- 1School of Nursing, Taihu University of Wuxi, Wuxi, China
- 2Department of Psychiatry, The Affiliated Mental Health Center of Jiangnan University, Wuxi, China
Objective: To investigate the sleep status and mental health of migrants elderly who followed their children (MEFC) and analyze the influencing factors.
Methods: A total of 583 MEFCs were surveyed using a general demographic questionnaire, the Pittsburgh Sleep Quality Index (PSQI) scale, and the Symptom Checklist 90 (SCL90) scale.
Results: The mean PSQI score for MEFCs was 6.98 ± 0.17, and the average SCL90 score was 64.06 ± 2.03. Multiple linear regression analysis indicated that health status and adaptation to the migration destination were associated with PSQI scores (P < 0.05). Health status, adaptation to the migration destination, and family harmony were associated with SCL90 scores (P < 0.05). The association coefficient between the total PSQI and SCL90 scores was r=0.462 (P < 0.05).
Conclusion: The sleep and mental health of MEFCs were at a normal level. Health status and adaptation influenced sleep status, while health status, adaptation, and family harmony impacted mental health. However, the association between mental health and sleep status was weak.
1 Introduction
Population aging is a problem that many countries and regions are facing (1). The World Health Organization predicts that by 2030, approximately one sixth of the global population will be over the age of 60 (2). By 2050, this proportion will rise to about one-fifth, and by then, the number of elderly people will reach 2.1 billion (3, 4). China is also facing the problem of an aging population (5). According to the Seventh National Census Bulletin of China (6), the population aged 60 and above has reached 260 million, accounting for 18.7% of the total population. The 2022 World Population Prospects report predicts that the elderly population aged 60 and above in China will significantly increase in the first half of the 21st century (7). It is expected that this population will reach its peak around 2050, with a total of approximately 580 million people. By 2050, 26.9% of China’s population will be over 65 years old (8–10). In recent years, the rapid growth of the Chinese economy has triggered changes in the social structure (11). The urbanization process in China has rapidly improved, with 49.68% in 2010 and 63.89% in 2020 (12, 13). More than 200 million rural people have migrated to cities and temporarily reside in there to obtain better employment opportunities (14). With the large-scale migration of people, China’s traditional family structure(all family members and relatives reside in the same area) is being disrupted. Many adults migrate for employment, leaving their original families behind, thus giving rise to special groups such as left-behind children (15), elders left behind (16), empty-nesters (17), solitary elders (18), and migrants elderly following their children (19). This article focuses on MEFCs(migrant elderly who relocate to follow their children).According to the Seventh National Census conducted by the National Bureau of Statistics, China has 264 million elderly individuals aged 60 and above, of which 13.72 million are part of the mobile population, with MEFCs accounting for 43% of this group (6). This study adopts the definition proposed by Fanlei Kong, they are elderly individuals who relocate to other regions to care for their grandchildren or support their children. The age of elderly individuals should be over 55 years old at least (20). Research on this group is limited internationally, with most studies focusing on China (21–23). This disparity may arise because migration patterns for elderly individuals differ between China and other countries. In Western countries, elderly individuals typically migrate voluntarily to access better retirement services, while in China, elderly individuals migrate mainly for family obligations, often not entirely by voluntary choice. They may have unique physical or mental difficulties (23). This study aims to examine sleep quality as a survival indicator and explore its relationship with mental health. By focusing on the sleep and mental health of MEFCs, this study seeks to understand their living conditions and provide a theoretical basis for future improvements in their quality of life.
Sleep is the longest activity that occupies 24 hours a day, and it is an important indicator of quality of life. Compared to young people and children, elderly people are more likely to experience sleep disorders (24, 25). In summary, common sleep disorders among elderly people include insomnia, early awakening, frequent nighttime awakenings, obstructive sleep apnea, restless leg syndrome, and so on (14, 26–28). But not all elderly people will experience sleep disorders, and the frequency of sleep disorders varies in different regions. For example, the incidence of insomnia among the elderly population ranges from 6-60% in different regions and it is not affected by rural or urban areas, developed or underdeveloped countries (29). Hublin (30) and Ursin’s (31) survey found that the prevalence of sleep disorders in Finland and Norway is 20.4% and 20% respectively. The prevalence of sleep disorders among Asian immigrants in the United States is 18.2% (32).The prevalence of sleep disorders among elderly people in China is 46% (33).There are few studies specifically studying the sleep status of MEFCs, but there is evidence to suggest that their sleep status may be better than that of elderly people living alone (34).
The World Health Organization defines mental health as: mental health is a good adaptive state, in which individuals are in a state of self harmony, actively interact with the environment, and can give full play to their mental potential (35). mental health includes emotional and social role taking components, as well as social skills and cognitive functions that affect participation in basic tasks and social roles (36). The elderly are prone to mental health problems due to withdrawal from social work, physical function decline and other reasons (37), In the past, there were many reports on the mental health problems of the elderly (38–41). According to a survey by the National Health Commission, 30.3% of older people in urban areas have mental health problems, while only 26.8% of older people in rural areas have mental health problems (42). According to China’s national mental health development report (released in 2021), depression is one of the common mental symptoms of the elderly in China. About one fifth (19.05%) of older people are in a mild depression state, and nearly one tenth (12.17%) of older people have moderate to high depression (43). There are also many reports on the mental health of the migrant elderly (44), most of which focus on depression and anxiety (45), loneliness (46), social adaptation and integration (47), and social support (48), while there are few studies on other aspects.
Regarding the influencing factors of sleep, some studies suggest that a decrease in melatonin secretion in the elderly can lead to more shallow sleep and less deep sleep in their sleep structure, making them prone to problems such as going to bed early, waking up early, and waking up frequently at night (24). Bad physical conditions, such as hypertension, diabetes, cardiovascular disease, depression, stress, cognitive impairment are also related to sleep disorders. Demographic characteristics and lifestyle factors may have an impact on the sleep quality of older people. For example, factors such as female gender, low education, divorce and widowhood, living alone, insufficient fruit intake, drinking tea, drinking alcohol, caffeine intake, use of certain drugs, falls, pain, and lack of physical activity are associated with poor sleep quality (49–51). Many studies have discussed the factors that affect mental health. One study summarized four dimensions that affect the mental health of the elderly: People’s own conditions (health status, people’s attitude, behavior, etc.), the impact of living places (public open space and residence, etc.), the impact of social, cultural and economic environment in life, and the impact of natural or man-made major disasters. As for the research on the relationship between sleep and mental health, previous studies believed that sleep and mental health may have a certain correlation (52, 53). However, its causal relationship has not yet been clear. We noticed that when studying the relationship between sleep and mental health of the elderly, most studies focused on the relationship between sleep status and depression, anxiety, loneliness (49, 52). Research on the relationship between other aspects of mental health and sleep is limited, and studies exploring the connection between sleep and the mental health of MEFCs are scarce.
Research on MEFCs first appeared in 2010 (54). Many studies have explored the problems of depression, anxiety, loneliness and social support of MEFCs (46, 55–57). However, there are few studies on the sleep problems of MEFCs (58). There are also few studies on the relationship between sleep and mental health of MEFCs (59). Our research will fill this gap. We investigated the sleep and mental health status of MEFCs, and analyzed its influencing factors and correlation, which will provide a theoretical basis for improving the quality of life of MEFCs.
2 Materials and methods
2.1 Research design
This was a cross-sectional survey conducted between June 20 and September 20, 2022. The study employed a convenient sampling method, conducting surveys in Shanghai, Jiangsu, Zhejiang, and Fujian provinces, targeting eligible migrant elderly individuals with questionnaires, including a general demographic questionnaire, the Pittsburgh Sleep Quality Index (PSQI), and the Symptom Checklist 90 (SCL90). This study did not involve animal or human experiments; all surveys were conducted with participants’ consent, the ethics committee of the Wuxi Taihu university approved the study.
2.2 Participants
Inclusion Criteria: MEFC aged 55 years or older who have left their original place of residence to live with their children settled elsewhere for more than six months. Exclusion Criteria: Individuals aged below 55 years, residents living locally, or those who have migrated for less than six months. Sample Size: A total of 626 questionnaires were distributed, with 583 valid questionnaires retrieved after excluding invalid responses, yielding a valid response rate of 93%.
2.3 Survey instrument
Relevant surveys were conducted using a general demographic questionnaire, the PSQI, and the SCL90 scales. The general demographic questionnaire included variables such as age, gender, educational background, health status, adaptation to the migration destination, family harmony level, income level, community facilities, and social activity participation.
The PSQI scale was used to evaluate participants’ sleep quality over the past month. The scale was developed by Buysse (60). It comprises 19 self-rated items and 5 observer-rated items, with 18 items forming 7 dimensions. Each dimension is scored on a scale of 0–3, and the total score ranges from 0 to 21, where higher scores indicate poorer sleep quality. A score of 0–5 indicates very good sleep quality, 6–10 indicates fair sleep quality, 11–15 indicates average sleep quality, and 16–21 indicates very poor sleep quality, the Cronbach’s α of Chinese PSQI is 0.994 (61).
The SCL90 scale is effective at distinguishing individuals with mental symptoms (potentially at risk of or already experiencing mental disorders). It is suitable for identifying a group’s potential mental disorders, types, and severity. It can also be used to examine the presence of psychosomatic illnesses. According to the Chinese normative data results, an SCL90 total score above 160 or an average item score above 2 suggests that further evaluation is needed. A score exceeding 200 indicates significant mental problems warranting mental counseling, while a score above 250 suggests more severe issues requiring detailed medical assessment, potential mental therapy, or medication under medical supervision. Using the Chinese version of SCL-90, the cronbach’s α of the scale is 0.98, the cronbach’s α of each factor score ranges from 0.80 to 0.91, and the validity of the scale is 0.963 (62, 63).
2.4 Survey process
After receiving training on the background information, questionnaire content and social survey skills of the whole study, 50 college students became investigators. These students are all sophomores majoring in nursing. The respondents were searched in the community where the investigator was located. After a 25 minute face-to-face interview between the investigator and the respondent, a questionnaire survey was conducted after confirming that the respondent met the screening conditions. The paper questionnaire and electronic questionnaire are used. The electronic questionnaire is preferred. If the survey object is inconvenient, the paper questionnaire is used. The questionnaire was completed anonymously, and the paper questionnaire was collected on the spot, while the electronic questionnaire was collected after the participants submitted all of their questionnaires. 626 MEFCs were initially selected and a questionnaire survey was conducted. The unqualified questionnaires were deleted, and 583 valid questionnaires were finally collected.
2.5 Statistical analysis
Data entry and statistical analysis were conducted using SPSS 22.0 software. Categorical data were described using proportions and percentages; continuous data were described using means and standard deviations. Group comparisons were conducted using t-tests or analysis of variance (ANOVA). Pearson correlation analysis was used to assess relationships, and multiple linear regression was employed to identify factors influencing MEFCs’ sleep and mental health.
