
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 14 February 2025
Sec. Public Mental Health
Volume 16 - 2025 | https://doi.org/10.3389/fpsyt.2025.1456909
This article is part of the Research TopicSexual Violence in Times of ConflictView all 4 articles
 Tsion Michael1
Tsion Michael1 Solomon Moges Demeke2*
Solomon Moges Demeke2*Introduction: Common mental disorders (CMDs) and suicidality are two of the most common psychological and mental health issues associated with acute and chronic sexual and gender-based violence (SGBV). Thus, the purpose of this study was to determine the magnitude of symptoms of CMDs, and suicidality among females experienced SGBV in Ethiopia.
Method: A cross-sectional study was conducted among 407 female survivors of SGBV in the One Stop Centers of the Amhara region. Data analysis was performed using SPSS version 25. The odds ratio at a p-value of 0.05 was used to determine the strength of the association of the independent variables with CMDs and suicidality.
Results: A total of 407 women participated in the study. Suicidality was reported by a quarter of the survivors (24.1%), while CMDs were reported by nearly two-thirds (61.7%). Being widowed (AOR = 3.0, 95% CI = 3.0 [1.22, 7.66]), having a family history of mental illnesses (AOR = 7.1, 95% CI = 7.1 [4.07, 12.39)], being low-income (AOR = 2.8, 95% CI = 2.8 [1.64, 5.06]), and current drug use (AOR = 2.9, 95% CI = 2.9 [1.63, 5.16]) were all linked with CMDs. Having a history of abortion (AOR = 4.1, 95% CI = 4.1 [1.9, 8.5]), CMDs (AOR = 4.6, 95% CI = 4.6 [2.0, 10.74]), and history of suicide (AOR = 3.41, 95% CI = 3.41 [1.22, 9.55]) were some of the characteristics that were substantially linked with suicidality.
Conclusion: Females with SGBV had a high prevalence of CMDs and suicidality and calls for comprehensive remedies.
Women residing in areas affected by conflict often endure widespread atrocities such as massacres, bombings, and the destruction of their homes. They also suffer injuries and fatalities, leading to displacement, ongoing insecurity, and poverty (1). Women are particularly susceptible to violence and hardships during times of war that are directly linked to their gender. For instance, sexual violence and rape are frequently employed as tactics in warfare in various global conflicts (2, 3).
SGBV is any assault, physical or verbal compulsion, or life-threatening deprivation aimed at a specific woman or girl that results in physical or psychological pain, misery, or the arbitrarily deprived of one’s freedom and fosters female subordination (4, 5). Sexual violence has the potential to inflict severe harm on the mental well-being of the victim, leading to serious impacts in the short, medium, or long term (6). Women are at risk of being kidnapped and forced into slavery, often subjected to torture and sexual abuse (7).
In areas affected by conflict, women and girls are at a higher risk of gender-based violence, which not only results in negative health effects but also hinders their ability to find work and participate in efforts to rebuild (8). During periods of conflict and displacement, women frequently bear a disproportionate burden of sexual violence and exploitation (9, 10). Research has shown that there are alarming rates of sexual violence in areas affected by conflict, with numbers ranging from 2.6% in Ukraine to 21.3% in South Sudan. Terribly, acts of sexual violence and human rights violations related to war persist worldwide, especially during conflicts in both low-income and some high-income nations (2, 11–16).
Gender-based violence (GBV) can have severe consequences on individuals’ physical and mental well-being, resulting in unplanned pregnancies, sexually transmitted infections, and fostering discrimination, stigma, and social isolation within families and communities. It is essential to address GBV and provide assistance to survivors to prevent these negative effects and facilitate healing and recovery (13, 17). There is a clear link between violence and mental health issues among women in research conducted in various countries with different income levels (18–21). The combination of war-related and gender-based violence is likely to have a detrimental impact on the health of women affected by conflict (22, 23). The impact of sexual violence during times of war can have severe psychological effects on survivors. These effects may manifest as post-traumatic stress disorder, anxiety disorders, physical symptoms with no apparent medical cause, psychological pain, dissociative disorders, severe depression, self-harming behaviors including suicidal thoughts, substance abuse, and a distorted perception of oneself and the world (19, 24–26). Gender-based violence is a significant factor in triggering mental health issues in women, stemming from a traumatic experience (27, 28). Females who have encountered gender-based violence are at a substantially greater likelihood of experiencing mental health problems within one to five years following the traumatic incident (29). A study conducted in Australia found that females who have been victims of GBV are twice as probable (58%) to develop typical mental illnesses like depression, anxiety, PTSD, substance abuse, or attempted suicide when compared to females who have not faced GBV (25).
The magnitude of gender-based violence among women in Ethiopia during wartime is alarmingly high, significantly linked to common mental disorders and suicidal behaviors. A study in North Shewa found a GBV prevalence of 58%, with psychological violence at 55%, physical violence at 30.1%, and sexual violence at 16% (30). In Tigray, 43.3% of women experienced at least one type of GBV, with 9.7% reporting sexual violence and 28.6% physical violence (31). Survivors often face mental health challenges, including anxiety (38.6%), depression (27.5%), and post-traumatic stress disorder (12.1%) (31). The SGBV often contributes to suicidal behaviors, with many survivors expressing feelings of hopelessness and isolation (32). A meta-analysis revealed that approximately 46.93% of women experience lifetime VAW, with 37.02% facing violence in the past year (33).
Sexual violence during times of conflict is a serious concern that frequently goes unnoticed or inadequately documented because of a variety of reasons. These may include the protracted duration of conflicts, societal and cultural obstacles, as well as other intricate factors (34). However, to the best of our knowledge no research has been conducted on the association of SGBV with common mental disorders and suicidal behaviors during times of war in Ethiopia. This study aimed to investigate the magnitude of symptoms of common mental disorders and suicidality among women SGBV survivors, as well as the factors associated with these issues. The results of this study will serve as a foundation to understand the extent of potential mental health consequences among GBV survivors in the Amhara Region of Ethiopia during periods of conflict. Additionally, the findings will offer valuable insights for humanitarian organizations, national and local authorities, in order to provide comprehensive support for survivors and to reduce the burden of the mental health consequences of SGBV.
