- 1Department of Special Education, University of Haifa, Haifa, Israel
- 2School of Psychological Sciences, University of Haifa, Haifa, Israel
- 3The Haifa Brain and Behavior Hub (HBBH), University of Haifa, Haifa, Israel
- 4The Edmond J. Safra Brain Research Center for the Study of Learning Disabilities, University of Haifa, Haifa, Israel
Introduction: The Community Assessment of Psychic Experiences (CAPE-42) is a reliable tool to assess psychotic experiences (PEs) in clinical and non-clinical populations, in research and clinical settings.
Methods: To investigate cultural differences in PEs and control for pathological behavior in non-clinical groups, we developed a Hebrew version of the CAPE-42 using the translation/back-translation method. A total of 359 Hebrew speaking Israelis participated in an online study comprising the CAPE-42, the Autistic Quotient (AQ), the Center for Epidemiological Study – Depression Scale (CES-D), and the Prodromal Questionnaire – Brief Version (PQ-B). We examined the psychometric properties of the Hebrew CAPE-42—including its factor structure, internal consistency, gender invariance, and validity. We also investigated the independent and interaction effects of psychotic and autistic traits on depressive symptoms.
Results: Reliability analysis demonstrated very good internal consistency, and confirmatory factor analysis supported the eight-factor model, which included depressive, social withdrawal, affective flattening, avolition, bizarre experiences, perceptual abnormalities, persecutory ideation, and magical thinking. Demonstrating its predictive and convergent validity, we found significant correlations with the CES-D and the PQ-B. The predictive model showed that both psychotic and autistic traits are independent, non-interacting, predictors of depressive symptoms.
Conclusions: The Hebrew CAPE-42 offers a valuable instrument for investigating PEs in the Hebrew-speaking population and facilitates cross-cultural studies.
1 Introduction
Psychotic experiences (PEs) affect approximately 7.2% of the general population, manifesting along a continuum from subclinical levels to severe psychotic disorders, such as schizophrenia (1–3). These experiences, even when not fully meeting diagnostic criteria for psychotic disorders, are significant risk factors that can impact normative behavior and frequently co-occur with other clinical conditions like affective and anxiety, and autism spectrum disorders (4–7). Despite this, the precise effects of PEs on typical behavior remain poorly understood (8). To advance our understanding of psychosis etiology, it is essential to use tools that measure the intensity and frequency of PEs in both clinical and non-clinical populations, and that capture individual differences in subdomains of PEs. Such tools can help differentiate between typical and pathological behavior, facilitating systematic modeling of psychosis-related conditions (1, 9), and providing a structured framework for directly investigating the interplay between psychotic disorders and other clinical conditions. The key example illustrating the latest need is the ongoing debate on comorbidity between autism and psychosis. While these disorders are defined as strictly distinct (10), some proposed an overlapping modeling of the two spectra, based on genetic, etiologic, and symptomatologic evidence (11–14). In this model, a co-occurrence of the two conditions predicts an aggravation of deficits. Alternatively, the diametric model suggests that the disorders lie at the opposite ends of a unidimensional spectrum, with typical functioning at the center (15, 16). This approach, supported mainly by genetic evidence (17, 18), suggests an opposite symptomatology and therefore, no possible co-occurrence. The revised diametric model allows for co-occurrence and assumes both overlapping and diametric symptomatology (19). Nevertheless, the effect of the relative combination of psychotic and autistic traits remains unclear. Similarly, their combined effects on conditions with high comorbidity (e.g., depression) are still discussed (7, 20–22). Understanding these complex interplays will provide insight into the variability in psychotic symptomatology.
Cross-cultural research is also crucial for understanding variations in the expression of PEs to adapt research and clinical tools to the targeted populations. Studies show that cultural and environmental differences can influence both the prevalence and the nature of PEs (23–25). Yet, these cultural aspects are still not well understood (26–28). This is perhaps because most tools were developed for the Western world, and often applied in non-Western cultures without validation, leading to over- or under-estimation of measurement. Therefore, to develop tools that are culturally appropriate and standardized for use in diverse populations, there is a need to adapt the instruments to other cultures and languages.
The Community Assessment of Psychic Experience (CAPE) is a widely used tool designed to assess PEs in non-clinical populations (29). This self-report questionnaire includes 42 items measuring the frequency of PEs and the associated distress. Unlike other scales such as the Prodromal Questionnaire – Brief version (i.e., self-report tool evaluating early signs of psychosis focused on the positive dimension (30)) and the Schizotypical Personality Questionnaire (i.e., self-report evaluating psychotic traits including positive symptoms, interpersonal deficits and disorganization (31)), the CAPE-42 measures a wider range of psychotic experiences, including positive (e.g., bizarre experiences, delusional ideation), negative (e.g., social withdrawal, and avolition) and depressive dimensions. This approach enables a more detailed understanding of the broad spectrum of PEs (32), making the CAPE-42 more suitable for broader epidemiological research in the general population and cross-cultural research (27, 28, 33). The specific composition of the questionnaire demonstrates good reliability and validity (32, 34), and shows strong predictive capabilities for anxiety, depression, and stress sensitivity (35). Furthermore, the scores in the dimensions evaluated by this self-questionnaire closely align with the scores from interview-based assessments (35). Therefore, the CAPE-42 has become one of the most commonly used tools to evaluate PEs in research, leading to a need for cross-cultural adaptation.
Despite extensive validation and application of the CAPE-42 across cultures and languages (e.g., English, French, Spanish, Persian, Italian (36–41)), there is a notable gap in its application within Semitic-speaking populations., generating a need to adapt this tool to Middle Eastern cultures and languages, like performed by Fekih-Romdhane et al. (33) with Arabic speakers in Lebanon, and in the present study with Hebrew speakers in Israel. Furthermore, we observe that cross-validation was not systematically performed in previous translations. This method ensures that the translated version keeps the psychometric properties of the original questionnaire, which is essential for the interpretability of findings from cross-cultural studies using different versions of the same tool.
To address this gap, in this study, we conducted translation and cross-validation of the CAPE-42 to Hebrew. Our aims were to (1) validate the CAPE-42 in the Hebrew language, (2) assess the validity of the new tool using various convergence analyses, and (3) demonstrate how the questionnaire can be used to assess co-occurence and interaction between PEs and other clinical spectra. To these ends, we performed translation and back-translation of the CAPE-42. Following the translation, we used an online version of the questionnaire to collect a large sample of the Hebrew-speaking population in Israel. Cross-validation analysis showed an overall very good internal consistency of the Hebrew version. Additionally, there was a strong association between the dimensions of the CAPE-42 and other scales measuring similar constructs. Finally, we demonstrated the suitability of the CAPE-42 to investigate the association between autistic and psychotic traits with depressive symptoms.
2 Methods
2.1 Participants
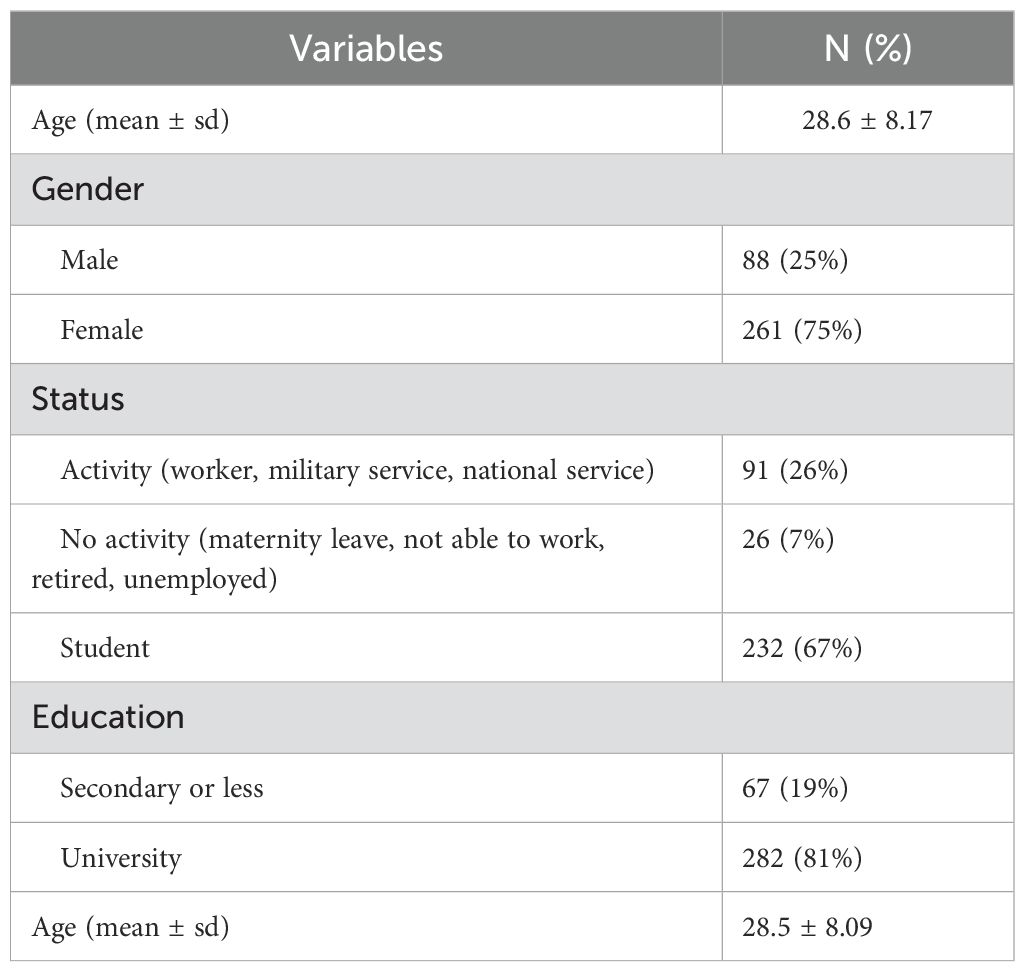
In total, 359 Israeli participated in the study. The mean age of the remaining sample (N= 349) was m = 28.6 years, sd = 8.19, and 75% were females. Demographic characteristics are displayed in Table 1. To participate in this study, participants were required to hold Israeli citizenship, reside in Israel, and be native Hebrew speakers. Using the Google Form restrictions, we ensured that subjects participated only once in the study. They all received monetary compensation, either as a 20 shekels gift card or in cash, and digital consent was obtained from all participants. Based on ethnicity questions, we excluded 10 participants who were unlikely to be native Hebrew speakers. The study protocol was approved by an Ethics Committee of the University of Haifa (046/20) according to the latest version of the Declaration of Helsinki (42).
