
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 17 April 2025
Sec. Psychological Therapy and Psychosomatics
Volume 16 - 2025 | https://doi.org/10.3389/fpsyt.2025.1566560
Background: Childhood maltreatment has been well established to contribute to the development and the poorer course of mental disorders across the lifespan. However, studies focusing on patients who are undergoing psychotherapy in natural settings are rare. On this background, the current study aimed to investigate (1) the prevalence of childhood maltreatment in routine care psychotherapy patients, (2) associations between childhood maltreatment and symptom severity, and (3) the influence of childhood maltreatment on treatment outcome.
Method: Data from N = 549 outpatients [60.3% female; age: M(SD) = 36.29 (13.47), range: 17–74 years] who received cognitive behavioral therapy at an outpatient clinic were collected. Self-report measures of childhood maltreatment, depression, anxiety, positive mental health, and treatment satisfaction were assessed before and after treatment.
Results: Any form of childhood maltreatment was reported by 57.6% of the study sample; women were more affected than men, and childhood maltreatment was associated with heightened symptom severity and lowered positive mental health. Emotional abuse was predictive of increased posttreatment depression, anxiety, and reduced positive mental health, whereas emotional neglect was predictive of lower patient-reported global treatment success—after controlling for age, gender, pretreatment depression, anxiety, and positive mental health.
Discussion: Childhood maltreatment is prevalent in routine care psychotherapy patients and associated with symptom severity as well as reduced treatment response. Emotional abuse and emotional neglect exert an especially pernicious influence; particular attention must therefore be paid to these respective childhood experiences, as they can easily go unnoticed in the early phases of psychotherapy.
Childhood maltreatment has been well established to contribute to the development and the poorer course of mental disorders across the lifespan (1). Childhood maltreatment is commonly defined as “all forms of physical and/or emotional ill-treatment, sexual abuse, neglect or negligent treatment or commercial or other exploitation, resulting in actual or potential harm to the child’s health, survival, development or dignity in the context of a relationship of responsibility, trust or power” (2). It is conceptualized as emotional, physical, and sexual abuse, or emotional and physical neglect before the age of 18 (3). It is estimated that one in four children will experience child abuse or neglect at some point in their lifetime and one out of seven children have experienced abuse over the last year. However, it is widely accepted that these statistics represent a significant underestimate of the prevalence of childhood maltreatment because the majority of abuse and neglect goes unreported (4).
Childhood maltreatment has severe and long-lasting effects on both mental and somatic health across the lifespan. About one-third of all adult-onset psychiatric disorders are related to childhood maltreatment, with effects on morbidity and mortality. It is associated with an earlier age of onset and more severe clinical course (i.e., symptom severity) and poorer treatment response to pharmaco-/psychotherapy (5, 6). Childhood maltreatment not only affects mental health but also increases the risk of obesity, diabetes, lung disease, and cardiovascular disorders (4, 7). Unfortunately, childhood maltreatment is common in the general population. For instance, a recent systematic review on the lifetime prevalence of self-reported childhood maltreatment revealed the following median prevalence rates for European countries: Sexual abuse 13.2%, emotional abuse 11.7%, physical abuse 12.2%, and neglect 27.0% (8).
In clinical samples, the prevalence rates are higher as evidenced in two meta-analyses: Nelson et al. (6) estimated the prevalence of different types of childhood maltreatment in adults suffering from depression. Kuzminskaite et al. (5) used data from the “Netherlands Study of Depression and Anxiety NESDA” including patients suffering from current and remitted depressive and/or anxiety disorders to calculate prevalence rates. In the Nelson et al. study, 45.6% of the sample had experienced at least one type of childhood maltreatment; in the Kuzminskaite et al. study, it was 53.9%; with emotional neglect (43.2%/44.0%) and emotional abuse (36.7%/28.5%) being the most prevalent types, followed by physical abuse (27.6%/15.4%), and sexual abuse (25.3%/19.7%).
Nelson et al. (6) also reported that all types of childhood maltreatment significantly increased the risk of adult depression in individuals with childhood maltreatment compared with those without childhood maltreatment. Furthermore, depressive disorder is twice as likely to take a chronic course in individuals with a history of childhood maltreatment, and childhood maltreatment has been shown to be associated with symptom severity (3, 5, 6, 9). Finally, evidence-based pharmacotherapies and psychotherapies seem to be less effective in patients with a history of childhood maltreatment compared to patients without childhood maltreatment, especially for depressed patients: In a meta-analysis by Nanni et al. (10), adults and adolescents with depression and childhood maltreatment were about 1.5 times more likely not to respond or remit after pharmacotherapy, psychotherapy, or combination treatment than depressed patients with no such experiences. These findings were extended by a meta-analysis of studies published in 2013, which suggested that adults with depression and childhood maltreatment were twice as likely not to respond to psychotherapy or pharmacotherapy (6). However, treatment outcomes in patients with childhood maltreatment have not been definitive. In the most recent meta-study by the Childhood Trauma Meta-Analysis Study Group (3), 29 trials—both RCTs and open trials—with depressed patients with and without childhood maltreatment were included. More than half (62%) of the patients reported a childhood maltreatment history. Treatment was efficacious in reducing depression severity for both individuals with and those without childhood maltreatment (vs. control condition). As such, despite having more severe depression at baseline, there was no significant difference in active treatment effects between individuals with and without childhood maltreatment. Inconsistent findings within these meta-analyses might be due to publication and selection bias (3) as well as different operationalization of therapy outcome (9).
To summarize, childhood maltreatment is a common risk factor for developing in particular depressive and anxiety disorder in adulthood. The prevalence of childhood maltreatment in patient samples is about 50%. All types of childhood maltreatment, predominantly emotional abuse/neglect, seem to be associated with psychological distress. Furthermore, childhood maltreatment is associated with earlier onset, more chronic or recurrent symptoms, and greater probability of having comorbidities, especially in depressed patients. However, very different samples have been included in the various trials, and up to date, there are only few studies focusing on patients who are undergoing psychotherapy in natural settings (9), which are not part of research projects with the usual restrictions (exclusion and inclusion criteria to sample homogenous patients, following strict treatment manuals, same length of treatment). Here we will focus on such a sample from an outpatient clinic with routine outcome monitoring. The following questions will be answered: Are there gender differences in terms of childhood maltreatment prevalence rates? Do different diagnostic groups differ in terms of childhood maltreatment type prevalence rates? Is symptom severity associated with childhood maltreatment? Are there differences in treatment outcome depending on the presence of childhood maltreatment? Consistent with previous studies, we expected (1) women to report more experiences with childhood maltreatment than men and (2) childhood maltreatment to be associated with symptom severity. No expectations were formulated with regard to the diagnostic groups, mainly because it was initially unclear which diagnostic groups would be available in sufficient numbers in the current sample. Furthermore, due to inconsistent findings (3, 6, 9, 10), no specific expectations were formulated with regard to maltreatment-related differences in treatment outcome.
