- 1Family Medicine Department, Faculty of Medicine, Dicle University, Diyarbakir, Türkiye
- 2Psychiatry Department, Faculty of Medicine, Dicle University, Diyarbakir, Türkiye
Background/Objectives: Patients with psychiatric disorders have high mortality and morbidity rates from infectious diseases, but low vaccination rates compared to the normal population. This study aimed to evaluate the vaccination rates for influenza, pneumococcal, and COVID-19 vaccines, and the levels of vaccine hesitancy among individuals with psychiatric disorders.
Methods: The study was a cross-sectional study among patients with psychiatric disorders. Participants’ vaccination statuses for influenza, pneumococcal, and COVID-19 vaccines during the pandemic were assessed, along with their vaccine hesitancy levels using a vaccine hesitancy scale. Data were collected between 01.03.2024 and 27.11.2024.
Results: The study included 500 patients diagnosed with psychiatric disorders. Only 3.6% of the participants had received the influenza vaccine in the previous year, 3.0% reported regular influenza vaccinations, and 76.2% had received the COVID-19 vaccine during the pandemic. Among the participants at risk for pneumococcal infection (14%), the vaccination rate was only 2%. Patients with attention deficit hyperactivity disorder (ADHD) (45.0%) and anxiety disorder (17.2%) had the highest rates of regular influenza vaccination, while those with psychosis (13.6%) and depression (14.6%) had the lowest (p=0.010). COVID-19 vaccination rates during the pandemic were highest in ADHD (90.0%), bipolar disorder (81.1%), and depression (80.8%), and lowest in psychosis (54.5%) and obsessive-compulsive disorder (64.3%)(p=0.002). Women (p=0.001), participants with below university education levels (p=0.009), and patients with psychosis showed greater vaccine hesitancy. Patients with ADHD and bipolar disorder had the most positive attitudes toward vaccination (p=0.021). Positive attitudes were also linked to recent or regular influenza vaccinations and COVID-19 or pneumococcal vaccinations (p<0.05).
Conclusions: Low vaccination rates and high vaccine hesitancy in psychiatric patients, particularly those with psychosis, necessitate targeted strategies to improve immunization coverage in this population.
Introduction
Psychiatric disorders are important public health problems and are also common in society. In a global meta-analysis, it was reported that 29.2% of the global population experienced a mental disorder at least once in their lifetime, and 17.6% met the diagnostic criteria for a disease (1).
Due to their physical and mental health, individuals with psychiatric disorders are more susceptible to diseases (2–5). When all causes of death are taken into account, mortality rates were significantly higher in patients with psychiatric disorders compared to the control group, while the median years of potential life lost was 10 years (6). Inequalities in their use of and access to health services (7), their lower utilization of primary care services (8), and their lower utilization of preventive healthcare compared to patients without a psychiatric diagnosis (9) may render them more susceptible to diseases. While increased stress has been generally associated with a tendency to increased risk of infection and symptomatic illness (10), in addition to the presence of chronic stress in these individuals, genetic components in susceptibility to infection are mentioned, and it has been shown that the occurrence of infections in individuals with mental illness may be partially genetically directed (5).
Individuals with psychiatric disorders are at risk for infectious diseases (2–6, 11). It has been reported that the risk of dying from infections is 2.71 times higher and the risk of dying from respiratory tract infections is 3.27 times higher in people with serious mental illness (11). Furthermore, obesity, type 2 diabetes, cardiovascular diseases, and respiratory tract diseases, which are more prevalent in patients with severe psychiatric disorders compared to the general population, have the potential to exacerbate the outcomes of respiratory tract infections (7, 12). Seminog defined severe mental illness as a risk factor for pneumococcal diseases, lobar pneumonia, pneumococcal pneumonia, pneumococcal septicemia, and meningitis (2). In the Nilsson study, it was shown that influenza/pneumonia and sepsis-related mortality rates and hospitalizations were higher in patients with psychiatric diagnoses (3). In a cohort study conducted in the USA, it was reported that persons with serious mental illness were more likely to be hospitalized or to die after a coronavirus disease-2019 (COVID-19) diagnosis compared with persons without serious mental illness (13). In a cohort study evaluating COVID-19 infection and mortality in patients with psychiatric diagnoses, it was reported that schizophrenia patients had approximately 4 times, those with mood disorders 2.76 times, and those with anxiety disorders 2.39 times higher mortality rates than the reference group (4). In a systematic review and meta-analysis, it was mentioned that individuals with schizophrenia had a sevenfold significantly higher mortality rate from pneumonia than the general population (14) and in another, those with bipolar disorder had a 3.18 times higher mortality risk due to respiratory system infections (15).
Vaccines are one of the most effective tools in the fight against infectious diseases (16). Despite the evidence of the efficacy and safety of vaccines, vaccine hesitancy is recognized by the WHO as one of the 10 greatest global threats (17). Vaccine hesitancy in patients with mental illness can jeopardize vaccine uptake, which can pose a critical public health problem. Studies show that vaccination rates are lower in this patient group (18–24). In Lorenz’s study, influenza vaccination rates in patients with psychiatric diagnoses were reported to be lower than in the general population (19). Influenza vaccination uptake among target groups in Spain was below desirable levels and has not improved significantly (20).
During the COVID-19 pandemic, research suggested that individuals with psychiatric disorders had lower vaccination rates compared to the general population (21, 22, 24). In a retrospective cohort study evaluating data from 23.4 million adults in the UK, it was found that those with mental illness were alarmingly less vaccinated against COVID-19 compared to those with other chronic diseases (23). In a study evaluating COVID-19 vaccination rates in patients with severe mental illness during the pandemic in Turkey, it was reported that vaccination rates were lower than in the general population (24). During the pandemic period, it was shown that hospitalization rates increased in schizophrenia patients as the pandemic progressed and survival rates decreased (25). During the COVID-19 pandemic, it was recommended that people with severe mental illness be prioritized as a vulnerable group for COVID-19 vaccination due to increased mortality and morbidity rates due to COVID-19 and accompanying aggravating factors, and in some countries, this patient group was prioritized for vaccination (26–28). It is recommended that people with severe mental illness should be routinely vaccinated with pneumococcal and influenza vaccines and prioritized for vaccination (2, 3, 11).
Individuals with psychiatric diagnoses may experience vaccine hesitancy, which can become more complex due to additional complicating factors such as their perceptions of their current diagnosis. In a US study investigating associations between psychiatric morbidity and COVID-19 vaccine hesitancy, vaccine hesitancy was more prevalent across all psychiatric comorbidities (22). Patients with schizophrenia, in particular, tend to be less vaccinated (21, 25) and characteristics such as age and education can be risk factors for vaccination hesitation (29). In a study conducted in Turkey, it was determined that having schizophrenia increased the risk of non-vaccination 2.7 times (30). In a study conducted in Japan, it was shown that individuals with moderately severe or severe levels of depression were more ambivalent about COVID-19 vaccination (31). In the USA, it was found that adults with anxiety and depression were less vaccinated compared to those without anxiety and depression and had more concerns about the efficacy of vaccines, side effects, and trust in the government (32).
In this study, we aimed to reveal influenza, pneumococcal, and COVID-19 vaccination rates, vaccine hesitancy, and related factors in adult individuals with psychiatric disorders. Revealing the vaccination rates, characteristics of vaccine hesitancy, and related factors in this patient group will contribute to the development of effective interventions at both individual and social levels and allow for the development of coping strategies against infectious diseases for individuals with psychiatric disorders, who can be considered an at-risk group for infectious diseases.
Materials and methods
This study was designed as a cross-sectional analytical study, and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were utilized in the preparation of the study (33). Ethics committee approval was obtained for the study (date: 14.02.2024 no: 114) The study was conducted in accordance with the Declaration of Helsinki.
Within the scope of the study, patients who were diagnosed with psychiatric disorders by a psychiatrist who attended the Dicle University Faculty of Medicine Hospital Mental Health Diseases and Family Medicine outpatient clinics, which are the two outpatient clinics most frequently visited by patients with psychiatric diagnosis, were invited to participate in the study. The number of people to be included in the study was calculated with the sample size calculator. By taking a medium effect size (0.5) p ≤ 0.05 and the pairwise hypothesis of 0.95 (95%) power at a 95% confidence interval into account, the minimum sample size was determined to be 373 people. Data were collected between 01.03.2024 and 27.11.2024. The minimum number of participants for the study was 373, but the study was terminated when the number of participants was reached to allow the analysis to be carried out among the sub-diagnoses, and therefore the total number of participants was 500. In addition, psychiatric patients repeatedly attended the outpatient clinic due to their treatment, and the study was terminated before the planned time to prevent repeated study participation of the same participants.
A face-to-face questionnaire was used for data collection, and written informed consent was obtained from the participants. The inclusion criteria included volunteering to participate in the study, being over 18 years of age, and having a psychiatric diagnosis. Patients diagnosed with schizophrenia and other psychotic disorders, bipolar disorder and related disorders, depression, anxiety disorders, obsessive-compulsive personality disorders (OCD), and attention deficit hyperactivity disorder (ADHD) were included in the study.
Variables
Participants’ sociodemographic characteristics (age, sex, educational status, marital status, and number of children), psychiatric diagnoses, chronic diseases, care status, and adult vaccination characteristics (influenza, COVID-19, and pneumococcal) were questioned and recorded. The Vaccine Hesitancy Scale was used as a scale. The Vaccine Hesitancy Scale is a valid and reliable scale consisting of nine items, the validity and reliability of which were established by Luyten et al. (34) and adapted into Turkish by Yılmaz et al. (35). The scale features a 5-point Likert-type response system, ranging from strongly disagree to strongly agree. The total score on the scale ranges from 9–45 points. The higher the score obtained from the scale, the lower the vaccine hesitation.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS), version 27.0 for Windows (SPSS Inc., Chicago, USA), a computer package program, was used for statistical analysis of the research data. As descriptive statistics, categorical variables were presented as numbers and percentages, and continuous variables were presented as mean ± standard deviation (minimum–maximum value) and median (IQR) according to distribution characteristics. Histogram and skewness-kurtosis were used to determine whether the data fit the normal distribution. In the comparison of two independent groups, the independent groups t-test or Mann-Whitney U test was used, and one-way analysis of variance (ANOVA) was used for more than two groups. The homogeneity of the variance in multiple groups was checked with Levene’s test, and since the variance was found to be homogeneous, Tukey’s post hoc test was used to determine which group was the source of the significance. The relationship between continuous data was evaluated by Pearson correlation analysis. Chi-square analysis was used to determine whether there was a statistical difference between two qualitative variables. Bonferroni-corrected post hoc analysis was used to determine which category was the source of significance in categorical data with more than two groups between which significance was found. The reliability (Cronbach α) coefficient of the scale for this sample was also calculated. The Cronbach α value of the scale was found to be 0.871 in our study. Hypotheses were two-way, and p<0.05 was considered statistically significant.
Results
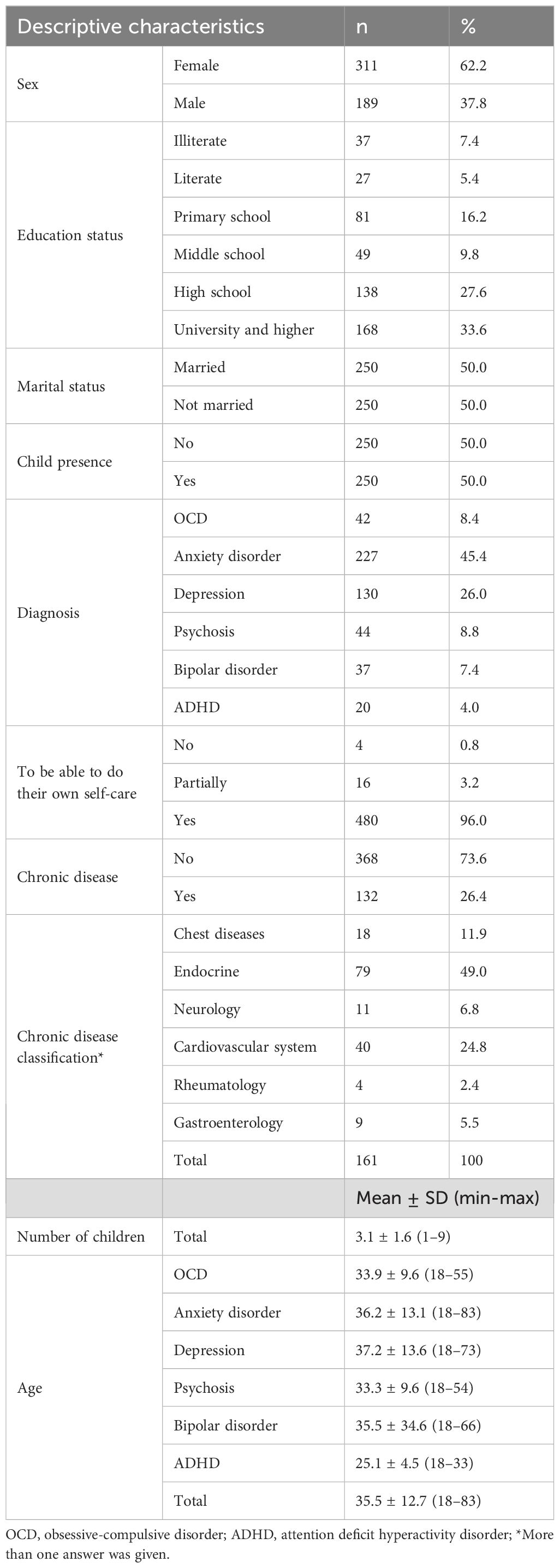
A total of 500 patients with psychiatric diagnoses participated in the study, and 62.2% of the participants were female, 50.0% were married, 50.0% had children, and 61.2% had a high school education level or higher (Table 1). Most of the participants were diagnosed with anxiety disorder, with 45.4% (n=227), and depression with 26.0% (n=130). These diagnoses were followed by psychosis (8.8%), OCD (8.4%), bipolar disorder (7.4%), and ADHD (4%). The mean age of all participants was 35.5 years, with the lowest mean age in patients with ADHD (25.1) and the highest mean age in patients with anxiety disorder (36.2). Furthermore, 96% of the participants stated that they were able to perform their own self-care. Of the participants, 132 (26.4%) stated that they had a chronic disease, and 127 (25.4%) stated the type of chronic disease. Among those with chronic diseases, 49% (n=79) had endocrine diseases, 24.8% (n=40) had cardiovascular diseases, 11.1% (n=18) had thoracic diseases, 6.8% (n=11) had neurological diseases, 5.5% (n=9) had gastroenterology, and 2.4% (n=4) had rheumatologic diseases.
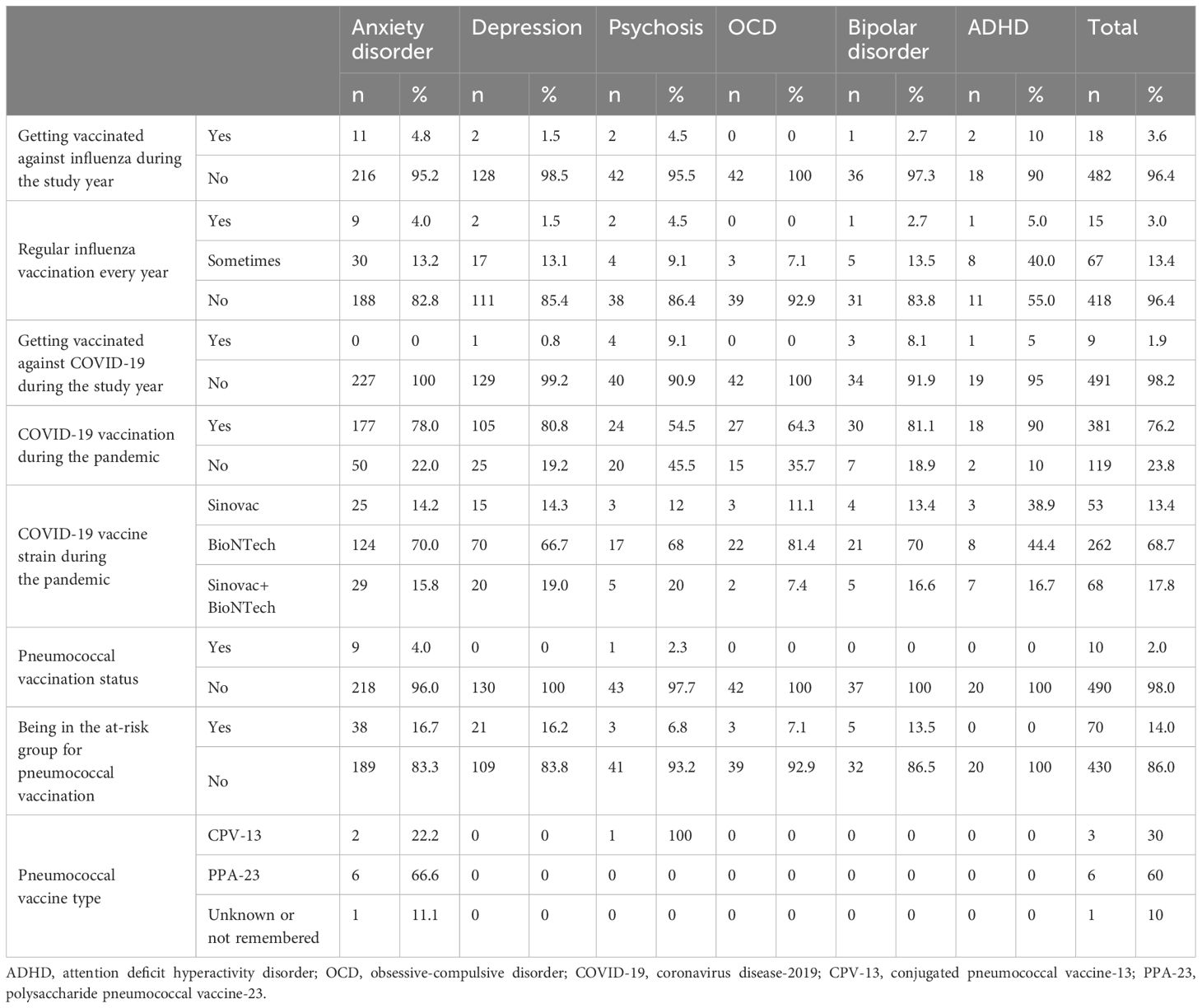
When we examined the vaccination status of all participants, only 3.6% (n=18) stated that they had received the influenza vaccine during the study year, while 3.0% (n=15) stated that they had received a regular influenza vaccine every year (Table 2). While 76.2% (n=381) had received the COVID-19 vaccine during the pandemic, the most common vaccine was the BioNTech vaccine, with 68.7% (n=262), and only 1.9% (n=9) had received the COVID-19 vaccine during the study year. While 14% (n=70) of all participants were in the at-risk group for the pneumococcal vaccine, the rate of pneumococcal vaccination was only 2%.
When the vaccination status was evaluated according to the diagnoses, it was found that 10% of those diagnosed with ADHD, 4.8% of those diagnosed with anxiety disorder (n=11), and 4.5% of those with psychosis (n=2) had received the influenza vaccine this year; these rates were 1.5% (n=2) for depression and 2.7% (n=1) for bipolar disorder, and those diagnosed with OCD did not receive any influenza vaccine during the study year. While 55% of those diagnosed with ADHD stated that they had received a regular influenza vaccination every year, 92.9% of those diagnosed with OCD and 86.4% of those with psychosis stated that they did not receive a regular influenza vaccination. During the pandemic, 90% (n=18) of those diagnosed with ADHD, 80.8% (n=105) of those diagnosed with depression, and 81.1% (n=30) of those diagnosed with bipolar disorder stated that they had received the COVID-19 vaccine. Patients diagnosed with psychosis (54.5% (n=24)) and OCD (64.3% (n=27)) were the least likely to have received the COVID-19 vaccine during the pandemic. While the rate of being in the risk group for pneumococcal vaccination was between 7.1% and 16.7% among the diagnostic groups (except for those with ADHD with 0%), the pneumococcal vaccination rates were 4.0% (n=9) for anxiety disorder and 2.3% (n=1) for patients diagnosed with psychosis, and no patients in the other diagnostic groups were vaccinated with the pneumococcal vaccine. The most commonly administered pneumococcal vaccine was the polysaccharide pneumococcal vaccine 23 (PPA-23), with 60% (n=6) of all patients and 66.6% (n=6) of patients with anxiety disorder who were in the at-risk group for the pneumococcal vaccine receiving the PPA-23 pneumococcal vaccine.
The descriptive characteristics of the participants’ regular influenza vaccination status and COVID-19 vaccination status during the pandemic were compared and are shown in Table 3. It was found that there was a statistically significant difference (p=0.010) in the comparison of psychiatric diagnoses and those who received the influenza vaccine every year or sometimes compared to those who did not; the psychiatric diagnosis group that received the influenza vaccine the most was the patient group with ADHD (45.0%) and then the patient group with anxiety (17.2%), while the patients diagnosed with psychosis (13.6%) and depression (14.6%) received the least. The Bonferroni correction showed that the difference was due to the difference between participants with ADHD and other diagnostic groups. Since the number of people who received influenza vaccination and COVID-19 vaccination this year fell to numbers that could not be statistically applied in subgroups, their evaluations were not included in the table.
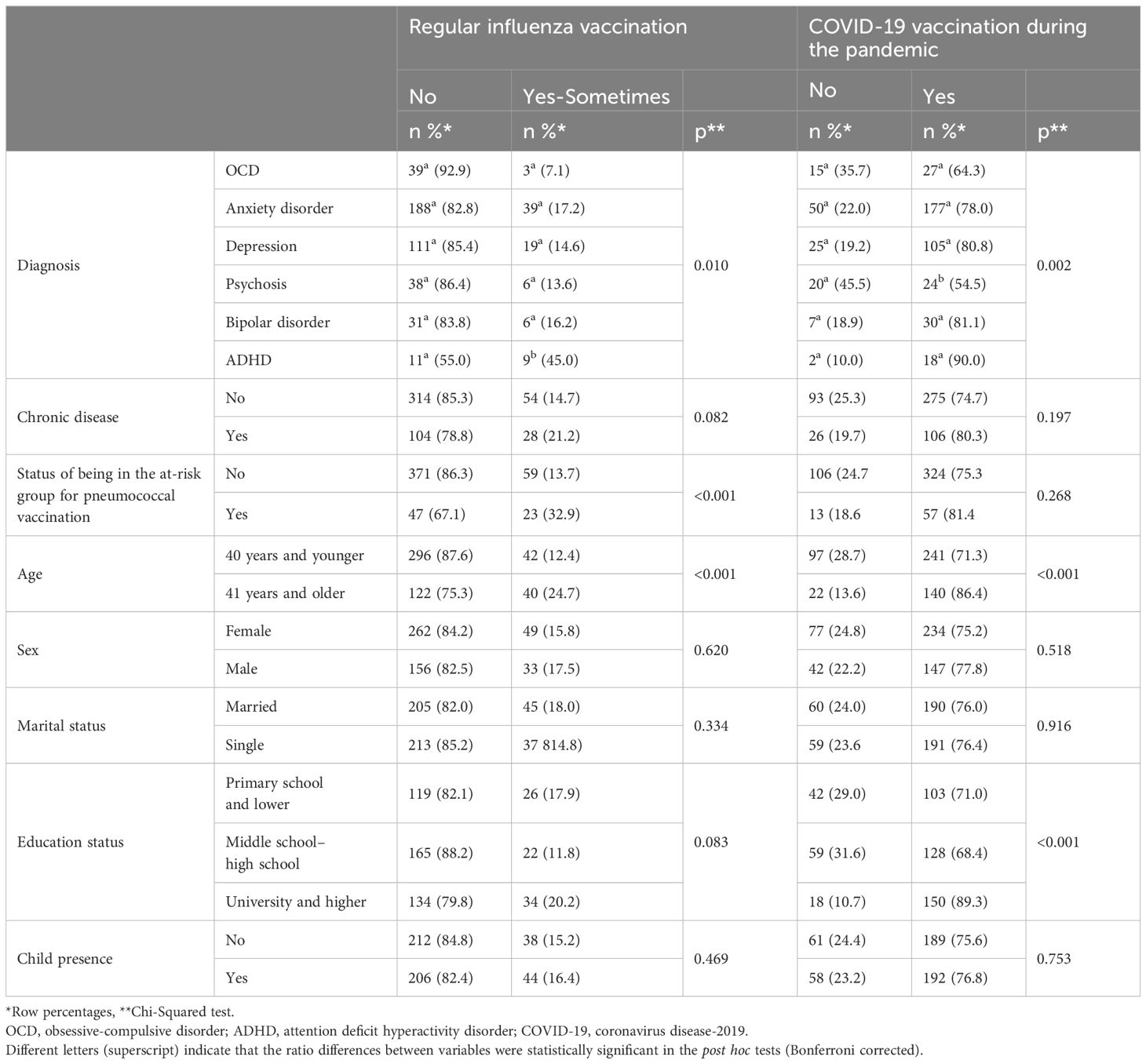
Table 3. Comparison of the descriptive characteristics of the participants and their status of receiving the influenza vaccine every year and the COVID-19 vaccine during the pandemic.
