
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 28 February 2025
Sec. Public Mental Health
Volume 16 - 2025 | https://doi.org/10.3389/fpsyt.2025.1478690
This article is part of the Research TopicCommunity Series In Mental-Health-Related Stigma and Discrimination: Prevention, Role, and Management Strategies, Volume IIIView all 19 articles
 Weiwei Wang1
Weiwei Wang1 Junhong Xia1
Junhong Xia1 Wei Chen2
Wei Chen2 Junhua Ye1
Junhua Ye1 Kun Xie1
Kun Xie1 Zhuona Zhang1
Zhuona Zhang1 Siti Mardhiana Binti Mohamad2
Siti Mardhiana Binti Mohamad2 Ahmad Naqib Shuid2*
Ahmad Naqib Shuid2*Background: Stigma related to mental health conditions has a negative impact on both the nursing staff and their patients. Most of the current research on stigma explores the impact of single factors on stigma and does not explore the relationship between knowledge, social distance and stigma among clinical nurses.
Methods: A convenience sampling method was used to conduct a questionnaire survey among 628 nurses from five hospitals in Liaoning Province in March 2021 and June 2021 using a combination of online and offline methods. To study the negative attitudes toward patients with mental illness among clinical nurses and to analyze the relationship between mental ill health stigma, social distancing, and mental health knowledge among nurses. The questionnaire includes Sociodemographic data, Scale for Assessing the Stigma of Mental Illness in Nursing (score range: 20~100, the higher the score, the less stigma attached to mental ill health), Mental Illness Social Distance Scale (score range: 6~30, the higher the score, the greater the social distance) and Mental Health and Mental Health Knowledge Questionnaire (score range: 0~25, the higher the score, the higher the knowledge level).
Results: The nurses’ mental ill health stigma score was 58.96 ± 9.38 points, the mean scores of psychiatric and general nurses were 58.86 ± 9.33 and 59.41 ± 9.58 points, respectively. Willingness to become a psychiatric nurse is a factor influencing the stigma of mental illness. The stigma of mental ill health, social distance and mental health knowledge of nurses are positively correlated (P<0.01). The mediation analysis demonstrated that mental health stigma significantly mediated the relationship between mental health knowledge and social distance (a= 0.599, P<0.001; b= -0.194, P<0.001). After accounting for stigma, the direct effect of mental health knowledge on social distance was no longer significant (c’=-0.007, P=0.078), highlighting the central role of stigma in this relationship.
Conclusions: Nurses mental ill health stigma is moderate and is the main mediating effect between mental health knowledge and social distancing. The pivotal role of mental health knowledge in shaping nurses’ attitudes and behaviors pertaining to social distancing in the context of mental illness. By combating stigma and enhancing mental health literacy among healthcare practitioners, we can foster environments that promote inclusive and compassionate care practices, thereby ameliorating patient outcomes and redressing disparities in mental health treatment.
Approximately 1 in every 8 people globally, or 970 million individuals, live with a mental ill health, a number that has increased due to greater awareness and improved mental ill health diagnostics (1). According to WMH surveys in 29 countries, it is estimated that approximately one in two people will suffer from at least one mental disorder by the age of 75 (2). The growing number of people with a mental health condition also imposes a significant burden on the economy, projected to rise to $6 trillion per year by 2030 (3). The Global Burden of Disease study highlights that mental ill health have been a significant contributor to the global burden of disease over the past 30 years (4). Low-and middle-income countries account for about three-quarters of the global burden of mental ill health. As a middle-income country, disability-adjusted life years (DALY) due to mental, neurological and substance use disorders in China account for about 15% to 20% of the global total, ranking first in the world (5). Such figures underscore the urgent need for targeted interventions to address the growing public health and socio-economic challenges posed by mental ill health.
The global ramifications of mental health disorders are particularly evident in China, where the convergence of a substantial population and an increasing prevalence of mental health issues poses significant public health and socio-economic challenges. Mental health represents a critical public health concern in China, characterized by a substantial patient population and considerable socio-economic burdens. Studies have indicated that in 2018, around 150 million people in China were affected by various mental ill health, with an incidence rate of approximately 17.5% (6). In 2021, the number of registered people with a severe mental ill health rose to 6.6 million (7). As of 2023, the China Mental Health Survey shows that the lifetime prevalence of mental ill health in China is about 16.6% (8), which means that about 230 million people will suffer from mental ill health in their lifetime. This growing burden places tremendous pressure on healthcare systems, particularly on nurses, who play a frontline role in providing care to people with a mental health condition. However, nursing stigma toward mental ill health remains a significant barrier to effective care. Thornicroft has stated, “In no country, society, or culture do people with a mental health condition receive the same acceptance and recognition as others” (9). The specific manifestations of mental ill health (10) often lead to these individuals being stigmatized as “different.” Nurses may also harbor discriminatory attitudes toward these patients, perceiving them as incompetent, unpredictable, destructive, and violent (11, 12). This discrimination can lead to a decline in care quality, hindering patient recovery and therapeutic outcomes. For clinical nurses, such stigma can negatively impact their professional identity and social interactions (13), posing significant barriers to their involvement in psychiatric nursing (14) and hindering the discipline’s development (15).