An institutional based cross-sectional study was conducted from December/2022 to March/2023, focusing on survivors of gender-based violence in the Amhara Region. The Amhara region of Ethiopia has a vibrant historical and cultural background shaped by its ethnic identity and socio-political dynamics. Known for its diverse cultural heritage, it offers numerous attractions that entice tourists globally (35). The region has been deeply impacted by war-related sexual violence, especially during the recent conflict involving the Tigray People’s Liberation Front. These acts have resulted in severe psychological and physical consequences for survivors. A total of 407 women who had sought assistance from the One Stop Centers in Debre Birhan, Dessie, and Woldia were included in the research. One-Stop Centers (OSCs) are facilities that offer an integrated, multi-sectoral response to the needs of survivors of SGBV in a single location. This facilitates access to essential services during a traumatic period and helps reduce trauma by minimizing the number of providers involved. As a result, survivors can avoid the distress of repeatedly recounting their experiences (36). These centers are designed to provide integrated services to survivors, ensuring access to medical, psychological, and legal support all in one location. They provide free services, including medical evaluations, treatment, psychosocial support, and legal aid. The center is staffed by a dedicated team that includes general practitioners, midwives, nurses, psychologists, pharmacists, laboratory professionals, and legal advisors (37). These centers were chosen from three different zones within the region. The participants were selected using a purposive sampling method, after the sample size proportionally allocated to each center.
Individuals 18 years and older were eligible to participate in the research study. The data were gathered by three local female professionals who are experts in psychology and social work, working at the One Stop Centers. Participants who were seriously ill, mentally incapacitated, or physically disabled were not included in the study. The Institutional Review Board of Addis Ababa University approved all procedures of the study, and ethical approval was obtained from each study site. Additionally, a support letter was obtained from the administrator of each study site. Prior to the interviews, verbal consent was obtained from all participants. They were informed that participation was voluntary and they had the right to withdraw at any time. Confidentiality of the information provided was guaranteed. Participants were also informed about their right to decline participation or withdraw at any time. Those who screened positive during the data collection process were referred to mental health services at the Hospital for further evaluation. The study followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) reporting guidelines.
Data was collected using a structured interviewer administered questionnaire to gather information on socio-demographic details, stress factors, the level of social support, the presence of medical conditions and a family background of mental disorders, as well as past or present use of substances for non-medical purposes.
The first part of the structured interview comprised questions assessing sociodemographic characteristics of the participants. This included age, marital status, religion, residence, educational level, participant occupational status, partner’s educational level, spouse’s occupational status, and income.
Symptoms of CMDs were assessed using the 20-item Self-Reporting Questionnaire (SRQ-20). SRQ has 20 items that indicate symptoms of non-psychotic mental illnesses. The SRQ-20 has a high internal consistency reliability (0.78), a sensitivity of 78.6%, and a specificity of 81.5% (38). Participants were taken to have CMDs in the previous month if their score was above or equal to eight (39).
the three forms of suicidal behaviors include suicidal ideation, planning, and attempt. The revised suicidal behavior questionnaire (SBQ-R) was used to assess suicidal behaviors. It has an overall result ranges from 3-18; participants who scored greater than or equal to seven were indicating suicidal behaviors (40).
the first two items of WHO ASSIST (Alcohol, Smoking, and Substance Involvement Screening Test) were employed to assess lifetime and present substance use. Current users had used substances (alcohol, khat, cigarettes) in the previous three months. Those who had used substances (alcohol, khat, cigarettes, and others) at least once were considered ever-users (41).
the List of Threatening Experiences (LTE) was used to evaluate stressful situations. It was designed to assess stressful life experiences and includes 12 types of unpleasant life occurrences. Participants were divided into two groups: those who experienced stressful life events of 0, 1, or 2 and those who had at least one or more tough life events in the prior six months (42).
the participants’ social support was assessed using the Oslo social support scale (Oslo-3). According to the Oslo social support scale (Oslo-3), which has a score range of 3 to 14, participants with scores of three to eight were considered to receive poor social support, and those with scores of 9 to 11 were considered to have moderate social support. In contrast, those with scores of between 12 and 14 were considered to have good social support (43).
The structured questionnaires were prepared in English, translated into Amharic (the local language) and then back translated into English to ensure the reliability and comprehensibility of the instruments by different language experts. The instruments were pretested in 5% (21) of the sample size in Shewa Robit Hospital. The final version of the questionnaires was established following the feedback from the pre-test. Data collectors and supervisors received a training regarding the study instruments and procedures, and ethical issues. The questionnaires were checked for its consistency and understandability. Supervisors carried out supervision at each site. The filled questionnaires were checked for completeness and reliability. Informed consent was obtained from each participant in verbal form prior to assessments.
At the end of the data collection, the questionnaires were checked for completeness. The data were edited, cleaned, coded, and entered into the computer using Epi-Data 4.6 version and exported, and analyzed using Statistical Package for Social Sciences (SPSS) version 25 (IBM). Analysis was done using both descriptive and inferential statistics. Descriptive statistics were used to describe the findings, including frequencies, and percentages. The presence of an association between symptoms of common mental disorders and suicidality, and independent variables was assessed using logistic regression analysis. Variables significant at bi-variable logistic regression i.e., p < 0.20 were entered into multivariable logistic regression. Statistical significance was considered at a p-value less than 0.05, and the strength of association was estimated in odds ratio with a 95% confidence interval.
The study included a total of 407 participants, with a response rate of one hundred percent. More than half of the respondents, 58%, were Orthodox Christians, 35.6% were Muslims, and 6.4% were Protestants. Below half were married (167 [41%]), while (113 [27.8%]), (85 [20.9%]), (42 [10.3%]), were single, widowed, and divorced or separated respectively. Three fourth of the participants (309 [75.9%]) lived in urban. Most participants (251 [61.7%]) had complete primary school (See Table 1).
More than half of the respondents (50.6%) had relatives with a history of mental illness, and more than three-quarters (79.9%) had suffered physical harm due to the sexual assault. Around 19.4% had unwanted pregnancies, 17% aborted pregnancies, and 2.5% gave birth to unwanted children. Three-fourths (75.2%) of the participants used substances in their lifetime, and 69.3% used them in the past three months (See Table 2).
Regarding the specific numbers related to the SGBV experienced by the participants, 224 (55.1%) reported experiencing physical violence, 101 (24.8%) reported sexual violence, and 82 (20.1%) reported emotional and psychological violence. Of those who had SGBV nearly two third (61.7%) of the participants were found to have common mental disorders (95% CI = [56.8% - 66.3%]) whereas 24.1% of the participants reported having suicidal behaviours (95% CI = [19.37% - 28%]) (See Figures 1, 2). Suicidal thought, plan, and attempt rates have been determined as (206 [50.6%], 21 [5.1%], and 68 [16.8%]), respectively.