3 Result
3.1 Sleep quality and mental health status of MEFCs
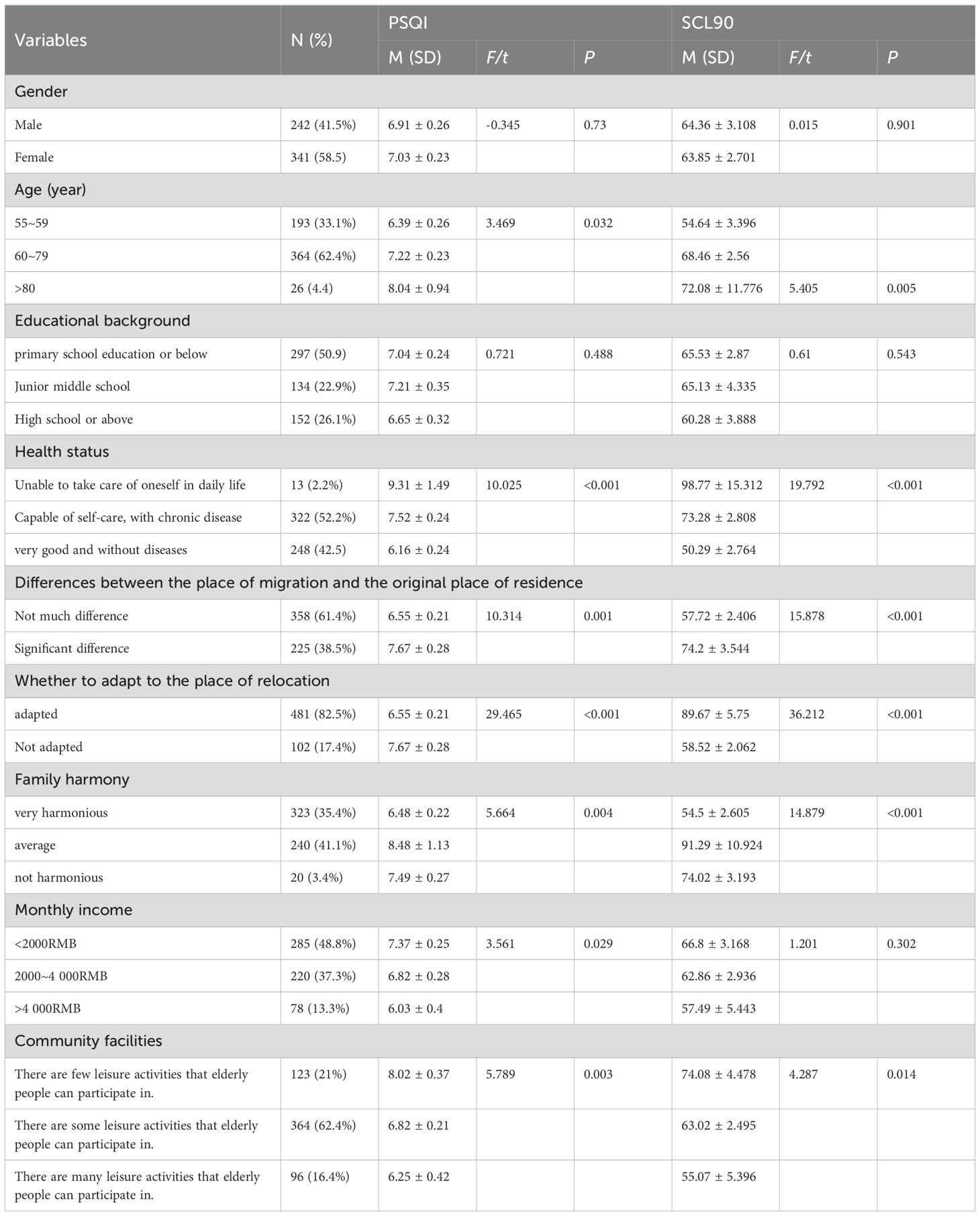
Table 1 presents the socio-demographic information of MEFCs. According to the data in Table 1, the study included 583 participants. The majority of participants were aged between 60 and 79 (62.4%), with 58.5% being female. Regarding education level, 26.1% of MEFCs participants had a high school education or above, while over half had a primary school education or below (50.9%). The monthly income level of MEFCs participants (48.8%) was less than 2000 yuan. Additionally, 52.2% of MEFCs participants suffered from chronic diseases.
The sleep quality of MEFCs was assessed using the PSQI scale, the total PSQI score was 6.98 ± 0.17, which falls into the “fair sleep quality” category. These results suggest that the overall sleep quality of MEFCs are within normal ranges.
Their mental health was evaluated using the SCL90 scale. The total SCL90 score was 64.06± 2.04, indicating “good mental health.” These results suggest that the overall mental health status of MEFCs are within normal ranges.
3.2 Factors influencing the sleep quality and the mental health of MEFCs
We investigated the relationship between nine items and sleep status and mental health status:: Gender (male/female); Age (55~59, 60~79, >80); Educational background (primary school or below, junior middle school, high school or above); Health status (unable to take care of oneself, capable of self-care with chronic disease, very good and without diseases);Is there a significant difference between the social and cultural environment of your new location and your previous place of residence? (not much difference, significant difference); Adaptation to the migration environment (adapted, not adapted); Family harmony level (very harmonious, average, not harmonious); Income level (<2000 yuan, 2000~4000 yuan, >4000 yuan); and Availability of recreational activities for the elderly in the community (few, some, many).
Multiple linear regression analysis revealed that health status and adaptation to the migration environment were significantly associated with the PSQI total score (P < 0.05), identifying them as the primary factors influencing sleep quality.
Multiple linear regression analysis showed that health status, adaptation to the migration environment, and family harmony were significantly associated with the SCL90 total score (P < 0.05), identifying them as the primary factors influencing mental health. Details are presented in Table 2.