Stigmatization affects patients by diminishing their empowerment, social inclusion, quality of life, willingness to seek help, and compliance with treatment (16). It exacerbates clinical symptoms, disrupts treatment, and damages job prospects and social relationships, leading to social isolation and involuntary medical behaviors, imposing heavy physical and mental burdens on patients and their families (17). Goffman (18), a key figure in stigma research, defined stigma as a socially constructed phenomenon where societal norms discredit an individual’s identity. He highlighted its dynamic nature and how stigmatized individuals manage their “spoiled identity.” The most widely accepted perspective today, proposed by Rusch et al. (19) conceptualizes stigma as involving stereotype (cognitive level), prejudice (emotional level), and discrimination (behavioral level). Stigma is socially constructed and manifests as exclusion, blame, or demeaning behaviors due to expected adverse social judgments (20). This social construction affects intellectual, emotional, and behavioral dimensions. Numerous studies have explored the link between knowledge and mental illness stigma, with desired social distance being a key behavioral response indicator. This measure reflects the degree of closeness or distancing that individuals hypothesize or desire in relation to others, serving as a proxy for group attitudes and social behaviors (21). When individuals endorse negative stereotypes about mental ill health, they exhibit prejudice and negative emotional reactions, leading to discrimination and exclusion of the stigmatized group, impacting social interactions. This phenomenon has been observed in China, where mental ill health has historically faced cultural and moral stigma (22). Studies indicate that people maintain greater social distance from stigmatized groups and seldom engage with them, aggravating public stigmatization (23, 24). When stigmatized individuals are aware of societal stigma, it increases social distance, forming a vicious cycle (25). This issue is also present among medical staff, as mental health workers often maintain significant social distance from patients and reject them (26).
Most existing studies focus on public discrimination against people with a mental health condition, with few addressing exclusionary behaviors and social distancing among nurses. According to the “Knowledge-Attitude-Practice model,” knowledge is crucial in reducing in-group bias against out-group members (27). Knowledge is also pivotal in combating mental health-related stigma (28, 29). Improving public mental health literacy can reduce stigmatizing attitudes (30). A systematic review of 515 studies identified knowledge as a key factor in reducing out-group bias (31). However, some studies reveal that while nurses possess good knowledge of mental ill health, their attitudes remain negative (32).
Currently, most stigma studies focus on people with mental health condition or their families, with limited research on nurses stigmatization. Qualitative studies suggest that stigma among nurses stems from attitudinal knowledge and behavior (33). However, quantitative research supporting these findings remains limited, and existing studies have yet to fully explore the nuanced relationship between knowledge, behavior, and stigma. This study aims to examine the correlation among mental health knowledge, social distance, and stigma among nurses, with the goals to (1) investigate the current state of mental ill health stigma among nurses and analyze its influencing factors, and (2) explore the mediating effects of stigma on the relationship between mental health knowledge and social distancing among clinical nurses.
In order to capture different perspectives in the nursing industry and effectively collect data from different levels and regions, this study used convenience sampling to select nurses who volunteered to participate in this study from five hospitals in Jinzhou and Dalian, Liaoning Province. 1) Affiliated Hospital of Jinzhou Medical University; 2) Jinzhou Kangning Hospital; 3) Wafangdian Central Hospital; 4) Wafangdian city women and Children’s Hospital and 5) Wafangdian city fourth hospital between March 2021 and June 2021. A total of 657 questionnaires were distributed, all of which were recovered. Among them, 628 were deemed valid, resulting in an effective recovery rate of 95.59%.
Inclusion criteria: 1) possess a nursing qualification certificate 2) volunteers for the study.
Exclusion criteria: 1) currently on vacation 2) Non-clinical frontline work.
This study used an online and offline method to collect data. Before distributing the questionnaire, the purpose and significance of the questionnaire were explained to the nurses, and the precautions for filling in the questionnaire were informed. After obtaining the consent of the nurses, the questionnaires were distributed to the nurses on site, and the nurses completed the questionnaires independently. The time for filling in the questionnaire was 5 to 10 minutes. After the questionnaires were completed, they were collected on the spot to check whether there were any omissions or errors. The nurses confirmed and modified them in time to ensure the integrity and quality of the questionnaires. The scales selected in this study have good reliability and validity, which can ensure the accuracy of the measurement. The researcher herself was responsible for the distribution and collection of the questionnaires, ensuring that the questionnaires were filled in within the specified time and independence during the filling process. In the process of collecting the questionnaires, the integrity of the questionnaires was checked, and the missing options were communicated and checked with the research subjects in time to ensure the integrity of the questionnaires. After the questionnaires were collected, the quality of the questionnaires was checked, and the questionnaires with a completion rate of less than 80% were deleted to ensure the scientific nature of the research. When entering the data, two people checked, and if there were any differences, the original data was found in time for verification to ensure the accuracy of the data.
The sociodemographic questionnaire included items on sex, age, education level, monthly income, level of interaction with mental health patients, exposure to mental health education, and willingness to specialize in psychiatric nursing.
The Scale for Assessing the Stigma of Mental Illness in Nursing (SASMIN) was developed in 2020 by Spanish scholar Dr. Meritxell based on the Peplau psychodynamic nursing model (34). A total of 20 items in 3 dimensions are scored on a 5-point Likert scale: 1 is completely disagree, and 5 is completely agree. They included Violence/Dangerousness (8 items), Disability (5 items), Irresponsibility and Lack of Competence (7 items). Items 2, 3, 5, 10, 13 and 15 are scored directly, and the rest are scored in reverse. The higher the score, the less stigma attached to mental ill health. The intragroup correlation coefficient was 0.906, and the Cronbach’s α coefficient was 0.825. In 2021, the Chinese version of the Scale for Assessing the Stigma of Mental Illness in Nursing was developed by myself and my research team (35), and its reliability and validity were tested. The results showed that the ICC value of the total table was 0.760, the retest reliability was 0.839, and the Cronbach’s α was 0.863, indicating good reliability and validity. In this study, the Cronbach’s α coefficient of this scale was 0.856, and the retest reliability was 0.884, indicating good reliability and validity.
The Mental Health and Mental Health Knowledge Questionnaire is one of the questionnaires on the investigation and evaluation of mental health work issued by the China Health and Family Planning Commission (former General Office of the Ministry of Health) in 2010 (36). The content of the questionnaire is basic knowledge of mental health. The higher the total score is, the better the mental health knowledge. According to the National Mental Health Work Plan (2015–2020) (37), the awareness rate of mental health knowledge of the urban general population should reach 70%, that of the rural population should reach 50% and that of school students should reach 80% in 2020.The questionnaire aligns with national mental health education goals.
American scholar Link (38) compiled a Social Distance Scale for mental illness, which was used to evaluate the degree of public rejection of people with a mental health condition. The theory is that the more biased people are against a social group, the less willing they are to associate with members of that group. The single-dimension, six-item scale includes living in the same community as a mentally ill person, being a neighbor of a mentally ill person, working with a mentally ill person, communicating with a mentally ill person on a daily basis, being a friend of a mentally ill person, and being a spouse of a mentally ill person. The Likert 5-point scoring method is adopted, and the answer of each item is the degree (out of 5) of willingness of the respondent, namely, “very willing, willing, neutral, unwilling, very unwilling”, recorded as 1 to 5 points, respectively. The cumulative score of the 6 items is the total social distance score, and the higher the score is, the greater the social distance between the individual and the external group. In this study, the intragroup correlation coefficient of this scale was 0.901, and the Cronbach’s α coefficient was 0.883, showing good reliability and validity.
Epidata Entry Mac version 13.0 was used for data entry and data documentation, SPSS for Mac version 26.0 was used for statistical analysis, and Sociodemographic data and stigma assessment scores, social distance scores, and mental health knowledge scores were statistically analyzed using the mean, standard deviation, frequency and component ratio. The Z-score was used to standardize and classify the stigma scores to explain the variability within the sample. T-test was used for comparison between two groups, one-way ANOVA was used for comparison of multiple groups, and multiple linear regression was used for analysis of influencing factors. Pearson’s two-tailed test was used to analyze the relationship between social distance from mental ill health, mental health and mental health knowledge among clinical nurses. To explore the mediating effect of social distance between mental health knowledge and stigma of mental ill health, the process bootstrap method was used, with a=0.05 as the test criterion.
Ethical approval will be obtained from the Institutional Review Board (IRB) or relevant ethics committee prior to data collection. Informed consent will be obtained from all participants, and steps will be taken to ensure the confidentiality and anonymity of their responses. Participants will be informed of their right to withdraw from the study at any time without consequences.
The study involved 628 nurses, consisting of 589 females (93.79%) and 39 males (7.21%). Regarding age distribution, young adults aged 20 to 39 comprised 77.1%, those aged 40 to 49 comprised 20.4%, and those aged 50 or older made up only 2.5%. The univariate analysis results indicate that, among sociodemographic factors, the willingness to become a psychiatric nurse is a significant factor influencing nurses’ stigma toward mental illness (P<0.0001). Further details can be found in Table 1.
The Scale for Assessing the Stigma of Mental Illness in Nursing yielded total scores of 58.96 ± 9.38 points for nurses, 58.86 ± 9.33 points for general nurses, and 59.41 ± 9.58 points for psychiatric nurses. Specifically, the scores for violence and danger were 22.68 ± 5.71 points, for ability deficiency were 14.64 ± 3.54 points, and for irresponsibility and lack of ability were 21.64 ± 3.83 points (refer to Table 2 for specifics). To evaluate nurses’ levels of mental ill health stigma, the total stigma score for each subject was converted to a Z score. Stigma levels were categorized into four tiers: no stigma, mild stigma, moderate stigma, and severe stigma. With an average Z value of 0 and a general range of -3 to 3, a Z score below -1.5 indicated severe stigma, -1.5 to 0 indicated moderate stigma, 0 to 1.5 indicated mild stigma, and above 1.5 indicated no stigma. The analysis revealed that out of the sample, 69 cases (10.99%) exhibited no stigma, 281 cases (43.47%) showed mild stigma, 248 cases (39.49%) had moderate stigma, and 38 cases (6.05%) displayed severe stigma (refer to Table 3 for detailed breakdown).
According to Pearson correlation analysis, the mental ill health stigma score of the nursing staff was negatively correlated with social distance (P<0.0001), negatively correlated with mental health knowledge (P<0.0001), and positively correlated with social distance and mental health knowledge (P<0.01). That is, the degree of mental illness stigma of nursing staff is positively correlated with social distance, and the degree of mental illness stigma is negatively correlated with mental health knowledge. All three are correlated; therefore, this information can be used to analyze the mediating effect. For detailed statistics, please refer to Table 4.
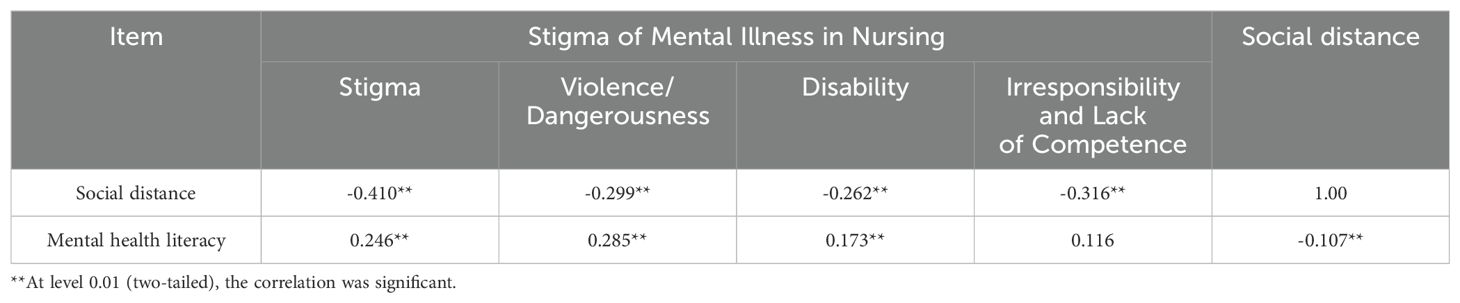
Table 4. Correlation of mental illness stigma, social distancing and mental health knowledge among caregivers.
Structural equation modeling (SEM) was used to test complex relationships between multiple variables simultaneously, including direct and indirect effects. Utilizing the theoretical framework of Knowledge-Attitude-Practice Model, a structural equation modeling was constructed, where mental health knowledge served as the independent variable (X), social distance from mental ill health as the dependent variable (Y), and stigma of mental ill health among nurses as the mediating variable (M), while controlling for sex, age, and education level. The findings revealed significant paths: a=0.599 ((P<0.0001)), b=-0.194 ((P<0.0001)), and c’=-0.007 (P=0.078). These results underscore the pivotal role of stigma as the primary mediating factor. Moreover, they indicate that mental health knowledge influences social distance from mental ill health predominantly through the mediation of mental ill health stigma. For comprehensive statistics, please refer to Tables 5, 6.
The findings of this study offer valuable insights into the dynamic interrelationships among mental health knowledge, stigma, and social distance within the cohort of clinical nurses in Liaoning, China. This research underscores the pivotal role that mental health knowledge plays in influencing nurses’ attitudes and behaviors toward individuals with mental illnesses. Importantly, the mediating effect of stigma on the relationship between knowledge and social distance highlights the intricate challenges involved in addressing mental health care disparities in clinical practice. By examining these factors within the nursing profession, the study contributes to an expanding body of evidence that underscores the significance of targeted educational interventions and stigma-reduction strategies. These strategies are essential for enhancing mental health care delivery and promoting a more inclusive clinical environment.
Regarding stigma among clinical nurses, findings from this study indicated an average stigma rating of 58.96 ± 9.38 among nursing staff, with 45.54% (286 cases) from the total sample exhibiting moderate to severe stigma. These results align with those of numerous previous studies (39), indicating a prevalent stigmatized attitude among nursing staff toward individuals with mental illness. Surveys of nursing students (40, 41) revealed similarly negative attitudes toward mental illness. Notably, these attitudes were observed to be more negative in comparison to those documented in a stigma survey involving 192 caregivers, as reported by Jin Xinxia (42). This discrepancy may be attributed to variations in the timing of measurement, given that Jin Xinxia’s study focused on clinical nurses at an earlier stage in their careers. Previous research has indicated that age serves as an independent factor influencing the stigma associated with mental illness among nursing professionals, with younger individuals exhibiting more positive attitudes (43, 44).
Subsequent analyses identified variations in attitudes toward mental illness across different demographic groups. The willingness of nurses to pursue a career in psychiatric nursing can significantly influence the prevalence of mental illness stigma among nursing professionals. Nurses who express a readiness to specialize in psychiatric nursing tend to exhibit lower levels of stigma, a finding corroborated by numerous studies. These studies suggest that an interest in psychiatric nursing is often linked to more positive attitudes and reduced stigma toward mental illness. For example, a study examining the stigmatizing attitudes of nurses and nurse managers toward mental illness found that those who actively supported and assisted patients with mental health conditions exhibited lower levels of stigma (45). This suggests that nurses inclined toward psychiatric nursing roles may have a greater capacity for understanding and empathizing with individuals experiencing mental illness, thereby reducing stigma. Moreover, another study investigated the impact of psychiatric nursing courses on students’ perceptions of mental illness and the field of psychiatric nursing. The results indicated that exposure to psychiatric nursing education significantly reduced negative beliefs about mental illness while fostering more positive attitudes toward psychiatric nursing as a profession (46). These findings highlight the crucial role of education in shaping nurses’ attitudes toward mental health, emphasizing the need for targeted training programs to reduce stigma and enhance mental health care. The results of this study showed that individuals who were willing to become psychiatric nurses usually showed lower stigmatization of mental illness, which may be related to their interest in psychiatric nursing and professional education background. This pathway of action is consistent with the hypothesis of this study. Therefore, further strengthening mental health education and professional training, especially targeted courses and practice opportunities for clinical nurses, may be an effective strategy to reduce stigma, improve nursing quality, and enhance patient outcomes.
Notably, psychiatric nurses demonstrate lower levels of mental health stigma compared to their non-psychiatric counterparts (47). This observation is consistent with the results of this study, although there was no statistically significant difference in the level of stigma between general nurses and psychiatric nurses. These results imply that professional background and roles may play a crucial role in shaping mental illness stigma. The frequent exposure of psychiatric nurses to mental illness cases in their professional environment may contribute to this reduced stigma. Existing quantitative research (48) and qualitative studies (49) support the “contact hypothesis.” However, contradictory evidence exists, such as studies indicating that family caregivers may display high levels of mental stigmatization despite their close interactions with patients. This phenomenon could be attributed to the substantial emotional, psychological, and social stress experienced by family caregivers in their caregiving roles, although the specific mechanisms warrant further investigation.
The results of this study underscore the persistent high degree of mental ill health stigma among nurses, emphasizing the urgency to address, adapt, and ameliorate these stigmatizing attitudes to enhance nursing care quality.
The results of this cross-sectional investigation illuminate the complex interplay between mental health knowledge and social distancing behaviors within the realm of clinical nursing, placing particular emphasis on the intervening role of stigma associated with mental ill health. Employing mediation model analysis and Pearson correlation, our study unveiled a significant correlation between the degree of mental ill health stigma among nurses and both their mental health knowledge and social distancing behaviors. Notably, diminished levels of stigma among clinical nurses were found to correspond with heightened mental health knowledge and closer interpersonal proximity. These findings are in consonance with prior research (50), which echoes the theoretical framework linking knowledge acquisition to belief formation and consequent behavioral change, underlining the critical importance of promoting health literacy to cultivate affirmative attitudes and conduct (51). The theoretical model of Knowledge-Attitude-Practice Model (KAP) (52) is one of the models for changing human health-related behaviors, used to understand and analyze the behavior change process. It divides the change in human behaviors into three continuous processes: acquiring knowledge, generating beliefs and changing behaviors. Knowledge is the foundation, belief is the driving force, and behavior change is the goal. Through learning of knowledge, people acquire health knowledge and skills, form health beliefs and attitudes, and finally promote the creation of healthy behaviors (53). The model provides a structured approach to analyze the interaction among the three and identify gaps in education and intervention needs.
