- Honghui Hospital, Xi’an Jiaotong University, Xi’an, Shaanxi, China
Objective: This study aims to analyze the impact of different surgical procedures on the prognosis and psychological state of patients with end-stage ankle arthritis (ESAA) by comparing two groups of patients with ESAA who have undergone total ankle replacement (TAR) and ankle arthrodesis (AA), and to investigate whether preoperative psychological status can alter the final clinical outcomes.
Methods: This study retrospectively collected data from 66 patients with ESAA who underwent AA surgery in the Foot and Ankle Surgery Department of Xi’an Honghui Hospital between 2016 and 2023. In July 2024, the final follow-up of patients was conducted via telephone or WeChat, with a follow-up duration of no less than 12 months. Before surgery and at the final follow-up, evaluations were conducted using the Chinese version of the Hospital Anxiety and Depression Scale (HADS), the Visual Analogue Scale (VAS) for pain (ranging from 0 to 100mm), and the American Orthopaedic Foot and Ankle Society (AOFAS) ankle and hindfoot score. The study compared differences in pain scores, functional scores, and psychological scores between patients in the TAR and AA groups before surgery and at the final follow-up. Additionally, patients who underwent TAR and AA were further subgrouped based on the severity of their preoperative psychological status, in order to analyze the impact of preoperative psychological conditions on surgical prognosis.
Results: A total of 66 patients with ESAA completed the follow-up. At the final follow-up, both the VAS and AOFAS scores in the TAR group and the AA group showed significant improvement compared to preoperative levels. Among them, the TAR group performed better in terms of AOFAS scores, but no significant difference was observed in VAS scores between the two groups. Additionally, there was no significant difference in HADS scores between the two groups at the final follow-up. Regardless of whether they belonged to the high-HADS group or the low-HADS group, patients showed significant improvement in clinical scores compared to preoperative levels. However, at the final follow-up, the clinical scores of the high-HADS group were significantly lower than those of the low-HADS group, and the incidence of complications in the high-HADS group was also higher.
Conclusion: This study found that both TAR and AA significantly improved patients’ psychology, pain, and functional activities. Both surgical methods demonstrated similar improvements in terms of final psychological status and pain relief. However, patients in the TAR group showed better ankle function and mobility. Patients with poorer preoperative psychological status had worse clinical outcomes and faced a higher risk of complications. The study indicates that both TAR and AA are effective treatment options for patients with ESAA, but poor preoperative psychological status is one of the important risk factors for poor prognosis. Therefore, when selecting a treatment approach, the patient’s psychological state and needs should be fully considered, and necessary psychological interventions and postoperative rehabilitation plans should be implemented to enhance the patient’s treatment outcomes and quality of life.
Introduction
End-Stage Ankle Arthritis (ESAA) is a severe stage of ankle arthritis, similar to end-stage hip arthritis, characterized by severely limited joint function and a very high disability rate (1). According to statistics, patients with ankle arthritis account for approximately 1% of the adult population worldwide and 2% to 4% of all osteoarthritis patients (2).Ankle degenerative disease is often intimately associated with prior trauma (3). Furthermore, it can also be caused by inflammatory joint diseases, hemochromatosis, and hemophilic arthropathy (4).Ankle Arthrodesis (AA) is considered the gold standard for the treatment of ESAA (5). With the continuous updating and improvement of ankle joint implants, the clinical outcomes of total ankle replacement (TAR) have also been significantly enhanced (6–8). Compared with patients undergoing Ankle Arthrodesis (AA), those receiving Total Ankle Replacement (TAR) exhibit better joint function and lower postoperative pain, although there is no significant difference in quality of life between the two surgical procedures (9–13). Furthermore, a meta-analysis study found that TAR has greater short-term advantages compared to AA, but in the medium to long term, TAR becomes disadvantageous due to higher complication and revision rates (14).
The high disability rate and corresponding decrement in quality of life attributable to ankle arthritis inevitably exert an impact on patients’ psychological status (15–17). Numerous scholarly studies have unveiled that psychosocial impairments adversely influence the outcomes and satisfaction associated with other orthopedic surgeries, particularly in the management of degenerative osteoarthritis (18–27). Studies have shown that patients with poorer preoperative psychological status tend to exhibit poorer prognosis and satisfaction after surgery, along with higher pain sensitivity (28) and a greater incidence of postoperative complications (29). However, the current psychological research targeting patients with ESAA appears relatively limited, primarily focusing on the field of TAR, while specific psychological studies on patients with AA are relatively scarce (30–34). This current state significantly restricts surgeons’ comprehensive and in-depth understanding of the psychological needs of this patient population.
Given the current research progress on psychological factors in ESAA surgery, we aim to clarify the changes in psychological status in terms of screening for anxiety, depression, as well as changes in clinical outcome as assessment of pain and ankle function following TAR and AA surgery. Furthermore, we hope to determine whether preoperative poorer psychological status has differential impacts on prognosis, thereby providing a reference for clinicians in devising treatment plans.