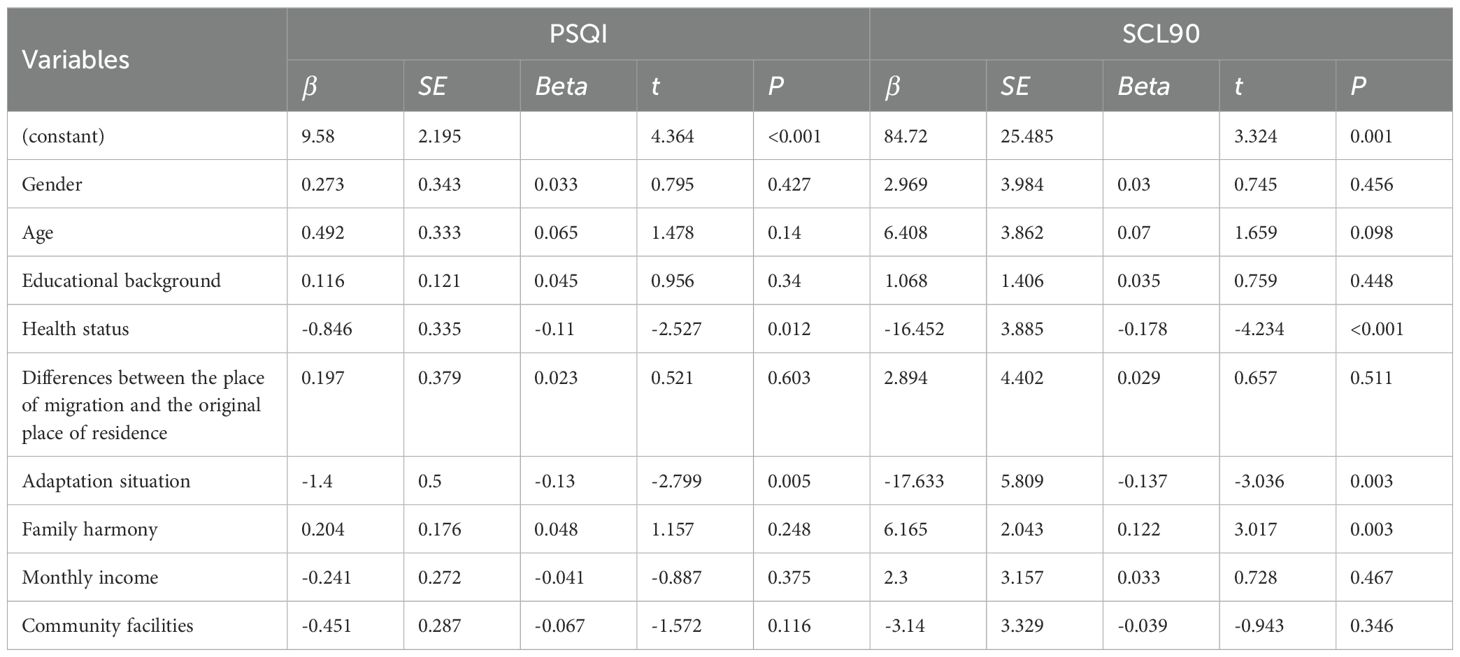
Table 2. multivariate analysis of sleep status scores and mental health status among MEFCs with different characteristics(n = 583).
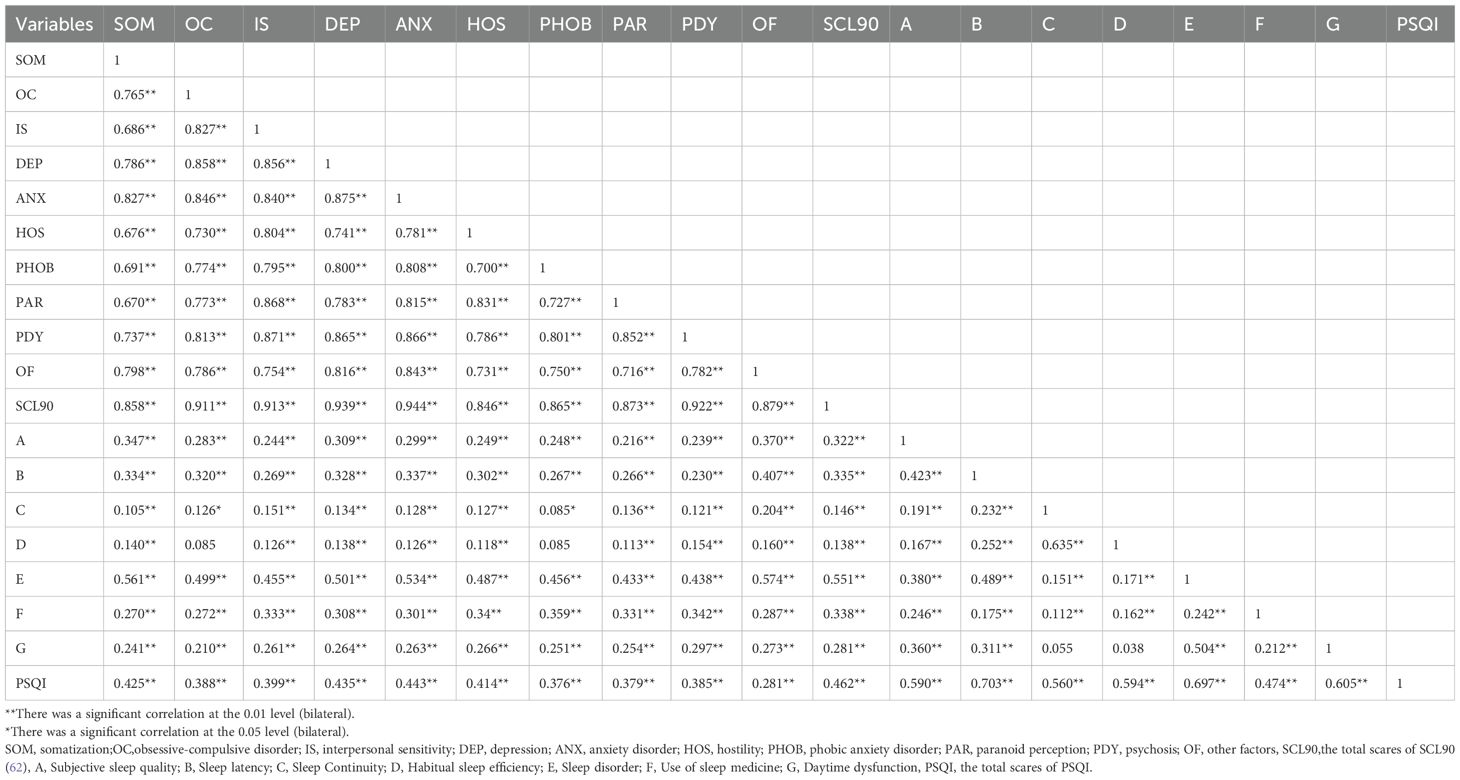
3.3 Correlation analysis between mental health and sleep quality
The correlation analysis was conducted on the mental health and sleep status of elderly people, and the results are as follows. The correlation coefficient between the total score of mental health status and sleep status is 0.462 (P<0.05), indicating a positive correlation between the mental health status and sleep status of migrant elderly people, but the correlation is not high. Details are presented in Table 3.
4 Discussion
In this survey, we analyzed the sleep and mental health status of MEFCs from Jiangsu, Shanghai, Fujian, Guangdong and other provinces in China, and investigated and analyzed the influencing factors. Our study found that the overall sleep and mental health status of MEFCs were at a normal level, and their health status and community adaptation status would affect their sleep status; health status, community adaptation and family harmony will affect mental health status. Sleep and mental health showed a positive correlation, but the correlation was not significant.
The PSQI score for MEFCs in this survey was 6.98 ± 0.17, and the score falls within the normal range, indicating that MEFCs’ sleep quality are normal. In this study, 10.1% of MEFCs suffered from sleep disorders. This finding compares favorably with Wang’s survey results, which indicated that 18.3% of MEFCs had sleep disorders (58).
According to the survey on the mental health of MEFCs, our study found that the average score of mental health of MEFCs was 64.06 ± 0.17, which was within the normal range.These findings align with Fanlei Kong ‘s (64) study, which also reported normal mental health in MEFCs. However, they contrast with Xiaona Yu ‘s (65) findings, which suggested poor mental health among MEFCs. She believes that among MEFCs, our study is inconsistent with Wang’s results. He believes that mental health has become one of the biggest challenges faced by MEFCs (44).
The survey results further indicated that health status and adaptation to the migration environment were independent factors influencing sleep quality, with statistically significant differences (P < 0.05).This result is consistent with previous results. The influencing factors of sleep include health, mental, social support, aging, and so on (26). These influencing factors are also applicable to MEFCs. Poor health, poor social adaptation will cause sleep disorders in the elderly (51, 66).
The results showed that health status, adaptation to the migration environment, and family harmony level were independent factors affecting mental health, with statistically significant differences (P < 0.05).This result is consistent with previous studies, mental health is related to many factors, and many studies have explored the influence of various factors on mental health. Some studies believe that people, places, processes and living environments may affect mental health (67). Previous studies have also shown that social support (68), health status (69), family harmony (42), and social adaptation (46, 70) can affect mental health.