The study sample comprises N = 549 adult outpatients [60.3% female; age: M(SD) = 36.29 (13.47), range: 17–74 years] undergoing individual cognitive behavioral therapy at an outpatient university clinic in the Ruhr area in Germany between April 2017 and September 2022. Participants were eligible for the current study if complete CTQ data were available. Assessments were conducted prior to treatment (T1) and again after 24 therapy sessions [T2; mean time between T1 and T2: (M) = 9.27 months, standard deviation (SD) = 3.22; number of therapy sessions: (M) = 23.60 sessions, (SD) = 1.43], which corresponds to a short-term therapy within the German insurance system. The most common primary diagnoses according to the International Classification of Diseases (ICD-10) were Recurrent Depressive Disorder (21.9%, n = 120), Adjustment Disorder (10.9%, n = 60), Single Episode Depressive Disorder (10.0%, n = 55), Social Phobia (9.5%, n = 52), Panic Disorder with/without Agoraphobia (9.1%, n = 50) and Dysthymia (7.8%, n = 43). Comparable few participants suffered from Posttraumatic Stress Disorder (PTSD; 4.9%, n = 27) or Borderline Personality Disorder (BPS; 3.1%, n = 17). All patients were Caucasian. Treatments were conducted by clinical psychologists in advanced CBT training, who provided treatment under close-meshed CBT supervision (every fourth session with a licensed CBT supervisor). Treatments generally followed published CBT guidelines for each disorder but were, in most cases, less standardized than in RCTs. Treatments were paid for by the German health insurance system.
All patients were informed that the clinic regularly conducts research and provided informed consent prior to participation. In order to assure a standard of quality, all clients seeking help at the clinic are required to fill out questionnaires prior to their intake. No compensation is given to clients for doing so. This study was reviewed and approved by the local ethics committee (318/2016).
Childhood Trauma Questionnaire (CTQ; 11). The CTQ is a retrospective self-report measure of adverse childhood experiences. The scale includes 28 items assessing sexual (SA, “made to do sexual things”), emotional (EA, “felt hated by family”) and physical abuse (PA, “hit hard enough to see a doctor”), and emotional (EN, “felt loved”) and physical neglect (PN, “wore dirty cloth”) with five items per subscale (and three items assessing dissimulation tendencies). All items are to be answered on a 5-point Likert scale ranging from “1” (never) to “5” (very often). The subscales of the German version of the CTQ (11) have been shown to have high internal consistency (α ≥.80) except for the subscale physical neglect (α = .55). Accordingly, internal consistency was good in the current sample: EA (α = .88), PA (α = .86), SA (α = .91), EN (α = .91), and PN (α = .64). Maltreatment is assumed when threshold scores for emotional abuse (≥10), emotional neglect (≥15), physical abuse (≥8), physical neglect (≥8), and sexual abuse (≥8) are met (12). Furthermore, the CTQ manual (13) contains thresholds to divide subscale scores into severity quartiles: “none/minimal” (EA < = 8, PA < = 7, SA = 5, EN < = 9, PN< = 7), “low to moderate” (EA > 8 and < = 12, PA > 7 and < = 9, SA > 5 and < = 7, EN > 9 and < = 14, PN > 7 and < = 9), “moderate to severe” (EA > 12 and < = 15, PA > 9 and < = 12, SA > 7 and < = 12, EN > 15 and < = 17, PN > 9 and < = 12), and “severe to extreme” (EA > = 16, PA > = 13, SA > = 13, EN > = 18, PN > = 13). Due to a technical error, one item of the sexual abuse subscale (“someone molested me”) was not presented to participants. Therefore, the total score of this subscale cannot be compared to other studies, and prevalence scores on sexual abuse cannot be reported in the current study.
Depression Anxiety Stress Scales (DASS-42 (14);). The DASS measures symptoms of depression, anxiety, and stress over the past week with 14 items per subscale. In the current study, only the depression subscale (e.g., “I felt that life was meaningless”) and the anxiety subscale (e.g., “I felt scared without any good reason”) were used. All items are rated on a 4-point Likert-type scale (0 = did not apply to me at all, 3 = applies to me very much or most of the time). Higher sum scores indicate more severe symptoms. All subscales have been shown to have high internal consistency (DASS-D: α = .81–.88; DASS-A: α = .78–.84 (15);). Accordingly, internal consistency was good in the current sample: DASS-D: α= .95 (T1) and α= .96 (T2); DASS-A: α= .88 (T1) and α= .91 (T2).
Positive Mental Health Scale (16). The PMH scale asks respondents to rate how much they agree with different statements on subjective and psychological well-being (e.g., “I enjoy my life”, “All in all, I am satisfied with my life”, “I feel that I am actually well equipped to deal with life and its difficulties”). The scale comprises nine items rated on a scale ranging from 1 (do not agree) to 4 (agree), with higher scores indicating greater positive mental health. Unidimensional structure, good convergent, and discriminant validity as well as high internal consistency (α >.81) have been demonstrated in various populations (16). Accordingly, Cronbach’s alpha was good in the current study: α=.90. (T1) and α= .93 (T2).
Global success ratings (17). Patients’ evaluation of their global therapy success was assessed with two items (“Have your expectations of the therapy been fulfilled”, “How much did the therapy benefit you overall?”) that are rated on a scale ranging from 1 (“on the opposite—it has become worse”) to 6 (“completely/very much”). Higher scores represent higher satisfaction with treatment. The two items are strongly correlated (r = .737, p <.001) and were summed up in the current study (18).
