a delivery infrastructure for CDSME programs, this grand-scale dissemination has solidified the presence of CDSME programs with great potential for long-term sustainability. While this initiative has achieved impressive participant reach and completion, it should be noted that many other organizations throughout the United States offered the intervention despite not receiving this ARRA funding. Because data from these organizations are not represented in the databased used in the current study, these findings are even more encouraging in that they underrepresent the actual translation of CDSME programs nationwide. Continued efforts are needed to track the progression and proliferation of this suite of programs to empower patients with self-management skills to deal with their chronic conditions.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
This paper is included in the Research Topic, “Evidence-Based Programming for Older Adults.” This Research Topic received partial funding from multiple government and private organizations/agencies; however, the views, findings, and conclusions in these articles are those of the authors and do not necessarily represent the official position of these organizations/agencies. All papers published in the Research Topic received peer review from members of the Frontiers in Public Health (Public Health Education and Promotion section) panel of Review Editors. Because this Research Topic represents work closely associated with a nationwide evidence-based movement in the US, many of the authors and/or Review Editors may have worked together previously in some fashion. Review Editors were purposively selected based on their expertise with evaluation and/or evidence-based programming for older adults. Review Editors were independent of named authors on any given article published in this volume.
Acknowledgments
The American Recovery and Reinvestment Act of 2009 (i.e., Recovery Act) Communities Putting Prevention to Work: Chronic Disease Self-Management Program initiative, led by the U.S. Administration on Aging in collaboration with the Centers for Disease Control and Prevention and the Centers for Medicare and Medicaid Services, allotted $32.5 million to support the translation of the Stanford program in 45 States, Puerto Rico, and the District of Columbia. The National Council on Aging served as the Technical Assistance Resource Center for this initiative and collected de-identified data on program participation.
References
1. Wagner EH, Glasgow RE, Davis C, Bonomi AE, Provost L, McCulloch D, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv (2001) 27(2):63–80.
2. Barr V, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, et al. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q (2003) 7(1):73. doi: 10.12927/hcq.2003.16763
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
3. Brady TJ, Murphy L, O’Colmain BJ, Beauchesne D, Daniels B, Greenberg M, et al. A meta-analysis of health status, health behaviors, and healthcare utilization outcomes of the chronic disease self-management program. Prev Chronic Dis (2013) 10:120112. doi:10.5888/pcd10.120112
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
4. Brady T, Murphy L, Beauchesne D, Bhalakia A, Chervin D, Daniels B, et al. Sorting Through the Evidence for the Arthritis Self-Management Program and the Chronic Disease Self-Management Program: Executive Summary of ASMP/CDSMP Meta-Analysis. Atlanta, GA: Centers for Disease Control and Prevention (CDC) (2011).
5. Stanford School of Medicine. Chronic Disease Self-Management Program (Better Choices, Better Health® Workshop) [cited 2014 July 12]. Available from: http://patienteducation.stanford.edu/programs/cdsmp.html
6. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA (2002) 288(19):2469–75. doi:10.1001/jama.288.19.2469
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
7. Lorig KR, Sobel DS, Stewart AL, Brown BW Jr, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care (1999) 37(1):5–14. doi:10.1097/00005650-199901000-00003
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
8. Ory MG, Ahn S, Jiang L, Smith ML, Ritter PL, Whitelaw N, et al. Successes of a national study of the chronic disease self-management program: meeting the triple Aim of health care reform. Med Care (2013) 51(11):992–8. doi:10.1097/MLR.0b013e3182a95dd1
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
9. Ahn S, Basu R, Smith ML, Jiang L, Lorig K, Whitelaw N, et al. The impact of chronic disease self-management programs: healthcare savings through a community-based intervention. BMC Public Health (2013) 13(1):1141. doi:10.1186/1471-2458-13-1141
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
10. Department of Health and Human Services. AoA Evidence-Based Prevention Programs. Washington, DC: Administration on Aging. (2013) [cited 2014 July 8]. Available from: http://www.aoa.gov/AoA_Programs/HPW/Title_IIID/index.aspx
11. U.S. Department of Health and Human Services, Administration on Aging. ARRA – Communities Putting Prevention to Work: Chronic Disease Self-Management Program. (2012) [cited 2014 June 14]. Available from: www.cfda.gov/index?s=program&mode=form&tab=step1&id=5469a61f2c5f25cf3984fc3b94051b5f
12. Ory MG, Smith ML, Kulinski KP, Lorig K, Zenker W, Whitelaw N. Self-management at the tipping point: reaching 100,000 Americans with evidence-based programs. J Am Geriatr Soc (2013) 61(5):821–3. doi:10.1111/jgs.12239
13. Lorig K. Living a Healthy Life with Chronic Conditions: Self-Management of Heart Disease, Arthritis, Diabetes, Asthma, Bronchitis, Emphysema & Others. 3rd ed. Boulder, CO: Bull Pub. Company (2006). 382 p.
14. Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process (1991) 50(2):248–87. doi:10.1016/0749-5978(91)90022-L
15. Kulinski KP, Boutaugh M, Smith ML, Ory MG, Lorig K. Setting the stage: measure seletion, coordination, and data collection for a national self-management initiative. Front Public Health (2015) 2:206. doi:10.3389/fpubh.2014.00206
16. Smith M, Belza B, Altpeter M, Ahn S, Dickerson J, Ory M. Disseminating an evidence-based disease self-management program for older Americans: implications for diversifying participant reach through delivery site adoption. In: Maddock J, editor. Rijeka. Croatia: InTech (2012). p. 385–404.
17. Smith ML, Ory MG, Belza B, Altpeter M. Personal and delivery site characteristics associated with intervention dosage in an evidence-based fall risk reduction program for older adults. Transl Behav Med (2012) 2(2):188–98. doi:10.1007/s13142-012-0133-8
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
18. Smith ML, Belza B, Braun KL, King S, Palmer RC, Sugihara NS, et al. National reach and dissemination of enhancefitness. Health Behav Policy Rev (2014) 1(2):150–60. doi:10.14485/HBPR.1.2.7
19. The art of health promotion. Am J Health Promot (2004) 18(4): TAH–1–TAH–12. doi:10.4278/0890-1171-18.4.TAHP-1
20. Erdem E, Korda H. Self-management program participation by older adults with diabetes: Chronic Disease Self-Management Program and Diabetes Self-Management Program. Fam Community Health (2014) 37(2):134–46. doi:10.1097/FCH.0000000000000025
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
21. Korda H, Erdem E, Woodcock C, Kloc M, Pedersen S, Jenkins S. Racial and ethnic minority participants in chronic disease self-management programs: findings from the communities putting prevention to work initiative. Ethn Dis (2012) 23(4):508–17.
22. Burdine JN, McLeroy K, Blakely C, Wendel ML, Felix MR. Community-based participatory research and community health development. J Prim Prev (2010) 31(1):1–7. doi:10.1007/s10935-010-0205-9
23. Anderson GF. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation (2010).
24. Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care (2011) 34(4):1047–53. doi:10.2337/dc10-1671
25. Ahn S, Tai-Seale M, Huber C Jr, Smith ML, Ory MG. Psychotropic medication discussions in older adults’ primary care office visits: so much to do, so little time. Aging Ment Health (2011) 15(5):618–29. doi:10.1080/13607863.2010.548055
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
Keywords: chronic disease self-management, evidence-based program, older adults, sustainability, program implementation, program reach, evaluation
Citation: Smith ML, Ory MG, Ahn S, Kulinski KP, Jiang L, Horel S and Lorig K (2015) National dissemination of chronic disease self-management education programs: an incremental examination of delivery characteristics. Front. Public Health 2:227. doi: 10.3389/fpubh.2014.00227
Received: 07 August 2014; Accepted: 24 October 2014;
Published online: 27 April 2015.
Edited by:
Sanjay P. Zodpey, Public Health Foundation of India, IndiaReviewed by:
Aida Mujkic, University of Zagreb, CroatiaRonit Elk, University of South Carolina, USA
Copyright: © 2015 Smith, Ory, Ahn, Kulinski, Jiang, Horel and Lorig. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthew Lee Smith, Department of Health Promotion and Behavior, College of Public Health, The University of Georgia, 330 River Road, 315 Ramsey Center, Athens, GA 30602, USA e-mail: health@uga.edu
 Matthew Lee Smith
Matthew Lee Smith Marcia G. Ory
Marcia G. Ory SangNam Ahn
SangNam Ahn Kristie P. Kulinski
Kristie P. Kulinski Luohua Jiang
Luohua Jiang Scott Horel2
Scott Horel2 Kate Lorig
Kate Lorig