- 1Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 2Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, National University Hospital, Singapore, Singapore
- 3Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 4Department of Psychological Medicine, National University Hospital, Singapore, Singapore
Introduction: Hepatitis B is a highly contagious viral infection that has long been a significant global health concern. Given its adverse effects on the course of the disease, evaluating psychiatric outcomes is important. Despite indications of an increased risk of psychological outcomes among those with hepatitis B, the extent of this association remains unclear.
Methods: This PRISMA-adherent systematic review (PROSPERO: CRD42024564246) searched PubMed, Embase, Cochrane, and PsycINFO for all studies evaluating the prevalence and risk of anxiety and depressive symptoms in individuals with hepatitis B. Random effects meta-analyses and meta-regression were used for primary analysis.
Results: A total of 31 studies were included. We identified a high prevalence of depressive symptoms (Proportion=19%, 95% CI: 11-31) and anxiety (Proportion=30%, 95% CI: 18-45) among individuals with hepatitis B. There was also a significantly increased risk of depressive symptoms (RR=1.45, 95% CI: 1.00-2.09, P=0.049) and anxiety (RR=1.40, 95% CI: 1.11-1.78) in individuals with hepatitis B compared to controls. Subgroup analyses indicated that older age and chronic hepatitis B infection were associated with a higher prevalence of anxiety and depressive symptoms. The systematic review found that being single, unemployed, having a lower income, a lower education level, high comorbidities, and a family history of mental illness were significant risk factors for poorer psychological outcomes.
Conclusion: Our study highlights an increased vulnerability to anxiety and depressive symptoms among individuals with hepatitis B. We emphasize the urgent need for early detection and additional support for this at-risk group.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42024564246.
Introduction
Hepatitis B, a highly contagious viral infection primarily affecting the liver, has long been a significant global health concern, infecting approximately 400 million people worldwide and resulting in one million deaths annually due to liver disease (1). This persistent viral infection can range from an inactive carrier state to progressive chronic hepatitis B, which may lead to severe liver complications such as cirrhosis and hepatocellular carcinoma, affecting 15-40% of individuals infected with hepatitis B (2).
Beyond these well-documented physical health impacts, there is a growing body of research on the negative psychological outcomes faced by individuals with hepatitis B as a chronic illness. A well-established bidirectional relationship exists between chronic physical illnesses and mental health disorders (3–9). Those with chronic infections such as hepatitis B encounter numerous challenges in managing their illness, ranging from the emotional burden of coping with a long-term condition to the side effects of antiviral therapies and the social stigma associated with their situation (10).
Such factors can significantly contribute to the development of mental health issues and adversely impact the treatment and prognosis of chronic disease. Elevated psychological symptoms, such as depression and anxiety, have been associated with reduced quality of life, poorer medication compliance and increased mortality (11).
In the specific context of hepatitis B, several studies have associated the presence of negative psychological outcomes with higher prevalence rates of psychological disorders among individuals with hepatitis B compared to healthy controls (12). A significant proportion (about 50%) of individuals with hepatitis B and hepatitis C also develop psychiatric illnesses (13). Among these individuals, particularly those with hepatitis B, the global Health-Related Quality of Life (HRQoL) is significantly worse than in the general population, and it appears to decrease as the liver disease advances (14). Notably, in individuals with hepatitis B, depressive symptoms have been associated with a higher risk of liver-related death (15).
Evaluating the psychological outcomes of hepatitis B is therefore important, given their negative impact on the course of the disease. Despite indications of an increased risk of psychological issues among those with hepatitis B, the extent of this association remains unclear, and reported prevalence rates of anxiety and depressive symptoms in individuals with hepatitis B differ across studies (16). Furthermore, only a limited number of studies have examined the prevalence of these symptoms in individuals with hepatitis B infection.
In light of these observations, a comprehensive synthesis of the existing literature is necessary to enhance our understanding of the relationship between hepatitis B and psychological outcomes. Therefore, this study aims to evaluate whether infection heightens the risk of developing psychological issues such as anxiety and depressive symptoms. The objective is to identify potential causes and modifiers of this association and provide a more precise estimate of the mental health burden linked to hepatitis B by integrating data from various research studies. By consolidating available evidence, this study seeks to inform clinical practice and direct future research to improve the comprehensive care of individuals living with hepatitis B.
Methodology
This systematic review is reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The protocol was registered on (PROSPERO: CRD42024564246).
Search strategy
A literature search was performed in PubMed, Embase, Cochrane and PsycINFO. Our search strategy combined terms for ‘hepatitis b’, ‘anxiety’ and ‘depression’. The database-controlled vocabulary was utilized to search for subject headings. Synonyms with appropriate truncations were used to search for title and abstract keywords. The search strategy was translated between the different databases. Examples of the search strategies for PubMed and EMBASE are found in Supplementary Table S1. We conducted a hand-searching process and performed both forward and backward searching to ensure inclusion of all relevant articles.
Inclusion and exclusion criteria
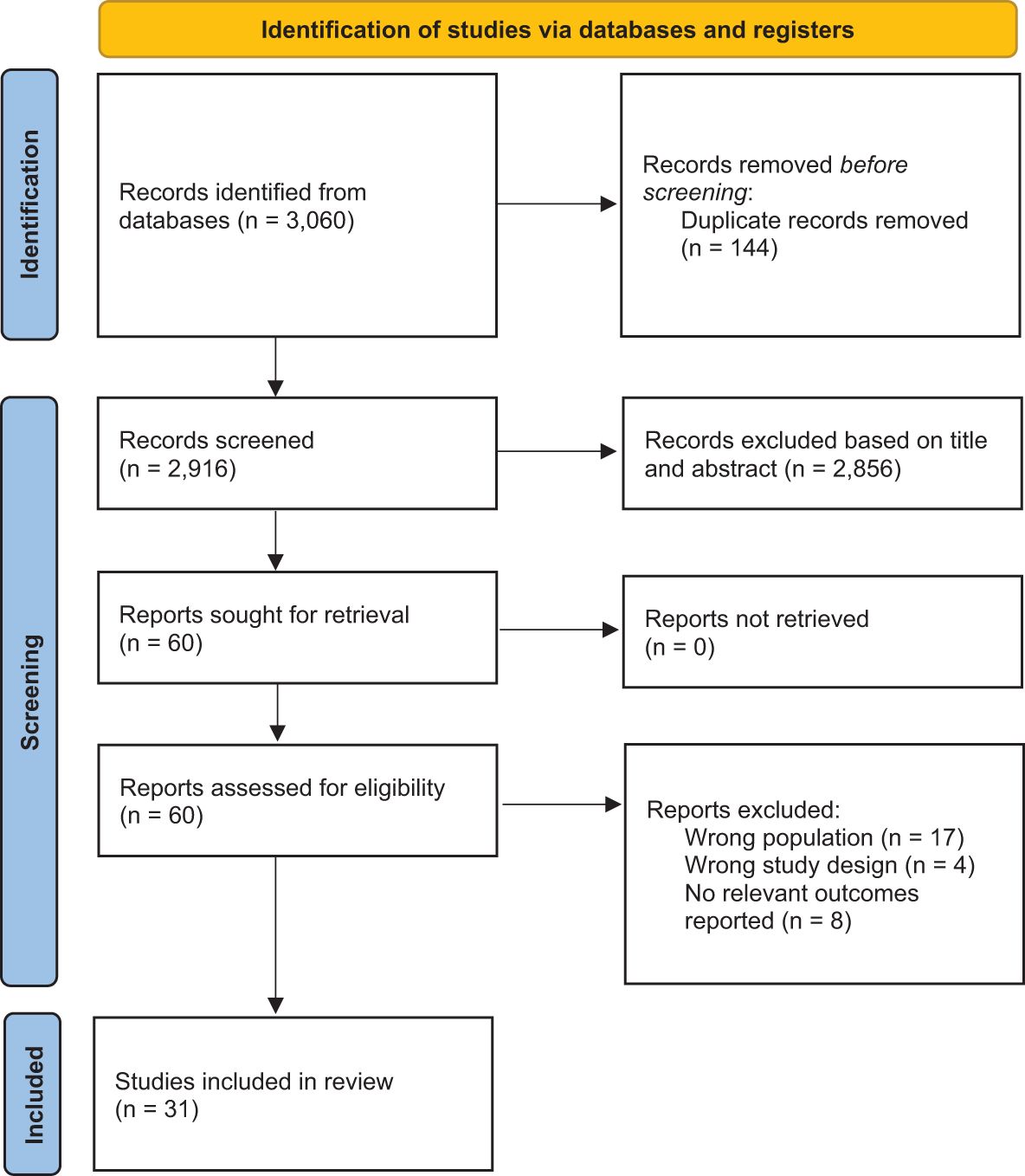
Two reviewers independently screened the titles and abstracts of the studies for eligibility, while a third reviewer addressed any discrepancies. All peer-reviewed studies published in English from 2000 to 2nd November 2024 that assessed the prevalence and risk of psychological outcomes in individuals with hepatitis B were included. The initial extraction date was 1st September 2024. To mitigate the small study effect, only studies with more than 50 individuals with hepatitis B were considered. Non-empirical studies, grey literature, and abstracts were excluded. The selection process is illustrated in Figure 1.
