- Department of Clinical Psychology, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran
Background: Emotion regulation (ER) and distress tolerance (DT) are considered transdiagnostic risk factors for a range of anxiety disorders. This study investigated the relationship between anxiety sensitivity (AS) and health anxiety (HA) in the general population, focusing on the mediating roles of DT and ER.
Methods: The study was conducted as a cross-sectional survey from October to December 2023 in Tehran Province, Iran. A total of 971 individuals participated in this study (52.8% female; mean age 39.04 years, SD=10.64). Participants completed self-report questionnaires to assess HA (The Short Health Anxiety Inventory), AS (The Anxiety Sensitivity Index-3), DT (The 15-item Distress Tolerance Scale) and ER (The 10-item Emotion Regulation Questionnaire). We used structural equation modeling (SEM) to examine the hypothesis that DT and ER would mediate the relationship between AS and the HA.
Results: AS was modestly related to all measures (r from -0.40 to 0.55). According to the SEM analysis, AS (β = 0.45, 95%CI [0.34, 0.56]) had a significant direct effect on HA. However, the analysis of the indirect effects revealed that both DT (β = 0.10, 95% CI [0.06, 0.16]) and emotion regulation strategies—cognitive reappraisal (β = 0.06, 95% CI [0.01, 0.11]) and expressive suppression (β = 0.11, 95% CI [0.06, 0.18])—act as partial mediators in the relationship between AS and HA.
Conclusions: AS plays a crucial role in predisposing individuals to HA. The mediating roles of DT and ER provide insight into the link between AS and HA. Nevertheless, the study’s cross-sectional design and reliance on a non-clinical sample limit the applicability of the results. Further research involving different samples and intervention studies is needed to validate and expand upon these findings.
1 Introduction
1.1 Health anxiety
Health anxiety (HA), alike known as illness anxiety, is a common issue, impacting up to 6% of general individuals at some point in their lives and up to twenty percent of medical outpatients (1). Excessive worry about one’s health and fear of getting sick are key features of HA, leading to constant monitoring of symptoms and unproductive facts seeking and safety measures (1). HA, while mild forms can encourage beneficial behaviors such as attending preventive medical check-ups, becomes a disabling condition when excessive. Severe health anxiety leads to significant distress, challenging patient-doctor relationships (2), increased healthcare utilization (3), and a considerable economic burden (4). It affects approximately 3.4% of the adult population (5) and is strongly associated with psychological distress and functional impairment (3, 5). As a serious and costly public health issue, untreated HA often becomes chronic (6), resulting in enduring consequences for individuals, healthcare systems, and society (7). The effect of HA on one’s health and the use of medical services can substantially elevate healthcare costs. In a natural longitudinal examination, it was revealed that individuals suffering from severe HA incurred 41–78% more healthcare expenses annually (2).
Numerous examinations have concentrated on the cognitive and emotional factors connected with a greater probability of experiencing excessive HA (8–10). In several studies (11–14), it has been discussed, investigated, and demonstrated that anxiety sensitivity (AS), emotion regulation (ER) and distress tolerance (DT) which are known as three transdiagnostic factors are linked to HA. These factors provide valuable insight into the underlying mechanisms of HA, offering potential targets for therapeutic interventions.
1.2 Health anxiety and anxiety sensitivity
Anxiety sensitivity (AS) as transdiagnostic risk factor for psychiatric disorders refers to the negative emotional reactions to anxiety-related senses or symptoms. It involves the fear of bodily senses related to physiological arousal and the belief that these senses may result in negative physical, social, or psychological impacts (15, 16). AS is a result of dysfunctional beliefs and can lead to intense anxiety-related fear of physical sensations. Several studies highlight the connection between AS and illness anxiety disorder. As part of the cycle of health anxiety, AS can intensify an individual’s tendency to be overly vigilant about bodily senses and to experience distress when they occur (17, 18). AS has been observed to be linked with HA in both non-clinical and clinical adult samples. Research has found that greater levels of AS relates to greater HA (11, 19). In contrast, the absence of a significant prospective relationship between AS and HA is incompatible with some earlier work (12).
1.3 Health anxiety and distress tolerance
Distress tolerance (DT) represents the capacity to endure unfavorable psychological and physical states (20). It influences how distressing stimuli are appraised and the perceived capability to manage them (21). DT measures a person’s capability to endure uncomfortable emotional states and assesses their ability to handle distress (22). The behavioral index of DT measures the mastery to handle a challenging situation or task while striving toward a goal in front of negative feelings (20).
Studies indicate that clinically meaningful anxiety levels are related to more down levels of DT (23). According to a study (24), these results imply that DT may be an essential component in the development of anxiety disorders in overall. Persistent anxiety symptoms may result from actions linked to low DT (25). Studies suggest that DT and HA are negatively associated in a wide variety of nonclinical individuals (25, 26). Individuals with low DT are driven to flee from interior experiences, which exacerbates anxiety, since they believe they are unable to tolerate bad internal states, such as by believing that illness-related beliefs are dangerous and uncontrollable (25, 26). The concept of DT has obtained little consideration in the literature on HA despite several studies highlighting its significant role in general anxiety (26–29).
1.4 Health anxiety and emotion regulation
Emotional regulation (ER) involves trying to alter emotions by either evoking or sustaining emotional experiences, or by adjusting and effectively manage their frequency, strength, or duration (30). Our theoretical framework is anchored in Gross’s (2015) process model of ER, which stands as the most commonly utilized model of ER within the field of affective science. This model introduces a framework for emotion regulation that categorizes strategies into five distinct groups: the selection of specific scenarios, the adjustment of those scenarios, the way attention is focused, the reappraisal of cognitive perceptions, and the modification of responses (31).
Within the Gross’s model, cognitive reappraisal (CR) and expressive suppression (ES) serve as primary illustrations of strategies for regulating emotions. CR, which focuses on changing cognitive antecedents, requires a reinterpretation or intentional alteration in the perception of an emotional event or stimulus, aiming for a more balanced or positive perspective. Conversely, ES targets the modulation of emotional responses by restraining the outward expression of emotions, essentially inhibiting any reaction during the last phase of the ER process (31). In the field of ER, CR is often considered an adaptive strategy and ES considered a maladaptive strategy. Utilizing CR regularly is correlated with numerous beneficial long-term effects, such as enhanced overall well-being and social functional (32). On the other hand, excessive reliance on ES generally correlates with suboptimal outcomes, including diminished social functional and well-being (33). Certainly, mental health conditions like depression and anxiety disorders are often typified by a decreased reliance on CR and an increased reliance on ES (34, 35). The number of research exploring the contribution of and/or association between HA and ER In adults. ER difficulties have been positively correlated with HA (36, 37). Studies show that unhealthy emotional regulation techniques like suppression and catastrophizing are connected to HA (38, 39). Also (40), discovered that ER served as a mitigating factor for HA, but its impact was not direct. Exploring the relationship between ER and HA is valuable because the findings could enhance our understanding of the origins of HA, potentially leading to more effective, evidence-based interventions and assessments.
1.5 Anxiety sensitivity, distress tolerance and emotion regulation
An important transdiagnostic factor is anxiety sensitivity (AS), which involves the fear of physiological arousal senses and the view that they could lead to negative outcomes (16). Another related transdiagnostic factor is difficulties in ER, which involves an individual’s capacity to detect, process, and reply to emotions (33, 41). Previous study in adults supports a connection between ER and AS over time (42). Prior research has found significant interacting effects despite the fact that AS and ER are distinctive transdiagnostic variables (43, 44). In fact, it has been demonstrated that AS and ER are connected to the emergence, maintenance, and management of anxiety-associated pathologies and symptoms (43–45). For instance, prior research indicates that reduced ER capacity may act to intensify AS, which in turn may impact a variety of other anxiety consequences such as worry and panic (43). Current empirical research and established theoretical models indicate that an individual’s ER capacity may have a role in the development of AS (44). On the other hand, elevated AS levels may theoretically make it more difficult for a person to use ER techniques that are necessary to reduce symptoms. Previous research in clinical populations demonstrates that modifications in ER and AS mediate abatement in anxiety symptoms in individuals with anxiety-related illnesses (e.g., social phobia, PTSD, and generalized anxiety disorder (45);. All of these findings point to the importance of ER in transdiagnostic anxiety processes, including sensitivity to anxiety and signs correlated with anxiety (41). However, it is not possible to interpret these effects as causative due to the cross-sectional character of these investigations.
The capacity of a person to withstand unfavorable emotional condition (DT) and their inclination to evaluate their own feelings of anxiety as detrimental (AS) are conceptually similar and yet can be considered as separate constructs. Schmidt et al. (2011) investigated the correlation between AS and DT, highlighting that DT involves a general capacity for enduring emotional distress, while AS pertains specifically to the endurance of anxiety and its associated feelings (41). They noted that DT encompasses a wide array of negative emotional experiences, but AS distinctly targets managing anxiety, suggesting the possibility that AS might act as an element within the broader trait of DT (22, 46). Accordingly, if individuals have lower grades of DT, they may be more likely to experience anxiety issues due to their reduced capacity to handle and endure negative emotional states, leading them to avoid or escape situations that provoke anxiety (28).
When DT and AS have been studied together, conflicting findings arise regarding their distinct connections with symptoms of anxiety. Some research shows that AS is strongly connected to anxiety symptoms, whereas DT is not (47), but alternate research suggests that DT is unusually associated with anxiety symptoms, whereas AS is not (24, 48). Differences in previous studies, findings are likely attributable to a variety of agents including disparities in the demographics of participants, such as their age and symptom severity, as well as methodological variations like the duration of the study and the methodologies applied (e.g., measures used).
