- 1Department of Psychiatry, Nursing, Midwifery, and Public Health, College of Health Sciences, Mattu University, Mattu, Ethiopia
- 2Department of Medicine, Gambella General Hospital, Gambella, Ethiopia
- 3Department of Midwifery, and Psychiatry, College of Health Sciences, Madda Walabu University, Sheshemene, Ethiopia
- 4Department of Midwifery, Institute of Health Sciences, Wollaga University, Nekemte, Ethiopia
- 5Department of Public Health, Mattu Health Sciences College, Mattu, Oromia, Ethiopia
Background: Among various mental disorders, anxiety disorder is commonly reported in HIV-positive individuals. Compared to the general population, people living with HIV/AIDS exhibit a higher prevalence of anxiety, with an estimated figure of 68.2% versus 29% in the general population. However, there is a scarcity of studies on the prevalence and associated factors of anxiety among people living with HIV/AIDS in Ethiopia.
Method: An institution-based cross-sectional study was conducted among 320 participants at Gambella General Hospital. The Beck Anxiety Inventory (BAI) scale, Fagerström Test for Nicotine Dependence (FTND), Severity of Dependence Scale (SDS), and the Alcohol Use Disorder Identification Test (AUDIT) were used to collect the data. Data analysis was performed using SPSS version 25. Bivariate and multivariable logistic regressions were employed to identify independently associated variables, and statistical significance was determined at a p-value <0.05.
Results: Out of a total of 323 samples, 320 respondents completed all items, resulting in a response rate of 99.07%. The results showed that 28.4% (95% CI = 23.2–33.9) of participants had anxiety. Factors such as being aged 25 to 40 years, having seen a counselor, HIV disclosure, alcohol use disorders, and perceived high stigma were significantly associated with anxiety in people living with HIV (PLWH).
Conclusion: In the study area, about two out of every seven people living with HIV/AIDS experienced anxiety symptoms. Factors such as being aged 25 to 40 years, having seen a counselor, HIV disclosure, alcohol use disorders, and perceived high stigma were significantly associated with anxiety in this population. Based on these findings, timely intervention is recommended to enhance the overall well-being and quality of life for people living with HIV (PLWH), leading to better health outcomes, reducing the burden of mental health issues, and supporting more holistic, patient-centered care.
Background
Among various mental disorders, anxiety disorders are one of the most common psychiatric illnesses associated with HIV (1). Anxiety disorders are more than twice as common among HIV+ individuals as in the general population (2). Overall, different studies have reported the incidence of anxiety disorders among people living with HIV/AIDS ranging from 0.6% to 68.2% (3, 4), compared to 29% in the general population (5).
Human immunodeficiency virus (HIV) is a major public health issue that has affected about 39.0 million (33.1–45.7 million) people as of the end of 2022. Of these, an estimated 25.6 million (21.6–30.0 million) people were from Africa (6). An estimated 753,100 people were living with HIV in Ethiopia, with the prevalence being higher among urban populations and women (7).
HIV/AIDS and anxiety disorders have a strong relationship (8). Anxiety disorders affect the prognosis of HIV, delay the time to viral suppression, and increase the rate of antiretroviral failure even after suppression (9). Anxiety may also contribute to behaviors that increase the risk of HIV infection, such as unprotected sex and substance use (10). In addition, anxiety disorders among HIV+ individuals lead to a lower quality of life (11), higher healthcare costs (12), an increased risk of suicide (13), worse health outcomes, and ultimately higher mortality (14). Besides the discomfort caused by anxiety disorders, they can interfere with an HIV+ person’s overall success in managing HIV, as they are a major cause of non-adherence to medication (2).
Although HIV is a public health concern, the mental health of PLHIV is often neglected (6, 15) and still requires more attention and focus. In particular, low-income countries pay almost no attention to or provide no treatment for the mental health of PLWH. This means that the anxiety experienced by PLWH has been largely overlooked.
It is crucial that the current study provides key recommendations to address the many factors associated with anxiety among PLWH and promote the health of the affected population. The aim of this study was to assess the prevalence and underlying causes of anxiety among HIV/AIDS patients at Gambella General Hospital in southwestern Ethiopia.
Methods
Study setting
The study was conducted at Gambella General Hospital, which is located in the Gambella Regional State, 760 km southwest of Addis Ababa.
Study design and period
An institution-based cross-sectional study was conducted from May 10 to 30, 2023.
Study population
All patients living with HIV who were on follow-up at Gambella General Hospital were included in the sample during the data collection period.
Eligibility criteria
Inclusion criteria: All adults living with HIV/AIDS, aged 18 years and above, who were on follow-up at the Gambella General Hospital ART clinic were included in the study.
Exclusion criteria: Participants who were unable to respond or were severely ill were excluded from the study.
Sample size determination
Using a single population proportion formula and the following assumptions—95% confidence level (Zα/2 = 1.96), 5% margin of error (d = 0.05), and a prevalence rate of anxiety among PLWHA of 25.6% (16)—the total sample size was calculated. Finally, by adding a 10% non-response rate, the total sample size was 323.
Sampling technique
A consecutive sampling technique was used to select 323 patients attending the Gambella General Hospital ART clinic during the study period. There were 4,357 adults with 350 ART clients who required follow-up in the ART clinic annually and monthly, respectively. The sample was collected until the required sample size was reached. To avoid repeating patients during the data collection period, if they came for a second visit, their patient card numbers were recorded on the questionnaires and cross-checked.
