- 1Department of Psychology, University of Innsbruck, Innsbruck, Austria
- 2Department of Psychology, University of Graz, Graz, Austria
- 3Department of Child and Adolescent Psychiatry, Psychotherapy and Psychosomatics, Medical University of Innsbruck, Innsbruck, Austria
- 4VAMED Clinic for Rehabilitation Montafon, Schruns, Austria
Background: Initial studies suggest that individuals with a history of traumatic life experiences, particularly childhood trauma, may be more susceptible to increased mental health problems in the wake of the COVID-19 pandemic.
Methods: The present cross-sectional study compared the mental health status of three cohorts of university students before (2016), at the beginning (2020) and at the end (2022) of the COVID-19 pandemic. The students in each cohort were divided into two groups: those with self-reported moderate/severe childhood trauma (n = 126) and those with no/mild childhood trauma (n = 438).
Results: Across all cohorts, students with moderate/severe childhood trauma consistently reported higher levels of psychological and physical stress compared to individuals with no/mild childhood trauma experiences. However, only the no/mild childhood trauma group exhibited an increase in mental health problems (i.e., heightened depressive symptoms and greater subjective impairment due to physical and psychological symptoms) during the COVID-19 pandemic. Furthermore, within the no/mild childhood trauma group, students in the 2022 cohort reported significantly higher psychological distress compared to those surveyed in 2020. In contrast, mental health scores among students with moderate/severe childhood trauma remained unchanged across the pre-pandemic and pandemic cohorts.
Conclusions: The findings of this study do not support the hypothesis that the COVID-19 pandemic disproportionately exacerbated mental health problems in individuals with a history of moderate to severe childhood trauma. Instead, our results suggest that the pandemic’s impact on mental health was more pronounced in students with no or only mild childhood trauma.
1 Introduction
The COVID-19 pandemic has been a major challenge worldwide, with numerous studies documenting an increase in mental illness (e.g., depression, anxiety disorders and other stress-related illnesses) following the outbreak of the pandemic [see, for a systematic review (1) or (2)]. Students in particular represent a vulnerable group who are exposed to a variety of stressors such as social, financial and emotional challenges, in addition to academic demands (3, 4). Even before the COVID-19 pandemic, students reported high levels of stress (5). Persistent stress can lead to poorer academic performance, higher dropout rates (6), and is one of the most important risk factors for mental (and physical) health (3).
The wide range of stress factors makes students particularly susceptible to mental illness. For instance, an international survey of universities found that more than a third of their students already met the DSM diagnostic criteria for depression or anxiety disorders (3), highlighting the vulnerability of this population. The shift to digital distance learning during the COVID-19 pandemic, exacerbated these challenges, leading to a further significant increase in anxiety symptoms, depression and post-traumatic stress disorder (PTSD) among students (7, 8). According to a study by Karasmanaki and Tsantopoulos (9), the shutdown of universities and the associated changes in university life constituted a massive disruption for students and had a significant impact on their well-being.
In the public media and numerous articles, the COVID-19 pandemic is sometimes referred to as a traumatic experience or collective trauma [see, for example (10)]. However, there is currently no single valid definition of “trauma”. The eleventh revision of the International Classification of Diseases, ICD-11 (11), defines a traumatic event as an “extremely threatening or distressing event”, which can be a single event or a series of events. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) operationalizes traumatic events as direct or indirect confrontation with death, whether actual or threatened, as well as with serious injury or sexual violence (12). Although the COVID-19 pandemic cannot be classified as a traumatic event according to these criteria, many researchers argue that it fulfills the requirements for trauma classification and consider it a traumatic event [e.g. (13)]. A study on COVID-19 and trauma-related symptoms in Austrians in spring 2021 revealed a prevalence of trauma-related symptoms of 18.1%, which, according to the authors (14), is higher than expected based on international data. The study found that symptoms of re-experiencing and, to a lesser extent, avoidance were more common in COVID-19 cases, while dissociative symptoms, hyperarousal, and negative mood were less prevalent. