- 1School of Clinical Medicine, Hangzhou Normal University, Hangzhou, China
- 2School of Nursing, Hangzhou Normal University, Hangzhou, China
Background: There is abundant evidence that an individual’s personality traits may influence their level of empathy. However, the role of death attitudes in the relationship between personality disorder functioning styles of nurses and their empathy remains to be elucidated.
Methods: Personality disorder functioning styles, death attitudes, and empathy levels were assessed in 614 Chinese trainee nurses using the Parker Personality Measure (PERM), the Death Attitude Scale-Revised (DAP-R), and the Jefferson Scale of Empathy-Health Professionals (JSE-HP).
Results: Among the trainee nurses, DAP-R Fear of Death, Death Avoidance, Escape Acceptance, Approach Acceptance, and Neutral Acceptance(-) partially mediated the negative correlations between all PERM styles except Obsessive-compulsive style and empathy. Furthermore, DAP-R Fear of Death, Escape Acceptance, and Approach Acceptance fully mediated that between Obsessive-compulsive style and empathy. Fear of Death and Death Avoidance attenuated empathy among those with higher Narcissistic and Dependent styles, respectively.
Conclusion: Death attitudes served as a mediator and moderator in the relationships between personality disorder functioning styles and empathy among trainee nurses, suggesting the need for targeted death education among early-career nurses with personality dysfunctions.
1 Introduction
Empathy in clinical practice involves recognizing and experiencing a patient’s emotions (emotional empathy), understanding their thoughts and feelings (cognitive empathy), and effectively communicating this understanding to the patient (behavioral empathy) (1, 2). Whilst empathy (particularly its emotional aspect) is susceptible to innate factors, it can also be developed through intellectual processes such as transpersonal thinking, enabling nurses to understand patients while maintaining objectivity (3–5). Clinical empathy boosts nurse engagement (6), strengthens the nurse-patient relationship (7), and is crucial for holistic care (1). Moreover, it enhances healthcare workers’ personal fulfillment (8) and protects against burnout (9). Empathy tends to be high in early adulthood (10), but gradually declines with age, particularly in emotionally demanding jobs (11). Studies show that nurses worldwide are increasingly experiencing compassion fatigue—characterized by depletion or absence of empathy and is often accompanied by burnout (1, 12, 13), especially in high-stress settings like ICUs (14). Similar trends of decreasing empathy have been observed in nursing students in the US and Italy among those with increased clinical exposure (15, 16), and even among those with limited clinical experience (17). These findings suggest that, in addition to external factors like work environment and workload, intrinsic factors also play a significant role in shaping empathy in early-career nurses.
Literature has showed that an individual’s capacity for empathy is closely linked to their personality profile (18). Using the Big Five personality model, one of the most influential personality theories, studies found that personality traits account for 15.1%-37.5% of the variation in empathy (19, 20). To be more specific, positive associations were found between conscientiousness (19–22), agreeableness (19–21, 23), openness (21, 23), and extraversion (21, 22) and empathy, while a negative association was found between neuroticism and empathy (19, 22) in undergraduates, medical students, and clinical nurses at different career stages. However, less attention has been given to personality disorder functioning styles (disordered personality traits), which deviate from the norm and may evolve into established personality disorders (24). According to the DSM-5, personality disorder functioning styles are classified into three clusters: Cluster A includes eccentric traits such as paranoid, schizoid, and schizotypal personalities; Cluster B is characterized by dramatic, impulsive, and moody traits, seen in borderline, antisocial, narcissistic, or histrionic personalities; and Cluster C involves anxious and fearful traits, represented by avoidant, dependent, or obsessive-compulsive personalities (25, 26). Prior research has indicated that some nursing students and trainees are particularly susceptible to stress and negative emotions, particularly in the context of the COVID-19 pandemic (27, 28), increasing the risk of compassion fatigue (29). Meanwhile, in many cases, high accessibility to stress and negative emotions was associated with personality dysfunctions (25). Therefore it is highly possible that nurses with personality disorder functioning styles have lower levels of empathy than healthy ones. Interestingly, some evidence has suggested conflicting conclusions. For example, narcissistic style, marked by apathy, distrust, and interpersonal dissociation, has been demonstrated to be negatively correlated with empathic concern (30). However, a study in Berlin (31) found that while individuals with narcissistic personality disorder had deficits in emotional empathy, their cognitive empathy remained intact. This suggests that personality disorder functioning styles may not universally reduce empathy, with other cognitive factors possibly mediating this relationship.
An individual’s attitudes toward death are shaped by their comprehensive conceptualization of death, encompassing their own mortality and that of others (32). People with positive attitudes toward death can deal effectively with the negative emotions associated with death, whereas people with negative attitudes often show fear and avoidance of death, or see death as a means of escaping reality (33, 34). Evidence showed that COVID-19 exacerbated fear of death, while those exposed to high levels of epidemic-related media content showed higher levels of empathy or sympathy (34). Death exposure and fear of death were also found positively correlated with attitudes toward the care of the dying among certain percentage of residents (35) and nursing students (36). However, for some healthcare workers and students, such exposure leads to a sharp decline in empathy (35, 37, 38), which might be correlated with their personality dysfunctions to some degree. Additionally, some patients with schizophrenia, who are at higher risk for suicidal behavior, exhibit diminished fear of death and heightened empathy (39). Such findings indicated that individuals with mental illness may experience a unique relationship between death attitudes and empathy compared to those in good health. Additionally, death attitudes differ across personality disorders. For instance, narcissistic personality disorder was found associated with greater fear of death and less suicidal ideation, whereas antisocial and borderline personality disorders were linked to higher rates of suicidal thoughts (40, 41). Therefore, it can be proposed that personality disorder functioning styles may influence empathy in trainee nurses through mediation of their death attitudes.
In addition, death attitudes have the potential to moderate the negative prediction of empathy by personality disorder functioning styles. For example, participation in end-of-life care courses has been shown to increase empathy among undergraduates (42). There is also evidence that individuals with borderline personality disorder, who often struggle with chronic self-harm ideation and high suicide rates (41), typically exhibit low empathy levels (43). While following the psychologically oriented treatment, these patients exhibited a decline in suicidal self-harm ideation (44) and an enhancement in empathy (45).
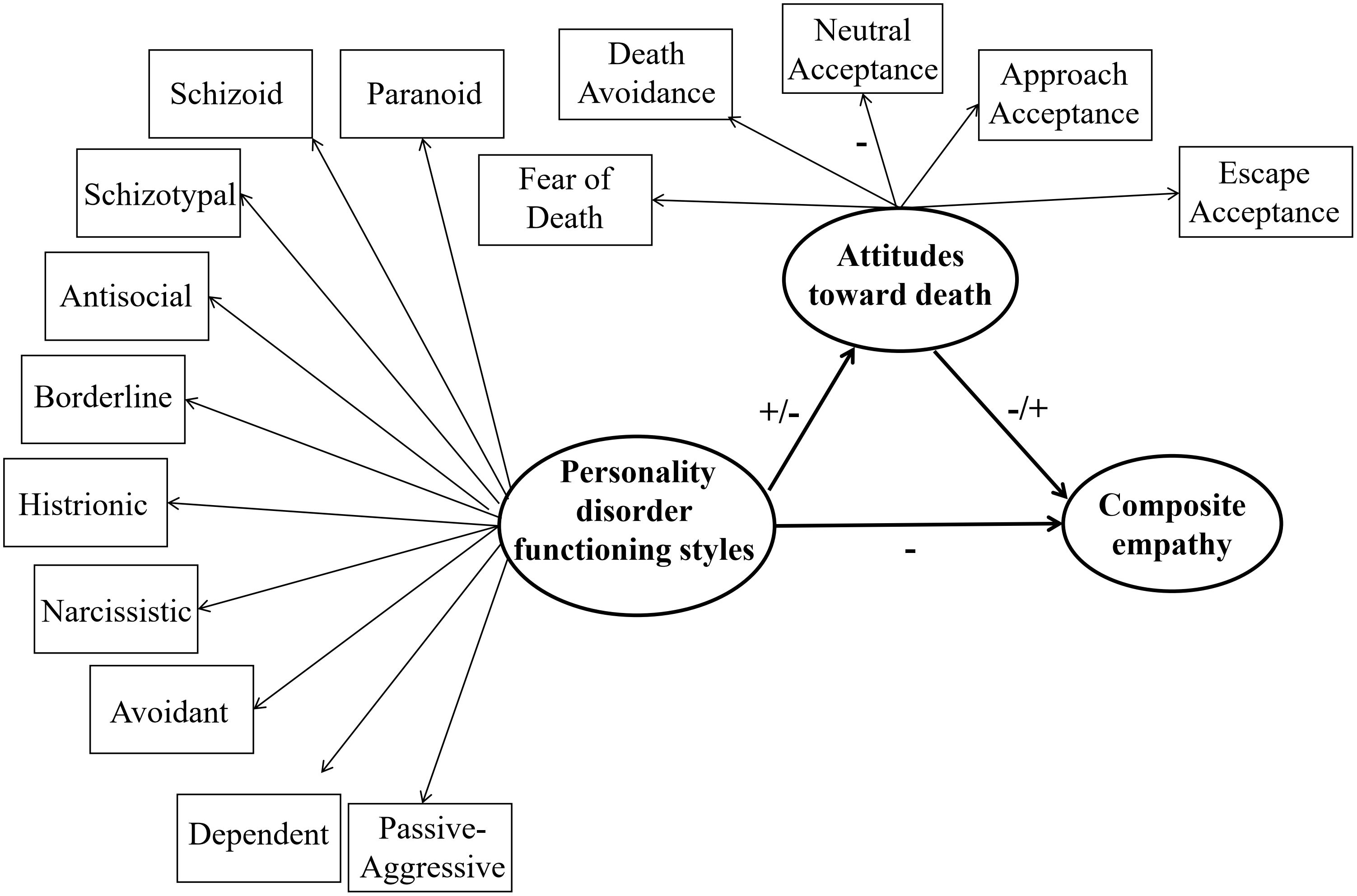
In general, previous studies indicated that empathy was associated with personality traits (18–22, 30, 31) and attitudes toward death (34–38). However, the precise role of death attitudes in the relationship between personality disorder functioning styles and empathy in trainee nurses remains unclear. Clarification of this will enrich theories about the mechanisms of personality influence on empathy, and facilitate the development of a targeted joint empathy and death education training program for early-career nurses in need. We hypothesized that: 1) personality disorder functioning styles are negatively associated with empathy in trainee nurses; 2) these styles reduce empathy through the mediation of negative death attitudes; 3) death attitudes moderate the relationships between personality disorder styles and empathy.