Data collection tools
Data was collected using a structured questionnaire by face-to-face interview. The levels of anxiety were assessed using the Beck Anxiety Inventory (BAI) scale. The BAI consists of 21 self-reported items (four-point scale) used to assess the intensity of physical and cognitive anxiety symptoms during the past week. Scores may range from 0 to 63: minimal anxiety levels (0–7), mild anxiety (8–15), moderate anxiety (16–25), and severe anxiety (26–63). Its test–retest reliability (1 week) = 0.75 (17). Perceived stigma was assessed using the short 12-item stigma scale. It was rated on four-point Likert scores (1 = strongly disagree to 4 = disagree), and the score ranged from 12 to 48 (18). In this study, the mean was used as the cutoff point. Participants scoring 22 or above were classified as “high perceived stigma,” whereas scores below 22 were considered “low perceived stigma.”
The Fagerstrom Test for Nicotine Dependence (FTND) was used to assess tobacco use disorder. It has six items, with a total score ranging from 0 to 10 to measure nicotine dependence. A cutoff point ≥5 was considered to indicate tobacco dependence (19, 20). Khat use disorder was assessed by using the tool Severity of Dependence Scale (SDS). It has five items that are scored on a four-point scale (0–3) (21). The alcohol use disorder identification test (AUDIT) was used to assess alcohol use disorders and is developed by the World Health Organization (WHO). The overall rating for AUDIT is 40. A score of 8 or greater is considered to be a drinking disorder (22, 23).
Data processing and analysis
Once all necessary data were obtained, the data were checked for completeness. Data were edited, cleaned, coded, and entered into EpiData version 3.1. Data were analyzed using SPSS version 25.0. For the analysis of obtained data, simple descriptive statistics were used. Bivariate analysis was used to see the significance of the association. Variables that show a strong association in bivariate analysis were entered into multivariable logistic regressions to control for confounders, and the significance of association was declared at p-value 0.05 with 95% confidence interval.
The Hosmer–Lemeshow test p-value = 0.126. The logistic regression model fits the data well, as the p-value is greater than 0.05. Multicollinearity was checked using variance inflation factors (VIF). The VIF values were less than 2.
Results
Socio-demographic and clinical-related factors and substance use characteristics of respondents
From the total of 323 participants, 320 completed all items. Among 320 participants, the majority were women. More than half were Protestant religion followers (Table 1). About five out of nine respondents have comorbid medical illnesses such as diabetes mellitus, asthma, TB, and hypertension (Table 2). About two-fifths of the participants have a lifetime history of khat chewing, and for every nine respondents, seven of them drink alcohol in their life (Table 3).

Table 1. Background characteristics of study participants among persons living with HIV/AIDS at Gambella General Hospital, South West Ethiopia, May 2023 (N =320).
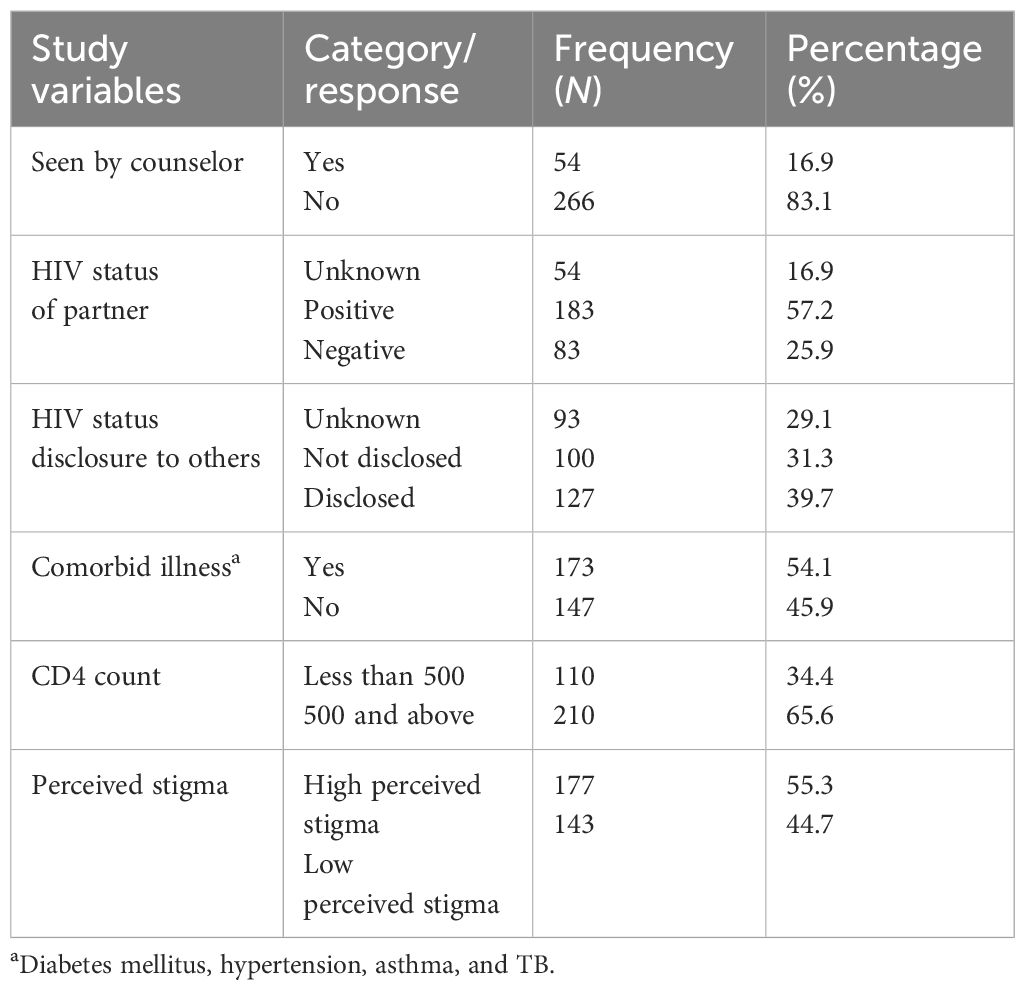
Table 2. HIV related clinical characteristics of study participants among persons living with HIV, Gambella General Hospital, South West Ethiopia, May 2023 (N =320).