Data extraction and analysis
Two reviewers independently performed the extraction. Subject matter information included demographics, the instruments and scales used to assess psychological outcomes, treatment modalities, chronicity of disease, comorbidities, characteristics of the control group, and the study’s main findings. The number of events and participants at risk regarding the specific outcomes were extracted. We pooled the prevalence for single-arm studies and the relative risk-ratio (RR) for double-arm studies. The reported psychological outcomes must be assessed using a validated instrument for patient-reported outcome measures or a clinical diagnosis made by a registered practitioner.
All analyses were conducted using R (version 4.1.0) along with the meta and metafor packages. A two-sided P value of <0.05 was deemed statistically significant. Metaprop was employed to meta-analyze the prevalence under a generalized linear mixed model (GLMM). For dichotomous outcomes, meta-analyses were carried out to estimate the relative risk of the psychological outcome (measured using RR compared to controls). We performed sensitivity analyses by identifying and excluding potential outliers, employing random-effects models, and conducting leave-one-out analysis. Subgroup analyses and meta-regression were performed to ascertain whether key hierarchical and categorical variables influenced the results.
I2 and τ2 statistics were used to represent between-study heterogeneity. An I2 of less than 30% indicated low heterogeneity, 30% to 60% suggested moderate heterogeneity and more than 60% demonstrated substantial heterogeneity (17). Egger’s test was used to assess quantitative publication bias (18). Visual inspection of funnel plot asymmetry was conducted to evaluate qualitative publication bias. If publication bias was suspected, a sensitivity analysis was conducted using the trim-and-fill method (R0 estimator and random effects models) to re-estimate the effect size after imputing for potential studies (19). We assumed a normal distribution of effect sizes around the center of the funnel plot if publication bias was absent (18).
Risk of bias
Two independent reviewers assessed the included studies’ risk of bias using the Joanna Briggs Institute (JBI) Critical Appraisal tool (20). A third reviewer resolved any discrepancies.
Results
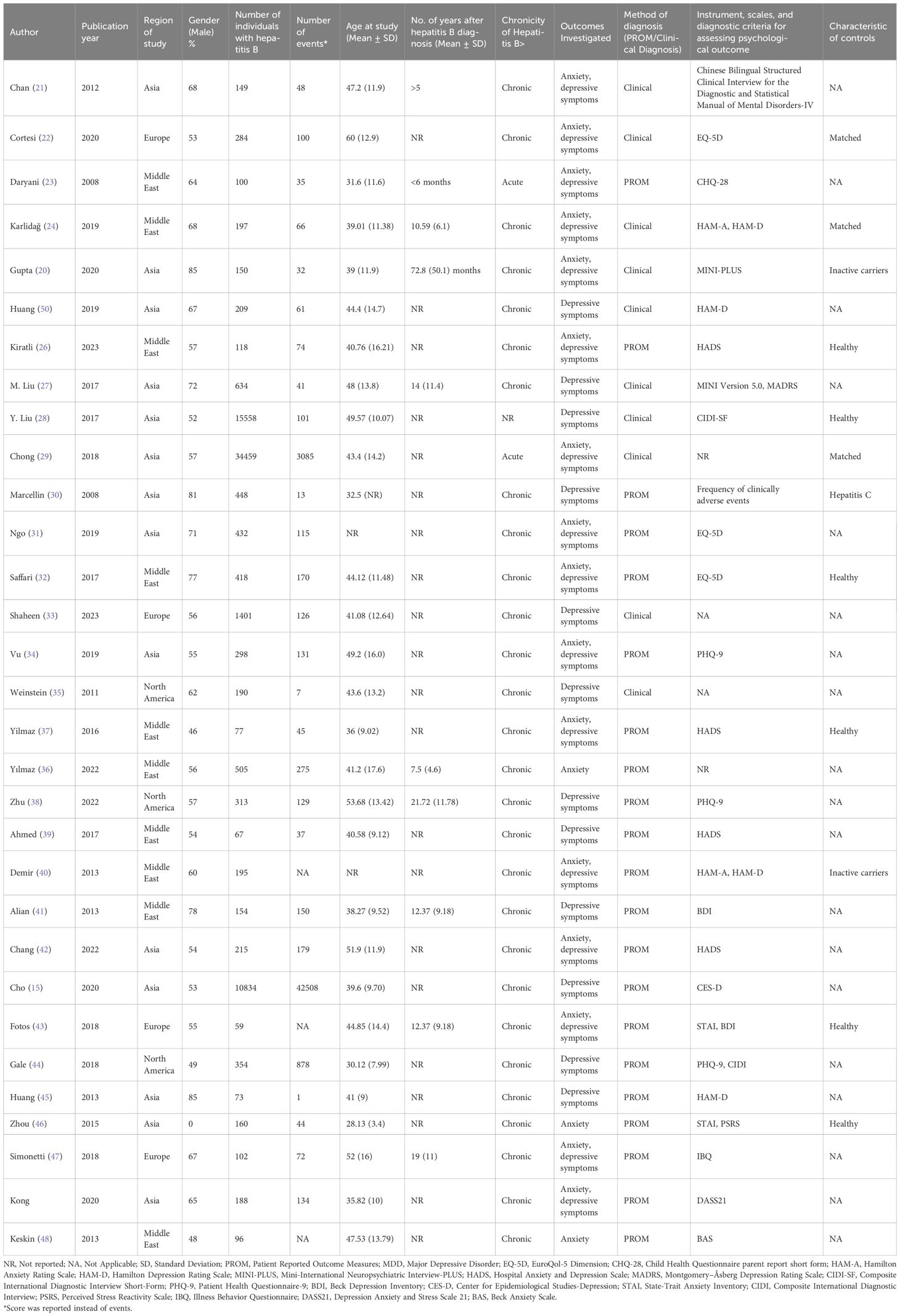
31 studies (21–49) were eventually included from 3,060 records (Figure 1). 14 were from Asia (15, 21, 25, 27–31, 34, 42, 45, 46, 49, 50), 10 were from the Middle East (23, 24, 30, 36, 37, 39–41, 48, 51), four were from Europe (22, 33, 43, 47), and three were from North America (35, 38, 44). 53,964 individuals with hepatitis B were included. The mean age of the individuals ranged from 31.6 to 60 years. Most of the studies investigated chronic individuals with hepatitis B, except for two (23, 29). 16 studies (21–26, 29, 31, 32, 34, 37, 40, 42, 43, 47) evaluated both anxiety and depression, 12 studies (15, 27, 28, 30, 33, 35, 38, 39, 41, 44, 45, 50) on depression and three studies (36, 46, 48) on anxiety only. The outcomes from 21 studies (23, 26, 30–32, 34, 36–49) were patient-reported outcome measures, and 10 studies (21, 22, 24, 25, 27–29, 33, 35, 50) with outcomes from a formal clinical diagnosis of depression. Eight studies (22, 24–26, 28–30, 32, 37, 40, 43, 46) were controlled studies. Six studies used healthy individuals from the general population as the comparator group (22, 24, 26, 29, 32, 43). One study used HBsAg-positive inactive carriers as the control group (40). One study used healthy pregnant women as the control group (46). The overall characteristics of the studies can be found in Table 1.
Depressive Symptoms
23 studies (15, 21–23, 25–31, 34, 35, 37–39, 41, 42, 44, 45, 47, 49, 50) evaluated the prevalence of depressive symptoms among individuals with hepatitis B. Meta-analysis of the 23 studies (15, 21–23, 25–31, 34, 35, 37–39, 41, 42, 44, 45, 47, 49, 50) (Figure 2) revealed that depressive symptoms were seen in 19% of individuals with hepatitis B (95%CI: 11-31).
Subgroup analyses of the prevalence of depressive symptoms among other categorical variables are found in Supplementary Table S2. Subgroup analyses showed that the prevalence of depressive symptoms was significantly higher in individuals with chronic hepatitis B (15, 21, 22, 25–28, 30, 31, 34, 35, 37–39, 41, 42, 44, 45, 47, 49, 50) (24%, 95%CI: 15-35) as compared to acute hepatitis B (23, 29) (10%, 95%CI: 2-38). The prevalence of depressive symptoms was significantly lower in the clinically assessed group (15, 21, 22, 25, 27–29, 35, 50) (8%, 95% CI: 3-19%) compared to the patient-reported group (23, 26, 30, 31, 34, 37–39, 41, 42, 44, 45, 47, 49) (28%, 95% CI: 17-44%). Studies of populations from the Middle East (23, 30, 37, 39, 41) had the highest prevalence of depressive symptoms (55%, 95%CI: 27-80) and studies from Asia (15, 21, 25, 27–31, 34, 42, 45, 49, 50) had the lowest prevalence of depressive symptoms (11%, 95%CI: 6-19). Subgroup analyses based on the instrument used to assess depressive symptoms were significant. Overall, gender, age at data collection and duration (years) since diagnosis did not significantly increase the prevalence of depressive symptoms. Meta-regression suggested that older age at data collection was significantly associated with the prevalence of depressive symptoms in individuals with hepatitis B (Supplementary Table S4).