Anxiety and AS are inversely correlated with DT (28, 49, 50). In both nonclinical and treatment-seeking populations, a correlation has been established between DT and AS (49, 51). Despite documented negative relationships between DT and AS, to our knowledge, no studies have clearly examined the associations among AS, DT, and symptoms of HA in one combined model
1.6 Distress tolerance and emotion regulation
The research suggests that DT likely influences the choice of specific ER strategies an individual uses. In emotion research, high DT aids adaptive emotive reactions to life tension by serving as an ER skill. It enables individuals to select and implement effective strategies during challenging situations (52, 53). To express it another way, DT serves as a broad factor relating to individual differences that facilitates particular behaviors for regulating emotions. This viewpoint suggests that people with high DT are probable to engage in positive ER practices such as problem-solving and labeling emotions when faced with stress, while those with low DT may resort to less effective ER techniques like suppression and avoidance (21, 54). Linking adaptive ER behaviors might provide a reason for the relationship between DT and health outcomes (55). Quantitative study conclusions suggest that there are meta-analytic relationship between DT and various ER strategies. The investigation revealed that high DT showed moderate connections with maladaptive ER methods like rumination, worry, experiential avoidance and expressive suppression, with correlations ranging between -.19 and -.57. Conversely, DT had relatively weaker positive associations with effective ER including reappraisal, mindfulness and problem-solving, with correlations ranging between.08 and.38 (52). Previous investigation on DT in healthy individuals has also demonstrated that higher DT is linked to adaptive ER, encompassing impulse control and emotional awareness (56, 57).
1.7 Summary
The problem of HA is significant in clinical settings and requires further clarification. AS is a crucial factor that predisposes individuals to HA. AS has been identified in early studies as a significant risk factor for HA (58), playing a predictive role in this study.
While previous research has explored the relationships between AS and HA, a critical gap remains in understanding the mechanisms that explain this link. Specifically, few studies have examined the mediating roles of DT and ER, two constructs that are central transdiagnostic factors of emotional disorders. Our study is among the first to integrate these variables into a comprehensive model, highlighting their mediating roles in the AS-HA relationship. Additionally, understanding these mediators is crucial for developing targeted interventions. Unlike earlier studies that primarily focused on direct relationships, this research provides insights into how and why AS translates into HA, offering practical applications for clinical settings.
As mentioned earlier, both HA and AS are associated with abnormal processing of ER and DT, AS may decrease people’s DT and then cause HA symptoms. While ER and DT have each been separately associated with various anxiety outcomes, the current work explicitly models both factors as potential mediators. This dual-mediation design offers a more comprehensive view of the underlying mechanisms at play, thereby illuminating practical intervention targets. Therefore, the primary purpose of the study was to specify the role of ER and DT in the association between AS and HA (see Figure 1). We conceptualized AS as comprising of three dimensions: (1) physical concerns, (2) social concerns and (3) cognitive concerns, while HA was analyzed in terms of two dimensions: illness likelihood and negative consequences of illness. ER was defined with two dimensions: cognitive reappraisal (CR) and expressive suppression (ES), while DT was investigated in four dimensions: regulation, tolerance, appraisal, and absorption. Based on existing publications and previous results, we developed several assumptions. Prior research has indicated a link between AS and HA. Consequently, we hypothesized a positive relationship between AS and HA. Additionally, we proposed that DT, ES, and CR would act as mediators between AS and HA.
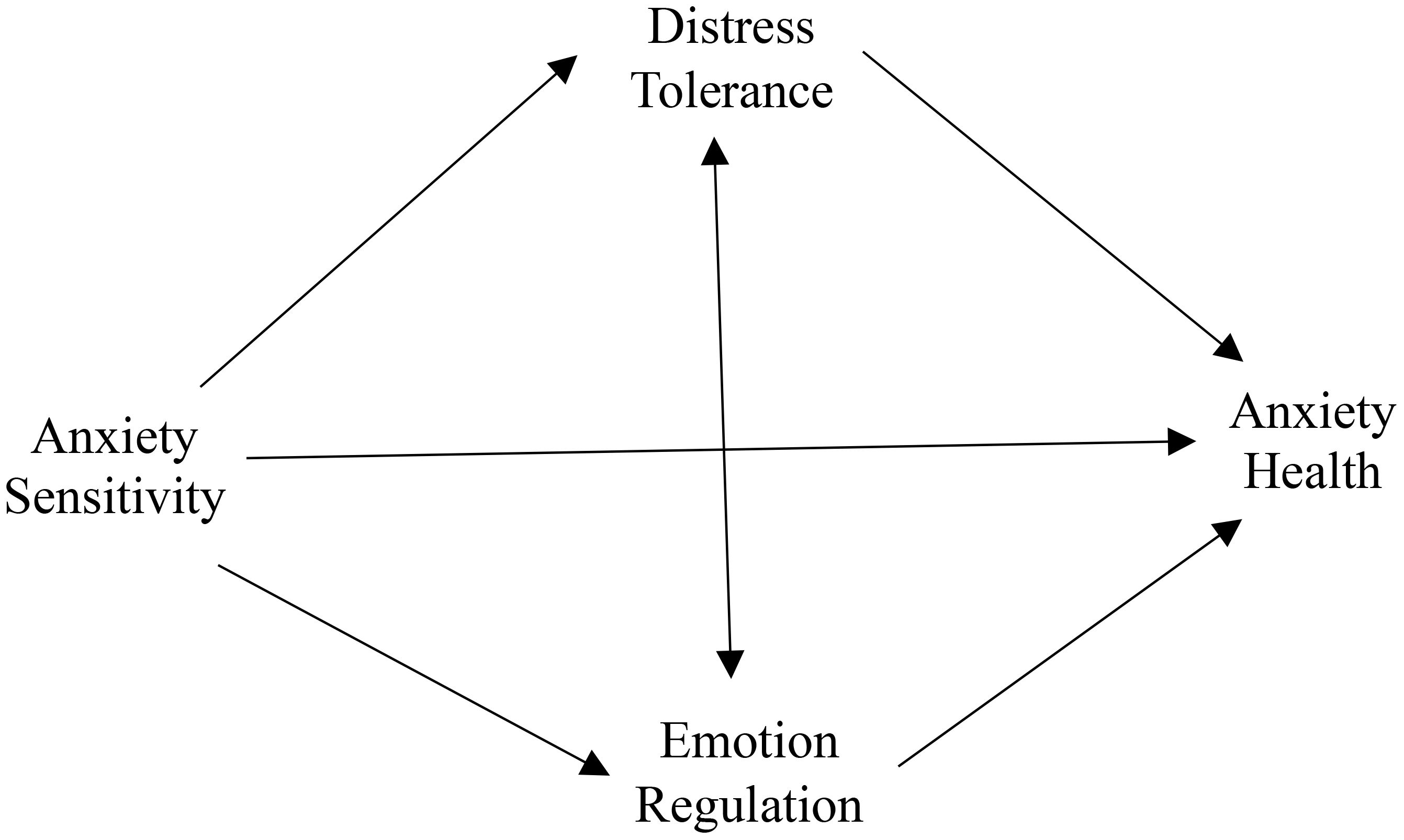
Figure 1. Initial hypothetical model of the relationship between anxiety sensitivity and anxiety health.
2 Method
2.1 Participants
This study used a convenience sample of 971 participants. The Participants were from Tehran city located in Iran country. The age group of the participants varied between 18 and 65 (MTotal = 39.04, SDTotal = 10.64). 52.8% were female (513 females; Mean age = 38.63, SD = 10.80) and 47.2% were male (458 males; Mean age = 39.49, SD = 10.44). The educational background of the participants varied: 3.7% (n=36) had some undergraduate education, 21.1% (n=205) held a diploma, 39.1% (n=380) had earned a bachelor’s degree, 30.4% (n=295) had obtained a master’s degree, and 5.7% (n=55) had achieved a doctoral degree. Concerning employment status, 57.8% (n=561) were employed, 26.9% (n=261) were student, 10.9% (n=106) were unemployed, 3% (n=29) were retired and 1.4% had lost their jobs. Fifty-nine percent of the sample reported their marital status as married (n=573), 41% as Single/divorced/windowed (n=398).
2.2 Procedure
The current study acquired approval from the Association for Ethics at the Iran University of Medical Sciences. Various social media platforms were utilized to recruit participants, from October to December 2023. Advertisements were placed on digital applications (such as WhatsApp, Instagram, Telegram) to invite participation in the investigation. A web link, which was provided in these advertisements, contained information about the study’s objective on its first page. By approving to participate and confirming the consent form, participants were then given access to do the surveys, submit demographic details, and receive a set of questionnaires. Participants must spend a minimum of 20 minutes completing questionnaires to ensure data quality. Participation required individuals to be a minimum of 18 years old. Participation was voluntary, with no compensation offered; moreover, participants were ensured confidentiality due to the unidentified essence of the questionnaire completion process.
Inclusion criteria comprised: (1) aged 18 to 65, (2) people who volunteered to take part in the study and (3) people who were able to done questionnaires on their own. Exclusion criteria included (1) inadequate proficiency in Persian and (2) no access to the Internet.