2.2 Measurements
All demographic questions and clinical questionnaires were presented and answered in Hebrew.
2.2.1 Demographic questionnaire
The first part of the survey consisted of demographic questions evaluating various aspects of the participants’ lives. Categories included age, sex/gender (participants reported the same information for both gender and sex), ethnicity, religiosity, education, professional activity, socio-economical background, personal and family history for neurodevelopmental conditions and physical disorders, physical activities, hobbies, and interests.
2.2.2 Community Assessment of Psychic Experiences (CAPE-42)
The CAPE-42 is a questionnaire consisting of 42 items designed to assess a spectrum of psychotic experiences, encompassing positive, negative, and depressive dimensions. The positive dimension evaluates symptoms adding to the participant’s experiences (e.g., delusions) through 20 items (see Supplementary Table 1 for item details). The negative dimension evaluates symptoms characterized by the loss of typical behavior (e.g., avolition) through 14 items. Finally, the depressive dimension is assessed through eight items. Participants rate the frequency of their experiences on a scale from 1 (never) to 4 (nearly always), which sums to a total score ranging from 42 to 168. We used the translation/back-translation method to adapt the questionnaire into Hebrew. Initially, a native Hebrew speaker proficient in English translated the questionnaire from English to Hebrew. Subsequently, a native English speaker proficient in Hebrew performed the back-translation from Hebrew to English. Discrepancies between the two English versions were addressed by four researchers, comprising both native Hebrew and English speakers, and adjustments were made to the Hebrew version accordingly. The distribution of responses to each item is provided in Supplementary Table 2, and the Hebrew version of the CAPE-42 is provided in the Supplementary Material, Appendix A.
2.2.3 Autism Spectrum Quotient (AQ-50)
The AQ questionnaire is a self-report tool designed to measure autistic traits in both general and clinical populations (43). It comprises 50 items organized into five dimensions (of 10 items each) of the autistic spectrum: social skills, attention to detail, attention switch, communication, and imagination. Each item is a statement, that participants respond to by indicating their level of agreement on a 4-point scale ranging from “definitely disagree” to “definitely agree”. Each item is scored as 0 or 1 based on agree/disagree, resulting in a total autistic quotient ranging from 0 to 50.
2.2.4 Center for Epidemiologic Studies (CES-D)
The CES-D is a widely used self-report questionnaire designed to assess depressive symptoms in the general population (44), and is commonly used in research and clinical settings to screen for depressive symptoms and monitor changes in depression severity over time. It consists of 20 items covering various aspects of depression, including sadness, feelings of guilt, or sleep disturbance. Participants rate the frequency of their experiences over the past week on a 4-point scale ranging from “rarely or none of the time” to “most or all the time”. The items are scored from 0 to 4 and summed to obtain a total score, which ranges from 0 to 60.
2.2.5 Prodromal Questionnaire — Brief Version (PQ-B)
The PQ-B questionnaire is a brief version of the 92-item Prodromal Questionnaire, a screening tool developed to evaluate symptoms indicative of the prodromal phase of psychosis, intending to identify individuals at high risk of developing psychotic disorders such as schizophrenia (45, 46). This short version retains 21 items assessing positive symptoms commonly observed in the prodromal phase. Participants respond to questions regarding personal experiences, indicating whether they have experienced each symptom and, if so, the extent to which these experiences have caused distress or impairment. Responses are scored on a 5-point Likert scale ranging from “strongly disagree” to “strongly agree”. Items answered “no” receive a score of 0, while those answered “yes” are scored from 1 to 5 based on the perceived impact of the experience. The total score is calculated as the sum of scores for all items, resulting in a score ranging from 0 to 105.
2.3 Procedures
The data were collected using a Google Form link between June and October 2023. After obtaining the digital consent, participants were informed about the study’s purpose (i.e., “to learn about certain aspects and experiences in your life”). They were assured of the questionnaire’s anonymity and encouraged to respond spontaneously without overthinking. The survey comprised 28 demographic questions, 50 questions from the AQ, 42 from the CAPE-42, 20 from the CES-D, and 21 from the PQ-B. An attentional check question was presented for every 30 items, and all participants succeeded in this task. Overall, participants answered 166 questions, which took approximately 30 minutes.
2.4 Data analyses
All analyses were executed in Rstudio version 4.3.2.
2.4.1 Preliminary analyses
We calculated the means and standard deviations of all assessed scales and the subscales of the CAPE-42 for the overall sample and by gender.
2.4.2 Confirmatory Factor Analysis (CFA)
The CFA was employed to evaluate the underlying structure of the variables set by examining the relationship between items and pre-defined latent factors. Employing the maximum likelihood method, we computed three parameters estimating the discrepancy between the observed covariance matrix and the model-implied covariance matrix. First, normed model chi-square () values below 3 indicated a good fit, between 3 and 5 an acceptable fit, and above 5 a mediocre fit. Second, Steiger-Linod Root Mean Square Error of Approximation (RMSEA) values below 0.06 indicate a good fit, and between 0.08 and 0.1 an acceptable fit. Third, Standardized Root Mean Square Residual (SRMR) values below 0.08 indicated a good fit and between 0.08 and 0.1 an acceptable fit. Additionally, CFA enabled the estimation of parameters by comparing the fit of the proposed model to a null or baseline model where variables were uncorrelated, namely the Tucker-Lewis index (TLI) and the Comparative Fit Index (CFI). For both estimates, values above 0.90 showed a good fit, and values between 0.90 and 0.85 showed an acceptable fit (47).
We conducted a CFA on the eight-factor (first-order) model on the CAPE (i.e., depressive, social withdrawal, affective flattening, avolition, bizarre experiences, perceptual abnormalities, persecutory ideation, and magical thinking (33)), and a CFA of the three original factors that were added to the model as second-order factors (29). In this last model, the factor negative dimension included social withdrawal, affective flattening, and avolition, and the positive dimension included bizarre experiences, perceptual abnormalities, persecutory ideation, and magical thinking.
2.4.3 Reliability
We used two main coefficients, the Cronbach’s α and McDonald’s ω, to assess the composite reliability of the translated version of the CAPE-42. Cronbach’s α is widely used to measure the internal consistency, by assessing the degree to which items within the instrument are interrelated (48, 49). However, because this coefficient may be influenced by both common and unique variances among items, which can lead to overestimated or underestimated reliability (50, 51), we also calculated omega (52), a more accurate assessment of reliability in tools involving multidimensionality as in the CAPE-42 (53, 54). A commonly accepted threshold for satisfactory reliability is 0.70 or higher. The omega and alpha coefficients indicated a very good reliability for the AQ (ω = 0.79, α = 0.81), CES-D (ω = 0.95, α = 0.93), and PQ-B (ω = 0.90, α = 0.88).
2.4.4 Convergence and predictive score
To evaluate the convergent validity of the translated version of the CAPE-42 in Hebrew, we estimated the convergence between subscales and other scores supposedly evaluating the same constructs. Here, the convergence was evaluated between the positive symptoms scores with the score derived from the PQ-B, and the depressive score with the score derived from the CES-D, using Pearson’s correlation. In addition, we evaluated the predictive validity of the translated CAPE-42 by calculating the Pearson’s correlation coefficient with the AQ and CES-D. The objective was to identify correlations that align with existing literature, providing a benchmark for expected associations between specific subscales of the CAPE-42 and corresponding dimensions of the AQ and CES-D (7). Correlations with values less than 0.10 were categorized as very weak, between 0.10 and 0.30 as weak, between 0.30 and 0.50 as moderate, between 0.50 and 0.70 as strong, and above 0.70 as very strong (55).
2.4.5 Gender invariance
Finally, to ensure that the translated version of the CAPE-42 was free from gender bias, we rigorously examined gender invariance as part of the validation process. By conducting independent t-tests, we aimed to identify potential gender-related variations in the scores.
2.4.6 Predictive model
There is a complex interplay between psychotic experiences and autistic traits in relation to depressive symptoms (7, 22). Previous studies mainly focused on the combined effect of autistic and positive psychotic traits. However, the revised diametric model suggests that the co-occurrence between autism and psychosis may manifest by an overlap between autistic and negative psychotic traits, highlighting the importance of including the negative psychotic subscale. Therefore, we aimed to elucidate how autistic, positive psychotic, and negative psychotic traits individually and synergistically influence depressive symptomatology by conducting a linear regression analysis that controlled for the potential confounding effect of Gender using the following model:
CES-D ∼ AQ + CAPEpos + CAPEpos × AQ + CAPEneg + CAPEneg × AQ + Gender.