The descriptive characteristics of the participants were compared with the status of influenza vaccination every year and COVID-19 vaccination in the pandemic, and a statistically significant result was found between the diagnostic groups and the status of COVID-19 vaccination in the COVID-19 pandemic (p=0.002); the psychiatry diagnostic group that stated that they received the vaccine the most was ADHD (90.0%) and bipolar disorder (81.1%), followed by patients diagnosed with depression (80.8%). The group that received the least COVID-19 vaccinations was the group of patients with psychosis (54.5%), followed by the group of patients with OCD (64.3%), and the Bonferroni correction showed that the statistically significant difference was due to the difference between participants diagnosed with psychosis and other diagnostic groups. The rate of regular influenza vaccination among those in the at-risk group for the pneumococcal vaccine was lower (32.9%) than among those who were not (67.1%); however, the rate of regular influenza vaccination was higher among those in the at-risk group for the pneumococcal vaccine than among those not in the at-risk group (32.9% versus 13.7%), and this difference was statistically significant (p=<0.001). Among all participants, regular influenza (p<0.001) and pandemic COVID-19 vaccination rates were significantly higher in people over 40 years of age and those with a university education or higher (p<0.001).
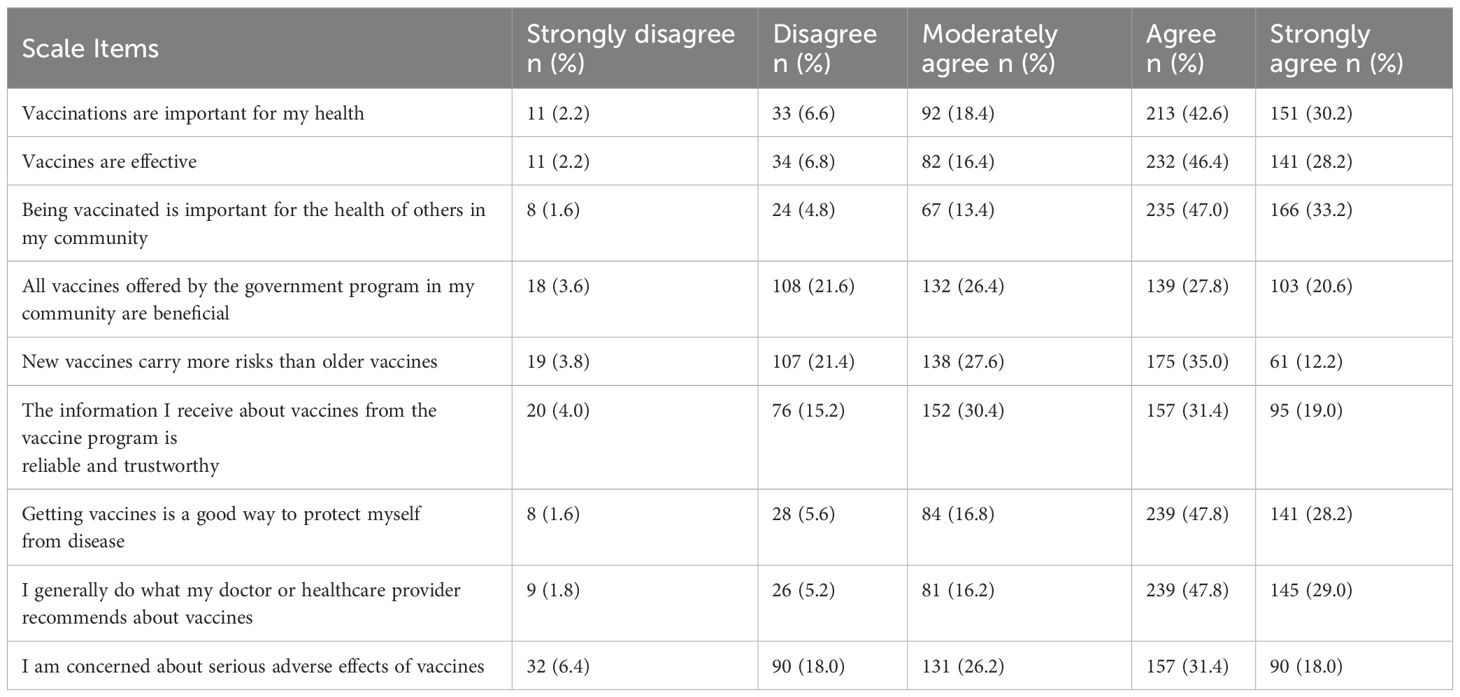
The responses of all participants to the vaccine hesitancy scale questions are presented in Table 4. In total, 91.2% (moderately agree to strongly agree) of the participants stated that vaccines are important for their health, 91.0% (moderately agree to strongly agree) stated that vaccines are effective, and 93.6% (moderately agree to strongly agree) stated that vaccination is important for the health of others in the community. Furthermore, 74.8% (moderately agree to strongly agree) of the participants agreed with the statement that all vaccines in the vaccination program offered by the government to the community are beneficial and that new vaccines carry more risk than old vaccines. It was found that 80.8% (moderately agree to strongly agree) of all the participants found the information they received about vaccines from the government’s vaccination program credible and reliable, while 75.6% were concerned about the serious side effects of vaccines. It was found that 92.8% of the participants agreed with the statement that getting vaccinated is a good way to protect themselves from disease, and 93% of the participants agreed with the statement that they usually follow the recommendations of their doctor and health institution about vaccines.
