- 1Division of Academic Affairs, Huizhou Health Sciences Polytechnic, Huizhou, China
- 2College of Nursing, Huizhou Health Sciences Polytechnic, Huizhou, China
- 3Institute Office, Huizhou Medicine Institute, Huizhou, China
- 4Department of Propaganda and Education, Health Bureau of Huizhou City, Huizhou, China
- 5Department of Health, Huizhou First Maternal and Child Health Care Hospital, Huizhou, China
- 6Institute Office, Huizhou No. 2 Hospital, Huizhou, China
Objective: This study aimed to assess the depression, anxiety, sleep disorders, and post-traumatic stress disorder (PTSD) among healthcare workers (HCWs) in Huizhou in the post-pandemic period.
Methods: A retrospective multicentric cross-sectional study was conducted from April 25 to May 25, 2023, involving 4,618 HCWs from 46 hospitals in Guangdong Province, China. Psychological well-being was measured using the PHQ-9, GAD-7, Insomnia Severity Index (ISI), and PTSD scales. Chi-square test and multivariable logistic regression were used to identify factors associated with depression, anxiety, insomnia and PTSD.
Results: The rates of anxiety, depression, insomnia, and PTSD were 45.0%, 59.4%, 40.5%, and 10.5%, respectively. HCWs who did not experience negative events were more likely to show anxiety (OR=2.082, 95%CI:1.734-2.499), depression (OR=2.013, 95%CI:1.647-2.460) and insomnia (OR=2.013, 95%CI:1.683-2.409).
Conclusion: There was a high prevalence of anxiety, depression, insomnia, and PTSD in the HCWs after the COVID-19 pandemic.
1 Introduction
The COVID-19 outbreak has led to severe physical and mental health issues, with psychological effects often being longer-lasting than physical injuries (1). It places a significant mental burden on frontline healthcare workers (HCWs), leading to depression, anxiety, burnout, and post-traumatic stress disorder (PTSD) among them (2). Indeed, HCWs face serious psychological burdens as their work environment and mental health is complicated and worsened when facing COVID-19 (3). Additionally, systematic reviews and meta-analyses report high rates of anxiety, depression, PTSD, and sleep disorders among HCWs (4, 5).
In December 2022, China faced a nationwide outbreak of Omicron, with increased pressure on HCWs due to policy changes and a rise in infections. HCWs faced high infection rates, relentless workloads, and traumatic conditions, all of which severely impacted their health. As immunity from COVID-19 vaccination and infection wanes over time, infections in China began to rise again in May 2023, fueled by new variants. This surge has placed additional strain on HCWs, exacerbating their workload and psychological stress. However, timely assessments and mental health interventions for frontline HCWs are relatively scarce (6, 7).
Many studies have investigated the mental health and well-being of HCWs in the COVID-19 pandemic (8, 9), however, our understanding of psychological effects in HCWs during the post-COVID-19 pandemic period is still limited due to rarity of studies. The impact of COVID-19 on HCWs varied worldwide due to different political, cultural, environmental, and geographical factors, as well as varying national responses. For instance, over 53% of HCWs in Zimbabwe experienced moderate to severe psychological distress (10), while approximately 40% of frontline nurses in Nigeria suffered from both anxiety and depression in the post-COVID-19 period (11). To our best knowledge, there is a lack of studies exploring anxiety, depression, insomnia, and PTSD among HCWs in Mainland China in the post-COVID-19 period. Therefore, this study was designed to investigate the incidence and risk factors of anxiety, depression, insomnia and PTSD among HCWs during the post-COVID-19 period in Huizhou, China.
2 Materials and methods
2.1 Participants
This retrospective multicentric cross-sectional study was performed from 25 April 2023 to 25 June 2023 with a random sampling approach in 37 hospitals and health centers community organizations located in 3 districts in Huizhou city, Guangdong Province, China. This survey was conducted during the rising phase of a nationwide COVID-19 outbreak. The respondents completed the electronic questionnaire during the breaks which also reduced unnecessary contact.
The inclusion criteria for participants were as follows: (a) employed HCWs at the hospital, including doctors, nurses, clinical and non-clinical personnels; (b) qualified HCWs possessing a valid Practice Certificate issued by the Ministry of Health of China; (c) voluntary participation in the study; (d) employed for at least 60 days at the end of 2022 during the COVID-19 pandemic. The exclusion criteria were as follows: (a) HCWs with pre-existing mental health conditions, such as schizophrenia, intellectual disabilities, depression, anxiety disorders, or organic diseases affecting the heart, brain, renal functions prior to enrollment; (b) refusal to participate in the survey; (c) incomplete responses in the online questionnaire. The studies involving humans were approved by Research Ethics Committee of Huizhou No. 2 Hospital (No. 2024-025). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
2.2 Questionnaire
In the study, data were collected using electronic questionnaires distributed via an online survey APP (https://www.wjx.cn/). The survey was anonymous and took about 10-15 min for each participant. Before distributing the questionnaire form, permission was obtained from department leaders in each hospital, and the researchers explained the purpose and anonymity of the survey to them. After obtaining the informed consent from the hospital staff, department heads sent the questionnaire to eligible HCWs. Two qualified staff reviewed the data. Among the 4,618 distributed questionnaires, 4,528 valid questionnaires (98.85%) were obtained after excluding 90 responses with insufficient data.