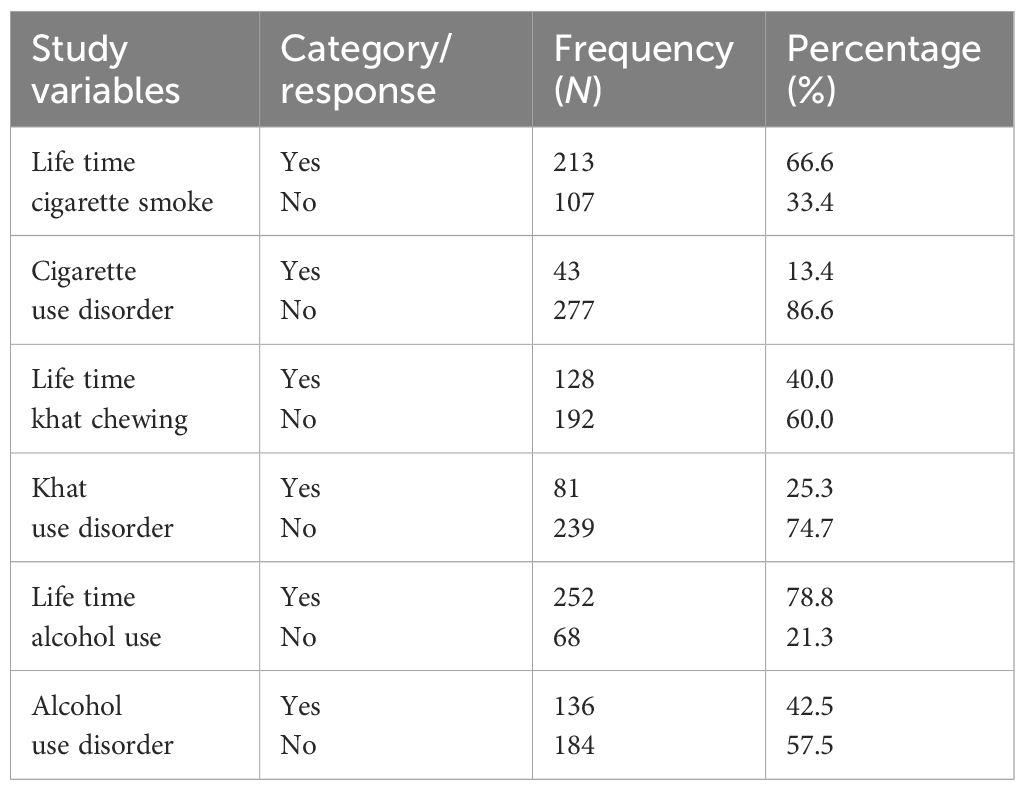
Table 3. Substance use characteristics of study participants among persons living with HIV, Gambella General Hospital, South West Ethiopia, May 2023 (N =320).
Prevalence of anxiety among PLWH
The prevalence of anxiety among adult people living with HIV/AIDS at Gambella General Hospital using the Beck Anxiety Inventory scale was 28.4.
Factors associated with anxiety among PLWH
Marital status, educational level, living arrangement, income per month, duration of being diagnosed with HIV/AIDS, cigarette use disorder, khat use disorder, and having another comorbid medical disorder were not significantly associated with having anxiety in the bivariate logistic regression. However, sex, residence, HIV status of partner, and number of CD4 count showed an association only in the bivariate analysis but did not show a significant association in the final model.
Multivariable logistic regression analysis revealed that age, seen by a counselor, HIV disclosure, alcohol use disorder, and perceived high stigma had a significant association with anxiety in PLWH (Table 4). Moreover, chi-square tests were conducted (Table 5). Regarding the interaction term tests (B = 0.104, p = 0.848), the effect of sex on anxiety did not change based on alcohol use disorder (Table 6).