However, studies have also hinted at a discrepancy, indicating that despite possessing extensive mental health knowledge, nurses may still harbor negative attitudes toward mental ill health—a phenomenon observed across various healthcare professions (32, 54). In recent years, mental ill health has gradually received attention from society. Mental health knowledge is now disseminated through multiple channels that provide basic psychological knowledge, but does not go deep enough to encourage society to readily accept people with a mental health condition.
Furthermore, our investigation underscores the nuanced role of stigma in mediating the relationship between mental health knowledge and social distancing behaviors among nurses. While mental health literacy serves as a cornerstone for fostering empathy and comprehension toward people with a mental health condition (55), the presence of stigma may impede the translation of this knowledge into supportive actions. Our findings underscore stigma’s function as a barrier, obstructing nurses’ full engagement in social distancing practices when tending to people with a mental health conditions. This underscores the imperative of addressing stigma within healthcare settings to cultivate environments conducive to equitable and compassionate care provision.
The implications of our findings for nursing practice are profound. Recognizing the influence of mental health knowledge on social distancing behaviors, healthcare institutions can institute targeted educational interventions (56) aimed at augmenting nurses’ comprehension of mental health issues and mitigating stigma. Equipping nurses with training programs (57) focused on fostering empathy, cultural sensitivity, and effective communication skills (58) can empower them to navigate intricate patient interactions with confidence and professionalism, ultimately elevating the caliber of care dispensed.
It’s crucial to stress the significance of providing insights into interventions aimed at enhancing mental health literacy and reducing stigma among clinical nurses. This discussion delves into potential avenues for intervention:
Firstly, implementing targeted education (59) and training programs (60) tailored to the specific needs of clinical nurses can significantly bolster their mental health literacy. These programs should encompass various aspects of mental health, including common disorders, symptoms, treatment modalities, and communication strategies. Utilizing methods such as case studies (61), direct patient interaction (62), role-playing exercises, and interactive workshops (63) can foster active learning and skill development among nurses.
Moreover, developing evidence-based practice guidelines specific to mental health care can furnish clinical nurses with clear protocols and best practices for assessing, managing, and supporting individuals with mental health concerns. It’s imperative to regularly update these guidelines to reflect advances in research and clinical practice, ensuring nurses have access to the most current information and recommendations.
Encouraging interdisciplinary collaboration between clinical nurses and mental health professionals is another pivotal strategy (64). Facilitating regular meetings, case consultations, and joint training sessions can promote knowledge sharing, skill exchange, and mutual support, enabling nurses to learn from experts in the field and access specialized resources and expertise (65).
Establishing peer support networks within healthcare organizations can provide clinical nurses with a safe and supportive space to discuss challenges, share experiences, and seek guidance related to mental health care (66). These networks can help reduce feelings of isolation, normalize discussions around mental health, and foster a culture of empathy and understanding among nurses.
Launching targeted anti-stigma campaigns aimed at raising awareness, challenging stereotypes, and promoting positive attitudes toward mental ill health can effectively combat stigma among clinical nurses. Leveraging various mediums such as posters, seminars, social media (67), and workshops can disseminate accurate information, challenge misconceptions, and encourage empathy and compassion toward individuals with mental health conditions.
Creating a supportive organizational culture that prioritizes mental health awareness and inclusivity necessitates strong leadership commitment (68). Hospital administrators and nursing leaders should actively champion initiatives to improve mental health literacy and reduce stigma, allocating resources (69), providing training opportunities, and acknowledging efforts to promote positive change within the organization.
Regularly evaluating the effectiveness of interventions to improve mental health literacy and reduce stigma among clinical nurses is crucial for identifying areas of improvement and refining strategies over time (70). Collecting feedback from nurses, monitoring key performance indicators, and conducting periodic assessments can help gauge the impact of interventions and inform future initiatives.
Furthermore, it’s noteworthy that while more knowledge about mental ill health doesn’t necessarily equate to increased stigma, studies have indicated a desire for more education and experiences related to mental ill health among participants (71). Therefore, broadening the scope and depth of mental health knowledge among nurses and teaching effective patient interaction strategies may help mitigate stigma. Additionally, nurses should be equipped with appropriate coping strategies for their mental health, as the well-being of healthcare professionals can significantly impact staff and patient safety.
This study highlights the intricate interplay between mental health knowledge, stigma, and social distance among clinical nurses in China. The findings reveal that stigma serves as a mediating factor influencing the relationship between knowledge and social distance. Nurses with higher levels of mental health knowledge exhibited lower stigma and greater willingness to engage with people with a mental health condition, underscoring the critical role of education in shaping attitudes and behaviors. From a theoretical perspective, this research enriches the understanding of stigma dynamics within the nursing profession by integrating the Knowledge-Attitude-Practice (KAP) model. Practically, the findings emphasize the urgent need for targeted educational interventions to address stigma and improve mental health literacy among nurses.
Despite these contributions, the study has limitations. The use of a convenience sample from a single region may limit the generalizability of the findings. Additionally, the cross-sectional design restricts causal inferences, necessitating longitudinal studies to further explore the causal pathways between knowledge, stigma, and social distance.
Future research should expand the scope to include diverse cultural and geographical contexts and investigate the effectiveness of stigma-reduction interventions in clinical settings. By addressing these challenges, future studies can provide more comprehensive insights into fostering stigma-free environments in healthcare and enhancing the professional development of nurses in mental health care.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Research and Academic Ethics Committee of Jinzhou Medical University; affiliation: Jinzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
WW: Data curation, Methodology, Writing – original draft. JX: Data curation, Investigation, Project administration, Writing – original draft. WC: Data curation, Resources, Supervision, Writing – original draft. JY: Methodology, Resources, Software, Writing – review & editing. KX: Data curation, Investigation, Writing – original draft. SB: Methodology, Validation, Writing – review & editing. AS: Writing – review & editing. ZZ: Data curation, Validation, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We thank everyone who worked on this article, my supervisor for help, my leader for support, the pioneers in the discipline for their preliminary research, and all participants for their free support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization (WHO). World mental health report: transforming mental health for all. (2022). Available online at: https://www.who.int/publications/i/item/9789240049338 (Accessed June 22, 2024).