2 Methods
2.1 Participants
A total of 626 trainee nurses from a general hospital in Hangzhou, China, were initially invited to participate in the anonymous online survey. A total of 614 valid responses were ultimately obtained (556 female and 58 male; mean age 21.85 ± 1.12, range 19 ~ 26 years). The remaining 12 responses were excluded on the grounds that they exhibited a standard score in excess of 65 on the Lie factor of the Parker Personality Measure, thereby indicating a low degree of accuracy in self-report. All the nurses were self-reported to have no history of psychiatric or neurological abnormalities, and they were not currently suffering from any acute or chronic illnesses. All participants were of Han Chinese ethnicity, had been engaged in hospital practice for a period of less than six months, and were assigned to rotate between different departments. Table 1 presents their demographic characteristics and corresponding comparisons of empathy levels. The study was approved by a local ethical committee (No. 2024029) and all participants gave their informed consent to participate.
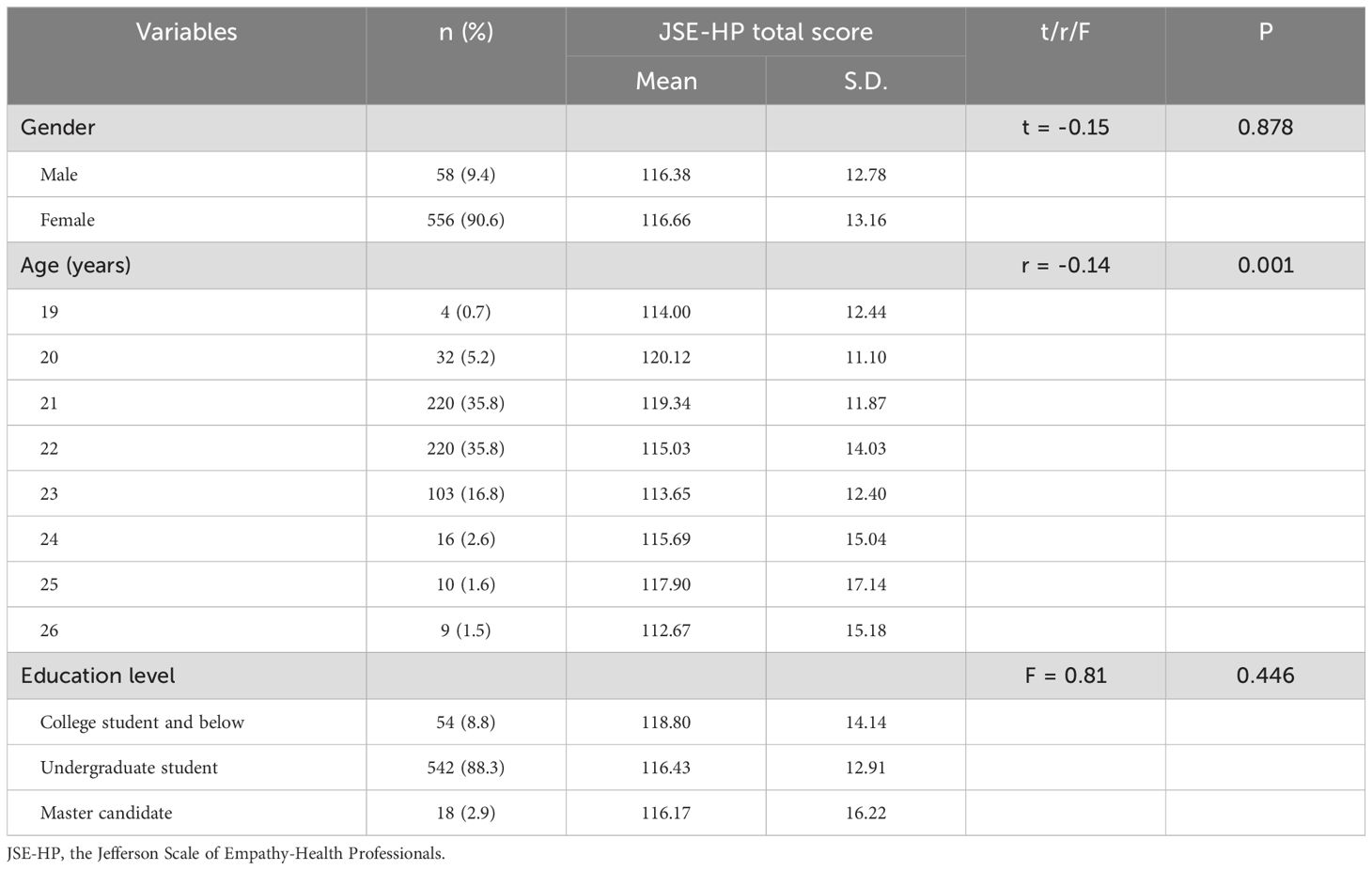
Table 1. Demographic characteristics and their relationships with empathy levels among trainee nurses (N = 614).
2.2 Questionnaires
2.2.1 The Parker Personality Measure (PERM)
The PERM (26) involves efficient and first-level clinical description of personality disorder types Paranoid, Schizoid, Schizotypal, Antisocial, Borderline, Histrionic, Narcissistic, Avoidant, Dependent, Obsessive-compulsive, and Passive-aggressive when the standardized scores for the dimensions are greater than 65. It contains 92 items, each item is scored on a 5-point Likert scale (1 = very unlike me, to 5 = very like me). Studies have shown that the Chinese version of PERM can help measure personality disorder functioning styles in clinical practice with good reliability and criterion validity (46, 47). Its Cronbach’s alpha in this study was 0.82.
2.2.2 The Death Attitude Profile-Revised (DAP-R)
The DAP-R is a questionnaire designed to measure attitudes toward death (32). It consists of 32 items divided into five subscales: Fear of Death, Death Avoidance, Escape Acceptance, Approach Acceptance, and Neutral Acceptance. Each item is scored on a 5-point Likert scale (1 = strongly disagree, to 5 = strongly agree). The Chinese version of the DAP-R has been shown to be reliable and valid (48), and its Cronbach’s alpha in this study was 0.88.
2.2.3 The Jefferson Scale of Empathy-Health Professionals (JSE-HP)
The JSE-HP is a widely used instrument for measuring empathy in the context of health professional education and patient care (49). It has three dimensions, namely Perspective taking (ability to understand the patient’s perspective, reflecting cognitive empathy), Compassionate care (expression of caring, concern, and empathy), and Walking in patient’s shoes (feeling what the patient is feeling, reflecting emotional empathy). Items are scored on a 7-point Likert scale (1 = strongly disagree, to 7 = strongly agree), with half of the items reversely scored. The similarity of the JSE-HP patterns in samples from different countries suggested that the scale was consistently reliable and valid regardless of cultural differences (50), and its Cronbach’s alpha in this study was 0.75. However, we only used its total score for analyses, because from a clinical perspective, improvement in composite empathy was actually more valuable than that in its individual dimensions.
2.3 Data analysis
Statistical analysis was performed using SPSS IBM Statistics v.26.0. Descriptive statistics were used to describe demographic variables such as age, gender, and education level of participants. Comparisons of the composite empathy scores between participants of different gender and education levels were made using Student’s t-test and one-way ANOVA, respectively, and the correlation between empathy and age was tested using Pearson correlation analysis. The significance of the P value was set at < 0.05. Once the influence of demographic variables on total JSE-HP scores was identified, these were used as covariates in further analyses.
For hypothesis 1, Pearson correlation analysis was used to test the relationships between scores on the PERM, DAP-R, and JSE-HP total score in the trainee nurses. For hypotheses 2 & 3, least squares regression (bootstrap method) was used to analyze the mediating and moderating roles of death attitudes in PROCESS plug-in of SPSS 26.0 (51). Breusch-Pagan test was conducted to detect the heteroscedasticity between personality styles, attitudes toward death, and empathy, and VIF and tolerance were calculated for test of linearity. Then each of the 11 personality disorder functioning styles (i.e., Paranoid, Schizoid, Schizotypal, Antisocial, Borderline, Histrionic, Narcissistic, Avoidant, Dependent, Obsessive-compulsive, and Passive-Aggressive) was used as an independent variable, and the composite empathy was used as the dependent variable, as illustrated in Figure 1. To eliminate the multicollinearity effects between the variables, the data were centralized prior to analysis. 95% confidence intervals (CIs) were estimated by the bias-corrected bootstrapping procedure, and the number of iterations was set to 5000. A non-zero 95% CI for the interaction term and indirect effect indicated that specific attitudes toward death had a significant moderating and mediating role in the interaction terms and indirect effects.
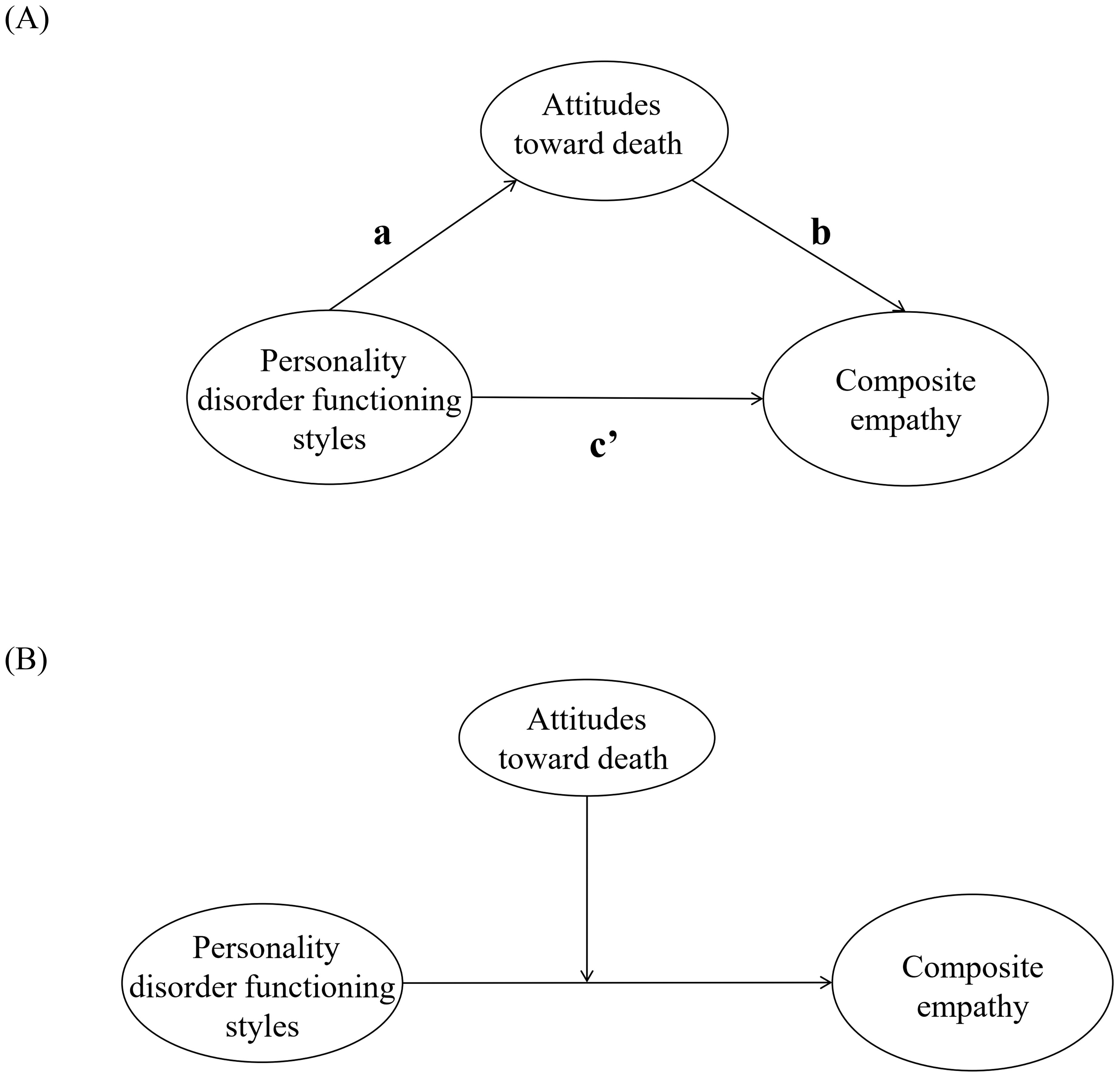
Figure 1. The theoretical (A) mediation and (B) moderation models in this study. Each model consists of 55 sub-models based on the potential mediating and moderating roles of five attitudes toward death between the 11 personality disorder styles and composite empathy in trainee nurses, respectively.
3 Results
As showed in Table 1, 90.6% of the participants were female, 88.4% were between 21 and 23 years old, 88.3% were undergraduate students (followed by undergraduate and masters students). The demographic distribution was basically consistent with previous studies on Chinese trainee nurses (52, 53). In addition, no significant differences were observed in JSE-HP total scores between trainee nurses of different genders (Cohen’s d = 0.02) (also see Supplementary Table 1 and results below) or education levels (η² = 0.003) (Ps > 0.05). However, higher scores were noted in younger nurses (r = -0.14, P = 0.001).
3.1 Test of correlations
Table 2 showed Pearson’s correlations with age as a covariate. All PERM personality disorder functioning styles were negatively correlated with JSE-HP total scores of the trainee nurses (all Ps < 0.001). The study found positive correlations between all personality disorder functioning styles and DAP-R Fear of Death, Death Avoidance, Escape Acceptance, and Approach Acceptance (all Ps < 0.001), and negative correlations between all personality styles except the Obsessive-compulsive and Neutral Acceptance (all Ps < 0.001 except for schizoid personality disorder; P < 0.01 for schizoid personality disorder). Furthermore, Fear of Death, Death Avoidance, Approach Acceptance, and Escape Acceptance exhibited negative correlations, while Neutral Acceptance exhibited a positive correlation with the JSE-HP total scores of the trainee nurses (all Ps < 0.001). See Supplementary Table 2 for more detailed descriptive statistics on scores of PERM, DAP-R, and JSE-HP among the participants. No other significant relationships were found between personality disorder functioning styles, death attitudes, and empathy in the trainee nurses.
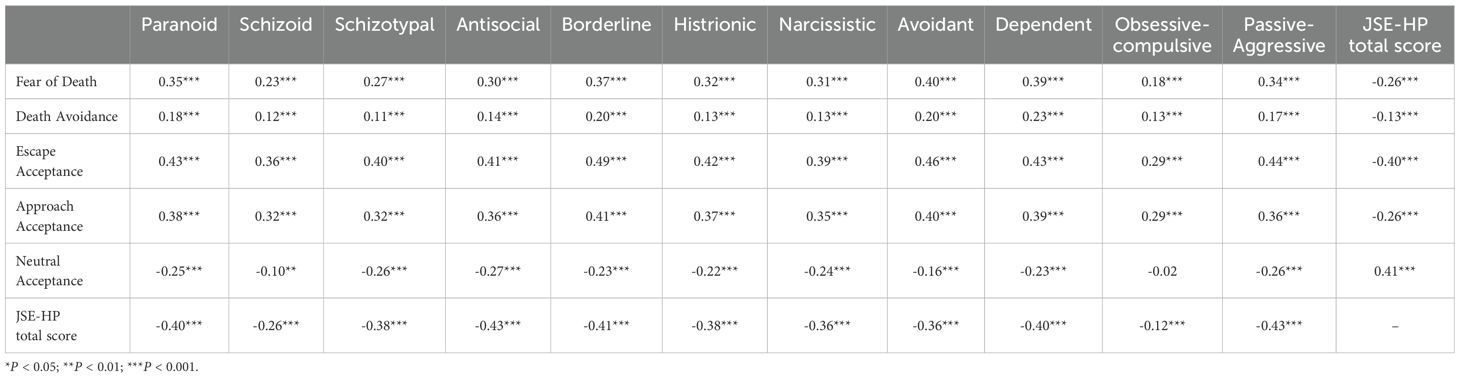
Table 2. Correlations between the scores on the factors of Parker Personality Measure, the dimensions of Death Attitude Profile Revised, and the Jefferson Scale of Empathy-Health Professionals (JSE-HP) in trainee nurses (N = 614).
3.2 Tests of mediating effects
There was no significant heteroscedasticity between personality styles and attitudes toward death or empathy (Ps > 0.05), while that between personality styles and empathy was significant (Ps < 0.01). Meanwhile, there was acceptable linearity between personality styles and attitudes toward death (VIFs = 1.95 ~ 8.92, tolerance = 0.11 ~ 0.51), between attitudes toward death and empathy (VIFs = 1.10 ~ 2.28, tolerance = 0.44 ~ 0.91), and between personality styles and empathy (VIFs = 1.95 ~ 8.92, tolerance = 0.11 ~ 0.51).