Patients and methods
Patients
This study was approved by the Ethics Review Committee (No: 202409007). The subjects were all ESAA patients who underwent TAR and AA surgeries in the Foot and Ankle Comprehensive Surgery Department of Xi’an Honghui Hospital between 2016 and 2023. Through case retrieval, it was ensured that all ESAA patients were undergoing TAR or AA for the first time and had a preoperative American Society of Anaesthesiologists (ASA) classification of I-II. In July 2024, the final follow-up of patients was conducted via telephone or WeChat, with a follow-up duration of no less than 12 months. Informed consent was obtained from all patients. Patients were excluded if they had previously undergone tibiotalar-calcaneal arthrodesis, if the surgery was intended for revision of a previous total ankle arthroplasty or ankle arthrodesis, if they had postoperative bone nonunion of the ankle due to previous trauma, if they were unable to communicate normally due to illness. The surgeries were performed by senior surgeons within our department, all of whom had similar levels of experience in both TAR and AA surgeries.
Outcome measures
We collected demographic data from the patients and assessed their pain and overall functional status using the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale and the Visual Analogue Scale (VAS) for pain both preoperatively and at the last follow-up. The Chinese Version of the Hospital Anxiety and Depression Scale (HADS) was used to investigate patients’ anxiety and depression levels both preoperatively and at the last follow-up.
The AOFAS Ankle-Hindfoot Scale, with a maximum score of 100 points, comprehensively and objectively assesses the patient’s ankle condition by encompassing pain (40%), function (50%), gait (10%), and other related indicators (35). The VAS is currently widely employed for pain assessment. It comprises a 100mm line, with one end denoting “no pain at all,” labeled as “0,” and the other end representing “the worst pain imaginable” or “pain at its most intense level,” labeled as “10.” Patients are instructed to mark a point on the line according to their own perception of pain (36). The HADS (37) consists of two subscales: Anxiety (HADS-A) and Depression (HADS-D). It includes seven items for assessing depression and seven items for assessing anxiety. There are six reverse-scored items in total, with five in the Depression subscale and one in the Anxiety subscale. Each item is rated on a 4-point scale ranging from 0 to 3, resulting in a total score range of 0 to 21. Scores of 0 to 7 indicate no symptoms, 8 to 10 suggest possible anxiety or depression, and 11 to 21 confirm the presence of anxiety or depression. We categorize scores of 8 or above as the high-HADS group (indicating a high risk of anxiety/depressive state), and scores below 8 as the low-HADS group (indicating a low risk of anxiety/depressive state) (37).
We first divided the patients into the TAR group and the AA group, and then further subclassified each surgical group into a low-HADS group (indicating a preoperative low risk of anxiety/depressive state) and a high-HADS group (indicating a preoperative high risk of anxiety/depressive state). We grouped patients according to their surgical techniques and preoperative psychological states, aiming not only to more intuitively reflect the differences in surgical outcomes between the two techniques, but also to ascertain whether preoperative psychological states have an impact on the prognosis of each surgical technique.
Statistical analysis
We reported the demographic information of the patient population and classified the patients into the TAR group and the AA group. Furthermore, each subgroup was further subdivided into the low-HADS group and the high-HADS group. Statistical analysis of the data was performed using SPSS software version 27.0 (IBM, New York, United States).Firstly, the Shapiro-Wilk test was used to assess the normality of the data distribution, in order to determine whether parametric or non-parametric tests should be employed. For measurement data that satisfy normal distribution, they are expressed as mean ± standard deviation (x ± s), and comparisons between two groups are conducted using the independent samples t-test, with paired t-test applied to paired measurement data. For measurement data that do not satisfy normal distribution, they are presented as M(P25, P75), and comparisons between two groups are performed using the Mann-Whitney U test, with the Wilcoxon Signed Rank Test applied to paired measurement data. For count data, they are represented as n(%), and comparisons between two groups of measurement data are conducted using the chi-square test. Baseline characteristics were compared using the independent samples t-test, Mann-Whitney U test, and chi-square test. Differences in preoperative and postoperative evaluation indicators were primarily analyzed using the independent samples t-test or Mann-Whitney U test. To evaluate the differences in various evaluation indicators between preoperative and last follow-up within the TAR and AA groups, we used the paired samples t-test or Wilcoxon Signed Rank Test. For the differences in preoperative and final clinical outcomes between the low HADS group and high HADS group within the same subgroup, we also conducted analysis using the independent samples t-test or Mann-Whitney U test. The significance level for statistical tests was set at P < 0.05.
