
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 28 February 2025
Sec. Addictive Disorders
Volume 16 - 2025 | https://doi.org/10.3389/fpsyt.2025.1479827
Introduction: Suicide is a major public health concern, particularly among people with alcohol use disorders (AUD). Rumination, as a dysfunctional emotion regulation strategy, and increased emotional reactivity may significantly influence suicide risk in this population.
Aim: The aim of this study was to assess whether different emotional reactivity mediate the association between ruminations and suicide risk, and whether AUD or control group (HC) status moderates these relationships.
Methods: A study was conducted with 152 participants, including 86 from AUD and 66 from HC. Self-report questionnaires measuring ruminations, emotional reactivity and suicide risk were used. Structural Equation Modeling, invariance analysis, and moderated mediation estimation were used in the analyses.
Results: The mediation analysis in the full sample revealed a significant indirect effect of rumination on suicide risk via emotional reactivity. Multi-group analysis indicated no significant differences in the mediation effect between the AUD and HC groups, with neither group showing a statistically significant indirect effect.
Conclusions: The findings indicate that emotional reactivity may serve as a key mechanism mediating the relationship between rumination and suicide risk. Therapeutic interventions should focus on reducing ruminations and emotion reactivity to effectively reduce suicide risk in this group. Further research is needed to better understand these mechanisms.
Suicide is one of the leading causes of death in the modern world. Each year, more than 800 000 people lose their lives to suicide as a result of a variety of circumstances (1). The theoretical construct of suicide is characterised by complexity and stages. The different stages of suicidal behaviour can be divided into suicidal thoughts, plans and attempts (2). Suicidal thoughts or ideation, is a broad term used to describe a range of ideas, fantasies or obsessions about ending one’s life (3). Suicide plans are mental representations of ways and strategies of action intended to lead to the successful realisation of an intention to take one’s own life. A suicide attempt, on the other hand, is a behaviour that leads to significant harm or a real threat to life (4).
Undoubtedly, one type of mental disorder that has a significant association with increased suicide risk is substance abuse. It has been confirmed in the literature that alcohol use disorders (hereafter AUD) increase suicide risk (5), and AUD with co-occurring mood disorders (6) represents the main psychiatric diagnosis for completed suicide attempts (7). Consumption of significant amounts of alcohol often immediately precedes the onset of suicidal thoughts and attempts, and analyses of post-mortem toxicological findings confirm the presence of alcohol in the blood among 30% of suicidal individuals (8).
Theoretical conceptions of the mechanisms underlying the predictive relationship between AUD and suicide risk include two complementary patterns: a proximal relationship due to acute alcohol intoxication and a distal (i.e. predisposing) relationship due to chronic alcohol use (9). The effects of alcohol intoxication, e.g. increased dysphoria, psychomotor agitation, impaired perception and impaired consciousness, can cause behavioural and affective disinhibition potentially reducing the fear of death that might otherwise act as a psychological barrier to suicide (10). In contrast, in the case of chronic alcohol use, the mechanisms of influence on suicide risk are more complex and involve both behavioural and neural processes related to the long-term effects of alcohol on brain structure and function.
People with a history of suicidal behaviour and those with AUD show similar changes in brain morphometry. According to neuroimaging studies, individuals with alcohol dependence experience impairments in higher cognitive functions, including inhibitory control and decision-making, which have been linked to structural changes in the prefrontal cortex area (PFC), including a significant reduction in grey matter volume in the dorsolateral prefrontal cortex (DLPFC) (11), medial (mPFC) (12), as well as orbitofrontal cortex (OFC) (13). Suicidal behaviour among individuals with a history of suicide is also associated with a reduction in grey matter volume in the PFC, particularly in the dlPFC involved in decision-making and inhibitory control (14–16).
Difficulties caused by emotional overreactions in response to negative stimuli and associated emotion dysregulation among people with AUD have been linked by researchers to increased activation of amygdala (17) as well as reduced amygdala volume (18). Similar results were obtained in a population of individuals with a history of suicidal thoughts, behaviours and attempts, where significant reductions in the grey matter in the amygdala were also found (19) and greater activation of this area during fMRI tasks (1).
Dysfunctional changes in the area of the reward system and habits in the AUD group have been linked to increased activity of nucleus accumbens (20) and decreased volume of the nucleus accumbens (21). In addition, studies have shown a significant reduction in the volume of both the caudate nucleus (22) and the putamen (23) in the AUD group, which have been linked to increased symptoms of alcohol dependence, impulse control disorders and increased risk of relapse (24, 25). Similarly, greater putamen activity has been noted among those with suicide attempts (26) and reduced grey matter volume in both putamen and caudate nucleus area (27).
One transdiagnostic risk factor for suicide is emotional dysregulation resulting from the use of maladaptive emotion regulation strategies (28, 29). In the research literature, rumination is defined as a dysfunctional emotion regulation strategy involving a repetitive and passive focus on symptoms of distress, as well as on the possible causes and consequences of these symptoms (30). Rumination is expressed by the presence of content-independent perseverative and/or fixational thoughts that result in a lack of problem solving (30) and thus leads to hyperactivation of emotional reactions (31). Research indicates that ruminations (measured as a state) are associated with increased HPA axis activity, resulting in higher levels of cortisol, the main stress hormone, although results for ruminations (measured as a trait) are less conclusive (32, 33). Furthermore, ruminations affect the sympathetic nervous system, as reflected in increased heart rate (HR) and blood pressure (BP) during stress-inducing fMRI tasks (34). Ruminations are associated with structural changes and brain activation. Research indicates that individuals with high levels of ruminations have altered volume in the DLPFC and anterior cingulate cortex (ACC), which affects their ability to regulate emotions and make decisions (35). fMRI studies have shown that ruminations are associated with impaired activation of the default mode network (36). The results confirm that rumination is an important factor in problematic alcohol use (37) and highlight the potential importance of therapeutic interventions targeting the mechanisms of ruminative strategies to treat alcohol dependence (38). Both cognitively (rumination) and interpersonally (co-rumination), the ruminative strategy is significantly associated with increased alcohol use in both adolescents and adults regardless of gender (39). In addition, individuals using ruminative strategies may similarly use alcohol to escape from or modulate distressing thoughts (39). The authors also showed that ruminations can directly or indirectly cause cognitive hunger experiences when an individual uses alcohol to interrupt the ruminative process, with the likelihood of relapse increasing due to the involvement of alcohol-dependent individuals in ruminations (40).
Empirical findings suggest that ruminations may mediate the impact of negative life events on suicidal thoughts (41). The authors highlight that rumination is positively related to suicidal thoughts and the likelihood of suicide attempts, through the maintenance of negative emotions and accompanying dysfunctional cognitive schemas (42). Rumination has been shown to be a predictor of the duration of suicidal thoughts (43). Furthermore, specific ruminations about suicide, i.e. repeated thoughts about suicide, have been shown to be associated with a higher prediction of a suicide attempt than other known risk factors (44) and may mediate the association between suicidal thoughts and suicide attempts across the life course (45). This scientific domain shows particular clinical potential in a population with AUD, due to the limited number of studies directly analysing the association between ruminations and suicide risk in this group. Undoubtedly, there is a need for further empirical exploration regarding this research issue and understanding complexity of mechanisms may contribute to the development of more effective therapeutic interventions.