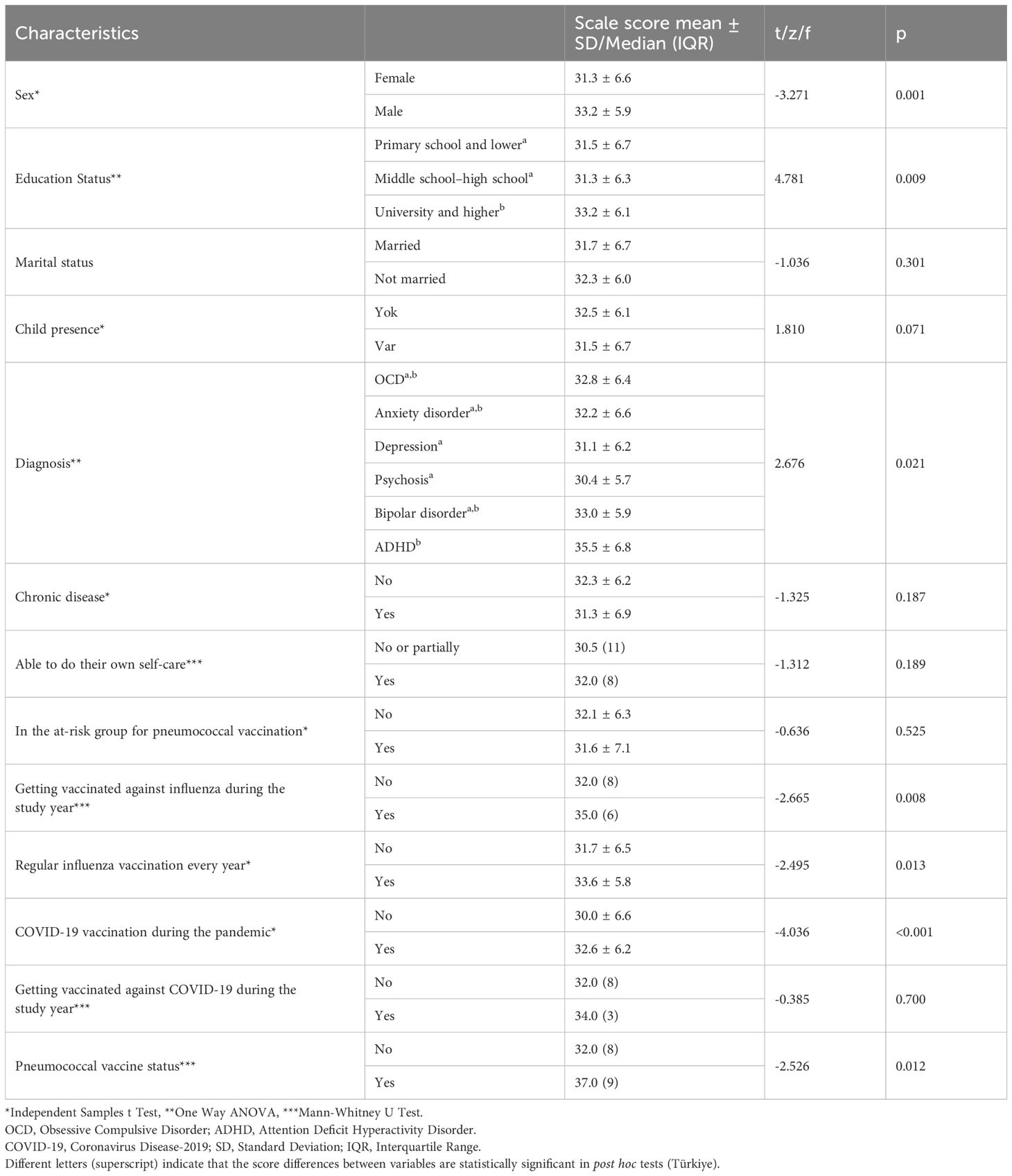
The mean total scale score of all participants was 32.0 ± 6.4 (9–45). Participants’ scores on the scale and descriptive characteristics are compared and shown in Table 5. Considering that a decrease in the score obtained on the vaccine hesitancy scale reflects an increase in hesitancy towards vaccination, it was found that the scale scores of women (p=0.001) and those with less than a university education (p=0.009) were statistically significantly lower; that is, their attitudes were more negative. When psychiatric diagnosis and scale scores were compared (p=0.021), it was observed that there was a statistically significant difference; the lowest scale scores were in the group of patients with psychosis (30.4 ± 5.7), followed by patients with depression (31.1 ± 31.1) and anxiety disorder (32.2 ± 6.6). The highest scale scores were found in patients diagnosed with ADHD (35.5 ± 6.8) and bipolar disorder (33.0 ± 5.9).
When the vaccination status of the participants was compared with their scores on the vaccine hesitancy scale (Table 5), it was found that the scale scores of those who received the influenza vaccine during the study year (p=0.008), those who stated that they received the regular influenza vaccine every year (p=0.013), those who received the COVID-19 vaccine during the pandemic (p=<0.001), and those who received the pneumococcal vaccine (p=0.012) were statistically significantly higher.
No significant correlation was found between the scale score and age (r=-0.068, p=0.128) and number of children (r=-0.017, p=0.792). In addition, those who received Sinovac and BioNTech vaccines during the pandemic were compared, and the scale score of those who received only the Sinovac vaccine was 30.79, while the scale score of those who received only the BioNTech vaccine was 33.0, and the difference was statistically significantly higher (p=0.018).
Discussion
Vaccination is one of the most important steps in the fight against infectious diseases and is of critical importance, especially for psychiatric patients who are at higher risk of infection, mortality, and morbidity. Although individuals with psychiatric disorders may be considered part of the at-risk group to be prioritized for vaccination, influenza and pneumococcal vaccination rates among these patients were found to be alarmingly low in our study. Regular influenza vaccination rates were significantly lower among patients with psychosis and depression compared to patients with other diagnoses, and COVID-19 vaccination rates were significantly lower among patients with psychosis and OCD during the pandemic. Women, participants with lower levels of education, and patients with psychosis showed more vaccine hesitancy. Positive attitudes were also associated with having recently or regularly been vaccinated against influenza and being vaccinated against COVID-19 or pneumococcal vaccine. Low vaccination rates and high vaccine hesitancy in psychiatric patients, especially those with psychosis, suggest the need for targeted strategies to improve vaccination coverage in this high-risk population.
Influenza has a negative effect on mortality and hospitalization rates in patients with psychiatric diagnoses (3); therefore, influenza vaccination is recommended in this patient group (11). Although influenza is a vaccine recommended to be administered annually, in this study, a very low rate of 3.6% of all participants stated that they received the influenza vaccine within a year, and 3.0% stated that they received the regular influenza vaccine. Low influenza vaccine coverage has also been reported in high-risk patient groups other than psychiatric disorders (20). Influenza vaccination rates have been found to be low among patients with psychiatric diagnoses in the literature; however, influenza vaccination rates were much higher in our study (19, 20, 36). In Greece, the influenza vaccination rates of patients with mental disorders between 2020 and 2022 were reported to be 43.2%, 39.8%, 40.7%, and 33.7%, respectively; the rate of those who received influenza vaccinations repeatedly over 3 years was 33.7% (36). A study conducted in the USA reported influenza vaccination rates of 28.4% and 24.2% in 2010 and 2011, respectively, lower than in the general population at that time (19). An ecological study analyzing data from 34 countries worldwide revealed an inverse correlation between influenza vaccine coverage and COVID-19 mortality (37) and recommended influenza vaccination to be administered primarily in at-risk groups during the pandemic (38). During and after the COVID-19 pandemic, there was an increase in influenza vaccination rates in adults in the general population compared to before (39). While the study in the USA was conducted before the pandemic (19), the study in Greece was conducted after the pandemic (36). Higher influenza vaccination rates after the pandemic may be associated with the impact of the pandemic; however, although our study was conducted 1 year after the official end of the pandemic (40), the fact that influenza vaccination rates were less than one-tenth of the rates reported in the Greek study is a remarkable result that is difficult to explain.