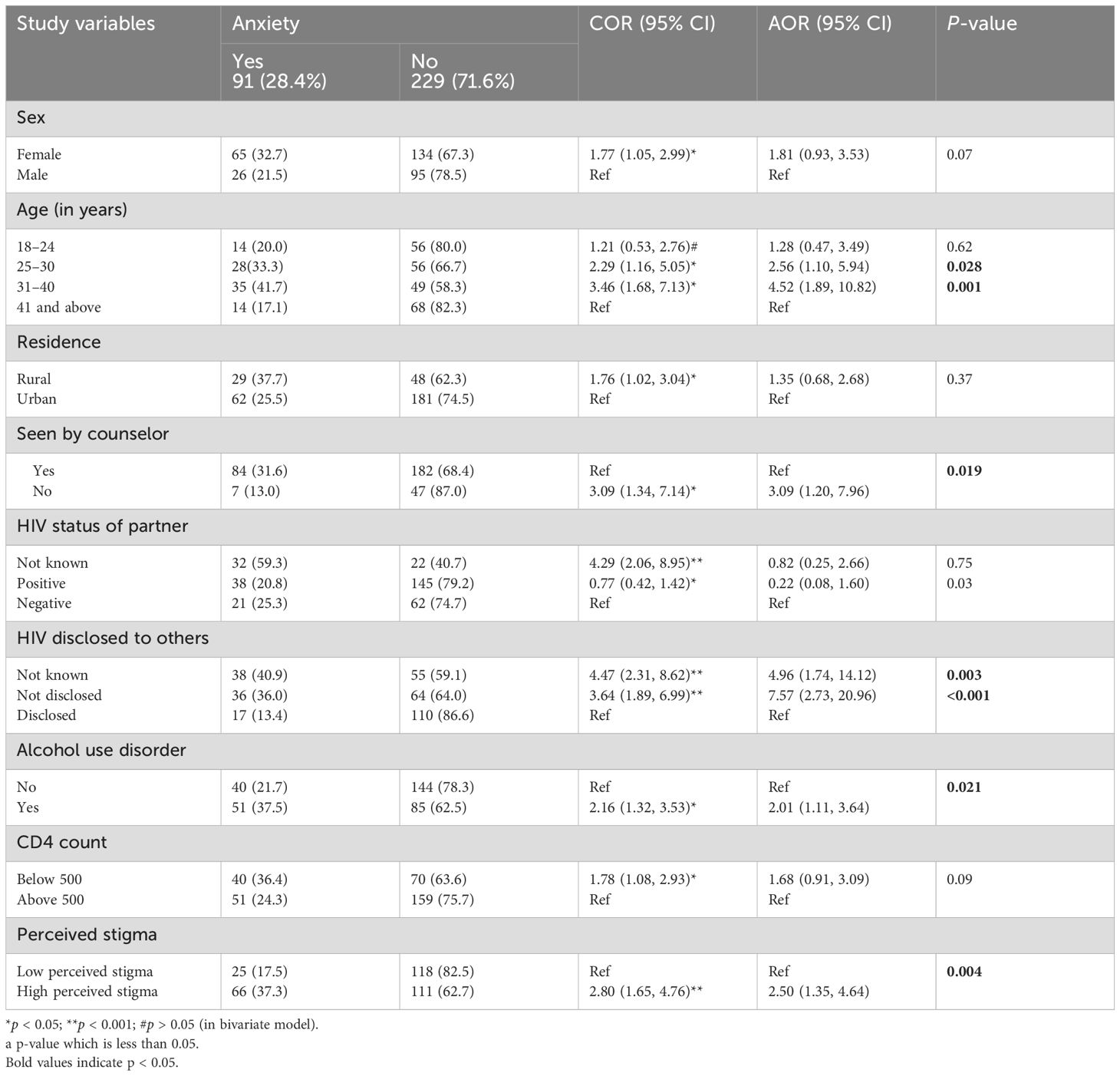
Table 4. Factors associated with anxiety by bivariate and multivariate logistic regression among PLWH, Gambella General Hospital, South West Ethiopia, May 2023 (N =320).
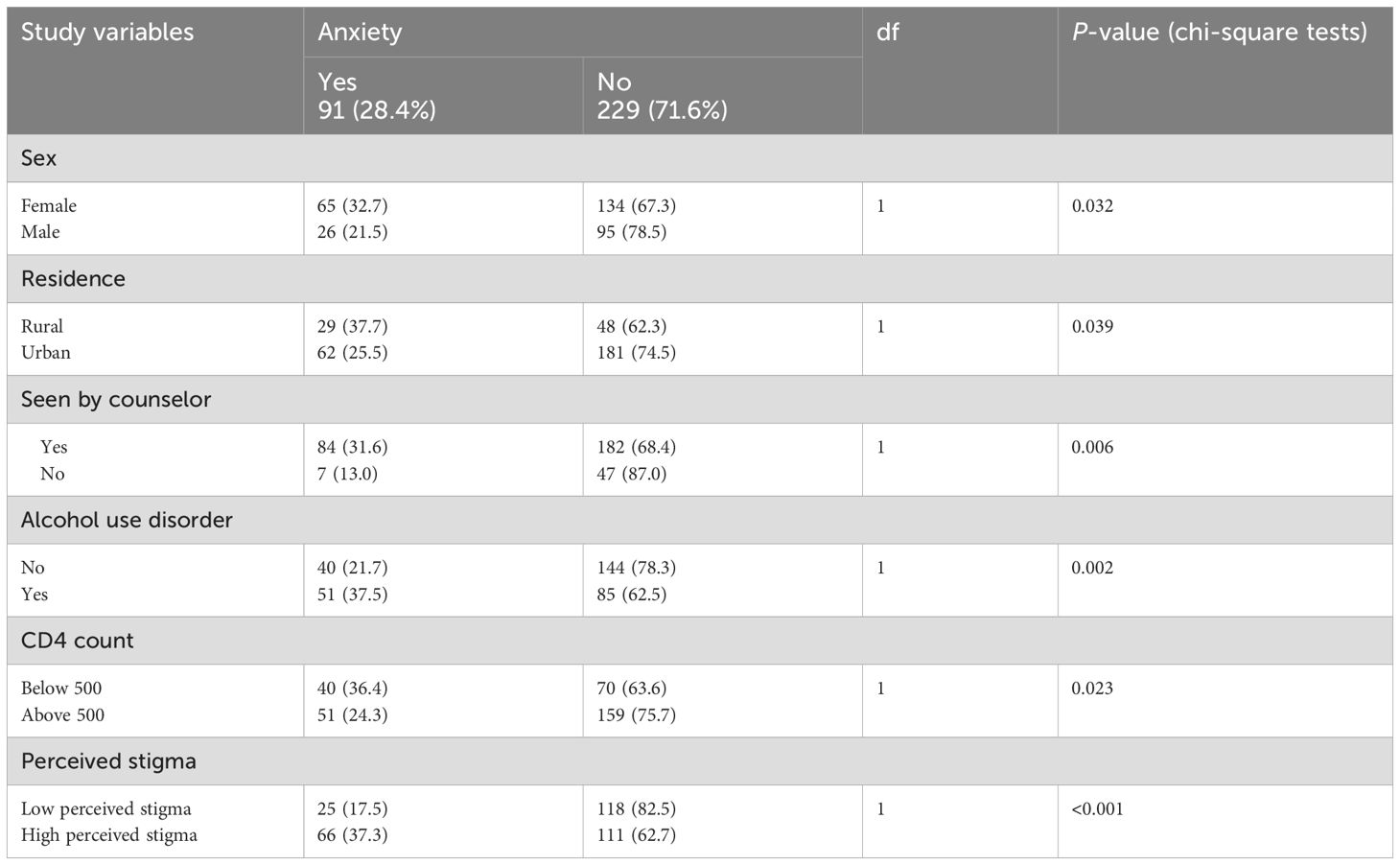
Table 5. Chi-square tests among PLWH, Gambella General Hospital, South West Ethiopia, May 2023 (N =320).