Results
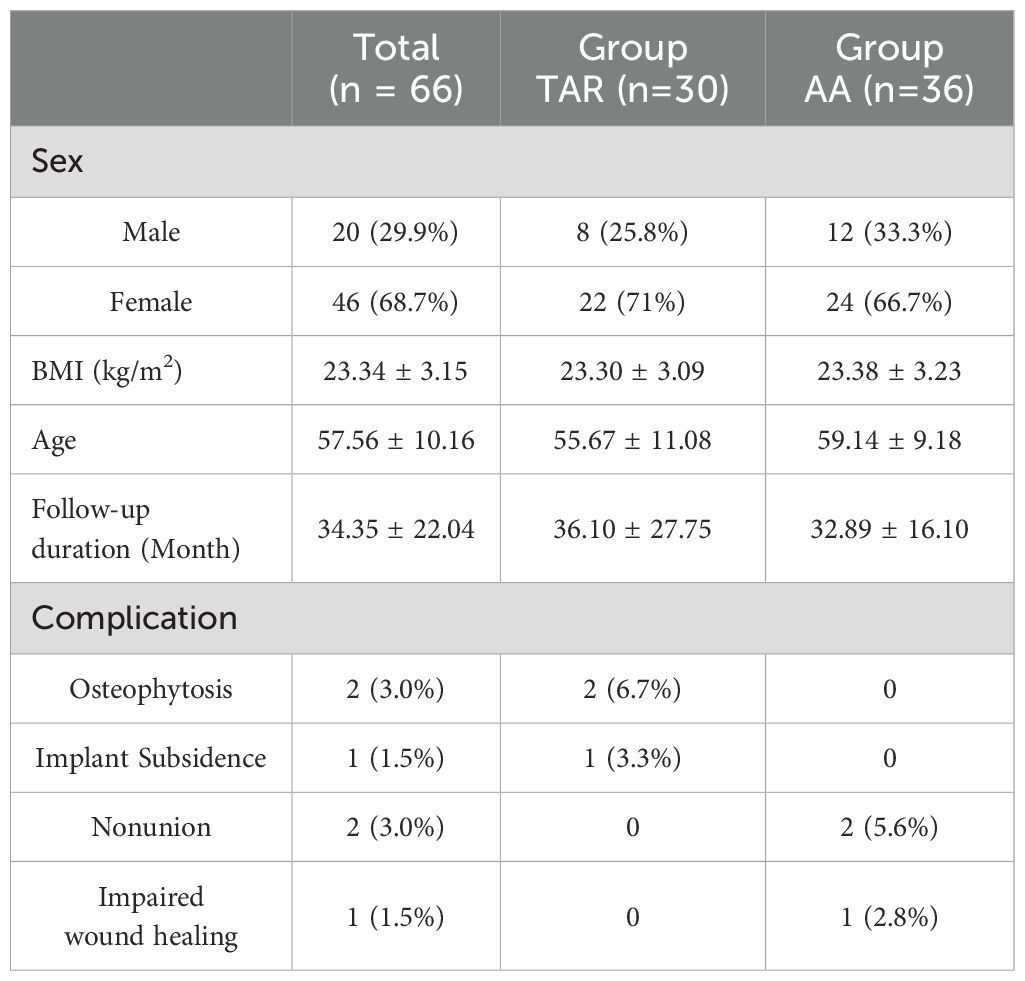
In our study, a total of 100 patients with eligible ESAA were enrolled, among which 66 patients completed the follow-up, resulting in a loss to follow-up rate of 44%. The most common reasons for loss to follow-up were change of contact information and refusal to participate in the final follow-up. Of the 66 patients who completed the follow-up, 30 were in the TAR group and 36 were in the AA group. The mean age of the patients was 57.56 ± 10.16 years, ranging from a minimum of 27 years to a maximum of 77 years. The average follow-up time for all patients was 34.35 ± 22.04 months, with the shortest follow-up being 12 months and the longest being 88 months. Preoperatively, 25 patients (37.88%) had high HADS scores. In the TAR group, 2 patients (6.7%) experienced postoperative osteophyte formation and 1 patient (3.3%) had prosthesis subsidence. In the AA group, 2 patients (5.6%) developed bone nonunion and 1 patient (2.8%) had poor wound healing. Baseline characteristics of the two patient groups are presented in Table 1.
There were no significant differences in the baseline preoperative scores between the TAR and AA groups (P > 0.05, Table 2). At the final follow-up, both groups demonstrated substantial improvements in their clinical outcomes compared to the preoperative state (p>0.05, Table 3). The TAR group showed superiority only in the AOFAS score, with a mean of 80.47 ± 12.56, compared to the AA group’s mean of 73.28 ± 8.81 (p<0.01, Table 2). However, there were no statistically significant differences in either the VAS score or the psychological score (HADS) between the two groups (P>0.05, Table 2). This suggests that both surgical approaches provide similar improvements in pain relief for ESAA, but TAR offers better ankle mobility.