Statistical analyses were conducted using SPSS 29. Maltreatment prevalence rates will be reported according to the cut-off scores established by Walker et al. (12): CTQ emotional abuse (≥10), CTQ emotional neglect (≥15), CTQ physical abuse (≥8), and CTQ physical neglect (≥8). Furthermore, maltreatment rates will be reported in accordance with the severity quartiles established by Bernstein et al. (13). In addition, rates of maltreatment are going to be reported separately for male and female gender, as well as for the different diagnostic groups. Assignment to a diagnostic group (yes/no) was based on the respective primary diagnosis. Only mental disorders with a prevalence rate 5% within the current sample were taken into account. Gender differences in the severity of maltreatment were investigated using t-test for independent samples. A series of multiple logistic regression analysis were used to examine the relative contribution of diagnostic groups, age, and gender to the prediction of the presence of emotional abuse, physical abuse, emotional neglect, and physical neglect. Associations between pretreatment symptom severity (DASS-D, DASS-A, PMH) and childhood maltreatment were established using correlation analyses. Changes in study variables from T1 to T2 were analyzed using t-tests for dependent samples. To identify significant predictors of posttreatment (T2) symptom severity (DASS-D, DASS-A), positive mental health (PMH), and global success ratings (GSR), a series of hierarchical regression analyses was calculated using age, gender, DASS-D (T1), DASS-A (T1), PMH (T1), and all CTQ subscales (T1) as predictors. Assuming a medium-sized effect (f2 = 0.15), an alpha error level of 5%, 11 predictors, and a sample size of N= 549, the test power was 1−ß ≥ 0.90 and therefore sufficient according to Cohen (19). In all hierarchical regression models, there was no violation of the multicollinearity assumption, as all values of tolerance were >.25, and all variance inflation factor values were <5 (20).
In total, 57.6% (n = 316) participants suffered from some kind of childhood maltreatment. Emotional abuse was reported by 43.5% participants (none/mild = 41.2%; low/moderate = 29.2%; moderate/severe = 10.0%; severe/extreme = 19.5%). Physical abuse was reported by 20.8% participants (none/mild = 79.2%; low/moderate = 8.6%; moderate/severe = 5.5%; severe/extreme = 6.8%). Emotional neglect was reported by 34.2% participants (none/mild = 33.9; low/moderate = 31.9%; moderate/severe = 15%; severe/extreme = 19.2%), and physical neglect was reported by 36.9% participants (none/mild = 63.1%; low/moderate = 18.3%; moderate/severe = 13.3%; severe/extreme = 5.3%).
Childhood maltreatment prevalence rates in regard to gender and diagnostic groups. Female participants suffered from more experiences with emotional abuse, t (546) = 3.81, p <.001, d = 0.33; sexual abuse, t(543) = 2.31, p = .01, d = 0.20; and physical neglect, t(545) = 2.21, p = .01, d = 0.19, than male participants (see also Table 1).
On a descriptive level, emotional abuse and emotional neglect were most prevalent in participants suffering from social phobia, whereas physical abuse and physical neglect were most prevalent in participants suffering from some kind of unipolar depression. In a series of multiple logistic regression models (see Table 2), Social Phobia, Dysthymia, and Major Depression (single episode) were most strongly associated (OR ≥2) with emotional neglect, whereas Dysthymia, Major Depression (single/recurrent), and Social Phobia were most strongly associated (OR ≥2) with physical neglect. None of the different disorders showed a notable association with emotional or physical abuse.
Childhood maltreatment and symptom severity. The presence of any kind of childhood maltreatment, except for sexual abuse, was associated with more severe pretreatment depression and anxiety as well as lower levels of positive mental health (see Table 3).
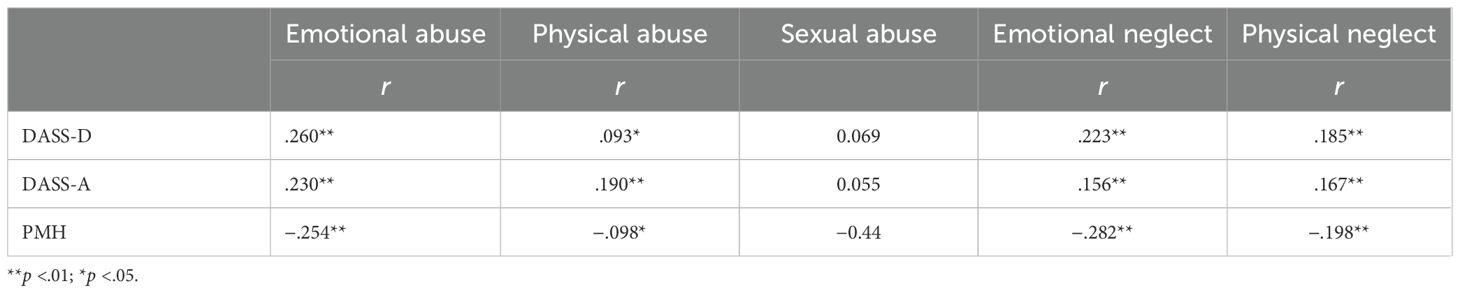
Table 3. Associations between pretreatment symptom severity and experiences with childhood maltreatment.
Childhood maltreatment and treatment outcome. T-tests for dependent samples revealed that depression (T1: M = 19.60, SD = 11.14; T2: M = 13.26, SD = 10.85), t(543) = 14.36, p ≤.001, d = .62, and anxiety (T1: M = 11.64, SD = 7.92; T2: M = 8.23, SD = 7.36), t(546) = 10.58, p ≤.001, d = 36, decreased whereas positive mental health (T1: M = 10.30, SD = 5.55; T2: M = 13.47, SD = 6.22), t(536) = 15.21, p ≤.001, d = 66, increased from before to after treatment. Tables 4–7 show the results of hierarchical linear regression analyses with posttreatment depression, anxiety, positive mental health, and global success as criterion variables. Emotional abuse was predictive of heightened posttreatment depression (see Table 4), posttreatment anxiety (see Table 5), and lowered posttreatment positive mental health (see Table 6)—after control of age, gender, pretreatment depression, anxiety, and positive mental health. Emotional neglect was predictive of lower patient posttreatment success rating (see Table 7). Sexual abuse, physical abuse, and physical neglect showed no predictive association in any of the investigated models. Of note, pretreatment positive mental health was shown to be predictive of therapy outcome in every investigated model. However, it has to be highlighted that adding the CTQ subscales in step 2 of each model only improved the model’s explained variance for posttreatment depression (see Table 4), but not for posttreatment anxiety, posttreatment positive mental health, and global success (see Tables 5–7).
