- 1Faculty of Nursing, Naval Medical University, Shanghai, China
- 2School of Health Management, Southern Medical University, Guangzhou, Guangdong, China
- 3Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Background: Maintenance hemodialysis (MHD) patients face substantial psychological challenges that impacting their overall quality of life. Flourishing, a concept within positive psychology, refers to a state of mental well-being and personal growth. Despite its importance, the factors influencing flourishing in MHD patients remain underexplored.
Aim: This cross-sectional study aimed to assess flourishing levels among MHD patients in Shanghai, China, and identify sociodemographic, disease-related, and psychological factors associated with flourishing, with implications for targeted interventions.
Method: From October to November 2022, 376 MHD patients across four hospitals completed validated scales measuring flourishing (PERMA Profiler), personality traits (TIPI-C), regulatory emotional self-efficacy (RES), perceived social support (PSSS), and quality of life (EQ-5D). Statistical analyses, including regression analysis, were used to identify factors associated with flourishing.
Results: The mean flourishing score was 6.28 ± 1.763, indicating moderate levels compared to general populations. Full-time employment (β = 0.749, p = 0.033), retirement (β = 0.675, p = 0.043), social support from friends/others (β = 0.039, p < 0.001), conscientiousness (β = 0.133, p < 0.001), and better quality of life (β = 1.281, p = 0.001) emerged as significant positive predictors. Conversely, longer dialysis duration (ρ = -0.135, p = 0.009) and higher perceived disease impact (β = -0.084, p = 0.268) were negatively associated with flourishing.
Conclusions: The findings highlight the complex interplay between sociodemographic, disease-related, and psychological factors in influencing the flourishing of MHD patients. The level of flourishing in MHD patients’ needs to be improved. Developing targeted interventions based on these relevant factors improves quality of life and thus contributes significantly to the well-being of MHD patients.
1 Introduction
Chronic kidney disease (CKD) is a global public health crisis, with over 553,000 patients in China relying on maintenance hemodialysis (MHD) for survival (1). While MHD sustains life, its physical, psychological, and socioeconomic burdens—including thrice-weekly treatments, dietary restrictions, employment disruptions, and financial strain—profoundly diminish patients’ quality of life (QoL) (2, 3). Consequently, MHD patients exhibit elevated rates of anxiety, depression, and social isolation (2, 4–6), underscoring the urgent need to shift from mere survival to holistic well-being.
Flourishing, defined as a state of optimal mental health characterized by positive emotions, purposeful engagement, and fulfilling relationships (7), has become as a critical target in chronic disease management. Grounded in Seligman’s PERMA framework (Positive emotion, Engagement, Relationships, Meaning, Accomplishment) (8), flourishing transcends the absence of pathology by emphasizing resilience and growth. Recent work by VanderWeele (9, 10) and House et al. (11) highlights its relevance in healthcare, particularly for populations navigating lifelong treatments like MHD. For these patients, flourishing may mitigate treatment-related distress and enhance adaptive coping (12). However, despite its theoretical promise, empirical data on flourishing in MHD patients remain scarce.
Personality traits, which are stable psychological characteristics, influence all aspects of patient behavior and are challenging to alter (13, 14). The Big Five Theory of Personality categorizes human personality traits into five dimensions: Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness (15). Previous studies have shown that flourishing is correlated with personality traits. Flourishing is significantly positively correlated with Conscientiousness, Agreeableness, Extraversion, and Openness, while it is significantly negatively correlated with Neuroticism (16). Understanding the personality traits of MHD patients may provide a foundation for personalized interventions aimed at enhancing their well-being.
Regulatory emotional self-efficacy (RES), defined as an individual’s confidence in managing emotional states, and consists perceived self-efficacy in managing anger/irritation (ANG), despondency/distress (DES), and positive affect (POS) (17). Under the dual pressure of physical and psychological stress imposed by their condition, MHD patients are prone to negative emotions such as anxiety and fear (18). RES plays a crucial role in shaping negative emotions (anger, depression and anxiety) and prosocial aggressive behavior (19). Related studies have shown that regulatory emotional self-efficacy is conducive to individuals experiencing more positive emotions, and individuals are prone to positive social interaction experiences (20). However, the relationship between RES and flourishing remains unclear and needs to be further explored.
Social support refers to the emotional and material assistance that an individual receives from social relationships, including family members, friends, significant others, and various organizations (21). MHD patients need to receive lifelong treatment, and social support is indispensable. Given the extensive impact of CKD on all aspects of life, social support from family, friends, and other significant individuals can help patients better adapt to their condition and self-management (22). Investigating the effects of different types of social support on flourishing can provide valuable insights into the needs of MHD patients and inform the development of targeted interventions.
As a relatively new and important construct in positive psychology, flourishing merits significant attention. The study aimed to assess flourishing levels among MHD patients in Shanghai, China, and identify sociodemographic, disease-related, and psychological factors associated with flourishing, with implications for targeted interventions. The present study proposed the following hypotheses:
H1: Sociodemographic factors (education, employment, marital status) are positively associated with flourishing.
H2: Disease-related factors (dialysis duration, perceived disease impact, quality of life) are associated with flourishing.
H3: Psychological factors (regulatory emotional self-efficacy, social support, personality traits) are positively associated with flourishing, except for neuroticism, which is negatively associated.
2 Methods
2.1 Procedure and ethics
This study was designed as a cross-sectional, multi-center investigation. Data collection occurred between October 1st and November 30th, 2022, targeting maintenance hemodialysis (MHD) patients from four hospitals in Shanghai. Participants were invited to complete a paper-based questionnaire, either independently or with the assistance from researchers during dialysis sessions. The study adhered to all relevant guidelines, regulations, and the principles of Declaration of Helsinki. Ethical approval was granted by the Committee on Ethics of Medicine, Naval Medical University. Informed consent was obtained from each participant, and when necessary, from their legal guardian. To ensure patient privacy and anonymity, no identifying information, including photographs, was collected. Participation was voluntary, with no monetary or material incentives provided.
2.2 Participants and sample
A convenience sampling method was employed to recruit participants, with specific eligibility criteria established. Inclusion criteria included individuals diagnosed with End-Stage Renal Disease (ESRD) according to the International Classification of Diseases (ICD-10), aged 18 years or older, who had been undergoing hemodialysis for a minimum of three months, possessed no perception disorders or communication problems, and were willing to provide informed consent. Exclusion criteria encompassed individuals who had undergone major surgery, suffered from severe psychiatric disorders (Schizophrenia, Bipolar Disorder, Schizoaffective Disorder, Persistent Delusional Disorder, Mental Disorders due to Epilepsy, Mental Retardation with Associated Mental Disorders), severe heart, liver, or respiratory failure, or malignant tumors. A power analysis using G*Power 3.1 was conducted to determine the target sample size required to detect effects in the planned analyses. For multiple linear regression with 19 predictor variables, an alpha of 0.05, and a power of 0.80, the recommended sample size was 133 participants. The obtained sample of 376 individuals exceeded this threshold, ensuring sufficient statistical power.
2.3 Measures
2.3.1 Sociodemographic characteristics questionnaire
The demographic questionnaire that was developed by the researchers contained questions on sociodemographic and disease-related characteristics of the patients such as gender, age, education, marital status, primary caregiver, employment, dialysis duration, presence of a co-morbid disease, kidney transplant experience, self-perceived degree of knowledge of disease-related information, self-perceived burden of medical expenses for disease, self-perceived degree of impact of disease on life.
