
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 27 March 2025
Sec. Adolescent and Young Adult Psychiatry
Volume 16 - 2025 | https://doi.org/10.3389/fpsyt.2025.1538476
This article is part of the Research TopicMental Health Challenges in Health Professions EducationView all 7 articles
 Zahra Jabari1†
Zahra Jabari1† Mohammad Eslami1†
Mohammad Eslami1† Amir Hossein Jalali Nadoushan2
Amir Hossein Jalali Nadoushan2 Salime Goharinezhad3
Salime Goharinezhad3 MohammadJavad Tavallaei1
MohammadJavad Tavallaei1 Elaheh Khodadoust1,4*
Elaheh Khodadoust1,4* Seyed Mohammad Hossein Mahmoodi2*
Seyed Mohammad Hossein Mahmoodi2*Introduction: Medical students face a high prevalence of mental disorders, such as depression, alongside inadequate mental health literacy (MHL). This study investigates the feasibility, and efficacy of an interactive, gamified educational program in improving participants’ MHL.
Method: Thirty-two Iranian medical students participated in a semi-experimental pretest-post-test study. An 18-hour online program, delivered using the flipped classroom method, focused on mental health first aid, stigma, stress management, and subjective well-being (SWB) skills. Participants were evaluated before, after, and four months post-program using the Mental Health Literacy Scale (MHLS), Mental Health Promoting Knowledge (MHPK), and World Health Organization-5 Well-being Index (WHO-5).
Results: Participants' mean age was 22.78 ( ± 4.54). Post-test results showed significant improvement in MHLS and MHPK scores (P-values< 0.05), which were sustained at the four-month follow-up (P-values>0.01). SWB improved in the post-test evaluation (P-value= 0.058).
Conclusion: The educational program effectively improved medical undergraduates’ MHL and SWB. Given the rising concerns about medical students’ mental health, implementing such curricula appears promising for long-term benefits.
The World Health Organization (WHO) defines health as a state of complete physical, mental, and social well-being, not merely the absence of disease or infirmity (1). Despite this definition, which emphasizes mental health as a key domain, mental health disorders account for around 14% of the global disease burden and eight million deaths annually (2, 3). Each year, about 800,000 people commit suicide, with a notable number of them being young individuals aged 15-24 (4).
The prevalence of mental health issues among medical science students is significantly higher than in the general population, with over half of those studying medicine experiencing psychological tensions (5–8). Furthermore, our previous investigation revealed low scores among university students. Additionally, there was a high rate of individuals screened positive for clinical depression (9). A meta-analysis found that approximately 28% of 17,560 medical students experience depression (10). This issue is also emphasized in many studies worldwide (11–14). Another meta-analysis showed that the prevalence of depression among medical students in the Middle East is around 31.8 %, which is more than the prevalence of depression in medical students in North America (30.3%), Asia (30.1%), South America (26.8%), and Europe (20%) (7).
In Iran, and specifically among medical students, the prevalence of depression and suicide ideation has become a rising concern (10, 15–18). According to the Iranian Psychiatric Association, there have been 16 cases of suicide by resident doctors in just nine months (19).
These estimates suggest that mental health disorders among medical students contribute to a significant public health challenge, necessitating urgent interventions to address this burden (20, 21). Improving mental health literacy (MHL), defined as 'knowledge and beliefs about mental disorders that aid in their recognition, management, or prevention,' can empower communities to pursue better mental health (22, 23). This definition is complemented by positive mental health literacy, which refers to a person’s knowledge about improving and preserving good mental health (23).
The WHO's comprehensive mental health action plan identifies public mental health awareness as one of the initial strategies in mental health prevention, with higher MHL associated with better mental health outcomes (24). In Iran, a cross-sectional study revealed a significant lack of MHL among medical students (25, 26). MHL is considered a modifiable factor (27, 28), and empowering students with resilience and mental health-related skills has been identified as a student support strategy (29). Developing preventive and educational interventions for this at-risk population is suggested, with improving MHL showing cost-effective and promising results (27, 30, 31). A systematic review of mental health first aid training trials revealed that improvement in different aspects of MHL is achievable, but long-term improvements are still a challenge (32).
While training programs are recommended to improve MHL, interactive teaching methods are necessary to create effective and practical learning. Studies suggest that methods such as gamification and scenario-based learning enhance educational outcomes by actively engaging participants and fostering critical thinking. These methods have shown promise in improving mental health literacy by creating immersive and memorable learning experiences (33–36). A systematic review by Mohammadi et al. (2020) highlighted the effectiveness of interactive methods, including role-playing, games, and multimedia approaches, in mental health literacy interventions among adolescents (37). However, their application in medical students remains underexplored. Recognizing the importance of improving mental health literacy (MHL) among medical students, our team developed and implemented an interactive, didactic program called *Psycheutopia* for a group of Iranian medical students. This initiative aimed to enhance their MHL as a critical step toward fostering their psychological well-being. In essence, our study had two primary objectives: first, to design a program tailored to improve MHL among medical students, and second, to evaluate its effectiveness.We hypothesize that Psycheutopia will significantly improve mental health literacy (MHL) and subjective well-being (SWB) among medical students.
In this study, we designed a curriculum and evaluated its efficacy in improving MHL. The study method contains two phases: A. Design and module development and B. implementation & evaluation. Each phase is explained below (Figure 1).
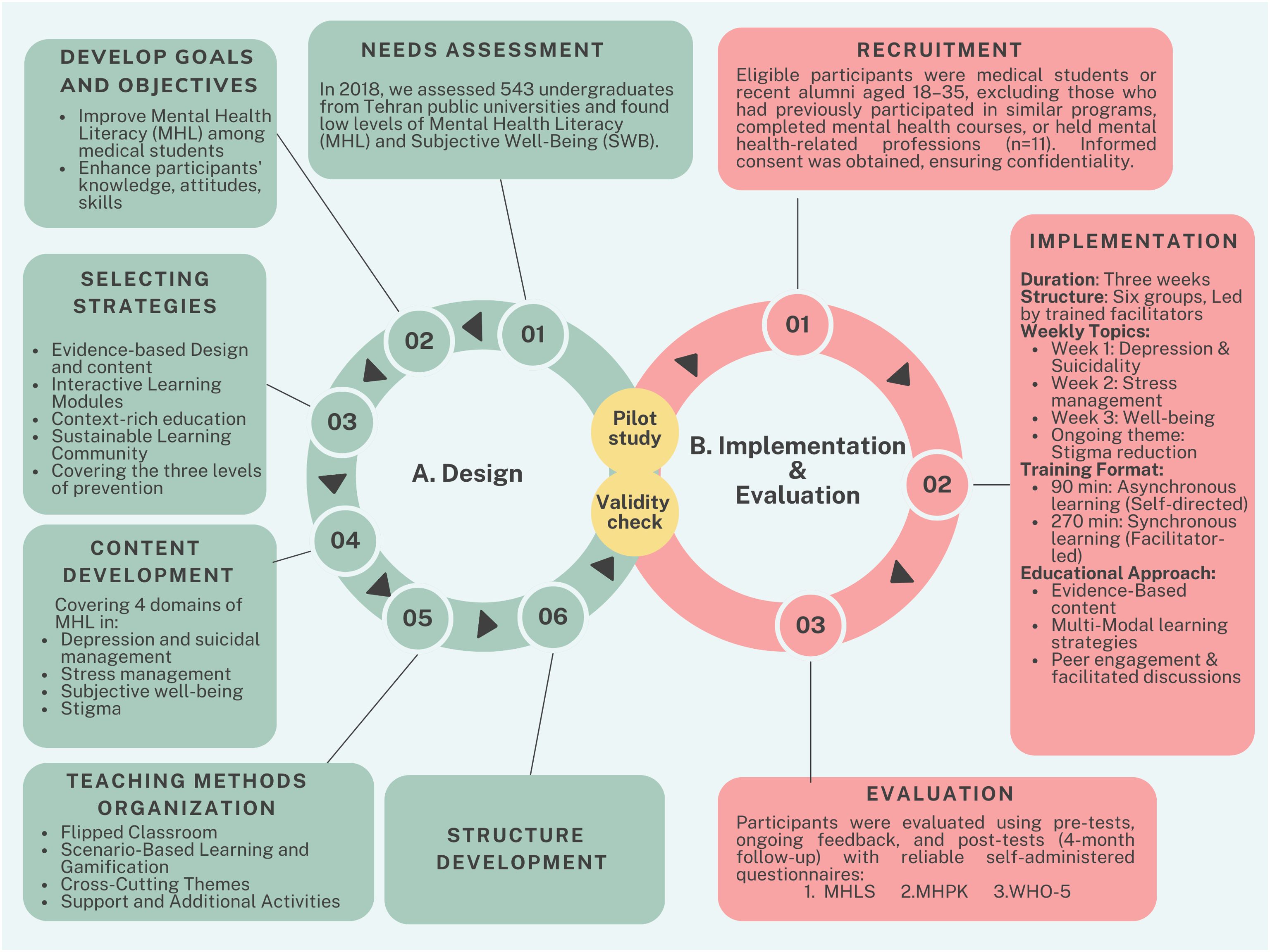
Figure 1. Overview of the Study Phases: The study was conducted in multiple phases, including the design, implementation & evaluation as the main phases. The figure illustrates the progression of these phases, (A) starting with program design and refinement, followed by validation and pilot testing to ensure feasibility. (B) The final phases involved program implementation and its subsequent evaluation to assess outcomes and effectiveness.
This curriculum was developed based on Harden's ten questions for curriculum planning as a guiding framework (38). After conducting a needs assessment study, we established the goals and objectives for this curriculum and selected relevant content and effective teaching strategies. The initial version of the program was piloted as a three-day in-person event in February 2020 and a sample size of 20 to 30 participants was considered sufficient for the pilot.
In response to the emerging COVID-19 pandemic, this program was subsequently adapted to an online format.
In 2018, our team conducted a descriptive cross-sectional study to measure the levels of MHL and SWB among the undergraduates of Tehran public universities. MHL qualities were measured in 543 students and the results revealed insufficient MHL and WB among the participants (26).
Our primary objective was to address the issue of inadequate MHL among students. As the initial step to improve MHL and Subjective Well-Being (SWB) among them, we concentrated on medical students. Despite mental disorder diagnosis and treatment being part of their curriculum, our needs assessment revealed their MHL levels were no different from those of other students.
In response to the needs assessment, we designed Psycheutopia as a comprehensive program with these objectives:
● Develop an effective educational program to enhance mental health literacy among medical students.
● Cater to the diverse educational needs of participants by covering topics across different levels of mental health prevention: illness first aid, primary prevention, and promotion.
● Improve participants’ knowledge, attitude, and, particularly, skills.
● Establish a learning community where educators, organizers, and participants can collectively learn, apply, and disseminate the acquired knowledge in the future.
To accomplish these ambitious objectives, we devised five key strategies:
● Evidence-based Design and content: Utilize exclusively evidence-based learning methods and materials.
● Interactive Learning Modules: Create a genuinely interactive educational environment that is also enjoyable to boost learners’ motivation and active participation throughout an online program.
● Context-rich education: Offer an education that is rich in context, making the topics applicable to the participants' daily lives. This approach helps translate knowledge into practice and fosters the development of higher cognitive skills in line with Bloom’s taxonomy.
● Covering the three levels of prevention: prepare the program in a way not only to reduce the risk of being involved by mental disorders but also to be capable of facing it and overcoming it during our lives.
● Sustainable Learning Community: Foster an ongoing learning community where participants can continuously share knowledge and best practices.
To pursue our objectives, the curriculum was constructed based on the four domains of MHL (22):
1. Understanding how to obtain and maintain good mental health.
2. Understanding mental disorders and treatment.
3. Decreasing stigma against mental illness.
4. Enhancing help-seeking efficacy.
A part of our curriculum focused on early detection and immediate support for mentally distressed peers, emphasizing self-care strategies during crises. This section specifically addressed depression and suicidality, the most common mental health challenges, and was adapted from the evidence-based Mental Health First Aid (MHFA) action plan. MHFA has demonstrated effectiveness in enhancing mental health literacy, reducing stigma, and fostering supportive behaviors (32, 36, 39, 40).
Secondly, medical students are dealing with daily psychological stress that makes them vulnerable to burnout, depression, and anxiety disorders. Learning stress management skills and fostering resilience were included in the program’s content to help students prevent mental disorders and promote their SWB and productivity (41).
Moreover, based on the World Health Organization’s (WHO) definition of health, being healthy is not just the absence of disease but a satisfactory status of well-being (1). Positive mental health literacy, which refers to a person’s knowledge about enhancing and preserving good mental health, was also addressed in this curriculum (42, 43).
Finally, stigma was approached independently in this program. Participants were challenged to think about different types of stigmas in various contexts and their roles in destigmatizing mental disorders and facilitating help-seeking behaviors.
Therefore, our content concentrated on four topics to address all domains of MHL (Figure 2). The content validity was verified by experts who reviewed and critically revised all created learning materials. Initially, in three sessions involving one psychiatry resident and three general medical students, the findings of previous studies on students' mental health literacy (MHL) were reviewed. This included a needs assessment previously conducted by our team and global studies aimed at improving MHL, such as those based on Mental Health First Aid (MHFA). Educational topics were selected with consideration of the cultural and linguistic context of the target population. In the next step, essential scientific content for these topics was gathered from public education resources. Subsequently, using scenario-based methods, games, and other interactive techniques, the format for delivering this content was developed. The content and its delivery format were then evaluated by two experts—a psychiatry resident and a psychiatry professor—who provided necessary revisions. This process was repeated until content validity and face validity were confirmed by the experts. Finally, to complete the assessment of face validity, four individuals from the target population also reviewed the materials.

Figure 2. Domains of mental health literacy: the figure illustrates the four core domains of mental health literacy addressed in this study, which formed the basis for the program, 's content development.
Aiming to create an online, interactive, and context-rich learning environment to foster life skills, and considering our objectives, we used various educational methods, including flipped classroom, scenario-based learning, gamification, self-reflective learning, and cross-cutting themes.
The program included 4.5 hours of asynchronous and 13.5 hours of synchronous sessions over three weeks. Asynchronous materials like educational videos were provided online, with support from facilitators. Weekly synchronous sessions involved missions and group activities to reinforce learning (43, 44).
Activities were designed around an engaging scenario with participants playing key roles in providing a context-rich environment. Gamification strategies such as storylines, instant feedback, and leaderboards were used to increase motivation and engagement (40).
The theme of stigma was integrated throughout the program with the aim of more in-depth training to change attitudes.
Participants received a mailed educational package to bridge the gap between online and in-person experiences. Additional support included an anonymous chat box for personal questions and weekly Q&A sessions with psychiatric residents. Emergency hotlines were also provided for ongoing support.
Teaching methods were adjusted to suit specific educational objectives, with different methods used for different topics, such as scenario-based learning for mental health first aid and self-reflective learning for subjective well-being. Examples of these educational activities are summarized in Table 1.
In the scenario of this program, participants play their role as citizens trying to make a utopia for mental health, which the name of this program Psycheutopia is inspired by. Participants spend three weeks in this program; each week is specified for a topic (depression and suicidality, stress management, and well-being), while a longitudinal topic (stigma) goes on during the whole workshop. During each week, materials and contents are presented to participants as the asynchronous part of the flipped classroom. At the end of the week, they practice what they have learned under the guidance of their facilitators during a synchronous session in groups of six. This structure is specifically designed to improve participants’ skills as mentioned above. A detailed instruction for the program is provided in Supplementary Material A.
In this quasi-experimental pre-post test study, the didactic program Psycheutopia was implemented over a three-week online course in 2021. This study was conducted at Iran University of Medical Sciences in Tehran, Iran upon the approval of the Bioethics Committee of the Iran University of Medical Sciences.
In this study, 43 students who volunteered to participate in this program were assessed for eligibility according to the following criteria: a) aged between 18 to 35 years, b) medical students, or alumni who graduated within the past six months, and c) able to participate in at least 80% of each synchronous session. Students with former experience in mental health, such as those who had participated in similar programs or mental health courses and those who had mental health-related professions, were excluded (n=11). Before the program’s initiation, the eligible participants provided informed consent to participate in this study, and they were assured that their personal information would be kept confidential.
Over three weeks, participants were divided into six groups, each supervised by a trained facilitator. These facilitators were students who had completed the pilot program and subsequently volunteered to join the team. Before the workshops, they underwent 10 hours of training, with their curriculum details outlined in Supplementary Materials B. Feedback on their performance was provided through fast-forward simulations, as described in Supplementary Materials A.
Each week focused on a specific theme: the first week addressed coping with depression and suicidal ideation, the second focused on stress management, and the third targeted improving overall well-being. Additionally, a longitudinal theme addressing stigma was integrated throughout the program.
Participants engaged in 90 minutes of asynchronous training weekly, followed by 270 minutes of interactive online sessions led by facilitators and trainers. Each topic included a comprehensive lesson plan with classroom activities and core and supplementary resources. To deliver the content, we used diverse media, including team-produced videos and podcasts. Influencers in the self-development field were also involved to enhance engagement. The program’s face and content validity were verified prior to implementation.
Our primary outcome was improving mental health literacy by the end of the program. In other words, Participants should be able to understand how to obtain and maintain positive mental health, understand mental disorders, decrease their stigma related to mental disorders, and enhance their help-seeking efficacy.
Our secondary outcome was that in addition to improving subjective well-being, lay the groundwork for developing stress management skills and mental health first aid skills not just as a person as a medical professional but as a member of society.
Evaluating outcomes were through summative assessments using self-administered online questionnaires, including the Mental Health Literacy Scale (MHLS) (45), the Mental Health Promoting Knowledge (MHPK) (46), and the World Health Organization (WHO)-5 Well-being Index (WHO-5) (47) questionnaires at baseline, after the program and at four-month follow-up. These tools measured various domains of MHL, positive mental health literacy, and subjective well-being, The psychometric properties of the utilized questionnaires are detailed in Supplementary Materials C.
Formative assessments also provided ongoing feedback during the program, involving self-reflective and peer assessments, with performance scored and ranked on a leaderboard (Figure 3).
Participants’ satisfaction with the program was evaluated at three-time points using a mixed-methods approach. A total of 17 quantitative questions were presented on a five-point Likert scale, addressing three domains:
1. Content satisfaction (four questions): Assessing the scientific quality and informativeness of the material.
2. Format satisfaction (four questions): Evaluating the presentation style and engagement.
3. Facilitator performance (nine questions): Measuring participants’ impressions of the facilitator’s skills and effectiveness.
In addition, seven open-ended qualitative questions were used to explore participants’ feedback in greater detail to identify general trends and consistency with quantitative findings.
The sample size was calculated using GPower software (version 3.1) for a two-sided paired t-test, with an expected effect size of 0.5, a significance level of 0.05, and a power of 80%. Adjustments for a potential dropout rate of 6% (2 participants) were also included, resulting in a planned recruitment of 32 participants to retain 30 effective participants.
The collected data were analyzed using SPSS 27.0. Numeric variables were reported as means with standard deviation (SD). Categorical variables were presented as percentages. The mean scores of the MHLS, MHPK, and SWB were analyzed according to a single-group design with repeated measurements analysis of variance (RM-ANOVA), and the Wilks’ Lambda test was used to test the normality of the data for the study variables. The graphs were created using GraphPad Prism version 9.1.1 for Mac, developed by GraphPad Software, San Diego, California, USA, available at www.graphpad.com. A two-sided significance level of 0.05 was used during the statistical testing and 95% confidence intervals (95% Cl) were calculated for the point estimates.
A total of 43 medical students volunteered to enroll in this semi-experimental study. Thirty-two candidates, including 18 females and 14 males, fulfilled the eligibility criteria (Figure 4).
The mean age of the participants was 22.78 (4.54). At baseline, 53.1% of participants reported having a friend or family member with a psychiatric condition. Ninety percent of participants judged their mental health status as healthy or relatively healthy, and 68.1% had never been visited by a psychiatrist or a mental health professional (Table 2).
A repeated measured ANOVA test revealed significant changes in MHLS (P-value<0.01(, MHPK (P-value=0.03), and SWB scores (P-value=0.02) over the four-month follow-up. The statistical results are summarized in Table 3 (Table 3).
As shown in Figure 5, the MHLS and MHPK scores significantly increased after the intervention (P-value= 0.02, P-value=0.03, respectively), and the changes were maintained during the four-month follow-up (P-value<0.01, P-value <0.01, respectively) in comparison with the baseline levels. Participants’ SWB scores increased by the end of the intervention (P-value=0.05, respectively); but decreased slightly after the workshop (Figure 5c) while remaining higher than baseline levels.
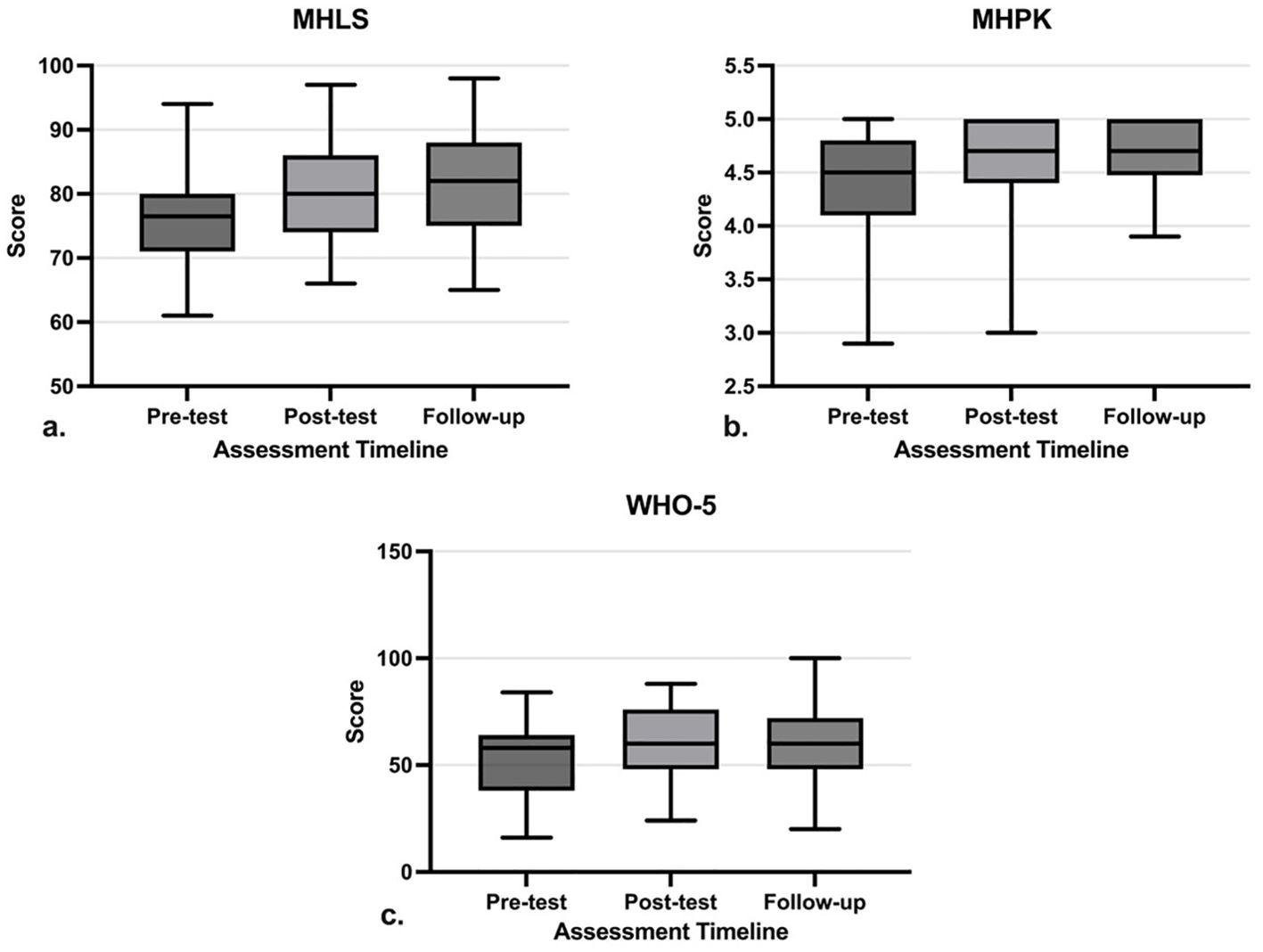
Figure 5. Trends of changes from pre-test to post-test and follow-up. The Whisker represents the range and the box demonstrates the 25th percentile (Q1) to the 75th percentile (Q3) with the median inside. (a) Mental Health Literacy Scale score, (b) Mental Health Promoting Knowledge score, (c) WHO-5 Wellbeing Index score.
The quantitative analysis of participants’ satisfaction demonstrated consistently high ratings across all assessed domains. Among the domains, facilitator performance received the highest rating (M = 4.65, SD = 0.45), followed by content satisfaction (M = 4.43, SD = 0.46) and format satisfaction (M = 4.32, SD = 0.56).
In this study, we designed and assessed the efficacy of Psycheutopia, a meticulously designed three-week online educational program aimed at enhancing the MHL among medical students. The program incorporated a range of interactive teaching methods and covered various aspects of mental health prevention and promotion. The results demonstrated a significant improvement in students’ MHL following the intervention, which was sustained at a four-month follow-up. Additionally, students’ well-being significantly improved both after the program and at the four-month follow-up. Our results demonstrated that participants with lower MHL showed substantial improvements following the intervention compared to those with higher MHL at the baseline.
The primary goal of this study was to enhance mental health literacy among medical students, with a focus on prevention and promotion. Mental health has been reframed into a spectrum ranging from complete health to illness, and it would be challenging to draw a line between different stages. Global mental health initiatives, such as the Lancet Commission, emphasize the importance of promoting mental health and reducing stigma as critical elements of sustainable development (48). To the best of our knowledge, only one educational program targeting medical specialties had a comprehensive approach to addressing the mental health continuum by far (49). Enhancing public awareness and encouraging help-seeking behaviors are particularly emphasized in Low- and Middle-Income Countries (LMICs), where targeted interventions like life skills education and stigma reduction are key strategies (50). While these interventions share common goals across populations, tailoring them to specific needs remains vital yet challenging.
This study demonstrated improvement in mental health literacy and positive mental health literacy after the program, which was sustained for four months. This result is consistent with other studies. Kurki et al. implemented a digital MHL program designed for medical students, focusing on life skills, stress management, and mindfulness. The program significantly improved mental health knowledge and reduced emotional symptoms, with these benefits persisting at a two-month follow-up. However, initial improvements in stress levels and help-seeking attitudes were not sustained, and stigma toward mental illness showed no significant change (49). In a peer-led program in university and secondary schools, Patalay et al. showed improvements in mental health literacy among school students, whereas a change in non-stigmatizing attitudes had the most significant effect size (51). Davies revealed that following a six-week e-learning mental health first aid program led to a decline in stigmatizing attitudes and improved helping intentions among medical students (52). A meta-analysis of 25 education interventions addressing MHL or stigma has shown these programs were associated with long-term improvements in MHL (53). It also emphasizes the importance of an educational condition to the outcome of the study. Consistent with our curriculum, this study suggests MHL is not limited to understanding symptoms and addressing other aspects of mental health literacy such as stigma, positive mental health literacy, and resilience is necessary and just relevant. On the other hand, the evidence around the long-term change in stigmatized attitudes following such interventions was less clear.
Another notable finding was the sustained improvement in well-being as the secondary outcome. Program components, such as stress management and practical skill-building, contributed directly to this outcome. Broader factors, including the program’s interactive nature, supportive environment, and the opportunity for meaningful engagement during the COVID-19 pandemic, may also have played a role. Some evidence suggests that interactive teaching methods can improve students’ well-being, regardless of the topic (54).
As stated in the Lancet Commission on Global Mental Health, the movement advocating for subjective well-being and happiness are one of the key indicators of a nation's development and it highlights the importance of promoting and protecting mental health for everyone, regardless of the presence of mental disorders (48). In our previous survey, we did not find a significant association between MHL and subjective well-being (9). Therefore, the improvement in well-being in this MHL educational program warrants further consideration.
The learning environment plays a crucial role in the success of such interventions. One of the primary challenges of mental health intervention in LMICs is the low compliance of the target population (55), which highlights the importance of using engaging and enjoyable teaching methods. Our teaching method was associated with a high level of satisfaction among participants while all participants completed the course of training. Participants highlighted the workshop’s engaging and informative content, the practicality of its delivery, and the facilitator’s expertise, collectively reflecting an overall very high level of satisfaction. Furthermore, the context-rich environment of Psycheutopia facilitated the translation of knowledge into practice. The relevance of the program to daily living situation, likely contributed to the sustained impact observed at the four-month follow-up. Consistent with our findings, previous studies have shown applying knowledge in real-world contexts, aligned with Bloom’s application level enhances student engagement, deepens understanding, and improves long-term retention (56). Moreover, incorporating student-centered elements into medical curricula can significantly reduce depressive symptoms (57).
The thoughtful design of the program and the novel use of various teaching methods to suit the audiences’ needs are other noteworthy features of this experience. Mohammadi identified five key factors that facilitate successful mental health interventions for adolescents: 1. Interactive learning environment, 2. Diverse and stimulating educational content, 3. trainers with different backgrounds, 3. Direct contact with people with mental disorders and 5. Utilizing technologies in education (37). These elements were integrated into the design of Psycheutopia, contributing to its effectiveness.
Sustainability and scalability are critical challenges in the design and implementation of such interventions (50). Similar to our experience, other successful online educational programs have found scenario-based or gamified teaching methods to be effective tools for creating a meaningful and engaging learning environment, for example, for nurses and adolescents (58, 59). Combining individual and team learning in an online environment may be a distinctive characteristic of Psycheutopia compared to similar interventions. In our program, learners exercise individually and then actively practice with other participants in online meetings.
Online interventions offer a cost-effective solution with broad accessibility. In a meta-analysis of 48 studies, the impact of internet-based mental health interventions on students has been evaluated as beneficial. These interventions have been found to enhance student's performance across various conditions (60). It is also recommended to reduce the role of specialists and facilitate community involvement in designing and implementing such interventions (48). Mental health program implemented by mental health professionals is associated with a significant cost, which poses a challenge to the feasibility and sustainability of such programs. Peer-delivered health promotion programs have shown efficacy in improving health literacy among students (51). Community-driven approaches further reduce reliance on specialists, addressing resource constraints in LMICs (48).
Psycheutopia exemplifies a community-based intervention created and implemented by medical students for their peers, building capacity under scientific supervision to make meaningful contributions. Students involved in the design and organization of the program not only contributed to its success but also benefited from learning and practicing the content themselves. Numerous interventions delivered by peers aim to improve young people's health, yet only a small number have been created and designed by young people themselves (61). Involving students in both the development and delivery of these programs has the potential to create more relevant and sustainable solutions (51). Additionally, evidence shows engaging students in the provision of a program is associated with their higher well-being and academic achievement, as well as long-term outcomes such as work success, personal development, and life-long learning (62). In several studies, the impact of peer-based mental health interventions on groups of students showed promising results (63–66), particularly in improving MHL (51). This concept is not limited to students, and the positive outcomes of Civil Engagement (CE) in the design and delivery of health services have been highlighted as an effective strategy to strengthen the health system (67, 68).