The study found the following factors to be significantly associated with common mental disorders: being widowed, having a family history of mental illness, a poor income, experiencing a stressful life event, and substance use in the previous three months. Compared to their counterparts, widowed participants had three times the odds of having common mental disorders (AOR= 3.0, 95% CI= [1.22 to 7.66]). When compared to those who did not have a family history of mental illness, the odds of developing common mental disorders were 7.1 times higher (AOR=7.1, 95% CI; [4.07 to 12.39]). Participants with less than 3052.4 ETB in a month’s earnings were 2.8 times (AOR=2.8, 95% CI= [1.64 to 5.06]) more likely to have common mental disorders than those with more than 3052.4 ETB in income per month. The odds of developing common mental disorders were 2.9 times greater among those who used substances (AOR=2.9, 95% CI= [1.63, 5.16]) than among nonusers. Age and social support were found to be unrelated to CMDs (See Table 3).
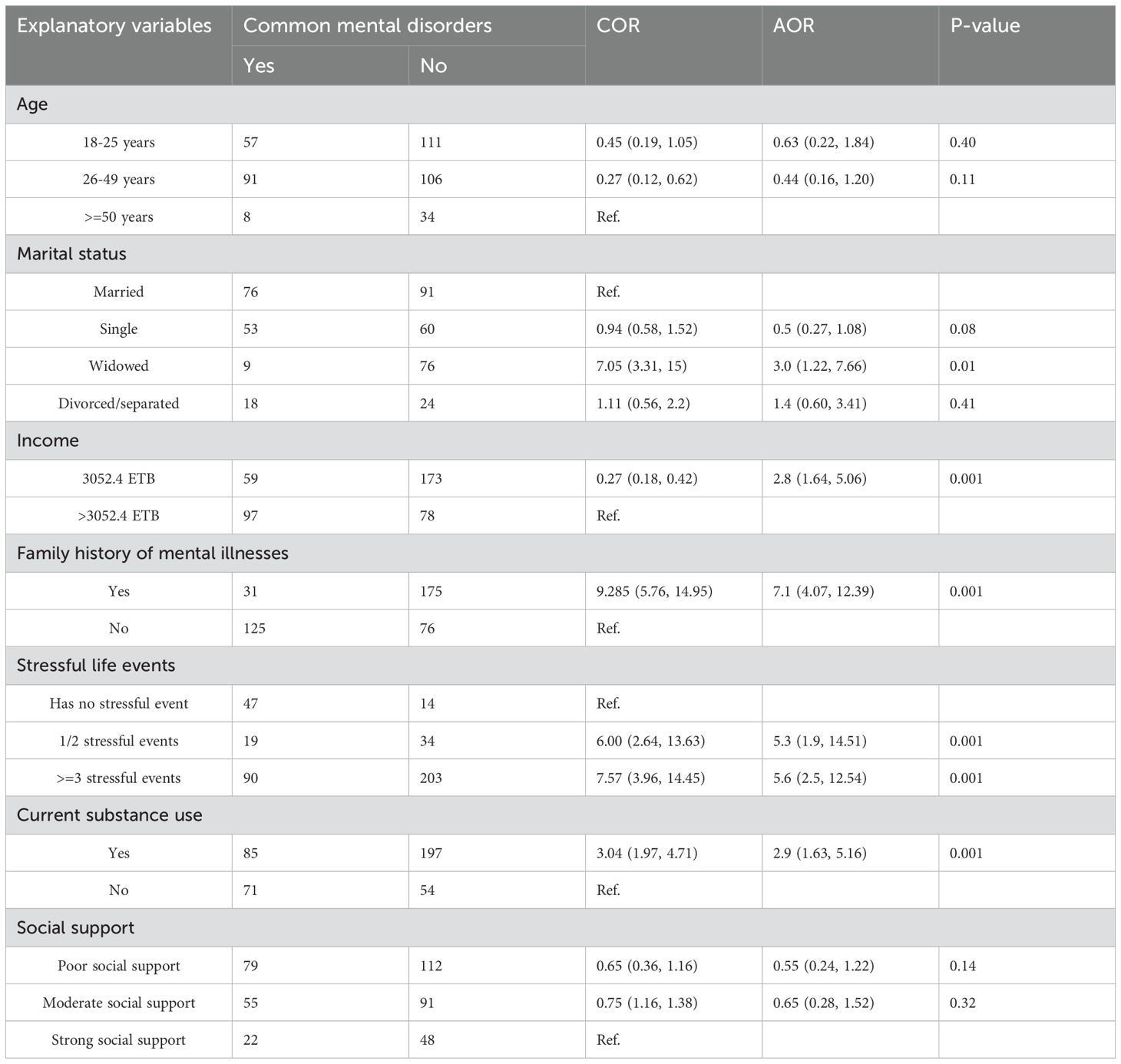
Table 3. Bivariable and Multivariable binary logistic regression analysis of common mental disorders among SGBV survivors of Amhara Region (n=407).
In contrast, in the multivariable analysis, being single, being widowed, having a mental illness in the family and having chronic physical issues, history of abortion, having physical illnesses related with the violence, those who had CMDs and previous history of suicide were significantly associated with suicidal behaviors. Participants with CMDs had a 4.6 fold (AOR=4.6, 95% CI= [2.0 to10.74]) increased likelihood of suicide behavior than those without CMDs. Survivors with a past suicide history were 3.4 times (AOR= 3.41, 95% CI= [1.22 to 9.55]) more likely to engage in suicidal behavior than their counterparts. When compared with individuals who did not have abortion, the odds of having suicidal behavior were 4.1 times (AOR= 4.1, 95% CI= [1.9 to 8.5]). Age, residence, educational position, income, stressful life events, and relatives with a history of suicide were not significantly associated with suicidal behavior (See Table 4). Surprisingly, the variables associated with the types of SGBV did not demonstrate a significant association with CMDs and suicidal behavior in the bivariable logistic regression analysis (See Table 2).