2.3.2 PERMA profiler of Chinese version
The PERMA scale is a 23-item measure of flourishing developed by Kern et al. (8). Widely utilized in the United States, Australia, Korea, Japan, and other global populations, it has been adapted by our research group into a Chinese version, demonstrating commendable reliability (8, 23–26). The scale encompasses 15 items measure PERMA (Positive emotions, Engagement, Relationships, Meaning and Accomplishments). There are additional three item subscales examine Overall Happiness, Loneliness, Physical Health and Negative Emotion. Each item is rated on a Likert-type scale ranging from 0 to 10. Dimension scores were calculated as the average score of the corresponding items. The flourishing score is derived from adding the PERMA Total to the Overall Happiness item. The research team translated the PERMA scale into Chinese and conducted an exploratory factor analysis on the survey results from 376 samples. The Chinese version retained all original items and factor analysis identified two dimensions: Positive experience and Self-accomplishment. The original subdomains of Positive emotions and Relationships were consolidated into a unified “positive experience” dimension, while Engagement, Meaning, and Accomplishment were combined to form a “Self-accomplishment” dimension. The two dimensions obtained by EFA were used for model fitting, and the results of model fitting indices showed χ2/df=3.234, RMSEA=0.095, GFI=0.858, CFI=0.894, IFI=0.895, and TLI=0.875. The Cronbach’s α of the scale in this study was 0.895 (95% CI [0.879, 0.910]).
2.3.3 Ten-item personality inventory in China
The Ten-Item Personality Inventory in China (TIPI-C), developed by Gosling et al. (27), serves as a tool to assess Big-Five personality traits. Jinde Li translated the TIPI into the Chinese version (28). Comprising 10 items distributed across five dimensions (E-Extroversion, A-Agreeableness, C-Conscientiousness, ES-Emotional Stability and O-Openness), the TIPI utilizes two items for each Big-Five personality dimension. Notably, items 2, 4, 6, 8, and 10 should be reverse-coded when computing the dimension score. Responses were recorded on a Likert scale ranging from 1 to 7 (1=strongly disagree, 7=strongly agree), with higher scores indicating a greater expression of the respective trait. The Cronbach’s α of the scale in this study was 0.6439 (95%CI [0.608, 0.678]). CFA proved that the goodness-of-fit indicators were acceptable (28).
2.3.4 Regulatory emotional self-efficacy scale
The Regulatory Emotional Self-Efficacy Scale (RES), initially designed by Caprara et al. and later revised by Yu Guoliang et al. (29), comprises a total of 12 questions distributed across three dimensions: Perceived self-efficacy in expressing positive affect (POS, 4 items), Perceived self-efficacy in managing despondency (DES, 5 items), and Perceived self-efficacy in managing anger (ANG, 3 items). Respondents provide ratings for each item on a 5-point Likert scale, ranging from 1 to 5. A higher score indicates a higher level of regulatory emotional self-efficacy exhibited by the investigator. The Cronbach’s α of the scale in this study was 0.872 (95% CI [0.850, 0.894]). Goodness-of-fit indicators were within acceptable levels (29).
2.3.5 Perceived social support scale
The Perceived Social Support Scale (PSSS) was employed to assess an individual’s perceived social support (30). Each participant’s responses were evaluated using a 12-item scale, comprising two subscales: family support (4 items) and friends and important others support (8 items). Participants provided responses to each item on a 7-point Likert scale. The scores of items within each dimension were aggregated, with higher scores indicating a greater perception of social support. The Cronbach’s α of the scale in this study was 0.875 (95%CI [0.853, 0.897]). Fit measures fell within the range of acceptability (30).
2.3.6 EuroQol five-dimensional questionnaire
The EuroQol five-dimensional questionnaire (EQ-5D), a globally recognized patient-reported outcome instrument renowned for its succinct and lucid items, is widely employed for health measurement and valuation due to its effective assessment capabilities. It has also become a commonplace tool for evaluating the quality of life among patients grappling with chronic kidney disease (31). The EQ-5D comprises two parts: a multidimensional health classification system and a visual analog assessment system. For this study, only the Multidimensional Health Classification System was utilized for assessment, considering the potential impact of personal researcher perception on the scoring values. The EQ-5D evaluates health across five dimensions—mobility (MOB), self-care (SC), usual activities (UA), pain/discomfort (PA), and anxiety/depression (MOOD)—with three severity levels in each dimension. It has established a corresponding utility value point system in China (1=no problems, 2=some/moderate problems, 3=extreme problems/unable) (32). The Cronbach’s α of the scale in this study was 0.766 (95%CI [0.735, 0.797]).
2.4 Statistical analysis
All statistical analyses were conducted using IBM SPSS 27.0. Data were initially entered into EpiData 3.0 to ensure accuracy and minimize entry errors, after which the dataset was imported into SPSS for further analysis. Descriptive statistics, including frequency distributions, means, and standard deviations (SD), were used to summarize participants’ sociodemographic and clinical characteristics.
Univariate analyses were performed to assess associations between flourishing scores and independent variables. For dichotomous variables, independent samples t-tests were applied when normality (assessed by the Shapiro-Wilk test) and homogeneity of variance (verified by Levene’s test) assumptions were satisfied; otherwise, the non-parametric Mann-Whitney U test was used. For multinomial categorical variables, one-way ANOVA was utilized when data met normality and equal variance requirements, while the Kruskal-Wallis H test was adopted as the non-parametric alternative when these assumptions were violated. Pearson correlation coefficients were calculated to assess linear relationships between continuous variables with normal distribution and homoscedasticity, whereas Spearman’s rank correlation coefficients were computed for variables violating these parametric assumptions.
A stratified stepwise regression model was constructed. Independent variables were grouped into three blocks: sociodemographic variables (e.g., education, marital status, employment), disease-related variables (e.g., dialysis duration, comorbidities, perceived disease impact), and psychological variables (e.g., personality traits, regulatory emotional self-efficacy, social support). Blocks 1 and 2 were entered using the enter method, while Block 3 was analyzed using stepwise selection (entry criteria: p < 0.05; removal criteria: p > 0.10). Effect sizes were calculated using Cohen’s f² for regression models, partial η² for ANOVA, and Cohen’s d or r for t-tests and correlations (33). The significance level was set at α = 0.05 (two-tailed).
3 Results
3.1 Participant’ s sociodemographic and disease-related characteristics
A total of 406 questionnaires were collected, of which 376 were deemed valid, resulting in a questionnaire validity rate of 92.61%. Among the 376 participants, the mean age was 58 ± 13.403 years, with an age range from 22 to 97 years. The mean duration of dialysis was 7 ± 6.601 years, with a range from 4 months to 34 years. Thirty of them (8.0%) had undergone renal transplantation. The number of patients surveyed with chronic diseases other than chronic kidney disease was 80.6% (203). The rest of the information is shown in Table 1.
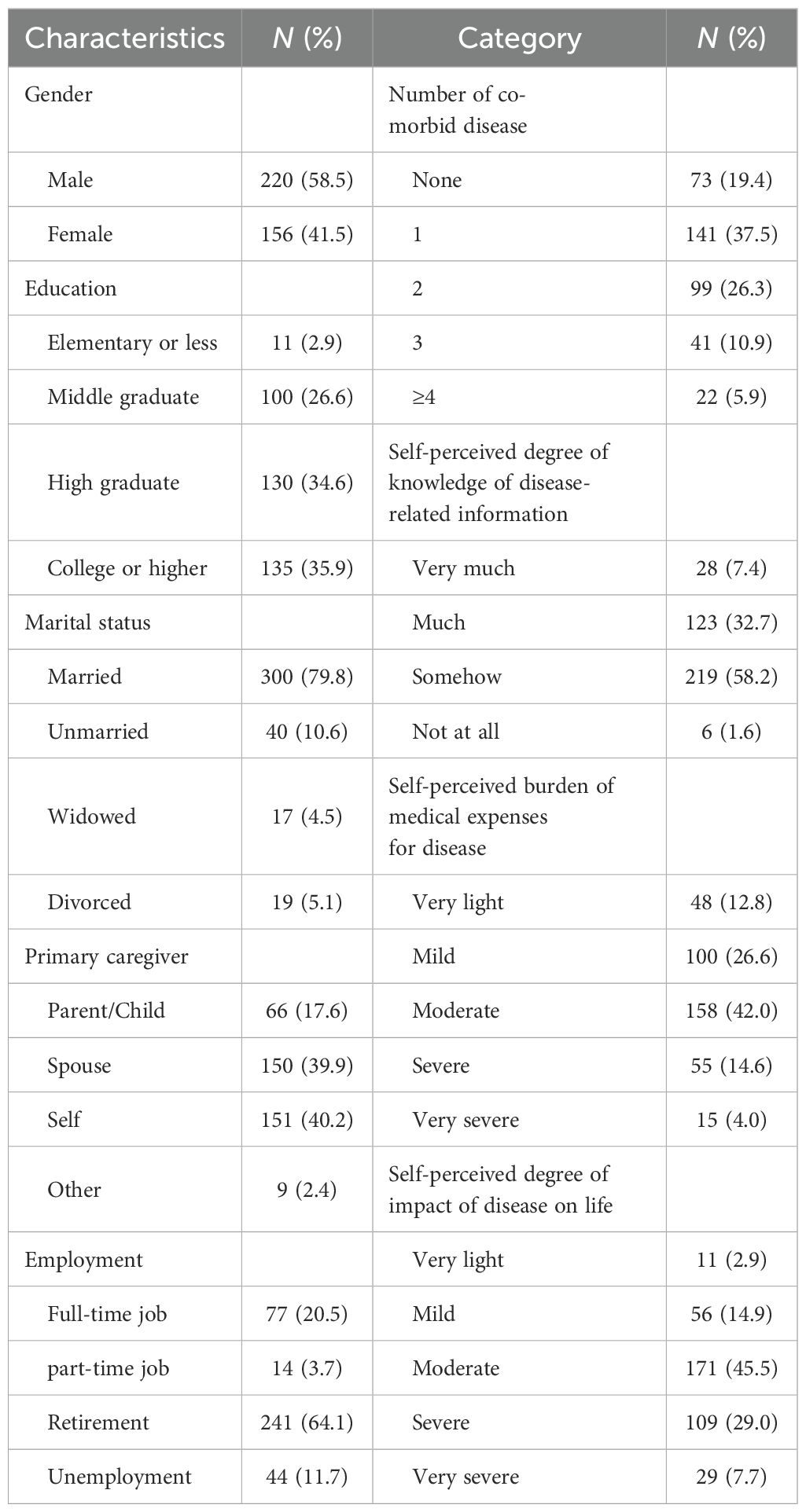
Table 1. Descriptive statistics for sociodemographic and clinical characteristics of participants (n=376).