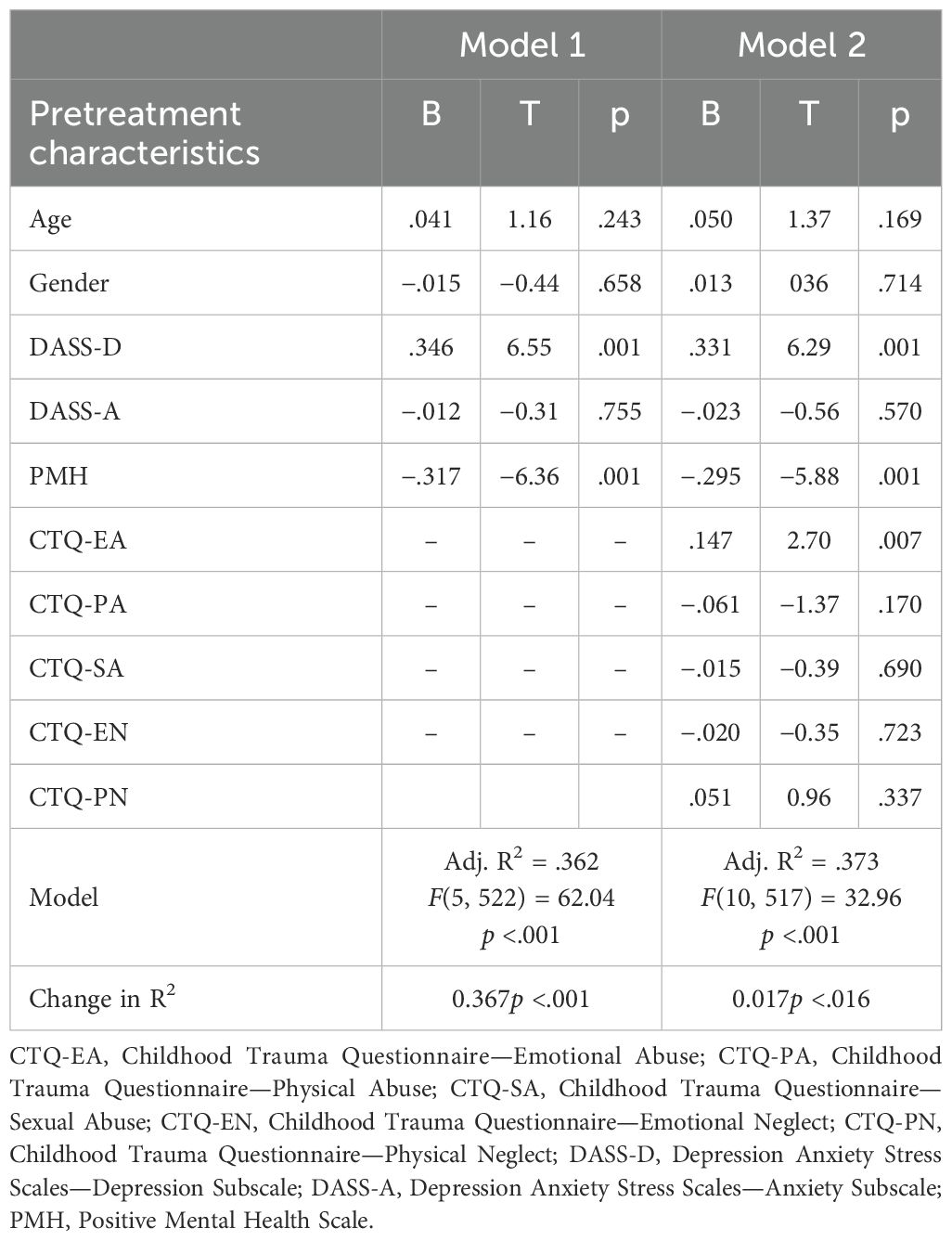
Table 4. Prediction of posttreatment depression by pretreatment symptomatology, positive mental health, and traumatic childhood experiences (n = 528).
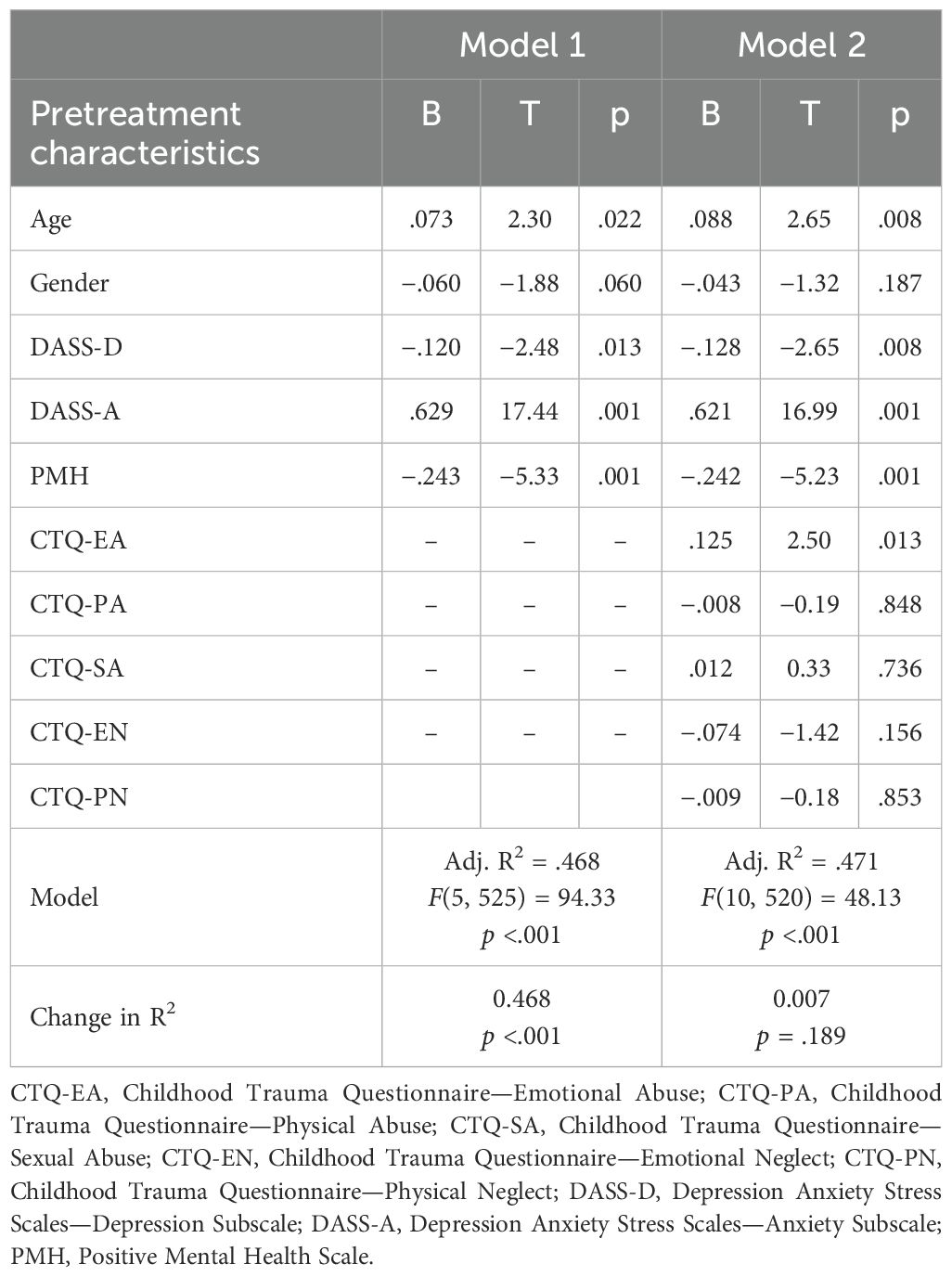
Table 5. Prediction of posttreatment anxiety by pretreatment symptomatology, positive mental health, and traumatic childhood experiences (n = 531).