Table 3 displayed the results of the mediating effect with age as a covariate. When Fear of Death, Escape Acceptance, or Approach Acceptance was taken as the mediator, direct associations were found between all the personality disorder functioning styles (except for the Obsessive-compulsive) and JSE-HP total scores in trainee nurses (Ps < 0.05). The paths from Schizoid, Schizotypal, Histrionic, and Narcissistic styles to all five DAP-R death attitudes, as well as from these death attitudes to the JSE-HP total score, were included. Additionally, the paths from Paranoid, Antisocial, Borderline, Avoidant, Dependent, and Passive-Aggressive styles to all death attitudes except for Death Avoidance, as well as from these death attitudes to the JSE-HP total score, were also included. Significant associations were found between Obsessive-compulsive style and all death attitudes except for Neutral Acceptance, as well as between these death attitudes and JSE-HP total score (all Ps < 0.05). The bootstrap method revealed that the 95% confidence intervals of indirect effects in all models did not contain zero. This indicated that Fear of Death, Death Avoidance, Escape Acceptance, Approach Acceptance and Neutral Acceptance (–) partially mediated the negative associations of Schizoid, Schizotypal, Histrionic, and Narcissistic styles with empathy levels in the trainee nurses respectively. Fear of Death, Escape Acceptance, Approach Acceptance and Neutral Acceptance (–) partially mediate the negative associations of Paranoid, Antisocial, Borderline, Avoidant, Dependent, and Passive-Aggressive styles with their empathy levels respectively. Death Avoidance (-) partially mediated the negative association of Obsessive-compulsive style with their empathy levels. Moreover, Fear of Death, Escape Acceptance, and Approach Acceptance fully mediated the negative association of Obsessive-compulsive style with their empathy levels respectively (also see Figure 2).
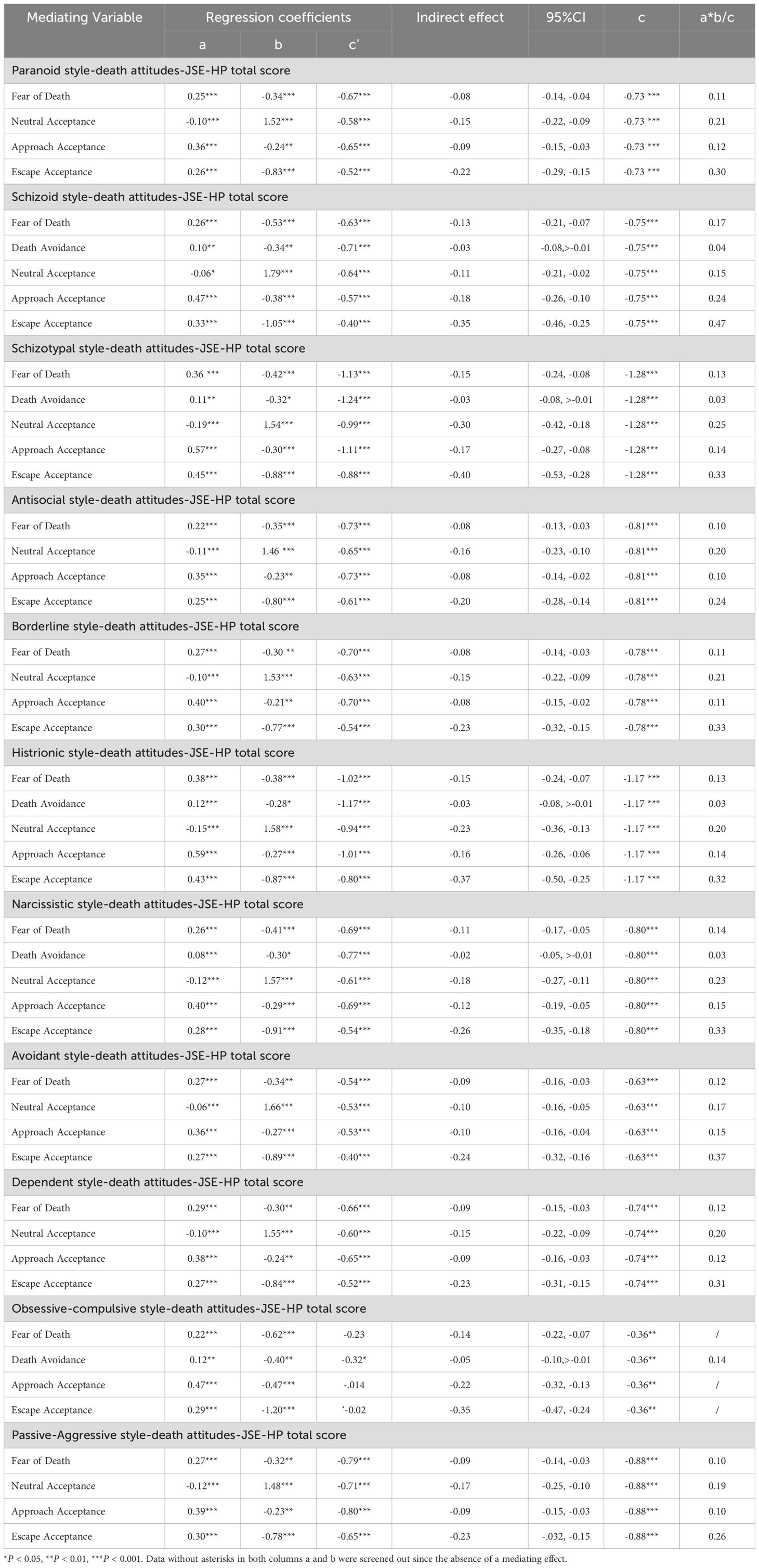
Table 3. Mediating effects of death attitudes on the relationships between personality disorder functioning styles and the JSE-HP total scores in trainee nurses (N = 614).
No other significant mediating effect of death attitude was found on the relationships between personality disorder functioning styles and empathy levels in the trainee nurses.
3.3 Tests of moderating effects
Table 4 displayed the results of the moderating effect with age as a covariate. The JSE-HP total score was negatively predicted by both Narcissistic and Dependent styles (Ps < 0.001). Additionally, the interactions between Narcissistic style and Fear of Death, as well as between Dependent style and Death Avoidance, positively predicted the JSE-HP total score (Ps < 0.05). These results indicated that Fear of Death and Death Avoidance strengthened the negative predictions of Narcissistic and Dependent styles on empathy levels in trainee nurses respectively, as presented in Figure 3. No other significant moderating effect of death attitude was found upon the predictions of personality disorder functioning styles on their empathy levels.
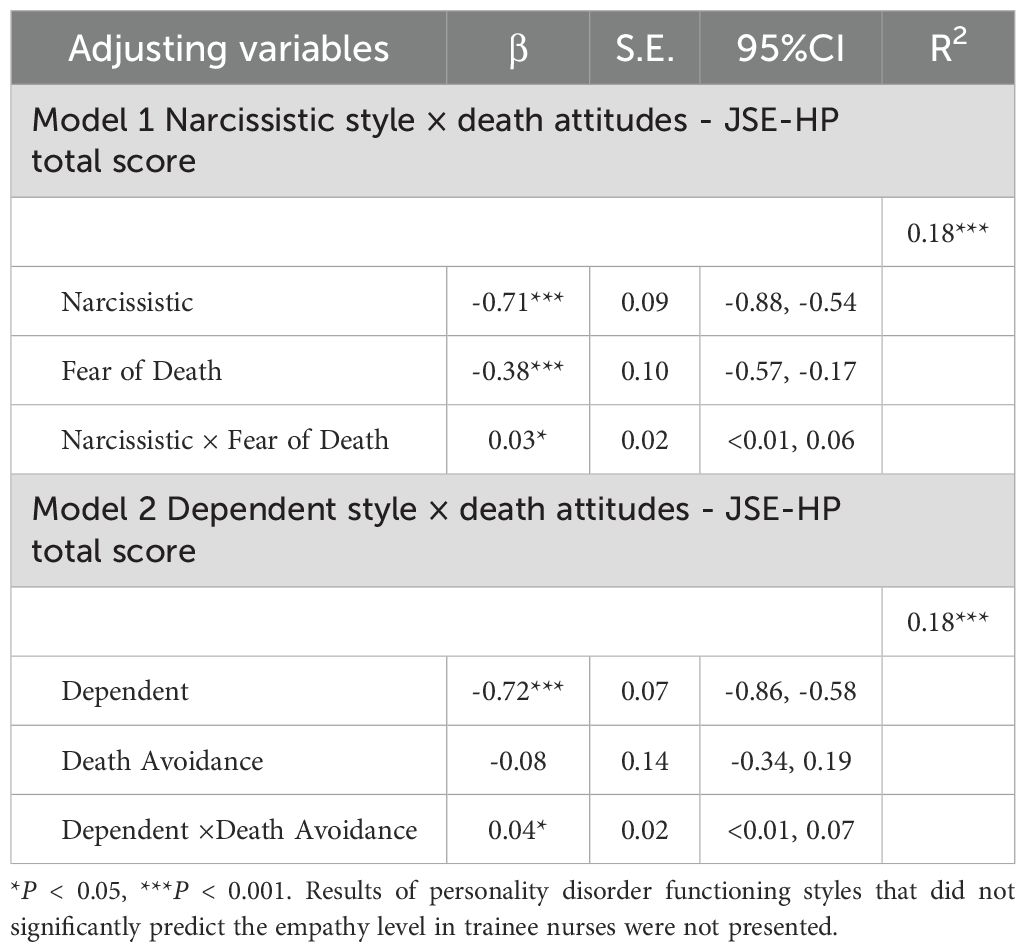
Table 4. Moderating roles of death attitudes in the predictions of personality disorder functioning styles on the JSE-HP total scores in trainee nurses (N = 614).