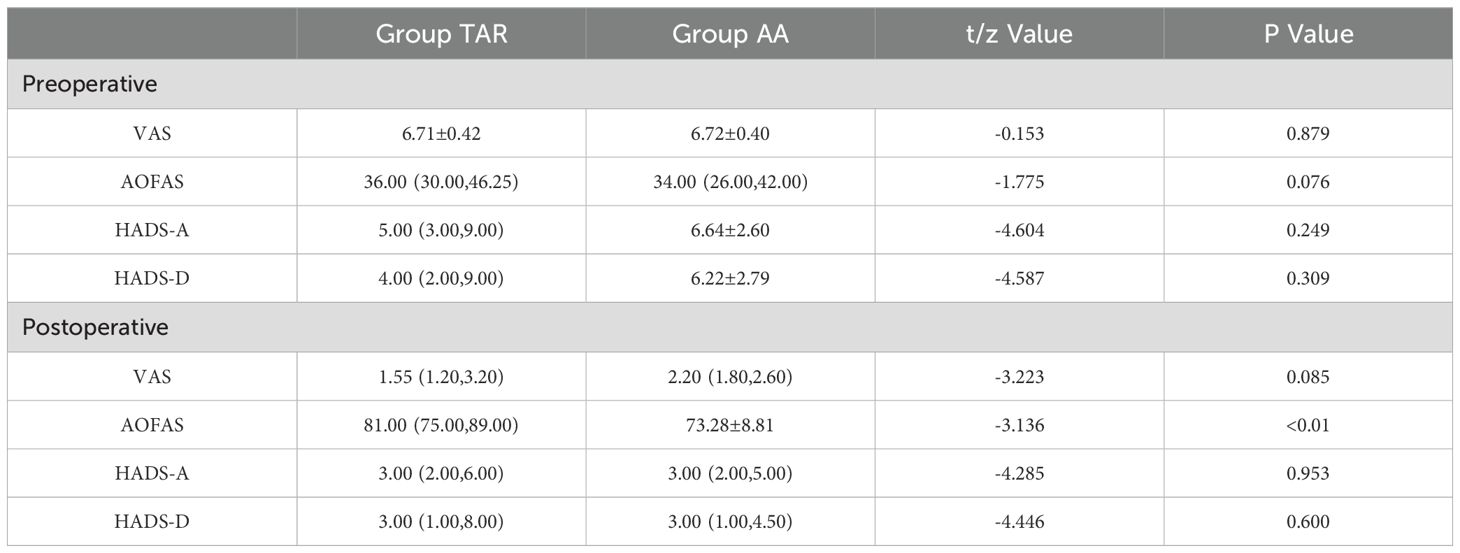
Table 2. Differences in baseline and final follow-up clinical outcome scores between the TAR and AA groups overall.
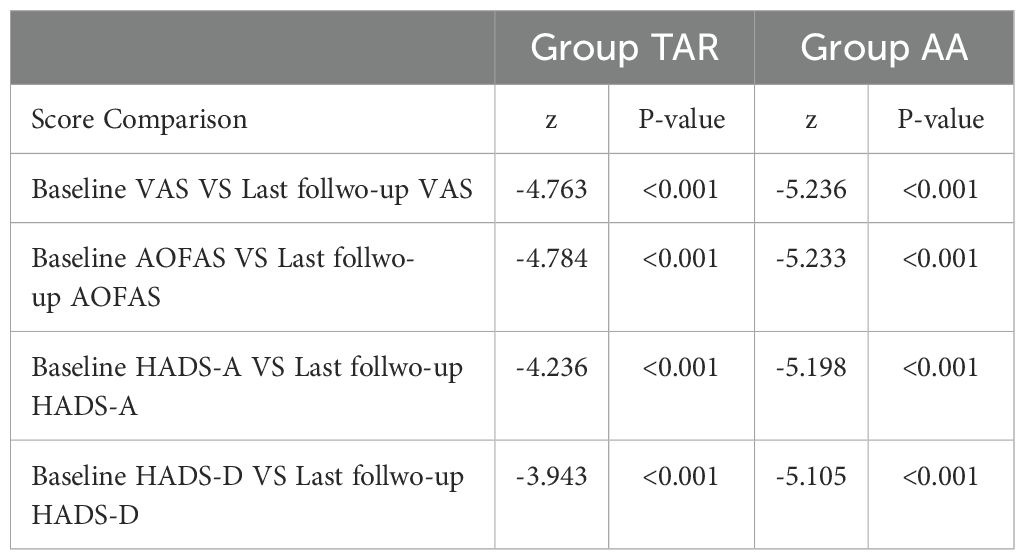
Table 3. Comparison of baseline and final follow-up clinical outcome scores within the TAR and AA groups.
In both the TAR and AA groups, regardless of whether the patients belonged to the low HADS group or the high HADS group preoperatively, their final clinical scores showed significant improvements compared to their preoperative baseline scores (p < 0.05), as shown in Table 4.
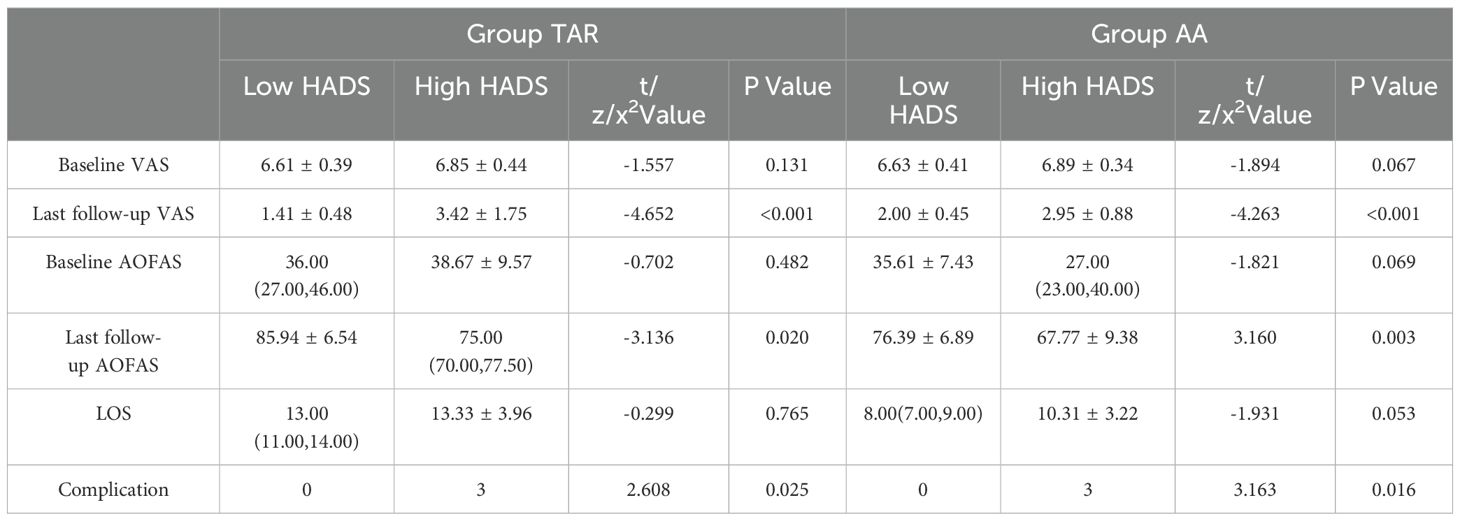
Table 4. Differences in improvement of final clinical outcome scores based on preoperative psychological status in the TAR and AA groups.