2.3 Measures
2.3.1 Health anxiety
The Short Health Anxiety Inventory (SHAI) is a tool used to consider health-related anxiety via 18 items. Over time, various factor constructions have been presented for the SHAI, but this study employed a two-factor model. The two factors used in this study are “health anxiety,” which comprises 14 items, and “negative consequences of illness,” which includes 4 items. Participants select from four response options per item to reflect their feelings over the past six months. Previous studies have indicated the SHAI to have high internal consistency (59). The Persian version (60) has demonstrated satisfactory internal consistency (α = .88 for overall scale), temporal stability (r = .7) and construct validity. In the current study, the SHAI demonstrated excellent internal consistency (α = .80).
2.3.2 Anxiety sensitivity
The Anxiety Sensitivity Index-3 (ASI-3) is a self-report questionnaire designed to assess sensitivity to anxiety symptoms across three domains: physiological, cognitive, and social. It contains 18 items that participants rate on a 5-point Likert scale ranging from 0 (Not at All) to 4 (Very Much). The ASI-3 provides both a total score and three subscale scores, with each subscale consisting of 6 items. Items are scored based on the frequency and severity of these symptoms, with total scores ranging from 0 to 72. Higher scores reflect greater sensitivity to anxiety (61). Research on the Persian versions of the ASI-3 has confirmed that both the total score and the subscales exhibit high internal consistency (with a Cronbach’s alpha of 0.93) and show strong convergent and divergent validity (19). In the current study, the ASI-3 indicated excellent reliability, with a Cronbach’s alpha of 0.94 for the total scale, and alpha values of 0.86 for the physiological, 0.85 for the cognitive, and 0.80 for the social subscales.
2.3.3 Distress tolerance
Simons & Gaher (2005) developed The Distress Tolerance Scale (DTS), a five-point Likert scale with 15 items ranging from 1 (Strongly Disagree) to 5 (Strongly Agree). Using confirmation factor analysis, it has been found that there is a higher-order General DTS factor that consists of all items and corresponds to the total score and that there are four lower-order factor scales: Appraisal (6 items); Tolerance (3 items); Absorption (3 items); and Regulation (3 items) (17). As part of the primary validation study, the DTS had high internal consistency in a college sample (Cronbach’s alpha = 0.89), good divergent, criterion, and convergent validity. In the current study for the DTS, the Cronbach alphas were: Total Scale = 0.87; Appraisal = 0.80; Absorption = 0.73; Tolerance = 0.78; and Regulation = 0.78.
2.3.4 Emotion regulation
The Emotion Regulation Questionnaire (ERQ), developed by Gross and John in 2003, is a tool developed to consider how people handle their emotions through two specific strategies: cognitive reappraisal (CR) and expressive suppression (ES). This questionnaire will be made up of 10 items ordered on a ranking from 1 (strongly disagree) to 7 (strongly agree). It includes four questions targeting expressive suppression and six questions focusing on cognitive reappraisal. Higher scores in each category reflect greater use of the respective ER strategy. the ERQ is known for its robust psychometric properties (62). In this study, the reliability of the ERQ was confirmed with Cronbach’s alpha scores of 0.73 for expressive suppression and 0.90 for cognitive reappraisal.
2.4 Data analyses
The study employed descriptive statistics to collection an overview of the participants’ socio-demographic characteristics and the scores of various study variables. To investigate the connections between AS and other variables, including mediators and outcomes, Pearson correlation analysis was conducted.
We applied a structural equation model (SEM) to test our hypothetical framework. Initially, the measurement models were assessed using the maximum likelihood (ML) approach, where all principal constructs were treated as latent variables. The suggested signs were described as follows: AS was represented by the combined scores of the three ASI-3 subscales; distress tolerance was reflected in the combined scores of the four DTS subscales; emotion regulation was denoted by the combined scores of the two ERQ subscales; and the total scores of health anxiety and negative consequences of illness denoted health anxiety. Ultimately, a SEM was designed to investigate the psychological pathways from AS to HA, considering sex and age as covariates for HA. The analysis was conducted using the ML method, and indirect effects were computed using a bootstrap technique with 5000 iterations. Statistical significance was determined at the 0.05 level if the bias-corrected bootstrap 95% confidence interval (CI) did not include zero (63). Based on the criteria proposed by Klin (2023), Chi-square index (χ2), comparative fit index (CFI; > 0.90), the goodness of fit index (GFI; < 0.95), the adjusted goodness of fit index (AGFI; < 0.90); in addition, values equal to or < 0.08 (values < 0.06 are more appropriate) for the RMSEA and SRMR suggest a good fit for the model (64). Statistical analyses were performed by utilizing the IBM SPSS (version 27.0) software package and the AMOS (version 24.0) software package.
3 Results
3.1 Descriptive statistics
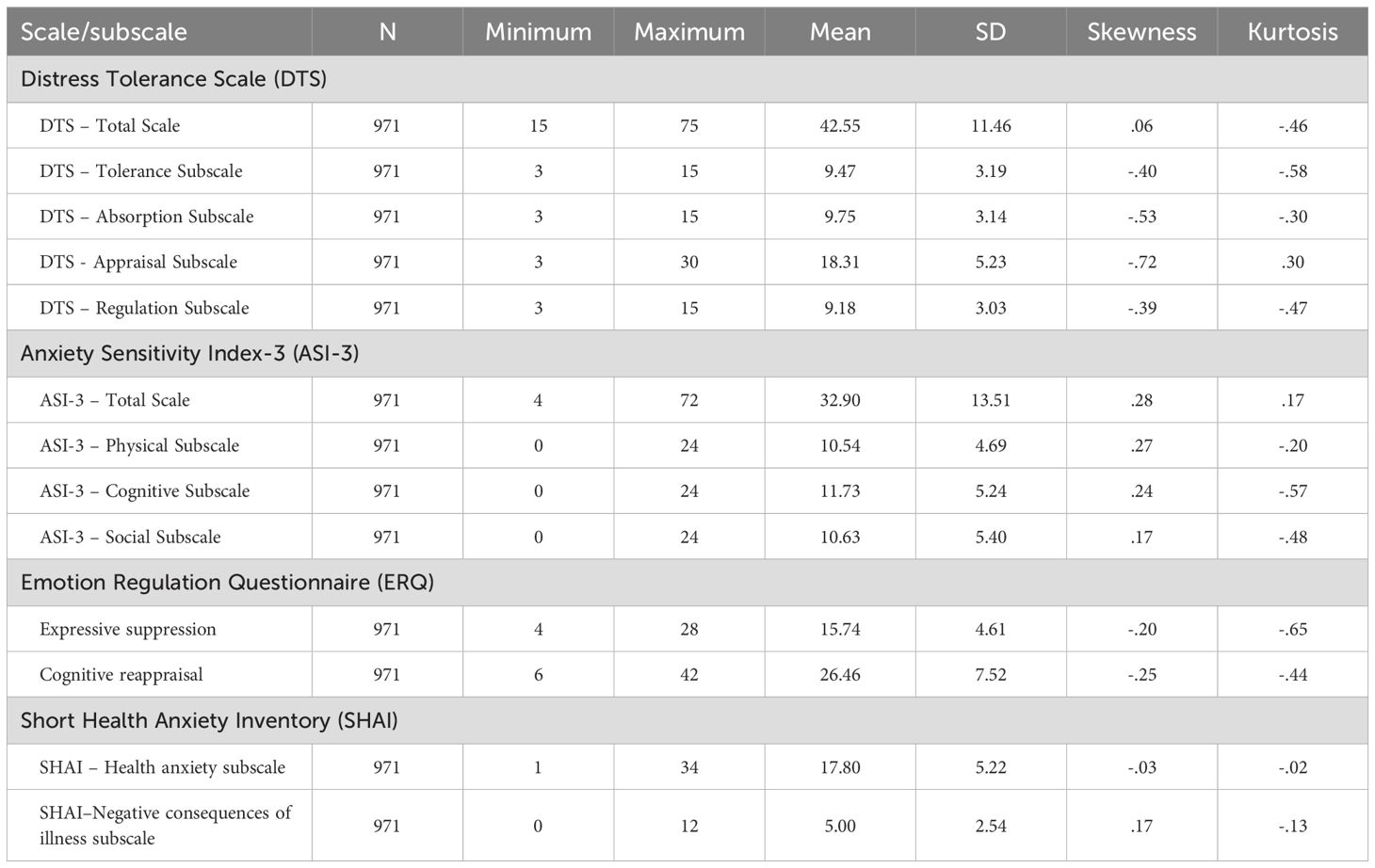
Table 1 provides an overview of the means, standard deviations, ranges, skewness, and kurtosis for the total and subscale scores of the SHAI, DTS, ASI-3, and ERQ-10. To assess the normality of these scores, normal Q-Q plots, histograms, and boxplots were visually inspected, and the kurtosis and skewness ratios were examined for each measure. The analysis indicated that all four measures followed an approximately normal distribution. There were no notable discrepancies between the mean and the five percent trimmed mean for each scale, suggesting that the data did not contain any significant outliers that could skew the results. Furthermore, the Cronbach’s alpha values for each scale exceeded the commonly accepted threshold of 0.70, implying strong internal consistency.