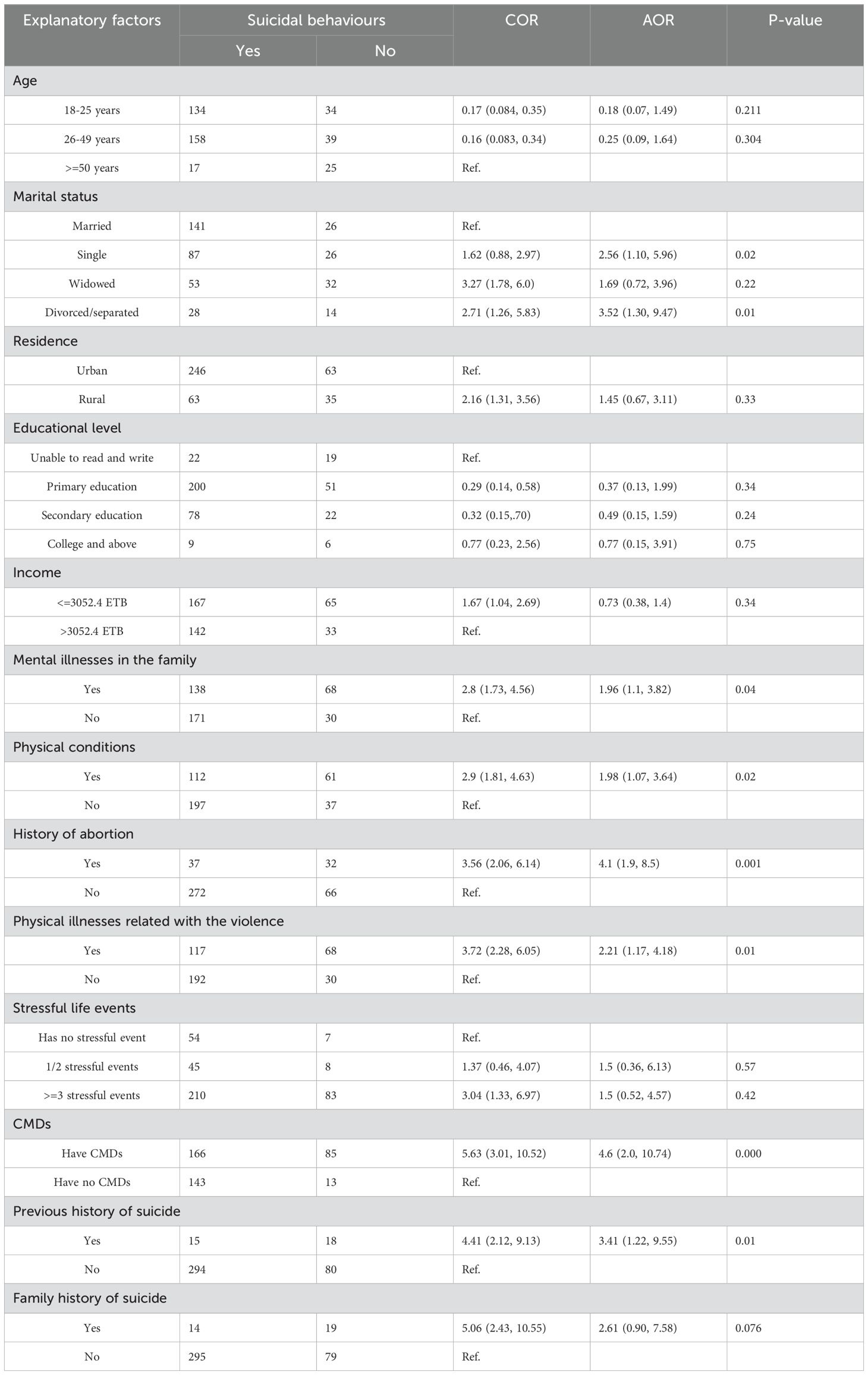
Table 4. Bivariable and Multivariable binary logistic regression analysis of suicidal behaviours among SGBV survivors of Amhara Region (n=407).
CMDs in GBV survivors in selected One Stop Centers in Amhara Region were 61.7%. The findings are consistent with an earlier Ethiopian study, which found a prevalence rate of 59.6% (44); however, it is higher than the study done in Australia (37%) (29), and lower than the study from Jamaica (77.3%) (25). The possible discrepancy could be attributable to differences in study design and the tool employed to assess the outcome variable. In this study, the SRQ-20 was employed to assess common mental disorders, whereas, in Australia and Jamaica, the Composite International Diagnostic Interview Version 3.0 was employed. The study in Australia employed a retrospective methodology, but the study in Jamaica used a high sample size. Another possible explanation for the disparity in the frequency of common mental disorders among survivors of gender-based violence is that the study was done in a post-war context.
Suicidal behavior was reported by nearly a quarter of the participants (24.1%). This is consistent with the findings of an Australian study, which showed a prevalence of (19.5%) (29). The current study’s prevalence rate, however, is higher than that reported in research conducted in five low and middle-income countries, which is (10.3%) (45), and Ethiopia (9.3%) (40). The possible reason for this variation is that previous research may have been conducted on a community sample and primary care attendees from the general population. Previous research employed the suicidality module of the Composite International Diagnostic Interview to assess suicidal behavior. On the other hand, the current study was conducted in a sample from war-affected areas to measure suicidal behavior using the Suicide Behaviors Questionnaire-Revised.
This study found a significant association between several independent variables and suicidal behavior. Of these factors, CMDs is one of the crucial factors contributing to suicidal behavior. CMDs were 4.6 times more common in people with Suicidal behavior than those without. Several studies conducted in low- and middle-income nations support this fact (45), Brazil (46), South Africa (47), and Ethiopia (48). All these studies confirmed that suicidal behavior is significantly associated with a common mental disorder. Experiencing physical and psychological trauma affects the survivor’s mental health, leading to suicide (49, 50). This might be due to the serotonergic deficiency and hypo activity associated with psychiatric disorders such as depression which increased the risk of suicide (51, 52). Another probable explanation is that depression directly influences survivors, making them feel frustrated, alone, and worthless, leading to suicidal conduct (53, 54).
The current study found that being single and widowed/separated were significantly related to suicidal behaviors. The odds of developing suicidal behavior were (AOR= 2.56) and (AOR= (3.52) times higher in those who are single and widowed/separated, respectively, than in their counterparts. This is congruent with the findings of studies from world mental health surveys conducted in seventeen countries, which found that being unmarried is one of the factors significantly correlated with suicide behavior (46).
Participants who had abortions had fourfold greater odds of having suicidal behavior than those who had not undergone abortions. This is consistent with a study conducted in the United States (55). This could be because sexual violence increases the likelihood of unwanted pregnancy and the decision to undergo an abortion. Abortion, in turn, may induce a mood disorder in a vulnerable individual. A woman with a mood problem is less likely to carry out a pregnancy, preferring abortion (55). Those with a suicide history were (AOR=3.41) times more likely to be involved in suicidal behaviors than those without a suicidal history. The finding has been supported by research conducted in Tigray, Ethiopia (48) and Washington (56), which reported that previous suicidal behavior is associated with current or recent suicidal behavior.