When the influenza vaccination status within 1 year was evaluated according to the diagnoses, it was found that the vaccination rates were very low in patients diagnosed with depression (1.5%), bipolar disorder (2.7%), psychosis (4.5%), and anxiety disorder (4.8%); no patient with OCD had received the influenza vaccine, and even in patients diagnosed with ADHD, the highest vaccination rate was 10%. Regular influenza vaccination rates were also significantly lower among patients with psychosis and depression compared to patients with other diagnoses. In the study conducted in Greece, higher rates were found among people with anxiety disorders (41.5%) and a depressive episode (41.1%), while the lowest rates were reported among patients with schizophrenia (26.8%), bipolar disorder (24.5%), and obsessive-compulsive disorder (22.2%) (36). Vaccination rates of patients with psychiatric diagnoses vary in the literature (41). Although respiratory tract infections have been associated with increased mortality and morbidity in patients with psychiatric diagnoses (2, 3, 11, 13), vaccination rates are generally reported to be lower in this patient group (18–24). Increased mortality rates reported, especially in patients with schizophrenia, emphasize the importance of vaccination in these patient groups (4, 13, 14). In the Lawrence study, it was reported that any mental health diagnosis increased the likelihood of influenza vaccination in the general sample, and the relationship between mental health diagnosis and the likelihood of influenza vaccination was stronger, especially in people with comorbidities (42). In Lawrence’s study, the fact that the patient group consisted of individuals over 65 years of age may be an important reason for increased influenza vaccine uptake. This age group is considered to be at risk for influenza due to their age and potential chronic diseases (43). Sociodemographic characteristics may have an impact on vaccine acceptance. Age, female sex, and some concomitant chronic diseases may increase influenza vaccine uptake. In a study conducted in Spain, while the rate of patients in the risk group defined for influenza was 19.2% above the age of 15 years, this rate increased to 54.4% above the age of 65 years and 41.6% with concomitant medical conditions (20). In this study, it was found that among all participants, the rate of regular influenza and pandemic COVID-19 vaccinations was significantly higher in people over the age of 40 and those with a university or higher education level. In a study conducted in Greece, being over 50 years of age, polypharmacy, and non-hospitalization to a psychiatry ward were positively associated with influenza vaccination (36). In addition, being 50 years of age or older and of the female sex were reported as predictor factors for CPV-13 vaccination. In Lorenz’s study, it was reported that people with education levels above high school tended to have fewer flu vaccinations because they thought that they would get the flu from more vaccines (19).
Patients with severe mental illness may be more susceptible to infectious diseases due to unhealthy lifestyle choices and medications that may accompany the associated metabolic comorbidities. Pneumococcal vaccination is recommended for individuals who are more vulnerable to pneumococcal infections, but having a psychiatric diagnosis is not included in the at-risk group (44). In a cohort study conducted by Seminog among patients with schizophrenia, bipolar disorder, depression, or anxiety, severe mental illness was considered a risk factor for pneumococcal disease, and an approximately 2.3-fold increased risk of pneumococcal disease was reported (2). It is recommended that these patient groups should be defined as a priority risk group for pneumococcal and influenza vaccination (2, 3, 11). In this study, while 14% of all participants were in the defined at-risk group for pneumococcal vaccination, the rate of pneumococcal vaccination was very low at only 2%. The most common type of pneumococcal vaccine reported to be administered was PPA-23 (60%), while the group that received the most pneumococcal vaccine was found to be patients with anxiety disorders. In a study conducted in Greece, the pneumococcal vaccination rates of patients with mental disorders were reported to be 28.8% for CPV-13 and 7.7% for PPA-23, and the highest vaccination rate was reported in patients diagnosed with depressive disorder (49.4%) (36). In our study, for pneumococcal vaccination, the rate of regular influenza vaccination was found to be lower in those in the at-risk group (32.9%) compared to those not in the at-risk group (67.1%); however, a statistically significant higher rate of regular influenza vaccination was found in those in the at-risk group for PPA-23 compared to those not in the risk group (32.9% versus 13.7%). The study in Greece reported that a person vaccinated with CPV-13 was 14 times more likely to have been vaccinated regularly against influenza within 1 year and 17.3 times more likely to have been vaccinated regularly against influenza within the last 3 years (36). In our study, the vaccination experiences of the participants were recorded by self-report, and health system records were not reviewed. The participants’ existing psychiatric diseases may have limited their recall of both vaccination status and vaccine type.
The COVID-19 pandemic caused high mortality and morbidity in patients with psychiatric disorders (4, 11, 13, 25); these patients had lower COVID-19 vaccine uptake (21–24), and due to increased poor clinical outcomes in patients with psychiatric disorders, it was recommended that these patients be prioritized during pandemic vaccinations (26–28). In our study, 76.2% of all participants reported having received a COVID-19 vaccine during the pandemic. While questioning the patients about their COVID-19 vaccination status, we did not ask about the number of vaccine doses, so the 76.2% rate corresponds to the number of people who had been vaccinated with at least one dose of any COVID-19 vaccine, and this rate was below the rate of at least one dose of vaccination (93.3%) during the pandemic period in Turkey (45). Maazerel reported that 93.0% of patients with psychiatric disorders received the COVID-19 vaccine during the pandemic, and there was no difference between psychiatric diagnoses (46). In a study conducted in Turkey, the rate of those who received at least 1 dose of vaccine was reported to be 83.7%, and no difference was reported between vaccination status and sociodemographic characteristics such as type of psychiatric diagnosis, age, and education level (24). In our study, it was found that the rate of COVID-19 vaccination during the pandemic was significantly higher in those over the age of 40 and those with a university or higher education level. A correlation was found between psychiatric diagnosis and vaccination status; the highest vaccination rate was found in the patient group diagnosed with ADHD (90.9%), followed by patients diagnosed with bipolar disorder (81.1%) and depression (80.0%); the group that stated that they were vaccinated the least were patients diagnosed with psychosis (54.5%) and OCD (64.3%). In Belgium, COVID-19 vaccination rates among patients with mental disorders were reported to be as high as in the general population (46). In a cohort study examining the electronic health records of 2.8 million people in the UK, COVID-19 vaccination rates of people with psychiatric diagnoses were found to be higher compared to the healthy control group (68.4%); the highest rates were found in people with recurrent major depression (77.1%), followed by those with bipolar disorder (75.7%); it was reported that people with psychotic disorder had the highest vaccine refusal rates (47). In a review examining possible predictors of COVID-19 vaccine hesitancy, schizophrenia was defined as a risk factor (29). Küçükparlak found that having a diagnosis of schizophrenia increased the risk of not getting the COVID-19 vaccine 2.7-fold (30). In a study conducted in Japan, generalized trust, mental health factors such as depression and generalized anxiety, and fear of COVID-19 were identified as predictors for COVID-19 vaccine hesitancy (31).
In this study, according to the scores obtained from the vaccine hesitancy scale, hesitation about vaccines was highest in patients diagnosed with psychosis, depression, and anxiety disorder, respectively, and the lowest level of hesitation was found in patients diagnosed with ADHD and bipolar disorder. The higher vaccine hesitancy in patients with psychosis, depression, and anxiety disorder may be due to the effect of these disorders on the cognitive function, risk perception, and decision-making processes of these individuals. Paranoid ideation or lack of trust in psychotic disorders, low energy levels in depressed individuals, and fears and concerns arising from misinformation about the vaccine in individuals with anxiety disorders may play a role in increased hesitancy. Therefore, specific strategies should be developed for different psychiatric diagnoses when combating vaccine hesitancy in patients with psychiatric disorders. In a study conducted in Turkey, it was observed that unvaccinated patients with schizophrenia stated that they thought that vaccines had serious side effects and caused homosexuality, and it was stated that the vaccination attitude in patients with schizophrenia might be influenced by conspiracy theories (30). In another study conducted in Turkey, a positive correlation was reported between the belief in conspiracy theories and vaccine hesitancy (48). A study evaluating psychiatric morbidity and COVID-19 vaccine hesitancy emphasized that vaccine hesitancy was more prevalent across all psychiatric comorbidities (22). Considering that vaccine hesitancy increases the risk of depression, peritraumatic stress, and anxiety even in a healthy population without a psychiatric diagnosis (49), it should be taken into account that possible increased vaccine hesitancy may increase the clinical burden of disease in patients with psychiatric disorders who may be under high stress and anxiety due to their existing psychiatric diagnoses during periods when the safety of vaccines is discussed more, such as pandemics. In addition, in our study, it was shown that vaccine hesitancy was higher in women and those with less than a university education. Furthermore, there was a positive relationship between vaccination behavior and vaccine hesitancy and vaccine hesitancy was lower in those who received regular influenza vaccination within 1 year and every year, those who received pneumococcal vaccination, and those who received a COVID-19 vaccination during the pandemic. The effect of concern about the safety of COVID-19 vaccines on the intention to be vaccinated has been shown (50). In Lorenz’s study, it was stated that those who perceived a greater degree of vaccine effectiveness were more likely to obtain flu vaccination (19).