3.2 Zero-order correlations
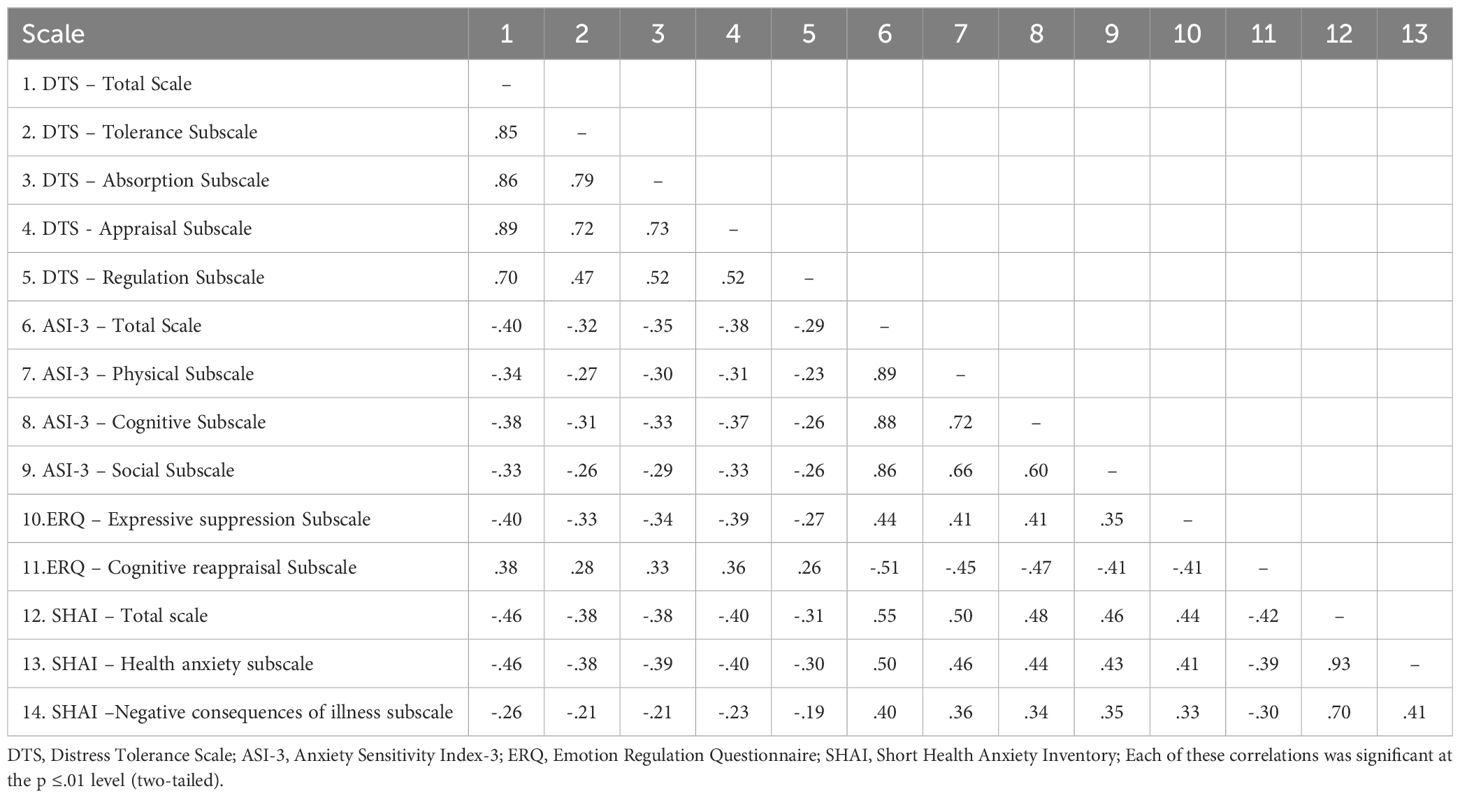
To explore the linkages among the study variables, Pearson correlation coefficients were calculated, and the results are presented in Table 2. The analysis revealed that AS had a statistically significant relationship with both DT and ER, and it was particularly positively correlated with HA.
The relationships between the study’s exogenous, mediator, and endogenous variables, both positive and negative correlations, are shown in Table 2. The endogenous variable SHAI was moderately correlated with several variables: ASI-3 (r = .55, p <.001), DT (r = −.46, p <.001), ERQ-Expressive Suppression (ERQ-ES; r = .44, p <.001), and ERQ-Cognitive Reappraisal (ERQ-CR; r = −.42, p <.001). In contrast, the exogenous variable ASI-3 was negatively correlated with DT (r = −.40, p <.001), positively correlated with ERQ-ES (r = .44, p <.001), and negatively correlated with ERQ-CR (r = −.51, p <.001). Among the mediators, a significant negative relationship was discovered between DT and ERQ-ES (r = −0.40, p <.001), whereas DT and ERQ-CR exhibited a significant positive correlation (r = .38, p <.001).
3.3 SEM analyses
The study assessed the mediating role of DT and ER on the relationship between AS and HA. To evaluate the proposed model, one SEM analysis was performed. Since there was adequate evidence supporting the assumption of normality, the MLE method was employed (64).
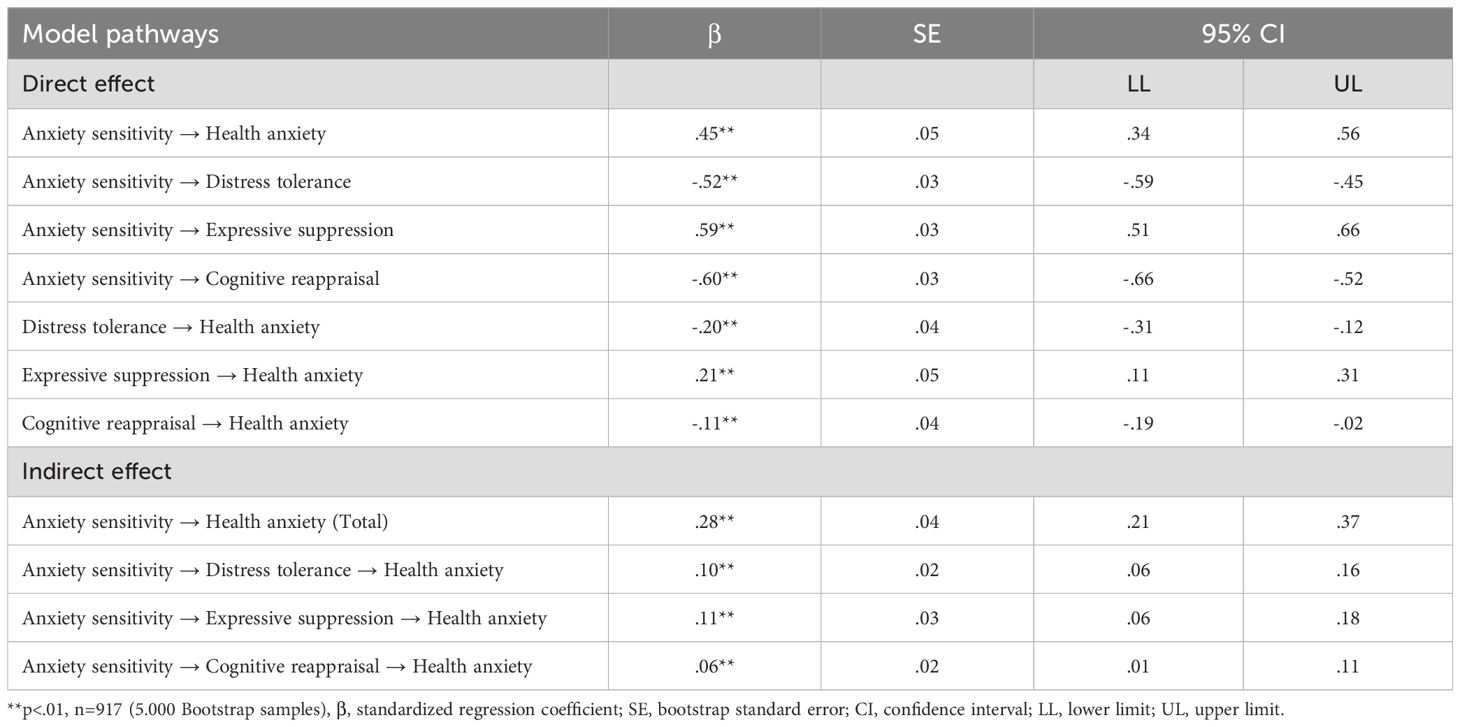
The model’s fit was evaluated using several criteria: chi-square (χ²), normed chi-square index (χ²/df), comparative fit index (CFI), goodness of fit index (GFI), adjusted goodness of fit index (AGFI), root-mean-square error of approximation (RMSEA), and standardized root mean squared residual (SRMR). The results showed that the model fit well with the data (χ² = 434.421, df = 144, χ²/df = 3.01, p < 0.001, GFI = .953, AGFI = .938, RMSEA = .046, SRMR = .052). The normed chi-square index was 3.01, which is below the acceptable limit of 5 (58). The RMSEA value for the model was.046, which is below the standard cut-off of.05 (64). The CFI, GFI, and AGFI values were.90,.95, and.93, respectively, all of which exceed the recommended value of.90 (58), indicating that the model fit the data well. Subsequently, standardized path coefficients for all proposed paths were analyzed, and the findings are depicted in Figure 2.