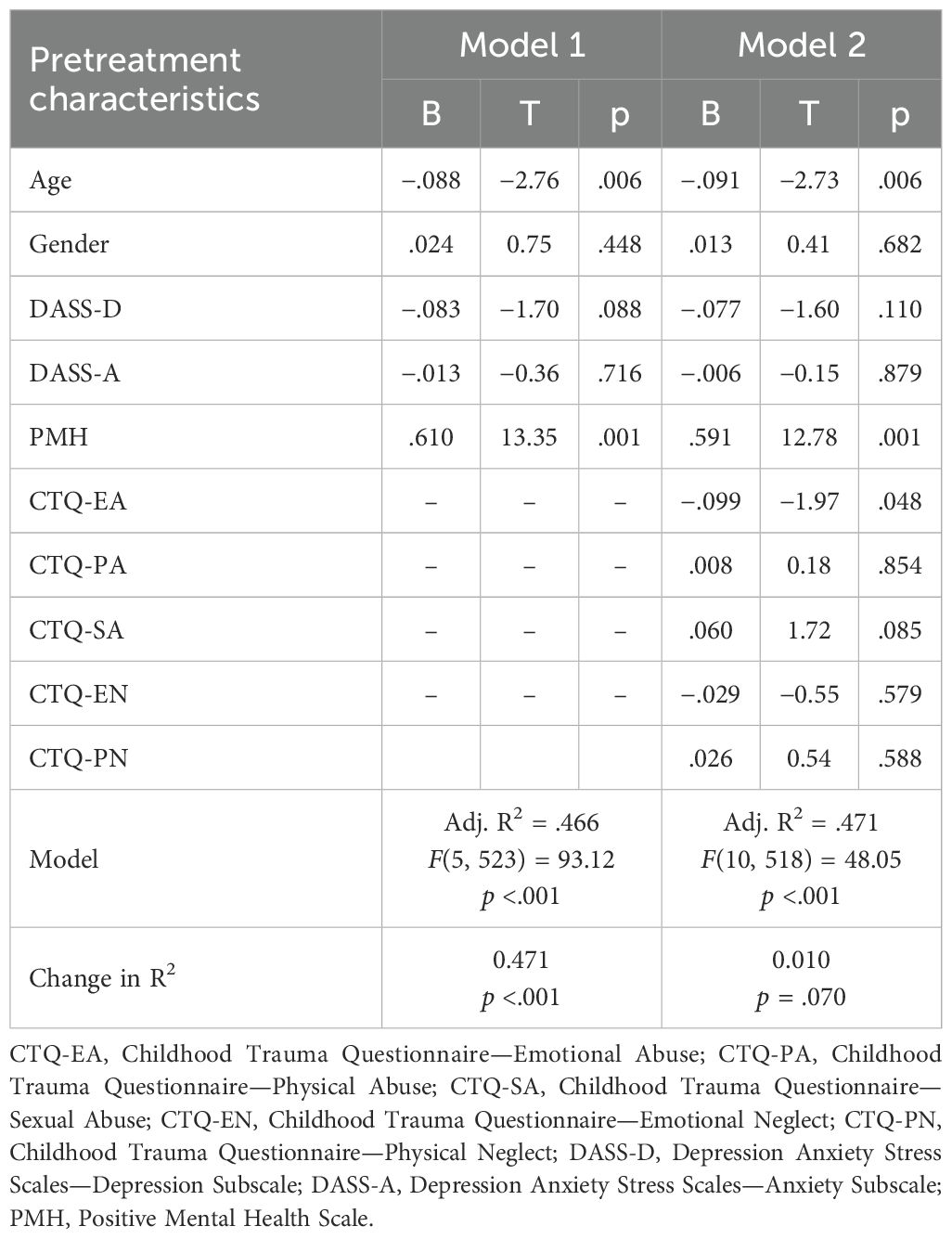
Table 6. Prediction of posttreatment positive mental health by pretreatment symptomatology, positive mental health, and traumatic childhood experiences (n = 529).