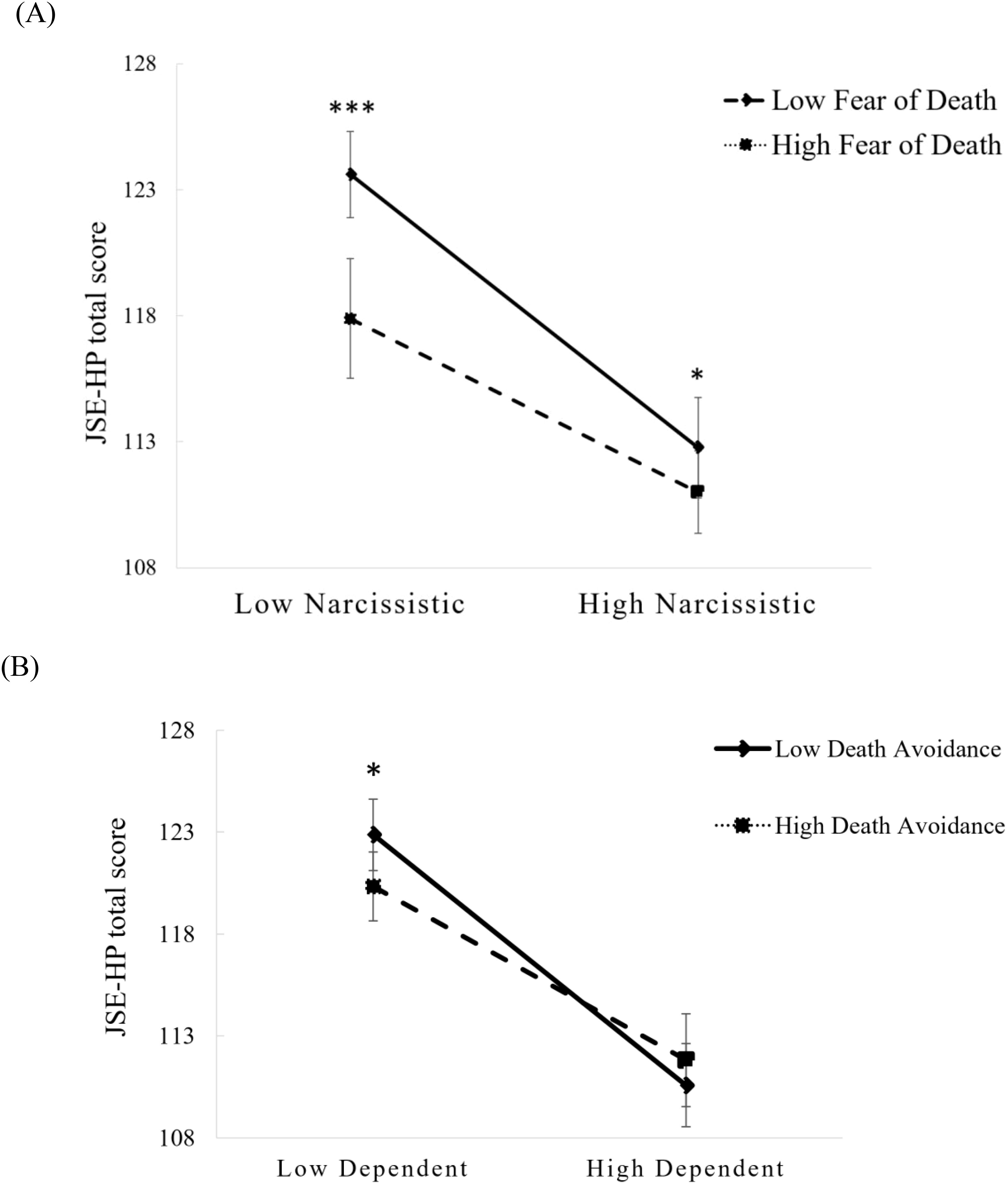
Figure 3. Interaction effects between (A) Fear of Death and Narcissistic style and (B) Death Avoidance and Dependent style on the JSE-HP total score of trainee nurses (N = 614). Error bands represent 95% confidence intervals. *P < 0.05; ***P < 0.001.
4 Discussion
In this study, we explored the relationships between personality disorder functioning styles, death attitudes, and empathy levels among trainee nurses. Regarding the influence of demographic information on composite empathy, we found no significant difference between genders, in contrast to some previous reports of lower levels in males (54, 55). We suggest that this may be due to the fact that the recently completed nursing education (including the nursing psychology curriculum) has improved the empathy of male trainee nurses (4) to a level similar to that of females. In general, we found that various personality disorder functioning styles were negatively associated with their empathy levels. Moreover, death attitudes like Fear of Death, Escape Acceptance, and Approach Acceptance mediated the relationships between all personality styles and their empathy levels; Neutral Acceptance mediated the relationships between all personality styles except Obsessive-compulsive and their empathy levels; besides, Death Avoidance mediated the relationship between some personality styles and their empathy levels. In addition, Fear of Death and Death Avoidance moderated the relationships between specific personality styles and their empathy levels. These results fully supported all of our hypotheses.
4.1 Correlations between the personality disorder functioning styles, death attitudes, and empathy levels in the trainee nurses
The current study revealed a negative association between each personality disorder functioning style and the empathy level of trainee nurses. Previous studies have shown that high level of non-adaptive personality traits, such as neuroticism, can be detrimental to the career development of nurses (56). Additionally, patients with personality disorders, such as schizoid, antisocial, narcissistic, or avoidant types, have been reported to have decreased empathetic concerns (30, 57–59). Such evidence supported our finding above. However, it is important to note that not all individuals with personality disorder lack empathy all the time. According to Ritter et al. (31), patients with narcissistic personality disorder underestimated their cognitive empathy and empathic behaviors on tests of empathic ability due to insufficient motivation, while in fact their cognitive empathy was normal, and it was their emotional empathy that was deficient. In addition, according to a review, patients with borderline personality disorder exhibited enhanced empathy in some social interaction situations, although these findings were contradicted by some other studies (60). Such evidence, on the one hand, conflicted with our results, and on the other hand, was suggesting that there were other factors influencing the relationship between personality disorder functioning styles and empathy, as we discussed below.
We found that attitudes toward death also influenced the empathy levels in trainee nurses. To be more specific, their JSE-HP total scores were negatively correlated with DAP-R Fear of Death, Death Avoidance, Approach Acceptance and Escape Acceptance, while positively correlated with Neutral Acceptance, in line with our previous findings on trainee nurses (61). Among the death attitudes, Fear of Death and Death Avoidance reflect negative thoughts and feelings about death, and a defense mechanism to keep death out of consciousness, respectively. On the contrary, Approach Acceptance and Escape Acceptance reflect a perception of death as a pathway to a blissful afterlife, and an escape from a painful existence, respectively. And unlike the attitudes above, Neutral Acceptance reflects a perception of death as a reality that is neither frightening nor desirable (32). Therefore, such findings implied that rational attitude like Neutral Acceptance of death instead of irrational ones, either fearing or desiring, was favorable for maintaining empathy at the right level. Although evidence showed that patients with schizophrenia with suicidal ideation had higher empathy levels compared to those without (62), indicating a positive correlation between an increase in tendency to death and higher empathy in patients with serious mental illness, other evidence supported the negative association between fear or avoidance of death and empathy in medical staff. For example, a study proved that the motivation of oncology nurses to care for terminally ill patients was negatively associated with death avoidance (63). Furthermore, we findings revealed that unlike empathy, the various personality disorder functioning styles were positively associated with the four irrational attitudes toward death mentioned above while negatively Neutral Acceptance, partly supported by the previous reports of increased fear of death in patients with narcissistic personality disorder, and higher suicidal ideation, which suggested higher desire for death, in patients with histrionic and antisocial personality disorders (40).