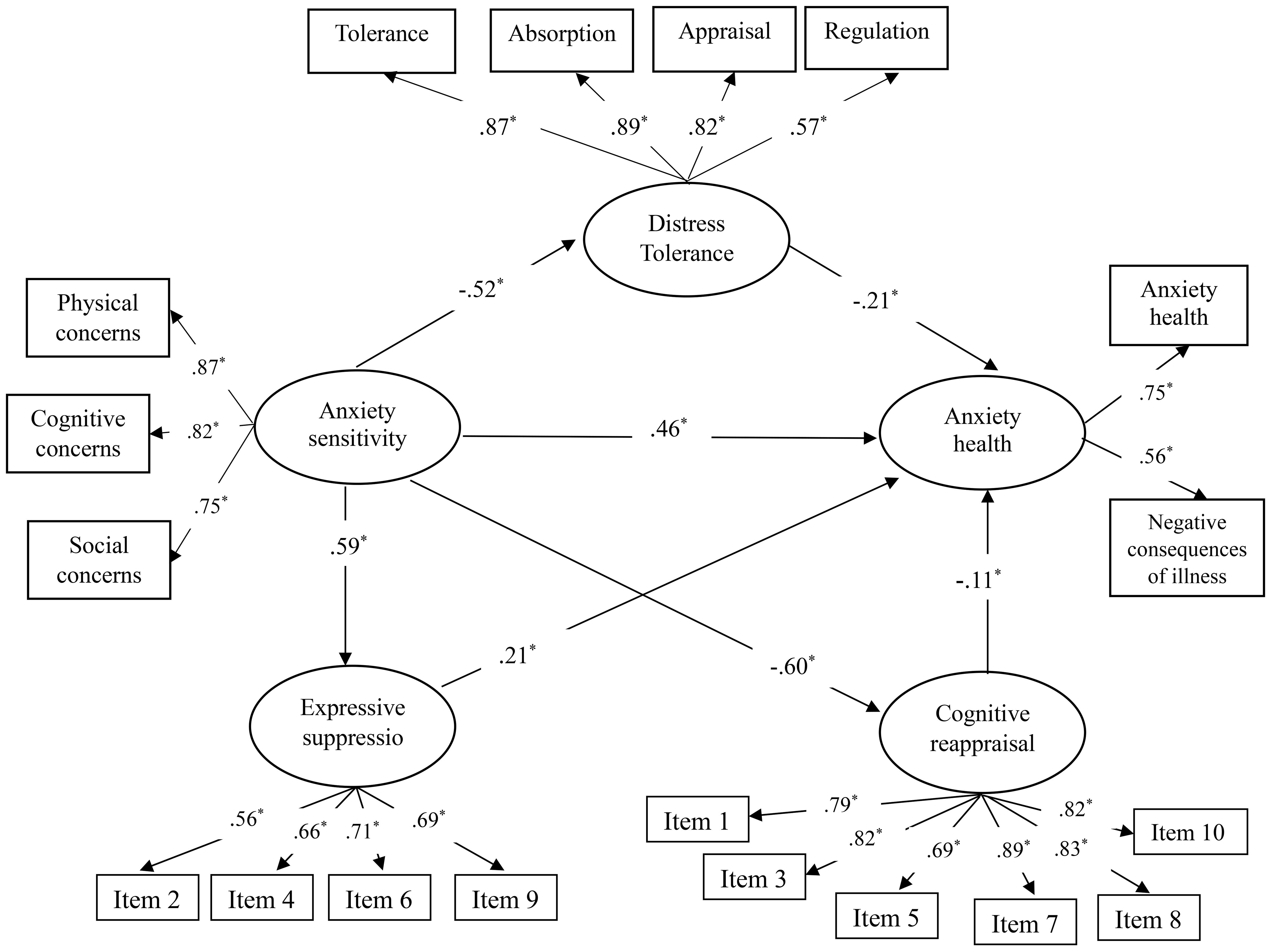
Figure 2. Final structural equation model. The symbol * indicates that the path coefficient is statistically significant, with p < 0.01.
Table 3 provides an overview of the standardized direct, indirect, and total effects within the proposed model. Bootstrap analysis confirmed that the total indirect effect of AS on HA is statistically significant (β = .45, p <.01). Specifically, the indirect pathways from AS to HA through DT (β = .10, p <.01), ER-ES (β = .11, p <.01), and ER-CR (β = .06, p <.01) were significant. Moreover, significant direct effects of DT (β = -.20, p <.01), ER-ES (β = .21, p <.01), and ER-CR (β = -.11, p <.01) on HA were observed. The direct effect of AS on HA remained significant even after considering the indirect effects, indicating that DT, ER-ES, and ER-CR act as partial mediators. Please see Table 3 for more information.
4 Discussion
The primary objective of the study was to explore how emotion regulation (ER) and distress tolerance (DT) influence the connection between anxiety sensitivity (AS) and health anxiety (HA). We hypothesized that DT, cognitive reappraisal (CR) and expressive suppression (ES) would mediate the link between AS and HA. Our findings reveal a positive correlation between AS and HA, with DT and ER acting as mediators in this correlation.
We supposed that AS would be associated with HA, and our findings confirmed this prediction. We discovered a positive, significant, and moderate correlation between the Anxiety Sensitivity Index-3 and the short Health Anxiety Inventory. The study demonstrated that higher AS is linked to higher HA scores, aligning with previous research (19, 65–67). AS has been extensively discussed as a factor that may contribute to HA, playing a role in its development or exacerbation (68). AS may lead to hyper-vigilance towards bodily senses and increased distress when these senses occur, which are key components of the HA process (18). People with high AS are likely to monitor unexplained bodily sensations, such as a hot flash, to quickly detect and address potential threats (69, 70). Consequently, a person who thinks that unexplained bodily sensations indicate a medical catastrophe will constantly check their body for changes, quickly notice them, misinterpret them as threats, and then experience increased anxiety.
The current research’s findings show that AS related to ER. This finding is compatible with previous study that has shown connection between AS and ER (42–44). However, document suggests that in individuals with high AS, deficits in ER may contribute to the development of anxiety-related disorders (44). Pickett, Lodis, Parkhill, and Orcutt (2012) proposed a model that conceptualizes AS is a typical susceptibility characteristic for psychopathology, which may originate from broader susceptibility facets including personality traits (65). According to this approach, maladaptive ER, a more expansive risk element, may lead to an increased disposition towards AS. Operating this top-down model, targeting ER in therapy could potentially reduce AS or even preclude its onset (71). Therefore, improving ER skills may help alleviate individuals’ fear of anxiety symptoms (i.e., AS), thereby reducing the risk of developing anxiety-related disorders.
Our study found a significant negative connection between HA and CR (adaptive ER), and a significant positive relationship between HA and ES (Maladaptive ER). These results are consistent with previous research (14, 36, 38, 39, 72), as participants with high and moderate levels of HA showed low ER skills and vice versa. Consistent with these findings, research revealed that individuals with somatic symptom disorder utilized fewer adaptive ER procedures and more maladaptive ones compared to a healthy group. This suggests that adults with HA exhibit a reduced use of adaptive emotion regulation strategies (37). HA is linked to a negative mindset, where potential symptoms trigger thoughts like, “I am certain I will get sick”. This cognitive process can trigger a destructive cycle of affective conditions, manifesting as illness anxiety disorder, along with maladaptive cognitions and behaviors such as excessive information-seeking (73). Previous study has demonstrated a strong association between difficulties in ER and various anxiety-related behavioral and cognitive aspects (74). Challenges in ER may cause individuals to adopt ineffective coping strategies for health concerns, like seeking health information online instead of consulting healthcare professionals (75). Effective ER helps prevent excessive online health information seeking and is linked to reduced levels of HA.
Additionally, we anticipated that ER would be a mediator in the association between AS and HA. For individuals with high HA, regularly searching for medical information online about their symptoms is intended to offer short-term relief from recurring feelings and negative thoughts. Previous research indicates that difficulties in ER play a mediating role in this process (76). Poor ER leads to maladaptive coping strategies for HA, such as seeking health data online instead of consulting medical professionals (39). Thus, effective ER acts as a protective factor against HA and is also associated with low AS. Therefore, improving ER skills in individuals may be an indirect way to reduce HA.
Consistent with previous research demonstrating an inverse relationship between AS and DT (25, 28, 49, 77), the correlation investigations indicated that DT was negatively associated with AS. This implies that fear of anxiety-related symptoms (AS) increases as an individual’s capacity to tolerate distress diminishes. These results suggest that people with low DT are more prone to fear arousal-related sensations. It is possible that those encountering significant distress or anxiety develop a reduced tolerance for distress, which in turn makes them more sensitive to health symptoms.
The relation between DT and HA found in this study aligns with previous research in adults. Understanding this relationship involves analyzing the components that define DT: tolerance, appraisal, regulation, and absorption (17). Simons & Gaher
(2005) describe that individuals with lower tolerance for negative emotions experience heightened distress and sensitivity to anxiety (tolerance). They frequently underestimate their ability to manage anxiety indications (appraisal), which leads to the use of ineffective coping procedures, such as avoidance (regulation). Moreover, their intolerance of negative emotions disrupts their functioning because they are overly preoccupied with their distress (absorption). This kind of functional impairment is also characteristic of anxiety disorders (22, 28). The negative correlation between DT and HA identified in our research supports these findings. The results support previous research highlighting the transdiagnostic role of negative emotion tolerance in anxiety and HA (24, 27, 28, 47).
We examined the connection between DT and two ER strategies: CR (changing one’s thinking about a situation to change its emotional consequence) and ES (suppressing the outward expression of emotions). The findings showed a negative correlation between CR and DT, and a positive correlation between ES and DT. These findings are consistent with previous research (52, 56, 78), as our participants who demonstrated moderate and high levels of DT scored low in CR. As predicted, low DT was significantly related to greater use of ES. Research indicates that DT likely influences the ER strategies an individual adopts. For instance, someone with low DT may negatively interpret a situation because they perceive negative emotions as unbearable. This perception can drive them to use regulatory strategies like suppression, which provide immediate relief but may lead to long-term negative results (21). Supporting this theory, studies have found that individuals with low DT are more prone to conceal negative emotions and are more motivated to use ineffective ER strategies to manage negative emotional conditions (21, 22).