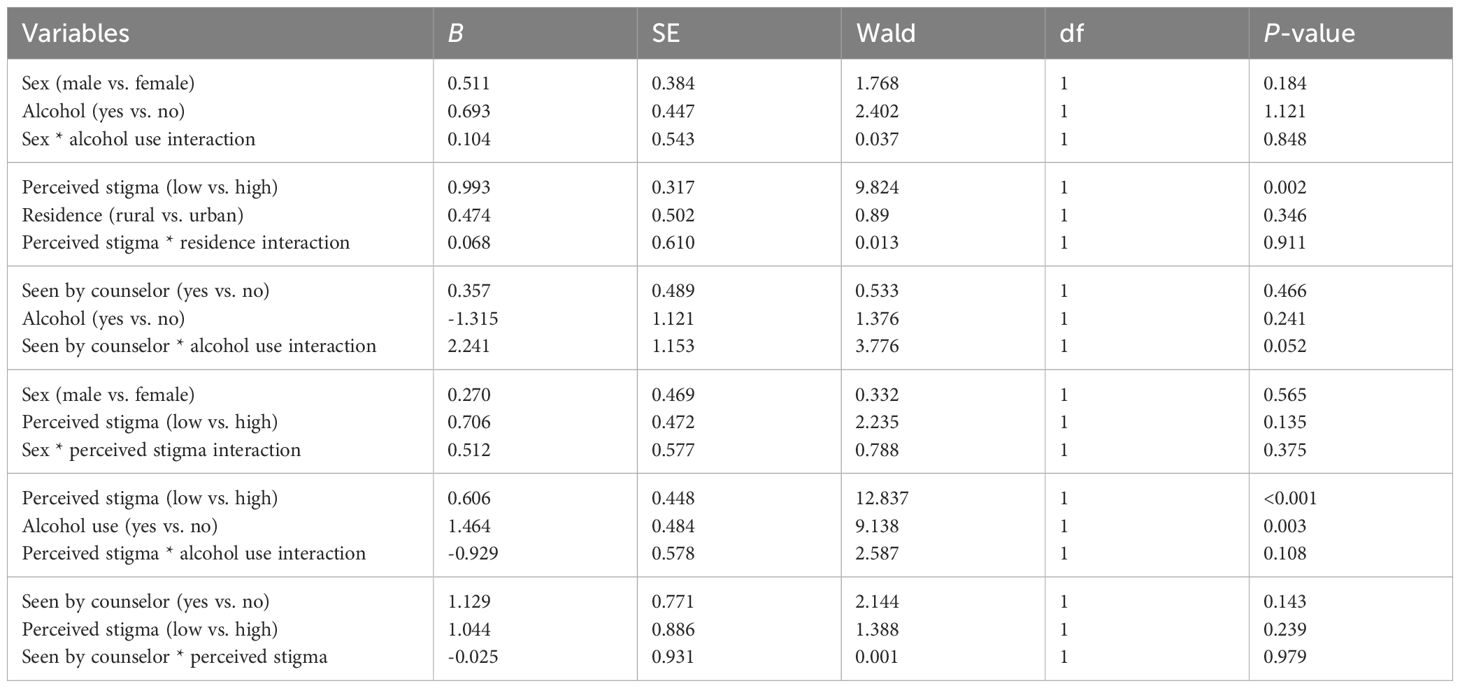
Table 6. Interaction term analysis among PLWH, Gambella General Hospital, South West Ethiopia, May 2023 (N =320).
Discussion
The results from this study indicated that the prevalence of anxiety among the adult population of HIV/AIDS-positive individuals was 28.4%. This finding is consistent with a previous study (16). A possible reason for this could be that both the current and the previous studies were conducted on populations with similar geographical and socioeconomic characteristics. This finding is lower when compared to the previous studies (24, 25). The possible reason might be the difference in population type. The previous study (24) was conducted among clients of voluntary counseling and HIV testing. People may feel very anxious and nervous when they voluntarily undergo a blood test and the virus is detected in their blood. However, our current study was conducted on individuals who were already diagnosed with HIV/AIDS and were undergoing treatment. The difference in study design may also impact the difference in results. The previous study (25) used a case–control design, while the current study employed a cross-sectional design. Another possible reason could be the inclusion of individuals who had not yet started HIV/AIDS treatment in the previous study. Additionally, the previous study was conducted only on individuals over 30 years of age. As is well known, people over 30 often have many responsibilities and experience higher levels of stress. The current finding is higher when compared to the previous study (26, 27). The reason might be that the previous study (27) used a systematic review approach. Additionally, the previous study was conducted in developed countries, where adequate medical services are available and people’s awareness is higher. Another discrepancy in the results is that a longer period of time has passed since the previous study (26) was conducted. As is well known, there is a long-term difference between the two studies, and their results differ. Therefore, these factors may explain why our research results are higher than those of the previous study.