2. McGrath JJ, Al-Hamzawi A, Alonso J, Altwaijri Y, Andrade LH, Bromet EJ, et al. Age of onset and cumulative risk of mental disorders: a cross-national analysis of population surveys from 29 countries. Lancet Psychiatry. (2023) 10:668–81. doi: 10.1016/S2215-0366(23)00193-1
3. Government of the Netherlands. ] (n.d). Available online at: https://www.government.nl/topics/mhpss/mhpss-worldwide-facts-and-figures (Accessed June 22, 2024).
4. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
5. Wu J, Wang Y, Wang L, Wu H, Li J, Zhang L. Trends and burden in mental disorder death in China from 2009 to 2019: a nationwide longitudinal study. Front Psychiatry. (2023) 14:1169502. doi: 10.3389/fpsyt.2023.1169502
6. Yubo R, Fenlan J. Key points of handling suspected mental patients’ alarm from a typical case. Public Secur Educ. (2018) 08:41–5.
7. China Youth Daily(CYD). More than 90% of China’s 6.6 million registered patients with severe mental disorders have received care and treatment (2022). Available online at: https://baijiahao.baidu.com/s?id=1735863760386850855&wfr=spider&for=pc (Accessed June 22, 2024).
8. Committee of the Kuomintang of China(CKC). Zhou Shihong: It is urgent to strengthen the prevention and treatment of mental health diseases (2022). Available online at: http://www.ahmg.gov.cn/newslist.Asp?Id=11773 (Accessed June 22, 2024).
9. Thornicroft G. Shunned: discrimination against people with mental ill-ness. Oxford: Oxford University Press (2006).
10. Bathje GJ, Pryor JB. The relationships of public and self-stigma to seeking mental health services. J Ment Health Couns. (2011) 33-2:161–77. doi: 10.17744/mehc.33.2.g6320392741604l1
11. Brunero S, Lamont S. Challenges, risks and responses. In: Elders R, Nizette K, O’Brien A, editors. Psychiatric and mental health nursing. Elsevier (2016). p. 552–76.
12. Seeman N, Tang S, Brown AD, Ing A. World survey of mental illness stigma. J Affect Disord. (2016) 190:115–21. doi: 10.1016/j.jad.2015.10.011
13. Canadian Mental Health Association(CMHA). Fast facts about mental illness . Available online at: https://cmha.ca/about-cmha/fast-facts-about-mental-illness (Accessed June 22, 2024).
14. Fino E, Agostini A, Mazzetti M, Colonnello V, Caponera E, Russo PM. There is a limit to your openness: mental illness stigma mediates effects of individual traits on preference for psychiatry specialty. Front Psychiatry. (2019) 10:775. doi: 10.3389/fpsyt.2019.00775
15. Happell B, Gaskin CJ. The attitudes of undergraduate nursing students towards mental health nursing: a systematic review. J Clin Nurs. (2013) 22:148–58. doi: 10.1111/jocn.12022
16. Rasmussen JD, Kakuhikire B, Baguma C, Ashaba S, Cooper-Vince CE, Perkins JM, et al. Portrayals of mental illness, treatment, and relapse and their effects on the stigma of mental illness: Population-based, randomized survey experiment in rural Uganda. PloS Med. (2019) 16:e1002908. doi: 10.1371/journal.pmed.1002908
17. Qin Y, Song LS. A review of the research on the stigma of mental disorders from the perspective of public mental health. Chin J Soc Med. (2021) 38:253–6.
19. Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. Eur psychiatry: J Assoc Eur Psychiatrists. (2005) 20:529–39. doi: 10.1016/j.eurpsy.2005.04.004
20. Tognazzini P, Davis C, Kean AM, Osborne M, Wong KK. Reducing the stigma of mental illness. Can nurse. (2008) 104:30–3.
21. Ma X, Li Q, LIU Y-g, Tian T, Ren Y, Ren Y. A review of research on social distance. Labor Secur World. (2019) 32:74–5.
22. Li M, Wu Z. Analysis of stigma in Chinese patients with severe mental illness and its countermeasures. Chin J Med Ethics. (2017) 30:383–7.
23. Xu Y, Qiu X. Living space, social distance and Migrant workers’ identity. In: Fujian forum: humanities and social sciences edition, vol. 11. (2017). p. 127–36.
24. Lin C-H, Lai TY, Chen YJ, Lin SK. Social distance towards schizophrenia in health professionals. ” Asia-Pacific psychiatry: Off J Pacific Rim Coll Psychiatrists vol. (2022) 14:e12506. doi: 10.1111/appy.12506
25. Zhao D. The Impact of stigmatized identity on Interpersonal Influence and social distance. Acta Psychologica Sin. (2013) 45:1283–94. doi: 10.3724/SP.J.1041.2013.01283
26. Zhu K, Wang F, Jiang Z, Zhang Z, Cui Q, Zhu C, et al. Analysis of Social distance between mental health workers and schizophrenic patients and its influencing factors. Chin J Public Health Administration. (2020) 37:131–3.