One explanation for this correlation is individuals who employ maladaptive regulation strategies, such as ES, are more likely to struggle with tolerating negative emotions. For example, individuals with high DT tend to assess their emotional experiences in a way that reduces the perceived need for ER. They possess a greater sense of confidence in their ability to manage distressing feelings, view negative emotions as non-threatening, and do not feel an immediate urge to avoid or reduce these emotions (22, 56). Consequently, they are more likely to accept their emotions without attempting to alter them (56). Another explanation is that individuals with higher DT often interpret emotional experiences (reappraisal) in a way that reduces their perceived need for ER. They believe they can manage distress effectively, view negative emotions as non-threatening, and do not feel a strong need to avoid or reduce these emotions (22). This perspective aligns with the idea that emotions do not require control, leading to less frequent use of active ER strategies (56). In our sample, this was evident from the association between higher DT and increased CR (reappraisal). Further research into how beliefs about emotion affect the association between DT and ER behaviors could provide additional insights into these phenomena.
Recent developments within the metacognitive model of emotion dysregulation (79) provide additional insights into the relationship between DT and ER. According to this model, distress internal states (e.g., negative thoughts or emotions) may activate dysfunctional metacognitive beliefs, which can lead to greater difficulties in ER, either directly or via maladaptive forms of mental control (79). Evidence from non-clinical and clinical samples, including individuals with affective disorders, eating disorders, and substance use disorders, supports the notion that these dysfunctional metacognitive processes exacerbate emotion dysregulation (80–82). For example, individuals who perceive their negative emotions as uncontrollable or catastrophic are more likely to engage in maladaptive ER strategies, such as avoidance or suppression, further reducing their DT (81, 82). Incorporating these perspectives into the current findings highlights the importance of targeting both metacognitive beliefs and ER strategies in interventions aimed at improving DT and reducing HA. Future research should explore how these metacognitive factors interact with DT and ER to influence HA, potentially offering new avenues for therapeutic approaches.
Furthermore, our study investigates the effect of mediation of DT and ER on the connection between AS and HA. The outcomes of bootstrapped parallel mediation studies showed that ER and DT partially mediated the association between AS and HA symptoms. This suggests that individuals with a higher capacity for emotional tolerance experience less emotional distress, which enables them handle negative automatic thoughts and prevent HA.
4.1 Limitations and directions for future studies
The findings of our study should be interpreted with caution due to several important limitations. These constraints are essential to consider when evaluating the results of this initial research. Firstly, the cross-sectional format of this study prohibits for conclusions about causality or the determination of temporal relationships. Although our findings suggest that DT and ER mediate the relationship between AS and HA, these conclusions should be considered exploratory and correlational rather than definitive. Longitudinal studies are needed to examine the directionality and potential causal pathways between AS, ER, DT, and HA over time. Without such evidence, we cannot definitively claim that improving DT or ER will directly reduce HA, or that these mediators are the underlying mechanisms of the relationship between AS and HA. Secondly, the sample composition must be acknowledged as a limitation. Our participants were not clinical subjects, and this limits the generalizability of the findings to populations with diagnosed health anxiety-related disorders, including illness anxiety disorder. The results may not apply to individuals with more severe manifestations of HA. Future studies should replicate this research with clinical populations to better understand how ER and DT operate in individuals with more pronounced HA symptoms. Thirdly, the use of convenience and snowball sampling methods in this study makes it difficult to ascertain whether the sample accurately represents the entire population of Iran. Future studies should consider using larger sample sizes and exploring the relationships between variables in diverse populations. Fourthly, the use of web-based surveys limits the ability to create random samples, as participants need internet access, leading to potential self-selection biases. It is recommended that this research be replicated on a larger national scale and that qualitative methodologies be used to uncover cultural nuances that quantitative methods cannot capture. Fifthly, although there are known disparities among ethnic groups in ER (62), this study did not control for potential cultural variances. In addition, there is a shortage of specific demographic data such as ethnicity, race, and socioeconomic status necessitates cautious interpretation of our findings. A further limitation is the reliance on self-report measures, which might potentially create common method variance. Future research could profit from adopting multimethod approaches, such as behavioral indicates of ER and DT.
On the clinical level, these findings show that those who fail to tolerate unpleasant emotions are at greater risk to develop different kinds of psychopathology related with emotion dysregulation, such as illness anxiety disorder. Our results indicate that treatments aimed at reducing HA symptoms by focusing on DT and ER could be particularly effective. Broadly targeting DT and ER may help lower HA levels. Understanding the role of DT as a mediator can assist physicians recognize those patients who will probably to benefit the most from specific therapies and establish suitable treatment suggestions. For example, people who have low DT levels might benefit more from Dialectical Behavior Therapy (DBT), which is specifically designed to enhance DT skills. DBT, a form of cognitive-behavioral therapy, incorporates Instruction in skills and functioning behavioral assessment alongside ideas of dialectical philosophy, mindfulness and styles of communication (83). DBT has been shown to improve ER in individuals with various anxiety and mood disorders (84). Since DBT targets ER, it may be an effective treatment for HA. Although no studies have yet employed DBT specifically for HA, research combining ER treatments with DBT has shown positive outcomes for individuals with HA. Additionally, DBT can educate persons who employ inefficient coping mechanisms in response to an unable to handle unpleasant negative emotions to find more effective strategies for addressing negative impact.
Our findings emphasize the importance of targeting both DT and ER in therapeutic interventions for HA. Cognitive-behavioral therapy (CBT) has been shown to be effective in enhancing DT by equipping individuals with skills to endure and manage distressing emotions (85). Additionally, metacognitive therapy (MCT) offers a promising approach to addressing difficulties in ER by focusing on modifying dysfunctional metacognitive beliefs (86). MCT aims to reduce the reliance on maladaptive forms of mental control and promote adaptive strategies for managing emotional distress. Incorporating these therapeutic approaches may improve outcomes for individuals experiencing health anxiety by addressing both the underlying mechanisms of DT and ER. These insights contribute to a more comprehensive understanding of the relationship between AS and HA and highlight the potential for integrative therapeutic approaches that address the interplay of DT, ER, and metacognitive processes.
5 Conclusions
As the first study to examine the role of DT and ER in explaining the link between AS and HA in an Iranian population, our results showed a strong correlation between AS and HA, consistent with existing adult literature. These findings show that AS is a key risk factor for HA, with DT and ER playing significant roles in this relationship. Future longitudinal studies are needed to affirm our findings, and AS and its related mechanisms should be considered in HA treatment. Although our study adds valuable insights into the understanding of HA, it represents only a portion of the knowledge necessary to develop a developmental, evidence-based model of HA. Understanding the causes of HA better will help in developing evidence-based evaluations and interventions for controlling HA.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by All participants gave written informed consent to participate. The study was approved by the Research Ethics Committees of Iran University of Medical Sciences (IR.IUMS.REC.1402.676). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HM: Conceptualization, Formal Analysis, Investigation, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. MP: Conceptualization, Investigation, Project administration, Supervision, Writing – review & editing. KZ: Conceptualization, Formal Analysis, Methodology, Supervision, Writing – review & editing. BG: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tyrer P. Recent advances in the understanding and treatment of health anxiety. Curr Psychiatry Rep. (2018) 20:49. doi: 10.1007/s11920-018-0912-0