Because rumination can lead to emotional arousal, it has been linked to increased emotional reactivity (46, 47). Furthermore, research suggests that rumination may prolong emotional reactivity following a negative event (32). Ruminations have been shown to correlate positively with emotional reactivity, particularly in the context of elevated cortisol levels and increased negative affect. This suggests a link between ruminations and physiological and behavioural markers of emotional reactivity (48).
Analyses of emotional reactivity as a potential risk factor for suicide have appeared in the literature (49). Researchers define emotional reactivity as a subjective predisposition to respond intensely to a wide range of emotional stimuli (especially of negative valence) and to recover slowly from emotional arousal (50, 51). Furthermore, the authors describe emotional reactivity in terms of emotion sensitivity/activation (e.g., speed of response to stimuli), emotion intensity (e.g., how strongly or intensely the emotion is felt) and emotion persistence (e.g., how long it takes to return to baseline after arousal) (51). Emotional reactivity has been linked to increased activation of the autonomic system and the HPA axis (48). Neuroimaging studies have shown that high emotional reactivity correlates with increased activation of the amygdala as well as the left PFC (52).
Among people with AUD, the accumulation of negative life events leads to an increase in negative emotional states (53). According to theories of emotional reactivity, individuals characterised by experiencing emotions with greater intensity may also have difficulty tolerating stressful situations (54). Therefore, the risk of AUD is high in individuals with high levels of emotional reactivity (55).
Theoretical models of suicide assume that along with a high level of emotional reactivity, there is significant clinical suffering that the individual cannot cope with, and suicide is a behavior aimed at escaping mental suffering (56). Also in the theoretical motivational-volitional model of suicide (57) emotional reactivity has been identified as one of the diatheses providing the background for the occurrence of suicidal thoughts. Similarly, empirical research indicates that there is a positive association between emotional reactivity and suicidal thoughts and attempts (58, 59). Furthermore, current research indicates higher levels of emotional reactivity among people with emotion dysregulation disorders, including patients with suicidal tendencies (60). However, the existing research literature on the relationship between suicide risk and emotional reactivity lacks empirical data that takes into account the context of maladaptive emotion regulation strategies, including ruminations. Also, the mediating mechanisms (i.e. how emotional reactivity relates to suicide risk) and moderating mechanisms underlying the relationship remain largely unexplored.
Research on the direct impact of rumination on suicide risk remains limited both among individuals with AUD and within the healthy control (HC) group. It has been demonstrated that rumination affects emotional reactivity, which may serve as a mediating variable (mediator) in the relationship between rumination and suicide risk. Consequently, modelling the indirect pathway involving emotional reactivity as a mediator warrants further investigation, particularly in AUD and HC groups, given the lack of prior studies addressing this associations.
The aim of the present study is to assess: a) intergroup differences in levels of ruminations, emotional reactivity (emotions with negative valence) and suicide risk, b) correlations between study variables, c) predictive structural model designed to examine the relationships between rumination, emotional reactivity, and suicide risk in two study groups: individuals with AUD and HC. The model posits that rumination has a direct effect on suicide risk, while emotional reactivity serves as a mediating variable in the relationship between rumination and suicide risk. Furthermore, group status (AUD vs. HC) moderates these relationships. Additionally, the analysis aimed to assess the invariance of the model across the two groups by examining intergroup differences in the structural relationships between the tested variables.
All together 152 participants took part in the study, which was conducted anonymously online via the study website. Data came from an ongoing project assessing emotion dynamics and regulation in the context of suicide risk factors and protective factors in people with a diagnosis of AUD compared to HC.
The AUD sample consisted of n = 86 subjects aged between 24 and 67 years (Mage = 39.15; SDage = 8.82), among whom nm = 54 were men (62.8%) and nw = 32 were women (37.2%). The majority of AUD respondents (46.5%) had a secondary education. Completed primary education was declared by 1.2% of people. Vocational school was completed by 8.1% of the respondents, while tertiary education was held by 38.4% of the respondents. Most people (67.4%) did not declare somatic diseases. The mean duration of abstinence in years among AUD subjects was M = 2.17, SD = 4.09. The AUD group was recruited from among those maintaining abstinence in inpatient wards and outpatient treatment addiction clinics. Inpatient treatment included an 8-week abstinence-based programme and intensive individual and group therapy. In contrast, outpatient treatment included patients in both partial and full remission. The diagnosis of AUD was based on the International Classification of Diseases and Health Problems (61) psychiatric diagnosis made on admission to the treatment unit. Due to the high overrepresentation of men in addiction treatment programmes, the AUD group in this study was predominantly male (62.8%). Patients were ineligible to participate in a treatment programme if they had a clinically significant cognitive deficit or met any of the following criteria: a history of psychosis, a co-occurring psychiatric disorder requiring current psychiatric treatment (e.g. history of psychosis, bipolar affective disorder) or the presence of acute alcohol withdrawal symptoms.
The HC group consisted of n = 66 people aged 18 to 57 years (Mage = 29.35; SDage = 9.46), of whom nm = 37 were men (56.1%) and nk = 29 were women (43.9%). Exclusion criteria for the HC group was the presence of an alcohol related problem and other exclusion criteria were similar to those for the AUD group. The majority of subjects in the HC group (56.1%) had a tertiary education. Completed primary education was declared by 3.0% of subjects. Secondary school was completed by 22.7% of the respondents, while those currently studying accounted for 13.6% of the respondents.
The study was approved by the Ethics Committee at Cardinal Stefan Wyszynski University in Warsaw (Evidence: 6/2023).
Sociodemographic characteristics (e.g. age, biological sex, education) were obtained by means of a self-report questionnaire.
Audit (62). The tool is a screening tool to determine the extent to which a person surveyed consumes alcohol. It contains ten questions that address three areas of alcohol use: risky drinking, harmful drinking and alcohol dependence. Each question is assigned a set of answers to choose from. Each answer is assigned a score (from 1 to 4). Reliability for the total score Cronbach’s alpha = 0.972.
The Hospital Anxiety Depression Scale (HADS) (63), Polish validation (64). A screening tool used to assess the severity of medication and depression symptoms. It is not used for clinical diagnosis. It contains 14 items, of which 7 form the anxiety subscale (HADS-A) and 7 form the depression subscale. For the depression scale, Cronbach’s alpha reliability = 0.752.
Cognitive Emotion Regulation Questionnaire (CERQ) (65), Polish validation (66):. A 36-item questionnaire designed to assess individual differences in cognitive emotion regulation in response to stressful, threatening or traumatic life events. The tool assesses nine 4-item dimensions: blaming self, blaming others, acceptance, refocusing on planning, positive refocusing, rumination, positive refocusing, positive refocusing, perspective taking and catastrophising. Responses are given on a 5-point Likert scale from 1 ‘almost never’ to ‘almost always’. Therefore, subscale scores can range from 4 to 20, with higher subscale scores indicating greater frequency of use of a particular cognitive strategy. Cronbach’s alpha reliability for the ruminations scale = 0.763.
Perth Emotional Reactivity Scale (PERS) (67) Polish version (30): is a 30-item self-report questionnaire used to assess traits (dimensions) of emotional reactivity. PERS examines emotional reactivity as defined by Becerra (67); that is, it measures the typical ease/speed of activation, intensity and duration of emotional reactions, and allows the assessment of emotional reactivity in relation to positive (e.g. joy) and negative (e.g. sadness) emotions separately. Scores for the six subscales and the two composite subscales can be obtained by summing the respondent’s responses (i.e. the numbers to be circled on the 5-point response scale) for the respective items. The higher the score for the individual subscales and the two composite subscales, the higher the level of the dimensions of emotional reactivity; in other words, this means that the emotion in question can be more easily/quickly activated, more intense and lasts longer. Cronbach’s alpha reliability for PERS General Emotional Reactivity scale = 0.928.