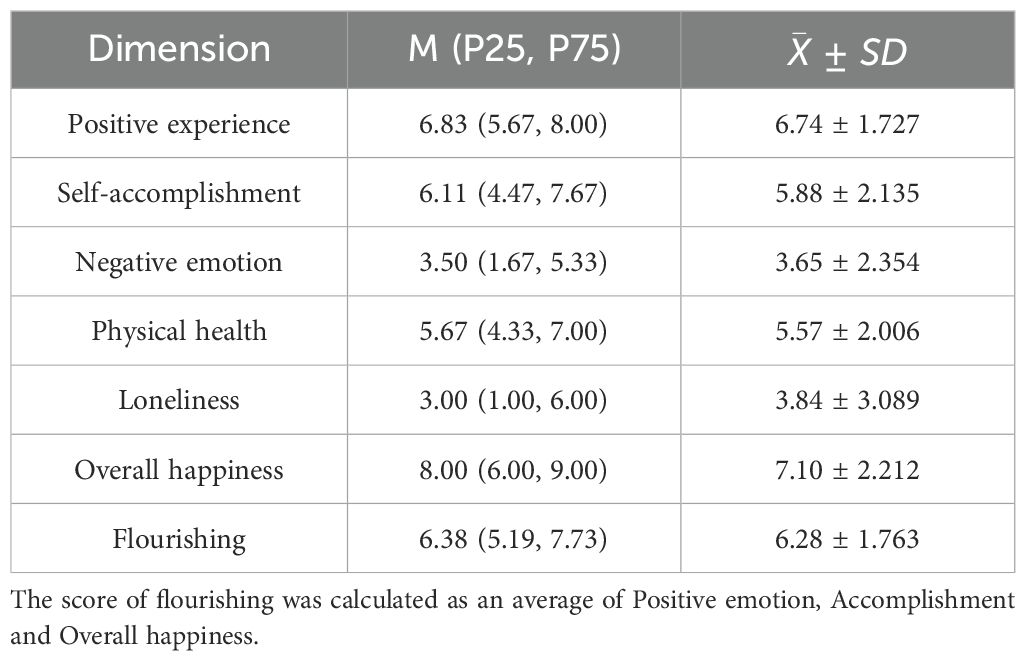
3.2 Flourishing levels in maintenance hemodialysis patients
The mean flourishing score was 6.28 ± 1.763 (scale range: 0–10), indicating moderate levels compared to general population (typically >7.0) (8). The result suggest there remains substantial potential for enhancing mental health outcomes within this surveyed population. Among PERMA dimensions, positive experience scored highest (6.74 ± 1.727), while self-accomplishment was the lowest (5.88 ± 2.135). Negative emotion and loneliness scores were 3.65 ± 2.354 and 3.84 ± 3.089, respectively, reflecting significant psychological distress. Table 2 summarizes PERMA-Profiler scores.
3.3 Sociodemographic and disease-related characteristics associated with flourishing
Flourishing scores varied significantly across sociodemographic and disease-related factors. The level of flourishing exhibited variations based on factors such as education, marital status, employment, dialysis duration, the presence of co-morbid diseases, the degree of knowledge regarding disease-related information, the financial burden of medical expenses, and the impact of the disease on life. Notably, dialysis duration demonstrated a significant negative correlation with the level of flourishing (ρ=-0.135, P=0.009) Table 3 presents the descriptive information for participant’s sociodemographic and disease-related characteristics by score of flourishing.
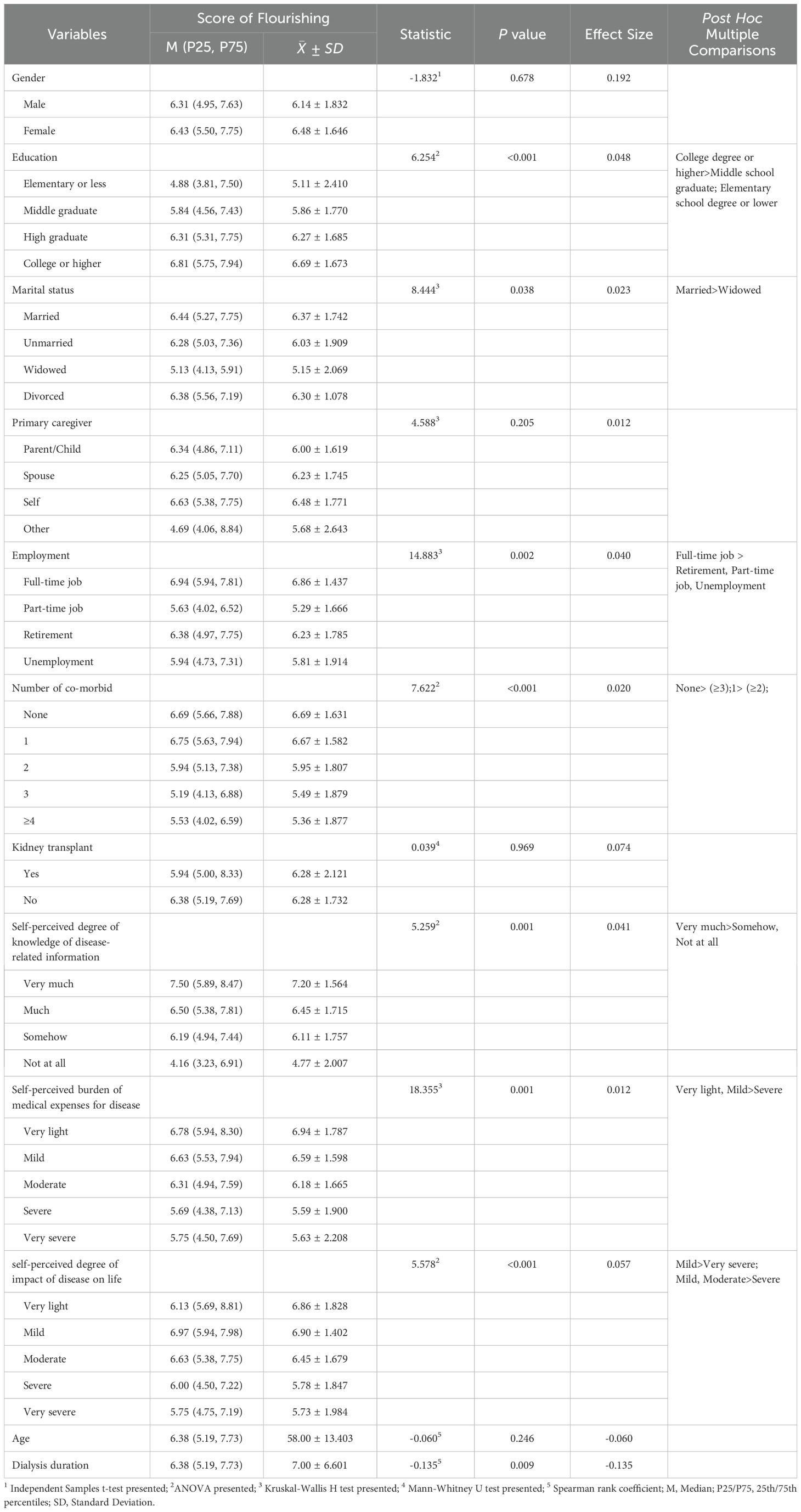
Table 3. Descriptive information for participant’s sociodemographic and disease-related characteristics by score of flourishing.