2.4.7 Principal component analysis
We conducted a Principal Component Analysis (PCA) to identify the latent structure between the AQ and the CAPE-42. Here, we aimed to compare the extracted structure with previous findings that conducted similar analyses on the two scales (19, 59, 60) to assess whether the component pattern observed in our study aligns with those identified in other versions of the questionnaire. Furthermore, we aimed to use the extracted structure to test the diametrical model, a dominant view suggesting an opposition between positive psychotic and autistic traits (15, 16, 56, 57), and a co-occurrence between negative psychotic and autistic traits (19, 58). We conducted a PCA on the five subscales of the AQ and 7 subscales of the CAPE-42. The depressive subscale of the CAPE-42 was excluded from the analyses to compare the results with studies that performed a PCA between autistic and psychotic scales (19, 59, 60). To determine the principal components to retain we used the eigenvalue > 1 criterion. The analysis was performed using a correlation matrix rather than the covariance matrix to standardize the variance of the variables and we did not apply any rotations to the components, similar to Nenadić et al. (19). To adjust for potential sample error-induced inflation of eigenvalues, we conducted Horn’s parallel analysis. Here, we expected a common latent structure between factors measuring negative psychotic and autistic traits, and an opposite latent structure between factors evaluating positive psychotic and autistic traits.
2.4.8 Canonical correlation analysis
To further explore the nature of the association between the dimensions of psychotic and autistic traits, we performed Canonical Correlation Analysis (CCA) (61) on the subscales of the AQ and CAPE-42, excluding the depressive dimension of the CAPE-42. CCA is a multivariate technique that identifies linear combinations of variables (i.e., canonical variates, or CVs) from each set that maximize the shared variance between the two datasets. The strength of these relationships was assessed using the canonical correlation coefficient rc for each CV. Wilks’ lambda, a likelihood ratio test, was used to evaluate the statistical significance of the association between the canonical variates (62). In addition, we examined key parameters, including the eigenvalue, the cumulative explained variance, and the shared explained variance, indicating respectively the amount of variance explained by each CV, the variance accounted for by the most significant CVs, and the extent to which the variance in one set is explained by the variance in the other set. Canonical loadings and standardized coefficients were examined to interpret the magnitude and direction of the contributions of each variable (i.e., subscale) to the CV. We considered variables with canonical loadings greater than 0.3 (in absolute value), and greater than their contribution in other CV, to strongly contribute to the CV of interest (63). The analysis was performed with the R packages yacca and CCP.
3 Results
3.1 Preliminary analyses
Our sample scored on the CAPE-42 with a total mean of m = 72.36 (sd = 15.66), and with means of m = 30.11 (sd = 6.91), m = 26.71 (sd = 6.83), m = 15.55 (sd = 4.60) on the positive, negative, and depressive subscales, respectively. Notably, six participants (1.72%) scored above 50 on the positive subscale, surpassing this suggested cut-off value (64). The summary of scores for all measured scales is provided in Table 2.
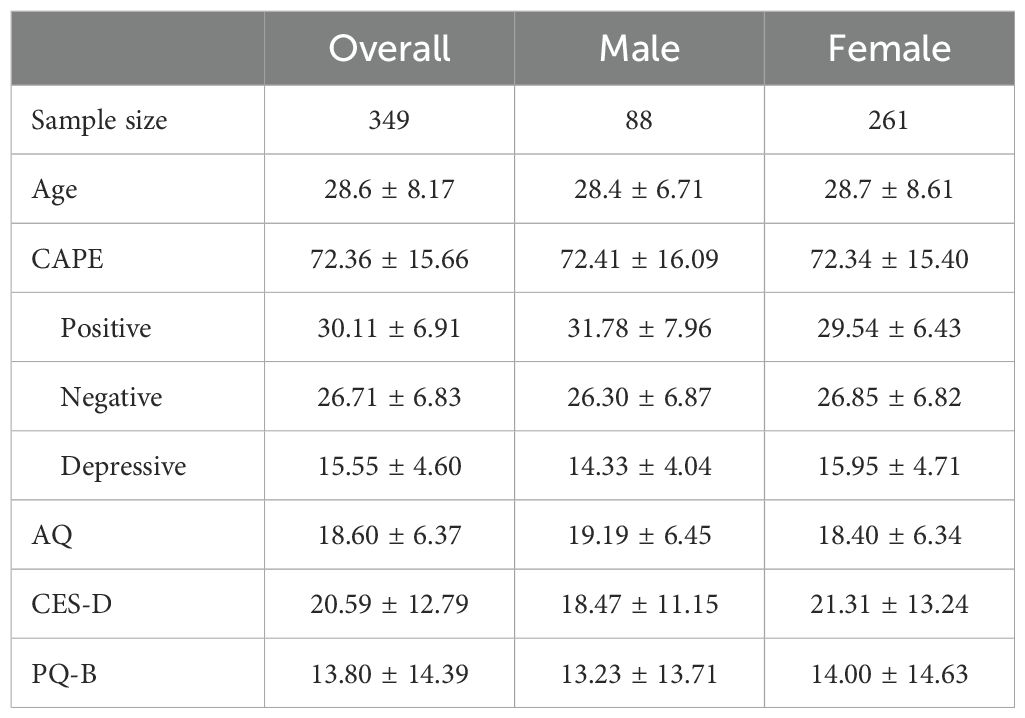
Table 2. Table summarizing the means and standard deviations for all assessed scales (CAPE-42, AQ, CES-D, PQ-B), and the subscales of the CAPE-42, presented for the overall sample and stratified by gender.
3.2 Confirmatory factor analysis
The CFA parameters of the eight-factor (first order) model of the CAPE indicated a fit from good (χ2/df = 1978.593/791 = 2.501, SRMR = 0.074, CFI = 0.804, and TLI = 0.787) to acceptable (RMSEA = 0.066 (90% CI 0.062 0.069)). The standardized estimates of factor loadings were adequate except for 6 items below 0.30 (Supplementary Table 1). The CFA fit of the eight-factor (first order) and the three-factor (second order) model showed a lesser good fit, with three parameters indicating a good fit (χ2/df = 2347.35/816 = 2.88, CFI = 0.748, TLI = 0.734, and two parameters indicating an acceptable fit (RMSEA = 0.073 (90% CI 0.070, 0.077), SRMR = 0.140). Furthermore, 24 items had factor loadings below the adequate threshold. With more parameters meeting the cutoff values indicating a good fit, and significantly more factor loadings being above the adequate threshold, we can conclude that the eight-factor model demonstrated the best fit for our data, consistent with the findings of Fekih‐Romdhane et al. (33) in their Arabic translation.
3.3 Reliability
The omega and alpha analyses revealed a general omega factor of ωg = 0.94, and an alpha coefficient of α = 0.93, indicating a high overall internal consistency. We subsequently calculated the internal consistency of each factor, revealing robust reliability for seven of the eight factors: Depressive (ωg = 0.90, α = 0.87), social withdrawal (ωg = 0.56, α = 0.55), affective flattening (ωg = 0.71, α = 0.70), avolition (ωg = 0.86, α = 0.82), bizarre experiment (ωg = 0.85, α = 0.75), perceptual abnormalities (ωg = 0.79, α = 0.74), persecutory ideation (ωg = 0.79, α = 0.71), and magical thinking (ωg = 0.70, α = 0.63). To investigate the low reliability in the social withdrawal factor, we calculated the mean of inter-item correlation between the items included in the subscale. The mean inter-item correlation (mr = 0.29) was within the adequate range (0.15 < mr < 0.5, with mr < 0.15 indicating that the items do not measure the same construct, and mr > 0.50, indicating that the questions are too similar/redundant (65)). In the future, incorporating additional questions might be considered to improve the sensitivity of this dimension and to capture better the inter-individual variability. Overall, these results confirm that the Hebrew CAPE-42 has very good overall and subscale-level internal consistencies.
3.4 Convergence and predictive scores
Convergence of the CAPE-42 were evaluated using correlation analyses between the PQ-B and CES-D with the two subscales of the CAPE-42 measuring similar constructs. The correlation between the positive dimension of the CAPE-42 and the PQ-B, r(347) = 0.64, p <.001, and between the depressive dimension of the CAPE-42 and the CES-D score, r(347) = 0.81, p <.001, were very strong. The expected correlation between positive psychotic traits and autistic traits (7) was moderate, r(347) = 0.32, p <.001. The correlation matrix between the scores of the subscales of the CAPE-42 with the other measures is displayed in Table 3. These correlation coefficients show a close association between the dimensions and subscales of the CAPE-42 with scales evaluating similar constructs, demonstrating a robust convergent validity for the translated CAPE-42.