Suicidal Behaviour Questionnaire Revised (SBQR) (68) pol. version (69). The questionnaire consists of four test items. The first three questions concern retrospective assessment: (1) “Have you ever thought about taking your own life or made an attempt to do so?”; (2) “How often have you had thoughts about taking your own life in the past year?”; (3) “Have you ever told someone about your intention to commit suicide or the likelihood that you might commit suicide”. The last, fourth question, concerns prospective assessment: (4) “How likely is it that one day you will attempt/attempt suicide?”. Responses are scored on a scale of 1 to 3 (questions 1-3) and 0 to 6 (question 4). Cronbach’s alpha reliability = 0.864.
In the first step of the analysis, a series of plots were generated to assess the relationships between the dependent variable, the mediator, and other variables. Both linear and quadratic functions were fitted to the observed data to evaluate their adequacy. This procedure was conducted separately for the alcoholic and healthy groups to assess the consistency of the relationships within each group. The series of plots and R-squared coefficients for both linear and quadratic functions, included in Supplementary Material A, demonstrated that linear relationships between variables were comparable to, or slightly weaker than, those for the quadratic function. However, the better fit of the quadratic function may have resulted from the small sample size and the presence of outliers, which could have significantly influenced the fit of both models. The visualised relationships confirmed the similarity in the fit of linear and quadratic functions; therefore, linear analyses were chosen for further investigation.
In the second step of the analysis, outliers were identified and smoothed. This smoothing procedure was performed using the statistical software SZTOS (70), designed to detect outliers in linear regression models testing moderation effects. The moderation procedure was applied because the slope-invariance procedure is a generalisation of simple interaction analysis.
The first step of the smoothing algorithm involved the random selection of the dependent variable, independent variable, and moderating variable, followed by the construction of a regression model. The randomness in selecting these variables aimed to minimise bias in the sequence of data imputation. Based on the specified regression model, the following influence measures were computed for each observation: studentised residuals, leverage values, and Cook’s distance (71). Observations with elevated values for these indicators were flagged, and missing values were inserted into the dependent variable columns of the identified rows. These missing values were then imputed using the random forests technique, which leveraged all available dataset information to predict the missing values. Additionally, if there were more than two independent, dependent, or moderating variables, the smoothed data from the first iteration were carried forward to subsequent smoothing analyses.
As mentioned earlier, missing data imputation via the random forests method was carried out using the missForest package from the CRAN repository (72) in R. This non-parametric method applies the random forests algorithm (73) to optimise the prediction of missing values. The random forests method involves randomly selecting observations (with replacement) to generate multiple decision trees containing different variables and observations from the dataset. When aggregated, these trees enable either regression-based prediction (for quantitative variables) or classification-based voting (for qualitative variables). The missing data imputation process using the random forests method consists of three iterative steps:
1. Determining the quantity and type (qualitative vs. quantitative) of missing data.
2. Replacing missing values with the mean (for continuous data) or mode (for categorical data).
3. Performing regression- or classification-based prediction of missing values using the random forests algorithm.
The entire dataset was randomly used in the missing value prediction process, and these steps were repeated until the prediction or classification error was minimised.
The results of the analysis are presented in Supplementary Material B, which includes a series of figures and tables. Figure a displays a plot of influential observations, Figure b presents the moderated relationships between variables in the model recalculated using raw data, and Figure c shows the moderated relationships recalculated using smoothed data predicted via the random forests technique. The analysis was performed on the full dataset, which consisted of N = 152 observations.
Based on both the raw and smoothed data, two structural equation models were estimated using the lavaan package (74). The estimator used was MLR (maximum likelihood estimation with robust Huber-White standard errors), which is recommended for small samples with non-normally distributed data (75). Model diagnostics for both datasets were evaluated using general Cook’s Distance in the influence.SEM package (76). The deltaChi method was omitted because the model demonstrated an almost ideal fit. These diagnostic procedures iteratively removed each observation (one at a time) and refitted the SEM model to the reduced dataset (N-1 cases). The recalculated general Cook’s Distance indicated that preprocessing the data resulted in fewer extreme observations. Even if an observation remained an outlier in the smoothed dataset, its influence was weaker than in the raw data. The results of the Cook’s Distance analysis are presented in Figures 1 and 2.
To determine whether the groups were of equal size, a chi-square test for one variable was conducted (Pearson, 1900). The analysis revealed that the groups were statistically equal in size, χ² (1) = 2.63; p = 0.105. The homogeneity of variance in both groups was assessed using Levene’s test (Levene, 1960). If the assumption of homogeneity of variance was met, the result of Student’s t-test was reported; otherwise, Welch’s t-test was used (Welch, 1951). Effect sizes were assessed using Cohen’s d measure (Cohen, 2013). Analyses using Spearman’s correlation were performed to examine the relationship between the variables under study. A 95% confidence interval (CI) was used in both analyses.
Due to differences in the level of variables analysed across groups, and based on previous literature on the relationships examined, further analyses included the controlling co-variables: age (77), biological sex (47), current severity of alcohol use (78), severity of depressive symptoms (79, 80), and education (81).
First, intergroup differences were examined for the primary variables under investigation, namely rumination, emotional reactivity, and suicide risk. Subsequently, correlations between these variables were analysed both within the entire sample and across individual groups. Additionally, correlations between rumination, emotional reactivity, and suicide risk were assessed to evaluate the predictive validity of the structural model. The analyses also included depression severity, alcohol consumption, age, gender, and education as control variables. Table 1 below presents the descriptive statistics for the analysed variables.
Individuals diagnosed with AUD had significantly higher mean scores across all the variables listed below compared to the control group, except for rumination. Specifically, the AUD sample attained a mean SBQR score of 7.81 ± 2.74. The authors of the scale proposed a cutoff score of 8 points for individuals in clinical samples (68). Detailed results are presented in Table 2.
Correlations between rumination, emotional reactivity, suicide risk, and control variables were computed separately for individuals with AUD and HC to identify significant associations and preliminarily confirm the validity of the proposed model. Table 3 presents the correlation coefficients for all variables in the entire sample, while Tables 4 and 5 display the correlation coefficients within each group.
In this study, the relationship between rumination (CERQ Rumination) and suicide risk (SBQR Score) was examined, with emotional reactivity (PERS General Emotional Reactivity) included as a mediator (Figure 3 presents conceptual model). The analysis was conducted using structural equation modelling (SEM) in R (lavaan package), and the estimation was performed using the MLR method (maximum likelihood estimation with robust standard errors), which provides robust estimates and adjusted standard errors.
The model fit analysis demonstrated a very good alignment between the model and the empirical data. The chi-square statistic for one degree of freedom was not statistically significant (χ²(1) = 0.01; p > 0.05), and other fit indices also indicated a high level of model-data fit (CFI = 1.00; TLI = 1.18; NFI = 1.00; IFI = 1.01; RMSEA = 0.00, 90% CI [0.00–0.07], PCLOSE = 0.942; SRMR = 0.00; GFI = 1.00; AGFI = 1.00). These results suggest that the model adequately reflects the structural relationships among the examined constructs. A detailed overview of all structural model parameter estimates is presented in Table 6.