4.2 The mediating effect of death attitudes on the relationships between personality disorder functioning styles and empathy levels in the trainee nurses
Our findings that DAP-R Fear of Death, Death Avoidance, Escape Acceptance, Approach Acceptance, and Neutral Acceptance (–) partially mediated the negative associations of Schizoid, Schizotypal, Histrionic, and Narcissistic styles with the empathy levels of trainee nurses; and Fear of Death, Escape Acceptance, Approach Acceptance and Neutral Acceptance (–) partially mediated the negative associations of Paranoid, Antisocial, Borderline, Avoidant, Dependent, and Passive-Aggressive styles with their empathy levels indicated that the decrease in empathy among nurses with specific disordered personality traits could be attributed to their loss of neutrality towards death and the adoption of irrational attitudes towards it. Nurses were indeed a population that needed to be frequently exposed to high life risk and death. For example, studies have reported mortality rates as high as 40% in emergency and ICU units (64, 65). And such frequent exposure has been found to increase compassion fatigue in nurses (66), not to mention susceptible nurses who already have non-adaptive personality traits. Furthermore, classic study has shown that patients with schizophrenia spectrum disorders experienced social and emotional withdrawal when negative symptoms intensified and suicidal ideation emerged (67). It could be plausible that desire for death may reduce empathy in individuals with cluster A personality styles which associated with the schizophrenia continuum. This evidence supported the present findings. The risk of suicide and self-harm was also common in individuals with Cluster B and Cluster C personality disorders (68, 69), which might leave them with no room to empathize with others. For example, in narcissistic patients, when their narcissism was severely threatened, patients would develop increased approach or escape acceptance of death to get rid of shame, which in turn led them to suicidal thoughts and behaviors (70), and they have been reported to lack the capacity for real empathy (71). Similarly, borderline personality disorder with high suicide rates also had difficulty understanding the emotions of others, leading to an inability to meet the needs of others (72). However, a correlation has also been found between their empathic impairment and the severity of mood and psychotic symptoms (73), suggesting the mediation of factors other than attitudes toward death.
Furthermore, Death Avoidance partially mediated the negative association between Obsessive-Compulsive style and empathy, whereas Fear of Death, Approach Acceptance and Escape Acceptance fully mediated the negative association of Obsessive-Compulsive style and empathy, implying that Obsessive-Compulsive style could impair the empathy of trainee nurses partly through psychological defenses against death-related information, or entirely by causing them to be afraid of death, desire death, or use death as an escape from the suffering of reality. Individuals with obsessive-compulsive style often alleviate their internal anxiety by adhering to strict rules and striving for perfection (74), and their attention is narrowed (75). Death, on the other hand, symbolizes ultimate loss of control and uncertainty (76). When they are filled with the fear of death, it is easy for them to neglect the emotional needs of others because of their obsession with maintaining inner order. Conversely, when they can no longer cope with the pressures of reality, they may simply turn to death as the most effective way to solve problems (77), thus eliminating the need to focus on the suffering itself, which can also lead to a drop in empathy for others (78, 79).
4.3 The moderating effect of death attitudes on the relationships between personality disorder functioning styles and empathy levels in the trainee nurses
The findings further revealed that Fear of death and Death Avoidance also negatively moderated the JSE-HP total scores of nurses with Narcissistic or Dependent personality style, which suggested that such death attitudes further weakened the empathic competence of these nurses. Previous researches suggested that individuals diagnosed with narcissistic personality disorder exhibit lower acceptance of death (40) and a deficiency in empathy (80), they may engage in helping behaviors solely for the purpose of gaining attention rather than out of empathy or morality (71). On the other hand, patients with dependent personality disorder had high levels of insecurity and lack of self-confidence. When they perceived a relationship to be in jeopardy, they would resort to suicidal or abusive behavior to gain the attention of others (81). They were therefore prone to a lack of empathy.
4.4 Limitations and future directions
It is important to consider the limitations of the study. Firstly, it was a cross-sectional design, so the relationships between personality disorder functioning styles, attitudes toward death and empathy were inferred and need further validation through longitudinal studies. Secondly, although the sample of trainee nurses was obtained from a large general hospital, subsequent multicenter, cross-cultural validation of the findings is encouraged, particularly in light of recent evidence on the influence of culture on empathy (82–84). Thirdly, as the data were collected from self-report questionnaires, there may be a reporting bias. Fourthly, different aspects of empathy were not modelled separately as the study focused on the impact of different personality disorder styles and attitudes toward death on composite empathy. However, further modelling and validation of emotional, cognitive, and behavioral empathy respectively using other-assessment tools is warranted. Finally, we have primarily examined the impact of different personality disorder styles on empathy in early-career nurses, and further validation is also warranted in more experienced nurses and other healthcare professionals who have greater workloads and potentially greater exposure to death.
5 Conclusions
The study identified personality disorder functioning styles that could reduce empathy levels in trainee nurses by increasing fear and avoidance of or tendency to death, or by decreasing neutrality towards death; and that fear and avoidance of death exacerbated the decline in empathy in trainee nurses with narcissistic and dependent personality styles. Therefore, appropriate and timely education about life and death should be provided to nurses with specific personality dysfunctions to reduce their fear and avoidance of death, thereby increasing their composite empathy and improving the quality of health care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Hangzhou Normal University, School of Nursing. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JP: Writing – original draft, Writing – review & editing. HW: Writing – review & editing, Formal analysis, Visualization. YW: Writing – review & editing, Resources, Validation. BZ: Funding acquisition, Project administration, Writing – original draft, Writing – review & editing, Data curation, Methodology, Visualization, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Ms. Jianing Pan was supported by the Starlight Program of Hangzhou Normal University, and Dr. Bingren Zhang was sponsored by the Teaching Construction and Reform Project of Hangzhou Normal University (No. 8015B30100123).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1532940/full#supplementary-material
Supplementary Table 1 | Demographic characteristics of the male and the two female subsamples.Using a random number table, two subsamples were randomly selected from the female trainee nurses. The student t-test showed that there was no significant difference between the male and the two female subsamples on the JSE-HP total score (using subsample 1: t = -0.25, P = 0.80, Cohen’s d = 0.05; using subsample 2: t = -0.79, P = 0.43, Cohen’s d = 0.14).
Supplementary Table 2 | Descriptive statistics on scores of the Parker Personality Measure, the Death Attitude Profile Revised, and the Jefferson Scale of Empathy-Health Professionals (JSE-HP) among trainee nurses (N = 614).
References
1. Decety J. Empathy in medicine: what it is, and how much we really need it. Am J Med. (2020) 133:561–6. doi: 10.1016/j.amjmed.2019.12.012
2. Harrison K. Compassion fatigue: understanding empathy. Vet Clin North Am Small Anim Pract. (2021) 51:1041–51. doi: 10.1016/j.cvsm.2021.04.020
3. Walker KM, Alligood MR. Empathy from a nursing perspective: Moving beyond borrowed theory. Arch Psychiatr Nurs. (2001) 15:140–7. doi: 10.1053/apnu.2001.23754
4. Fernandez AV, Zahavi D. Basic empathy: Developing the concept of empathy from the ground up. .Int J Nurs Stud. (2020) 110:103695. doi: 10.1016/j.ijnurstu.2020.103695
5. Abramson L, Uzefovsky F, Toccaceli V, Knafo-Noam A. The genetic and environmental origins of emotional and cognitive empathy: Review and meta-analyses of twin studies. Neurosci Biobehav Rev. (2020) 114:113–33. doi: 10.1016/j.neubiorev.2020.03.023
6. Martos Martínez Á, Pérez-Fuentes MDC, Molero Jurado MDM, Simón Márquez MDM, Barragán Martín AB, Gázquez Linares JJ. Empathy, affect and personality as predictors of engagement in nursing professionals. Int J Environ Res Public Health. (2021) 18:4110. doi: 10.3390/ijerph18084110
7. Barker ME, Crowfoot G, King J. Empathy development and volunteering for undergraduate healthcare students: A scoping review. Nurse Educ Today. (2022) 116:105441. doi: 10.1016/j.nedt.2022.105441
8. Delgado N, Delgado J, Betancort M, Bonache H, Harris LT. What is the link between different components of empathy and burnout in healthcare professionals? A Systematic Rev Meta-Analysis Psychol Res Behav Manag. (2023) 16:447–63. doi: 10.2147/PRBM.S384247
9. Cairns P, Isham AE, Zachariae R. The association between empathy and burnout in medical students: a systematic review and meta-analysis. BMC Med Educ. (2024) 24:640. doi: 10.1186/s12909-024-05625-6
10. Eisenberg N, Eggum ND. Empathy-related and prosocial responding: Conceptions and correlates during development. In: Sullivan BA, Snyder M, Sullivan JL, editors. Cooperation: The political psychology of effective human interaction. Hoboken, New Jersey: Blackwell Publishing (2008). p. 53–74.