Those with relatives with a history of mental illness were nearly twice as likely to develop suicidal behaviors as those without a comparative history of mental illness. This is also consistent with research conducted in Tigray, Ethiopia (48). The possible reason may be that the presence of a family history of mental health problems might disturb their social life due to the effect of stigma and discrimination, which ultimately leads to poor social support and further worsen the risk of having suicidal behavior (57, 58).
The odds of developing suicidal behavior were nearly twice as likely (AOR=1.98) among those with chronic illnesses and were (AOR=2.21) times more likely among those with violence-related physical health problems than their counterparts. These findings were consistent with studies conducted in Greece (59), Kenya (60), Canada (61), and a review of literature of studies conducted in Africa (62). The possible explanation for this might be that chronic illnesses are often related to functional limitations, dissatisfaction with their life, and reduced quality of life, which in turn. Due to the restriction to daily living activities, functional limitations cause discouragement, depression, and suicidality (63, 64). In addition, a history of violence could be a risk factor for suicidal behavior because repeated exposure to painful stimuli increases the risk for suicidality (65).
The study found that having relatives with a history of mental illness increases the likelihood of having common mental disorders by 7.1 times compared to not having a comparative history of mental illness. This is consistent with the findings of research done by Illu Ababora (66). A possible explanation can be that the mental disorders often exhibit a genetic component, with studies indicating that individuals with a family history of mental illness are more likely to inherit vulnerabilities to these conditions (67). Additionally, experiencing sexual abuse serves as a significant stressor that can lead to profound and long-term psychological distress (68).
A monthly income of less than or equal to 3052.4 ETB is significantly associated with common mental diseases. Those with a monthly income of less than 3052.4 ETB are 2.8 times more likely to suffer from a common mental disorder higher than those with a monthly income greater than 3052.4 ETB. The likely reason for this association is that many of the participants (35.1%) were homemakers and were unemployed (32.7%) and were expected to take care of many household responsibilities may predispose them to be financial, emotional, and physical strain and make them prone to psychological problems (69).
Compared to individuals who do not use substances, the risk of a common mental disorder is approximately three times higher. Current substance usage was associated with an increased chance of developing a common mental disorder. Butajira’s findings are consistent with earlier research (70) and Jimma, Ethiopia (71). The possible reason for this is that individuals with mental distress are likely to use substances to improve their symptoms (71).
The odds of having a common mental disorder among widowed participants have three times the odds of developing a common mental disorder when compared to their counterparts. The result is in line with a study done in Ethiopia (70). The possible explanation for this is that widowed individuals are likely to lose their primary source of emotional and social support, and this will, in turn, lead them to helplessness, hopelessness, isolation, and depression (72, 73).
The odds of developing common mental disorders are (AOR=5.3) times greater in individuals with one or two stressful life experiences and (AOR=5.6) times higher in those with three or more stressful life events. The result is supported by earlier research done in (74), Iran (75), and Brazil (76). This finding can be explained by the fact that stressors may alter the body’s reaction by firing the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis. Stress causes a rise in oxidative stress, contributing to the deterioration of cells (77, 78). Furthermore, stressful life experiences may play a unique role in the start and worsening of psychiatric issues (79, 80).
The current study showed an increased prevalence of common mental disorders and suicidal behavior among survivors of gender-based violence. Common mental disorders are substantially associated with being widowed, having relatives with a history of mental illness, having a low income, having life stresses, and using substances in the past three months. Being single and widowed, having relatives with a history of mental illness, developing a chronic medical condition, developing a history of abortion, having a physical illness related to violence, CMDs, and having a previous history of suicide were the factors significantly associated with suicidal behavior. The high prevalence rates necessitate comprehensive interventions such as screening and treatment of common mental disorders and suicide among survivors of gender-based violence.
This study has strengths and limitations. Standard instruments were used to measure the outcome variables. Health professionals who are experienced were collected the data. The research will also serve as a baseline for further studies. However, the study has limitations. Its cross-sectional design restricts the ability to establish causality between risk factors and mental health outcomes. In addition, selecting participants solely from help centers may introduce selection bias, as women seeking assistance may differ in characteristics and levels of CMDs and suicidality from those who do not. This limits the generalizability of the results to the broader affected population and makes it challenging to apply findings to similar contexts in Ethiopia or elsewhere. To enhance the representativeness of the sample, future studies should include women from various contexts, both urban and rural, as well as those not seeking help at centers. Furthermore, it is important to explore cultural and stigma-related factors that could influence women’s access to mental health support and alter the relationship between risk factors and CMDs or suicidality.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Institutional Review Board of Addis Ababa University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
TM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. SD: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to thank everyone involved in this study, including the participants, data collectors, and One Stop Center coordinators for their valuable contributions.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, Adjusted Odds Ratio; CMDs, Common Mental disorders; DSM, Diagnostic and Statistical Manual of Mental Disorders; GBD, Global Burden of Diseases; GBV, Gender Based Violence; OSCs, One-Stop Centers; OSSS, Oslo Social Support Scale; OR, Odds Ratio; SBQ – R, Suicidal Behavior Questionnaire Revised; SGBV, Sexual and Gender-Based Violence; SRQ, Self Reporting Questionnaire; SPSS, Statistical Packages for the Social Sciences.
1. Alsaba K, Kapilashrami A. Understanding women’s experience of violence and the political economy of gender in conflict: the case of Syria. Reprod Health Matters. (2016) 24:5–17. doi: 10.1016/j.rhm.2016.05.002
2. Goessmann K, Ibrahim H, Neuner F. Association of war-related and gender-based violence with mental health states of Yazidi women. JAMA Netw Open. (2020) 3:e2013418–e. doi: 10.1001/jamanetworkopen.2020.13418
3. Durbach A, Chappell L. Leaving behind the age of impunity: Victims of gender violence and the promise of reparations. Int Feminist J Politics. (2014) 16:543–62. doi: 10.1080/14616742.2014.941251