Among patients undergoing TAR and AA, there were no significant differences in preoperative VAS scores and preoperative AOFAS scores between the low-HADS group and the high-HADS group (p > 0.05). However, among patients in the preoperative high-HADS group, those who underwent TAR and AA had significantly lower VAS scores and AOFAS scores at the final follow-up compared to patients in the preoperative low-HADS group (p < 0.05). There was no significant difference in the length of stay (LOS) between the low-HADS group and the high-HADS group (p > 0.05). In terms of postoperative complications, the incidence was significantly higher in the high-HADS group compared to the low-HADS group (P < 0.05), as shown in Table 4.
Discussion
To determine whether the better range of motion observed postoperatively in TAR compared to AA can lead to better psychological improvement for patients, we compared the final clinical outcomes and psychological scores between TAR and AA. There is robust evidence that emotional disorders such as depression and anxiety have significant negative impacts on the prognosis of patients with knee and hip arthritis (18–27), but research in the field of foot and ankle surgery is still scarce. Given the significant differences in etiology, functional impairment, and clinical manifestations between ESAA and other end-stage arthritides, this specificity may exert varying degrees of influence on an individual’s psychological state, pain perception, and daily function. Therefore, we further investigated the differences in final clinical outcomes between ESAA patients with preoperative high-risk and low-risk anxiety/depression states who underwent TAR and AA treatment, in order to comprehensively assess the impact of psychological status on treatment efficacy.
At the final follow-up, patients who underwent either TAR or AA reported significant improvements in outcome indicators compared to their preoperative status. However, patients with high HADS scores reported more severe pain and poorer function at the final follow-up compared to those with low preoperative HADS scores. A large number of previous studies have clearly demonstrated that psychological distress is an important risk factor for poor surgical outcomes in patients with musculoskeletal diseases. It not only adversely affects the degree of postoperative pain but also significantly reduces patients’ functional recovery and overall satisfaction (23–27, 38). Cunningham et al. conducted a correlation analysis of risk factors affecting outcomes after TAR surgery and found that depression had a negative effect on patient-reported outcomes (32). In a recent study by Cunningham et al., preoperative mental health status and depression were analyzed as risk factors, and it was found that although the clinical outcomes of all patients improved compared to the preoperative status, the improvement in final outcomes was relatively poorer among patients with preoperative depression and poorer mental health (33). Kim et al. used the Center for Epidemiologic Studies Depression Scale (CES-D) and the Patient Health Questionnaire-9 (PHQ-9) to assess preoperative depression status in TAR patients. The study found that patients with depression had lower final clinical indicators compared to those without depression (34). However, it is noteworthy that there were no statistically significant differences in the two key indicators, preoperative VAS scores and AOFAS scores, between the two groups (34), which is consistent with our analysis results.
Our study also found that regardless of whether patients had poor or good preoperative psychological status, their psychological state significantly improved after undergoing TAR and AA surgical interventions. This finding suggests that preoperative anxiety and depression are largely reversible, and this positive psychological transformation is likely directly related to the effective surgical intervention. However, at the final follow-up stage, despite patients in the TAR group showing a significant advantage in terms of joint range of motion compared to the AA group, there was no statistically significant difference between the two groups in the two psychological assessment dimensions of HADS-A and HADS-D. Drawing upon previous research findings, we speculate that the absence of statistically significant differences in psychological scores may be associated with the equivalent performance of TAR and AA in postoperative pain relief, gait recovery, and overall patient satisfaction (14, 39–42). Nevertheless, we must recognize that psychological states can be influenced by various factors (43), necessitating further in-depth research in the future to investigate this matter.