Correlation analysis between sleep quality and mental health showed a positive but weak correlation (r =0.462), indicating a minimal relationship between the two. This result is consistent with previous studies (71). Most of the previous studies explored the relationship between depression and anxiety and sleep. People with depression and anxiety are more likely to have sleep disorders, and sleep disorders will also be reduced when the symptoms of depression and anxiety improve. This study confirms this view (52, 72).
This study innovatively investigated the living conditions of MEFCs from the perspective of sleep and mental health. In previous studies, most studies focused on the mental conditions of the elderly, such as anxiety, depression, loneliness (64, 65, 73–79). However, there are few studies on the sleep status of MEFCs (58), and there is little literature on the relationship between sleep and mental health status of MEFCs (64). Our research will fill the gap in this field. This research will help us more comprehensively understand the living status of the MEFCs, and provide a theoretical basis for improving the quality of life of MEFCs.
This study has several limitations. First, the cross-sectional data used cannot effectively establish causal relationships. Second, mental health includes various aspects, such as anxiety and depression, which were not discussed in this study but should be considered in future research. Third, other factors, such as medication use, may influence elderly sleep quality. Additionally, health-related information could act as a confounding factor. Future research should explore the impact of such factors on the sleep and mental health of the elderly. Fourth, there is still a lack of sufficient data on the correlation between the dimensions of mental health and sleep status, and the accurate correlation needs to be more determined in the future. Lastly, although we tried to expand the number of questionnaires collected, the snowball sampling method used in this paper is also a limiting factor, which may cause insufficient data collection.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Wuxi Taihu university. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KY: Writing – original draft. SS: Writing – original draft. LW: Investigation, Writing – original draft. ZC: Investigation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Jiangsu provincial natural science foundation for higher education 17KJD310004, 23KJD180008.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. (2020) 139:6–11. doi: 10.1016/j.maturitas.2020.05.018
2. Kanasi E, Ayilavarapu S, Jones J. The aging population: demographics and the biology of aging. Periodontology. (2016) 72:13–8. doi: 10.1111/prd.12126
3. United Nations. Decade of healthy ageing. World Health Organization (2022). Available at: https://www.who.int/initiatives/decade-of-healthy-ageing (Accessed April 18, 2023).