2. Hanel G, Henningsen P, Herzog W, Sauer N, Schaefert R, Szecsenyi J, et al. Depression, anxiety, and somatoform disorders: Vague or distinct categories in primary care? Results from a large cross-sectional study. J Psychosom Res. (2009) 67:189–97. doi: 10.1016/j.jpsychores.2009.04.013
3. Bobevski I, Clarke DM, Meadows G. Health anxiety and its relationship to disability and service use: findings from a large epidemiological survey. Biopsychosocial Sci Med. (2016) 78:13–25. doi: 10.1097/psy.0000000000000252
4. Hannah K, Marie K, Olaf H, Stephan B, Andreas D, Wilson Michael L, et al. The global economic burden of health anxiety/hypochondriasis- a systematic review. BMC Public Health. (2023) 23:2237. doi: 10.1186/s12889-023-17159-5
5. Sunderland M, Newby JM, Andrews G. Health anxiety in Australia: prevalence, comorbidity, disability and service use. Br J Psychiatry. (2013) 202:56–61. doi: 10.1192/bjp.bp.111.103960
6. Rask CU, Gehrt TB, Rimvall MK, Frostholm L. Health anxiety. Z Psychol. (2020) 228:141–4. doi: 10.1027/2151-2604/a000407
7. Risør BW, Frydendal DH, Villemoes MK, Nielsen CP, Rask CU, Frostholm L. Cost effectiveness of internet-delivered acceptance and commitment therapy for patients with severe health anxiety: A randomised controlled trial. PharmacoEconomics - Open. (2022) 6:179–92. doi: 10.1007/s41669-021-00319-x
8. Asmundson GJ, Fergus TA. The concept of health anxiety. In: The Clinician’s Guide to Treating Health Anxiety. London, United Kingdom: Elsevier (2019). p. 1–18. doi: 10.1016/B978-0-12-811806-1.00001-9
9. Asmundson GJG, Abramowitz JS, Richter AA, Whedon M. Health anxiety: current perspectives and future directions. Curr Psychiatry Rep. (2010) 12:306–12. doi: 10.1007/s11920-010-0123-9
10. O’Bryan EM, McLeish AC, Johnson AL. The role of emotion reactivity in health anxiety. Behav Modif. (2017) 41:829–45. doi: 10.1177/0145445517719398
11. Horenstein A, Rogers AH, Bakhshaie J, Zvolensky MJ, Heimberg RG. Examining the role of anxiety sensitivity and intolerance of uncertainty in the relationship between health anxiety and likelihood of medical care utilization. Cognit Ther Res. (2019) 43:55–65. doi: 10.1007/s10608-018-9980-z
12. Bredemeier K, Church LD, Bounoua N, Feler B, Spielberg JM. Intolerance of uncertainty, anxiety sensitivity, and health anxiety during the COVID-19 pandemic: Exploring temporal relationships using cross-lag analysis. J Anxiety Disord. (2023) 93:102660. doi: 10.1016/j.janxdis.2022.102660
13. Wright KD, Lebell MANA, Carleton RN. Intolerance of uncertainty, anxiety sensitivity, health anxiety, and anxiety disorder symptoms in youth. J Anxiety Disord. (2016) 41:35–42. doi: 10.1016/j.janxdis.2016.04.011
14. Love S, Sharman R, Kannis-Dymand L. Emotion regulation and the specific associations with health anxiety. Psychol Stud (Mysore). (2018) 63:410–8. doi: 10.1007/s12646-018-0469-3
15. Olatunji BO, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychol Bull. (2009) 135:974–99. doi: 10.1037/a0017428
16. Smits JAJ, Otto MW, Powers MB, Baird SO. 1 - Anxiety sensitivity as a transdiagnostic treatment target. In: Smits JAJ, Otto MW, Powers MB, Baird SO, editors. The Clinician’s Guide to Anxiety Sensitivity Treatment and Assessment. London, United Kingdom: Academic Press (2019). p. 1–8. doi: 10.1016/B978-0-12-813495-5.00001-2
17. Abramowitz JS, Olatunji BO, Deacon BJ. Health anxiety, hypochondriasis, and the anxiety disorders. Behav Ther. (2007) 38:86–94. doi: 10.1016/j.beth.2006.05.001
18. Warwick HMC, Salkovskis PM. Hypochondriasis. Behav Res Ther. (1990) 28:105–17. doi: 10.1016/0005-7967(90)90023-C
19. Shabani MJ, Mohsenabadi H, Gharraee B, Shayanfar F, Corcoran VP, McKay D. Psychological correlates of health anxiety in response to the coronavirus (COVID-19) pandemic: a cross-sectional online study in Iran. Int J Cognit Ther. (2023) 16:103–22. doi: 10.1007/s41811-022-00152-y
20. Zvolensky MJ, Vujanovic AA, Bernstein A, Leyro T. Distress tolerance: theory, measurement, and relations to psychopathology. Curr Dir Psychol Sci. (2010) 19:406–10. doi: 10.1177/0963721410388642
21. Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychol Bull. (2010) 136:576–600. doi: 10.1037/a0019712
22. Simons JS, Gaher RM. The distress tolerance scale: development and validation of a self-report measure. Motivation Emotion. (2005) 29:83–102. doi: 10.1007/s11031-005-7955-3
23. Lee SY, Park CL, Russell BS. Does distress tolerance interact with trait anxiety to predict challenge or threat appraisals? Pers Individ Dif. (2018) 132:14–9. doi: 10.1016/j.paid.2018.05.014
24. Laposa JM, Collimore KC, Hawley LL, Rector NA. Distress tolerance in OCD and anxiety disorders, and its relationship with anxiety sensitivity and intolerance of uncertainty. J Anxiety Disord. (2015) 33:8–14. doi: 10.1016/j.janxdis.2015.04.003
25. Wright CD, Nelson CI, Brumbaugh JT, McNeil DW. The role of distress tolerance as a potential mechanism between anxiety sensitivity and gut-specific anxiety. Int J Behav Med. (2020) 27:717–25. doi: 10.1007/s12529-020-09912-6
26. Sauer KS, Jungmann SM, Witthöft M. Emotional and behavioral consequences of the COVID-19 pandemic: the role of health anxiety, intolerance of uncertainty, and distress (In)Tolerance. Int J Environ Res Public Health. (2020) 17:7241. doi: 10.3390/ijerph17197241
27. Fergus TA, Bardeen JR, Orcutt HK. Examining the specific facets of distress tolerance that are relevant to health anxiety. J Cognit Psychother. (2015) 29:32–44. doi: 10.1891/0889-8391.29.1.32
28. Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety symptomatology: the association with distress tolerance and anxiety sensitivity. Behav Ther. (2010) 41:567–74. doi: 10.1016/j.beth.2010.04.002
29. Lindner C, Kotta I, Marschalko EE, Szabo K, Kalcza-Janosi K, Retelsdorf J. Increased risk perception, distress intolerance and health anxiety in stricter lockdowns: self-control as a key protective factor in early response to the COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19:5098. doi: 10.3390/ijerph19095098
30. Garnefski N, Kraaij V. The cognitive emotion regulation questionnaire: Psychometric features and prospective relationships with depression and anxiety in adults. Eur J Psychol Assess. (2007) 23:141–9. doi: 10.1027/1015-5759.23.3.141
31. Gross JJ. Emotion regulation: current status and future prospects. Psychol Inq. (2015) 26:1–26. doi: 10.1080/1047840X.2014.940781
32. Goldin PR, McRae K, Ramel W, Gross JJ. The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol Psychiatry. (2008) 63:577–86. doi: 10.1016/j.biopsych.2007.05.031
33. Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clin Psychol Rev. (2017) 57:141–63. doi: 10.1016/j.cpr.2017.09.002
34. Lincoln TM, Schulze L, Renneberg B. The role of emotion regulation in the characterization, development and treatment of psychopathology. Nat Rev Psychol. (2022) 1:272–86. doi: 10.1038/s44159-022-00040-4
35. Preece DA, Becerra R, Robinson K, Gross JJ. The emotion regulation questionnaire: psychometric properties in general community samples. J Pers Assess. (2020) 102:348–56. doi: 10.1080/00223891.2018.1564319
36. Bardeen JR, Fergus TA. An examination of the incremental contribution of emotion regulation difficulties to health anxiety beyond specific emotion regulation strategies. J Anxiety Disord. (2014) 28:394–401. doi: 10.1016/j.janxdis.2014.03.002
37. Martin A, Gitzen H. The role of health anxiety for emotion regulation in somatic symptom disorder. J Psychosom Res. (2017) 97:160. doi: 10.1016/j.jpsychores.2017.03.267
38. Fang S, Mushtaque I. The moderating role of health literacy and health promoting behavior in the relationship among health anxiety, emotional regulation, and cyberchondria. Psychol Res Behav Manage. (2024) 17:51–62. doi: 10.2147/prbm.S446448
39. Görgen SM, Hiller W, Witthöft M. Health anxiety, cognitive coping, and emotion regulation: A latent variable approach. Int J Behav Med. (2014) 21:364–74. doi: 10.1007/s12529-013-9297-y
40. Jungmann SM, Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? J Anxiety Disord. (2020) 73:102239. doi: 10.1016/j.janxdis.2020.102239
41. Cisler JM, Olatunji BO, Feldner MT, Forsyth JP. Emotion regulation and the anxiety disorders: an integrative review. J Psychopathol Behav Assessment. (2010) 32:68–82. doi: 10.1007/s10862-009-9161-1
42. Church LD, Shayani DR, Stumps A, Bounoua N, Wieand K, Spielberg JM. Gender differences in the transactional associations between anxiety sensitivity and emotion regulation over time. J Mood Anxiety Disord. (2023) 4:100037. doi: 10.1016/j.xjmad.2023.100037
43. Allan NP, Norr AM, Macatee RJ, Gajewska A, Schmidt NB. Interactive effects of anxiety sensitivity and emotion regulation on anxiety symptoms. J Psychopathol Behav Assessment. (2015) 37:663–72. doi: 10.1007/s10862-015-9484-z
44. Kashdan TB, Zvolensky MJ, McLeish AC. Anxiety sensitivity and affect regulatory strategies: Individual and interactive risk factors for anxiety-related symptoms. J Anxiety Disord. (2008) 22:429–40. doi: 10.1016/j.janxdis.2007.03.011
45. Asnaani A, Tyler J, McCann J, Brown L, Zang Y. Anxiety sensitivity and emotion regulation as mechanisms of successful CBT outcome for anxiety-related disorders in a naturalistic treatment setting. J Affect Disord. (2020) 267:86–95. doi: 10.1016/j.jad.2020.01.160
46. Schmidt NB, Mitchell M, Keough M, Riccardi C. Anxiety and its disorders. In: Distress tolerance: Theory, research, and clinical applications. Guilford Press, New York, NY (2011). p. 105–25.