This study showed that participants aged 25 to 40 years were more likely to report an anxiety disorder compared to those aged 41 years and older. This finding is inconsistent with the previous result (28). The possible reason could be that the tool used to assess anxiety and the methods of analysis in the current study differ from those in the previous study. People in their 20s and 30s are adults, and this age group also represents the productive workforce. Additionally, most people get married around this age, and they have responsibilities both to their nation and to their family. They are self-sufficient at this age and often go above and beyond to help others. The study’s findings indicate that patients with HIV/AIDS in this age range who also meet the aforementioned criteria are more likely to develop anxiety than those over 41 years old who also report having anxiety symptoms.
Compared to their peers, the participants who saw the counselor exhibited fewer anxiety symptoms. This finding is supported by the previous study (29). As is well known, counseling helps patients with issues that medicine cannot address. The goal of the counseling process is to help clients become more aware of their mental processes and to teach them how to use useful, adaptable thoughts and behaviors to cope with a variety of situations (30). Patients gain insight into how their thoughts affect their anxiety symptoms during the cognitive portion of therapy. By learning to alter these mental habits, they can reduce the likelihood and severity of anxiety symptoms.
According to the current findings, participants who disclosed their HIV/AIDS status to a third party reported feeling less anxious than those who did not. This finding aligns with a previous study conducted in Zimbabwe, which found that positive disclosure correlates significantly with psychosocial measures (31). HIV disclosure or telling others that you are HIV positive offers many potential benefits. By encouraging partner HIV testing and increasing condom negotiation and use, HIV partner disclosure can reduce the amount of unprotected sexual activity. It can also encourage individuals to disclose their status to partners or others (32, 33). If people stop hiding their illnesses and reach out to those in need, they will eventually receive care.
In this study, compared to individuals without alcohol use disorders, those with alcohol use disorders experienced higher levels of anxiety. This finding is also supported by a previous study, which stated that individuals who used substances had higher anxiety levels (34). The symptoms of anxiety and alcohol use often coincide and overlap (35). Improper use of antiretroviral medication persists even after alcohol consumption. Other mental disorders, such as anxiety, may arise as a direct or indirect result of improper medication use (36). Therefore, alcohol users tend to experience a wider range of anxiety symptoms.
Still this study found that individuals with HIV/AIDS who perceived stigma as strong reported more anxiety symptoms than those who did not. This result is consistent with a previous study (37). HIV/AIDS stigma refers to the negative attitudes, thoughts, and feelings that individuals living with the virus have about themselves as a result of their HIV condition (38). There is a link between mental health issues and the stigma surrounding HIV. When people are concerned about something, they are more likely to experience mental health problems, including anxiety. As a result, the majority of stigmatized HIV/AIDS participants reported experiencing anxiety.
Conclusion
At Gambella General Hospital, two out of every seven people living with HIV (PLWH) reported anxiety symptoms. Multivariable logistic regression analysis revealed that being aged 25 to 40 years, seeing a counselor, HIV disclosure, alcohol use disorders, and perceived high stigma were significantly associated with anxiety in this population. This study highlights the significant prevalence of anxiety among people living with HIV (PLWH), underscoring the critical need for routine anxiety screening in this population. The findings emphasize the importance of further research to better understand the causal relationships between anxiety and other variables in this context. By integrating mental health services into ART clinics, healthcare providers can offer more comprehensive care, addressing both physical and mental health needs. Routine anxiety screening would not only improve early detection but also ensure timely intervention, ultimately enhancing the overall well-being and quality of life for PLWH. This approach could lead to better health outcomes, reduce the burden of mental health issues, and support more holistic, patient-centered care.
Limitation of the study
A limitation of this study is that the sample size was small and drawn from a single general hospital, which may not be representative of the broader population. As a result, the findings may have limited generalizability to other hospitals or healthcare settings, especially those in different geographical areas or with differing patient demographics. Therefore, the conclusions drawn from this study may not fully apply to populations outside the specific context of the study’s location or to the general population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The Mattu University Institutional Research Ethics Review Committee granted ethics approval. Next, the College of Health Sciences provided the authorization letter. Participation was completely voluntary, with no economic or other motivation, and each participant has signed written informed consent for their participation.
Author contributions
ZA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WB: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AD: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LW: Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation. MH: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. GT: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YW: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WG: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MH: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BT: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SH: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Mattu University and Gambella General Hospital for giving us the opportunity. We are also grateful to our study participants, data collectors/supervisors, and heads of departments for their great contribution and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ART, antiretroviral therapy; ARV, antiretroviral; AUDIT, Alcohol Use Disorder Identification Test; BAI, Beck Anxiety Inventory scale; CI, confidence interval; FTND, Fagerstrom Test for Nicotine Dependence; HIV, human immunodeficiency virus; HIV/AIDS, human immunodeficiency virus/acquired immunodeficiency syndrome; km, kilometer; PLWH, persons living with HIV/AIDS; SDS, Severity of Dependence Scale; US, United States; WHO, World Health Organization.
References
1. Rezaei S, Ahmadi S, Rahmati J, Hosseinifard H, Dehnad A, Aryankhesal A, et al. Global prevalence of depression in HIV/AIDS: a systematic review and meta-analysis. BMJ Support Palliat Care. (2019) 9:404–12. doi: 10.1136/bmjspcare-2019-001952
2. HIV Mental Health Treatment Issues (2012). Available online at: https://www.psychiatry.org/FileLibrary/Psychiatrists/Practice/Professional-Topics/HIV-Psychiatry/FactSheet-Anxiety-2012.pdf (Accessed January 19, 2023).