2.3 Methods
We collected the socio-demographic characteristics of participants, including gender, age, marital status, education, professional title, job type, years of work, hospital degree, health condition, the number of children, having been infected with COVID-19 infection, negative events (infection and sequelae after infection including physical problems; psychological problems; and economic pressure, social isolation, interruption of education, death of relatives and friends), as well as use of psychological support.
Mental health assessments were conducted using the Generalized Anxiety Disorder Scale (GAD-7), the Patient Health Questionnaire (PHQ-9), the Insomnia Severity Index (ISI), as well as the PTSD evaluation.
GAD-7 was adopted to assess the anxiety of each participant based on a four-point Likert scale (0-3) with a total score ranging from 0-21 (12). It is reliable to measure anxiety allied with clinical features showing strong consistency and good test-retest reliability, according to the previous description (13). The scoring criteria were as follows: 0-4 points for no anxiety; 5-9 for mild anxiety; 10-14 points for moderate anxiety, and >15 points for severe anxiety (14). The Cronbach’s alpha of GAD-7 in our study was reliable with a score of 0.947.
Depressive symptoms were assessed based on the PHQ-9 (15), a widely used tool for evaluating depression over the past two weeks. The PHQ-9 consisted of nine items, each scored from 0 (not at all) to 3 (almost every day), with total scores ranging from 0 to 27. Scores are classified as follows: 0-4 for no depression, 5-9 for mild depression, 10-14 for moderate depression, and >15 for severe depression. Its reliability was high in our study with the Cronbach’s alpha value of 0.917.
ISI is used to screen insomnia in general practice, assessing sleep-related issues over the past two weeks, which consists of seven items with a total score of 28 points. A score of 0-7 indicates no insomnia, while scores in a range of 8-14, 15-21, 22-28 suggests subclinical insomnia, moderate insomnia, and severe insomnia, respectively (16). In this study, its reliability was high with a Cronbach’s alpha of 0.941. The cutoff score for insomnia symptoms was set at 8.
The PTSD Checklist for DSM-5-Short Form (PCL-5), a 20-item self-report measure, was utilized to assess the frequency and severity of PTSD symptoms over the past month, using a 5-point Likert scale (0 = not at all; 4 = extremely). Total scores range from 0 to 80, with a cut-off score of 31-33 indicating a provisional PTSD diagnosis (17). In this study, the scale demonstrated strong reliability, with a Cronbach’s alpha of 0.947.
2.4 Statistical analysis
Data analysis was conducted using SPSS Statistics (Version 25.0, IBM, USA). Descriptive analysis was used to assess basic demographic data, with frequencies and percentages used to present counting data. Categorical variables were compared using the Chi-square test or Fisher’s exact test. Factors related to the anxiety, depression, ISI, and PTSD were analyzed using a univariate model, followed by multivariable logistic regression. All tests were two-sided, and a P value of <0.05 was considered significant.
3 Results
3.1 Demographic characteristics
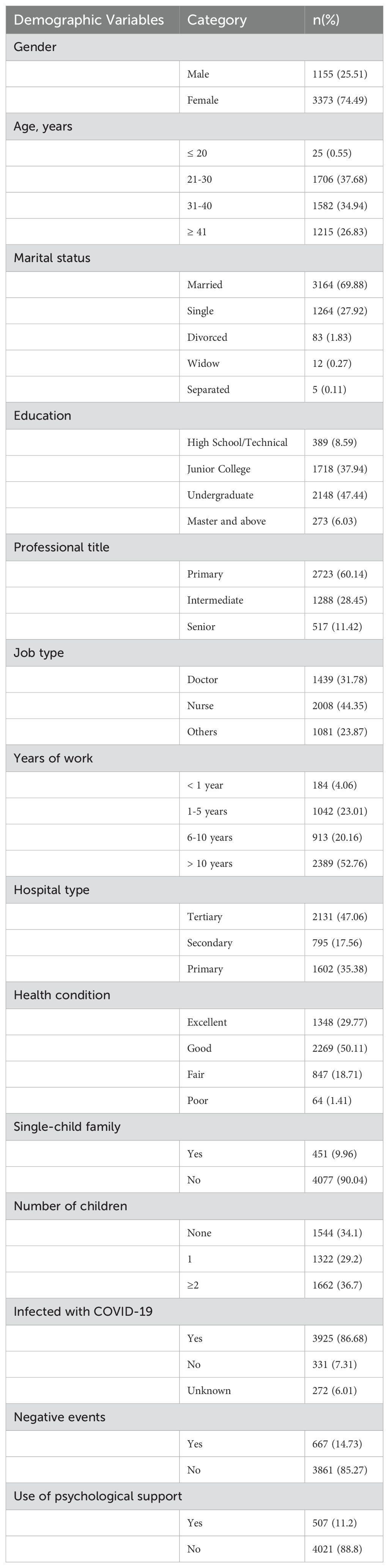
Among the participants, 1,155 (25.51%) were male, with the majority (37.68%) aging in 21-30 years old. The majority were married (69.88%), and in terms of education, most held either an undergraduate degree (47.44%) or a junior college diploma (37.94%). A significant portion (60.14%) had a primary or lower job title. For the occupation, nearly half (44.35%) of the participants were nurses. For the working time per day, over half (52.76%) reported a working duration of more than 10 hr. per day (Table 1).
3.2 Univariate logistic regression analysis
Among the 4,528 participants, the prevalence of anxiety, depression, insomnia, and PTSD symptoms was 45.0%, 59.4%, 40.5%, and 10.5%, respectively. For the univariate logistic regression analysis of anxiety symptoms, the variables with a P value of less than 0.05 were adopted including gender, age, education, professional title, job type, years of work, hospital type, health condition, number of children, negative events, as well as use of psychological support during COVID-19. For the depression symptoms, the adopted variables with a P value of less than 0.05 were gender, age, education, job type, hospital type, years of work, health condition, number of children, negative events, as well as use of psychological support during COVID-19. For insomnia, the variables with a P value of less than 0.05 included education, professional title, job type, years of work, hospital type, health condition, negative events, as well as use of psychological support during COVID-19. The variables for the PTSD symptoms with a P value of less than 0.05 included age, education, job type, years of work, health condition, negative events, and use of psychological support during COVID-19 (Supplementary Tables 1-4).
3.3 Multivariate logistic regression analysis
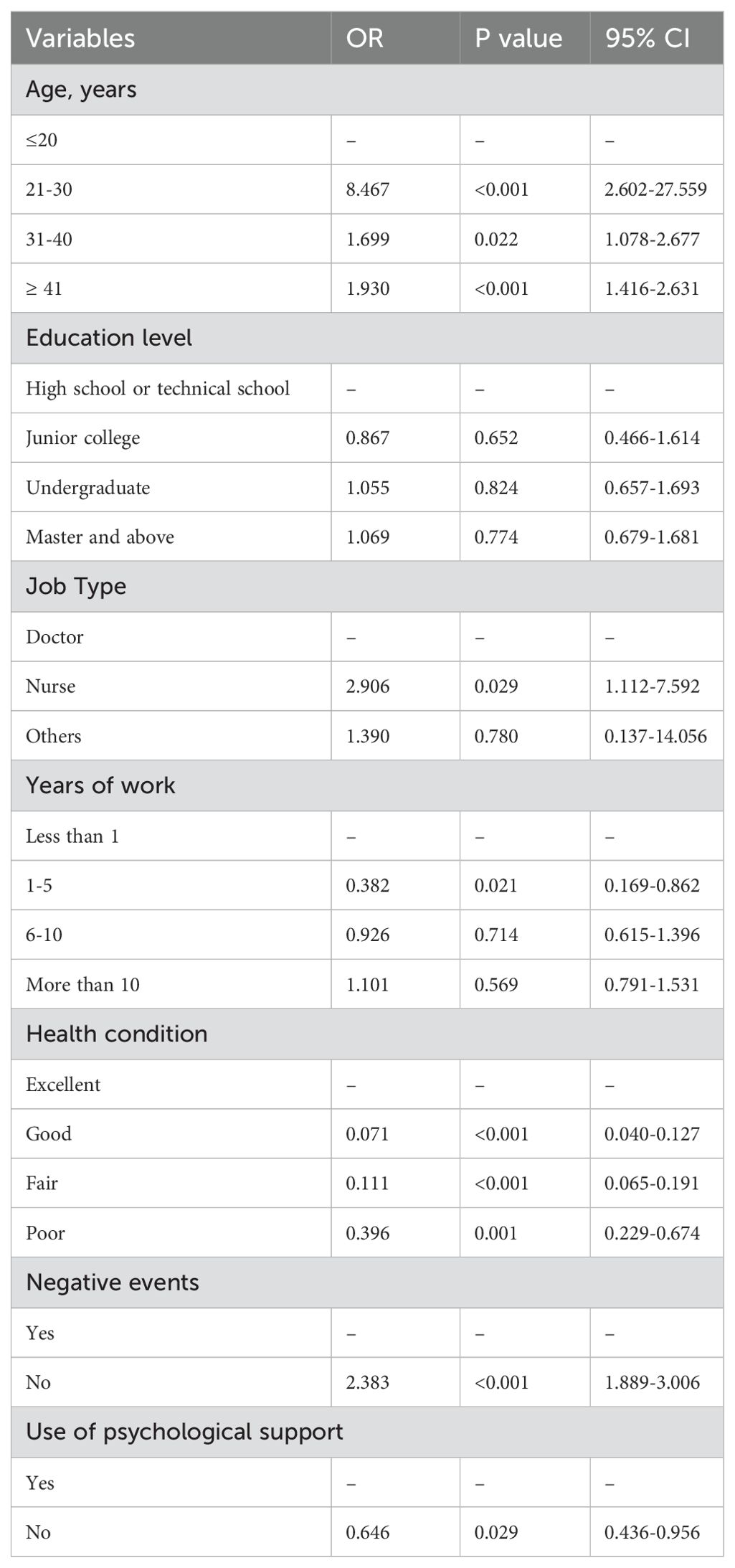
These statistically significant variables in univariate analysis were then adopted in the multivariate logistic regression analysis. Table 2 presented a multivariable logistic regression analysis of factors related to anxiety symptoms among participants. HCWs aged over 41 years old were more likely to experience anxiety than those under 20 (OR=1.435, 95%CI: 1.182-1.742). Compared to those with a high school or technical school education, those with a junior college education were less likely to report anxiety (OR=0.570, 95%CI: 0.385-0.842). Regarding professional titles, HCWs with intermediate titles were less likely to report anxiety compared to those with primary or lower titles (OR=0.722, 95%CI: 0.556-0.093). HCWs with 1-5 years of work experience were also less likely to report anxiety than those with less than 1 year of experience (OR=0.557, 95%CI: 0.364-0.852). Those in good, fair, or poor health, compared to excellent health, were more likely to experience anxiety symptoms. HCWs with two or more children were also more likely to report anxiety than those with no children. Additionally, HCWs who had not experienced negative events (OR=2.082, 95%CI: 1.734-2.499) were more likely to show anxiety. Unexpectedly, HCWs with no psychological support were likely to show reduced risk of anxiety (OR=0.889, 95%CI: 0.727-1.087).
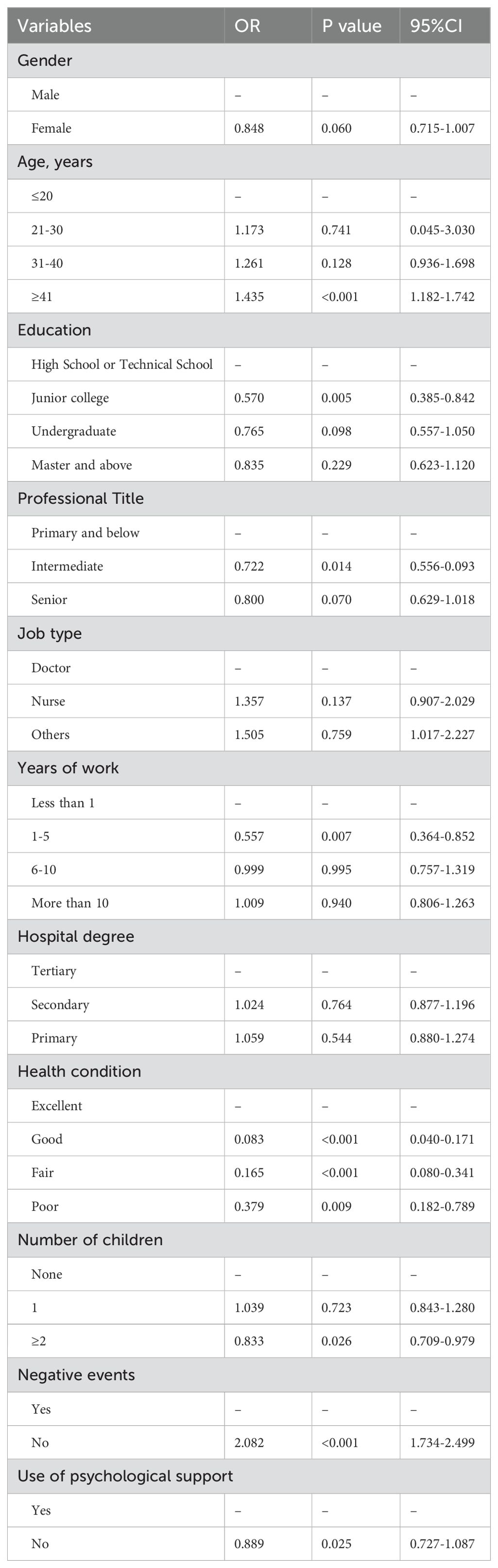
Table 2. Multivariable logistic regression analysis of related factors of anxiety symptoms among the HCWs.
Table 3 showed the multivariable logistic regression analysis of related factors of depression among the participants. Compared with male HCWs, female HCWs showed reduced risks of depression (OR=0.744, 95%CI: 0.627-0.883). HCWs of junior college showed reduced risks of developing depression compared with the high school or technical school HCWs (OR=0.561, 95%CI:0.382-0.823). In addition, HCWs who did not experience negative events showed increased risks of depression (OR=2.013, 95%CI:1.647-2.460) and those underwent no psychological support showed reduced risks of depression (OR=0.798, 95%CI:0.654-0.973).