4. Goldberg P, Kelly N. International human rights and violence against women. Getzville, New York: HeinOnline (1993).
5. Sanjel S. Gender-based violence: a crucial challenge for public health. Kathmandu Univ Med J. (2013) 11:179–84. doi: 10.3126/kumj.v11i2.12499
6. Josse E. [amp]]lsquo;They came with two guns’: the consequences of sexual violence for the mental health of women in armed conflicts. Int Rev Red Cross. (2010) 92:177–95. doi: 10.1017/S1816383110000251
7. Usta J, Farver JAM, Zein L. Women, war, and violence: surviving the experience. J Women’s Health. (2008) 17:793–804. doi: 10.1089/jwh.2007.0602
8. Jewkes R, Jama-Shai N, Sikweyiya Y. Enduring impact of conflict on mental health and gender-based violence perpetration in Bougainville, Papua New Guinea: a cross-sectional study. PloS One. (2017) 12:e0186062. doi: 10.1371/journal.pone.0186062
9. McAlpine A, Hossain M, Zimmerman C. Sex trafficking and sexual exploitation in settings affected by armed conflicts in Africa, Asia and the Middle East: systematic review. BMC Int Health Hum Rights. (2016) 16:1–16. doi: 10.1186/s12914-016-0107-x
10. Vu A, Adam A, Wirtz A, Pham K, Rubenstein L, Glass N, et al. The prevalence of sexual violence among female refugees in complex humanitarian emergencies: a systematic review and meta-analysis. PloS Currents. (2014) 6. doi: 10.1371/currents.dis.835f10778fd80ae031aac12d3b533ca7
11. Amowitz LL, Reis C, Lyons KH, Vann B, Mansaray B, Akinsulure-Smith AM, et al. Prevalence of war-related sexual violence and other human rights abuses among internally displaced persons in Sierra Leone. Jama. (2002) 287:513–21. doi: 10.1001/jama.287.4.513
12. Bartels SA, Scott JA, Mukwege D, Lipton RI, VanRooyen MJ, Leaning J. Patterns of sexual violence in Eastern Democratic Republic of Congo: reports from survivors presenting to Panzi Hospital in 2006. Conflict Health. (2010) 4:1–10. doi: 10.1186/1752-1505-4-9
13. Kinyanda E, Musisi S, Biryabarema C, Ezati I, Oboke H, Ojiambo-Ochieng R, et al. War related sexual violence and it’s medical and psychological consequences as seen in Kitgum, Northern Uganda: A cross-sectional study. BMC Int Health Hum Rights. (2010) 10:1–8. doi: 10.1186/1472-698X-10-28
14. Ellsberg M, Ovince J, Murphy M, Blackwell A, Reddy D, Stennes J, et al. No safe place: Prevalence and correlates of violence against conflict-affected women and girls in South Sudan. PloS One. (2020) 15:e0237965. doi: 10.1371/journal.pone.0237965
15. Bitar S. Sexual violence as a weapon of war: the case of ISIS in Syria and Iraq. Uppsala, Sweden: Uppsala University (2015).
16. Capasso A, Skipalska H, Guttmacher S, Tikhonovsky NG, Navario P, Castillo TP. Factors associated with experiencing sexual violence among female gender-based violence survivors in conflict-afflicted eastern Ukraine. BMC Public Health. (2021) 21:1–16. doi: 10.1186/s12889-021-10830-9
17. Kelly JT, Betancourt TS, Mukwege D, Lipton R, Vanrooyen MJ. Experiences of female survivors of sexual violence in eastern Democratic Republic of the Congo: a mixed-methods study. Conflict Health. (2011) 5:1–8. doi: 10.1186/1752-1505-5-25
18. Walsh K, Keyes KM, Koenen KC, Hasin D. Lifetime prevalence of gender-based violence in US women: Associations with mood/anxiety and substance use disorders. J Psychiatr Res. (2015) 62:7–13. doi: 10.1016/j.jpsychires.2015.01.002
19. Trevillion K, Oram S, Feder G, Howard LM. Experiences of domestic violence and mental disorders: a systematic review and meta-analysis. PloS One. (2012) 7:e51740. doi: 10.1371/journal.pone.0051740
20. Fisher J, Tran TD, Biggs B, Dang TH, Nguyen TT, Tran T. Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. Int Health. (2013) 5:29–37. doi: 10.1093/inthealth/ihs012
21. Rees S, Fisher J. Gender-based violence and women's mental health: How should the GP respond?. Med Today. (2016) 17(3):14–20.
22. Morina N, Akhtar A, Barth J, Schnyder U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: a systematic review. Front Psychiatry. (2018) 9:433. doi: 10.3389/fpsyt.2018.00433
23. Turrini G, Purgato M, Ballette F, Nosè M, Ostuzzi G, Barbui C. Common mental disorders in asylum seekers and refugees: umbrella review of prevalence and intervention studies. Int J Ment Health Syst. (2017) 11:1–14. doi: 10.1186/s13033-017-0156-0
24. Liebling-Kalifani H, Ojiambo-Ochieng R, Marshall A, Were-Oguttu J, Musisi S, Kinyanda E. Violence against women in Northern Uganda: The neglected health consequences of war. J Int Women’s Stud. (2008) 9(3):174–92. Available at: https://vc.bridgew.edu/jiws/vol9/iss3/10.
25. Rees S, Silove D, Chey T, Ivancic L, Steel Z, Creamer M, et al. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. Jama. (2011) 306:513–21. doi: 10.1001/jama.2011.1098
26. Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PloS Med. (2013) 10:e1001439. doi: 10.1371/journal.pmed.1001439
27. Beydoun HA, Beydoun MA, Kaufman JS, Lo B, Zonderman AB. Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Soc Sci Med. (2012) 75:959–75. doi: 10.1016/j.socscimed.2012.04.025
28. Campbell JC. Health consequences of intimate partner violence. Lancet. (2002) 359:1331–6. doi: 10.1016/S0140-6736(02)08336-8
29. Rees S, Steel Z, Creamer M, Teesson M, Bryant R, McFarlane AC, et al. Onset of common mental disorders and suicidal behavior following women’s first exposure to gender based violence: a retrospective, population-based study. BMC Psychiatry. (2014) 14:1–8. doi: 10.1186/s12888-014-0312-x
30. Asefa EY, Haile AB, Mohamed OY, Berhanu D. The magnitude of gender-based violence, health consequences, and associated factors among women living in post-war woredas of North Shewa zone, Amhara, Ethiopia, 2022. Front Global women’s Health. (2024) 5:1335254. doi: 10.3389/fgwh.2024.1335254
31. Fisseha G, Gebrehiwot TG, Gebremichael MW, Wahdey S, Meles GG, Gezae KE, et al. War-related sexual and gender-based violence in Tigray, Northern Ethiopia: a community-based study. BMJ Global Health. (2023) 8:e010270. doi: 10.1136/bmjgh-2022-010270
32. Tewabe DS, Azage M, Wubetu GY, Fenta SA, Worke MD, Asres AM, et al. Gender-based violence in the context of armed conflict in Northern Ethiopia. Conflict Health. (2024) 18:1. doi: 10.1186/s13031-023-00563-4
33. Kassa GM, Abajobir AA. Prevalence of violence against women in Ethiopia: a meta-analysis. Trauma Violence Abuse. (2020) 21:624–37. doi: 10.1177/1524838018782205
34. Stachow E. Conflict-related sexual violence: a review. BMJ Military Health. (2020) 166:183–7. doi: 10.1136/jramc-2019-001376
35. Alamineh GA, Hussein JW, Mulu YE, Taddesse B. The negative cultural impact of tourism and its implication on sustainable development in Amhara Regional State. Cogent Arts Humanities. (2023) 10:2224597. doi: 10.1080/23311983.2023.2224597
36. Undie C-C, Ngebeh J, Namwebya JH, Karugaba J. Practice-based learning: Observations on One-Stop Centers in refugee settings. Sauti/VOICE Program Brief no. 5. Nairobi: UNHCR EHAGL Africa Bureau and Population Council (2019).