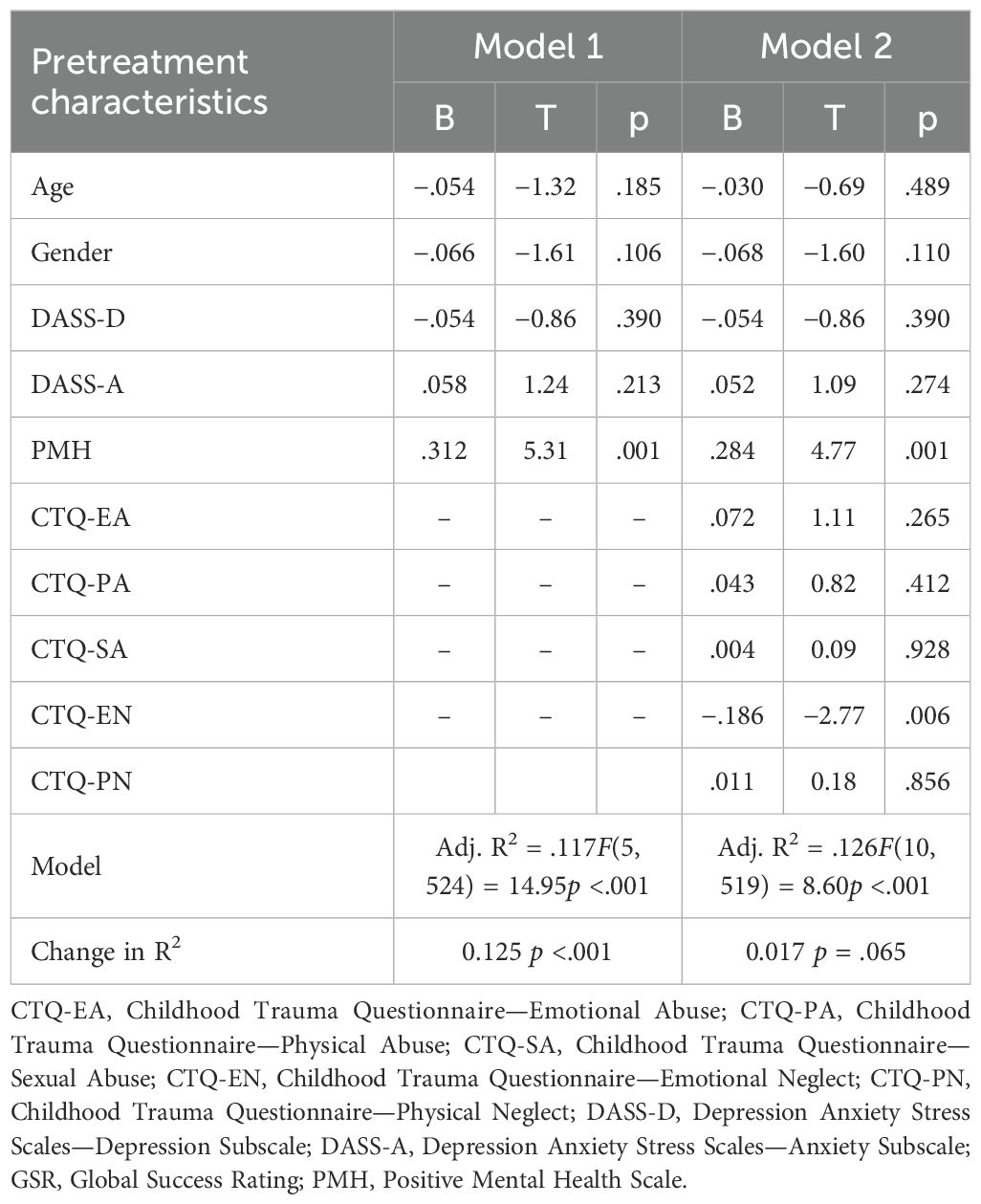
Table 7. Prediction of Global Success by symptomatology, positive mental health, and traumatic childhood experiences (n = 530).
In a series of exploratory analysis, it could be shown that all result patterns remain the same when entering Posttraumatic Stress Disorder (PTSD) diagnosis (yes/no) as a further predictor variable.
In line with previous studies (5, 6), the present study found a high burden of childhood maltreatment, particularly emotional abuse and neglect (7), in outpatient psychotherapy patients. Some form of maltreatment was reported by 57.6% of the study sample. Out of the participants with childhood maltreatment, the majority scored in the mild childhood trauma index range (31.9% to 79.2%), yet 5.2% to 19.5% scored in the extreme range. Women were more affected than men (9), and in the context of social phobias and unipolar depression, particularly close links were found with childhood neglect (21). Furthermore, the study results complement previous studies showing an association between childhood maltreatment and symptom severity (5, 6) as well as reduced optimism (21). In this sense, the present study found that individuals who reported any type of childhood maltreatment at baseline, except for sexual abuse, suffered from higher levels of depression and anxiety severity as well as reduced positive mental health. The results underscore the corrosive effect of childhood maltreatment. The finding on sexual abuse may be related to the fact that such experiences were rather seldom in the present study sample.
In terms of treatment response, self-reported emotional abuse was predictive of increased posttreatment depression, anxiety, and reduced positive mental health. Emotional neglect was predictive of lower patient-reported global treatment success. The influence of childhood maltreatment on treatment outcome is small in size (9); however, all associations were shown when age, gender, pretreatment depression, anxiety, and positive mental health were controlled for. With regard to routine short-term psychotherapeutic care, it was thus shown—as in other studies (6, 10)—that childhood maltreatment is associated with a lower response to psychotherapy. The corresponding effect was shown in relation to a sample of patients suffering from a variety of diagnoses and receiving short-term cognitive behavioral therapy in a routine care context. Of note, the effect was only found for forms of emotional abuse or emotional neglect, whereas no corresponding effects were shown for sexual abuse or physical abuse/neglect. This finding is consistent with earlier study findings, showing that from all types of childhood maltreatment, emotional abuse and/or emotional neglect seemed to show the most profound effect on personality characteristics, negative cognition, stress system dysregulation, and poorer lifestyle (7). It has been speculated that “the explanations for the particularly strong link between emotional maltreatment and negative cognitions is that in the case of emotional abuse or emotional neglect, negative self-associations are explicitly handed to the child by the parent (e.g., “you are worthless”)” (7). However, it might be necessary to further differentiate between emotional neglect and emotional abuse (22): emotional neglect is characterized by deprivation in attachment, emotional validation, and interpersonal stimulation, whereas emotional abuse is characterized by threat to one’s personal integrity. It has been shown that deprivation is, for example, associated with diminished verbal fluency (23) as well as anhedonia (24), whereas threat is, for example, associated with avoidance (25). Against this background, it might be speculated that experiences with deprivation and threat affect the therapeutic process and therapy response in different ways. In line with this, emotional neglect and emotional abuse are predictive of different types of therapy outcome in the current study. However, no far-reaching conclusions should be drawn until this pattern of findings has been replicated. However, a closer examination of the underlying mechanisms by which different types of childhood maltreatment affect the treatment process is urgently needed. Interestingly—and as a secondary finding—positive mental health, as measured by the PMH scale (15), was found to be predictive of every single treatment outcome measure assessed in this study. This is consistent with previous studies in which PMH was found to be a predictor of treatment outcome after exposure therapy (26–28) and points to the considerable importance of resilience factors, such as positive mental health, in overcoming psychological distress.