27. Pettigrew TF, Tropp LR. How does intergroup contact reduce prejudice? Meta-analytic tests of three mediators. Eur J Soc Psychol. (2008) 38:922–34. doi: 10.1002/ejsp.504
28. Lopez V, Sanchez K, Killian MO, Eghaneyan BH. Depression screening and education: an examination of mental health literacy and stigma in a sample of Hispanic women. BMC Public Health. (2018) 18:646. doi: 10.1186/s12889-018-5516-4
29. Alsahali S. Knowledge and attitude of pharmacy students toward people with mental illnesses and help-seeking: A cross-sectional study from Saudi Arabia. Pharm (Basel Switzerland). (2021) 9:82. doi: 10.3390/pharmacy9020082
30. Saito AS, Creedy DK. Determining mental health literacy of undergraduate nursing students to inform learning and teaching strategies. Int J Ment Health Nurs. (2021) 30:1117–26. doi: 10.1111/inm.12862
31. Fang Q, Zhang TM, Wong YLI, Yau YY, Li XH, Li J, et al. The mediating role of knowledge on the contact and stigma of mental illness in Hong Kong. Int J Soc Psychiatry. (2021) 67:935–45. doi: 10.1177/0020764020975792
32. Zhao R, Wang J, Zhao X, et al. Investigation of mental illness knowledge and attitude of psychiatric nurses. Contemp Nurses (next issue). (2015) 07:21–4.
33. Riffel T, Chen S-P. Exploring the knowledge, attitudes, and behavioural responses of healthcare students towards mental illnesses-A qualitative study. Int J Environ Res Public Health. (2019) 17:25. doi: 10.3390/ijerph17010025
34. Sastre-Rus M, Tomás-Sábado J, Juliá-Sanchis R, Roldán-Merino JF, Puig-Llobet M, Lluch-Canut MT. Development and psychometric testing of a scale for assessing the associative stigma of mental illness in nursing. J Clin Nurs. (2020) 29:4300–12. doi: 10.1111/jocn.15467
35. Wang W, Cui H, Zhang W, Xu X, Dong H. Reliability and validity of the chinese version of the scale for assessing the stigma of mental illness in nursing. Front Psychiatry. (2021) 12:754774. doi: 10.3389/fpsyt.2021.754774
36. China Health and Family Planning Commission (CHFPC). Notice of the General Office of the Ministry of Health on Issuing the Survey and Evaluation Program of Mental Health Indicators (2010). Available online at: http://www.nhc.gov.cn/jkj/s5888/201003/c6487d3f272e4e7b88d30347ff6a2299.shtml (Accessed June 22, 2024).
37. The national mental health work plan (2015-2020) (2015). Available online at: http://www.gov.cn/xinwen/2015-06/18/content_2881371.htm (Accessed June 22, 2024).
38. Zhu K. Current situation and Influencing factors of social integration in schizophrenia patients. (Master’s thesis). Wuhan University of Science and Technology (2019).
39. Jacq K, Norful AA, Larson E. Nurses’ and mental health technicians’ Attitudes and social acceptance of people with mental illness. Issues Ment Health Nurs. (2021) 42:365–75. doi: 10.1080/01612840.2020.1799272
40. Bennett J, Stennett R. Attitudes towards mental illness of nursing students in a Baccalaureate programme in Jamaica: a questionnaire survey. J Psychiatr Ment Health Nurs. (2015) 22:599–605. doi: 10.1111/jpm.12234
41. Babicki M, Małecka M, Kowalski K, Bogudzińska B, Piotrowski P. Stigma levels toward psychiatric patients among medical students-A worldwide online survey across 65 countries. Front Psychiatry. (2021) 12:798909. doi: 10.3389/fpsyt.2021.798909
42. Jin XX. A survey on the stigma of severe mental illness in 192 nursing staff. China Health Industry. (2018) 15:185–6.
43. Oliveira AM, Machado D, Fonseca JB, Palha F, Silva Moreira P, Sousa N, et al. Stigmatizing attitudes toward patients with psychiatric disorders among medical students and professionals. Front Psychiatry. (2020) 11:326. doi: 10.3389/fpsyt.2020.00326
44. Anosike C, Aluh DO, Onome OB. Social distance towards mental illness among undergraduate pharmacy students in a Nigerian university. East Asian Arch psychiatry: Off J Hong Kong Coll Psychiatrists. (2020) 30:57–62. doi: 10.12809/eaap1924
45. Tei-Tominaga M, Asakura T, Asakura K. Stigma towards nurses with mental illnesses: a study of nurses and nurse managers in hospitals in Japan. Int J Ment Health Nurs. (2014) 23:316–25. doi: 10.1111/inm.12052
46. Ciydem E, Avci D. Effects of the psychiatric nursing course on students’ beliefs toward mental illness and psychiatric nursing perceptions in Turkey. Perspect Psychiatr. (2022) 58:348–54. doi: 10.1111/ppc.12796
47. Ács A, Mészáros J, Balogh Z. Egészségügyi szakdolgozók mentális zavarokkal kapcsolatos ismereteinek és a betegekkel szembeni attitűdjének vizsgálata” [Examining health professionals’ knowledge and attitudes towards mental disorders. Orvosi hetilap. (2020) 161:56–66. doi: 10.1556/650.2020.31577
48. Gu L, Xu D, Yu M. Mediating effects of stigma on the relationship between contact and willingness to care for people with mental illness among nursing students. Nurse Educ Today. (2021) 103:104973. doi: 10.1016/j.nedt.2021.104973
49. Nguyen E, Chen TF, O'Reilly CL. Evaluating the impact of direct and indirect contact on the mental health stigma of pharmacy students. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1087–98. doi: 10.1007/s00127-011-0413-5
50. Zheng Y, Zhang Z, Gong Q. Study on the Effect of Mental health knowledge on the discrimination of patients with mental disorders. Chin J Med Ethics. (2017) 30:1002–1005 + 1029.