At the final follow-up, no complications were observed in the low-HADS groups of both the TAR and AA groups. However, in the TAR group, two patients with high-HADS scores before surgery developed osteophyte hyperplasia accompanied by pain, and underwent a second joint debridement surgery. In addition, one more patient suffered from abnormal limb alignment as a result of prosthesis subsidence. In the AA group, two patients with preoperative high-HADS group had nonunion and one had poor wound healing. These results indicate that poor preoperative psychological status may increase the risk of postoperative complications, which is consistent with the findings of Harmer’s research in the hip and knee joint areas (29). Simultaneously, we observed that preoperative psychological status did not significantly affect patients’ LOS. This finding is consistent with the results of Sutherland et al.’s study on risk factors for ESAA surgery (44). This indicates that preoperative psychological status may influence the incidence of postoperative complications, but its impact on the LOS may be relatively minor, and LOS may be influenced by other factors. Therefore, conducting preoperative psychological assessments and providing appropriate interventions for patients have positive implications for reducing the risk of postoperative complications. However, the management of LOS requires comprehensive consideration of multiple factors for optimization.
In this study, patients undergoing ESAA were self-assessed using the HADS upon admission to evaluate their preoperative psychological state, which generally results in less observer bias. Furthermore, the use of appropriate scale tools can improve time and cost benefits, making it feasible for routine application in orthopedic clinical practice. By thoroughly obtaining and analyzing the patient’s clinical history and conducting systematic mental health screenings, once a patient is identified with higher psychological risks, they should be promptly referred to professional mental health experts, and based on this, a targeted and personalized exercise and rehabilitation plan should be developed. By taking such measures, surgeons can more effectively mitigate the risk of adverse clinical prognosis that patients may face due to psychological issues, thereby providing solid support and assurance for the patient’s overall rehabilitation process.
This study has several limitations. Firstly, regional bias and sample size constraints may affect the generalizability of the results, and we still require large-sample, multicenter studies to further validate the conclusions of this study. Secondly, the generalization of psychological assessment tools also needs to be considered, and interdisciplinary teams are required in the later stages to deepen psychological assessment and treatment planning. Finally, the retrospective design, accompanied by high loss to follow-up rates and retrospective bias, may lead to biased results. It is recommended that future studies adopt randomized controlled trials to enhance scientific rigor and objectivity. These limitations should be fully considered when interpreting and generalizing the results of this study to ensure the reliability, validity, and broad applicability of the research conclusions.
Conclusion
We found that both TAR and AA significantly improved patients’ psychological well-being, pain, and functional activities, with similar improvements in final psychological status and pain relief. In terms of ankle range of motion, TAR was superior to AA. However, patients with poorer preoperative psychological status had significantly worse clinical outcomes and a higher risk of complications compared to those with better preoperative psychological status. This study indicates that both TAR and AA are effective treatment options for ESAA, but poorer preoperative psychological status is one of the risk factors for poor prognosis after TAR and AA surgeries. Therefore, when selecting a treatment approach, the patient’s psychological state and needs should be fully considered, and necessary psychological interventions and postoperative rehabilitation plans should be implemented to enhance the patient’s treatment outcomes and quality of life.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee, Honghui Hospital, Xi’an Jiaotong University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HW: Data curation, Investigation, Visualization, Writing – original draft, Writing – review & editing. SC: Data curation, Investigation, Writing – original draft. GL: Formal analysis, Writing – original draft. JL: Conceptualization, Resources, Supervision, Writing – review & editing. JX: Conceptualization, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Glazebrook M, Daniels T, Younger A, Foote CJ, Penner M, Wing K, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surgery. Am. (2008) 90:499–505. doi: 10.2106/JBJS.F.01299
2. Barg A, Pagenstert GI, Hügle T, Gloyer M, Wiewiorski M, Henninger HB, et al. Ankle osteoarthritis: etiology, diagnostics, and classification. Foot Ankle Clinics. (2013) 18:411–26. doi: 10.1016/j.fcl.2013.06.001