From a clinical–therapeutic perspective, the results point to the need for therapists to always assess whether and to what extent childhood maltreatment is reported. In routine practice, the Childhood Trauma Screener (29)—a short form of the CTQ with five items—might be used to inform case conceptualization and instigate further assessment of childhood maltreatment in the early phase of therapy. Particular attention should be paid here to emotional abuse/neglect, i.e., forms of maltreatment that may be less obvious and therefore—unlike serious sexual or physical abuse—potentially less clearly represent the focus of complaints. Exposure to childhood maltreatment—especially emotional abuse/neglect—may alter basic cognitive assumptions about the self and others, which over time may become ingrained in an individual’s personality (7). This stronger internalization of negative self-assumptions may require adapted therapy methods (e.g., emotion-focused/experiential interventions, autobiography-oriented interventions, more repetition), which should be taken into account when planning treatment. In contrast to traumatization that manifests itself in Posttraumatic Stress Disorder, however, there are fewer clear treatment recommendations for the more subtle forms of maltreatment. More research is needed here. In this context, it would also be important to investigate whether patients with childhood maltreatment actually need adapted interventions or simply more therapy sessions.
There are several limitations relevant to the current study. First, it is important to be aware that the CTQ is a retrospective self-report measure of childhood maltreatment. This, as well as the fact that the use of different cut-off scores is associated with different maltreatment prevalence rates (30), underscores the need to regard reported maltreatment rates as approximate values. Second, the CTQ does not allow to assess the age at which maltreatment was experienced. It was therefore impossible to investigate whether maltreatment during specific time windows exerts a particularly negative influence (31). Third, only main effects of the different maltreatment types were considered in the present study. Since maltreatment types are highly interrelated and frequently occur together (32), it would be important in future studies to also investigate cumulative effects of different maltreatment types on treatment response. Fourth, only comparatively few different disorder diagnoses could be considered separately in the present study. It therefore remains unclear to what extent the findings found here can be generalized to patients suffering from other disorders. This is truer since assignment to a diagnostic group (yes/no) was based on the primary diagnosis in the current study and did not take comorbidities into account. In future studies on larger samples, it would be interesting to not only investigate a more diverse range of disorders but also investigate specific combinations of comorbid disorders. Fifth, due to a technical error—as already mentioned—no prevalence data on the frequency of sexual abuse could be provided. Nevertheless, sexual abuse experiences could still be taken into account in the majority of the analyses conducted. Finally, a specific form of operationalizing treatment outcome was used in the present regression analyses (33). In other studies, treatment outcome has been operationalized differently: some studies focus on response and/or remission rates (6, 9, 10), whereas other studies focus on standardized mean differences (34). All of these approaches may be justified, but it is important to have a close look at the operationalization of treatment outcomes when considering different studies together, especially as this may have an impact on the results (3, 9).
In sum, the current study highlights the importance of taking experiences with childhood maltreatment into account in psychotherapeutic routine care: Childhood maltreatment is very prevalent and associated with symptom severity as well as reduced treatment response in short-term psychotherapy. Emotional abuse and emotional neglect exert an especially pernicious influence; particular attention must therefore be paid to these respective childhood experiences, as they can easily go unnoticed in the early phases of psychotherapy.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of the Faculty of Psychology, Ruhr-Universität Bochum, Germany (318/2016). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
TT: Conceptualization, Writing – original draft, Writing – review & editing. KH: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. SF: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. JM: Resources, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
We acknowledge support by the Open Access Publication Funds of the Ruhr-Universität Bochum.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Jaffee SR. Child maltreatment and risk for psychopathology in childhood and adulthood. Annu Rev Clin Psychol. (2017) 13:525–51. doi: 10.1146/annurev-clinpsy-032816-045005
2. World Health Organization (WHO). Report on the consultation of child abuse prevention. Geneva: WHO (1999).
3. CTMSG, Childhood Trauma Meta-Analysis Study Group. Treatment efficacy and effectiveness in adults with major depressive disorder and childhood trauma history: A systematic review and meta-analysis. Lancet Psychiatry. (2022) 9:860–73. doi: 10.1016/S2215-0366(22)00227-9
4. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: Increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiat. (2020) 177:20–36. doi: 10.1176/appi.ajp.2019.19010020
5. Kuzminskaite E, Vinkers CH, Milaneschi Y, Giltay EJ, Penninx BWJH. Childhood trauma and its impact on depressive and anxiety symptomatology in adulthood: A 6-year longitudinal study. J Affect Disord. (2022) 312:322–30. doi: 10.1016/j.jad.2022.06.057
6. Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: Meta-analysis. Br J Psychiat. (2017) 210:96–104. doi: 10.1192/bjp.bp.115.180752
7. Kuzminskaite E, Penninx BWJH, van Harmelen AL, Elzinga BM, Hovens JGFM, Vinkers C. Childhood trauma in adult depressive and anxiety disorders: An integrated review on psychological and biological mechanisms in the NESDA cohort. J Affect Disord. (2021) 283:179–91. doi: 10.1016/j.jad.2021.01.054
8. Moody G, Cannings-John R, Hood K, Kemp A, Robling M. Establishing the international prevalence of self-reported child maltreatment: A systematic review by maltreatment type and gender. BMC Pub Health. (2018) 18:1164. doi: 10.1186/s12889-018-6044-y
9. Spitzer C, Masuhr O, Jaeger U, Euler S. Kindheitstraumatisierungen und Behandlungsergebnis nach stationärer Psychotherapie. Psychotherapeut. (2019) 64:281–8. doi: 10.1007/s00278-019-0360-2
10. Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiat. (2012) 169:141–51. doi: 10.1176/appi.ajp.2011.11020335
11. Klinitzke G, Romppel M, Häuser W, Brähler E, Glaesmer H. The German version of the Childhood Trauma Questionnaire (CTQ)—Psychometric characteristics in a representative sample of the general population. PPmP. (2012) 62:47–51. doi: 10.1055/s-0031-1295495
12. Walker EA, Gelfand A, Katon WJ, Koss MP, Von Korff M, Bernstein D, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. (1999) 107:332–9. doi: 10.1016/s0002-9343(99)00235-1
13. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/s0145-2134(02)00541-0
14. Lovibond PF, Lovibond SH. Manual for the Depression Anxiety Stress Scales. 2nd ed. Book, Sydney: Psychology Foundation (1995).