In the path analysis, the examined model accounted for the effect of rumination on suicide risk through a single mediator - emotional reactivity. The model also controlled for the effects of age, sex, education, depression severity (HADS Depression), and alcohol use severity (AUDIT Score). Additionally, correlations between rumination and control variables were estimated, allowing for the consideration of their potential influence on the analysed relationships (see Table 1 in Supplementary Material C). A significant positive association was found between rumination and emotional reactivity (β = 0.24; Z = 2.91; p < 0.01), indicating that higher levels of rumination were significantly associated with heightened emotional reactivity. Furthermore, elevated emotional reactivity significantly increased suicide risk (β = 0.25; Z = 3.33; p < 0.001). However, the direct effect of rumination on suicide risk was not statistically significant (β = 0.07; Z = 1.05; p > 0.05), suggesting that this relationship primarily occurs via emotional reactivity.
The mediation effects in the full sample revealed a statistically significant indirect effect (b = 0.060; s.e. = 0.030; Z = 2.003; p = 0.045). This finding suggests that rumination contributes to increased suicide risk through heightened emotional reactivity. Furthermore, the lack of a significant direct effect of rumination on suicide risk strengthens the hypothesis of full (or predominant) mediation. The R² values indicated that the model explained 45% of the variance in suicide risk (R² = 0.45) and 21% of the variance in emotional reactivity (R² = 0.21), highlighting the model’s substantial predictive capability.
Further analysis of path coefficient invariance revealed significant differences in model fit between models assuming equal versus varying regression slopes across groups (χ²(13) = 36.82; p < 0.001). The lower χ² value suggests that the model accounting for group differences in specific paths provides a better fit to the data.
A multi-group analysis was conducted to examine the potential moderate mediation effect by group status (AUD vs. HC). Table 7 presents the comparison of model parameter estimates between the AUD and HC groups. The overall mediation effect did not significantly differ between groups (Z = 1.05; p = 0.294). However, separate estimates of the indirect effect within each group indicated that in the HC group, the indirect effect (b = 0.048; s.e. = 0.032; Z = 1.493; p = 0.135) and in the AUD group (b = 0.010; s.e. = 0.017; Z = 0.585; p = 0.558) did not reach statistical significance.
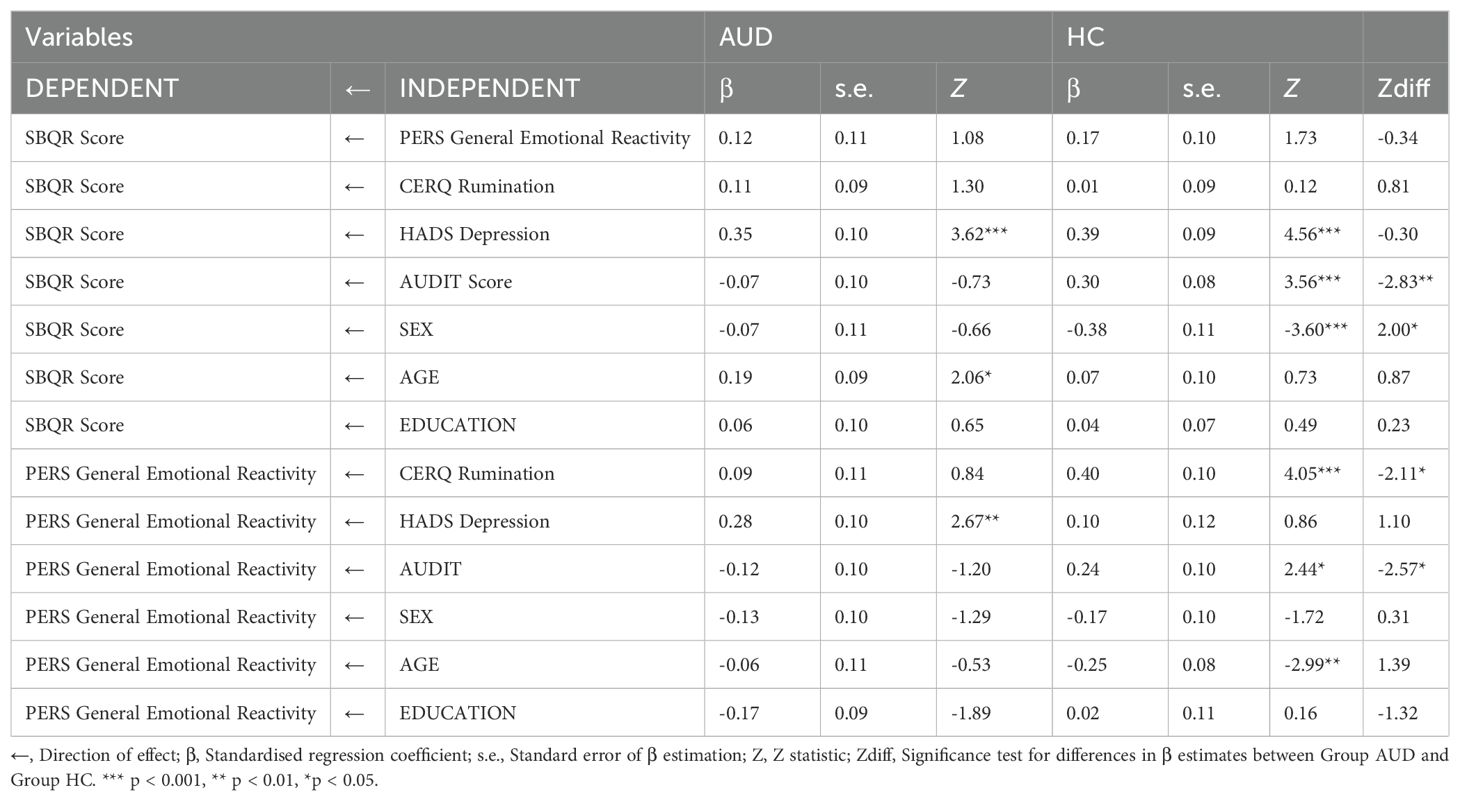
Table 7. Comparison of model parameter estimates across AUD and HC groups defined by the GROUP variable.
The aim of this article was to examine the associations between rumination, emotional reactivity, and suicide risk (i.e., the presence of suicidal thoughts, plans, and attempts) in individuals with AUD and in a healthy control group. The analysis also included depressive symptoms and other sociodemographic variables (age, gender, education), as well as alcohol use severity. To the authors’ knowledge, this is the first study to use structural equation modelling (SEM) to estimate the influence of the analysed effects of rumination and emotional reactivity on suicide risk, as well as possible differences between the studied groups (AUD vs. HC). Therefore, in the next section of the article, we will compare our results with reports from other studies that analysed similar variables but in different contexts or groups.
In the tested model, in the entire studied sample, it turned out that rumination did not exert a significant direct effect on suicide risk. This is particularly interesting in the context of the research literature cited earlier, in which rumination was a predictor of suicide risk. However, our findings are consistent with other studies suggesting that rumination may operate through more complex mechanisms and mediators (82–85).
Our study confirmed that ruminations are significantly positively associated with emotional reactivity, and that increased emotional reactivity, in turn, significantly and positively affects suicide risk. Moreover, a significant mediation effect (b = 0.06, p = 0.045) of ruminations on suicide risk via emotional reactivity was obtained in the whole sample. This result is consistent with the concepts emphasising that intense and persistent ruminative states may lead to an increased susceptibility to reacting to emotions of negative valence. In turn, increased emotional reactivity facilitates the emergence and maintenance of suicidal thoughts. This sequence of events – from chronic, negative ruminations to the escalation of emotional reaction – may promote the development of suicidal behavior. It should also be noted that in our model, depressive symptoms turned out to be a key predictor of both emotional reactivity and suicidal risk, which confirms previous findings that depression is one of the most important risk factors in the context of suicidal behavior. suicidal.