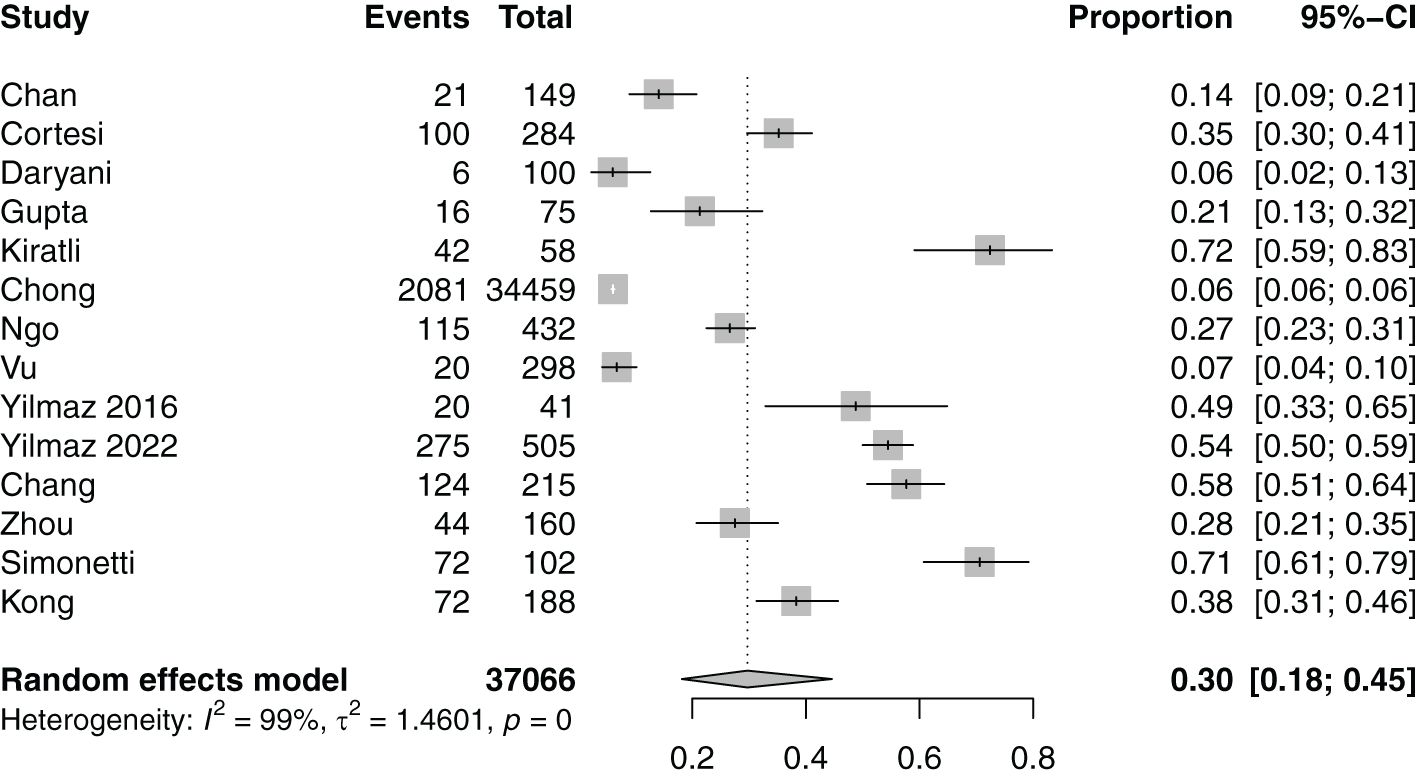
Anxiety
14 studies (21–23, 25, 26, 29, 31, 34, 36, 37, 42, 46, 47, 49) evaluated the prevalence of anxiety among individuals with hepatitis B. Meta-analysis of the 14 studies (21–23, 25, 26, 29, 31, 34, 36, 37, 42, 46, 47, 49) (Figure 3) revealed that anxiety was observed in 30% of individuals with hepatitis B (95%CI: 18-45).
Subgroup analyses of the prevalence of anxiety among other categorical variables are found in Supplementary Table S3. Subgroup analyses showed that anxiety prevalence was significantly higher in individuals with chronic hepatitis B (21, 22, 25, 26, 31, 34, 36, 37, 42, 46, 47, 49) (37%, 95%CI: 25-50) as compared to acute hepatitis B (23, 29) (6%, 95%CI: 2-19). Overall, region, gender, scales used to measure anxiety, outcome measure (clinical diagnosis or patient-reported outcome measure), age at data collection and duration from diagnosis did not significantly increase the prevalence of anxiety. Meta-regression suggested that older age at data collection and duration (years) since diagnosis was significantly associated with anxiety prevalence in individuals with hepatitis B (Supplementary Table S4).
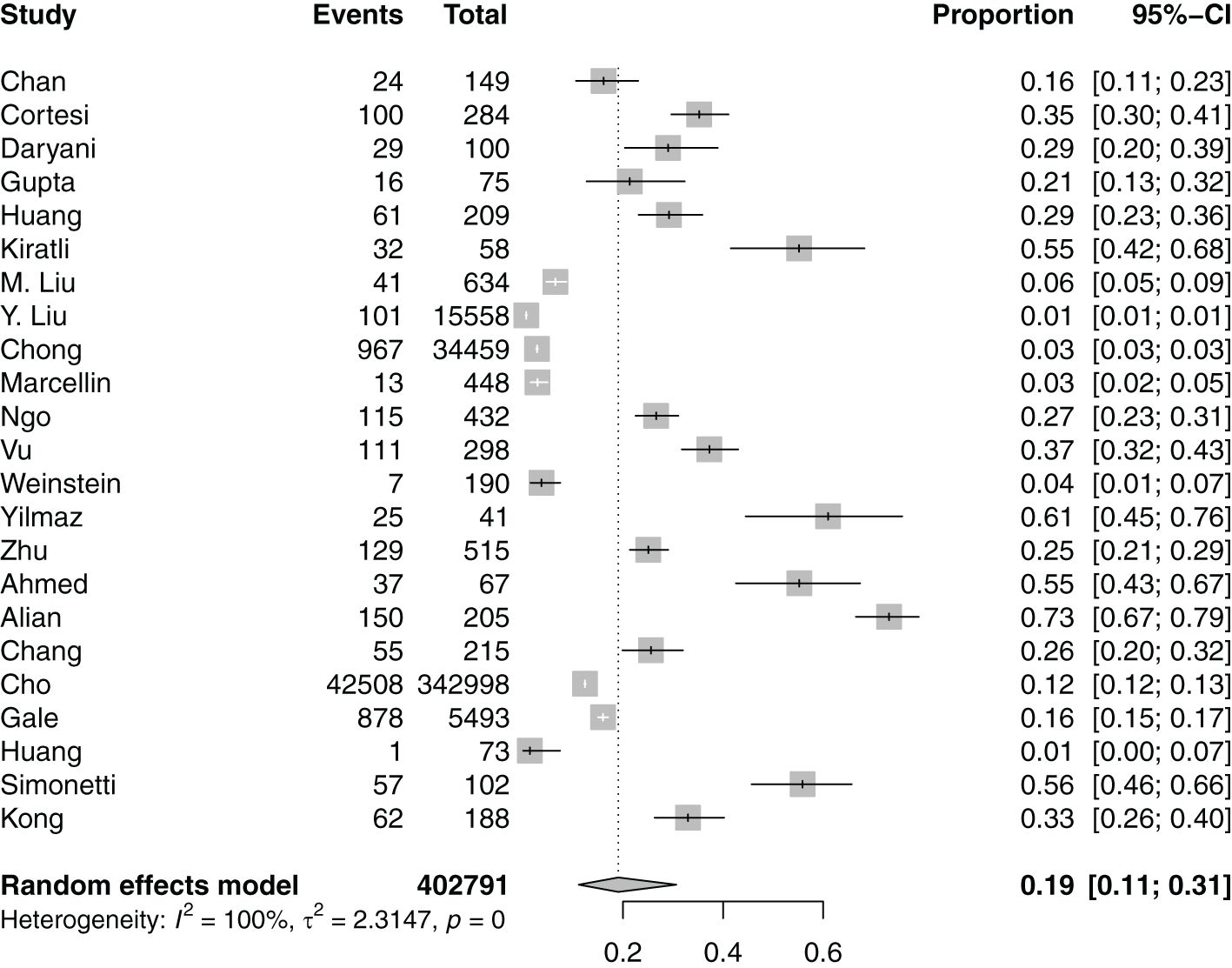
Five studies (22, 25, 26, 28, 29) were analyzed to investigate the relative risk of depressive symptoms in individuals with hepatitis B. Meta-analysis of the five studies (22, 25, 26, 28, 29) (Figure 4A) reported a statistically significant increase in the risk of depressive symptoms in individuals with hepatitis B compared to the comparator arm (RR=1.45, 95%CI: 1.00-2.09, P=0.049). Five (22, 25, 26, 29, 46) studies were analyzed to evaluate the relative risk of anxiety in individuals with hepatitis B. Meta-analysis of the five studies (22, 25, 26, 29, 46) (Figure 4B) indicated a statistically significant increased risk of anxiety in individuals with hepatitis B compared to the comparator arm (RR=1.40, 95% CI: 1.11-1.78).