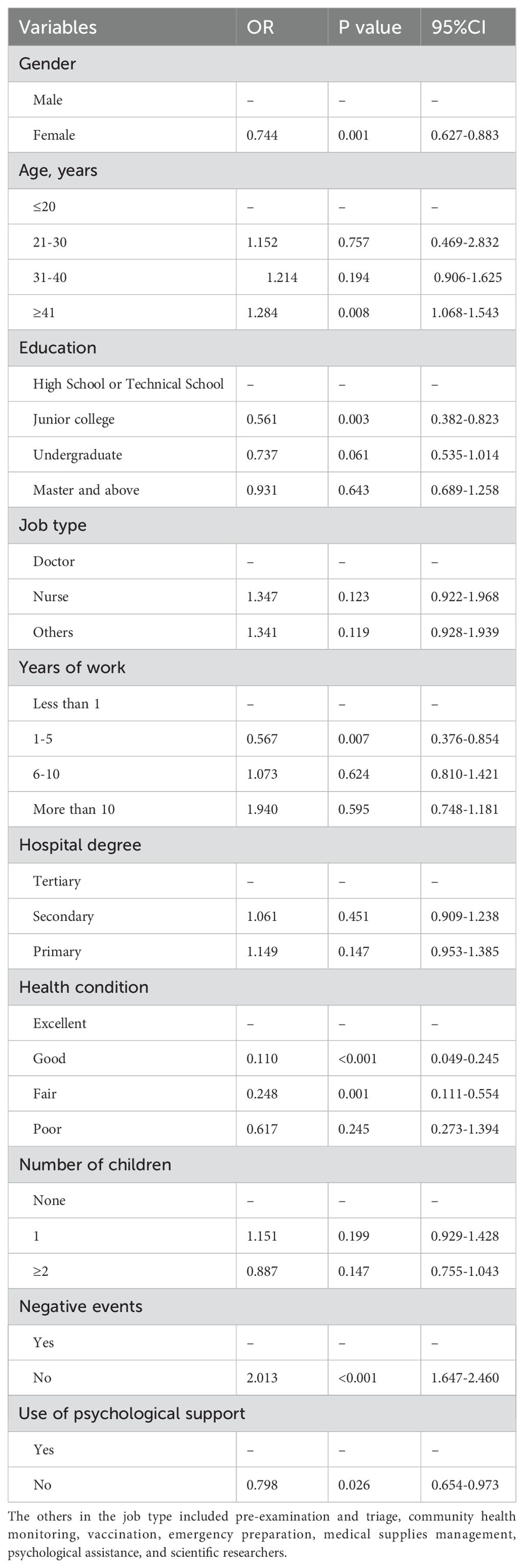
Table 3. Multivariable logistic regression analysis of related factors of depressive symptoms among the HCWs.
In terms of insomnia, compared with years of work less than 1, HCWs worked for 1-5 years were less likely to show insomnia (OR=0.536, 95%CI:0.369-0.777). Compared to HCWs working in the tertiary hospitals, those worked in the secondary hospitals showed increased risks of insomnia (OR=1.236, 95%CI:1.056-1.446). HCWs who did not experience negative events were more likely to show insomnia (OR=2.013, 95%CI:1.683-2.409, Table 4).
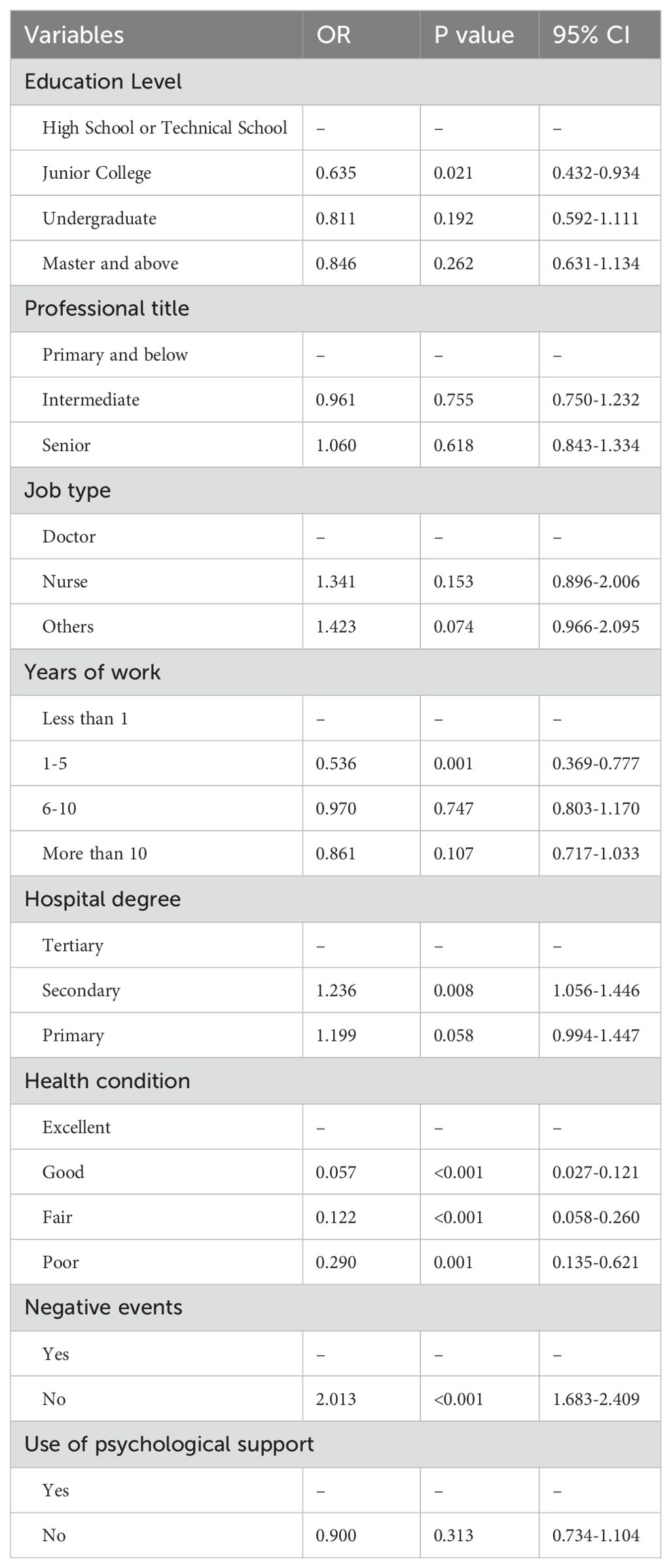
Table 4. Multivariable logistic regression analysis of related factors of insomnia symptoms among the HCWs.