The tested structural model explained approximately 45% of the variance in suicide risk and approximately 21% of the variance in emotional reactivity. These results are consistent with other reports indicating that cognitive factors (such as rumination) and emotional factors (including increased reactivity) combined with depressive symptoms may jointly contribute significantly to explaining the complex phenomenon of suicidal (49, 51, 86).
Invariance analysis showed that some of the regression slopes differed between the groups, which was confirmed by a significant difference in the fit of the models (χ²(13) = 36.82; p < 0.001). This means that some of the relationships between variables take slightly different values in both groups. For example, in the control group, the intensity of alcohol use turned out to be a significantly positive predictor of suicide risk, while in the AUD group this effect was insignificant and had a negative direction. On the other hand, in the AUD group, depression retained a significant, positive effect on suicide risk, which did not differ substantially from the effect in the control group, although the strength of the relationship may have differed slightly.
From the perspective of testing moderated mediation, the most important thing is that group status (AUD vs. HC) did not significantly change the indirect effect of rumination on suicide risk via emotional reactivity. In other words, the mechanism itself, in which ruminations translate into suicidal behaviours mainly due to increased emotional reactivity, did not depend in a statistically significant way on membership in the studied group. The effect obtained in the HC group is surprising in the context of another study, which showed that emotional reactivity was a significant predictor of suicidal thoughts and behaviours among people from the general population (59), however, in this study only the healthy population was assessed, and emotional reactivity was tested as an independent variable, and the authors did not control for depressive symptoms and current level of alcohol consumption as covariates.
Our result, however, may indicate that the analysed subgroups are too small to obtain the moderated mediation effect, as well as the significant mediation effect expected in the HC group, although our result suggests that some differences in the intensity of specific predictors (e.g. depression, alcohol use or gender) may modify this relationship in each of the groups. Similarly, Nolen-Hoeksema and Harrell (87) have shown that rumination is strongly associated with depression and perceived negative affect in alcohol abusers, which in the long term may lead to suicide risk. However, healthy individuals, in contrast to those with AUD, often have access to more adaptive emotion regulation strategies that allow them to effectively modulate negative emotion reactivity (88).
These findings have important clinical implications. Therapeutic interventions and pharmacological treatment for people with AUD should specifically focus on reducing the severity of ruminative thoughts. Ruminations-focused interventions, such as metacognitive therapy and ruminations-focused cognitive behavioural therapy (89), have shown significant efficacy in the treatment of depression (90). In addition, there is some evidence to suggest that mindfulness-based cognitive therapy, which also places a strong emphasis on eliminating ruminative processes, is effective in therapy of patients with suicidal thoughts (91). More recently, forms of brief online interventions targeting ruminations have also emerged and have been found to be acceptable and effective in reducing symptoms of ruminations, worry anxiety and depression (92). For emotional reactivity, mindfulness meditation is a particularly promising intervention, as it has been found to simultaneously reduce physiological overreactivity and, in addition, reduce the severity of ruminations (93). Therefore, empirical studies on the effectiveness of such interventions in the AUD population are therefore scientifically proven and necessary in prevention and therapy of suicide risk. The aforementioned metacognitive therapy and cognitive-behavioural therapy focused on ruminations may be implemented into therapeutic programme for people with AUD representing a valuable form in reducing suicide risk. Certainly, these promising results require further exploration considering very limited research done in this field in AUD group. On the other hand, there is also research conducted on pharmacological interventions aimed at reducing the severity of ruminations. For example, combining amisulpride with antidepressant therapy in patients with treatment-resistant depression led to marked improvements in psychopathology in most patients, including those with severe ruminations (94). Aripiprazole monotherapy appears effective in reducing ruminations in cases of non-psychotic depression (95). Given that patients exhibiting increased ruminations are beneficiaries of treatment with antipsychotics (96), it is reasonable to focus future research on evaluating the efficacy of these therapies also in the AUD population who use this maladaptive emotion regulation strategy excessively.
Several limitations of this study are worth noting. First of all, the study was cross-sectional, which limits the ability to draw cause-and-effect conclusions. In addition, variables were measured as traits rather than as momentary mental states, meaning that they were analysed independently of situational context and temporal implications and thus limiting insight into the dynamics of the mutual links between the variables presented. This is important particularly in the AUD group, as their emotional state, the regulatory strategies used and potential suicidal behaviour can fluctuate considerably depending on a number of factors related to both clinical variables and situational context. Finally, testing a model of such complexity may introduce the risk of over-interpreting the results therefore the conclusions drawn from its validation are preliminary analyses requiring further scientific exploration.
Future research should use a longitudinal approach such as Ecological Momentary Assessment (EMA) to better understand the dynamic and time-varying relationships between ruminations, emotional reactivity and suicide risk. The use of EMA may also help to identify everyday emotional triggering moments (trigger moments) and explore how the activation, intensity and duration of negative emotions affect the relationship between ruminations and suicide risk, and in particular whether there are specific patterns of emotional reactivity that increase suicide risk in the AUD group (97). In line with research on variability and flexibility of emotion regulation, it is worth considering an analysis of whether different patterns of ruminative strategy use over time directly predict suicide risk in the AUD group (98).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