15. Scholten S, Velten J, Bieda A, Zhang XC, Margraf J. Testing measurement invariance of the Depression, Anxiety, and Stress Scales (DASS-21) across four countries. Psychol Assess. (2017) 29:1376–90. doi: 10.1037/pas0000440
16. Lukat J, Margraf J, Lutz R, van der Veld WM, Becker ES. Psychometric properties of the positive mental health scale (PMH-scale). BMC Psychol. (2016) 4:8. doi: 10.1186/s40359-016-0111-x
17. Michalak J, Kosfelder J, Meyer F, Schulte D. Messung des Therapieerfolgs: Veränderungsmaße oder retrospektive Erfolgsbeurteilung [Measuring therapy outcome–pre-post effect sizes and retrospective measurement. Z Klin Psych Psychoth. (2003) 32:94–103. doi: 10.1026/1616-3443.32.2.94
18. Von Brachel R, Hirschfeld G, Berner A, Willutzki U, Teismann T, Cwik JC, et al. Long-term effectiveness of Cognitive Behavioral Therapy in routine outpatient care: A 5- to 20-year follow-up study. Psychother Psychosom. (2019) 88:225–35. doi: 10.1159/000500188
19. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Lawrence Erlbaum Associates (1988).
20. Urban D, Mayerl J. Regressionsanalyse: Theorie, Technik und Anwendung. New York: VS Verlag für Sozialwissenschaften (2006).
21. Spinhoven P, Elzinga BM, Hovens JG, Roelofs K, Zitman FG, van Oppen P, et al. The specificity of childhood adversities and negative life events across the life span to anxiety and depressive disorders. J Affect Disord. (2010) 126:103–12. doi: 10.1016/j.jad.2010.02.132
22. McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. (2014) 47:578–91. doi: 10.1016/j.neubiorev.2014.10.012
23. Miller AB, Sheridan MA, Hanson JL, McLaughlin KA, Bates JE, Lansford JE, et al. Dimensions of deprivation and threat, psychopathology, and potential mediators: A multi-year longitudinal analysis. J Abnorm Psychol. (2018) 127:160–70. doi: 10.1037/abn0000331
24. Wang X, Lu J, Liu Q, Yu Q, Fan J, Gao F, et al. Childhood experiences of threat and deprivation predict distinct depressive symptoms: A parallel latent growth curve model. J Affect Disord. (2022) 319:244–51. doi: 10.1016/j.jad.2022.09.061
25. Milojevich HM, Norwalk KE, Sheridan MA. Deprivation and threat, emotion dysregulation, and psychopathology: Concurrent and longitudinal associations. Dev Psychopathol. (2019) 31:847–57. doi: 10.1017/S0954579419000294
26. Teismann T, Brailovskaia J, Totzeck C, Wannemüller A, Margraf J. Predictors of remission from panic disorder, agoraphobia and specific phobia in outpatients receiving exposure therapy: The importance of positive mental health. Behav Res Ther. (2018) 108:40–4. doi: 10.1016/j.brat.2018.06.006
27. Wannemüller A, Gruszka P, Chwalek S, Fröhlich S, Mulders M, Schaumburg S, et al. Large-group one-session treatment: feasibility in highly height fearful individuals and predictors of outcome. Front Psychol. (2019) 10:2411. doi: 10.3389/fpsyg.2019.02411
28. Margraf J, Teismann T, Brailovskaia J. Predictive power of positive mental health: a scoping review. J Happiness Stud. (2024) 25:81. doi: 10.1007/s10902-024-00788-x
29. Grabe HJ, Schulz A, Schmidt CO, Appel K, Driessen M, Wingenfeld K, et al. A brief instrument for the assessment of childhood abuse and neglect: the Childhood Trauma Screener (CTS). Psychiatr Prax. (2012) 39:109–15. doi: 10.1055/s-0031-1298984
30. Weitkämper A, Kellner M, Iffland JR, Driessen M, Kley H, Neuner F, et al. Childhood maltreatment in individuals with Schizophrenia Spectrum Disorders: The impact of cut-off scores on prevalence rates. Front Psychiatry. (2021) 12:692492. doi: 10.3389/fpsyt.2021.692492
31. Schalinski I, Teicher MH, Nischk D, Hinderer E, Müller O, Rockstroh B. Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative and depressive symptoms in adult inpatients. BMC Psychiatry. (2016) 16:295. doi: 10.1186/s12888-016-1004-5
32. Cecil CA, Viding E, Fearon P, Glaser D, McCrory EJ. Disentangling the mental health impact of childhood abuse and neglect. Child Abuse Negl. (2017) 63:106–19. doi: 10.1016/j.chiabu.2016.11.024
33. Alden LE, Taylor CT, Laposa JM, Mellings TMB. Impact of social developmental experiences on cognitive-behavioral therapy for generalized social phobia. J Cog Psychother. (2006) 20:7–16. doi: 10.1891/jcop.20.1.7
Keywords: childhood maltreatment, emotional abuse, emotional neglect, psychotherapy, cognitive behavior therapy
Citation: Teismann T, Hahlweg K, Friedrich S and Margraf J (2025) Childhood abuse and neglect in routine care psychotherapy patients. Front. Psychiatry 16:1566560. doi: 10.3389/fpsyt.2025.1566560
Received: 25 January 2025; Accepted: 24 March 2025;
Published: 17 April 2025.
Edited by:
Andreas Dinkel, Technical University of Munich, GermanyReviewed by:
Frank Neuner, Bielefeld University, GermanyCopyright © 2025 Teismann, Hahlweg, Friedrich and Margraf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tobias Teismann, dG9iaWFzLnRlaXNtYW5uQHJ1Yi5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.