HCWs over 20 years old had a higher risk of PTSD symptoms compared to those 20 or younger. Similarly, those with good, fair, or poor health were more likely to report PTSD symptoms compared to those in excellent health. Lastly, HCWs experienced no negative events were also more likely to show PTSD symptoms (OR=2.383, 95% CI: 1.889-3.006), while those with no psychological support showed reduced risk of PTSD symptoms (OR=0.646, 95% CI: 0.436-0.956, Table 5).
4 Discussion
This study examined the effects of the COVID-19 pandemic on frontline HCWs in Huizhou after the COVID-19 prevention and control policies in China. We assessed anxiety, depression, PTSD, and sleep quality of the HCWs, which revealed that the prevalence rates of anxiety, depression, insomnia, and PTSD were 45.0%, 59.4%, 40.5% and 10.5%, respectively. These rates were lower than those observed among Chinese HCWs during the peak of the pandemic and also lower than Xiao’s study, which reported 62.51% for anxiety, 69.20% for depression, and 76.78% for insomnia among nurses (18). One possible explanation was that HCWs in our study were more prepared during this period to reduce their anxiety, depression, insomnia, and PTSD. Over time, their fear and anxiety diminished as they adapted to the ongoing nature of COVID-19. However, mental health issues can persist long after recovery (19). Therefore, continued evaluation of the mental health of COVID-19 survivors is essential.
In the COVID-19 crisis, frontline HCWs encountered immense physical and mental pressure. They managed a growing number of patients, faced risks of infection, and struggled with limited resources and emotional support (20). In addition, COVID-19 infection would further increase their anxiety and depression. Similarly, the general public is also at risk of psychological distress, increasing the overall anxiety burden among the HCWs. The sudden shortage of HCWs and the number surge in cases, especially after the full liberation of COVID-19 prevention, have increased pressure on HCWs to provide adequate care in Mainland China. In the presence of high COVID-19 case numbers per capita, junior doctors in the US who directly cared for patients with a COVID-19 diagnosis experienced elevated levels of anxiety and depression (21). In contrast, in a study performed in Australia, the authors indicated that junior doctors were mentally well and able to function at a high level during a global pandemic (22). In our study, multivariable logistic regression analysis revealed that junior HCWs, particularly those with 1-5 years of experience or 2 or more children, showed reduced risks of developing anxiety and depression compared with the other counterparts. Female HCWs were more prone to show anxiety and depression than their male counterparts, possibly due to greater sensitivity, weaker psychological endurance, and the burden of balancing work with childcare and household duties (23). Consistently, they reported higher rates of depression during COVID-19, influenced by individual factors like lack of social support and organizational factors such as heavy workloads and lack of recognition. However, some studies highlight specific situations where male HCWs experienced higher levels of psychological distress. For example, unemployment and isolation due to quarantine had a more pronounced negative effect on mental health in male HCWs, particularly increasing depression and anxiety levels. The role of employment appears crucial in influencing male emotional states, with unemployed male HCWs more severely impacted by the psychological effects (24, 25). In this study, female HCWs did not show increased risks of anxiety and depression compared with the male counterparts. In the future, more sample sized studies are required to further illustrate the sex differences in depression and anxiety during the post-COVID-19 period.
Various psychosocial factors during COVID-19, such as stress, anxiety, depression, workload, and uncertainty about disease control, significantly impacted sleep quality. In a previous study, grassroots HCWs, facing increased responsibilities after community management phase, experienced greater work pressure and sleep deprivation (26). Additionally, reduced income during the pandemic contributed to insomnia, especially among those with low annual income and 1-5 years of experience (27). Our data showed that HCWs in secondary hospitals were more likely to show insomnia (OR=1.236, 95%CI:1.056-1.446), as their incomes were lower compared with those in the tertiary hospitals. In some cases, the prevalence of insomnia among frontline HCWs reached 30% to 60% during the peak of the crisis (28). This significant rise in sleep disturbances was driven by increased workload, prolonged exposure to high-stress environments, fear of infection, and emotional fatigue from witnessing severe patient outcomes and death. These challenges have underscored the need for targeted interventions to address the sleep-related and broader psychological health challenges faced by HCWs during and after the pandemic (29, 30). In a previous study focused on the combined impact of gender and age on PTSD and insomnia during COVID-19 outbreak in China, Liu et al. reported that females above 50 years of age showed a lower level of depressive symptoms (OR = 0.448, 95%CI: 0.220–0.911) compared with females aged 18–25 (31). Consistently, our data showed that HCWs aged 21 or more showed increased risks of PTSD compared with those aged less than 20 years. Existing literatures showed that poor health generally increased the risk of PTSD. For instance, HCWs who experienced physical exhaustion, illness, or long-term health complications were often more susceptible to PTSD because they had fewer physical and psychological resources to cope with the trauma (32). Unexpectedly, our data showed that HCWs with good, fair or poor conditions showed reduced risks of developing PTSD compared with these with excellent health conditions. One possible explanation was that those with excellent conditions were more likely to take more tasks during and after COVID-19, which may face more challenges than others. In the future, we will expand our sample size to illustrate this. HCWs who did not experience negative events (e.g. physical and mental problems, financial pressure, death of relatives and friends) were more likely to show anxiety (OR=2.082, 95%CI:1.734-2.499), depression (OR=2.013, 95%CI:1.647-2.460) and insomnia (OR=2.013, 95%CI:1.683-2.409). This may reveal the complexity of mental health mechanisms under the special context of the epidemic. This phenomenon needs to be explained in multiple dimensions. For example, long-term exposure to high-risk environments, uncertainty about the direction of the epidemic, and other persistent low-intensity stress are not included in negative events, but cause psychological symptoms through cumulative effects. Although they have not experienced negative events, excessive alertness to potential risks leads to continuous activation of the sympathetic nervous system, resulting in psychological reactions similar to anxiety, depression and insomnia. It is also possible that those who have experienced negative events can gain growth resilience by reconstructing cognition, while those who have not experienced it lack this opportunity for psychological reconstruction and instead fall into a sense of meaninglessness. In short, in extreme stress situations, we need to pay attention to the identification of implicit stress.