51. Soltis-Jarrett V. The future of psychiatric-mental health nursing: observe, reflect, and take action to empower knowledge for the greater good. Issues Ment Health Nurs. (2023) 44:1071–9. doi: 10.1080/01612840.2023.2270066
52. Rahaman KS, Majdzadeh R, Holakouie Naieni K, Raza O. Knowledge, attitude and practices (KAP) regarding chronic complications of diabetes among patients with type 2 diabetes in dhaka. Int J Endocrinol Metab. (2017) 15:e12555. doi: 10.5812/ijem.12555
53. Cleary A, Dowling M. Knowledge and attitudes of mental health professionals in Ireland to the concept of recovery in mental health: a questionnaire survey. J Psychiatr Ment Health Nurs. (2009) 16:539–45. doi: 10.1111/j.1365-2850.2009.01411.x
54. Rayan A. Cultural misconceptions, attitudes, knowledge, and beliefs about mental illness among Jordanian nurses working in psychiatric units. J continuing Educ Nurs. (2022) 53:513–20. doi: 10.3928/00220124-20221006-09
55. Crowe A, Mullen PR, Littlewood K. Self-stigma, mental health literacy, and health outcomes in integrated care. J Couns Dev. (2018) 96:267–77. doi: 10.1002/jcad.12201
57. Valentim O, Moutinho L, Laranjeira C, Querido A, Tomás C, Longo J, et al. Looking beyond Mental Health Stigma”: An Online Focus Group Study among Senior Undergraduate Nursing Students. Int J Environ Res Public Health. (2023) 20:4601. doi: 10.3390/ijerph20054601
58. Potts LC, Bakolis I, Deb T, Lempp H, Vince T, Benbow Y, et al. Anti-stigma training and positive changes in mental illness stigma outcomes in medical students in ten countries: a mediation analysis on pathways via empathy development and anxiety reduction. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1861–73. doi: 10.1007/s00127-022-02284-0
59. Pepa PA, Hsia SL, Lee KC. Impact of a psychiatry elective on mental health stigma among pharmacy students. Currents Pharm Teach Learn. (2021) 13:711–6. doi: 10.1016/j.cptl.2021.01.029
60. Jenkins E, Currie LM, Hirani S, Garrod E, Goodyear T, McGuinness L, et al. Enhancing nurses’ capacity to provide concurrent mental health and substance use disorder care: A quasi-experimental intervention study. Nurse Educ Today. (2022) 117:105483. doi: 10.1016/j.nedt.2022.105483
61. Martin A, Chilton J, Gothelf D, Amsalem D. Physician self-disclosure of lived experience improves mental health attitudes among medical students: A randomized study. J Med Educ curricular Dev. (2020) 7:2382120519889352. doi: 10.1177/2382120519889352
62. Zavorotnyy M, Klatte S, Yang Y, Liu W, Wagner U, Kircher T. The effects of a psychiatric clerkship on stigmatizing attitudes toward mental disorders as held by German medical students. Front Psychiatry. (2023) 14:1306403. doi: 10.3389/fpsyt.2023.1306403
63. Brenner LD, Wei H, Sakthivel M, Farley B, Blythe K, Woodruff JN, et al. Breaking the silence: A mental health initiative to reduce stigma among medical students. Acad medicine: J Assoc Am Med Colleges. (2023) 98:458–62. doi: 10.1097/ACM.0000000000005090
64. American Association of Colleges of Nursing. The Essentials: core competencies for professional nursing education (2021). Available online at: https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf (Accessed June 22, 2024).
65. Alyousef SM, Alhamidi SA. Nurse views of obstacles encountered by nurses in Saudi Arabia during the provision of psychiatric care. Arch Psychiatr Nurs. (2023) 44:8–17. doi: 10.1016/j.apnu.2023.03.005
66. Kamalzadeh L, de Filippis R, El Hayek S, Heidari Mokarar M, Jatchavala C, Koh EBY, et al. Impact of stigma on the placement of mental health facilities: insights from early career psychiatrists worldwide. Front Psychiatry. (2023) 14:1307277. doi: 10.3389/fpsyt.2023.1307277
67. El Halabi S, Fish E, Boroon M, de Filippis R, El Hayek S, Larnaout A, et al. The role of arts in moderating mental health-related stigma: views of early career psychiatrists and trainees from different parts of the world. Front Psychiatry. (2024) 15:1293142. doi: 10.3389/fpsyt.2024.1293142
68. Rushton CH, Boston-Leary K. Nurses suffering in silence: Addressing the stigma of mental health in nursing and healthcare. Nurs Manage. (2022) 53:7–11. doi: 10.1097/01.NUMA.0000853148.17873.77
69. Domingue J-L, Jager F, Lusk J, Davis A, Ezeani C, Perkins M, et al. An integrative review of mental health nurses’ and other professionals’ Experience of associative stigma. Issues Ment Health Nurs. (2022) 43:843–51. doi: 10.1080/01612840.2022.2055243
70. de Filippis R, El Hayek S, Shalbafan M. Editorial: Community series in mental-health-related stigma and discrimination: prevention, role, and management strategies, volume II. Front Psychiatry. (2024) 15:1384836. doi: 10.3389/fpsyt.2024.1384836
71. Porfyri G-N, Athanasiadou M, Siokas V, Angelopoulos K, Skarpari S, Zagalioti S-C, et al. Mental illness through the perspective of undergraduate medical students in Greece: a cross-sectional study at Aristotle University of Thessaloniki. Front Psychiatry. (2023) 14:1228539. doi: 10.3389/fpsyt.2023.1228539
Keywords: mental health knowledge, stigma, social distance, clinical nurses, interdisciplinary care, nursing environment
Citation: Wang W, Xia J, Chen W, Ye J, Xie K, Zhang Z, Binti Mohamad SM and Shuid AN (2025) Exploring the interplay of mental health knowledge, stigma, and social distance among clinical nurses: a study in Liaoning, China. Front. Psychiatry 16:1478690. doi: 10.3389/fpsyt.2025.1478690
Received: 10 August 2024; Accepted: 10 February 2025;
Published: 28 February 2025.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Najmeh Shahini, Golestan University of Medical Sciences, IranCopyright © 2025 Wang, Xia, Chen, Ye, Xie, Zhang, Binti Mohamad and Shuid. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmad Naqib Shuid, bmFxaWJAdXNtLm15
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.