MW: Conceptualization, Data curation, Formal Analysis, Methodology, Writing – original draft, Investigation. KKa: Data curation, Formal Analysis, Methodology, Visualization, Writing – review & editing. KKu: Conceptualization, Supervision, Writing – review & editing, Formal Analysis.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1479827/full#supplementary-material
1. Dobbertin M, Blair KS, Carollo E, Blair JR, Dominguez A, Bajaj S. Neuroimaging alterations of the suicidal brain and its relevance to practice: an updated review of MRI studies. Front Psychiatry. (2023) 14:1083244. doi: 10.3389/fpsyt.2023.1083244
2. Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. (2016) 12:307–30. doi: 10.1146/annurev-clinpsy-021815-093204
3. Onaemo VN, Fawehinmi TO, D’Arcy C. Risk of suicide ideation in comorbid substance use disorder and major depression. PloS One. (2022) 17:e0265287. doi: 10.1371/journal.pone.0265287
4. Klonsky ED, Saffer BY, Bryan CJ. Ideation-to-action theories of suicide: a conceptual and empirical update. Curr Opin Psychol. (2018) 22:38–43. doi: 10.1016/j.copsyc.2017.07.020
5. Kim AM. Alcohol consumption and suicide rate: A cross-sectional analysis in 183 countries. Psychiatry Res. (2021) 295:113553. doi: 10.1016/j.psychres.2020.113553
6. Salles J, Stephan F, Molière F, Bennabi D, Haffen E, Bouvard A, et al. Indirect effect of impulsivity on suicide risk through self-esteem and depressive symptoms in a population with treatment-resistant depression: A FACE-DR study. J Affect Disord. (2024) 347:306–13. doi: 10.1016/j.jad.2023.11.063
7. Conner KR, Bagge CL. Suicidal behavior. Alcohol Res Curr Rev. (2019) 40:arcr.v40.1.02. doi: 10.35946/arcr.v40.1.02
8. Giesbrecht N, Farkouh EK, Pavalaghanthan H, Orpana H. Prevention of alcohol-related suicide: a rapid review. Drugs Educ Prev Policy. (2024) 31:1–26. doi: 10.1080/09687637.2022.2114877
9. Brady J. The association between alcohol misuse and suicidal behaviour. Alcohol Alcohol Oxf Oxfs. (2006) 41:473–8. doi: 10.1093/alcalc/agl060
10. Rizk MM, Herzog S, Dugad S, Stanley B. Suicide risk and addiction: the impact of alcohol and opioid use disorders. Curr Addict Rep. (2021) 8:194–207. doi: 10.1007/s40429-021-00361-z
11. Uhl GR, Koob GF, Cable J. The neurobiology of addiction. Ann N Y Acad Sci. (2019) 1451:5–28. doi: 10.1111/nyas.13989
12. Xie JY, Li RH, Yuan W, Du J, Zhou DS, Cheng YQ, et al. Advances in neuroimaging studies of alcohol use disorder (AUD). Psychoradiology. (2022) 2:146–55. doi: 10.1093/psyrad/kkac018
13. Shields CN, Gremel CM. Orbitofrontal cortex in alcohol dependence: A disrupted cognitive map? Alcohol Clin Exp Res. (2020) 44:1952–64. doi: 10.1111/acer.14441
14. Benedetti F, Radaelli D, Poletti S, Locatelli C, Falini A, Colombo C, et al. Opposite effects of suicidality and lithium on gray matter volumes in bipolar depression. J Affect Disord. (2011) 135:139–47. doi: 10.1016/j.jad.2011.07.006
15. Schmaal L, van Harmelen AL, Chatzi V, Lippard ETC, Toenders YJ, Averill LA, et al. Imaging suicidal thoughts and behaviors: a comprehensive review of 2 decades of neuroimaging studies. Mol Psychiatry. (2020) 25:408–27. doi: 10.1038/s41380-019-0587-x
16. Wagner G, Schultz CC, Koch K, Schachtzabel C, Sauer H, Schlösser RG. Prefrontal cortical thickness in depressed patients with high-risk for suicidal behavior. J Psychiatr Res. (2012) 46:1449–55. doi: 10.1016/j.jpsychires.2012.07.013
17. Gerhardt S, Berhe O, Moessnang C, Horning M, Kiefer F, Tost H, et al. Lack of amygdala habituation to negative emotional faces in alcohol use disorder and the relation to adverse childhood experiences. Addict Biol. (2023) 28:e13251. doi: 10.1111/adb.13251
18. Tomasi D, Wiers CE, Manza P, Shokri-Kojori E, Michele-Vera Y, Zhang R, et al. Accelerated aging of the amygdala in alcohol use disorders: relevance to the dark side of addiction. Cereb Cortex. (2021) 31:3254–65. doi: 10.1093/cercor/bhab006
19. Harenski CL, Harenski KA, Calhoun VD, Kiehl KA. Source-based morphometry reveals gray matter differences related to suicidal behavior in criminal offenders. Brain Imaging Behav. (2018) 14(1):1–9. doi: 10.1007/s11682-018-9957-2
20. Huang Y, Mohan A, De Ridder D, Sunaert S, Vanneste S. The neural correlates of the unified percept of alcohol-related craving: a fMRI and EEG study. Sci Rep. (2018) 8:923. doi: 10.1038/s41598-017-18471-y
21. Bracht T, Soravia L, Moggi F, Stein M, Grieder M, Federspiel A, et al. The role of the orbitofrontal cortex and the nucleus accumbens for craving in alcohol use disorder. Transl Psychiatry. (2021) 11:1–10. doi: 10.1038/s41398-021-01384-w
22. Boutte D, Calhoun VD, Chen J, Sabbineni A, Hutchison K, Liu J. Association of genetic copy number variations at 11 q14.2 with brain regional volume differences in an alcohol use disorder population. Alcohol Fayettev N. (2012) 46:519–27. doi: 10.1016/j.alcohol.2012.05.002
23. Sullivan EV, Deshmukh A, De Rosa E, Rosenbloom MJ, Pfefferbaum A. Striatal and forebrain nuclei volumes: contribution to motor function and working memory deficits in alcoholism. Biol Psychiatry. (2005) 57:768–76. doi: 10.1016/j.biopsych.2004.12.012
24. Zahr NM, Pfefferbaum A. Alcohol’s effects on the brain: neuroimaging results in humans and animal models. Alcohol Res Curr Rev. (2017) 38:183–206.
25. Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. (2016) 3:760–73. doi: 10.1016/S2215-0366(16)00104-8
26. Malhi GS, Das P, Outhred T, Gessler D, John Mann J, Bryant R. Cognitive and emotional impairments underpinning suicidal activity in patients with mood disorders: an fMRI study. Acta Psychiatr Scand. (2019) 139:454–63. doi: 10.1111/acps.13022
27. Ho TC, Cichocki AC, Gifuni AJ, Catalina Camacho M, Ordaz SJ, Singh MK, et al. Reduced dorsal striatal gray matter volume predicts implicit suicidal ideation in adolescents. Soc Cognit Affect Neurosci. (2018) 13:1215–24. doi: 10.1093/scan/nsy089
28. Rogers ML, Joiner TE. Rumination, suicidal ideation, and suicide attempts: A meta-analytic review. Rev Gen Psychol. (2017) 21:132–42. doi: 10.1037/gpr0000101
29. Tang H, Xiong T, Shi J, Chen Y, Liu X, Zhang S, et al. Global and reflective rumination are related to suicide attempts among patients experiencing major depressive episodes. BMC Psychiatry. (2021) 21:117. doi: 10.1186/s12888-021-03119-z
30. Larionow P, Preece DA, Mudło-Głagolska K. Psychometric properties of the polish version of the perth emotional reactivity scale. Int J Cognit Ther. (2023) 16:460–78. doi: 10.1007/s41811-023-00172-2
31. Yalvaç EBK, Gaynor K. Emotional dysregulation in adults: The influence of rumination and negative secondary appraisals of emotion. J Affect Disord. (2021) 282:656–61. doi: 10.1016/j.jad.2020.12.194
32. Zoccola PM, Dickerson SS, Zaldivar FP. Rumination and cortisol responses to laboratory stressors. Psychosom Med. (2008) 70:661–7. doi: 10.1097/PSY.0b013e31817bbc77
33. Zoccola PM, Dickerson SS. Assessing the relationship between rumination and cortisol: A review. J Psychosom Res. (2012) 73:1–9. doi: 10.1016/j.jpsychores.2012.03.007
34. Ottaviani C, Shapiro D, Fitzgerald L. Rumination in the laboratory: what happens when you go back to everyday life? Psychophysiology. (2011) 48:453–61. doi: 10.1111/j.1469-8986.2010.01122.x
35. Sin ELL, Shao R, Geng X, Cho V, Lee TMC. The neuroanatomical basis of two subcomponents of rumination: A VBM study. Front Hum Neurosci. (2018) 12:324. doi: 10.3389/fnhum.2018.00324