Several limitations of our study should be noted. First, as it is based on cross-sectional data, no causal relationships can be inferred, and ongoing changes in psychological status of HCWs were not examined. Longer-term research may yield more accurate results. Second, the use of self-reported scales is limited by perceptions and potential biases of each participant in survey distribution. Third, self-reported psychological responses may be affected by recall bias, highlighting the need for more qualitative and in-depth studies in this area. Fourth, this is a retrospective analysis, and we could not analyze the long-term effects in the participants.
5 Conclusion
In this study, we investigated the prevalence of anxiety, depression, insomnia, and PTSD in the HCWs after the COVID-19 pandemic. Our study reported prevalence rates of 45.0% for anxiety, 59.4% for depression, 40.5% for insomnia, and 10.5% for PTSD. In addition, we also screened the risk factors for anxiety, depression, insomnia and PTSD.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by Research Ethics Committee of Huizhou No. 2 Hospital (No. 2024-025). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XW: Data curation, Formal analysis, Methodology, Resources, Software, Writing – original draft. FF: Methodology, Resources, Software, Validation, Visualization, Writing – original draft. AG: Conceptualization, Investigation, Project administration, Supervision, Validation, Writing – review & editing. YW: Data curation, Formal analysis, Methodology, Software, Writing – original draft. WP: Investigation, Methodology, Validation, Writing – original draft. XZho: Investigation, Methodology, Validation, Writing – original draft. XZha: Investigation, Project administration, Visualization, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Science and Technology Project of Social Development in Huizhou Science and Technology Bureau (grant No.: 2022CQ010015).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1520361/full#supplementary-material
References
1. Chaudhary R, Rohilla M, Chauhan S, Saini M, Aman S, Singla H, et al. The pandemic’s unseen wounds: COVID-19’s profound effects on mental health. Ann Med Surg (Lond). (2023) 85:4954–63. doi: 10.1097/ms9.0000000000001223
2. Liu H, Zhou N, Zhou Z, Tao X, Kong Y, Zhang M. Symptoms of post traumatic stress disorder and their relationship with the fear of COVID-19 and COVID-19 burden among health care workers after the full liberalization of COVID-19 prevention and control policy in China: a cross-sectional study. BMC Psychiatry. (2023) 23:902. doi: 10.1186/s12888-023-05399-z
3. Zhou Y, Liu A, Pu Z, Zhou M, Ding H, Zhou J. An investigation of the psychological stress of medical staff in Shanghai shelter hospital during COVID-19. Front Psychol. (2023) 14:1083793. doi: 10.3389/fpsyg.2023.1083793
4. Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int J Clin Health Psychol. (2021) 21:100196. doi: 10.1016/j.ijchp.2020.07.007
5. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
6. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
7. Jia X, You L, An Q. Practices and outcomes of promoting the competencies of psychological assistance professionals in defeating the COVID-19 pandemic. Psychol Stud (Mysore). (2021) 66:361–8. doi: 10.1007/s12646-021-00615-w
8. Smallwood N, Willis K. Mental health among healthcare workers during the COVID-19 pandemic. Respirology. (2021) 26:1016–7. doi: 10.1111/resp.14143
9. Biber J, Ranes B, Lawrence S, Malpani V, Trinh TT, Cyders A, et al. Mental health impact on healthcare workers due to the COVID-19 pandemic: a U.S. cross-sectional survey study. J Patient Rep Outcomes. (2022) 6:63. doi: 10.1186/s41687-022-00467-6
10. Chingono RMS, Nzvere FP, Marambire ET, Makwembere M, Mhembere N, Herbert T, et al. Psychological distress among healthcare workers accessing occupational health services during the COVID-19 pandemic in Zimbabwe. Compr Psychiatry. (2022) 116:152321. doi: 10.1016/j.comppsych.2022.152321
11. Kwaghe AV, Kwaghe VG, Habib ZG, Kwaghe GV, Ilesanmi OS, Ekele BA, et al. Stigmatization and psychological impact of COVID-19 pandemic on frontline healthcare Workers in Nigeria: a qualitative study. BMC Psychiatry. (2021) 21:518. doi: 10.1186/s12888-021-03540-4
12. Johnson SU, Ulvenes PG, Øktedalen T, Hoffart A. Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. (2019) 10:1713. doi: 10.3389/fpsyg.2019.01713
13. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
14. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
15. Yu X, Tam WW, Wong PT, Lam TH, Stewart SM. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry. (2012) 53:95–102. doi: 10.1016/j.comppsych.2010.11.002
16. Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
17. Rajkumari B, Akham N, Konjengbam OK, Pangambam AD, Ningthoujam SD. Post-traumatic stress disorder among COVID-19 survivors in Manipur: A cross-sectional study. J Family Med Prim Care. (2022) 11:2139–45. doi: 10.4103/jfmpc.jfmpc_1474_21
18. Xiao J, Liu L, Peng Y, Wen Y, Lv X, Liang L, et al. Anxiety, depression, and insomnia among nurses during the full liberalization of COVID-19: a multicenter cross-sectional analysis of the high-income region in China. Front Public Health. (2023) 11:1179755. doi: 10.3389/fpubh.2023.1179755
19. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. (2009) 31:318–26. doi: 10.1016/j.genhosppsych.2009.03.001
20. Vera San Juan N, Martin S, Badley A, Maio L, Gronholm PC, Buck C, et al. Frontline health care workers’ Mental health and well-being during the first year of the COVID-19 pandemic: analysis of interviews and social media data. J Med Internet Res. (2023) 25:e43000. doi: 10.2196/43000
21. Kannampallil TG, Goss CW, Evanoff BA, Strickland JR, McAlister RP, Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS One. (2020) 15:e0237301. doi: 10.1371/journal.pone.0237301
22. Bartholomew A, Sanatkar S, Counson I, Harvey SB. Junior doctors’ mental health and coronavirus disease safety concerns. Aust N Z J Public Health. (2022) 46:307–13. doi: 10.1111/1753-6405.13213
23. Zhu H, Yang X, Xie S, Zhou J. Prevalence of burnout and mental health problems among medical staff during the COVID-19 pandemic: a systematic review and meta-analysis. BMJ Open. (2023) 13:e061945. doi: 10.1136/bmjopen-2022-061945
24. Levy I. Stress, anxiety, and depression in times of COVID-19: Gender, individual quarantine, pandemic duration and employment. Front Public Health. (2022) 10:999795. doi: 10.3389/fpubh.2022.999795
25. Vallières F, Murphy J, McBride O, Shevlin M, Gilmore B, Travers Á, et al. The role of psychosocial factors in explaining sex differences in major depression and generalized anxiety during the COVID-19 pandemic. BMC Public Health. (2022) 22:1563. doi: 10.1186/s12889-022-13954-8
26. Nguyen TT, Le XTT, Nguyen NTT, Nguyen QN, Le HT, Pham QT, et al. Psychosocial impacts of COVID-19 on healthcare workers during the nationwide partial lockdown in Vietnam in April 2020. Front Psychiatry. (2021) 12:562337. doi: 10.3389/fpsyt.2021.562337
27. Premo EM, Magnuson KA, Lorenzo NE, Fox NA, Noble KG. Mental health and sleep quality of low-income mothers of one-year-olds during the COVID-19 pandemic. Infant Ment Health J. (2023) 44:572–86. doi: 10.1002/imhj.22074
28. Chatterjee SS, Chakrabarty M, Banerjee D, Grover S, Chatterjee SS, Dan U. Stress, sleep and psychological impact in healthcare workers during the early phase of COVID-19 in India: A factor analysis. Front Psychol. (2021) 12:611314. doi: 10.3389/fpsyg.2021.611314
29. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
30. Salari N, Khazaie H, Hosseinian-Far A, Ghasemi H, Mohammadi M, Shohaimi S, et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Global Health. (2020) 16:92. doi: 10.1186/s12992-020-00620-0
31. Liu C, Liu D, Huang N, Fu M, Ahmed JF, Zhang Y, et al. The combined impact of gender and age on post-traumatic stress symptoms, depression, and insomnia during COVID-19 outbreak in China. Front Public Health. (2020) 8:620023. doi: 10.3389/fpubh.2020.620023
Keywords: depression, insomnia, post-traumatic, cross-sectional study, stress disorder
Citation: Wang X, Fu F, Gan A, Wu Y, Pan W, Zhou X and Zhang X (2025) Psychological status of healthcare workers in the post-COVID 19 period in China: a retrospective multicentric cross-sectional study. Front. Psychiatry 16:1520361. doi: 10.3389/fpsyt.2025.1520361
Received: 31 October 2024; Accepted: 20 March 2025;
Published: 07 April 2025.
Edited by:
Feten Fekih-Romdhane, Tunis El Manar University, TunisiaReviewed by:
Fengjiao Chen, Sichuan University, ChinaSolomon Debela Bekeko, University of Gondar, Ethiopia
Copyright © 2025 Wang, Fu, Gan, Wu, Pan, Zhou and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aihua Gan, aHpzeXhoMjIxOTUzMEAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Xiaoli Wang1†
Xiaoli Wang1† Aihua Gan
Aihua Gan