11. Wieck C, Kunzmann U, Scheibe S. Empathy at work: The role of age and emotional job demands. Psychol Aging. (2021) 36:36–48. doi: 10.1037/pag0000469
12. Graves J, Joyce C, Hegazi I. From empathy to compassion fatigue: A narrative review of implications in healthcare. In: Empathy: advanced research and applications. London, United Kingdom: IntechOpen (2023). p. 1–28. doi: 10.5772/intechopen.107399
13. Marshman C, Hansen A, Munro I. Compassion fatigue in mental health nurses: A systematic review. J Psychiatr Ment Health Nurs. (2022) 29:529–43. doi: 10.1111/jpm.12812
14. Ramírez-Elvira S, Romero-Béjar JL, Suleiman-Martos N, Gómez-Urquiza JL, Monsalve-Reyes C, Cañadas-De-la-Fuente GA, et al. Prevalence, risk factors and burnout levels in intensive care unit nurses: A systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18:11432. doi: 10.3390/ijerph182111432
15. Ward J, Cody J, Schaal M, Hojat M. The empathy enigma: an empirical study of decline in empathy among undergraduate nursing students. J Prof Nurs. (2012) 28:34–40. doi: 10.1016/j.profnurs.2011.10.007
16. Ferri P, Rovesti S, Panzera N, Marcheselli L, Bari A, Di Lorenzo R. Empathic attitudes among nursing students: a preliminary study. Acta BioMed. (2017) 88:22–30. doi: 10.23750/abm.v88i3-S.6610
17. Konrath SH, O’Brien EH, Hsing C. Changes in dispositional empathy in American college students over time: a meta-analysis. Pers Soc Psychol Rev. (2011) 15:180–98. doi: 10.1177/1088868310377395
18. Sharp C. Adolescent personality pathology and the alternative model for personality disorders: self development as nexus. Psychopathology. (2020) 53:198–204. doi: 10.1159/000507588
19. Wan Q, Jiang L, Zeng Y, Wu X. A big-five personality model-based study of empathy behaviors in clinical nurses. Nurse Educ Pract. (2019) 38:66–71. doi: 10.1016/j.nepr.2019.06.00560
20. Wang C, Wu Q, Feng M, Wan Q, Wu X. International nursing: research on the correlation between empathy and China’s big five personality theory: implications for nursing leaders. Nurs Adm Q. (2017) 41:E1–E10. doi: 10.1097/NAQ.0000000000000219
21. Melchers MC, Li M, Haas BW, Reuter M, Bischoff L, Montag C. Similar personality patterns are associated with empathy in four different countries. Front Psychol. (2016) 7:290. doi: 10.3389/fpsyg.2016.00290
22. Airagnes G, du Vaure CB, Galam E, Bunge L, Hoertel N, Limosin F, et al. Personality traits are associated with cognitive empathy in medical students but not with its evolution and interventions to improve it. J Psychosom Res. (2021) 144:110410. doi: 10.1016/j.jpsychores.2021.110410
23. Magalhães E, Costa P, Costa MJ. Empathy of medical students and personality: Evidence from the Five-Factor Model. Med Teach.(2012) 34:807–12. doi: 10.3109/0142159X.2012.702248
24. Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. (2015) 385:717–26. doi: 10.1016/S0140-6736(14)61995-4
25. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. In: DSM-5, 5th edition. American Psychiatric Association, Arlington, VA (2013).
26. Parker G, Hadzi-Pavlovic D. A question of style: refining the dimensions of personality disorder style. J Pers Disord. (2001) 15:300–18. doi: 10.1521/pedi.15.4.300.19186
27. Eweida RS, Rashwan ZI, Desoky GM, Khonji LM. Mental strain and changes in psychological health hub among intern-nursing students at pediatric and medical-surgical units amid ambience of COVID-19 pandemic: A comprehensive survey. Nurse Educ Pract. (2020) 49:102915. doi: 10.1016/j.nepr.2020.102915
28. Riedel B, Horen SR, Reynolds A, Hamidian Jahromi A. Mental health disorders in nurses during the COVID-19 pandemic: implications and coping strategies. Front Public Health. (2021) 9:707358. doi: 10.3389/fpubh.2021.707358
29. Yi LJ, Cai J, Ma L, Lin H, Yang J, Tian X, et al. Prevalence of compassion fatigue and its association with professional identity in junior college nursing interns: A cross-sectional study. Int J Environ Res Public Health. (2022) 19:15206. doi: 10.3390/ijerph192215206
30. Baskin-Sommers A, Krusemark E, Ronningstam E. Empathy in narcissistic personality disorder: from clinical and empirical perspectives. Pers Disord. (2014) 5:323–33. doi: 10.1037/per0000061
31. Ritter K, Dziobek I, Preissler S, Rüter A, Vater A, Fydrich T, et al. Lack of empathy in patients with narcissistic personality disorder. Psychiatry Res. (2011) 187:241–7. doi: 10.1016/j.psychres.2010.09.013
32. Wong PTP, Reker GT, Gesser G. Death Attitude Profile—Revised: A multidimensional measure of attitudes toward death. In: Death anxiety handbook: Research, instrumentation, and application. Abingdon, Oxfordshire, UK: Taylor & Francis (1994). p. 121–48.
33. Faronbi JO, Akinyoola O, Faronbi GO, Bello CB, Kuteyi F, Olabisi IO. Nurses’ Attitude toward caring for dying patients in a Nigerian teaching hospital. SAGE Open Nurs. (2021) 7:23779608211005213. doi: 10.1177/23779608211005213
34. Chen X, Liu T, Li P, Wei W, Chao M. The relationship between media involvement and fear of death of self-quarantined people in the COVID-19 outbreak in China: the mediating roles of empathy and sympathy. Omega (Westport). (2022) 85:974–89. doi: 10.1177/0030222820960283
35. McFarland DC, Malone AK, Roth A. Acute empathy decline among resident physician trainees on a hematology-oncology ward: an exploratory analysis of house staff empathy, distress, and patient death exposure. Psychooncology. (2017) 26:698–703. doi: 10.1002/pon.4069
36. Yu H, Sun CY, Xie LF, Wang L, Song JY, Zhu Y, et al. Using a mediating model of death attitude and meaning in life to understand nursing students attitude about hospice care. Nurse Educ Today. (2022) 116:105448. doi: 10.1016/j.nedt.2022.105448
37. Medina-Fernández J, Torres-Soto NY, Casco-Gallardo K, Ruiz-Lara A, Martínez-Ramírez B, Fuentes-Fernández E. Fear and coping with death in intensive care nurses: a structural model predictor of compassion fatigue. Invest Educ Enferm. (2023) 41:e12. doi: 10.17533/udea.iee.v41n1e12
38. Ünlü G, Uludağ A. The relationship between cognitively-based clinical empathy and attitudes toward death and dying in medical students. Teach Learn Med. (2021) 33:49–57. doi: 10.1080/10401334.2020.1794881
39. Wang W, Zhou Y, Wang J, Xu H, Wei S, Wang D, et al. Prevalence, clinical correlates of suicide attempt and its relationship with empathy in patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. (2020) 99:109863. doi: 10.1016/j.pnpbp.2020.109863
40. Yaqoob N, Ahsan S. Impact of mood disorders and personality disorders on suicide intent among self-harm patients. Pak J Med Sci. (2023) 39:491–6. doi: 10.12669/pjms.39.2.6140
41. Oumaya M, Friedman S, Pham A, Abou Abdallah T, Guelfi JD, Rouillon F. Personnalité borderline, automutilations et suicide: revue de la littérature [Borderline personality disorder, self-mutilation and suicide: literature review. Encephale. (2008) 34:452–8. doi: 10.1016/j.encep.2007.10.007
42. Petersen CL, Schiltz S. Care of the spirit: effects of an interdisciplinary undergraduate end-of-life course on knowledge, competence, and response empathy. J Hosp Palliat Nurs. (2020) 22:298–304. doi: 10.1097/NJH.0000000000000660
43. Jeung H, Herpertz SC. Impairments of interpersonal functioning: empathy and intimacy in borderline personality disorder. Psychopathology. (2014) 47:220–34. doi: 10.1159/000357191
44. Löf J, Clinton D, Kaldo V, Rydén G. Symptom, alexithymia and self-image outcomes of Mentalisation-based treatment for borderline personality disorder: a naturalistic study. BMC Psychiatry. (2018) 18:185. doi: 10.1186/s12888-018-1699-6
45. Prada P, Badoud D, Nicastro R, Dieben K, Rüfenacht E, Dayer A, et al. Implémentation francophone de la thérapie basée sur la mentalisation (TBM) pour le trouble de personnalité limite [Mentalization based treatment (MBT) for borderline personality disorder among a population of French-speaking patients. Encephale. (2019) 45:133–8. doi: 10.1016/j.encep.2018.04.003
46. Wang W, Hu L, Mu L, Chen DH, Song Q, Zhou MP, et al. Functioning styles of personality disorders and five-factor normal personality traits: a correlation study in Chinese students. BMC Psychiatry. (2003) 3:11. doi: 10.1186/1471-244X-3-11
47. Fan H, Zhu Q, Ma G, Shen C, Zhang B, Wang W. Predicting personality disorder functioning styles by the Chinese Adjective Descriptors of Personality: a preliminary trial in healthy people and personality disorder patients. BMC Psychiatry. (2016) 16:302. doi: 10.1186/s12888-016-1017-0
48. Tang L, Zhang L, Li YX, Zhou LJ, Cui J, Meng XL, et al. Validation and reliability of a Chinese version Death Attitude Profile-Revised (DAP-R) for nurses. J Nurs Sci. (2014) 29:64–6. doi: 10.3870/hlxzz.2014.14.064
49. Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, measurement and relationship to gender and specialty. Am J Psychiatry. (2002) 159:1563–9. doi: 10.1176/appi.ajp.159.9.1563
50. Hojat M, DeSantis J, Shannon SC, Mortensen LH, Speicher MR, Bragan L, et al. The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. (2018) 23:899–920. doi: 10.1007/s10459-018-9839-9
51. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press (2017) p. 335–7.