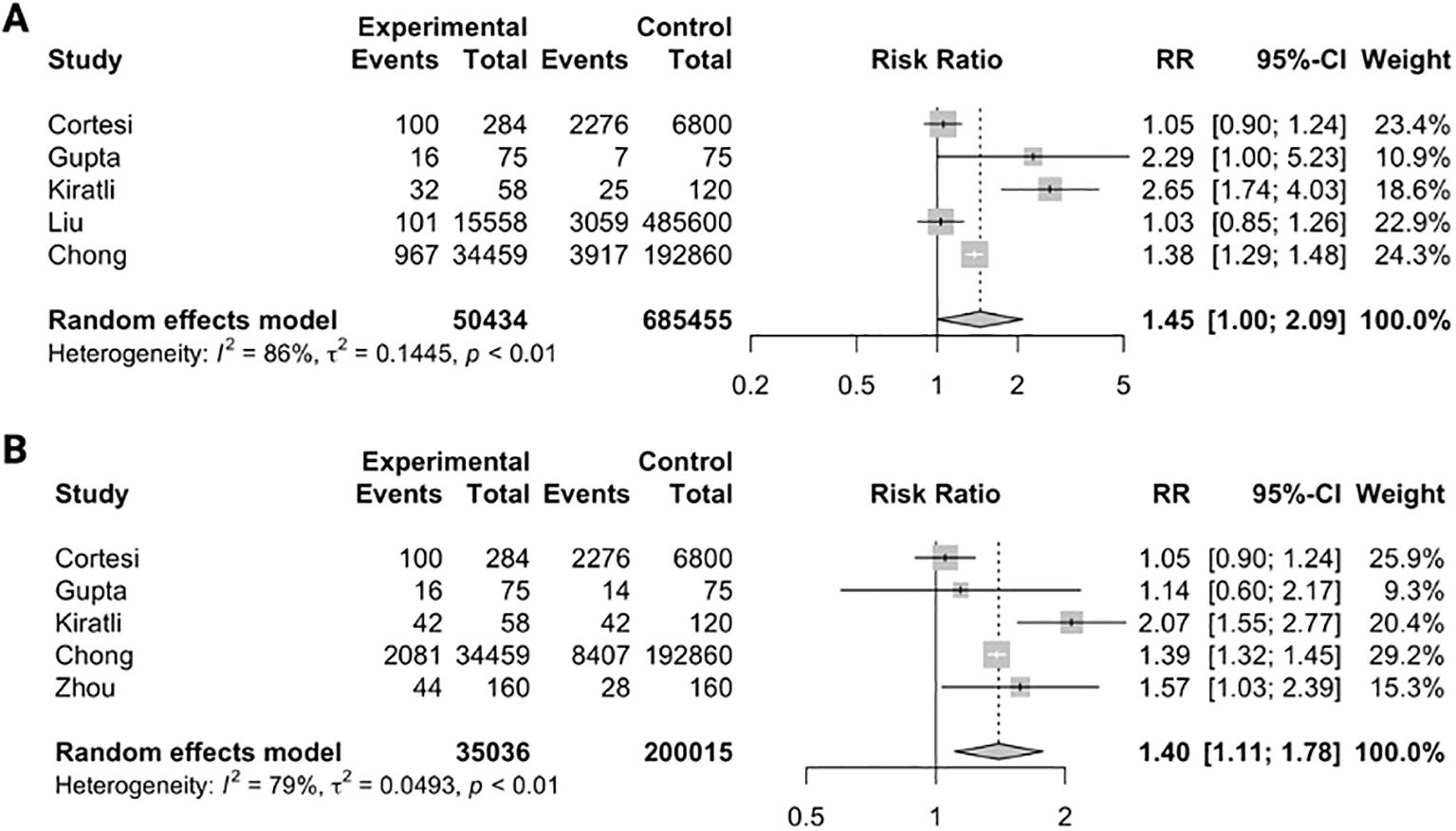
Figure 4. Relative risk ratios of having depressive symptoms (A) and anxiety (B) in individuals with hepatitis B when compared to comparator.
Risk-of-bias and publication bias
The quality of the methodology of the 31 studies (21–49) was assessed using the JBI checklist and is presented in Supplementary Table S12. Some risk of bias was identified. Sensitivity analyses were conducted employing funnel plots, trim-and-fill, and Egger’s test, which indicated some publication bias (Supplementary Figures S1-S10). However, the leave-one-out analyses did not reveal any individual studies that would influence the overall results.
Systematic review
Education level
Eight studies (15, 23, 24, 28, 34, 38, 48, 49) reported the confounding effect of education on the psychological outcomes of individuals with hepatitis B (Supplementary Table S5). Five (15, 23, 24, 34, 49) out of eight (15, 23, 24, 28, 34, 38, 48, 49) studies reported a significant association between lower education levels and higher levels of depression and anxiety. Three (28, 38, 48) studies found no significant association between education levels and psychological outcomes.
Comorbidities
Eight (15, 31, 33, 34, 40, 42–44) studies reported the confounding effect of comorbidities on the psychological outcomes of individuals with hepatitis B (Supplementary Table S6). All eight studies (15, 31, 33, 34, 40, 42–44) reported a significant association between having a higher number of comorbidities and a higher likelihood of having depression and anxiety. Interestingly, individuals with alcoholic liver disease (42), liver transplant (31), and herpes simplex virus-2 (44) had worse psychological outcomes.
Marital status
Eight (23, 24, 31, 34, 36, 38, 48, 49) studies reported the confounding effect of marital status on the psychiatric outcomes of individuals with hepatitis B (Supplementary Table S7). Seven (23, 31, 34, 36, 38, 48, 49) (23, 24, 31, 34, 36, 38, 48, 49) studies showed a significant association between marital status and psychological outcomes. Five (23, 31, 36, 38, 49) out of the seven (23, 31, 34, 36, 38, 48, 49) studies revealed that being single increased the risk of poorer psychological outcomes. Conversely, Vu (34) and Keskin et al (48). reported a significant association between having a spouse, partner or being married and a higher likelihood of worse psychological outcomes.
Treatment
Six (29, 40–42, 45, 49) studies reported the confounding effect of treatment factors on the psychological outcomes of individuals with hepatitis B (Supplementary Table S8). Kong (49) and Huang et al (45). reported a significant association between a longer duration of treatment and an increased risk of psychological outcomes. Alian et al (41). saw a significantly higher prevalence of depression in participants who received interferon treatment and those who did not. Chang (42) and Demir et al (40). did not observe any significant association between interferon therapy treatment and the prevalence of psychological outcomes. Chong et al (29). found no significant association between antiviral therapy and an increased risk of bipolar disorder.
Income
Five (21, 23, 28, 34, 38) studies reported the confounding effect of income on the psychiatric outcomes of individuals with hepatitis B (Supplementary Table S9). Four (21, 23, 28, 34) out of five (21, 23, 28, 34, 38) studies reported that Hepatitis B carriers with a lower family income were significantly more likely to have poorer psychological outcomes. Zhu et al (38). did not find any significant relationship between income and depression severity in both treatment and non-treatment groups.
Employment status
Three (34, 38, 43) studies reported the confounding effect of employment status on the psychological outcomes of individuals with hepatitis B (Supplementary Table S10). Two (38, 43) out of three (34, 38, 43) studies reported a significant association between unemployment and a higher prevalence of worse psychological outcomes. Interestingly, Vu et al (34). found a significant association between freelancers and a lower likelihood of depression.
Family history
Three (21, 24, 40) studies reported the confounding effect of family history on psychological outcomes of individuals with hepatitis B (Supplementary Table S11). Two (21, 24) out of three (21, 24, 40) studies revealed a significant association between a positive family history of mental illness and worse psychological outcomes. In contrast, Demir et al (40). found no significant association between a family history of Hepatitis B infection or cirrhosis and psychological outcomes.
Discussion
To the best of our knowledge, this study is the first systematic review and meta-analysis examining the prevalence and risk of anxiety and depressive symptoms among individuals with hepatitis B. Our findings indicated a high prevalence of anxiety and depressive symptoms in those with hepatitis B compared to individuals without the condition. Subgroup analyses identified risk factors for anxiety and depressive symptoms, including older age and chronic hepatitis B infection. The systematic review highlighted that being single, unemployed, having a lower income, lower educational attainment, high comorbidity, and a family history of mental illness were significant risk factors associated with poorer psychological outcomes.
We further compared the prevalence and risk of anxiety and depressive symptoms in individuals with hepatitis B against those with other diseases (Supplementary Table S15). Our review found that the prevalence of anxiety and depressive symptoms in individuals with hepatitis B was 30% and 19% respectively, a notably sharp increase compared to the general population, which stands at 4% and 5% respectively (52, 53). Subsequent meta-analysis also revealed a 1.45-fold increase in the risk of depression and a 1.4-fold increase in the risk of anxiety in individuals with hepatitis B compared to the comparator group. The apparent discrepancies in these risk figures highlight the significant psychological burden that may be associated with chronic illness. It is imperative that the healthcare system directs attention not only to treating physical ailments but also to the often-overlooked mental repercussions of hepatitis B.
Furthermore, the prevalence of anxiety among individuals with hepatitis B is higher than that of patients with type 2 diabetes, which is approximately 21.8 (54). The increased prevalence of adverse mental health outcomes in those with hepatitis B may be attributed to the infectious nature and social stigma associated with the condition; whereas diabetes is a non-transmissible disease, hepatitis B can be transmitted through means such as blood, sharing needles, and sexual fluid (55). The concerns that individuals may harbor about the infectiousness of their diagnosis can lead to heightened stress and consequently result in a higher prevalence of psychiatric disorders. Public misconceptions about hepatitis B and its mode of transmission may further amplify the social stigma surrounding these individuals. In a study conducted in Singapore on the general public, over 50% of respondents surveyed believed that hepatitis B could be transmitted by sharing food (56). These misconceptions may result in differential treatment or even avoidance of these individuals, thereby fostering feelings of exclusion or social isolation, which are closely linked to the development of depression (57). Additionally, the prevalence of depression in individuals with hepatitis B is comparable to the prevalence of anxiety among those with asthma, which ranges between 11-13 (58). This similarity further underscores the debilitating impact that chronic disease can have on an individual’s mental health. This aligns with existing literature, which has shown that conditions such as cholesterol disease, kidney disease, coronary heart disease, and asthma are all significantly associated with mental health problems experienced by patients (59).