47. Michel NM, Rowa K, Young L, McCabe RE. Emotional distress tolerance across anxiety disorders. J Anxiety Disord. (2016) 40:94–103. doi: 10.1016/j.janxdis.2016.04.009
48. Kraemer KM, Luberto CM, McLeish AC. The moderating role of distress tolerance in the association between anxiety sensitivity physical concerns and panic and PTSD-related re-experiencing symptoms. Anxiety Stress Coping. (2013) 26:330–42. doi: 10.1080/10615806.2012.693604
49. Probert-Lindström S, Perrin S. An examination of distress tolerance, anxiety sensitivity, and intolerance of uncertainty in adults in routine psychiatric care. Acta Psychol (Amst). (2023) 235:103902. doi: 10.1016/j.actpsy.2023.103902
50. Ranney RM, Berenz E, Rappaport LM, Amstadter A, Dick D, Spit for Science Working G. Anxiety sensitivity and distress tolerance predict changes in internalizing symptoms in individuals exposed to interpersonal trauma. Cognit Ther Res. (2022) 46:217–31. doi: 10.1007/s10608-021-10234-4
51. Allan NP, Macatee RJ, Norr AM, Schmidt NB. Direct and interactive effects of distress tolerance and anxiety sensitivity on generalized anxiety and depression. Cognit Ther Res. (2014) 38:530–40. doi: 10.1007/s10608-014-9623-y
52. Naragon-Gainey K, McMahon TP, Chacko TP. The structure of common emotion regulation strategies: A meta-analytic examination. Psychol Bull. (2017) 143:384–427. doi: 10.1037/bul0000093
53. Tull MT, Aldao A. Editorial overview: New directions in the science of emotion regulation. Curr Opin Psychol. (2015) 3:iv–x. doi: 10.1016/j.copsyc.2015.03.009
54. Jeffries ER, McLeish AC, Kraemer KM, Avallone KM, Fleming JB. The role of distress tolerance in the use of specific emotion regulation strategies. Behav Modif. (2016) 40:439–51. doi: 10.1177/0145445515619596
55. Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. (2010) 30:217–37. doi: 10.1016/j.cpr.2009.11.004
56. Larrazabal MA, Naragon-Gainey K, Conway CC. Distress tolerance and stress-induced emotion regulation behavior. J Res Personality. (2022) 99:104243. doi: 10.1016/j.jrp.2022.104243
57. Van Eck K, Warren P, Flory K. A variable-centered and person-centered evaluation of emotion regulation and distress tolerance: links to emotional and behavioral concerns. J Youth Adolesc. (2017) 46:136–50. doi: 10.1007/s10964-016-0542-y
58. Norton PJ, Sexton KA, Walker JR, Ron Norton G. Hierarchical model of vulnerabilities for anxiety: replication and extension with a clinical sample. Cognit Behav Ther. (2005) 34:50–63. doi: 10.1080/16506070410005401
59. Salkovskis PM, Rimes KA, Warwick HM, Clark DM. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med. (2002) 32:843–53. doi: 10.1017/s0033291702005822
60. Panahi S, Asghari Moghadam MA, Shaeeri MR, Eghtedar Nejhad S. Psychometric properties of a Persian version of the short form of health anxiety inventory in non-clinical Iranian populations. Q Educ Measurement. (2010) 1:21–46.
61. Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess. (2007) 19:176–88. doi: 10.1037/1040-3590.19.2.176
62. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. (2003) 85:348–62. doi: 10.1037/0022-3514.85.2.348
63. MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. (2002) 7:83–104. doi: 10.1037/1082-989x.7.1.83
64. Kline RB. Principles and practice of structural equation modeling. 4th ed. New York, NY: Guilford Press (2023).
65. Warren AM, Zolfaghari K, Fresnedo M, Bennett M, Pogue J, Waddimba A, et al. Anxiety sensitivity, COVID-19 fear, and mental health: results from a United States population sample. Cognit Behav Ther. (2021) 50:204–16. doi: 10.1080/16506073.2021.1874505
66. Fergus TA, Bardeen JR. Anxiety sensitivity and intolerance of uncertainty: Evidence of incremental specificity in relation to health anxiety. Pers Individ Differences. (2013) 55:640–4. doi: 10.1016/j.paid.2013.05.016
67. Blakey SM, Abramowitz JS. Psychological predictors of health anxiety in response to the zika virus. J Clin Psychol Med Settings. (2017) 24:270–8. doi: 10.1007/s10880-017-9514-y
68. Abramowitz JS, Braddock A. Psychological Treatment of Health Anxiety and Hypochondriasis: A Biopsychosocial Approach. Cambridge, MA: Hogrefe & Huber (2008).
69. Krautwurst S, Gerlach AL, Gomille L, Hiller W, Witthöft M. Health anxiety – An indicator of higher interoceptive sensitivity? J Behav Ther Exp Psychiatry. (2014) 45:303–9. doi: 10.1016/j.jbtep.2014.02.001
70. Gerolimatos LA, Edelstein BA. Predictors of health anxiety among older and young adults. Int Psychogeriatr. (2012) 24:1998–2008. doi: 10.1017/s1041610212001329
71. Pickett SM, Lodis CS, Parkhill MR, Orcutt HK. Personality and experiential avoidance: A model of anxiety sensitivity. Pers Individ Differences. (2012) 53:246–50. doi: 10.1016/j.paid.2012.03.031
72. Canlı D, Karaşar B. Health anxiety and emotion regulation during the period of COVID-19 outbreak in Turkey. Psychiatr Danub. (2020) 32:513–20. doi: 10.24869/psyd.2020.513
73. Fergus TA, Asmundson GJG. Cognitive and behavioral mechanisms of health anxiety. In: The clinician’s guide to treating health anxiety: Diagnosis, mechanisms, and effective treatment. Elsevier Academic Press, San Diego, CA, US (2019). p. 43–64.
74. Scarlett L, Baikie E, Chan SWY. Fear of falling and emotional regulation in older adults. Aging Ment Health. (2019) 23:1684–90. doi: 10.1080/13607863.2018.1506749
75. Singh K, Brown RJ. From headache to tumour: An examination of health anxiety, health-related Internet use and ‘query escalation’. J Health Psychol. (2016) 21:2008–20. doi: 10.1177/1359105315569620
76. Błachnio A, Przepiórka A, Kot P, Cudo A, Steuden S. The role of emotional functioning in the relationship between health anxiety and cyberchondria. Curr Psychol. (2023) 42:31240–50. doi: 10.1007/s12144-022-04126-3
77. Mitchell MA, Riccardi CJ, Keough ME, Timpano KR, Schmidt NB. Understanding the associations among anxiety sensitivity, distress tolerance, and discomfort intolerance: A comparison of three models. J Anxiety Disord. (2013) 27:147–54. doi: 10.1016/j.janxdis.2012.12.003
78. Lass ANS, Winer ES, Collins AC, Rokke PD. The associations among distress tolerance, unhelpful coping behaviors, and symptoms of depression: A network analysis. Cognit Ther Res. (2020) 44:1077–90. doi: 10.1007/s10608-020-10131-2
79. Mansueto G, Jarach A, Caselli G, Ruggiero GM, Sassaroli S, Nikčević A, et al. A systematic review of the relationship between generic and specific metacognitive beliefs and emotion dysregulation: A metacognitive model of emotion dysregulation. Clin Psychol Psychother. (2024) 31:e2961. doi: 10.1002/cpp.2961
80. Palmieri S, Sassaroli S, Ruggiero GM, Caselli G, Spada MM, Mansueto G. Emotion dysregulation in patients with eating disorders: the role of metacognitions and repetitive negative thinking. Cognit Ther Res. (2023) 47:655–68. doi: 10.1007/s10608-023-10398-1
81. Mansueto G, Marino C, Palmieri S, Offredi A, Sarracino D, Sassaroli S, et al. Difficulties in emotion regulation: The role of repetitive negative thinking and metacognitive beliefs. J Affect Disord. (2022) 308:473–83. doi: 10.1016/j.jad.2022.04.086
82. Mansueto G, Palmieri S, Sassaroli S, Ruggiero GM, Caselli G, Calligaro D, et al. Emotion dysregulation in participants with substance use disorders: A metacognitive perspective. J Affect Disord. (2024) 363:63–71. doi: 10.1016/j.jad.2024.07.144
83. Pederson LD. Dialectical behavior therapy: A contemporary guide for practitioners. Chichester, United Kingdom: John Wiley & Sons (2015). doi: 10.1002/9781118957882
84. Neacsiu AD, Eberle JW, Kramer R, Wiesmann T, Linehan MM. Dialectical behavior therapy skills for transdiagnostic emotion dysregulation: A pilot randomized controlled trial. Behav Res Ther. (2014) 59:40–51. doi: 10.1016/j.brat.2014.05.005
85. Hedman-Lagerlöf E, Axelsson E. Chapter six - cognitive behavioral therapy for health anxiety. In: Hedman-Lagerlöf E, editor. The Clinician’s Guide to Treating Health Anxiety. London, United Kingdom: Academic Press (2019). p. 79–122. doi: 10.1016/j.brat.2014.05.005
Keywords: anxiety sensitivity, health anxiety, distress tolerance, emotion regulation, transdiagnostic approach
Citation: Mohsenabadi H, Pirmoradi M, Zahedi Tajrishi K and Gharraee B (2025) A transdiagnostic approach to investigate of the relationships between anxiety sensitivity and health anxiety: the mediated roles of distress tolerance and emotion regulation. Front. Psychiatry 16:1478442. doi: 10.3389/fpsyt.2025.1478442
Received: 09 August 2024; Accepted: 20 January 2025;
Published: 05 February 2025.
Edited by:
Carlos Forero, International University of Catalonia, SpainReviewed by:
Giovanni Mansueto, University of Florence, ItalyNéstor Sánchez Martínez, Spanish National Research Council (CSIC), Spain
Copyright © 2025 Mohsenabadi, Pirmoradi, Zahedi Tajrishi and Gharraee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammadreza Pirmoradi, UGlybW9yYWRpLm1yQGl1bXMuYWMuaXI=
 Hamid Mohsenabadi
Hamid Mohsenabadi Mohammadreza Pirmoradi*
Mohammadreza Pirmoradi* Komeil Zahedi Tajrishi
Komeil Zahedi Tajrishi