52. Wang R, Ye H, Liu Q, Dai W. Analysis on the status and influencing factors of stress among nursing students in late-stage of clinical practice. J Bengbu Med Coll. (2023) 48:1436–40. doi: 10.13898/j.cnki.issn.1000-2200.2023.10.024
53. Jiang C, Jiang Y, Zhou X, Zeng Y, Xu D, Li Y, et al. The current situation and influencing factors of internship nursing students’ career exploration behavior. Int J Nurs Stud. (2019) 38:5. doi: 10.3760/cma.j.issn.1673-4351.2019.09.007
54. Christov-Moore L, Simpson EA, Coudé G, Grigaityte K, Iacoboni M, Ferrari PF. Empathy: gender effects in brain and behavior. Neurosci Biobehav Rev. (2014) 46 Pt 4:604–27. doi: 10.1016/j.neubiorev.2014.09.001
55. Rochat MJ. Sex and gender differences in the development of empathy. J Neurosci Res. (2023) 101:718–29. doi: 10.1002/jnr.25009
56. Mason R, Roodenburg J, Williams B. What personality types dominate among nurses and paramedics: A scoping review? Australas Emerg Care. (2020) 23:281–90. doi: 10.1016/j.auec.2020.06.001
57. Johansen MS, Normann-Eide E, Normann-Eide T, Wilberg T. Emotional dysfunction in avoidant compared to borderline personality disorder: a study of affect consciousness. Scand J Psychol. (2013) 54:515–21. doi: 10.1111/sjop.12076
58. Attademo L, Bernardini F, Spatuzzi R. Suicidality in individuals with schizoid personality disorder or traits: A clinical mini-review of a probably underestimated issue. Psychiatr Danub. (2021) 33:261–5. doi: 10.24869/psyd.2021.261
59. Tasios K, Douzenis A, Gournellis R, Michopoulos I. Empathy and violence in schizophrenia and antisocial personality disorder. Healthcare (Basel). (2023) 12:89. doi: 10.3390/healthcare12010089
60. Dinsdale N, Crespi BJ. The borderline empathy paradox: evidence and conceptual models for empathic enhancements in borderline personality disorder. J Pers Disord. (2013) 27:172–95. doi: 10.1521/pedi.2013.27.2.172
61. Wei T, Guo M, Jin H, Zhang B. Attachment styles and empathy in trainee nurses: the mediating and moderating roles of attitudes toward death. Front Psychol. (2024) 15:1445587. doi: 10.3389/fpsyg.2024.1445587
62. Liu J, Zhao K, Zhou S, Hong L, Xu Y, Sun S, et al. Suicidal ideation in Chinese adults with schizophrenia: associations with neurocognitive function and empathy. BMC Psychiatry. (2023) 23:311. doi: 10.1186/s12888-023-04739-3
63. Braun M, Gordon D, Uziely B. Associations between oncology nurses’ attitudes toward death and caring for dying patients. Oncol Nurs Forum. (2010) 37:E43–9. doi: 10.1188/10.ONF.E43-E49
64. Brinkman S, Bakhshi-Raiez F, Abu-Hanna A, de Jonge E, de Keizer NF. Determinants of mortality after hospital discharge in ICU patients: literature review and Dutch cohort study. Crit Care Med. (2013) 41:1237–51. doi: 10.1097/CCM.0b013e31827ca4f9
65. West E, Barron DN, Harrison D, Rafferty AM, Rowan K, Sanderson C. Nurse staffing, medical staffing and mortality in Intensive Care: An observational study. Int J Nurs Stud. (2014) 51:781–94. doi: 10.1016/j.ijnurstu.2014.02.007
66. Papazian L, Hraiech S, Loundou A, Herridge MS, Boyer L. High-level burnout in physicians and nurses working in adult ICUs: a systematic review and meta-analysis. Intensive Care Med. (2023) 49:387–400. doi: 10.1007/s00134-023-07025-8
67. Fenton WS, McGlashan TH, Victor BJ, Blyler CR. Symptoms, subtype, and suicidality in patients with schizophrenia spectrum disorders. Am J Psychiatry. (1997) 154:199–204. doi: 10.1176/ajp.154.2.199
68. Casillas A, Clark LA. Dependency, impulsivity, and self-harm: traits hypothesized to underlie the association between cluster B personality and substance use disorders. J Pers Disord. (2002) 16:424–36. doi: 10.1521/pedi.16.5.424.22124
69. Massaal-van-der-Ree LY, Eikelenboom M, Hoogendoorn AW, Thomaes K, van Marle HJF. Cluster B versus cluster C personality disorders: A comparison of comorbidity, suicidality, traumatization and global functioning. Behav Sci (Basel). (2022) 12:105. doi: 10.3390/bs12040105
70. Gabbard GO. Narcissism and suicide risk. Ann Gen Psychiatry. (2022) 21:3. doi: 10.1186/s12991-022-00380-8
71. Di Giacomo E, Andreini E, Lorusso O, Clerici M. The dark side of empathy in narcissistic personality disorder. Front Psychiatry. (2023) 14:1074558. doi: 10.3389/fpsyt.2023.1074558
72. Grzegorzewski P, Kulesza M, Pluta A, Iqbal Z, Kucharska K. Assessing self-reported empathy and altruism in patients suffering from enduring borderline personality disorder. Psychiatry Res. (2019) 273:798–807. doi: 10.1016/j.psychres.2018.12.109
73. Harari H, Shamay-Tsoory SG, Ravid M, Levkovitz Y. Double dissociation between cognitive and affective empathy in borderline personality disorder. Psychiatry Res. (2010) 175:277–9. doi: 10.1016/j.psychres.2009.03.002
74. Pinto A, Teller J, Wheaton MG. Obsessive-compulsive personality disorder: A review of symptomatology, impact on functioning, and treatment. Focus (Am Psychiatr Publ). (2022) 20:389–96. doi: 10.1176/appi.focus.20220058
75. Pinto A, Je S, al G, Eu W, Simpson HB. Capacity to delay reward differentiates obsessive-compulsive disorder and obsessive-compulsive personality disorder. Biol Psychiatry. (2014) 75:653–9. doi: 10.1016/j.biopsych.2013.09.007
76. Talati Z. Death as the ultimate loss of control: comparing the effects of mortality salience and loss of control through an examination of moderators and outcomes. Perth, WA: The University of Western Australia (2013).
77. Angelakis I, Gooding P, Tarrier N, Panagioti M. Suicidality in obsessive compulsive disorder (OCD): a systematic review and meta-analysis. Clin Psychol Rev. (2015) 39:1–15. doi: 10.1016/j.cpr.2015.03.002
78. Wang CXY, Pavlova A, At F, Consedine NS. Beyond empathy decline: Do the barriers to compassion change across medical training? Adv Health Sci Educ Theory Pract. (2022) 27:521–36. doi: 10.1007/s10459-022-10100-2
79. Bora E. Social cognition and empathy in adults with obsessive compulsive disorder: A meta-analysis. Psychiatry Res. (2022) 316:114752. doi: 10.1016/j.psychres.2022.114752
80. Mitra P, Torrico TJ, Fluyau D. Narcissistic personality disorder. In: StatPearls. StatPearls, Treasure Island (FL (2024).
81. Bornstein RF. Illuminating a neglected clinical issue: societal costs of interpersonal dependency and dependent personality disorder. J Clin Psychol. (2012) 68:766–81. doi: 10.1002/jclp.21870
82. Eichbaum Q, Barbeau-Meunier CA, White M, Ravi R, Grant E, Riess H, et al. Empathy across cultures - one size does not fit all: from the ego-logical to the eco-logical of relational empathy. Adv Health Sci Educ Theory Pract. (2023) 28:643–57. doi: 10.1007/s10459-022-10158-y
83. Chopik WJ, O’Brien E, Konrath SH. Differences in empathic concern and perspective taking across 63 countries. J Cross-Cult. Psychol. (2016) 48:23–38. doi: 10.1177/002202211667
Keywords: personality disorder functioning style, death attitude, empathy, mediating effect, moderating effect, trainee nurse
Citation: Pan J, Wu H, Wang Y and Zhang B (2025) Personality disorder functioning styles and empathy in trainee nurses: the mediating and moderating roles of death attitudes. Front. Psychiatry 16:1532940. doi: 10.3389/fpsyt.2025.1532940
Received: 22 November 2024; Accepted: 07 March 2025;
Published: 27 March 2025.
Edited by:
Qing Zhao, Chinese Academy of Sciences (CAS), ChinaReviewed by:
Roxane J. Itier, University of Waterloo, CanadaSeth Winward, Faculty of Arts, University of Waterloo in collaboration with reviewer RJI
Jing Shao, Zhejiang University, China
Evelyn Acoba, Central Luzon State University, Philippines
Copyright © 2025 Pan, Wu, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bingren Zhang, YmluZ3JlbnpAaHpudS5lZHUuY24=
 Jianing Pan2
Jianing Pan2 Bingren Zhang
Bingren Zhang