Increasing the vaccine uptake of these patients with psychiatric disorders will contribute positively to their life expectancy and quality. Adding preventive care healthcare units to mental health centers where vaccination can also be performed (51) and reminding patients of vaccination by sending messages or emphasizing the importance of vaccination may increase vaccine uptake. There is evidence that integration of mental health and community mental health center services can have a profound positive impact on the severe and persistent mental illness population (52). Including the vaccination status of patients in the patient assessment and follow-up protocols of psychiatrists may increase the awareness of vaccination in patients and contribute positively to vaccination rates and negative vaccine hesitancy. In the Lorenz study, it was found that those who received vaccine education from their doctor were 4 times more likely to be vaccinated for influenza (19).
Limitations of our study include the possibility of recall bias due to the fact that it was a single-center and cross-sectional survey study and that the participant group consisted of a population already suffering from a psychiatric illness and whose recall or ability to comment could be affected due to their illness or medications.
Conclusion
In conclusion, in our study, we evaluated the vaccination rates and vaccine hesitancy of patients with psychiatric disorders and found that COVID-19 vaccination rates among this group were low and influenza and pneumococcal vaccination rates were extremely low. Our findings clearly demonstrate the need for strategic interventions for the patient group, and the relationships between vaccination status and vaccine hesitancy and sociodemographic characteristics emphasize the importance of planning interventions taking into account psychiatric diagnoses and sociodemographic characteristics of individuals. Although more research has been conducted on COVID-19 vaccination rates of individuals with psychiatric disorders during the pandemic, data on vaccination rates against respiratory infections, especially pneumococcal vaccines, are limited. Therefore, there is a need to support the literature with more studies in this field.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the corresponding author upon reasonable request and following approval by the ethics committee.
Ethics statement
This study was approved by the Non-Interventional Ethics Committee of Dicle University (decision no: 114, date:14.02.2024). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
VP: Conceptualization, Data curation, Investigation, Methodology, Resources, Visualization, Writing – original draft, Writing – review & editing. BU: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. PB: Conceptualization, Formal analysis, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank Lütfiye Gür Elez and Zeynep Aybek Dinler for their support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ADHD, attention deficit hyperactivity disorder; COVID-19, coronavirus disease-2019; CPV-13, conjugated pneumococcal vaccine-13; OCD, obsessive-compulsive disorder; PPA-23, polysaccharide pneumococcal vaccine-23.
References
1. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol. (2014) 43:476–93. doi: 10.1093/ije/dyu038
2. Seminog OO, Goldacre MJ. Risk of pneumonia and pneumococcal disease in people with severe mental illness: English record linkage studies. Thorax. (2013) 68:171–6. doi: 10.1136/thoraxjnl-2012-202480
3. Nilsson NH, Bendix M, Öhlund L, Widerström M, Werneke U, Maripuu M. Increased risks of death and hospitalization in influenza/pneumonia and sepsis for individuals affected by psychotic disorders, bipolar disorders, and single manic episodes: A retrospective cross-sectional study. J Clin Med. (2021) 10:4411. doi: 10.3390/jcm10194411
4. Teixeira AL, Krause TM, Ghosh L, Shahani L, MaChado-Vieira R, Lane SD, et al. Analysis of COVID-19 infection and mortality among patients with psychiatric disorders, 2020. JAMA Netw Open. (2021) 4:e2134969. doi: 10.1001/jamanetworkopen.2021.34969
5. Nudel R, Wang Y, Appadurai V, Schork AJ, Buil A, Agerbo E, et al. A large-scale genomic investigation of susceptibility to infection and its association with mental disorders in the Danish population. Transl Psychiatry. (2019) 9:283. doi: 10.1038/s41398-019-0622-3
6. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502
7. Hert M DE, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. (2011) 10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x
8. Levinson Miller C, Druss BG, Dombrowski EA, Rosenheck RA. Barriers to primary medical care among patients at a community mental health center. Psychiatr Serv. (2003) 54:1158–60. doi: 10.1176/appi.ps.54.8.1158
9. Lord O, Malone D, Mitchell AJ. Receipt of preventive medical care and medical screening for patients with mental illness: a comparative analysis. Gen Hosp Psychiatry. (2010) 32:519–43. doi: 10.1016/j.genhosppsych.2010.04.004
10. Cohen S. Psychosocial vulnerabilities to upper respiratory infectious illness: implications for susceptibility to coronavirus disease 2019 (COVID-19). Perspect Psychol Sci. (2021) 16:161–74. doi: 10.1177/1745691620942516
11. Ronaldson A, Santana IN, Carlisle S, Atmore KH, Chilman N, Heslin M, et al. Severe mental illness and infectious disease mortality: a systematic review and meta-analysis. EClinicalMedicine. (2024) 77:102867. doi: 10.1016/j.eclinm.2024.102867
12. Mazereel V, Detraux J, Vancampfort D, van Winkel R, De Hert M. Impact of psychotropic medication effects on obesity and the metabolic syndrome in people with serious mental illness. Front Endocrinol (Lausanne). (2020) 11:573479. doi: 10.3389/fendo.2020.573479
13. Murphy KA, McGinty EE, Daumit GL. Hospitalization, mechanical ventilation, and mortality after COVID-19 among adults with or without serious mental illness. Psychiatr Serv. (2022) 73:335–8. doi: 10.1176/appi.ps.202100151
14. Correll CU, Solmi M, Croatto G, Schneider LK, Rohani-Montez SC, Fairley L, et al. Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry. (2022) 21:248–71. doi: 10.1002/wps.20994
15. Biazus TB, Beraldi GH, Tokeshi L, Rotenberg LS, Dragioti E, Carvalho AF, et al. All-cause and cause-specific mortality among people with bipolar disorder: a large-scale systematic review and meta-analysis. Mol Psychiatry. (2023) 28:2508–24. doi: 10.1038/s41380-023-02109-9
16. Vaccines and immunization. WHO. Available at: https://www.who.int/countries/tur/ (Accessed January 8, 2025).
17. Ten threats to global health in 2019. WHO. Available at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (Accessed January 8, 2025).