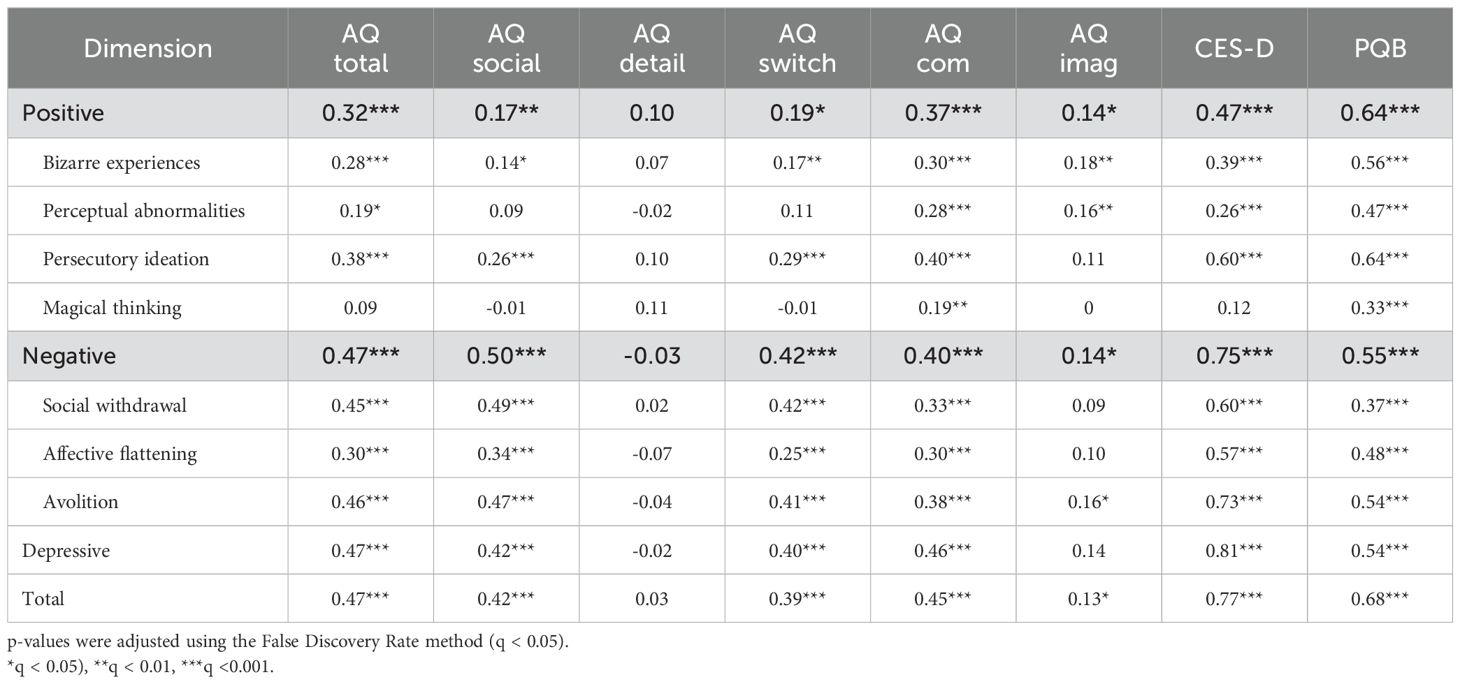
Table 3. Table of correlation coefficients (r values) between dimensions of the CAPE-42 with other total and dimensional measures.
3.5 Gender invariance
The unpaired t-tests (Table 4) revealed no significant difference between males and females in the total score of the CAPE-42 after applying FDR corrections (q represents the corrected p-values), t(145.52) = 0.03, q = 0.974, the negative dimension, t(148.93) = 0.65, q = 0.708 and the positive dimension, t(127.45) = 2.39, p = 0.070. However, significant gender differences were observed in two subscales of the positive dimension, bizarre experiences, t(125.59) = 2.83, q = 0.020, and perceptual abnormalities, t(114.51) = 3.19, q = 0.011, where males showed significantly higher scores. Moreover, we found a difference in the depressive dimension, with females exhibiting a significantly higher score than males, t(173.06) = 3.13, q = .011, consistent with Fekih-Romdhane et al. (33). These results indicate that the Hebrew CAPE-42 does not generate gender biases and captures only the gender-based disparity in depressive traits within psychotic conditions (66).
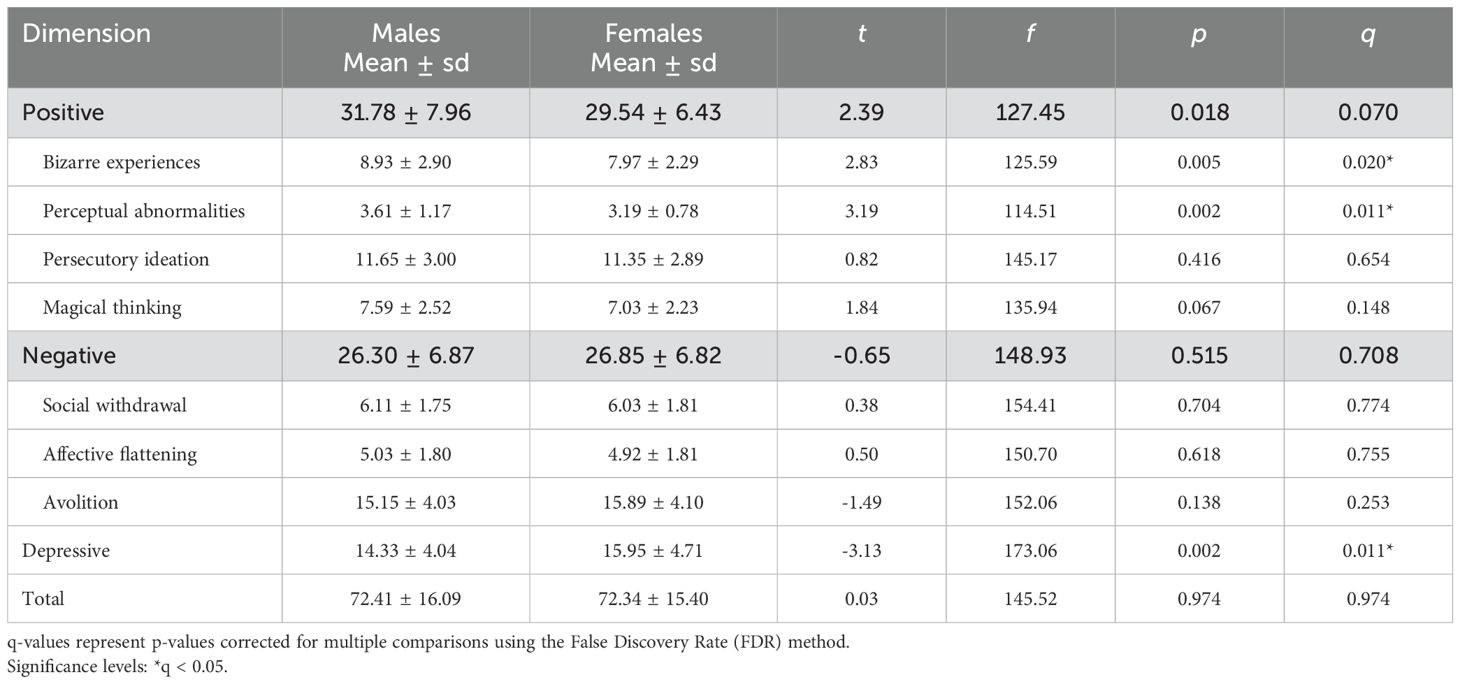
Table 4. Table displaying results of t-tests analyzing the differences between gender in the dimensions and the total score of the CAPE-42.
3.6 Predictive model
A linear regression analysis was conducted to investigate the independent effects of AQ, CAPE positive, CAPE negative, and the interaction between AQ and CAPE positive and between AQ and CAPE negative on the CES-D score, while controlling for Gender. The regression model was statistically significant and explained approximately 59.30% of the variance of the CES-D score (F(6, 342) = 83.04, p <.001, adjusted R² = .586). The results indicate that the AQ score (B = 2.12, se = 0.51, t = 4.17, p <.001), the CAPE positive score (B = 1.18, se = 0.59, t = 1.98, p = .049), and the CAPE negative score (B = 8.15, se = 0.60, t = 13.68, p <.001) were significant positive predictors of the CES-D score. The variable Gender (male) was a significant negative predictor (B = -2.85, se = 1.04, t = -2.74, p = .007). The interaction between AQ and CAPE positive scores (B = 0.34, se = 0.59, t = 0.59, p = .558), as well as the interaction between AQ and CAPE negative scores (B = -0.89, se = 0.51, t = -1.76, p = .079) were not significant. These findings suggest that autistic, positive and negative psychotic traits independently contribute to depressive symptoms. Furthermore, the results are consistent with the gender invariance analysis, confirming that participants’ gender is a predictor of depressive symptoms.