Subgroup analyses have revealed a significantly higher prevalence of depressive symptoms in individuals with chronic hepatitis B (24%) compared to those with acute hepatitis B (10%). We also observed a notably higher prevalence of anxiety in individuals with chronic hepatitis B (37%) in contrast to acute hepatitis B (6%). These findings are supported by current literature, which demonstrates a well-recognized link between chronic illnesses and mental health disorders (60–62). The discrepancy in our findings may be attributed to biological factors, such as neurotransmitter imbalances associated with chronic illness (63–65). While the stress that infections impose on the immune system triggers cytokine release, which is beneficial in the short term for combating infections, prolonged exposure to inflammatory cytokines can lead to the emergence of neuropsychiatric disorders like depression. Chronic hepatitis B induces ongoing inflammation and activates cell-mediated immunity, which has been shown to play a key role in influencing both the risk of developing depression and its progression (66). Conversely, it has also been noted that individuals experiencing depression and fatigue display increased inflammatory immune activation (67). This underscores the bidirectional relationship between chronic hepatitis B and psychiatric disorders, whereby persistent inflammation not only contributes to depressive symptoms but is also affected by the presence of chronic health conditions.
In addition to biological factors, one of the mainstays of chronic hepatitis B treatment is interferon therapy (68). The adverse side effects of interferon therapy, which are well documented in the literature to include depressive symptoms and anxiety, are plausible contributing factors to our findings (69, 70). Pinto et al (71). describe the prevalence of depression during interferon treatment as 30-70% (72). It has been postulated that interferon-alpha activates the enzyme indoleamine 2,3-dioxygenase (IDO), which shifts tryptophan metabolism away from serotonin production towards the kynurenine pathway (73). This shift ultimately reduces serotonin levels in the brain, a depletion that is widely recognized as a driver of depression (73). Lastly, while acute hepatitis B is curable even without treatment, chronic hepatitis B may never be cured (74). Thus, individuals suffering from the latter could experience intensified feelings of helplessness and other negative emotions that are linked to the development of mental health disorders.
Subgroup analyses have identified older age as a risk factor for a higher prevalence of adverse psychological outcomes for both depressive symptoms and anxiety. Several factors contribute to the increased vulnerability of this group to negative mental health outcomes. Firstly, the natural progression of chronic hepatitis B over time, characterized by repeated cycles of injury, healing, and fibrosis, eventually leads to cirrhosis and even liver cancer (75). Increasing age serves as a predictor for these adverse outcomes in HBeAg-positive individuals (76), such as a heightened risk of developing fibrosis and a reduced likelihood of sustained viral suppression (77, 78). The awareness of being at an increased risk for severe health complications due to age can significantly exacerbate anxiety and depression among older individuals. Furthermore, older adults are more likely to experience multimorbidity than their younger counterparts (79). The physical pain and mental fatigue associated with managing multiple chronic illnesses predispose them to a greater risk of developing depression and anxiety (62, 80). Moreover, older adults face an elevated risk of social isolation and loneliness, arising from factors such as the loss of a partner or loved ones, decreased mobility, sensory impairments, and limited familiarity with technology (81). This isolation can negatively impact mental health outcomes, as numerous studies have underscored a significant connection between social isolation and psychiatric disorders like depression and anxiety (66, 82). These findings highlight the detrimental effects of social isolation on mental health, a connection that is particularly pronounced in the elderly population, given their heightened risk of social isolation.
Our systematic review has also identified lower education levels, lower income and unemployment as causative factors in higher levels of depression and anxiety. Our findings are aligned with the current literature, which consistently demonstrates a strong correlation between lower educational attainment and elevated levels of depression and anxiety (83, 84). The relationship between education, income and employment is closely intertwined and studied extensively. Mirowsky et al (85). have shown that higher educational attainment leads to increasingly stable employment, which provides higher incomes. These greater financial resources contribute to one’s higher socioeconomic status and enable wealth accumulation, allowing greater accessibility to quality healthcare and resources for managing mental wellbeing (86). Education also enhances individuals’ knowledge and skills, which can be utilized to develop coping strategies for regulating mental health (87). Furthermore, individuals from low socioeconomic backgrounds face greater exposure to daily stressors, and the cumulative effects of such stressors are pertinent predictors of poorer mental health outcomes in the long run (88).
An increasing number of comorbidities have been identified as risk factors for anxiety and depression. The relationship between comorbidities and poor psychological outcomes is well documented in scientific literature. Lim et al (89). write that those with chronic health conditions face a higher risk of loneliness and its subsequent health impacts. In alignment with this, Ronaldson et al (90). found that individuals with more than one physical health condition tended to have worse mental health than their physically healthier counterparts. The debilitating diagnosis of a chronic illness may threaten an individual’s sense of purpose and meaning in life (91). Individuals with chronic illnesses are also more likely to self-inflict social isolation, as they may perceive themselves as different compared to their healthy counterparts, thus reducing their contact and participation in social activities (51, 92). This is confounded by their disabling symptoms and related discomfort, or they may struggle to engage in social activities due to a lack of energy. Consequently, chronically ill individuals may find themselves lacking emotional support from a healthy social circle, placing them at a heightened risk of developing anxiety and depression.
We have also identified a family history of mental illness as a risk factor for anxiety and depression. This is no surprise, as numerous reputable studies have demonstrated similar findings. Streit et al (93). showed that a family history is linked to increased depression. It was also found that students with a family history of mental illnesses were more likely to report clinically significant depressive symptoms (94). There is growing evidence of the genetic vulnerability involved in developing adverse mental health outcomes. For example, Sullivan et al (95). showed that there is a two-to-three-fold increase in the risk of depression among first-degree relatives of individuals with depression. These conclusions suggest that there is validity in the assertion that a family history of mental illness is a risk factor for anxiety and depression.
Finally, we observed that being married offers a protective advantage against the risk of developing anxiety and depression. The social support provided by marriage exerts far stronger effects than support from friends (96). Thoits et al. (97). suggest that social support is most beneficial when it comes from individuals who share similar characteristics and values and have successfully navigated similar challenges. Hence, the spouse often serves as the pivotal source of support due to the interconnectedness of their relationship with the individual. Furthermore, spousal support is not only unique and sometimes more effective than other forms of support, but in times of crisis, the spouse is often the first person to whom individuals turn for help (98, 99). The presence of such social support fosters a safe environment for individuals to share their feelings and process their emotions, thereby bolstering their mental well-being (100). Social support also positively influences health outcomes by reducing mood-related symptoms and increasing help-seeking behavior and treatment compliance (101). Like many chronic diseases, hepatitis B is associated with a significant impact on mental health (8, 102–104). By identifying and elucidating the psychological burden amongst individuals with hepatitis B, further interventions may be instituted to alleviate this burden (105–107).
Limitations
Our study should be interpreted with due consideration of certain limitations. Firstly, there was high heterogeneity in the reporting of outcomes that we were unable to account for, such as the variety of instruments used to evaluate depressive symptoms and anxiety among the studies. There were also insufficient studies with a control arm, and among those studies that did include a control arm, data on anxiety and depressive symptoms were available for five studies each. Due to the heterogeneity across different social contexts, we could not perform subgroup meta-analyses for variables such as education level, comorbidities, marital status, treatment factors, income level, employment status and family history. Nonetheless, we were still able to systematically review those factors. Secondly, we did not obtain individual patient data for our meta-analysis as the available data was insufficient to study individual risk factors affecting psychological outcomes. However, we could still analyze the key characteristics of the subgroups we planned for, including age, gender, years since hepatitis diagnosis, chronicity, outcome measure, and region. Thirdly, a large proportion of our studies originate from Asia and the Middle East, with a small proportion from the US and Europe. This may limit the generalizability of these findings to the Caucasian population. However, it is known that the burden of Hepatitis B in Asia far exceeds that in the US, Europe and Oceania (108), which reflects the higher number of studies conducted in Asia. It is well-established that individuals with psychiatric comorbidities are less likely to adhere to treatment regimens for both their chronic illnesses and mental health conditions, leading to adverse health outcomes (109). We hence emphasize the need for early detection and intervention for mental health comorbidities in individuals with hepatitis B.
Conclusion
Our study highlights an increased susceptibility to anxiety and depressive symptoms in individuals with hepatitis B. Notably, factors such as older age, chronicity, being single, unemployed, having a lower income, a lower education level, high comorbidities, and a family history of mental illness are significant contributors to adverse psychological outcomes. Providing tailored mental health support for this vulnerable group can enhance treatment adherence, mitigate the disease burden, and improve overall well-being. Urgent interventions and further research are necessary to elucidate additional prognostic factors to devise targeted strategies to alleviate the burden of anxiety and depressive symptoms in these individuals. Future research could focus on developing a standardized assessment of mental health in individuals with hepatitis B to identify those at risk of psychological distress. This would facilitate the provision of targeted psychosocial support, potentially improving health and treatment outcomes for these individuals.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
CL: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. GG: Methodology, Writing – original draft. TY: Methodology, Writing – original draft. SR: Methodology, Writing – review & editing. SL: Writing – review & editing. AK: Writing – review & editing. AL: Supervision, Writing – review & editing. CH: Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Funding for this publication will be provided by National University Health System (NUHS) Department funding. NUHS had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1546545/full#supplementary-material
References
1. Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. (2004) 11:97–107. doi: 10.1046/j.1365-2893.2003.00487.x
2. McMahon BJ. The natural history of chronic hepatitis B virus infection. Hepatology. (2009) 49:S45–55. doi: 10.1002/hep.22898
3. Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and anxiety in heart failure: A review. Harv Rev Psychiatry. (2018) 26:175–84. doi: 10.1097/HRP.0000000000000162
4. Bădescu SV, Tătaru C, Kobylinska L, Georgescu EL, Zahiu DM, Zăgrean AM, et al. The association between Diabetes mellitus and Depression. J Med Life. (2016) 9:120–5.