18. Jia R, Coupland C, Vinogradova Y, Qureshi N, Turner E, Vedhara K. Mental health conditions and COVID-19 vaccine outcomes: A scoping review. J Psychosom Res. (2024) 183:111826. doi: 10.1016/j.jpsychores.2024.111826
19. Lorenz RA, Norris MM, Norton LC, Westrick SC. Factors associated with influenza vaccination decisions among patients with mental illness. Int J Psychiatry Med. (2013) 46:1–13. doi: 10.2190/PM.46.1.a
20. Sanz-Rojo S, Jiménez-García R, López-de-Andrés A, de Miguel-Diez J, Perez-Farinos N, Zamorano-León JJ. Influenza vaccination uptake among high-risk target groups and health care workers in Spain and change from 2017 to 2020. Vaccine. (2021) 39:7012–20. doi: 10.1016/j.vaccine.2021.10.059
21. Huang H, Zhu XM, Liang PW, Fang ZM, Luo W, Ma YM, et al. COVID-19 vaccine uptake, acceptance, and hesitancy among persons with mental disorders during the second stage of China’s nationwide vaccine rollout. Front Med (Lausanne). (2021) 8:761601. doi: 10.3389/fmed.2021.761601
22. llon M, Dang AP, Barnes JB, Buresh J, Peloquin GD, Hogan AC, et al. Associations between psychiatric morbidity and COVID-19 vaccine hesitancy: An analysis of electronic health records and patient survey. Psychiatry Res. (2022) 307:114329. doi: 10.1016/j.psychres.2021.114329
23. Curtis HJ, Inglesby P, MacKenna B, Walker AJ, Morley J, Mehrkar A, et al. Trends, regional variation, and clinical characteristics of COVID-19 vaccine recipients: a retrospective cohort study in 23. 4 million patients using OpenSAFELY. BMJ Open. (2022) 12:e061622. doi: 10.1136/bmjopen-2022-061622
24. Kılıç OHT, Akdeniz G, Göksu MG, Manoğlu BG. COVİD-19 VACCİNATİON RATES IN PATİENTS WİTH SEVERE MENTAL. Izmir Democracy Univ Health Sci J. (2023) 6:435–44. doi: 10.52538/iduhes.1334814
25. Tzur Bitan D, Kridin K, Cohen AD, Weinstein O. COVID-19 hospitalisation, mortality, vaccination, and postvaccination trends among people with schizophrenia in Israel: a longitudinal cohort study. Lancet Psychiatry. (2021) 8:901–8. doi: 10.1016/S2215-0366(21)00256-X
26. De Hert M, Mazereel V, Detraux J, Van Assche K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry. (2021) 20:54–5. doi: 10.1002/wps.20826
27. De Picker LJ, Dias MC, Benros ME, Vai B, Branchi I, Benedetti F, et al. Severe mental illness and European COVID-19 vaccination strategies. Lancet Psychiatry. (2021) 8:356–9. doi: 10.1016/S2215-0366(21)00046-8
28. Mazereel V, Van Assche K, Detraux J, De Hert M. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. (2021) 8:444–50. doi: 10.1016/S2215-0366(20)30564-2
29. Farcas A, Christi P, Fagen J, Iftene F. Possible predictors of Covid-19 vaccine hesitancy in the psychiatric population - A scoping review. Psychiatry Res Commun. (2022) 2:100075. doi: 10.1016/j.psycom.2022.100075
30. Kucukparlak İ, Fikret Giynas F, Gica S. Effects of beliefs, conspiracy theories, and vaccine hesitancy on the vaccination status of patients with severe mental illness in a tertiary psychiatric care hospital in Türkiye. Psychiatry Clin Psychopharmacol. (2023) 33:272–9. doi: 10.5152/pcp.2023.23615
31. Sekizawa Y, Hashimoto S, Denda K, Ochi S, So M. Association between COVID-19 vaccine hesitancy and generalized trust, depression, generalized anxiety, and fear of COVID-19. BMC Public Health. (2022) 22:126. doi: 10.1186/s12889-021-12479-w
32. Nguyen KH, Chen S, Morris K, Chui K, Allen JD. Mental health symptoms and association with COVID-19 vaccination receipt and intention to vaccinate among adults, United States. Prev Med. (2022) 154:106905. doi: 10.1016/j.ypmed.2021.106905
33. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. (2007) 335:806–8. doi: 10.1136/bmj.39335.541782.AD
34. Luyten J, Bruyneel L, van Hoek AJ. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine. (2019) 37:2494–501. doi: 10.1016/j.vaccine.2019.03.041
35. Yılmaz N, Öke Karakaya P, Sönmez S. Aşı Tereddüdü Ölçeğinin türkçe geçerlik ve güvenirliği. İşletme Bilimi Dergisi. (2021) 9:499–517. doi: 10.22139/jobs.962519
36. Kantidakis EE, Symvoulakis EK, Basta M, Chourdaki E, Dimitriou H. Vaccination coverage of persons using hospital outpatient mental health services at Heraklion, Crete, Greece: A cross-sectional study during pandemic. Psychiatriki. (2024) 35(4):282–92. doi: 10.22365/jpsych.2024.019
37. Paget J, Caini S, Cowling B, Esposito S, Falsey AR, Gentile A, et al. The impact of influenza vaccination on the COVID-19 pandemic? Evidence and lessons for public health policies. Vaccine. (2020) 38:6485–6. doi: 10.1016/j.vaccine.2020.08.024
38. WHO SAGE Seasonal Influenza Vaccination Recommendations during the COVID-19 Pandemic . Available online at: https://www.who.int/publications/m/item/who-sage-seasonal-influenza-vaccination-recommendations-during-the-covid-19-pandemic (Accessed January 17, 2025).
39. Lin J, Li C, He W. Trends in influenza vaccine uptake before and during the COVID-19 pandemic in the USA. Public Health. (2023) 225:291–8. doi: 10.1016/j.puhe.2023.10.028
40. WHO. Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic . Available online at: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic (Accessed January 17, 2025).
41. Bonkat N, Fellendorf FT, Dalkner N, Reininghaus EZ. Severe mental disorders and vaccinations - a systematic review. World J Biol Psychiatry. (2022) 23:501–16. doi: 10.1080/15622975.2021.2013095
42. Lawrence T, Zubatsky M, Meyer D. The association between mental health diagnoses and influenza vaccine receipt among older primary care patients. Psychol Health Med. (2020) 25:1083–93. doi: 10.1080/13548506.2020.1717557
43. CDC. Influenza (Flu). Available online at: https://www.cdc.gov/flu/vaccines/vaccinations.html:~:text=the%20flu%20shot-,Everyone%206%20months%20and%20older%20should%20get%20a%20flu%20vaccine,Flu%20vaccination%20has%20important%20benefits (Accessed January 17, 2025).
44. CDC. Pneumococcal vaccine recommendations . Available online at: https://www.cdc.gov/pneumococcal/hcp/vaccine-recommendations/index.html (Accessed January 17, 2025).
45. Republic of Türkiye ministry of health covıd-19 vaccine information platform . Available online at: https://covid19asi.saglik.gov.tr/ (Accessed January 18, 2025).
46. Mazereel V, Vanbrabant T, Desplenter F, De Hert M. COVID-19 vaccine uptake in patients with psychiatric disorders admitted to or residing in a university psychiatric hospital. Lancet Psychiatry. (2021) 8:860–1. doi: 10.1016/S2215-0366(21)00301-1
47. Hassan L, Sawyer C, Peek N, Lovell K, Carvalho AF, Solmi M, et al. COVID-19 vaccination uptake in people with severe mental illness: a UK-based cohort study. World Psychiatry. (2022) 21:153–4. doi: 10.1002/wps.20945
48. Nazlı ŞB, Yığman F, Sevindik M, Deniz Özturan D. Psychological factors affecting COVID-19 vaccine hesitancy. Ir J Med Sci. (2022) 191:71–80. doi: 10.1007/s11845-021-02640-0
49. Palgi Y, Bergman YS, Ben-David B, Bodner E. No psychological vaccination: Vaccine hesitancy is associated with negative psychiatric outcomes among Israelis who received COVID-19 vaccination. J Affect Disord. (2021) 287:352–3. doi: 10.1016/j.jad.2021.03.064
50. Gica S, Altunbek HB, Karaca S, Sahingoz M, Cinar-Tanriverdi E. Investigation of the effect of attachment and some important psychiatric clinical entities on the relationship between COVID-19 vaccine hesitancy and distrust in vaccines. Curr Res Rev Psychol Psychiatry. (2022) 2:157–68.
51. Xiong GL, Iosif AM, Suo S, Mccarron RM, Koike A, Onate J, et al. Understanding preventive health screening services use in persons with serious mental illness: how does integrated behavioral health primary care compare? Int J Psychiatry Med. (2015) 48:279–98. doi: 10.2190/PM.48.4.d
Keywords: psychiatric disorder, vaccine, vaccine hesitancy, influenza, influenza vaccine, pneumococcus, pneumococcal vaccine, COVID 19
Citation: Demir Pervane V, Uyar B and Erten Bucaktepe PG (2025) Influenza, pneumococcal, and COVID-19 vaccination coverage and hesitancy in adults with psychiatric disorders. Front. Psychiatry 16:1566348. doi: 10.3389/fpsyt.2025.1566348
Received: 24 January 2025; Accepted: 24 March 2025;
Published: 22 April 2025.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Olgu Aygün, Izmir Bozyaka Training and Research Hospital, TürkiyeŞenay Koçakoğlu, Harran University Faculty of Medicine, Türkiye
Copyright © 2025 Demir Pervane, Uyar and Erten Bucaktepe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vasfiye Demir Pervane, dmFzZml5eWVkZW1pckBob3RtYWlsLmNvbQ==
 Vasfiye Demir Pervane
Vasfiye Demir Pervane Betül Uyar
Betül Uyar Pakize Gamze Erten Bucaktepe1
Pakize Gamze Erten Bucaktepe1