4. World Health Organization (WHO). Ageing and health. World Health Organization (2022). Available at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (Accessed March 23, 2023).
5. Hanmo Y. New trends in population ageing and new characteristics of the elderly population in China. Population Stud. (2022) 46:104–16.
6. National Bureau of Statistics. Bulletin of the Seventh National Population Census (No. 5) (2021). Available online at: https://www.stats.gov.cn/sj/tjgb/rkpcgb/qgrkpcgb/202302/t20230206_1902005.html (Accessed July 25, 2023).
7. United Nations. World Population Propects 2019,Volume II: Demographic Profiles (2022). Available online at: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/un_2019_wpp_vol2_demographic_profiles.pdf (Accessed December 06, 2022).
8. Fang EF, Xie C, Schenkel JA, Wu C, Long Q, Cui H, et al. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. (2020) 64:101174. doi: 10.1016/j.arr.2020.101174
9. Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, et al. The world report on ageing and health: A policy framework for healthy ageing. Lancet. (2016) 387:2145–54. doi: 10.1016/S0140-6736(15)00516-4
10. Peng X. China’s demographic history and future challenges. Science. (2011) 333:581–7. doi: 10.1126/science.1209396
11. Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, et al. Urbanisation and health in China. Lancet. (2012) 379:843–52. doi: 10.1016/S0140-6736(11)61878-3
12. Zhu YG, Jones KC. Urbanisation and health in China. Lancet. (2010) 376:232–3. doi: 10.1016/S0140-6736(10)61142-7
13. Islam J, Ali MJ, Mithun S. Slums in India: making sense of place in urban planning [Article; Early Access. GeoJournal. (2020) 87:1913–28. doi: 10.1007/s10708-020-10357-3
14. Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24:197–205. doi: 10.1016/j.arr.2015.08.003
15. Gao W. Research onmental health education of rural left behind children from the perspective of moral education. Jilin Educ. (2024) 36):43–5.
16. Gudongdong b. The spiritual needs of the rural left behind elderly to “help the poor”: theoretical interpretation, practical difficulties and path choice. Contemp economic Manage. (2025) 1:13.
17. Luo X, Wei X, Yanting X, Guowu X. Informal social support and physical andmental health of empty nest elderly in China: the moderating effects of chronic diseases. China Health Manage. (2024) 41:1292–6.
18. Niu D. Research on health care for the elderly living alone from the perspective of collaborative governance. Int Public relations. (2024) 18):101–3.
19. Guyuqi. The dilemma of spiritual and cultural needs of rural migrant elderly and its solutions. Int Public relations. (2024) 18):44–6.
20. Kong F, Kong M, Li C, Shixue L, Jun L. Relevant research progress at home and abroad on migrant elderly. Chin J Gerontology. (2020) 40:2443–7.
21. Zhenjing L, Li J, Li Y. The effect of psychotherapy on cognitive function in elderly patients with comorbidities of depression and anxiety. Chin J Health Psychol. (2016) 24:752–5.
22. Yu X. A survey on the current status of anxiety and depression in the elderly and a study on the impact of mental intervention on it. Master's Thesis. Qingdao, China: Qingdao University (2018).
23. Rojas V, Le Blanc HP, Sunil. TS. US retirement mi Mexico: understanding is sues of adaptation, networking, and social integration. Migration&Integration. (2014) 15:257–73. doi: 10.1007/s12134-013-0278-4
24. Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: Sleep disorders commonly found in older people. Can Med Assoc J. (2007) 176:1299–304.
25. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-Analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. (2004) 27:1255–73. doi: 10.1093/sleep/27.7.1255
26. Rodriguez JC, Dzierzewski JM, Alessi CA. Sleep problems in the elderly. Med Clin North Am. (2015) 99:431–9. doi: 10.1016/j.mcna.2014.11.013
27. Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult – a mini-review. Gerontology. (2010) 56:181–9. doi: 10.1159/000236900
28. Cooke JR, Ancoli-Israel S. Normal and abnormal sleep in the elderly. Handb Clin Neurol. (2011) 98:653–65. doi: 10.1016/B978-0-444-52006-7.00041-1
29. Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. (2018) 18:155–65. doi: 10.1111/psyg.12319
30. Hublin C, Kaprio J, Partinen M, Koskenvuo M. Insufficient sleep—A population-based study in adults. Sleep. (2001) 24:392–400. doi: 10.1093/sleep/24.4.392
31. Ursin R, Bjorvatn B, Holsten F. Sleep duration, subjective sleep need, and sleep habits of 40-to 45- year-olds in the Hordaland Health Study. Sleep. (2005) 28:1260. doi: 10.1093/sleep/28.10.1260
32. Lee S, Ryu S, Lee GE, Kawachi I, Morey BN, Slopen N. The association of acculturative stress with self-reported sleep disturbance and sleep duration among Asian Americans. Sleep. (2022) 45:zsab298. doi: 10.1093/sleep/zsab298
33. Wang Z, Zhao M, Chen T, Zile G. Sleep disturbance prevalence rate among Chinese older people: a meta-analysis. Chin Gen Pract. (2022) 5:2036–43.