5. Low CE, Loke S, Pang GE, Sim B, Yang VS. Psychological outcomes in patients with rare cancers: a&xa0;systematic review and meta-analysis. eClinicalMedicine. (2024) 72. doi: 10.1016/j.eclinm.2024.102631
6. Low CE, Loke S, Rana S, Sim B, Ho CSH. Prevalence and incidence of suicide, suicidal ideation and self-harm in caregivers of cancer patients: A systematic review and meta-analysis. Gen Hosp Psychiatry. (2024) 90:35–43. doi: 10.1016/j.genhosppsych.2024.06.011
7. Low CE, Yau CE, Tan RY, Ong VCS, Ho RCM, Ho CSH, et al. Association of depression with all-cause and cancer-specific mortality in older adults with cancer: Systematic review, meta-analysis, and meta-regression. J Geriatric Oncol. (2024) 15. doi: 10.1016/j.jgo.2023.101700
8. Lee ARYB, Yau CE, Low CE, Li J, Ho RCM, Ho CSH. Severity and longitudinal course of depression, anxiety and post-traumatic stress in paediatric and young adult cancer patients: A systematic review and meta-analysis. J Clin Med. (2023) 12:1784. doi: 10.3390/jcm12051784
9. Kant R, Yadav P, Barnwal S, Dhiman V, Abraham B, Gawande K. Prevalence and predictors of depression in type 2 diabetes mellitus. J Educ Health Promot. (2021) 10:352. doi: 10.4103/jehp.jehp_1507_20
10. Toumi M, Wallace J, Cohen C, Marshall C, Kitchen H, Macey J, et al. Experience and impact of stigma in people with chronic hepatitis B: a qualitative study in Asia, Europe, and the United States. BMC Public Health. (2024) 24:611. doi: 10.1186/s12889-023-17263-6
11. Bujang MA, Musa R, Liu WJ, Chew TF, Lim CTS, Morad Z. Depression, anxiety and stress among patients with dialysis and the association with quality of life. Asian J Psychiatry. (2015) 18:49–52. doi: 10.1016/j.ajp.2015.10.004
12. Arslan N, Büyükgebiz B, Oztürk Y, Akay AP. Depression and anxiety in chronic hepatitis B: effect of hepatitis B virus infection on psychological state in childhood. Turk J Pediatr. (2003) 45:26–8.
13. Özkan M, Çorapçioglu A, Balcioglu I, Ertekin E, Khan S, Özdemir S, et al. Psychiatric morbidity and its effect on the quality of life of patients with chronic hepatitis B and hepatitis C. Int J Psychiatry Med. (2006) 36:283–97. doi: 10.2190/D37Y-X0JY-39MJ-PVXQ
14. Ong SC, Mak B, Aung MO, Li SC, Lim SG. Health-related quality of life in chronic hepatitis B patients. Hepatology. (2008) 47:1108–17. doi: 10.1002/hep.22138
15. Cho IY, Chang Y, Sung E, Sohn W, Kang JH, Shin H, et al. Depressive symptoms and risk of liver-related mortality in individuals with hepatitis B virus infection: a cohort study. Sci Rep. (2020) 10:20812. doi: 10.1038/s41598-020-77886-2
16. Kausar R. State anxiety and coping strategies used by patients with hepatitis C in relation to interferon therapy. Pakistan Journal of Social and Clinical Psychology in 2011 (2018) 9(1):16–20.
17. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.v21:11
18. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
19. Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x
20. Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. (2020) 18:2127–33.
21. Chan H, Yu CS, Li SY. Psychiatric morbidity in Chinese patients with chronic hepatitis B infection in a local infectious disease clinic. East Asian Arch Psychiatry. (2012) 22:160–8.
22. Cortesi PA, Conti S, Scalone L, Jaffe A, Ciaccio A, Okolicsanyi S, et al. Health related quality of life in chronic liver diseases. Liver Int. (2020) 40:2630–42. doi: 10.1111/liv.v40.11
23. Daryani NE, Bashahsati M, Karbalaeian M, Keramati MR, Daryani NE, Yazdi AS. Prevalence of psychiatric disorders in hepatitis B virus carriers in Iranian charity for hepatic patients support (December 2004-august 2005). Hepat Mon. (2008) 8:201–5.
24. Karlidag GE, Atmaca M. The relationship between duration, stage and, treatment of illness and depression or anxiety in patients with chronic hepatitis B/Kronik hepatit B hastalarinda hastalik suresi, evresi ve tedavisinin depresyon ve anksiyete iliskisi. Anadolu Psikiyatri Dergisi. (2019) 20:515.
25. Gupta R, Avasthi A, Chawla YK, Grover S. Psychiatric morbidity, fatigue, stigma and quality of life of patients with hepatitis B infection. J Clin Exp Hepatol. (2020) 10:429–41. doi: 10.1016/j.jceh.2020.04.003
26. Kiratli KDÖ, Köse Ş. Evaluation of depression, anxiety and health-related quality of life in patients with hepatitis B virus-infection. FLORA. (2023) 28:264–74.
27. Liu M, Li L, Zheng SJ, Zhao J, Ungvari GS, Hall BJ, et al. Prevalence of major depression and its associations with demographic and clinical characteristics and quality of life in Chinese patients with HBV-related liver diseases. Arch Psychiatr Nurs. (2017) 31:287–90. doi: 10.1016/j.apnu.2017.02.004
28. Liu Y, Tang K, Long J, Zhao C. The association between hepatitis B self-awareness and depression: Exploring the modifying effects of socio-economic factors. J Viral Hepatitis. (2017) 24:330–6. doi: 10.1111/jvh.2017.24.issue-4
29. Chong L-W, Hsu C-C, Lee C-Y, Chou R-H, Lin C-L, Chang K-H, et al. Association of viral hepatitis and bipolar disorder: a nationwide population-based study. J Trans Med. (2018) 16:173. doi: 10.1186/s12967-018-1542-3
30. Marcellin P, Lau GKK, Zeuzem S, Heathcote EJ, Pockros PJ, Reddy KR, et al. Comparing the safety, tolerability and quality of life in patients with chronic hepatitis B vs chronic hepatitis C treated with peginterferon alpha-2a. Liver Int. (2008) 28:477–85. doi: 10.1111/j.1478-3231.2008.01696.x
31. Ngo XM, Nguyen TTH, Nguyen TTT, Doan LNG, Ngo NT, Lam TV, et al. Quality of life among Vietnamese patients with chronic hepatitis B: A cross-sectional study based on a self-report survey. SRP. (2019) 10:167–72.
32. Saffari M, Pakpour AH, Al Zaben F, Koenig HG. Is there an association between Health Related Quality of Life, socio-demographic status and Fatigue in Patients with Chronic Hepatitis B? Acta Gastroenterol Belg. (2017) 80:229–36.
33. Shaheen AA, Kaplan GG, Sharkey KA, Lethebe BC, Swain MG. Impact of depression and antidepressant use on clinical outcomes of hepatitis B and C: a population-based study. Hepatol Commun. (2023) 7:e0062. doi: 10.1097/HC9.0000000000000062
34. Vu TTM, Le TV, Dang AK, Nguyen LH, Nguyen BC, Tran BX, et al. Socioeconomic vulnerability to depressive symptoms in patients with chronic hepatitis B. Int J Environ Res Public Health. (2019) 16:255. doi: 10.3390/ijerph16020255
35. Weinstein AA, Kallman Price J, Stepanova M, Poms LW, Fang Y, Moon J, et al. Depression in patients with nonalcoholic fatty liver disease and chronic viral hepatitis B and C. Psychosomatics. (2011) 52:127–32. doi: 10.1016/j.psym.2010.12.019
36. Mutlu Yilmaz E, Yildiz IE, Sehmen E. Stigma, discrimination and living with hepatitis B in Turkey. Iranian Red Crescent Med J (IRCMJ). (2022) 24.
37. Yilmaz A, Ucmak F, Dönmezdil S, Kaya MC, Tekin R, Günes M, et al. Somatosensory amplification, anxiety, and depression in patients with hepatitis B: impact on functionality. Med (Baltimore). (2016) 95:e3779. doi: 10.1097/MD.0000000000003779
38. Zhu L, Lu W, Gamoso W, Tan Y, Johnson C, Ma GX. The association between modifiable lifestyle behaviors and depression among Asian Americans with chronic hepatitis B by medication status. Brain Sci. (2022) 12:188. doi: 10.3390/brainsci12020188
39. Ahmed J, Butt N, Rathore R, Iqbal A, Mehmood H, Waseem T. Prevalence of depression in patients of chronic hepatitis B and C presenting to Mayo Hospital Lahore. Pakistan J Med Health Sci. (2017).