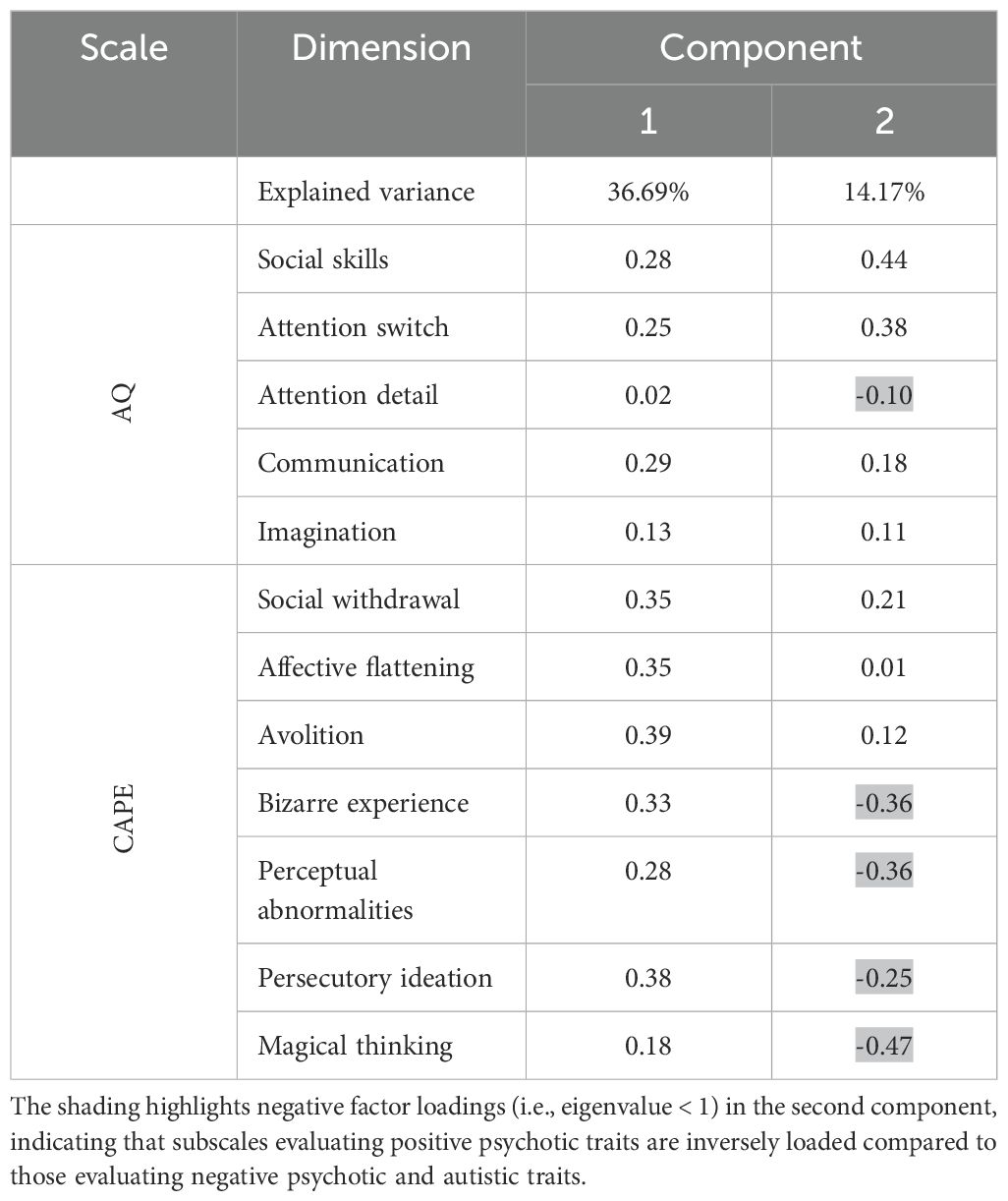
3.7 Principal component analysis
The PCA of the AQ and the CAPE-42 subscales identified four principal components. Two principal components were retained after correcting for sample error-induced inflation of eigenvalues, using Horn’s parallel analysis (see Figure 1 for factor loadings in the two retained principal components, and Supplementary Table 3 for the factor loadings in the four original principal components). The first principal component explained 36.69% of the variance (m = 36.69, sd = 2.10) and the second accounted for 14.17% (m = 14.17, sd = 1.70), together, totaling 50.86% of the variance. All factors positively loaded on the first component. However, we observed a diametric structure in the second component between subscales measuring negative psychotic and autistic traits, and positive psychotic traits. Factors related to autistic traits (i.e., social skills, attention switch, communication, imagination) and negative psychotic traits (i.e., avolition and social withdrawal) showed positive loadings, while factors associated with positive psychotic traits (i.e., persecutory ideation, magical thinking, bizarre experience, perceptual abnormality), and attention to detail showed negative loadings (see Table 5).
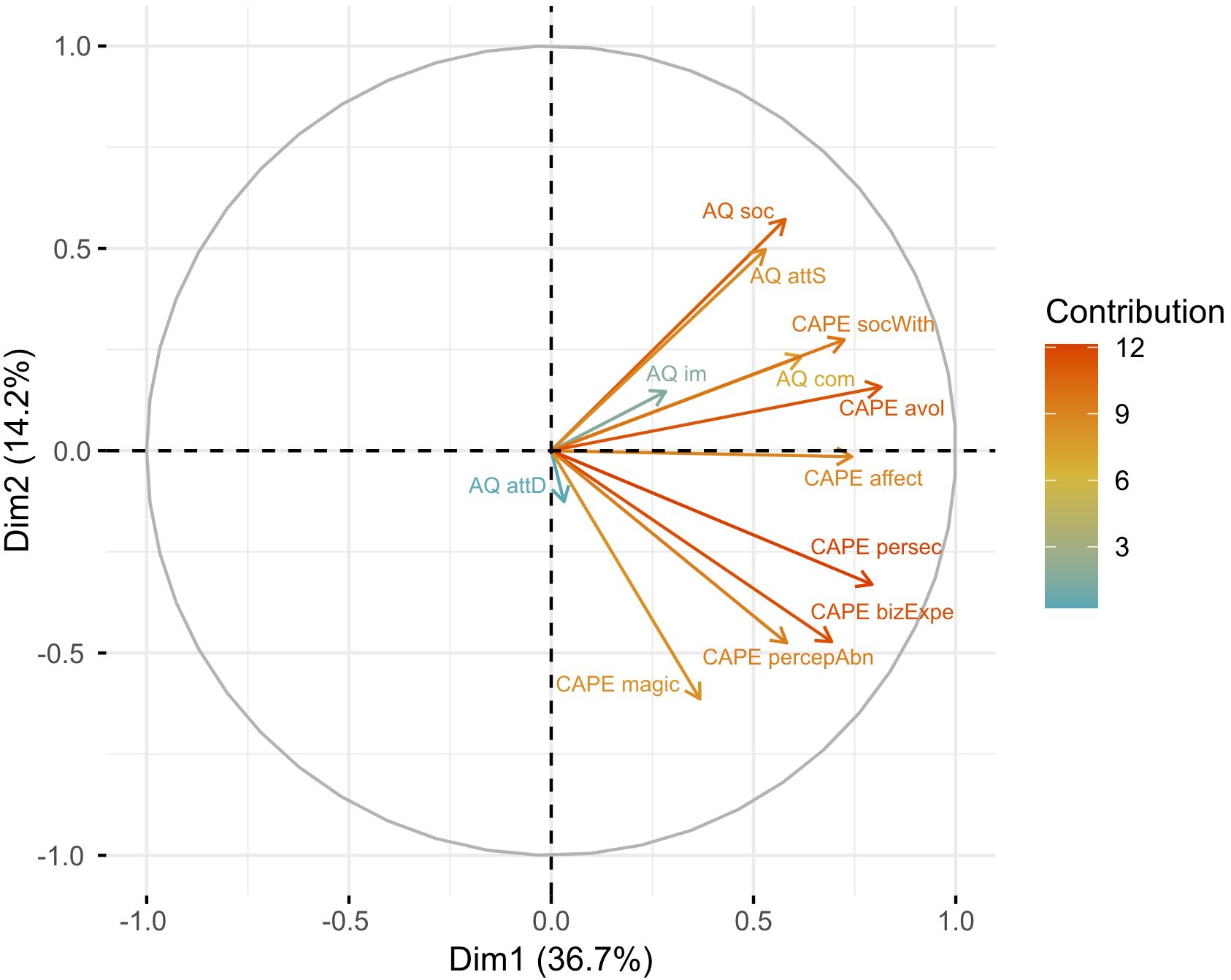
Figure 1. Visualization of the PCA illustrating the contribution of seven factors from the CAPE-42 and five factors from the AQ to the two principal components extracted. The position along the axes indicates the extent to which a variable aligns with the patterns of variation captured by the first (x-axis) and the second (y-axis) components. The results indicate that most AQ subscales and two subscales of the CAPE-42 measuring negative symptoms (i.e., avolition and social withdrawal) have opposite loadings (i.e., positive values in Dimension 2) to the positive subscales of the CAPE-42 and the attention to detail subscale of the AQ (i.e., negative values in Dimension 2). The affective flattening from the negative dimension of the CAPE-42 effectively has no contribution to the second factor (value = 0.01). This demonstrates a diametric structure between dimensions evaluating negative psychotic and autistic traits, on the one hand, and positive psychotic experiences on the other.
The associations between the AQ and CAPE-42 subscales identified through the CCA closely reflected the component structure revealed by the PCA. Therefore, the results of the CCA are presented in Supplementary results and Supplementary Tables 4, 5.
4 Discussion
The primary aim of this study was to examine the psychometric properties of the Hebrew translation of the CAPE-42 in a sample of Hebrew-speaking adults from the general population in Israel.
We systematically translated and validated the CAPE-42 using the translation/back-translation method, and its association with the AQ, CES-D, and PQ-B. Overall, participants’ scores were consistent with those reported in the literature (35, 37, 38, 67), and only six participants (1.72%) exceeded the suggested cut-off value. This suggests that our sample included a small proportion of participants with elevated psychotic traits, indicating a higher risk for psychotic-related disorders. Alpha and omega reliability coefficients supported high internal consistency within the overall questionnaire and all factors, except social withdrawal. However, since reliability measures are not fully suitable for inter-item correlations with less than 10 items, the mean inter-item correlation of the social withdrawal subscale demonstrated good internal consistency despite the low reliability scores. The CFA indicated that the eight-factor model (33) fits our data better than the original structure proposed by Stefanis et al. (29), which adds the three original dimensions as a second-order factor. These findings suggest that the three dimensions might obscure the variability within and between individual experiences when modeling PEs. In contrast, the eight-factor model provides a more nuanced representation of the internal structure, reflecting better the multifactorial nature of psychosis and PEs. Therefore, we recommend using the subscale scores for research and deep phenotyping.