3.4 Correlation analysis of flourishing and personality traits, regulatory emotional self-efficacy, social support and quality of life
Spearman’s rank correlation (ρ) was used due to non-normality. Spearman’s correlation analysis revealed significant associations between flourishing levels and psychological variables (see Figure 1). All five traits (Extraversion, Agreeableness, Conscientiousness, Emotional Stability, Openness) showed positive correlations (ρ= 0.27–0.42, p < 0.001). RES total score (ρ = 0.58, p < 0.001) and its subdimensions (p < 0.05) were strong positive associated to Flourishing. Both family support (p = 0.038) and support from friends/others (p < 0.001) contributed to flourishing.
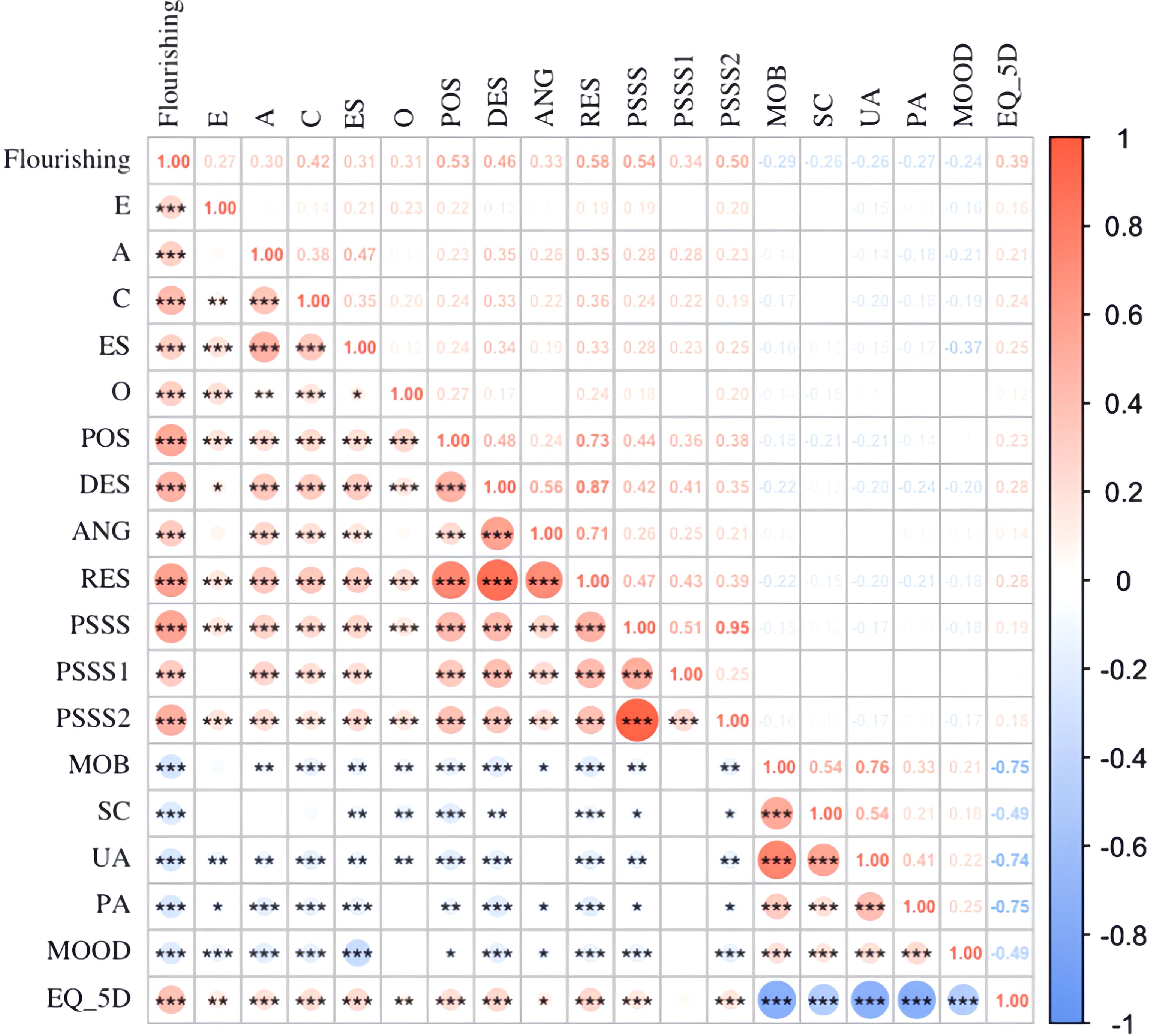
Figure 1. Bivariate correlations of study variable (n=376). E represents extroversion; A represents agreeableness; C represents conscientiousness; ES represents emotional stability; O represents openness; POS represents Perceived self-efficacy in expressing positive affect; DES represents perceived self-efficacy in managing despondency; ANG represents perceived self-efficacy in managing anger; RES represents regulatory emotional self-efficacy; PSSS represents social support; PSSS1 represents family support; PSSS2 represents friends and important others support; MOB represents mobility; SC represents self-care represents; UA represents usual activities; PA represents pain/discomfort; MOOD represents anxiety/depression; EQ_5D represents quality of life.*P<0.05, **P<0.01, ***P<0.001.