3. Van Den Heuvel L, Chishinga N, Kinyanda E, Weiss H, Patel V, Ayles H, et al. Frequency and correlates of anxiety and mood disorders among TB- and HIV-infected Zambians. AIDS Care Psychol Socio-Medical Asp AIDS/HIV. (2013) 25:1527–35. doi: 10.1080/09540121.2013.793263
4. Brown MJ, Cohen SA, DeShazo JP. Psychopathology and HIV diagnosis among older adults in the United States: disparities by age, sex, and race/ethnicity. Aging Ment Heal. (2020) 24:1746–53. doi: 10.1080/13607863.2019.1636201
5. Liu X, Wang H, Zhu Z, Zhang L, Cao J, Zhang L, et al. Exploring bridge symptoms in HIV-positive people with comorbid depressive and anxiety disorders. BMC Psychiatry. (2022) 22:1–10. doi: 10.1186/s12888-022-04088-7
6.. Epidemiological fact sheet HIV, HIV statistics, globally and by WHO region, 2023. Switzerland: WHO (2023). Available at: https://cdn.who.int/media/docs/default-source/hq-hiv-hepatitis-and-stis-library/j0294-who-hiv-epi-factsheet-v7.pdf (Accessed January 30, 2023).
7. WHO, CDC. UPDATE/ETHIOPIA HIV/AIDS Progress in 2014 . Available online at: https://www.afro.who.int/sites/default/files/2017-05/Ethiopia_update-sheet-on-hiv—aids-programme_2014_final.pdf (Accessed January 27, 2023).
8. Brandt C, Zvolensky MJ, Woods SP, Gonzalez A, Safren SA, O’Cleirigh CM. Anxiety symptoms and disorders among adults living with HIV and AIDS: A critical review and integrative synthesis of the empirical literature. Clin Psychol Rev. (2017) 51:164–84. doi: 10.1016/j.cpr.2016.11.005
9. Pence BW, Miller WC, Gaynes BN, Eron JJ. Psychiatric illness and virologic response in patients initiating highly active antiretroviral therapy. J Acquir Immune Defic Syndr. (2007) 44:159–66. doi: 10.1097/QAI.0b013e31802c2f51
10. Cook JA, Burke-Miller JK, Steigman PJ, Schwartz RM, Hessol NA, Milam J, et al. Prevalence, comorbidity, and correlates of psychiatric and substance use disorders and associations with HIV risk behaviors in a multisite cohort of women living with HIV. AIDS Behav. (2018) 22:3141–54. doi: 10.1007/s10461-018-2051-3
11. Sherbourne CD, Hays RD, Fleishman JA, Vitiello B, Magruder KM, Bing EG, et al. Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. Am J Psychiatry. (2000) 157:248–54. doi: 10.1176/appi.ajp.157.2.248
12. Rothbard AB, Miller K, Lee S, Blank M. Revised cost estimates of medicaid recipients with serious mental illness and HIV-AIDS. Psychiatr Serv. (2009) 60:974–7. doi: 10.1176/ps.2009.60.7.974
13. Keiser O, Spoerri A, Brinkhof M, Hasse B, Gayet-Ageron A, Tissot F, et al. Suicide in HIV-Infected individuals and the General population in Switzerland, 1988-2008. Am J Psychiatry. (2010) 167:143–50. doi: 10.1176/appi.ajp.2009.09050651
14. Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: Longitudinal analysis from the HIV epidemiology research study. J Am Med Assoc. (2001) 285:1466–74. doi: 10.1001/jama.285.11.1466
15. Godfrey C, Nkengasong J. Prioritizing mental health in the HIV/AIDS response in africa. N Engl J Med. (2023) 389(7):581–3. doi: 10.1056/NEJMp2305399
16. Kechine T, Ali T. Anxiety and associated factors among clients on highly active antiretroviral therapy (HAART) in public hospitals of southern Ethiopia: A multi-center cross-sectional study. Psychol Res Behav Manag. (2022) 15:3889–900. doi: 10.2147/PRBM.S385630
17. Beck AT, Brown G, Epstein N, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. (1988) 56:893–7. doi: 10.1037/0022-006X.56.6.893
18. Reinius M, Wettergren L, Wiklander M, Svedhem V, Ekström AM, Eriksson LE. Development of a 12-item short version of the HIV stigma scale. Health Qual Life Outcomes. (2017) 15:1–9. doi: 10.1186/s12955-017-0691-z
19. Klinsophon Bsc T, Phd J, Thaveeratitham P. Reliability of the thai version of the fagerstrom test for nicotine dependence (FTND). J Med Assoc Thai. (2017) 100:1130–4.
20. Kozlowski LT, Frecker RC. The fagerstrom test for nicotine dependence: A revision of the fagerstrom tolerance questionnaire. Br J Addict. (1991) 86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x
21. Kassim S, Islam S, Croucher R. Validity and reliability of a Severity of Dependence Scale for khat (SDS-khat). J Ethnopharmacol. (2010) 132:570–7. doi: 10.1016/j.jep.2010.09.009
22. WHO. The Alcohol Use Disorders Identification Test: Interview Version (2001). Available online at: http://whqlibdoc.who.int/hq/2001/who_msd_msb_01.6a.pdf (Accessed January 27, 2023).