Furthermore, gender analysis showed no evidence for a gender-biased translation, with gender differences only appearing in dimensions consistent with previous findings, such as the depressive dimension. Finally, we conducted a predictive model to evaluate the contribution of autistic (i.e., AQ) and psychotic (i.e., CAPE positive and negative) traits to depressive scores (i.e., CES-D), while controlling for gender. The results showed that autistic and psychotic traits independently predict higher depression scores, while the male gender was a negative predictor.
We found strong correlations between dimensions of the CAPE-42 and other scales measuring similar constructs, supporting the validation of the new tool. We also found a moderate correlation between the positive dimension of the CAPE-42 and autistic traits. This moderate correlation contributes to the current ongoing debate regarding the association between autistic and psychotic traits. Previous research has produced mixed results; some studies found no correlation between these traits (68, 69), others reported a negative correlation (56, 58), and some a positive correlation (70, 71). Additionally, the PCA results, indicating an opposite loading of factors measuring autistic and negative psychotic traits, and positive psychotic traits, are aligned with previous research investigating the structure of tools evaluating autistic and psychotic traits (19, 59). These findings support the diametric model (15, 16, 56, 57), which places autism and psychosis at opposite ends of a single spectrum, as well as the revised diametrical model (19, 58), which suggests that while negative psychotic and autistic traits overlap, positive psychotic traits oppose autistic traits.
Moreover, these results indicate that investigating the overlap between the two conditions provides a valuable framework for understanding their comorbidity. Evidence indicates that individuals with autism have an increased risk of developing psychosis, and vice versa (72, 73). While these findings are generally attributed to shared genetic (74–76) and neurobiological factors (77, 78), the symptom overlap between the two conditions may also play a role (79). However, distinguishing overlapping symptoms from clinical comorbidity remains challenging due to the limitations in current diagnostic tools, potentially leading to mis- or underdiagnosis. Indeed, we believe that measuring autistic traits/symptoms in psychosis, and vice versa, requires tools specifically designed for the clinical populations, by considering the overlapping symptoms, as well as possible differences in the expression of symptoms due to the co-occurrence (80, 81).
This study provides a significant and reliable tool for research and clinical purposes in assessing PEs and related disorders within the Hebrew-speaking population. In the future, this adapted questionnaire will allow for the screening of psychotic experiences in both non-clinical and clinical populations, which in turn will aid in the understanding of the deep phenotyping of psychotic disorders, and identifying traits that may serve as early indicators of clinical conditions. Additionally, this tool will help to explore the implication of PEs in other clinical conditions, either as protective, aggravating factors, or comorbidity. For example, our research provides insight into the independent effect of autistic and psychotic traits on depressive symptoms (7, 22). While comorbidity in clinical conditions typically exacerbates depressive symptoms (82), our findings suggest that there is no enhancement of depressive symptoms from the interaction between autistic and positive psychotic traits. Nonetheless, this contributes to the growing body of research supporting the need to examine the interaction between trait dimensions in order to better understand their combined impact on outcomes (7, 71, 83).
Finally, this research provides a valuable tool that can be integrated into cross-cultural studies, crucial for understanding variations in PEs across different cultures and the implication of the cultural factor in symptom modulation. Studies have shown a higher frequency of PEs among minority groups living in Western countries (23–25, 84). Identifying the risk factors that contribute to differences in the prevalence of psychotic disorders is essential for adapting diagnosis tools (85) and improving patient rehabilitations, though their investigation represents significant challenges. Differences in prevalence may be influenced by genetic, cultural, or social-environmental factors. Previous research that investigated population differences based on countries’ socioeconomic status yielded inconsistent results. For example, some studies found a higher frequency of PEs is middle/high-income countries (26), while others found higher frequencies in low/middle-income countries, with greater distress level reported in high-income countries (27). Another challenge in cross-cultural studies is the variation in the expressions of the PEs, which can be influenced by religious beliefs, help-seeking behavior, and societal stigmatization (86). Therefore, the CAPE-42 in Hebrew will enable the inclusion of the Hebrew-speaking population in cross-cultural studies, a relevant population to disentangle some genetic, cultural, and social-environmental risk factors due to some unique characteristics of the Hebrew-speaking population in Israel (e.g., high-income country, local and global geopolitical conflict, Semitic culture, inter-generational history, and diverse genetic origins [e.g., European Middle-Eastern, North-African, Ethiopian]).
4.1 Study limitations
Here, we validated the CAPE-42 in Hebrew over a restricted population (i.e., primarily students, and 75% of females). As such, the sample may not fully represent the general population, which could limit the generalization of our findings. However, it is important to highlight that the demographic items revealed significant diversity within our sample (e.g., salary, religiosity, marital situation, and geographic area of residence).
Furthermore, the sample is only from a non-clinical population. However, a screening tool must distinguish between clinical and non-clinical individuals, and accurately assess psychotic experiences within the clinical population. This is particularly challenging for conditions like psychotic disorders where the main symptoms, such as delusions, can affect self-awareness. Therefore, the tool must be validated on both groups to evaluate additional psychometric properties, such as the sensitivity, specificity, and cutoff value. To our knowledge, only Boonstra et al. (64) measured these psychometric characteristics, proposing a cutoff of 50 on the positive dimension, which results in a sensitivity of 77% and specificity of 71%. While our findings show that the tool demonstrated good reliability in the non-clinical population, its validity within the clinical population should be tested in future research. Moreover, the tool’s validation could have benefited from gold-standard clinical interviews to control for potential biases associated with self-report tools (e.g., social desirability, variability in the understanding of the questions).
5 Conclusions
The properties of the CAPE-42 make it a crucial tool for evaluating PEs in both research and clinical environments. This study, following a rigorous translation and validation procedure, provides a validated version of the questionnaire, with high psychometric qualities, for the Hebrew-speaking population. This tool is essential for screening PEs in both clinical and non-clinical populations in the perspective of a better understanding of the phenotype and early signs of psychotic disorders, and the comorbidity and interactions with other conditions. Furthermore, it could be employed to investigate cross-cultural differences in the expression of PEs, a recent lead that could provide insights into the implications of culture and environment on the manifestations of PEs.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://osf.io/kwjyr/?view_only=a2a1272052c64ed0b1da262f0bacef06.
Ethics statement
The study involving humans was approved by th Ethics Committee of the University of Haifa (046/20). The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LF: Data curation, Formal Analysis, Visualization, Writing – original draft. AA: Conceptualization, Formal Analysis, Methodology, Supervision, Validation, Visualization, Writing – review & editing. BH: Conceptualization, Methodology, Validation, Writing – review & editing. AY: Conceptualization, Methodology, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. We would like to thank our funding sources: the Israel Science Foundation (Grant No. 1980/18 to AY), the Binational Science Foundation (Grant No. 2020234 to B-SH), and the Maof Fellowship for the Integration of Outstanding Faculty, Council for Higher Education (2023–2025, to AA-A).
Acknowledgments
We would like to thank Marissa Hartston and Miriam Ziv for their valuable contributions in the translation/back-translation procedure.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1548310/full#supplementary-material
References
1. Linscott RJ, Van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: On the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. (2013) 43:1133–49. doi: 10.1017/S0033291712001626
2. Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: A 15-year longitudinal study. Arch Gen Psychiatry. (2000) 57:1053–8. doi: 10.1001/archpsyc.57.11.1053
3. Johns LC, Van Os J. The continuity of psychotic experiences in the general population. Clin Psychol Rev. (2001) 21:1125–41. doi: 10.1016/S0272-7358(01)00103-9
4. Welham J, Scott J, Williams G, Najman J, Bor W, O’Callaghan M, et al. Emotional and behavioural antecedents of young adults who screen positive for non-affective psychosis: A 21-year birth cohort study. Psychol Med. (2009) 39:625–34. doi: 10.1017/S0033291708003760
5. Kelleher I, Cannon M. Psychotic-like experiences in the general population: Characterizing a high-risk group for psychosis. Psychol Med. (2011) 41:1–6. doi: 10.1017/S0033291710001005
6. Healy C, Brannigan R, Dooley N, Coughlan H, Clarke M, Kelleher I, et al. Childhood and adolescent psychotic experiences and risk of mental disorder: A systematic review and meta-analysis. Psychol Med. (2019) 49:1589–99. doi: 10.1017/S0033291719000485
7. Sampson KN, Upthegrove R, Abu-Akel A, Haque S, Wood SJ, Reniers R. Co-occurrence of autistic and psychotic traits: Implications for depression, self-harm and suicidality. Psychol Med. (2021) 51:1364–72. doi: 10.1017/S0033291720000124
8. Birkenæs V, Refsum Bakken N, Frei E, Jaholkowski P, Smeland OB, Tesfaye M, et al. Psychometric properties and diagnostic associations of the short-form Community Assessment of Psychic Experiences in a population-based sample of 29–021 adult men. Schizophr Bull. (2023) 49(5):1229–38. doi: 10.1093/schbul/sbad074
9. Polanczyk G, Moffitt TE, Arseneault L, Cannon M, Ambler A, Keefe RSE, et al. Etiological and clinical features of childhood psychotic symptoms: results from a birth cohort. Arch Gen Psychiatry. (2010) 67:328. doi: 10.1001/archgenpsychiatry.2010.14
10. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th edition. Arlington, VA: American Psychiatric Association (2022).