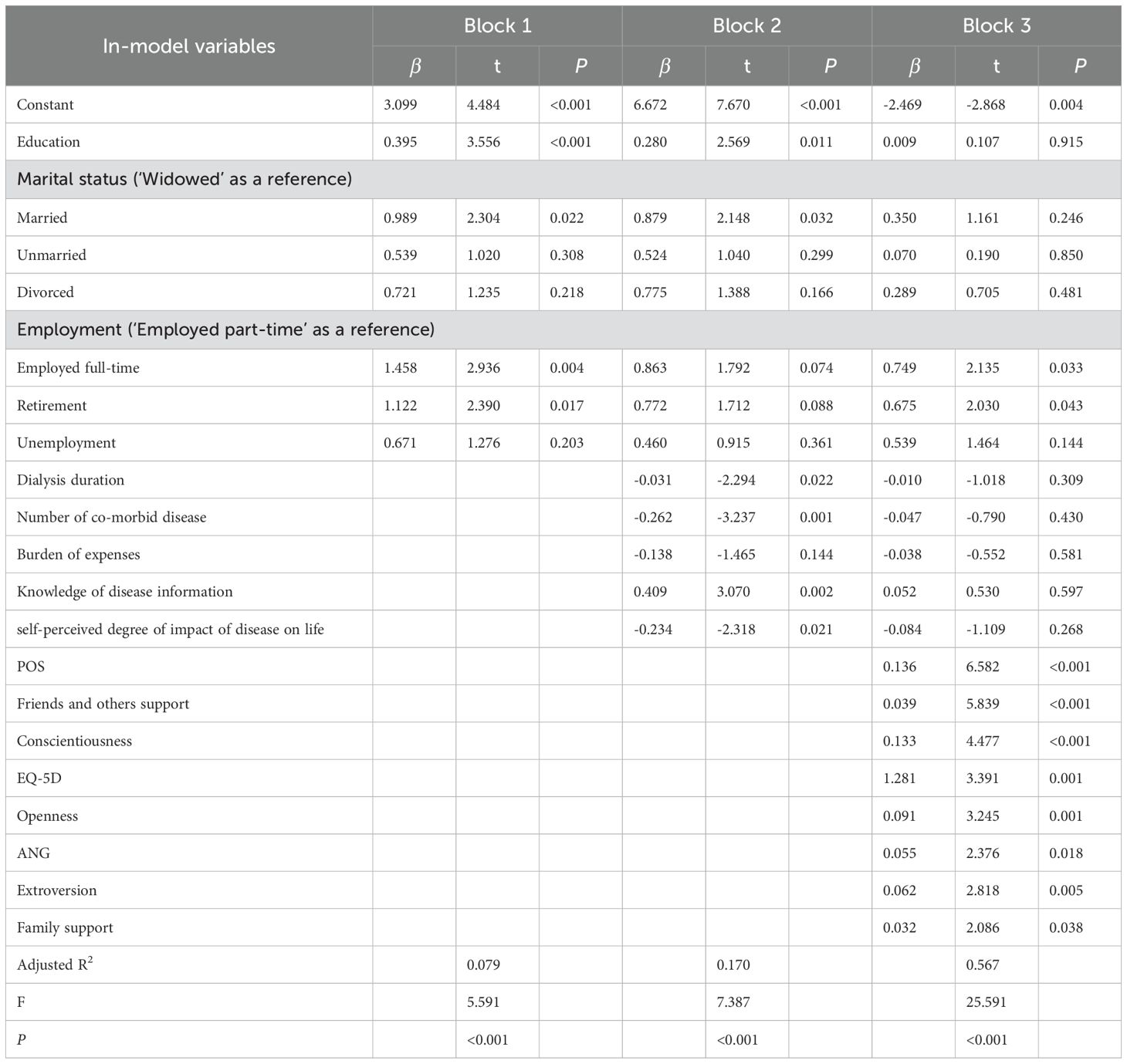
3.5 Regression analysis of flourishing in maintenance hemodialysis patients
Stratified stepwise regression identified 10 variables explaining 56.7% of the variance in flourishing (adjusted R² = 0.567, F = 25.591, p < 0.001), with effect size of f² ≈ 1.31. The Durbin-Watson statistic of the model was 1.721, with the tolerance ranging from 0.140 to 0.883. The detailed results are outlined in Table 4. The variables of Agreeableness (A), Emotional Stability (ES), and Perceived self-efficacy in managing despondency (DES) were ultimately excluded from the final model. The following variables were identified as positive associated with flourishing: employed full-time (β=0.749, P<0.05), retirement (β=0.675, P <0.05), Perceived self-efficacy in expressing positive affect (β=0.137, P <0.001), Friends and others support (β=0.039, P <0.001), Conscientiousness (β=0.133, P <0.001), EQ-5D (β=1.281, P =0.001), Openness (β=0.091, P =0.001), Perceived self-efficacy in managing anger (β=0.055, P <0.05), Extroversion (β=0.062, P <0.05), Family support (β=0.032, P <0.05). Supplementary Table 1 shows the value labels of characteristics.
4 Discussion
4.1 Flourishing of MHD patients needs improvement
This study assessed the level of flourishing among MHD patients using the PERMA framework and explored its influencing factors. The mean flourishing score remains significantly lower than general population norms (>7.0) (8). Notably, the “self-accomplishment” dimension scored lowest, likely reflecting the profound disruption of life goals caused by dialysis schedules and physical limitations. These results underscore that merely sustaining survival is insufficient; enabling patients to thrive requires addressing psychological and social barriers.
Seligman defines subjective well-being in five domains. Positive emotions are an important part of well-being. Research indicates that MHD patients are prone to distress from disease symptoms and anxiety about complications, which negatively impacts their emotional well-being. The physical limitations and social role changes imposed by dialysis may exacerbate negative emotions. (34). Engagement, defined as a deep psychological involvement characterized by intense concentration, is also compromised due to the physical weakness experienced by MHD patients (8). This weakness often hinders daily activities, leaving patients fatigued and may be less engaged in life (35). Relationships are fundamental to life and including social ties, social networks, and received support. MHD patients receive dialysis treatments 2-3 times per week (36), which require patients to travel frequently to and from the hospital, affecting the quality of their socialization and the interpersonal relationships of MHD patients. The “meaning” aspect, which involves having a sense of purpose and feeling that one’s life is valuable, is particularly affected in MHD patients due to the lifelong nature of treatment. The numerous restrictions imposed by dialysis, such as dietary limitations, reduced ability to travel, and fatigue at work, could lead to a diminished sense of life’s meaning (37). The “accomplishment” aspect scored lowest, likely reflecting the profound disruption of life goals caused by dialysis schedules and physical limitations (38).
4.2 Factors influencing flourishing in MHD patients
4.2.1 Sociodemographic factors
The study found that several sociodemographic factors influence the flourishing among MHD patients, supporting Hypothesis 1 (H1). Higher education levels and a greater understanding of disease-related information were associated with higher levels of flourishing, consistent with previous research findings (39, 40). Patients with higher education tend to have better self-regulation skills, which contributes to improved quality of life and mental health (41). The study’s findings suggest that intimate relationships stemming from marriage, stable employment status positively influence the flourishing of MHD patients. Previous research has indicated that MHD patients with a partner feel more cared for and supported, and a stable and warm intimate relationship promotes their mental health (42). Employment status emerged as the sole sociodemographic variable entering the hierarchical linear regression equation in this study. Univariate analysis results further highlight that MHD patients with full-time employment exhibit the highest level of flourishing. Despite the impact of MHD on their daily lives, individuals with full-time jobs can still engage in work activities, derive a sense of value from completing tasks, and thereby bolster their mental health (43).
4.2.2 Disease-related factors
The duration of MHD treatment, the perceived impact of the disease on life, and the financial burden of medical expenses were all found to be negatively associated with flourishing, supporting Hypothesis 2 (H2). These findings align with existing literature, which suggests that prolonged dialysis leads to weakened physiological functions, decreased immunity, and an increased burden of chronic diseases, all of which negatively impact quality of life and flourishing (44). With the prolonged duration of MHD, patients experience weakened physiological functions, decreased immunity, increased chronic diseases, and a heightened impact on their daily lives (45). Consequently, the quality of life is further compromised, adversely affecting the level of flourishing. Existing studies corroborate the significant impact of patients’ quality of life on mental health, particularly in MHD patients who often contend with elevated levels of depression and anxiety due to the influence of the disease and its treatment (46, 47). The long-term treatment regimen places greater economic and life pressure on MHD patients, may negatively influence their flourishing (48). Regression analysis underscores that quality of life has the most substantial impact on flourishing, highlighting the critical need for interventions aimed at alleviating the burden of disease and improving quality of life.
4.2.3 Psychological factors
Personality traits were found to significantly influence flourishing, with extroversion, conscientiousness, and openness being positively associated with higher flourishing levels. Neuroticism scores were reverse-coded (i.e., higher scores reflect emotional stability), resolving the apparent contradiction. Neuroticism was negatively associated with flourishing. Hypothesis 3 were proved. Personality traits are known to shape daily behaviors and mental health outcomes, with extroverted and conscientious individuals more likely to experience strong mental health (49). The univariate analysis of this study revealed that extroversion among the Big Five personality traits of maintenance hemodialysis patients had a higher correlation with the dimension of positive experience, while conscientiousness and openness had a higher correlation with the dimension of self-accomplishment. Extroversion is characterized by sociability, talkativeness, self-confidence, and preferred emotional expression (50). People receive MHD who are extroverted may experience more positive emotions through social and emotional expression. People with openness are imaginative and creative, eager to try and learn new things, and more likely to adopt new ways of achieving goals (51). Conscientious individuals are organized and prefer to plan, leading to better disease management and goal achievement (52).