34. Wang J, Pang M, Jiang X, Li H, Xu J, Liu G, et al. The chain mediation model of social support and life satisfaction among migrant older adults with children: The role ofmental health and sleep quality. Arch Gerontol Geriatr. (2023) 115:105122. doi: 10.1016/j.archger.2023.105122
35. WHO. Promotingmental health : concepts, emerging evidence, practice : summary report/a report from the World Health Organization, Department ofmental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. Geneva: World Health Organization (2004).
36. Hoisington AJ, Stearns-Yoder KA, Schuldt SJ, Beemer CJ, Maestre JP, Kinney KA, et al. Ten questions concerning the built environment andmental health. Build Environ. (2019) 155:58–69. doi: 10.1016/j.buildenv.2019.03.036
37. McDougall CW, Hanley N, Quilliam RS, Bartie PJ, Robertson T, Griffiths M, et al. Neighbourhood blue space andmental health: A nationwide ecological study of antidepressant medication prescribed to older adults. Landsc Urban Plan. (2021) 214:104132.
38. Murniati N, Al Aufa B, Kusuma D, Kamso S. A Scoping Review on Biopsychosocial Predictors ofmental Health among Older Adults. Int J Environ Res Public Health. (2022) 19:10909. doi: 10.3390/ijerph191710909
39. Yang J, Ren Y, Li J. The influence of physical exercise on the spiritual well-being of the elderly: the mediator role of mental resilience. Chin J Clin Psychol. (2021) 29:191–4. doi: 10.16128/j.cnki.1005-3611.2021.01.039
40. Werneck AO, Peralta M, Tesler R, Marques A. Cross-sectional and prospective associations of lifestyle risk behaviors clustering with elevated depressive symptoms among middle-aged and older adults. Maturitas. (2022) 155:8–13. doi: 10.1016/j.maturitas.2021.09.010
41. Zhang C, Zhang S, Niu Q. A new perspective of urban-rural differences: the impact of social support on themental health of the older adults: A case from shaanxi province, China. Healthcare. (2021) 9:112. doi: 10.3390/healthcare9020112
42. Li L, Yu L. The influence of pension mode on themental health of older adults-evidence from older adults in China. Int J Environ Res Public Health. (2021) 19:119. doi: 10.3390/ijerph19010119
43. Fu XL, Zhang K. Report on Nationalmental Health Development in China (2024). Available online at: https://cmhr.psych.ac.cn/NationalmentalHealthStatus.html (Accessed 19 July 2024).
44. Wang J, Lai DWL. mental health of older migrants migrating along with adult children in China: A systematic review. Ageing Soc. (2022) 42:786–811. doi: 10.1017/S0144686X20001166
45. Li H, Kong F. Effect of morbidities, depression, anxiety, and stress on oral health-related quality of life among migrant elderly following children in weifang, China. Int J Environ Res Public Health. (2022) 19:4677. doi: 10.3390/ijerph19084677
46. Xu J, Liu G, Li H, Jiang X, Zhou S, Wang J, et al. Association between social integration and loneliness among the female migrant older adults with children: the mediating effect of social support. BMC Geriatr. (2024) 24:4. doi: 10.1186/s12877-023-04569-8
47. Li Y. Research on the Social Readjustment of rural migrant elderly under the ecosystem theory – Based on the survey of J community in Luoyang. Zhongnan Agric Sci Technol. (2023) 44:126–128+134.
48. Zong D, Lu Z, Shi X, Shan Y, Li S, Kong F. Mediating effect of family support on the relationship between acculturation and loneliness among the migrant elderly following children in Jinan, China. Front Public Health. (2022) 10:934237. doi: 10.3389/fpubh.2022.934237
49. Su Y, Wang SB, Zheng H, Tan WY, Li X, Huang ZH, et al. The role of anxiety and depression in the relationship between physical activity and sleep quality: a serial multiple mediation model. J Affect Disord. (2021) 290:219–26. doi: 10.1016/j.jad.2021.04.047
50. Nguyen HT, Nguyen CC, Le Hoang T. Falls among older adults during the COVID-19 pandemic: a multicenter cross-sectional study in Vietnam. Clin Interv Aging. (2022) 17:1393–404. doi: 10.2147/CIA.S382649
51. Bolina AF, Rodrigues RAP, Tavares DMS, Haas VJ. Factors associated with the social, individual and programmatic vulnerability of older adults living at home. Rev Esc Enferm USP. (2019) 53:e03429–9. doi: 10.1590/S1980-220X2017050103429
52. Wu CY, Su TP, Fang CL, Chang MY. Sleep quality among community-dwelling elderly people and its demographic,mental, and physical correlates. J Chin Med Assoc. (2012) 75:75–80. doi: 10.1016/j.jcma.2011.12.011
53. Mahmoudi H, Saffari M, Movahedi M, Sanaeinasab H, Rashidi-Jahan H, Pourgholami M, et al. A mediating role formental health in associations between COVID – 19 - related self - stigma, PTSD, quality of life, and insomnia among patients recovered from COVID – 19. Brain Behav. (2021) 11:e02138.
54. Yao Z, Wang X. Spiritual life and community integration of the old person moving into the city. Soc Work. 9:43–5.
55. Liu G, Li S, Kong F. Association between Sense of belonging and loneliness among the migrant elderly following children in Jinan, Shandong Province, China: the moderating effect of migration pattern. Int J Environ Res Public Health. (2022) 19:4396. doi: 10.3390/ijerph19074396
56. Xie J, Zhu Q, Wang X. A study on the health status of China’s elderly migrant population and its influencing factors. Urban Dev Stud. (2020) 27:30–5.
57. Li H, Kong F. Effect of Morbidities, Depression, Anxiety, and Stress on Oral Health-Related Quality of Life among Migrant Elderly Following Children in Weifang, ChinaWhy elderly people who move with the family become vulnerable tomental disorders. Friends Older Comrades. (2020) 12:42–3.