11. Chisholm K, Lin A, Abu-Akel A, Wood SJ. The association between autism and schizophrenia spectrum disorders: A review of eight alternate models of co-occurrence. Neurosci Biobehav Rev. (2015) 55:173–83. doi: 10.1016/j.neubiorev.2015.04.012
12. Carroll LS, Owen MJ. Genetic overlap between autism, schizophrenia and bipolar disorder. Genome Med. (2009) 1:102. doi: 10.1186/gm102
13. Stone WS, Iguchi L. Do apparent overlaps between schizophrenia and autistic spectrum disorders reflect superficial similarities or etiological commonalities? Am Chin J Med Sci. (2011) 4:124. doi: 10.7156/v4i3p124
14. Jutla A, Foss-Feig J, Veenstra-VanderWeele J. Autism spectrum disorder and schizophrenia: An updated conceptual review. Autism Res. (2022) 15:384–412. doi: 10.1002/aur.2659
15. Abu-Akel A, Bailey AL. The possibility of different forms of theory of mind impairment in psychiatric and developmental disorders. Psychol Med. (2000) 30:735–8. doi: 10.1017/S0033291799002123
16. Crespi B, Badcock C. Psychosis and autism as diametrical disorders of the social brain. Behav Brain Sci. (2008) 31:241–61. doi: 10.1017/S0140525X08004214
17. Abu-Akel A. Genetic variations in the SNP rs850807 reflect a trade-off between autism and paranoia symptom expressions: a comment on Crespi et al., 2018. Biol Lett. (2018) 14:20180108. doi: 10.1098/rsbl.2018.0108
18. Crespi B, Stead P, Elliot M. Comparative genomics of autism and schizophrenia. Proc Natl Acad Sci. (2010) 107:1736–41. doi: 10.1073/pnas.0906080106
19. Nenadić I, Meller T, Evermann U, Schmitt S, Pfarr J-K, Abu-Akel A, et al. Subclinical schizotypal vs. autistic traits show overlapping and diametrically opposed facets in a non-clinical population. Schizophr Res. (2021) 231:32–41. doi: 10.1016/j.schres.2021.02.018
20. Shi Z, Theisinger LA, Allenmark F, Pistorius RL, Müller HJ, Falter-Wagner CM. Predictive coding in ASD: inflexible weighting of prediction errors when switching from stable to volatile environments. Neuroscience. (2022). doi: 10.1101/2022.01.21.477218
21. Abu-Akel AM, Wood SJ, Hansen PC, Apperly IA. Perspective-taking abilities in the balance between autism tendencies and psychosis proneness. Proc R Soc B Biol Sci. (2015) 282:20150563. doi: 10.1098/rspb.2015.0563
22. Upthegrove R, Abu-Akel A, Chisholm K, Lin A, Zahid S, Pelton M, et al. Autism and psychosis: Clinical implications for depression and suicide. Schizophr Res. (2018) 195:80–5. doi: 10.1016/j.schres.2017.08.028
23. Johns LC, Nazroo JY, Bebbington P, Kuipers E. Occurrence of hallucinatory experiences in a community sample and ethnic variations. Br J Psychiatry. (2002) 180:174–8. doi: 10.1192/bjp.180.2.174
24. Fearon P, Kirkbride JB, Morgan C, Dazzan P, Morgan K, Lloyd T, et al. Incidence of schizophrenia and other psychoses in ethnic minority groups: Results from the MRC AESOP Study. Psychol Med. (2006) 36:1541–50. doi: 10.1017/S0033291706008774
25. Laurens KR, West SA, Murray RM, Hodgins S. Psychotic-like experiences and other antecedents of schizophrenia in children aged 9–12 years: A comparison of ethnic and migrant groups in the United Kingdom. Psychol Med. (2008) 38:1103–11. doi: 10.1017/S0033291707001845
26. McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: A cross-national analysis based on 31–261 respondents from 18 countries. JAMA Psychiatry. (2015) 72:697–705. doi: 10.1001/jamapsychiatry.2015.0575
27. Vermeiden M, Janssens M, Thewissen V, Akinsola E, Peeters S, Reijnders J, et al. Cultural differences in positive psychotic experiences assessed with the Community Assessment of Psychic Experiences-42 (CAPE-42): A comparison of student populations in the Netherlands, Nigeria and Norway. BMC Psychiatry. (2019) 19:1–15. doi: 10.1186/s12888-019-2210-8
28. Wüsten C, Schlier B, Jaya ES, Fonseca-Pedrero E, Peters E, Verdoux H, et al. Psychotic experiences and related distress: A cross-national comparison and network analysis based on 7141 participants from 13 countries. Schizophr Bull. (2018) 44:1185–94. doi: 10.1093/schbul/sby087
29. Stefanis NC, Hanssen M, Smirnis NK, Avramopoulos DA, Evdokimidis IK, Stefanis CN, et al. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. (2002) 32:347–58. doi: 10.1017/S0033291701005141
30. Loewy RL, Stuart B, Schlosser D, Vinogradov S, Cannon TD. Prodromal psychosis screening with the Prodromal Questionnaire-Brief version (PQ-B). In: Early Interv Psychiatry. Wiley-Blackwell Publishing, Inc, COMMERCE PLACE, 350 MAIN ST, MALDEN 02148: MA USA (2008). p. A40–0.
31. Raine A, Benishay D. The SPQ-B: A brief screening instrument for schizotypal personality disorder. J Pers Disord. (1995) 9:346–55. doi: 10.1521/pedi.1995.9.4.346
32. Mark W, Toulopoulou T. Psychometric properties of “community assessment of psychic experiences”: Review and meta-analyses. Schizophr Bull. (2016) 42:33–44. doi: 10.1093/schbul/sbv088
33. Fekih-Romdhane F, Farah N, Malaeb D, Cheour M, Obeid S, Hallit S. Validation of the Arabic version of the Community Assessment of Psychic Experiences (CAPE-42) in a large sample of young adults from the general population. Int J Ment Health Addict. (2023) 22(5):2649–66. doi: 10.1007/s11469-023-01011-3
34. Villacura-Herrera C, Pérez J, Jones PB, Núñez D. Internal consistency and temporal stability of the Community Assessment of Psychic Experiences (CAPE): A reliability generalization meta-analysis. Psychiatry Res. (2024) 338:115988. doi: 10.1016/j.psychres.2024.115988
35. Konings M, Bak M, Hanssen M, Van Os J, Krabbendam L. Validity and reliability of the CAPE: a self-report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr Scand. (2006) 114:55–61. doi: 10.1111/j.1600-0447.2005.00741.x
36. Armando M, Nelson B, Yung AR, Saba R, Monducci E, Dario C, et al. Psychotic experience subtypes, poor mental health status and help-seeking behaviour in a community sample of young adults. Early Interv Psychiatry. (2012) 6:300–8. doi: 10.1111/j.1751-7893.2011.00303.x
37. Barragan M, Laurens KR, Navarro JB, Obiols JE. Psychotic-like experiences and depressive symptoms in a community sample of adolescents. Eur Psychiatry. (2011) 26:396–401. doi: 10.1016/j.eurpsy.2010.12.007
38. Brenner K, Schmitz N, Pawliuk N, Fathalli F, Joober R, Ciampi A, et al. Validation of the English and French versions of the Community Assessment of Psychic Experiences (CAPE) with a Montreal community sample. Schizophr Res. (2007) 95:86–95. doi: 10.1016/j.schres.2007.06.017
39. Fonseca-Pedrero E, Paino M, Lemos-Giraldez S, Muniz J. Validation of the Community Assessment Psychic Experiences-42 (CAPE-42) in Spanish college students and patients with psychosis. Actas Esp Psiquiatr. (2012) 40:169–76.