Regulatory emotional self-efficacy, the cognitive process by which individuals regulate mood changes in this study, POS and ANG entered the regression equation for the factors associated with flourishing. Zhenghong et al. also showed that regulatory emotional self-efficacy can positively influence well-being (53). Expressing positive emotions is one of the types of disclosure, and individuals who express positive emotions have certain positive tendencies in both explicit and implicit situations and being good at disclosure also plays an important role in the promotion of mental health (54). Patients who can effectively manage their emotions are better equipped to cope with the psychological challenges posed by chronic illness, leading to higher levels of flourishing (55).
Social support was strongly associated with flourishing in all dimensions in this study, further supporting Hypothesis 3 (H3). This implicates that better and broader social relationships are positive affect the level of flourishing, which is in line with the other studies (56, 57). Social support is a major external factor that affects the psychological state and quality of life of patients. Good social support has been shown to predict better emotional states and increase resilience in coping with traumatic events (58, 59). Patients discussing and sharing their feelings with others can receive helpful advice and assistance, which may lead to increased confidence in coping with the illness and ultimately positive emotions (60, 61). Social support provides patients with necessary resources such as emotional, informational, and financial assistance to encourage patients to rethink the meaning of life (62). Therefore, social support has a facilitating effect on flourishing. In this study, family support was more correlated with patients’ flourishing level compared to friends and others support. Family caregivers had the highest percentage of caregivers in this study. The role of family caregivers, who often provide the primary support for MHD patients, was particularly emphasized. They may be burdened by physical, psychological, financial, and time constraints, potentially limiting the support they can provide. (63). Peer support, such as sharing experiences with fellow patients, can offer significant benefits, including information, emotional support, and a sense of community (64), which may enhances quality of life and flourishing.
4.3 Implications for practices
The insights garnered from this study underscore the multifaceted nature of flourishing among MHD patients, highlighting the interplay between sociodemographic, disease-related, and psychological factors. Healthcare professionals can leverage these findings to develop comprehensive interventions aimed at enhancing the well-being of MHD patients.
4.3.1 Educational interventions
Given the positive correlation between knowledge of disease and flourishing, tailored educational programs can be designed to enhance patients’ understanding of their condition. These programs should aim to empower patients with knowledge about disease management, coping strategies, and the importance of adherence to treatment protocols.
4.3.2 Psychological support
The significant impact of personality traits and emotional self-efficacy on flourishing suggests the need for psychological interventions. Cognitive-behavioral therapy (CBT) and resilience training can be integrated into patient care to bolster emotional regulation skills, reduce anxiety and depression, and promote positive affect (65). Griva et al. developed an intervention program known as HED-Start. This program integrates CBT, positive psychology, and self-management strategies to assist new patients in successfully transitioning to the hemodialysis phase (66).
4.3.3 Social support
Facilitating support networks is crucial. Healthcare providers can organize support groups where patients share experiences and coping strategies. Additionally, involving family members in educational sessions can strengthen the support system, ensuring that patients receive comprehensive care both within and outside clinical settings (67).
4.3.4 Holistic care
Adopting a patient-centered care approach that integrates physical, psychological, and social aspects of health can lead to better outcomes. Multidisciplinary teams, including nephrologists, psychologists, social workers, and nutritionists, can collaboratively develop and implement individualized care plans.
5 Conclusion
The study elucidates the complex interrelations among various factors influencing the flourishing of MHD patients. By identifying key predictors such as quality of life, personality traits, regulatory emotional self-efficacy, and social support, healthcare professionals can devise targeted interventions. Emphasizing a holistic approach that addresses educational, psychological, social, and economic dimensions holds promise in enhancing the well-being and quality of life for patients undergoing maintenance hemodialysis.
6 Limitation
While this study offers valuable insights into flourishing among maintenance hemodialysis (MHD) patients, several limitations warrant attention. First, the cross-sectional design inherently precludes causal inferences, necessitating future longitudinal investigations to elucidate the temporal dynamics of flourishing and its predictors among MHD patients. Second, the reliance on non-random sampling methods may constrain the generalizability of the findings, suggesting a need for broader, randomized recruitment strategies in subsequent research. Third, the analytical framework did not incorporate dialysis adequacy indicators (e.g., kt/V), which limits the ability to explore associations between biochemical parameters of dialysis quality and clinical or psychosocial outcomes. To address these gaps, future studies should integrate longitudinal data with biochemical markers such as kt/V to refine predictive models and deepen mechanistic understanding. Additionally, complementing subjective measures with objective assessments (e.g., biomarkers, clinician-rated scales) and contextualizing findings within cultural frameworks could enhance the ecological validity and nuance of interpretations. Collectively, these advancements would provide a more holistic perspective on flourishing in MHD patients, bridging gaps between biomedical parameters, psychosocial constructs, and culturally situated care practices.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Committee on Ethics of Medicine, Naval Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
XZ: Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. HY: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. YQL: Investigation, Writing – review & editing. JY: Investigation, Writing – review & editing. YQ: Data curation, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. YG: Investigation, Writing – review & editing. YL: Investigation, Writing – review & editing. LC: Investigation, Writing – review & editing. JW: Conceptualization, Methodology, Writing – review & editing. JC: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1480308/full#supplementary-material
References
1. Thurlow JS, Joshi M, Yan G, Norris KC, Agodoa LY, Yuan CM, et al. Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am J Nephrol. (2021) 52:98–107. doi: 10.1159/000514550
2. Simões ESAC, Miranda AS, Rocha NP, Teixeira AL. Neuropsychiatric disorders in chronic kidney disease. Front Pharmacol. (2019) 10:932. doi: 10.3389/fphar.2019.00932
3. Zazzeroni L, Pasquinelli G, Nanni E, Cremonini V, Rubbi I. Comparison of quality of life in patients undergoing hemodialysis and peritoneal dialysis: a systematic review and meta-analysis. Kidney Blood Press Res. (2017) 42:717–27. doi: 10.1159/000484115
4. Chan KM, Cheung CY, Chan YH, Chan HW, Chak WL, Chau KF. Prevalence and impact of anxiety and depression in Chinese peritoneal dialysis patients: A single centre study. Nephrol (Carlton). (2018) 23:155–61. doi: 10.1111/nep.12970
5. Gadia P, Awasthi A, Jain S, Koolwal GD. Depression and anxiety in patients of chronic kidney disease undergoing haemodialysis: A study from western Rajasthan. J Family Med Prim Care. (2020) 9:4282–6. doi: 10.4103/jfmpc.jfmpc_840_20
6. Musa AS, Pevalin DJ, Al Khalaileh MAA. Spiritual well-being, depression, and stress among hemodialysis patients in Jordan. J Holist Nurs. (2018) 36:354–65. doi: 10.1177/0898010117736686
7. Seligman MEP. Positive psychology: A personal history. Annu Rev Clin Psychol. (2019) 15:1–23. doi: 10.1146/annurev-clinpsy-050718-095653
8. Butler J, Kern ML. The PERMA-Profiler: A brief multidimensional measure of flourishing. Int J Wellbeing. (2016) 6:1–48. doi: 10.5502/ijw.v6i3.526
9. VanderWeele TJ. On the promotion of human flourishing. Proc Natl Acad Sci U S A. (2017) 114:8148–56. doi: 10.1073/pnas.1702996114
10. VanderWeele TJ, McNeely E, Koh HK. Reimagining health-flourishing. JAMA. (2019) 321:1667–8. doi: 10.1001/jama.2019.3035
11. House TR, Wightman A. Enabling flourishing: novel approaches in palliative medicine for children with advanced kidney disease. Curr Opin Nephrol Hypertension. (2023) 32:41–8. doi: 10.1097/mnh.0000000000000839
12. Edgar A, Pattison S. Flourishing in health care. Health Care Anal. (2016) 24:161–73. doi: 10.1007/s10728-016-0315-5
13. Sutin AR, Zonderman AB, Ferrucci L, Terracciano A. Personality traits and chronic disease: implications for adult personality development. J Gerontol B Psychol Sci Soc Sci. (2013) 68:912–20. doi: 10.1093/geronb/gbt036
14. Weixi K, François ES, Sònia P, Kaya W, Antonio M. Personality traits and dimensions of mental health. Sci Rep. (2023) 13(1):7091. doi: 10.1038/s41598-023-33996-1
15. Oliver PJ, Sanjay S. Five Trait taxonomy: History, measurement, and theoretical perspectives. In Pervin L. A., John O. P. (Eds.), Handbook of personality: Theory and research 2nd ed. Guilford Press. pp. 102–138.