23. Lawford BR, Barnes M, Connor JP, Heslop K, Nyst P, Young RMD. Alcohol use disorders identification test (AUDIT) scores are elevated in antipsychotic-induced hyperprolactinaemia. J Psychopharmachol. Vol. 26. World Health Organization Department of Mental Health and Substance Dependence (2012).
24. Dirriba AB. Prevalence of Anxiety Disorder and Associated Factors among Voluntary Counseling and HIV Testing Clients at Governmental Health Centers in 2017 in Addis Ababa, Ethiopia. Iran J Psychiatry. (2021) 16:389–98. doi: 10.18502/ijps.v16i4.7226
25. Omuojine JP, Nguah SB, Ayisi-Boateng NK, Sarfo FS, Ovbiagele B. Contemporary prevalence and predictors of anxiety among patients living with HIV/AIDS in Ghana. Ghana Med J. (2022) 56:169–75. doi: 10.4314/gmj.v56i3.6
26. Olagunju AT, Adeyemi JD, Erinfolami AR, Ogundipe OA. Factors associated with anxiety disorders among HIV-positive attendees of an HIV clinic in Lagos, Nigeria. Int J STD AIDS. (2012) 23:389–93. doi: 10.1258/ijsa.2011.011200
27. Ji J, Zhang Y, Ma Y, Jia L, Cai M, Li Z, et al. People who living with HIV/AIDS also have a high prevalence of anxiety disorders: a systematic review and meta-analysis. Front Psychiatry. (2024) 15:1–12. doi: 10.3389/fpsyt.2024.1259290
28. Chandalia TA, Patoliya HM. Anxiety among AIDS patients: the role of age, gender and residence. Int J Indian Psychol. (2015) 3:143–50.
29. Sen GA, Ila. Impact of counselling upon anxiety and depression of AIDS patients. J Indian Acad Appl Psychol. (2010) 36:249–54.
30. Lenz AS. Cognitive behavioral therapy for anxiety: application of the F.E.A.R. Model for adults. Behav Psychother. (1986) 14:283–94. https://www.tamucc.edu/education/departments/cnep/texchip/files/2018/materials_20180224/cbt_for_anxiety_manual.pdf.
31. Patel R, Ratner J, Gore-Felton C, Kadzirange G, Woelk G, Katzenstein D. HIV disclosure patterns, predictors, and psychosocial correlates among HIV positive women in Zimbabwe. AIDS Care. (2012) 24:358–68. doi: 10.1080/09540121.2011.608786
32. Pinkerton SD, Galletly CL. Reducing HIV transmission risk by increasing serostatus disclosure: A mathematical modeling analysis. AIDS Behav. (2008) 11:698–705. doi: 10.1007/s10461-006-9187-2
33. King R, Katuntu ÆD, Lifshay ÆJ, Packel ÆL, Batamwita ÆR, Johansson E, et al. Processes and outcomes of HIV serostatus disclosure to sexual partners among people living with HIV in Uganda. AIDS Behav. (2008) 12:232–43. doi: 10.1007/s10461-007-9307-7
34. Chen W, Shiu C, Yang JP, Li CR, Wang K, Zhang L, et al. Substance use, anxiety, and self-management efficacy in HIV-positive individuals: A mediation analysis. J Subst Use. (2018) 00:1–7. doi: 10.1080/14659891.2018.1436603
35. Sabourin BC, Stewart SH. Alcohol use and anxiety disorders. Anxiety Heal Behav Phys Illn. (2008), 28–55. http://www.springer.com/978-0-387-74752-1.
36. WHO. Excutive Board 124th Session. Provison agenda item 4.3. HIV AIDS Ment Health: Rep By Secretariat. (2008). https://iris.who.int/handle/10665/2107.
37. Algarin AB, Sheehan DM, Varas-Diaz N, Fennie K, Zhou Z, Spencer EC, et al. Enacted HIV-related stigma’s association with anxiety & Depression among people living with HIV (PLWH) in Florida. AIDS Behav. (2021) 25:93–103. doi: 10.1007/s10461-020-02948-5
Keywords: anxiety, Gambella General Hospital, PLWH, Ethiopia, Mattu University
Citation: Abdu Z, Belayneh W, Dule A, Alemu SS, Wedajo LF, Hajure M, Tesfaye GM, Workneh YA, Gezimu W, Adem Hussen M, Tefera B and Habib S (2025) Adult HIV/AIDS patients are more likely to experience anxiety symptoms. Front. Psychiatry 16:1507020. doi: 10.3389/fpsyt.2025.1507020
Received: 06 October 2024; Accepted: 03 January 2025;
Published: 29 January 2025.
Edited by:
Vsevolod Konstantinov, Penza State University, RussiaReviewed by:
Vincent James Hooper, SPJ GLOBAL, United Arab EmiratesAmelia Dias Teixeira, Federal University of Rio Grande do Sul, Brazil
Copyright © 2025 Abdu, Belayneh, Dule, Alemu, Wedajo, Hajure, Tesfaye, Workneh, Gezimu, Adem Hussen, Tefera and Habib. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zakir Abdu, emFraXJhYmR1NDVAZ21haWwuY29t
 Zakir Abdu
Zakir Abdu Wondwossen Belayneh2
Wondwossen Belayneh2 Aman Dule
Aman Dule Solomon Seyife Alemu
Solomon Seyife Alemu Lema Fikadu Wedajo
Lema Fikadu Wedajo Mohammedamin Hajure
Mohammedamin Hajure Yadeta Alemayehu Workneh
Yadeta Alemayehu Workneh Wubishet Gezimu
Wubishet Gezimu Mustefa Adem Hussen
Mustefa Adem Hussen Bilisumamulifna Tefera
Bilisumamulifna Tefera