36. Zhou HX, Chen X, Shen YQ, Li L, Chen NX, Zhu ZC, et al. Rumination and the default mode network: Meta-analysis of brain imaging studies and implications for depression. NeuroImage. (2020) 206:116287. doi: 10.1016/j.neuroimage.2019.116287
37. Bravo AJ, Pilatti A, Pearson MR, Mezquita L, Ibáñez MI, Ortet G. Depressive symptoms, ruminative thinking, drinking motives, and alcohol outcomes: A multiple mediation model among college students in three countries. Addict Behav. (2018) 76:319–27. doi: 10.1016/j.addbeh.2017.08.028
38. Caselli G, Ferretti C, Leoni M, Rebecchi D, Rovetto F, Spada MM. Rumination as a predictor of drinking behaviour in alcohol abusers: a prospective study. Addiction. (2010) 105:1041–8. doi: 10.1111/j.1360-0443.2010.02912.x
39. Felton JW, Havewala M, Myerberg L, Lee J, Collado A. Rumination and Co-Rumination and their Associations with Alcohol-Related Problems and Depressive Symptoms among College Students. J Ration-Emotive Cogn-Behav Ther. (2022) 40:388–405. doi: 10.1007/s10942-021-00418-y
40. Vilus B, Perich T. The relationship between rumination, depression and self-stigma in hazardous drinkers: an exploratory study. Discovery Psychol. (2021) 1:6. doi: 10.1007/s44202-021-00006-2
41. Rogers ML, Jeon ME, Duffy ME, Joiner TE. Thinking too much: Rumination as a catalyst of the real-time associations between affective states and suicidal ideation. J Consult Clin Psychol. (2022) 90:670–81. doi: 10.1037/ccp0000753
42. Holdaway AS, Luebbe AM, Becker SP. Rumination in relation to suicide risk, ideation, and attempts: exacerbation by poor sleep quality? J Affect Disord. (2018) 236:6–13. doi: 10.1016/j.jad.2018.04.087
43. Teismann T, Forkmann T. Rumination, entrapment and suicide ideation: A mediational model. Clin Psychol Psychother. (2017) 24:226–34. doi: 10.1002/cpp.1999
44. Hensel LM, Forkmann T, Teismann T. Suicide-specific rumination as a predictor of suicide planning and intent. Behav Res Ther. (2024) 180:104597. doi: 10.1016/j.brat.2024.104597
45. Teismann T, Forkmann T, Michalak J, Brailovskaia J. Repetitive negative thinking about suicide: associations with lifetime suicide attempts. Clin Psychol Eur. (2021) 3:1–14. doi: 10.32872/cpe.5579
46. Hilt LM, Pollak SD. Getting out of rumination: comparison of three brief interventions in a sample of youth. J Abnorm Child Psychol. (2012) 40:1157–65. doi: 10.1007/s10802-012-9638-3
47. Somers JA, Borelli JL, Hilt LM. Depressive symptoms, rumination, and emotion reactivity among youth: moderation by gender. J Clin Child Adolesc Psychol. (2020) 49:106–17. doi: 10.1080/15374416.2018.1466304
48. Hilt LM, Aldao A, Fischer K. Rumination and multi-modal emotional reactivity. Cognit Emot. (2015) 29:1486–95. doi: 10.1080/02699931.2014.989816
49. Wang L, Cui Q, Liu J, Zou H. Emotion reactivity and suicide risk in patients with depression: the mediating role of non-suicidal self-injury and moderating role of childhood neglect. Front Psychiatry. (2021) 12:707181. doi: 10.3389/fpsyt.2021.707181
50. Klonsky ED, Victor SE, Hibbert AS, Hajcak G. The multidimensional emotion questionnaire (MEQ): rationale and initial psychometric properties. J Psychopathol Behav Assess. (2019) 41:409–24. doi: 10.1007/s10862-019-09741-2
51. Nock MK, Wedig MM, Holmberg EB, Hooley JM. The emotion reactivity scale: development, evaluation, and relation to self-injurious thoughts and behaviors. Behav Ther. (2008) 39:107–16. doi: 10.1016/j.beth.2007.05.005
52. Fitzgerald JM, Phan KL, Kennedy AE, Shankman SA, Langenecker SA, Klumpp H. Prefrontal and amygdala engagement during emotional reactivity and regulation in generalized anxiety disorder. J Affect Disord. (2017) 218:398–406. doi: 10.1016/j.jad.2017.05.013
53. Kõlves K, Chitty KM, Wardhani R, Värnik A, de Leo D, Witt K. Impact of alcohol policies on suicidal behavior: A systematic literature review. Int J Environ Res Public Health. (2020) 17:7030. doi: 10.3390/ijerph17197030
54. DiPierro-Sutton M, Poquiz J, Brown S, Fite P, Bortolato M. Models predicting the role of emotion reactivity in the link between reasons for not using and lifetime substance use. J Am Coll Health. (2022) 70:527–35. doi: 10.1080/07448481.2020.1756828
55. Gottfredson NC, Hussong AM. Drinking to dampen affect variability: findings from a college student sample. J Stud Alcohol Drugs. (2013) 74:576–83. doi: 10.15288/jsad.2013.74.576
56. Klonsky ED, Pachkowski MC, Shahnaz A, May AM. The three-step theory of suicide: Description, evidence, and some useful points of clarification. Prev Med. (2021) 152:106549. doi: 10.1016/j.ypmed.2021.106549
57. O’Connor RC, Kirtley OJ. The integrated motivational–volitional model of suicidal behaviour. Philos Trans R Soc B Biol Sci. (2018) 373:20170268. doi: 10.1098/rstb.2017.0268
58. Polanco-Roman L, Moore A, Tsypes A, Jacobson C, Miranda R. Emotion reactivity, comfort expressing emotions, and future suicidal ideation in emerging adults. J Clin Psychol. (2018) 74:123–35. doi: 10.1002/jclp.22486
59. Shapero BG, Farabaugh A, TereChina O, DeCross S, Cheung JC, Fava M, et al. Understanding the effects of emotional reactivity on depression and suicidal thoughts and behaviors: Moderating effects of childhood adversity and resilience. J Affect Disord. (2019) 245:419–27. doi: 10.1016/j.jad.2018.11.033
60. Denning DM, Perry TR, Reilly EE, Berner LA, Velkoff EA, Kaye WH, et al. Associations of suicide risk with emotional reactivity, dysregulation, and eating disorder treatment outcomes. Suicide Life Threat Behav. (2022) 52:1126–39. doi: 10.1111/sltb.12907
61. Organization WH. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization (1992). p. 377.
62. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addict Abingdon Engl. (1993) 88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
63. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
64. Nezlek JB, Rusanowska M, Holas P, Krejtz I. The factor structure of a Polish language version of the hospital anxiety depression scale (HADS). Curr Psychol. (2021) 40:2318–26. doi: 10.1007/s12144-019-0164-0
65. Garnefski N, Kraaij V. The cognitive emotion regulation questionnaire. Eur J Psychol Assess. (2007) 23:141–9. doi: 10.1027/1015-5759.23.3.141
66. Marszał-Wiśniewska M, Fajkowska M. Właściwości psychometryczne kwestionariusza poznawczej regulacji emocji (Cognitive emotion regulation questionnaire; CERQ). Stud Psychol. (2010) 49:19–39.
67. Becerra R, Preece D, Campitelli G, Scott-Pillow G. The assessment of emotional reactivity across negative and positive emotions: development and validation of the perth emotional reactivity scale (PERS). Assessment. (2019) 26:867–79. doi: 10.1177/1073191117694455
68. Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. (2001) 8:443–54. doi: 10.1177/107319110100800409
69. Chodkiewicz J, Gruszczyńska E. Polska adaptacja Zrewidowanego Kwestionariusza Zachowań Samobójczych A. Osmana i współpracowników. Psychiatr Pol. (2020) 54:101–11. doi: 10.12740/PP/OnlineFirst/93492
70. Hryniewicz K, Milewska A. SZTOS: System Zautomatyzowanego Tworzenia Opisu Statystycznego (Wersja SZTOS) [software] (2023). Retrieved from https://sztos-it.com/.