37. Tilahun T, Oljira R, Getahun A. Sexual assault cases managed at a referral hospital in Western Ethiopia: A retrospective cross-sectional study. SAGE Open Med. (2022) 10:20503121221126328. doi: 10.1177/20503121221126328
38. Netsereab TB, Kifle MM, Tesfagiorgis RB, Habteab SG, Weldeabzgi YK, Tesfamariam OZ. Validation of the WHO self-reporting questionnaire-20 (SRQ-20) item in primary health care settings in Eritrea. Int J Ment Health Syst. (2018) 12:1–9. doi: 10.1186/s13033-018-0242-y
39. Melkam M, Nenko G, Demilew D. Common mental disorders and associated factors among high school students in Debre Markos Town, Northwest Ethiopia: an institutional-based cross-sectional study. BMJ Open. (2022) 12:e059894. doi: 10.1136/bmjopen-2021-059894
40. Molla A, Nigussie J, Girma B. Prevalence and associated factors of suicidal behavior among pregnant mothers in southern Ethiopia: a cross-sectional study. BMC Public Health. (2022) 22:490. doi: 10.1186/s12889-022-12957-9
41. Onifade P, Bello A, Abiodun O, Sotunsa J, Ladipo O. Psychometric properties of alcohol smoking and substance involvement screening test (Assist V3. 0) among university students. J Addict Behav Ther Rehab. (2014) 3:2–7. doi: 10.4172/2324-9005.1000126
42. Brugha T, Bebbington P, Tennant C, Hurry J. The List of Threatening Experiences: a subset of 12 life event categories with considerable long-term contextual threat. psychol Med. (1985) 15:189–94. doi: 10.1017/S003329170002105X
43. Dalgard OS, Dowrick C, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, et al. Negative life events, social support and gender difference in depression: a multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:444–51. doi: 10.1007/s00127-006-0051-5
44. Sewalem J, Molla A. Mental distress and associated factors among women who experienced gender based violence and attending court in South Ethiopia: a cross-sectional study. BMC women’s Health. (2022) 22:187. doi: 10.1186/s12905-022-01770-6
45. Jordans M, Rathod S, Fekadu A, Medhin G, Kigozi F, Kohrt B, et al. Suicidal ideation and behaviour among community and health care seeking populations in five low-and middle-income countries: a cross-sectional study. Epidemiol Psychiatr Sci. (2018) 27:393–402. doi: 10.1017/S2045796017000038
46. Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. (2008) 192:98–105. doi: 10.1192/bjp.bp.107.040113
47. Naidoo S, Collings SJ. Suicidal and death ideation in a cohort of psychiatric outpatients: Prevalence and risk factors. Psychol Develop Soc. (2017) 29:288–300. doi: 10.1177/0971333617716849
48. Tsegay A, Damte A, Kiros A. Determinants of suicidal ideation among patients with mental disorders visiting psychiatry outpatient unit in Mekelle town, psychiatric clinics, Tigray, Northern Ethiopia: a case–control study. Ann Gen Psychiatry. (2020) 19:1–12. doi: 10.1186/s12991-020-00270-x
49. García-Moreno C, Pallitto C, Devries K, Stöckl H, Watts C, Abrahams N. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: World Health Organization (2013). doi: 10.1161/CIRCRESAHA.116.307547
50. Carlson CE, Witte SS, Pala AN, Tsai LC, Wainberg M, Aira T. The impact of violence, perceived stigma, and other work-related stressors on depressive symptoms among women engaged in sex work. Global Soc Welfare. (2017) 4:51–7. doi: 10.1007/s40609-017-0085-5
51. Kovacic Z, Henigsberg N, Pivac N, Nedic G, Borovecki A. Platelet serotonin concentration and suicidal behavior in combat related posttraumatic stress disorder. Prog Neuropsychopharmacol Biol Psychiatry. (2008) 32:544–51. doi: 10.1016/j.pnpbp.2007.10.014
52. Courtet P, Baud P, Abbar M, Boulenger J-P, Castelnau D, Mouthon D, et al. Association between violent suicidal behavior and the low activity allele of the serotonin transporter gene. Mol Psychiatry. (2001) 6:338–41. doi: 10.1038/sj.mp.4000856
53. Deyessa N, Berhane Y, Alem A, Ellsberg M, Emmelin M, Hogberg U, et al. Intimate partner violence and depression among women in rural Ethiopia: a cross-sectional study. Clin Pract Epidemiol Ment Health. (2009) 5:1–10. doi: 10.1186/1745-0179-5-8
54. Pompili M, Gibiino S, Innamorati M, Serafini G, Del Casale A, De Risio L, et al. Prolactin and thyroid hormone levels are associated with suicide attempts in psychiatric patients. Psychiatry Res. (2012) 200:389–94. doi: 10.1016/j.psychres.2012.05.010
55. Mota NP, Burnett M, Sareen J. Associations between abortion, mental disorders, and suicidal behaviour in a nationally representative sample. Can J Psychiatry. (2010) 55:239–47. doi: 10.1177/070674371005500407
56. Hallgren KA, Ries RK, Atkins DC, Bumgardner K, Roy-Byrne P. Prediction of suicide ideation and attempt among substance-using patients in primary care. J Am Board Family Med. (2017) 30:150–60. doi: 10.3122/jabfm.2017.02.160264
57. Dachew BA, Azale Bisetegn T, Berhe Gebremariam R. Prevalence of mental distress and associated factors among undergraduate students of University of Gondar, Northwest Ethiopia: a cross-sectional institutional based study. PloS One. (2015) 10:e0119464. doi: 10.1371/journal.pone.0119464
58. Yimam K, Kebede Y, Azale T. Prevalence of common mental disorders and associated factors among adults in Kombolcha Town, Northeast Ethiopia. J Depression Anxiety. (2014) 1:007. doi: 10.4172/2167-1044.S1-007
59. Skapinakis P, Bellos S, Koupidis S, Grammatikopoulos I, Theodorakis PN, Mavreas V. Prevalence and sociodemographic associations of common mental disorders in a nationally representative sample of the general population of Greece. BMC Psychiatry. (2013) 13:1–14. doi: 10.1186/1471-244X-13-163