3. Thomas AC, Hubbard-Turner T, Wikstrom EA, Palmieri-Smith RM. Epidemiology of posttraumatic osteoarthritis. J Athletic Training. (2017) 52:491–6. doi: 10.4085/1062-6050-51.5.08
4. Goldberg AJ, Macgregor A, Dawson J, Singh D, Cullen N, Sharp RJ, et al. The demand incidence of symptomatic ankle osteoarthritis presenting to foot & ankle surgeons in the United Kingdom. Foot (Edinburgh Scotland). (2012) 22:163–6. doi: 10.1016/j.foot.2012.02.005
5. Strasser NL, Turner NS. Functional outcomes after ankle arthrodesis in elderly patients. Foot Ankle Int. (2012) 33:699–703. doi: 10.3113/FAI.2012.0699
6. Mcalister JE, Duelfer KA. Updates on total ankle arthroplasty. Clinics Podiatric Med Surg. (2023) 40:725–33. doi: 10.1016/j.cpm.2023.05.013
7. Maccario C, Paoli T, Romano F, D'Ambrosi R, Indino C, Usuelli FG. Transfibular total ankle arthroplasty: a new reliable procedure at five-year follow-up. Bone Joint J. (2022) 104-B:472–8. doi: 10.1302/0301-620X.104B4.BJJ-2021-0167.R5
8. Knupp M, Stufkens SA. Update on total ankle arthroplasty. Therapeutische Umschau. Rev Therapeutique. (2022) 77(10):511–6. doi: 10.1024/0040-5930/a001225
9. Dalat F, Trouillet F, Fessy MH, Bourdin M, Besse JL. Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: Retrospective study of 54 cases. Orthopaedics traumatology Surg research: OTSR. (2014) 100:761–6. doi: 10.1016/j.otsr.2014.07.018
10. Esparragoza L, Vidal C, Vaquero J. Comparative study of the quality of life between arthrodesis and total arthroplasty substitution of the ankle. J Foot Ankle Surg. (2011) 50:383–7. doi: 10.1053/j.jfas.2011.03.004
11. Lawton CD, Butler BA, Dekker RG, Prescott A, Kadakia AR. Total ankle arthroplasty versus ankle arthrodesis-a comparison of outcomes over the last decade. J Orthopaedic Surg Res. (2017) 12:76. doi: 10.1186/s13018-017-0576-1
12. Goldberg AJ, Chowdhury K, Bordea E, Blackstone J, Brooking D, Deane EL, et al. Total ankle replacement versus ankle arthrodesis for patients aged 50-85 years with end-stage ankle osteoarthritis: the TARVA RCT. Health Technol Assess. (2023) 27:1–80. doi: 10.3310/PTYJ1146
13. Goldberg AJ, Chowdhury K, Bordea E, Hauptmannova I, Blackstone J, Brooking D, et al. Total ankle replacement versus arthrodesis for end-stage ankle osteoarthritis: A randomized controlled trial. Ann Internal Med. (2022) 175:1648–57. doi: 10.7326/M22-2058
14. Liu S, Wang Y, Zhang M, Wei P, Li Y, Wang T, et al. A comparative study of modern total ankle replacement and ankle arthrodesis for ankle osteoarthritis at different follow-up times: A systematic review and meta-analysis. Int Orthopaedics. (2023) 47:1493–510. doi: 10.1007/s00264-023-05753-6
15. Rajapakshe S, Sutherland JM, Wing K, Crump T, Liu G, Penner M, et al. Health and quality of life outcomes among patients undergoing surgery for end-stage ankle arthritis. Foot Ankle Int. (2019) 40:1129–39. doi: 10.1177/1071100719856888
16. Nakagawa R, Yamaguchi S, Kimura S, Sadamasu A, Yamamoto Y, Sato Y, et al. Association of anxiety and depression with pain and quality of life in patients with chronic foot and ankle diseases. Foot Ankle Int. (2017) 38:1192–8. doi: 10.1177/1071100717723133
17. Paget LDA, Tol JL, Kerkhoffs GMMJ, Reurink G. Health-related quality of life in ankle osteoarthritis: A case-control study. Cartilage. (2021) 13:1438S–44S. doi: 10.1177/19476035211025814
18. Ali A, Lindstrand A, Sundberg M, Flivik G. Preoperative anxiety and depression correlate with dissatisfaction after total knee arthroplasty: A prospective longitudinal cohort study of 186 patients, with 4-year follow-up. J Arthroplasty. (2017) 32:767–70. doi: 10.1016/j.arth.2016.08.033
19. Götz JS, Benditz A, Reinhard J, Schindler M, Zeman F, Grifka J, et al. Influence of anxiety/depression, age, gender and ASA on 1-year follow-up outcomes following total hip and knee arthroplasty in 5447 patients. J Clin Med. (2021) 10:3095. doi: 10.3390/jcm10143095
20. Hampton SN, Nakonezny PA, Richard HM, Wells JE. Pain catastrophizing, anxiety, and depression in hip pathology. Bone Joint J. (2019) 101-B:800–7. doi: 10.1302/0301-620X.101B7.BJJ-2018-1309.R1
21. Duivenvoorden T, Vissers MM, Verhaar JAN, Busschbach JJ, Gosens T, Bloem RM, et al. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthritis Cartilage. (2013) 21:1834–40. doi: 10.1016/j.joca.2013.08.022
22. de Filippis R, Mercurio M, Segura-Garcia C, De Fazio P, Gasparini G, Galasso O. Defining the minimum clinically important difference (MCID) in the hospital anxiety and depression scale (HADS) in patients undergoing total hip and knee arthroplasty. Orthopaedics traumatology Surg research: OTSR. (2024) 110:103689. doi: 10.1016/j.otsr.2023.103689
23. Khatib Y, Madan A, Naylor JM, Harris IA. Do psychological factors predict poor outcome in patients undergoing TKA? A systematic review. Clin Orthopaedics Related Res. (2015) 473:2630–8. doi: 10.1007/s11999-015-4234-9
24. Alattas SA, Smith T, Bhatti M, Wilson-Nunn D, Donell S. Greater pre-operative anxiety, pain and poorer function predict a worse outcome of a total knee arthroplasty. Knee Surgery Sports Traumatology Arthroscopy. (2017) 25:3403–10. doi: 10.1007/s00167-016-4314-8