16. Zhang Y, Yang Y. Psychometric evaluation of the Chinese flourishing scale in college students and its associations with personality traits. Modern Communication. (2018), 168–9. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=14CuGbpFC1DWM5X9RFYaMAESPElUvZdVN1_C0mttZsSo-BpsT5XakMM5qZg8y2XiOVPw6htx24eTHqphpaUNtBYUpoT4pVGemV2rSrdxLSP4EY47qaxXqt3VNSeiTqXIxkgMBSsKh5UiLU9pZpDkZG-e3CZOF0AgXGOgKmRAEEZTl2fFWZfM7MFEJB8EcDO2b4MVgqDazSw=&uniplatform=NZKPT&language=CHS (Accessed March 7, 2025).
17. Caprara GV, Di Giunta L, Eisenberg N, Gerbino M, Pastorelli C, Tramontano C. Assessing regulatory emotional self-efficacy in three countries. Psychol Assess. (2008) 20:227–37. doi: 10.1037/1040-3590.20.3.227
18. Liu X, Yang X, Yao L, Zhang Q, Sun D, Zhu X, et al. Prevalence and related factors of depressive symptoms in hemodialysis patients in northern China. BMC Psychiatry. (2017) 17:128. doi: 10.1186/s12888-017-1294-2
19. Mesurado B, Vidal EM, Mestre AL. Negative emotions and behaviour: The role of regulatory emotional self-efficacy. J Adolesc. (2018) 64:62–71. doi: 10.1016/j.adolescence.2018.01.007
20. Lü L, Jiyu Z, Xiaoxi H, Feng H, Xiangping L, Long H, et al. Regulatory emotional self-efficacy and prosocial behavior: A moderated mediation model. SAGE Open. (2023) 2023(1):1–7. doi: 10.1177/21582440231152407
21. Hans OFV. Dimensions of social support: a conceptual framework for research. Soc Psychiatry. (1985) 20:156–62. doi: 10.1007/bf00583293
22. Yuanyuan S, Lin C, Wenxiu W, Dongrui Y, Xiaolian J. Social support, sense of coherence, and self-management among hemodialysis patients. Western J Nurs Res. (2021) 44(4):367–74. doi: 10.1177/0193945921996648
23. Bartholomaeus JD, Iasiello MP, Jarden A, Burke KJ, van Agteren J. Evaluating the psychometric properties of the PERMA profiler. J Well-Being Assess. (2020) 4:163–80. doi: 10.1007/s41543-020-00031-3
24. Choi SP, Suh C, Yang JW, Ye BJ, Lee CK, Son BC, et al. Korean translation and validation of the Workplace Positive emotion, Engagement, Relationships, Meaning, and Accomplishment (PERMA)-Profiler. Ann Occup Environ Med. (2019) 31:e17. doi: 10.35371/aoem.2019.31.e17
25. Umucu E, Wu JR, Sanchez J, Brooks JM, Chiu CY, Tu WM, et al. Psychometric validation of the PERMA-profiler as a well-being measure for student veterans. J Am Coll Health. (2020) 68:271–7. doi: 10.1080/07448481.2018.1546182
26. Watanabe K, Kawakami N, Shiotani T, Adachi H, Matsumoto K, Imamura K, et al. The Japanese Workplace PERMA-Profiler: A validation study among Japanese workers. J Occup Health. (2018) 60:383–93. doi: 10.1539/joh.2018-0050-OA
27. Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five personality domains. J Res Pers. (2003) 37:504–28. doi: 10.1016/S0092-6566(03)00046-1
28. Li J. Psychometric properties of ten-item personality inventory in China. China J Health Psychol. (2013) 21:1688–92. doi: 10.13342/j.cnki.cjhp.2013.11.008
29. Wen S, Tang D, Yu G. The characteristics of regulatory emotional self-efficacy in Chinese graduate students. J psychol Sci. (2009) 32:666–8. doi: 10.16719/j.cnki.1671-6981.2009.03.025
30. Huang L, Jiang Q, Ren W. A study of the correlation between coping styles, social support and psychosomatic symptoms in cancer patients. Chin Ment Health J. (1996), 160–1. https://kns.cnki.net/kcms2/article/abstract?v=WVDzDAe5jxawnPOmlAsbAipE_cIOKehzDMGAtA2qhTdcG8I8y_SOkvyRlNUhm1p3FfpVuiGCDrE8uR-q3Z-C67f18YxTbZDgj4lMMzYNFrZoKqbXmqKJb6ZUI0i6Rz4FqyTaZrHTsgE=&uniplatform=NZKPT&language=CHS (Accessed March 7, 2025).
31. Lightfoot CJ, Howell M, Smith AC. How to assess quality of life in persons with chronic kidney disease. Curr Opin Nephrol Hypertens. (2021) 30:547–54. doi: 10.1097/mnh.0000000000000740
32. Wu C. Chinese version of the EQ-5D value set: Applicability in Chinese General population. PhD). Huazhong University of Science and Technology (2017). Available at: https://kns.cnki.net/kcms2/article/abstract?v=WVDzDAe5jxbtvKa5whTEYYEPGmXhGzzeTfekOhwBEM9JqCKamXW2aS4lXtnn75AHLHgSErSbk3yxpUaeOFIkQCI8419QqxwGbqkweVggitMaz8N_Sz4ixYe0fIxoh3iyEM9qc5sndh3LZvTGl8S3Nw==&uniplatform=NZKPT&language=CHS (Accessed March 7, 2025).
34. Yulu L, Bin Z, Jianqin S, Lei M. Depression in maintenance hemodialysis patients: What do we need to know? Heliyon. (2023) 9(9):e19383. doi: 10.1016/j.heliyon.2023.e19383
35. Jacobson J, Ju A, Baumgart A, Unruh M, O’Donoghue D, Obrador G, et al. Patient perspectives on the meaning and impact of fatigue in hemodialysis: A systematic review and thematic analysis of qualitative studies. Am J Kidney Dis. (2019) 74:179–92. doi: 10.1053/j.ajkd.2019.01.034
36. Hua L, Quan H, Limin W, Kehui S, Meng W, Jinhong X, et al. P1539THE influence of different hemodialysis frequency on MHD patients was analyzed BASED on the data of three consecutive years. Nephrol Dialysis Transplantation. (2020) 35(Supplement_3):gfaa142.P1539. doi: 10.1093/ndt/gfaa142.p1539
37. Nicole SR, Talia G, Amanda D, Martin H, Jonathan CC, Germaine W, et al. Australian rural caregivers’ Experiences in supporting patients with kidney failure to access dialysis and kidney transplantation: A qualitative study. Am J Kidney Dis. (2022) 80(6):773–82.e1. doi: 10.1053/j.ajkd.2022.05.015
38. Dąbrowska-Bender M, Dykowska G, Żuk W, Milewska M, Staniszewska A. The impact on quality of life of dialysis patients with renal insufficiency. Patient Prefer Adherence. (2018) 12:577–83. doi: 10.2147/ppa.S156356
39. Curtin RB, Sitter DC, Schatell D, Chewning BA. Self-management, knowledge, and functioning and well-being of patients on hemodialysis. Nephrol Nurs J. (2004) 31(4):378.