40. Aktuğ Demir N, Çelik M, Kölgelier S, Sümer S, Aksöz S, Demir LS, et al. Comparison of the level of depression and anxiety in inactive hepatitis B carriers and chronic hepatitis B patients. Turk Psikiyatri Derg. (2013) 24:248–52.
41. Alian S, Masoudzadeh A, Khoddad T, Dadashian A, Ali Mohammadpour R. Depression in hepatitis B and C, and its correlation with hepatitis drugs consumption (interfron/lamivodin/ribaverin). Iran J Psychiatry Behav Sci. (2013) 7:24–9.
42. Chang R-Y, Hsueh-Hua-Ho S, Tsai H-L, Koo M. Association of anxiety and depression with chronic liver diseases in patients with noncardiac chest pain: A cross-sectional study. Medicine. (2022) 101:e29620. doi: 10.1097/MD.0000000000029620
43. Fotos NV, Elefsiniotis I, Patelarou A, Giakoumidakis K, Patelarou E, Kouros A, et al. Psychological disorders and quality of life among patients with chronic viral hepatitis: A single-center cross-sectional study with pair-matched healthy controls. Gastroenterol Nurs. (2018) 41:206–18. doi: 10.1097/SGA.0000000000000339
44. Gale SD, Berrett AN, Erickson LD, Brown BL, Hedges DW. Association between virus exposure and depression in US adults. Psychiatry Res. (2018) 261:73–9. doi: 10.1016/j.psychres.2017.12.037
45. Huang YW, Hu JT, Hu FC, Chang CJ, Chang HY, Kao JH, et al. Biphasic pattern of depression and its predictors during pegylated interferon-based therapy in chronic hepatitis B and C patients. Antivir Ther. (2013) 18:567–73. doi: 10.3851/IMP2441
46. Zhou F, Li J, Lin K, Ji P, Sun Y. Across-sectional study on anxiety and stress in pregnant women with chronic HBV infection in the People’s Republic of China. Neuropsychiatr Dis Treat. (2015) 11:2225–32.
47. Simonetti G, Gitto S, Golfieri L, Gamal N, Loggi E, Taruschio G, et al. Quality of life of hepatitis B virus surface antigen-positive patients with suppressed viral replication: comparison between inactive carriers and nucleot(s)ide analog-treated patients. Eur J Gastroenterol Hepatol. (2018) 30:14–20. doi: 10.1097/MEG.0000000000000999
48. Keskin G, Gümüs AB, Orgun F. Quality of life, depression, and anxiety among hepatitis B patients. Gastroenterol Nurs. (2013) 36:346–56. doi: 10.1097/SGA.0b013e3182a788cc
49. Kong L-N, Yao Y, Li L, Zhao Q-H, Wang T, Li Y-L. Psychological distress and self-management behaviours among patients with chronic hepatitis B receiving oral antiviral therapy. J Adv Nursing. (2021) 77:266–74. doi: 10.1111/jan.14610
50. Huang X, Zhang H, Qu C, Liu Y, Bian C, Xu Y. Depression and insomnia are closely associated with thyroid hormone levels in chronic hepatitis B. Med Sci Monit. (2019) 25:2672–8. doi: 10.12659/MSM.914444
51. Polenick CA, Perbix EA, Salwi SM, Maust DT, Birditt KS, Brooks JM. Loneliness during the COVID-19 pandemic among older adults with chronic conditions. J Appl Gerontol. (2021) 40:804–13. doi: 10.1177/0733464821996527
52. Depression Facts and Statistics: Healthline (2023). Available online at: https://www.healthline.com/health/depression/facts-statistics-infographic (Accessed January 2, 2025).
53. Javaid SF, Hashim IJ, Hashim MJ, Stip E, Samad MA, Ahbabi AA. Epidemiology of anxiety disorders: global burden and sociodemographic associations. Middle East Curr Psychiatry. (2023) 30:44. doi: 10.1186/s43045-023-00315-3
54. Maimaitituerxun R, Chen W, Xiang J, Xie Y, Kaminga AC, Wu XY, et al. Prevalence of anxiety and associated factors among inpatients with type 2 diabetes mellitus in China: A cross-sectional study. Psychiatr Quarter. (2023) 94:371–83. doi: 10.1007/s11126-023-10040-z
55. World Health Organisation. Hepatitis B. Geneva, Switzerland: WHO (2024). Available at: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b:~:text=Hepatitis%20B%20can%20cause%20a,a%20mother%20to%20her%20baby (Accessed January 2, 2025).
56. Lu W, Mak B, Lim SG, Aung MO, Wong ML, Wai CT. Public misperceptions about transmission of hepatitis B virus in Singapore. Ann Acad Med Singap. (2007) 36:797–800. doi: 10.47102/annals-acadmedsg.
57. Luo M. Social isolation, loneliness, and depressive symptoms: A twelve-year population study of temporal dynamics. J Gerontol B Psychol Sci Soc Sci. (2023) 78:280–90. doi: 10.1093/geronb/gbac174
58. Choi HG, Kim JH, Park JY, Hwang YI, Jang SH, Jung KS. Association between asthma and depression: A national cohort study. J Allergy Clin Immunol Pract. (2019) 7:1239–45.e1. doi: 10.1016/j.jaip.2018.10.046
59. Huang Y, Loux T, Huang X, Feng X. The relationship between chronic diseases and mental health: A cross-sectional study. Ment Health Prev. (2023) 32:200307. doi: 10.1016/j.mhp.2023.200307
60. Swathi M, Manjusha S, Vadakkiniath IJ, Gururaj A. Prevalence and correlates of stress, anxiety, and depression in patients with chronic diseases: a cross-sectional study. Middle East Curr Psychiatry. (2023) 30:66. doi: 10.1186/s43045-023-00340-2
61. Canadian Mental Health Association. The relationship between Mental Health, Mental Illness and Chronic Physical Conditions. Toronto, Ontario, Canada: Canadian Mental Health Association (2008). Available at: https://ontario.cmha.ca/documents/the-relationship-between-mental-health-mental-illness-and-chronic-physical-conditions/:~:text=Some%20chronic%20physical%20conditions%20can,which%20can%20impact%20brain%20function.&text=People%20living%20with%20chronic%20physical%20conditions%20often%20experience%20emotional%20stress,development%20of%20depression%20and%20anxiety (Accessed January 2, 2025).
62. National Institute of Mental Health. Understanding the Link Between Chronic Disease and Depression. Bethesda, Maryland, USA: National Institute of Mental Health (2024). Available at: https://www.nimh.nih.gov/health/publications/chronic-illness-mental-health:~:text=People%20who%20have%20a%20chronic,as%20Parkinson%27s%20disease%20or%20stroke (Accessed January 2, 2025).
63. Hayley S, Poulter MO, Merali Z, Anisman H. The pathogenesis of clinical depression: stressor- and cytokine-induced alterations of neuroplasticity. Neuroscience. (2005) 135:659–78. doi: 10.1016/j.neuroscience.2005.03.051
64. Hayley S, Merali Z, Anisman H. Stress and cytokine-elicited neuroendocrine and neurotransmitter sensitization: implications for depressive illness. Stress. (2003) 6:19–32. doi: 10.1080/1025389031000091167
65. Felger JC, Lotrich FE. Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience. (2013) 246:199–229. doi: 10.1016/j.neuroscience.2013.04.060
66. Berk M, Williams LJ, Jacka FN, O’Neil A, Pasco JA, Moylan S, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. (2013) 11:200.
67. Köhler CA, Freitas TH, Maes M, de Andrade NQ, Liu CS, Fernandes BS, et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr Scand. (2017) 135:373–87.
68. Zhang M, Wan M, Wang W, Lin S, Zhang X. Effect of interferon therapy on quality of life in patients with chronic hepatitis B. Sci Rep. (2024) 14:2461. doi: 10.1038/s41598-024-51292-4
69. Lai JY, Ho JX, Kow ASF, Liang G, Tham CL, Ho Y-C, et al. Interferon therapy and its association with depressive disorders – A review. Front Immunol. (2023) 14. doi: 10.3389/fimmu.2023.1048592
70. Hunt CM, Dominitz JA, Bute BP, Waters B, Blasi U, Williams DM. Effect of interferon-alpha treatment of chronic hepatitis C on health-related quality of life. Dig Dis Sci. (1997) 42:2482–6. doi: 10.1023/A:1018852309885
71. Taylor MW, Feng GS. Relationship between interferon-gamma, indoleamine 2,3-dioxygenase, and tryptophan catabolism. FASEB J. (1991) 5:2516–22. doi: 10.1096/fasebj.5.11.1907934
72. Pinto EF, Andrade C. Interferon-related depression: A primer on mechanisms, treatment, and prevention of a common clinical problem. Curr Neuropharmacol. (2016) 14:743–8. doi: 10.2174/1570159X14666160106155129
73. Wichers MC, Maes M. The role of indoleamine 2,3-dioxygenase (IDO) in the pathophysiology of interferon-alpha-induced depression. J Psychiatry Neurosci. (2004) 29:11–7.
74. Kumar S. Overview of Acute Viral Hepatitis MSD Manual Consumer Version: MSD Manual (2024). Available online at: https://www.msdmanuals.com/en-sg/home/liver-and-gallbladder-disorders/hepatitis/overview-of-acute-viral-hepatitis (Accessed January 2, 2025).