25. Visser MA, Howard KJ, Ellis HB. The influence of major depressive disorder at both the preoperative and postoperative evaluations for total knee arthroplasty outcomes. Pain Med. (2019) 20:826–33. doi: 10.1093/pm/pny107
26. O’Connor JP, Holden P, Gagnier JJ. Systematic review: preoperative psychological factors and total hip arthroplasty outcomes. J Orthopaedic Surg Res. (2022) 17:457. doi: 10.1186/s13018-022-03355-3
27. Badura-Brzoza K, Zajac P, Kasperska-Zajac A, Brzoza Z, Matysiakiewicz J, Piegza M, et al. Anxiety and depression and their influence on the quality of life after total hip replacement: preliminary report. Int J Psychiatry Clin Pract. (2008) 12:280–4. doi: 10.1080/13651500802095012
28. Diei C, Mehdipour S, Wall PV, Gabriel RA. The association of depression and anxiety with postoperative opioid use following total joint arthroplasty. Heliyon. (2023) 9:e18813. doi: 10.1016/j.heliyon.2023.e18813
29. Harmer JR, Wyles CC, Duong SQ, Morgan Iii RJ, Maradit-Kremers H, Abdel MP. Depression and anxiety are associated with an increased risk of infection, revision, and reoperation following total hip or knee arthroplasty. Bone Joint J. (2023) 105-B:526–33. doi: 10.1302/0301-620X.105B5.BJJ-2022-1123.R1
30. Wilson JM, Schwartz AM, Farley KX, Bariteau JT. Preoperative depression influences outcomes following total ankle arthroplasty. Foot Ankle Specialist. (2021) 15:321–9. doi: 10.1177/1938640020951657
31. Mercer NP, Lezak BA, Hedbany D, Butler JJ, Krebsbach S, Bloom DA, et al. The impact of mental health disorders on outcomes following total ankle arthroplasty: A systematic review. Foot Ankle Surg. (2025) 4:S1268-7731(25)00001-3. doi: 10.1016/j.fas.2025.01.005
32. Cunningham DJ, Deorio JK, Nunley JA, Easley ME, Adams SB. The effect of patient characteristics on 1 to 2-year and minimum 5-year outcomes after total ankle arthroplasty. J Bone Joint Surgery. Am. (2019) 101:199–208. doi: 10.2106/JBJS.18.00313
33. Cunningham DJ, Steele JR, Allen NB, Nunley JA, Adams SB. The impact of preoperative mental health and depression on outcomes after total ankle arthroplasty. J Bone Joint Surgery. Am. (2021) 103:131–8. doi: 10.2106/JBJS.20.00395
34. Kim TY, Lee HW, Jeong BO. Influence of depressive symptoms on the clinical outcomes of total ankle arthroplasty. J Foot Ankle Surg. (2020) 59:59–63. doi: 10.1053/j.jfas.2019.07.001
35. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. (1994) 15:349–53. doi: 10.1177/107110079401500701
36. Bodian CA, Freedman G, Hossain S, Eisenkraft JB, Beilin Y. The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology. (2001) 95:1356–61. doi: 10.1097/00000542-200112000-00013
37. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
38. Wertli MM, Held U, Lis A, Campello M, Weiser S. Both positive and negative beliefs are important in patients with spine pain: findings from the Occupational and Industrial Orthopaedic Center registry. Spine J. (2018) 18:1463–74. doi: 10.1016/j.spinee.2017.07.166
39. Seo SG, Kim EJ, Lee DJ, Bae KJ, Lee KM, Lee DY. Comparison of multisegmental foot and ankle motion between total ankle replacement and ankle arthrodesis in adults. Foot Ankle Int. (2017) 38:1035–44. doi: 10.1177/1071100717709564
40. Braito M, Dammerer D, Kaufmann G, Fischler S, Carollo J, Reinthaler A, et al. Are our expectations bigger than the results we achieve? a comparative study analysing potential advantages of ankle arthroplasty over arthrodesis. Int Orthopaedics. (2014) 38:1647–53. doi: 10.1007/s00264-014-2428-5
41. Saltzman CL, Mann RA, Ahrens JE, Amendola A, Anderson RB, Berlet GC, et al. Prospective controlled trial of STAR total ankle replacement versus ankle fusion: initial results. Foot Ankle Int. (2009) 30:579–96. doi: 10.3113/FAI.2009.0579
42. Flavin R, Coleman SC, Tenenbaum S, Brodsky JW. Comparison of gait after total ankle arthroplasty and ankle arthrodesis. Foot Ankle Int. (2013) 34:1340–8. doi: 10.1177/1071100713490675
43. Manwell LA, Barbic SP, Roberts K, Durisko Z, Lee C, Ware E, et al. What is mental health? Evidence towards a new definition from a mixed methods multidisciplinary international survey. BMJ Open. (2015) 5:e007079. doi: 10.1136/bmjopen-2014-007079
Keywords: end-stage ankle arthritis, ankle arthrodesis, ankle arthroplasty, psychological factors, prognosis
Citation: Wang H, Cao S, Liu G, Lu J and Xu J (2025) Impact of psychological factors on the final clinical outcomes of patients undergoing ankle arthrodesis and ankle replacement. Front. Psychiatry 16:1550465. doi: 10.3389/fpsyt.2025.1550465
Received: 23 December 2024; Accepted: 17 February 2025;
Published: 06 March 2025.
Edited by:
Saraswati Dhungana, Institute of Medicine, NepalReviewed by:
Pratikchya Tulachan, Institute of Medicine, NepalRika Rijal, Kathmandu University, Nepal
Copyright © 2025 Wang, Cao, Liu, Lu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junkui Xu, NTY4NzIwODE4QHFxLmNvbQ==
 Hongze Wang
Hongze Wang Shihang Cao
Shihang Cao Geng Liu
Geng Liu Junkui Xu
Junkui Xu