58. Jiang X, Liu G, Xu J, Li H, Wang J, Pang M, et al. The relationship between oral health status, loneliness, and sleep quality among the migrant elderly following children in Weifang, Shandong Province, China: A comparative analysis on different migration types. Front Public Health. (2023) 10:1053690. doi: 10.3389/fpubh.2022.1053690
59. Wang J, Qin W, Pang M, Zhao B, Xu J, Li S, et al. The Effect of Chronic Disease andmental Health on Sleep Quality among Migrant Elderly Following Children in Weifang City, China. Int J Environ Res Public Health. (2022) 19:12734. doi: 10.3390/ijerph191912734
60. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
61. Liu X, Tang M, Hu L, Wang A, Wu H, Zhao G, et al. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiatry. (1996) 29:103–7.
62. Yu Y, Wan C, Huebner ES, Zhao X, Zeng W, Shang L. Psychometric properties of the symptom check list 90 (SCL-90) for Chinese undergraduate students. J Ment Health. (2019) 28:213–9. doi: 10.1080/09638237.2018.1521939
63. Shi LY, Huang SP, Zhuo L. Reliability validity and reference value of symptom checklist 90 for college students. Chin J Sch. Health. (2013) 34:223–4. doi: 10.16835/j.cnki.1000-9817.2013.02.035
64. Lu J, Liu K. Sleep quality andmental health of the elderly in China: evidence from longitudinal data. China popul. Dev Stud. (2021) 5:378–93. doi: 10.1007/s42379-021-00096-4
65. Zeng L, Yang Z, Zhang J, Wan R. The study on themental adaption and social integration of migrant workers. J Guizhou Educ Univ. (2017) 33:53–60.
66. Wang P, Song L, Wang K, Han X, Cong L, Wang Y, et al. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: a population-based study. Aging Clin Exp Res. (2020) 32:125–31. doi: 10.1007/s40520-019-01171-0
67. Vahabi S, Lak A, Panahi N. Driving the determinants of older people’smental health in the context of urban resilience: a scoping review. BMC Geriatr. (2023) 23:711. doi: 10.1186/s12877-023-04387-y
68. Yunlong D, Zhonghua Y, Xiangyi C. Correlation between social support, family function and subjective well-being of the elderly. Chin J Gerontology. (2012) 32:3501–3.
69. Yaka E, Keskinoglu P, Ucku R, Yener GG, Tunca Z. Prevalence and risk factors of depression among community dwelling elderly. Arch Gerontol Geriatr. (2014) 59:150–4. doi: 10.1016/j.archger.2014.03.014
70. Felton BJ, Shinn M. Social integration and social support: moving “social support” beyond the individual level. J Community Psychol. (1992) 20:103–15. doi: 10.1002/1520-6629(199204)20:2<103::AID-JCOP2290200202>3.0.CO;2-4
71. Orhan FO, Tuncel D, Taş F, Demirci N, Ozer A, Karaaslan MF. Relationship between sleep quality and depression among elderly nursing home residents in Turkey. Sleep Breath. (2012) 16:1059–67.
72. Peng L. Impact of sleep quality on themental health of in the elderly. Chin J Gerontology. (2013) 33:1622–4.
73. Liu G, Li S, Kong F. Association between social support, smartphone usage and loneliness among the migrant elderly following children in Jinan, China:a cross-sectional study. BMJ Open. (2022) 12:e060510.
74. Domènech-Abella J, Mundó J, Haro JM, Rubio-Valera M. Anxiety, depression, loneliness and social network in the elderly: longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J Affect Disord. (2019) 246:82–8. doi: 10.1016/j.jad.2018.12.043
75. Sultana R, Downer B, Chen NW, Raji M, Fernandez D, Al Snih S. Relationship between diabetes-related complications and sleep complaints in older mexican americans. J Prim Care Community Health. (2022) 13:1–8. doi: 10.1177/21501319221123471
76. Jing R, Xu T, Rong H, Lai X, Fang H. Longitudinal association between sleep duration and depressive symptoms in chinese elderly. Nat Sci Sleep. (2020) 12:737–47. doi: 10.2147/NSS.S269992
77. Zaidel C, Musich S, Karl J, Kraemer S, Yeh CS. Psychosocial factors associated with sleep quality and duration among older adults with chronic pain. Popul Health Manage. (2021) 24:101–9. doi: 10.1089/pop.2019.0165
78. Alves ÉS, Pavarini SCI, Luchesi BM, Ottaviani AC, Cardoso JFZ, Inouye K. Duration of night sleep and cognitive performance of community older adults. Rev Latino-Am Enfermagem. (2021) 29:e3439–9. doi: 10.1590/1518-8345.4269.3439
Keywords: MEFC, sleep status, mental health, investigation, elderly people
Citation: Yu K, Song S, Wu L and Chen Z (2025) Investigation and analysis of sleep and mental health status among MEFCs. Front. Psychiatry 16:1458291. doi: 10.3389/fpsyt.2025.1458291
Received: 02 July 2024; Accepted: 10 January 2025;
Published: 28 January 2025.
Edited by:
Angela J Grippo, Northern Illinois University, United StatesReviewed by:
Xiaoxu Jiang, Shandong University, ChinaWiwik Afridah, Nahdlatul Ulama University of Surabaya, Indonesia
Copyright © 2025 Yu, Song, Wu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhe Chen, NDUwNzI1OTcxQHFxLmNvbQ==
 Kangying Yu
Kangying Yu Shaozheng Song1
Shaozheng Song1 Zhe Chen
Zhe Chen