The primary limitation of this study is its semi-experimental design and lacking a control group. Although we compared measurements to students’ previous results using paired matches, the inclusion of a non-intervened group could have provided a clearer picture of the program’s efficacy.One limitation of our study is the selection of the target population, as participants were recruited on a voluntary basis. This self-selection process may introduce bias, as individuals who volunteered may differ in significant ways from the general population, such as being more motivated or health-conscious. Additionally, the majority of our participants were female, which may limit the generalizability of our findings to male populations. Future studies should aim for more diverse sampling methods to ensure a more representative distribution of participants across genders and other demographic factors. Additionally, while skill development was assessed through ongoing formative feedback, data on actual skill acquisition was not collected. Future studies should include skill development measures to complement knowledge-based outcomes. The subjective nature of well-being assessments is another limitation, and future research should explore different dimensions of well-being, such as affective and cognitive aspects, using more comprehensive measures. Additionally, mental health is influenced by various biological, developmental, and environmental factors. Thus, a holistic and systemic approach is essential to achieve meaningful improvements, with MHL enhancement as one component of broader mental health strategies.
This study presents a feasible and replicable framework for integrating MHL programs into undergraduate curricula. Future research should evaluate the program’s applicability to the non-medical student population and assess its long-term efficacy.
Psycheutopia demonstrated the potential of an online educational intervention in increasing mental health literacy and improving the well-being of medical students. The results maintained after four months suggest that the achievements are persistent. The community-based nature of this experience highlights the importance of empowering students to train and support their peers. Key strategies for success included the use of evidence-based content, novel teaching methods, interactive learning, and a focus on making the experience enjoyable and relevant. These elements can be considered when designing future educational interventions for medical students.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were conducted at Iran University of Medical Sciences upon approval of the Bioethics Committee (approval number: IR.IUMS.REC.1402.334). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
ZJ: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. ME: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. AJ: Supervision, Writing – original draft, Writing – review & editing. SG: Supervision, Writing – original draft, Writing – review & editing. MT: Data curation, Writing – original draft, Writing – review & editing. EK: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. SM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
Special thanks to Marzieh Rastkerdar, Mahdi Banijamali, Mohammad Salehi Shadkami, Fatemeh Saberdoust, Sanaz Soleimani, Zahra Najjari, the Abrak group, and everybody who helped in implementing this program.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1538476/full#supplementary-material
MHL, Mental Health Literacy; SWB, Subjective Well-being; MHFA, Mental Health First Aid; MHPK, Mental Health-Promoting Knowledge; MHLS, Mental Health Literacy Scale; WHO-5, World Health Organization (WHO)-5 well-being index (WHO-5); RM-ANOVA, Repeated Measurements Analysis of Variance; SBL, Scenario-Based Learning; SGD, Small Group Discussion; GBL, Game-based Learning; SRL, Self-Reflecting Learning; RP, Role-play.
1. Saracci R. The World Health Organisation needs to reconsider its definition of health. BMJ. (1997) 314:1409. doi: 10.1136/bmj.314.7091.1409
2. Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. (2007) 370:859–77. doi: 10.1016/S0140-6736(07)61238-0
3. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502
4. Prasad J, Abraham V, Minz S, Abraham S, Joseph A, Muliyil J, et al. Rates and factors associated with suicide in Kaniyambadi block, Tamil Nadu, South India, 2000–2002. Int J Soc Psychiatry. (2006) 52:65–71. doi: 10.1177/0020764006061253
5. Soares SJB, Fernandes CFG, Tabalipa R, Kogima F, Jubini MAM, Dias IMV, et al. Common mental disorders among medical students: systematic review and meta-analysis of Brazilian studies. Sao Paulo Med J. (2022) 140:615–22. doi: 10.1590/1516-3180.2021.0851.r1.27012022
6. Zeng W, Chen R, Wang X, Zhang Q, Deng W. Prevalence of mental health problems among medical students in China: A meta-analysis. Medicine. (2019) 98:e15337. doi: 10.1097/MD.0000000000015337
7. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: A meta-analysis. Med education. (2016) 50:456–68. doi: 10.1111/medu.2016.50.issue-4
8. Backović DV, Maksimović M, Davidović D, Ilić-Živojinović J, Stevanović D. Stress and mental health among medical students. Srpski arhiv za celokupno lekarstvo. (2013) 141:780–4. doi: 10.2298/SARH1312780B
9. Mahmoodi SMH, Rasoulian M, Khodadoust E, Jabari Z, Emami S, Ahmadzad-Asl M. The well-being of Iranian adult citizens; is it related to mental health literacy? Front Psychiatry. (2023) 14:1127639. doi: 10.3389/fpsyt.2023.1127639
10. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. (2016) 316:2214–36. doi: 10.1001/jama.2016.17324
11. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Acad Med. (2006) 81:354–73. doi: 10.1097/00001888-200604000-00009
12. El-Gilany A-H, Amro M, Eladawi N, Khalil M. Mental health status of medical students: a single faculty study in Egypt. J Nervous Ment Disease. (2019) 207:348–54. doi: 10.1097/NMD.0000000000000970
13. Jadoon NA, Yaqoob R, Raza A, Shehzad MA, Zeshan SC. Anxiety and depression among medical students: a cross-sectional study. JPMA J Pakistan Med Assoc. (2010) 60:699–702.
14. Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: A cross-sectional study. Med education. (2005) 39:594–604. doi: 10.1111/j.1365-2929.2005.02176.x
15. Nakhostin-Ansari A, Sherafati A, Aghajani F, Khonji MS, Aghajani R, Shahmansouri N. Depression and anxiety among Iranian medical students during COVID-19 pandemic. Iranian J Psychiatry. (2020) 15:228. doi: 10.18502/ijps.v15i3.3815
16. Vasegh S, Mohammadi M-R. Religiosity, anxiety, and depression among a sample of Iranian medical students. Int J Psychiatry Med. (2007) 37:213–27. doi: 10.2190/J3V5-L316-0U13-7000
17. Ashrafi A, Kadhum M, Molodynski A, Bhugra D. Mental health and wellbeing among Iranian medical students: a descriptive study. Int J Soc Psychiatry. (2022) 68:1248–52. doi: 10.1177/00207640211047880
18. Saeed F, Ghalehnovi E, Saeidi M, Ali Beigi N, Vahedi M, Shalbafan M, et al. Factors associated with suicidal ideation among medical residents in Tehran during the COVID-19 pandemic: a multicentric cross-sectional survey. PloS One. (2024) 19:e0300394. doi: 10.1371/journal.pone.0300394
19. Devi S. Iranian medic suicides spark criticism of working conditions. Lancet. (2024) 403:1010. doi: 10.1016/S0140-6736(24)00530-0
20. Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. (2019) 394:240–8. doi: 10.1016/S0140-6736(19)30934-1
21. Tan S, Sherina M, Rampal L, Normala I. Prevalence and predictors of suicidality among medical students in a public university. Med J Malaysia. (2015) 70:1–5.
22. Jorm AF. Mental health literacy: Public knowledge and beliefs about mental disorders. Br J Psychiatry. (2000) 177:396–401. doi: 10.1192/bjp.177.5.396
23. Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. (2012) 67:231. doi: 10.1037/a0025957
24. Organization WH. Comprehensive Mental Health Action Plan 2013-2030 Vol. 2021. . Geneva: World Health Organization (2021).
25. Bennett H, Allitt B, Hanna F. A perspective on mental health literacy and mental health issues among Australian youth: Cultural, social, and environmental evidence! Front Public Health. (2023) 11:1065784. doi: 10.3389/fpubh.2023.1065784
26. Mahmoodi SMH, Ahmadzad-Asl M, Eslami M, Abdi M, Hosseini Kahnamoui Y, Rasoulian M. Mental health literacy and mental health information-seeking behavior in Iranian university students. Front Psychiatry. (2022) 13:893534. doi: 10.3389/fpsyt.2022.893534
27. Nobre J, Oliveira AP, Monteiro F, Sequeira C, Ferré-Grau C. Promotion of mental health literacy in adolescents: a scoping review. Int J Environ Res Public Health. (2021) 18:9500. doi: 10.3390/ijerph18189500
28. Curtin EL, Widnall E, Dodd S, Limmer M, Simmonds R, Russell AE, et al. The Peer Education Project to improve mental health literacy in secondary school students in England: a qualitative realist evaluation. Lancet. (2022) 400:S34. doi: 10.1016/S0140-6736(22)02244-9
29. Sandars J, Patel R, Steele H, McAreavey M. Developmental student support in undergraduate medical education: AMEE Guide No. 92. Med teacher. (2014) 36:1015–26. doi: 10.3109/0142159X.2014.917166
30. Campos L, Dias P, Duarte A, Veiga E, Dias CC, Palha F. Is it possible to “find space for mental health” in young people? Effectiveness of a school-based mental health literacy promotion program. Int J Environ Res Public Health. (2018) 15:1426. doi: 10.3390/ijerph15071426
31. Lanfredi M, Macis A, Ferrari C, Rillosi L, Ughi EC, Fanetti A, et al. Effects of education and social contact on mental health-related stigma among high-school students. Psychiatry Res. (2019) 281:112581. doi: 10.1016/j.psychres.2019.112581
32. Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. PLoS One. (2018) 13:e0197102. doi: 10.1371/journal.pone.0197102
33. Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med education. (2018) 18:1–12. doi: 10.1186/s12909-018-1144-z
34. Hur J-W, Kim B, Park D, Choi S-W. A scenario-based cognitive behavioral therapy mobile app to reduce dysfunctional beliefs in individuals with depression: a randomized controlled trial. Telemedicine e-Health. (2018) 24:710–6. doi: 10.1089/tmj.2017.0214
35. Krishnamurthy K, Selvaraj N, Gupta P, Cyriac B, Dhurairaj P, Abdullah A, et al. Benefits of gamification in medical education. Clin Anatomy. (2022) 35:795–807. doi: 10.1002/ca.23916
36. Jenkins E, Daly Z, McAuliffe C, McGuinness L, Richardson C, Hill TG, et al. Advancing socioecological mental health promotion intervention: A mixed methods exploration of Phase 1 Agenda Gap findings. Front Public Health. (2023) 11:1066440. doi: 10.3389/fpubh.2023.1066440
37. Mohammadi AS, Panahi S, Sayarifard A, Ashouri A. Identifying the prerequisites, facilitators, and barriers in improving adolescents' mental health literacy interventions: A systematic review. J Educ Health promotion. (2020) 9:322. doi: 10.4103/jehp.jehp_623_20
38. Harden RM. Ten questions to ask when planning a course or curriculum. Med education. (1986) 20:356–65. doi: 10.1111/j.1365-2923.1986.tb01379.x
39. Kitchener BA, Jorm A, Kelly DC. Mental health first aid Australia: Mental Health First Aid Australia. (2018). Australia: Mental Health First Aid Australia.
40. Mamakli S, Alimoğlu MK, Daloğlu M. Scenario-based learning: preliminary evaluation of the method in terms of students’ academic achievement, in-class engagement, and learner/teacher satisfaction. Adv Physiol Education. (2023) 47:144–57. doi: 10.1152/advan.00122.2022
41. Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. (2013) 37:158–64. doi: 10.1176/appi.ap.12010003
42. Kushlev K, Heintzelman SJ, Lutes LD, Wirtz D, Oishi S, Diener E. ENHANCE: Design and rationale of a randomized controlled trial for promoting enduring happiness & well-being. Contemp Clin trials. (2017) 52:62–74. doi: 10.1016/j.cct.2016.11.003
43. Heintzelman SJ, Kushlev K, Lutes LD, Wirtz D, Kanippayoor JM, Leitner D, et al. ENHANCE: Evidence for the efficacy of a comprehensive intervention program to promote subjective well-being. J Exp Psychology: Applied. (2020) 26:360. doi: 10.1037/xap0000254
44. Oudbier J, Spaai G, Timmermans K, Boerboom T. Enhancing the effectiveness of flipped classroom in health science education: a state-of-the-art review. BMC Med Education. (2022) 22:34. doi: 10.1186/s12909-021-03052-5
45. Ghaedamini Harouni G, Sajjadi H, Forouzan AS, Ahmadi S, Ghafari M, Vameghi M. Validation of the Persian version of the mental health literacy scale in Iran. Asia-Pacific Psychiatry. (2022) 14:e12447. doi: 10.1111/appy.12447;46
46. Mahmoodi MH, Ahmadzad-Asl M, Rasoulian M. Mental health positive knowledge questionnaire: translation and cultural adaptation and psychometric properties. Soc Welfare Quarterly. (2021) 21:245–73.
47. Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother psychosomatics. (2015) 84:167–76. doi: 10.1159/000376585
48. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
49. Kurki M, Gilbert S, Mishina K, Lempinen L, Luntamo T, Hinkka-Yli-Salomäki S, et al. Digital mental health literacy-program for the first-year medical students’ wellbeing: a one group quasi-experimental study. BMC Med education. (2021) 21:1–11. doi: 10.1186/s12909-021-02976-4
50. Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, et al. Global priorities for addressing the burden of mental, neurological, and substance use disorders. Disease Control Priorities, Third Edition (2016) 4:1-27. doi: 10.1596/978-1-4648-0426-7
51. Patalay P, Annis J, Sharpe H, Newman R, Main D, Ragunathan T, et al. A pre-post evaluation of OpenMinds: A sustainable, peer-led mental health literacy programme in universities and secondary schools. Prev Science. (2017) 18:995–1005. doi: 10.1007/s11121-017-0840-y
52. Davies EB, Beever E, Glazebrook C. A pilot randomised controlled study of the mental health first aid eLearning course with UK medical students. BMC Med education. (2018) 18:1–12. doi: 10.1186/s12909-018-1154-x
53. Freţian AM, Graf P, Kirchhoff S, Glinphratum G, Bollweg TM, Sauzet O, et al. The long-term effectiveness of interventions addressing mental health literacy and stigma of mental illness in children and adolescents: systematic review and meta-analysis. Int J Public Health. (2021) 66:1604072. doi: 10.3389/ijph.2021.1604072
54. AlFaris EA, Naeem N, Irfan F, Qureshi R, van der Vleuten C. Student centered curricular elements are associated with a healthier educational environment and lower depressive symptoms in medical students. BMC Med Education. (2014) 14:192. doi: 10.1186/1472-6920-14-192
55. Purgato M, Uphoff E, Singh R, Pachya AT, Abdulmalik J, van Ginneken N. Promotion, prevention and treatment interventions for mental health in low-and middle-income countries through a task-shifting approach. Epidemiol Psychiatr Sci. (2020) 29:e150. doi: 10.1017/S204579602000061X
56. Huang WD, Loid V, Sung JS. Reflecting on gamified learning in medical education: a systematic literature review grounded in the Structure of Observed Learning Outcomes (SOLO) taxonomy 2012—2022. BMC Med education. (2024) 24:20. doi: 10.1186/s12909-023-04955-1
57. AlFaris EA, Naeem N, Irfan F, Qureshi R, van der Vleuten C. Student centered curricular elements are associated with a healthier educational environment and lower depressive symptoms in medical students. BMC Med education. (2014) 14:1–7. doi: 10.1186/1472-6920-14-192
58. Tuijnman A, Kleinjan M, Olthof M, Hoogendoorn E, Granic I, Engels RC. A game-based school program for mental health literacy and stigma on depression (moving stories): Cluster randomized controlled trial. JMIR Ment Health. (2022) 9:e26615. doi: 10.2196/26615
59. Yusoff MSB, Pa MNM, Rahim AFA. Mental health of medical students before and during medical education: A prospective study. J Taibah Univ Med Sci. (2013) 8:86–92. doi: 10.1016/j.jtumed.2013.03.004
60. Harrer M, Adam SH, Baumeister H, Cuijpers P, Karyotaki E, Auerbach RP, et al. Internet interventions for mental health in university students: A systematic review and meta-analysis. Int J Methods Psychiatr Res. (2019) 28:e1759. doi: 10.1002/mpr.v28.2
61. Harden A, Oakley A, Weston R. A review of the effectiveness and appropriateness of peer-delivered health promotion for young people. Geneva: Institute of Education, University of London. (1999).
62. Kassab SE, Taylor D, Hamdy H. Student engagement in health professions education: AMEE Guide No. 152. Med Teacher. (2023) 45:949–65. doi: 10.1080/0142159X.2022.2137018
63. Moir F, Henning M, Hassed C, Moyes SA, Elley CR. A peer-support and mindfulness program to improve the mental health of medical students. Teach Learn Med. (2016) 28:293–302. doi: 10.1080/10401334.2016.1153475
64. Zheng Y, Wang W, Zhong Y, Wu F, Zhu Z, Tham Y-C, et al. A peer-to-peer live-streaming intervention for children during COVID-19 homeschooling to promote physical activity and reduce anxiety and eye strain: cluster randomized controlled trial. J Med Internet Res. (2021) 23:e24316. doi: 10.2196/24316
65. Murphy R, Clissold E, Keynejad RC. Problem-based, peer-to-peer global mental health e-learning between the UK and Somaliland: a pilot study. BMJ Ment Health. (2017) 20:142–6. doi: 10.1136/eb-2017-102766
66. Mastroleo NR. Brief interventions to reduce college student drinking. In: Brief Interventions for Adolescent Alcohol and Substance Abuse, vol. 405. (2018). New York: Guilford Press.
67. Organization WH. WHO Global Strategy on People-Centred and Integrated Health Services: Interim Report. Geneva: World Health Organization. (2015).
Keywords: mental health literacy, mental health education, mental health intervention, medical students, subjective well-being, stress management, depression, suicide
Citation: Jabari Z, Eslami M, Jalali Nadoushan AH, Goharinezhad S, Tavallaei M, Khodadoust E and Mahmoodi SMH (2025) Psycheutopia: an innovative educational program to enhance mental health literacy among medical students. Front. Psychiatry 16:1538476. doi: 10.3389/fpsyt.2025.1538476
Received: 02 December 2024; Accepted: 03 March 2025;
Published: 27 March 2025.
Edited by:
You You, Peking University, ChinaReviewed by:
Dr. Naseem Akhtar Qureshi, Al-Falah University, IndiaCopyright © 2025 Jabari, Eslami, Jalali Nadoushan, Goharinezhad, Tavallaei, Khodadoust and Mahmoodi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elaheh Khodadoust, RWxhaGVoLmtob2RhZG91c3RAZ21haWwuY29t; Seyed Mohammad Hossein Mahmoodi, TWFobW9vZGkuc21oQGl1bXMuYWMuaXI=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.