60. Jenkins R, Njenga F, Okonji M, Kigamwa P, Baraza M, Ayuyo J, et al. Prevalence of common mental disorders in a rural district of Kenya, and socio-demographic risk factors. Int J Environ Res Public Health. (2012) 9:1810–9. doi: 10.3390/ijerph9051810
61. Lapierre S, Desjardins S, Préville M, Berbiche D, Lyson Marcoux M. Wish to die and physical illness in older adults. Psychology. (2015) 5(2):125–37. doi: 10.17265/2159-5542/2015.02.005
62. Mars B, Burrows S, Hjelmeland H, Gunnell D. Suicidal behaviour across the African continent: a review of the literature. BMC Public Health. (2014) 14:1–14. doi: 10.1186/1471-2458-14-606
63. Habtamu Y, Admasu K, Tullu M, Kebede A. Magnitude of common mental disorders and factors associated among people living in Addis Ababa Ethiopia 2018: community based cross-sectional study. BMC Psychiatry. (2022) 22:1–10. doi: 10.1186/s12888-022-03783-9
64. Mellqvist Fässberg M, Östling S, Braam AW, Bäckman K, Copeland JR, Fichter M, et al. Functional disability and death wishes in older Europeans: results from the EURODEP concerted action. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1475–82. doi: 10.1007/s00127-014-0840-1
66. Engidaw NA, Abdu Z, Chinani I. Prevalence and associated factors of common mental disorders among residents of Illu Ababore zone, southwest Ethiopia: a cross-sectional study. Int J Ment Health Syst. (2020) 14:1–8. doi: 10.1186/s13033-020-00394-3
67. Hamad AF, Monchka BA, Bolton JM, Plana-Ripoll O, Roos LL, Elgendi M, et al. The Intergenerational Transfer of Mental Disorders: A Population-Based Multigenerational Linkage Study: Le transfert intergénérationnel des troubles mentaux: une étude sur les liens multigénérationnels basée sur la population. Can J Psychiatry. (2024) 07067437241255096. doi: 10.1177/07067437241255096
68. Banyard VL, Williams LM, Siegel JA. The long-term mental health consequences of child sexual abuse: An exploratory study of the impact of multiple traumas in a sample of women. J Traumatic Stress. (2001) 14:697–715. doi: 10.1023/A:1013085904337
69. Kerebih H, Soboka M. Prevalence of common mental disorders and associated factors among residents of Jimma town, South West Ethiopia. J Psychiatry. (2016) 19:373. doi: 10.4172/2378-5756.1000373
70. Alem A, Kebede D, Woldesemiat G, Jacobsson L, Kullgren G. The prevalence and socio-demographic correlates of mental distress in Butajira, Ethiopia. Acta Psychiatrica Scand. (1999) 100:48–55. doi: 10.1111/j.1600-0447.1999.tb10694.x
71. Damena T, Mossie A, Tesfaye M. Khat chewing and mental distress: a community based study, in jimma city, southwestern Ethiopia. Ethiopian J Health Sci. (2011) 21:37–46. doi: 10.4314/ejhs.v21i1.69042
72. Manii D, Ammerman D. Men and cancer: a study of the needs of male cancer patients in treatment. J Psychosocial Oncol. (2008) 26:87–102. doi: 10.1300/J077v26n02_06
73. Feder KA, Heatherington L, Mojtabai R, Eaton WW. Perceived marital support and incident mental illness: evidence from the National Comorbidity Survey. J Marital Family Ther. (2019) 45:668–83. doi: 10.1111/jmft.12343
74. Jenkins R, Mbatia J, Singleton N, White B. Common mental disorders and risk factors in urban Tanzania. Int J Environ Res Public Health. (2010) 7:2543–58. doi: 10.3390/ijerph7062543
75. Hassanzadeh A, Heidari Z, Feizi A, Hassanzadeh Keshteli A, Roohafza H, Afshar H, et al. Association of stressful life events with psychological problems: a large-scale community-based study using grouped outcomes latent factor regression with latent predictors. Comput Math Methods Med. (2017) 2017. doi: 10.1155/2017/3457103
76. Lima MS, Beria JU, Tomasi E, Conceicao AT, Mari JJ. Stressful life events and minor psychiatric disorders: an estimate of the population attributable fraction in a Brazilian community-based study. Int J Psychiatry Med. (1996) 26:211–22. doi: 10.2190/W4U4-TCTX-164J-KMAB
77. Gidron Y, Russ K, Tissarchondou H, Warner J. The relation between psychological factors and DNA-damage: a critical review. Biol Psychol. (2006) 72:291–304. doi: 10.1016/j.biopsycho.2005.11.011
78. Feizi A, Aliyari R, Roohafza H. Association of perceived stress with stressful life events, lifestyle and sociodemographic factors: a large-scale community-based study using logistic quantile regression. Comput Math Methods Med. (2012) 2012. doi: 10.1155/2012/151865
79. Low NC, Dugas E, O’Loughlin E, Rodriguez D, Contreras G, Chaiton M, et al. Common stressful life events and difficulties are associated with mental health symptoms and substance use in young adolescents. BMC Psychiatry. (2012) 12:1–10. doi: 10.1186/1471-244X-12-116
80. Osler M, Bendix L, Rask L, Rod NH. Stressful life events and leucocyte telomere length: Do lifestyle factors, somatic and mental health, or low grade inflammation mediate this relationship? Results from a cohort of Danish men born in 1953. Brain Behav Immunity. (2016) 58:248–53. doi: 10.1016/j.bbi.2016.07.154
Keywords: common mental disorders, suicidality, sexual and gender based violence, Amhara, Ethiopa
Citation: Michael T and Demeke SM (2025) Symptoms of common mental disorders and suicidality among female survivors of war related sexual and gender based violence in one stop centers of the Amhara region, Ethiopia: a multicenter cross-sectional study. Front. Psychiatry 16:1456909. doi: 10.3389/fpsyt.2025.1456909
Received: 29 June 2024; Accepted: 27 January 2025;
Published: 14 February 2025.
Edited by:
Thomas G. Schulze, University Medical Center Göttingen, GermanyReviewed by:
Sandra Patricia Trujillo, University of Antioquia, ColombiaCopyright © 2025 Michael and Demeke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Solomon Moges Demeke, c29sbW9ubW9nZUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.