71. Fox J, Weisberg S. An R companion to applied regression. SAGE Publications Inc (2019). Available at: https://us.sagepub.com/en-us/nam/an-r-companion-to-applied-regression/book246125.
72. Stekhoven DJ, Bühlmann P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinforma Oxf Engl. (2012) 28:112–8. doi: 10.1093/bioinformatics/btr597
74. Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Software. (2012) 48:1–36. doi: 10.18637/jss.v048.i02
75. Lai K. Estimating standardized SEM parameters given nonnormal data and incorrect model: methods and comparison. Struct Equ Model Multidiscip J. (2018) 25:600–20. doi: 10.1080/10705511.2017.1392248
76. Pastore M, Gianmarco A. influence.SEM: case influence in structural equation models (2022). Available online at: https://cran.r-project.org/web/packages/influence.SEM/index.html (Accessed October 13, 2022).
77. Robinette JW, Charles ST. Age, rumination, and emotional recovery from a psychosocial stressor. J Gerontol B Psychol Sci Soc Sci. (2016) 71:265–74. doi: 10.1093/geronb/gbu097
78. Kopera M, Zaorska J, Trucco EM, Suszek H, Kobyliński P, Zucker RA, et al. Childhood trauma, alexithymia, and mental states recognition among individuals with alcohol use disorder and healthy controls. Drug Alcohol Depend. (2020) 217:108301. doi: 10.1016/j.drugalcdep.2020.108301
79. Perez J, Beale E, Overholser J, Athey A, Stockmeier C. Depression and alcohol use disorders as precursors to death by suicide. Death Stud. (2022) 46:619–27. doi: 10.1080/07481187.2020.1745954
80. Carton L, Pignon B, Baguet A, Benradia I, Roelandt JL, Vaiva G, et al. Influence of comorbid alcohol use disorders on the clinical patterns of major depressive disorder: A general population-based study. Drug Alcohol Depend. (2018) 187:40–7. doi: 10.1016/j.drugalcdep.2018.02.009
81. Phillips JA, Hempstead K. Differences in U.S. Suicide rates by educational attainment, 2000–2014. Am J Prev Med. (2017) 53:e123–30. doi: 10.1016/j.amepre.2017.04.010
82. Polanco-Roman L, Gomez J, Miranda R, Jeglic E. Stress-related symptoms and suicidal ideation: The roles of rumination and depressive symptoms vary by gender. Cognit Ther Res. (2016) 40:606–16. doi: 10.1007/s10608-016-9782-0
83. Rosario-Williams B, Miranda R. Prospective relation between ruminative subtypes and suicide ideation: moderating role of problem solving. Cognit Ther Res. (2023) 47:574–86. doi: 10.1007/s10608-023-10373-w
84. Valderrama J, Miranda R, Jeglic E. Ruminative subtypes and impulsivity in risk for suicidal behavior. Psychiatry Res. (2016) 236:15–21. doi: 10.1016/j.psychres.2016.01.008
85. Horwitz AG, Czyz EK, Berona J, King CA. Rumination, brooding, and reflection: prospective associations with suicide ideation and suicide attempts. Suicide Life Threat Behav. (2019) 49:1085–93. doi: 10.1111/sltb.12507
86. Liu S, You J, Ying J, Li X, Shi Q. Emotion reactivity, nonsuicidal self-injury, and regulatory emotional self-efficacy: A moderated mediation model of suicide ideation. J Affect Disord. (2020) 266:82–9. doi: 10.1016/j.jad.2020.01.083
87. Nolen-Hoeksema S, Harrell ZA. Rumination, depression, and alcohol use: tests of gender differences. J Cognit Psychother. (2002) 16:391–403. doi: 10.1891/jcop.16.4.391.52526
88. Fox HC, Hong KA, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addict Behav. (2008) 33:388–94. doi: 10.1016/j.addbeh.2007.10.002
89. Watkins ER, Roberts H. Reflecting on rumination: Consequences, causes, mechanisms and treatment of rumination. Behav Res Ther. (2020) 127:103573. doi: 10.1016/j.brat.2020.103573
90. Langenecker SA, Westlund Schreiner M, Bessette KL, Roberts H, Thomas L, Dillahunt A, et al. Rumination-focused cognitive behavioral therapy reduces rumination and targeted cross-network connectivity in youth with a history of depression: replication in a preregistered randomized clinical trial. Biol Psychiatry Glob Open Sci. (2024) 4:1–10. doi: 10.1016/j.bpsgos.2023.08.012
91. Zhang B, Fu W, Guo Y, Chen Y, Jiang C, Li X, et al. Effectiveness of mindfulness-based cognitive therapy against suicidal ideation in patients with depression: A systematic review and meta-analysis. J Affect Disord. (2022) 319:655–62. doi: 10.1016/j.jad.2022.09.091
92. Joubert AE, Grierson AB, Li I, Sharrock MJ, Moulds ML, Werner-Seidler A, et al. Managing Rumination and worry: A randomised controlled trial of an internet intervention targeting repetitive negative thinking delivered with and without clinician guidance. Behav Res Ther. (2023) 168:104378. doi: 10.1016/j.brat.2023.104378
93. Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of Mindfulness-Based Stress Reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: a waitlist-controlled study. J Behav Med. (2012) 35:262–71. doi: 10.1007/s10865-011-9357-1
94. Rittmannsberger H. Amisulpride as an augmentation agent in treatment resistant depression: A case series and review of the literature. Psychiatr Danub. (2019) 31:148–56. doi: 10.24869/psyd.2019.148
95. Hou YC, Lai CH. Aripiprazole monotherapy can relieve ruminations in a case with nonpsychotic depression. J Neuropsychiatry Clin Neurosci. (2014) 26:E32–33. doi: 10.1176/appi.neuropsych.13100324
96. Lee Y, Kang NI, Lee KH, Piao Y, Cui Y, Kim SW, et al. Effects of antipsychotics on rumination in patients with first-episode psychosis. Prog Neuropsychopharmacol Biol Psychiatry. (2020) 103:109983. doi: 10.1016/j.pnpbp.2020.109983
97. Blanke ES, Brose A, Kalokerinos EK, Erbas Y, Riediger M, Kuppens P. Mix it to fix it: Emotion regulation variability in daily life. Emotion. (2020) 20:473–85. doi: 10.1037/emo0000566
Keywords: alcohol use disorder, ruminations, emotional reactivity, suicide risk, negative affect
Citation: Wojtczak M, Karasiewicz K and Kucharska K (2025) A moderated mediation model in assessing links between rumination, emotional reactivity, and suicidal risk in alcohol use disorder. Front. Psychiatry 16:1479827. doi: 10.3389/fpsyt.2025.1479827
Received: 12 August 2024; Accepted: 13 February 2025;
Published: 28 February 2025.
Edited by:
Matthew J. Hoptman, Nathan S. Kline Institute for Psychiatric Research, United StatesReviewed by:
Naseem Akhtar Qureshi, Al-Falah University, IndiaCopyright © 2025 Wojtczak, Karasiewicz and Kucharska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mateusz Wojtczak, bXQud29qdGN6YWtAc3R1ZGVudC51a3N3LmVkdS5wbA==; Karol Karasiewicz, S2FyYXNpZXdpY3pLYXJvbEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.