40. Momtaz YA, Hamid TA, Haron SA, Bagat MF. Flourishing in later life. Arch Gerontol Geriatr. (2016) 63:85–91. doi: 10.1016/j.archger.2015.11.001
41. Kondirolli F, Sunder N. Mental health effects of education. Health Econ. (2022) 31 Suppl 2:22–39. doi: 10.1002/hec.4565
42. Bellier-Teichmann T, Golay P, Bonsack C, Pomini V. Patients’ Needs for care in public mental health: unity and diversity of self-assessed needs for care. Front Public Health. (2016) 4:22. doi: 10.3389/fpubh.2016.00022
43. Vooijs M, Leensen MCJ, Hoving JL, Wind H, Frings-Dresen MHW. Value of work for employees with a chronic disease. Occup Med (Lond). (2018) 68:26–31. doi: 10.1093/occmed/kqx178
44. Songül D, Dilek A, Funda E. Association between spiritual well-being and resilience among Turkish hemodialysis patients. J Religion Health. (2020) 59:3097–109. doi: 10.1007/s10943-020-01000-z
45. Ali A, Sami AR, Mohammad R. Quality of life and general well-being in people receiving hemodialysis treatment: A cross-sectional study. Jordan J Nurs Res. (2022) 2(1):19–28. doi: 10.14525/jjnr.v2i1.07
46. Kim Y. Mental health and quality of life according to sleep in cancer survivors. Perspect Psychiatr Care. (2022) 58:2442–8. doi: 10.1111/ppc.13079
47. López MTM, Rodríguez-Rey R, Montesinos F, de Galvis SR, Ágreda-Ladrón MR, Mayo EH. Factors associated with quality of life and its prediction in kidney patients on haemodialysis. Nefrologia (Engl Ed). (2022) 42:318–26. doi: 10.1016/j.nefroe.2022.07.007
48. Coulombe S, Radziszewski S, Meunier S, Provencher H, Hudon C, Roberge P, et al. Profiles of recovery from mood and anxiety disorders: A person-centered exploration of people’s engagement in self-management. Front Psychol. (2016) 7:584. doi: 10.3389/fpsyg.2016.00584
49. Anglim J, Horwood S, Smillie LD, Marrero RJ, Wood JK. Predicting psychological and subjective well-being from personality: A meta-analysis. Psychol Bull. (2020) 146:279–323. doi: 10.1037/bul0000226
50. Power RA, Pluess M. Heritability estimates of the Big Five personality traits based on common genetic variants. Transl Psychiatry. (2015) 5:e604. doi: 10.1038/tp.2015.96
52. Takuji A, Yuki T, Daisuke T. Association between the Big Five personality traits and medication adherence in patients with cardiovascular disease: A cross-sectional study. PLoS ONE. (2022) 17(12):e0278534. doi: 10.1371/journal.pone.0278534
53. Zhenghong X, Juan D. A mental health informatics study on the mediating effect of the regulatory emotional self-efficacy. Math Biosci Eng. (2021) 18(3):2775–88. doi: 10.3934/mbe.2021141
54. Kyoung-Sook L, Seong-Ah A. Self-reflection, emotional self disclosure, and posttraumatic growth in nursing students: A cross-sectional study in South Korea. Healthcare. (2023) 11(19):2616. doi: 10.3390/healthcare11192616
55. Pauletto M, Grassi M, Passolunghi MC, Penolazzi B. Psychological well-being in childhood: The role of trait emotional intelligence, regulatory emotional self-efficacy, coping and general intelligence. Clin Child Psychol Psychiatry. (2021) 26:1284–97. doi: 10.1177/13591045211040681
56. Siamak K, Hassan Ali V, Nasrollah M, Sonay S, Mojtaba Rahimian B. Mental health, social support, and death anxiety in patients with chronic kidney failure. J Nervous Ment Dis. (2021) 209(11):809–13. doi: 10.1097/nmd.0000000000001386
57. Soneymol G, Zaidi SZH, Syed Sajid Husain K. Stress, anxiety and perceived social support among hemodialysis patients with chronic kidney disease. Int J Health Sci (IJHS). (2022) 6(S1):9494–507. doi: 10.53730/ijhs.v6ns1.7184
58. Su YJ, Chow CC, Yen CI, Chuang SS. Posttraumatic growth among burn survivors 2 years after the 2015 Formosa Fun Coast Water Park explosion in Taiwan. Psychol Trauma. (2020) 12:11–9. doi: 10.1037/tra0000458
59. Schultz BE, Corbett CF, Hughes RG, Bell N. Scoping review: Social support impacts hospital readmission rates. J Clin Nurs. (2022) 31:2691–705. doi: 10.1111/jocn.16143
60. Sharp L, Redfearn D, Timmons A, Balfe M, Patterson J. Posttraumatic growth in head and neck cancer survivors: Is it possible and what are the correlates? Psychooncology. (2018) 27:1517–23. doi: 10.1002/pon.4682
61. Zhang L, Lu Y, Qin Y, Xue J, Chen Y. Post-traumatic growth and related factors among 1221 Chinese cancer survivors. Psychooncology. (2020) 29:413–22. doi: 10.1002/pon.5279
62. Xu W, Fu G, An Y, Yuan G, Ding X, Zhou Y. Mindfulness, posttraumatic stress symptoms, depression, and social functioning impairment in Chinese adolescents following a tornado: Mediation of posttraumatic cognitive change. Psychiatry Res. (2018) 259:345–9. doi: 10.1016/j.psychres.2017.09.088
63. Gilbertson EL, Krishnasamy R, Foote C, Kennard AL, Jardine MJ, Gray NA. Burden of care and quality of life among caregivers for adults receiving maintenance dialysis: A systematic review. Am J Kidney Dis. (2019) 73:332–43. doi: 10.1053/j.ajkd.2018.09.006
64. Alireza I, Maryam H, Parvaneh A, Shahrazad S, Maryam F. The effects of peer support on depression, anxiety, and stress among patients receiving hemodialysis. Iranian Red Crescent Med J. (2019) e66321. doi: 10.5812/ircmj.66321
65. Mehrotra R, Cukor D, Unruh M, Rue T, Heagerty P, Cohen SD, et al. Comparative efficacy of therapies for treatment of depression for patients undergoing maintenance hemodialysis. Ann Internal Med. (2019) 170(6):369–79. doi: 10.7326/m18-2229
66. Griva K, Chia JMX, Goh ZZS, Wong YP, Loei J, Thach TQ, et al. Effectiveness of a brief positive skills intervention to improve psychological adjustment in patients with end-stage kidney disease newly initiated on haemodialysis: protocol for a randomised controlled trial (HED-Start). BMJ Open. (2021) 11:1–11. doi: 10.1136/bmjopen-2021-053588
67. Sousa H, Ribeiro O, Paúl C, Costa E, Frontini R, Miranda V, et al. “Together we stand”: A pilot study exploring the feasibility, acceptability, and preliminary effects of a family-based psychoeducational intervention for patients on hemodialysis and their family caregivers. Healthcare (Basel). (2021) 9(11):1585. doi: 10.3390/healthcare9111585
Keywords: maintenance hemodialysis, chronic kidney disease, flourishing, PERMA, social support, quality of life
Citation: Zeng XQ, Yan HL, Qian YQ, Li YQ, Yang J, Gong YL, Liu Y, Chen LJ, Wu J and Chu J (2025) Flourishing and its influencing factors among maintenance hemodialysis patients in Shanghai, China: a cross-sectional study. Front. Psychiatry 16:1480308. doi: 10.3389/fpsyt.2025.1480308
Received: 13 August 2024; Accepted: 25 February 2025;
Published: 27 March 2025.
Edited by:
Saïd Boujraf, Sidi Mohamed Ben Abdellah University, MoroccoReviewed by:
Miguel Landa-Blanco, National Autonomous University of Honduras, HondurasRajat Sanker Roy Biswas, Chattagram Maa-O-Shishu Hospital Medical College, Bangladesh
Aaron Wightman, University of Washington, United States
Wafaa Fadili, UHC Mohammed VI, Morocco
Copyright © 2025 Zeng, Yan, Qian, Li, Yang, Gong, Liu, Chen, Wu and Chu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Wu, cWluZ3FpbmcyMDAzMDUxMUAxNjMuY29t; Jing Chu, Y2h1amluZzE5OTlAc21tdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Xiao Qing Zeng
Xiao Qing Zeng Hong Li Yan
Hong Li Yan Yue Qin Qian
Yue Qin Qian Yong Qi Li
Yong Qi Li Jie Yang
Jie Yang Yan Lin Gong1
Yan Lin Gong1 Yi Liu
Yi Liu Li Jing Chen
Li Jing Chen Jing Chu
Jing Chu