40. Mirzaei Poueenak F, Ghanbari Pirkashani N, Nooripour R, Hosseini SR, Mazloomzadeh M, Shirkhani M. Psychometric validation of the Persian version of the community assessment of psychotic experiences-42 (CAPE-42) in Iranian college students. Psychosis. (2022) 14:81–92. doi: 10.1080/17522439.2020.1861075
41. Verdoux H, Sorbara F, Gindre C, Swendsen JD, Van Os J. Cannabis use and dimensions of psychosis in a nonclinical population of female subjects. Schizophr Res. (2003) 59:77–84. doi: 10.1016/S0920-9964(01)00401-7
42. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191. doi: 10.1001/jama.2013.281053
43. Baron-Cohen S, Wheelwright S, Skinner R, Martin J, Clubley E. The Autism-Spectrum Quotient (AQ): Evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. (2001) 31:5–17. doi: 10.1023/A:1005653411471
44. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
45. Loewy RL, Pearson R, Vinogradov S, Bearden CE, Cannon TD. Psychosis risk screening with the Prodromal Questionnaire — Brief Version (PQ-B). Schizophr Res. (2011) 129:42–6. doi: 10.1016/j.schres.2011.03.029
46. Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD. The prodromal questionnaire (PQ): Preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophr Res. (2005) 79:117–25. doi: 10.1016/j.schres.2005.03.007
47. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
48. Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrika. (1951) 16:297–334. doi: 10.1007/BF02310555
50. Raykov T, Marcoulides GA. Thanks coefficient alpha, we still need you! Educ Psychol Meas. (2019) 79:200–10. doi: 10.1177/0013164417725127
51. McNeish D. Thanks coefficient alpha, we’ll take it from here. Psychol Methods. (2018) 23:412–33. doi: 10.1037/met0000144
53. Dunn TJ, Baguley T, Brunsden V. From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. (2014) 105:399–412. doi: 10.1111/bjop.12046
54. Goodboy AK, Martin MM. Omega over alpha for reliability estimation of unidimensional communication measures. Ann Int Commun Assoc. (2020) 44:422–39. doi: 10.1080/23808985.2020.1846135
55. Cohen J. Quantitative methods in psychology: a power primer. Psychol Bull. (1992) 112:1155–9. doi: 10.1037//0033-2909.112.1.155
56. Crespi B, Dinsdale N. Autism and psychosis as diametrical disorders of embodiment. Evol Med Public Health. (2019) 1:121–38. doi: 10.1093/emph/eoz021
57. Abu-Akel A. Theory of mind in autism, schizophrenia, and in-between. Behav Brain Sci. (2008) 31:261–2. doi: 10.1017/S0140525X08004226
58. Zhou H, Yang H, Gong J, Cheung EFC, Gooding DC, Park S, et al. Revisiting the overlap between autistic and schizotypal traits in the non-clinical population using meta-analysis and network analysis. Schizophr Res. (2019) 212:6–14. doi: 10.1016/j.schres.2019.07.050
59. Dinsdale NL, Hurd PL, Wakabayashi A, Elliot M, Crespi BJ. How are autism and schizotypy related? Evidence from a non-clinical population. PLoS One. (2013) 8:e63316. doi: 10.1371/journal.pone.0063316
60. Del Giudice M, Klimczuk ACE, Traficonte DM, Maestripieri D. Autistic-like and schizotypal traits in a life history perspective: Diametrical associations with impulsivity, sensation seeking, and sociosexual behavior. Evol Hum Behav. (2014) 35:415–24. doi: 10.1016/j.evolhumbehav.2014.05.007
61. Hotelling H. Relations between two sets of variates. Biometrika. (1936) 28:321–77. doi: 10.1093/biomet/28.3-4.321
62. Bartlett MS. A note on tests of significance in multivariate analysis. Math Proc Camb Philos Soc. (1939) 35:180–5. doi: 10.1017/S0305004100020880
63. Lambert ZV, Durand RM. Some precautions in using canonical analysis. J Mark Res. (1975) 12:468–75. doi: 10.1177/002224377501200411
64. Boonstra N, Wunderink L, Sytema S, Wiersma D. Improving detection of first-episode psychosis by mental health-care services using a self-report questionnaire. Early Interv Psychiatry. (2009) 3:289–95. doi: 10.1111/j.1751-7893.2009.00147.x
65. Cohen R, Swerdlik M. Psychological testing and assessment. 6th ed. New York: McGraw Hill (2005).
66. Barajas A, Ochoa S, Obiols JE, Lalucat-Jo L. Gender differences in individuals at high risk of psychosis: A comprehensive literature review. Sci World J. (2015) 2015:430735. doi: 10.1155/2015/430735
67. Ziermans TB, Schirmbeck F, Oosterwijk F, Geurts HM, De Haan L, Genetic Risk and Outcome of Psychosis (GROUP) Investigators. Autistic traits in psychotic disorders: prevalence, familial risk, and impact on social functioning. Psychol Med. (2021) 51:1704–13. doi: 10.1017/S0033291720000458
68. Rawlings D, Locarnini A. Dimensional schizotypy, autism, and unusual word associations in artists and scientists. J Res Pers. (2008) 42:465–71. doi: 10.1016/j.jrp.2007.06.005
69. Claridge G, McDonald A. An investigation into the relationships between convergent and divergent thinking, schizotypy, and autistic traits. Pers Individ Differ. (2009) 46:794–9. doi: 10.1016/j.paid.2009.01.018
70. Ramain J, Mohr C, Abu-Akel A. How cognitive control, autistic and schizotypal traits shape context adaptation of divergent thinking. J Creat Behav. (2021) 55:783–99. doi: 10.1002/jocb.489
71. Yildirim E. The effect of the interaction between autistic traits and psychotic proneness on empathy: A cross-sectional study with a non-clinical sample. Adv Autism. (2023) 9:364–76. doi: 10.1108/AIA-04-2022-0019
72. Lugo Marín J, Alviani Rodríguez-Franco M, Mahtani Chugani V, Magán Maganto M, Díez Villoria E, Canal Bedia R. Prevalence of schizophrenia spectrum disorders in average-IQ adults with autism spectrum disorders: A meta-analysis. J Autism Dev Disord. (2018) 48:239–50. doi: 10.1007/s10803-017-3328-5
73. Skokauskas N, Frodl T. Overlap between autism spectrum disorder and bipolar affective disorder. Psychopathology. (2015) 48:209–16. doi: 10.1159/000435787
74. Gandal MJ, Haney JR, Parikshak NN, Leppa V, Ramaswami G, Hartl C, et al. Shared molecular neuropathology across major psychiatric disorders parallels polygenic overlap. Science. (2018) 359:693–7. doi: 10.1126/science.aad6469
75. Velthorst E, Froudist-Walsh S, Stahl E, Ruderfer D, Ivanov I, Buxbaum J, et al. Genetic risk for schizophrenia and autism, social impairment and developmental pathways to psychosis. Transl Psychiatry. (2018) 8:204. doi: 10.1038/s41398-018-0229-0
76. Fromer M, Roussos P, Sieberts SK, Johnson JS, Kavanagh DH, Perumal TM, et al. Gene expression elucidates functional impact of polygenic risk for schizophrenia. Nat Neurosci. (2016) 19:1442–53. doi: 10.1038/nn.4399
77. Sugranyes G, Kyriakopoulos M, Corrigall R, Taylor E, Frangou S. Autism spectrum disorders and schizophrenia: meta-analysis of the neural correlates of social cognition. PloS One. (2011) 6:e25322. doi: 10.1371/journal.pone.0025322
78. Pinkham AE, Hopfinger JB, Pelphrey KA, Piven J, Penn DL. Neural bases for impaired social cognition in schizophrenia and autism spectrum disorders. Schizophr Res. (2008) 99:164–75. doi: 10.1016/j.schres.2007.10.024
79. Pina-Camacho L, Parellada M, Kyriakopoulos M. Autism spectrum disorder and schizophrenia: boundaries and uncertainties. BJPsych Adv. (2016) 22:316–24. doi: 10.1192/apt.bp.115.014720
80. Varcin KJ, Herniman SE, Lin A, Chen Y, Perry Y, Pugh C, et al. Occurrence of psychosis and bipolar disorder in adults with autism: A systematic review and meta-analysis. Neurosci Biobehav Rev. (2022) 134:104543. doi: 10.1016/j.neubiorev.2022.104543
81. Vaskinn A, Abu-Akel A. The interactive effect of autism and psychosis severity on theory of mind and functioning in schizophrenia. Neuropsychology. (2019) 33:195–202. doi: 10.1037/neu0000499
82. Thaipisuttikul P, Ittasakul P, Waleeprakhon P, Wisajun P, Jullagate S. Psychiatric comorbidities in patients with major depressive disorder. Neuropsychiatr Dis Treat. (2014), 2097–103. doi: 10.2147/NDT.S72026
83. Abu-Akel A, Wood SJ, Upthegrove R, Chisholm K, Lin A, Hansen PC, et al. Psychosocial functioning in the balance between autism and psychosis: evidence from three populations. Mol Psychiatry. (2022) 27:2976–84. doi: 10.1038/s41380-022-01543-5
84. Cantor-Graae E, Selten J-P. Schizophrenia and migration: A meta-analysis and review. Am J Psychiatry. (2005) 162:12–24. doi: 10.1176/appi.ajp.162.1.12
85. Adeponle AB, Thombs BD, Groleau D, Jarvis E, Kirmayer LJ. Using the cultural formulation to resolve uncertainty in diagnoses of psychosis among ethnoculturally diverse patients. Psychiatr Serv. (2012) 63:147–53. doi: 10.1176/appi.ps.201100280
Keywords: CAPE-42, cross-validation, Hebrew, psychometric properties, psychosis
Citation: Fazioli L, Abu-Akel A, Hadad B-S and Yashar A (2025) Validation of the Hebrew version of the Community Assessment of Psychic Experiences in a sample of Israeli Hebrew speakers. Front. Psychiatry 16:1548310. doi: 10.3389/fpsyt.2025.1548310
Received: 19 December 2024; Accepted: 16 April 2025;
Published: 14 May 2025.
Edited by:
Giorgio Di Lorenzo, University of Rome Tor Vergata, ItalyReviewed by:
Marta Bosia, Vita-Salute San Raffaele University, ItalyJacqueline Clauss, Massachusetts General Hospital and Harvard Medical School, United States
Copyright © 2025 Fazioli, Abu-Akel, Hadad and Yashar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laurina Fazioli, bGF1cmluYS5mYXppb2xpQGhvdG1haWwuZnI=
†These authors share first authorship
 Laurina Fazioli
Laurina Fazioli Ahmad Abu-Akel
Ahmad Abu-Akel Bat-Sheva Hadad1,3,4
Bat-Sheva Hadad1,3,4 Amit Yashar
Amit Yashar