75. Croagh CM, Lubel JS. Natural history of chronic hepatitis B: phases in a complex relationship. World J Gastroenterol. (2014) 20:10395–404. doi: 10.3748/wjg.v20.i30.10395
76. Lai M, Hyatt BJ, Nasser I, Curry M, Afdhal NH. The clinical significance of persistently normal ALT in chronic hepatitis B infection. J Hepatol. (2007) 47:760–7. doi: 10.1016/j.jhep.2007.07.022
77. Chen YC, Chu CM, Liaw YF. Age-specific prognosis following spontaneous hepatitis B e antigen seroconversion in chronic hepatitis B. Hepatology. (2010) 51:435–44. doi: 10.1002/hep.23348
78. Croagh CM, Bell SJ, Slavin J, Kong YX, Chen RY, Locarnini S, et al. Increasing hepatitis B viral load is associated with risk of significant liver fibrosis in HBeAg-negative but not HBeAg-positive chronic hepatitis B. Liver Int. (2010) 30:1115–22. doi: 10.1111/j.1478-3231.2010.02267.x
79. Divo MJ, Martinez CH, Mannino DM. Ageing and the epidemiology of multimorbidity. Eur Respir J. (2014) 44:1055–68. doi: 10.1183/09031936.00059814
80. Triolo F, Harber-Aschan L, Belvederi Murri M, Calderón-Larrañaga A, Vetrano DL, Sjöberg L, et al. The complex interplay between depression and multimorbidity in late life: risks and pathways. Mech Ageing Dev. (2020) 192:111383. doi: 10.1016/j.mad.2020.111383
81. Gerlach LB, Solway ES, Malani PN. Social isolation and loneliness in older adults. JAMA. (2024) 331:2058–. doi: 10.1001/jama.2024.3456
82. Li L, Pan K, Li J, Jiang M, Gao Y, Yang H, et al. The associations of social isolation with depression and anxiety among adults aged 65 years and older in Ningbo, China. Sci Rep. (2024) 14:19072. doi: 10.1038/s41598-024-69936-w
83. Chlapecka A, Kagstrom A, Cermakova P. Educational attainment inequalities in depressive symptoms in more than 100,000 individuals in Europe. Eur Psychiatry. (2020) 63:e97. doi: 10.1192/j.eurpsy.2020.100
84. Li L, Sun W, Luo J, Huang H. Associations between education levels and prevalence of depressive symptoms: NHANES (2005–2018). J Affect Disord. (2022) 301:360–7. doi: 10.1016/j.jad.2022.01.010
85. Mirowsky J. Education, Social Status, and Health, 1st ed. New Brunswick, NJ: Aldine Transaction (2023). doi: 10.4324/97813513280812003.
86. Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. (2018) 39:273–89. doi: 10.1146/annurev-publhealth-031816-044628
87. Soong RY, Low CE, Ong V, Sim I, Lee C, Lee F, et al. Exercise interventions for depression, anxiety, and quality of life in older adults with cancer: A systematic review and meta-analysis. JAMA Netw Open. (2025) 8:e2457859–e. doi: 10.1001/jamanetworkopen.2024.57859
88. Niemeyer H, Bieda A, Michalak J, Schneider S, Margraf J. Education and mental health: Do psychosocial resources matter? SSM Popul Health. (2019) 7:100392.
89. Lim MH, Manera KE, Owen KB, Phongsavan P, Smith BJ. The prevalence of chronic and episodic loneliness and social isolation from a longitudinal survey. Sci Rep. (2023) 13:12453. doi: 10.1038/s41598-023-39289-x
90. Ronaldson A, Arias de la Torre J, Prina M, Armstrong D, Das-Munshi J, Hatch S, et al. Associations between physical multimorbidity patterns and common mental health disorders in middle-aged adults: A prospective analysis using data from the UK Biobank. Lancet Regional Health – Europe. (2021) 8. doi: 10.1016/j.lanepe.2021.100149
91. Goodwin GM. Depression and associated physical diseases and symptoms. Dialogues Clin Neurosci. (2006) 8:259–65. doi: 10.31887/DCNS.2006.8.2/mgoodwin
92. Tan JY, Ge G, Low CE, Rana S, Tan TYZ, Fang NBJ, et al. Suicide and suicidal ideation among survivors of childhood cancer: A systematic review and meta-analysis. JAMA Netw Open. (2025) 8:e2457544–e. doi: 10.1001/jamanetworkopen.2024.57544
93. Streit F, Völker MP, Klinger-König J, Zillich L, Frank J, Reinhard I, et al. The interplay of family history of depression and early trauma: associations with lifetime and current depression in the German national cohort (NAKO). Front Epidemiol. (2023) 3:1099235. doi: 10.3389/fepid.2023.1099235
94. Perich T, Andriessen K. The impact of family history of mental illness on mental health help seeking in university students. J Ment Health. (2024), 1–7. doi: 10.1080/09638237.2024.2361235
95. Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. (2000) 157:1552–62. doi: 10.1176/appi.ajp.157.10.1552
96. Dehle C, Larsen D, Landers JE. Social support in marriage. Am J Family Ther. (2001) 29:307–24. doi: 10.1080/01926180126500
97. Thoits PA. Social support as coping assistance. J Consult Clin Psychol. (1986) 54:416–23. doi: 10.1037/0022-006X.54.4.416
98. Burke RJ, Weir T. Marital helping relationships: the moderators between stress and well-being. J Psychol. (1977) 95:121–30. doi: 10.1080/00223980.1977.9915868
99. Blood RO Jr., Wolfe DM. Husbands and wives: The dynamics of family living. Glencoe, Illinois: Free Press Glencoe (1960).
100. Acoba EF. Social support and mental health: the mediating role of perceived stress. Front Psychol. (2024) 15. doi: 10.3389/fpsyg.2024.1330720
101. Vaingankar JA, Abdin E, Chong SA, Shafie S, Sambasivam R, Zhang YJ, et al. The association of mental disorders with perceived social support, and the role of marital status: results from a national cross-sectional survey. Arch Public Health. (2020) 78:108. doi: 10.1186/s13690-020-00476-1
102. Lee ARYB, Low CE, Yau CE, Li J, Ho R, Ho CSH. Lifetime burden of psychological symptoms, disorders, and suicide due to cancer in childhood, adolescent, and young adult years: A systematic review and meta-analysis. JAMA Pedia. (2023) 177:790–9. doi: 10.1001/jamapediatrics.2023.2168
103. Wijeratne T, Sales C. Understanding why post-stroke depression may be the norm rather than the exception: the anatomical and neuroinflammatory correlates of post-stroke depression. J Clin Med. (2021) 10. doi: 10.3390/jcm10081674
104. Medeiros GC, Roy D, Kontos N, Beach SR. Post-stroke depression: A 2020 updated review. Gen Hosp Psychiatry. (2020) 66:70–80. doi: 10.1016/j.genhosppsych.2020.06.011
105. Low CE, Pillay RM, Teo FJJ, Loh CYL, Yau CE, Yan Bin Lee AR, et al. Educational interventions to reduce depression and anxiety in older adults with cancer in the community: a systematic review, meta-analysis and meta-regression of randomised controlled trials. Age Ageing. (2024) 53:afae111. doi: 10.1093/ageing/afae111
106. Massey CN, Feig EH, Duque-Serrano L, Wexler D, Moskowitz JT, Huffman JC. Well-being interventions for individuals with diabetes: A systematic review. Diabetes Res Clin Pract. (2019) 147:118–33. doi: 10.1016/j.diabres.2018.11.014
107. Fisher V, Li WW, Malabu U. The effectiveness of mindfulness-based stress reduction (MBSR) on the mental health, HbA1C, and mindfulness of diabetes patients: A systematic review and meta-analysis of randomised controlled trials. Appl Psychol Health Well Being. (2023) 15:1733–49. doi: 10.1111/aphw.12441
108. Alberts CJ, Clifford GM, Georges D, Negro F, Lesi OA, Hutin YJF, et al. Worldwide prevalence of hepatitis B virus and hepatitis C virus among patients with cirrhosis at country, region, and global levels: a systematic review. Lancet Gastroenterol Hepatol. (2022) 7:724–35. doi: 10.1016/S2468-1253(22)00050-4
Keywords: hepatitis B, viral infection, mental health, depression, anxiety
Citation: Low CE, Ge G, Yeong TJJ-M, Rana S, Loke S, Kow WC, Lee ARYB and Ho CSH (2025) Burden of psychological symptoms and disorders among individuals with hepatitis B: a systematic review, meta-analysis and meta-regression. Front. Psychiatry 16:1546545. doi: 10.3389/fpsyt.2025.1546545
Received: 17 December 2024; Accepted: 06 March 2025;
Published: 24 March 2025.
Edited by:
Marcin Siwek, Jagiellonian University, PolandReviewed by:
Adrian Andrzej Chrobak, Jagiellonian University, PolandKaterina Karaivazoglou, University of Patras, Greece
Paweł Dębski, Medical University of Silesia, Poland
Copyright © 2025 Low, Ge, Yeong, Rana, Loke, Kow, Lee and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cyrus Su Hui Ho, cGNtaHNoQG51cy5lZHUuc2c=
†These authors have contributed equally to this work and share first authorship
 Chen Ee Low
Chen Ee Low Genevieve Ge1†
Genevieve Ge1† Wei Chieh Kow
Wei Chieh Kow Ainsley Ryan Yan Bin Lee
Ainsley Ryan Yan Bin Lee Cyrus Su Hui Ho
Cyrus Su Hui Ho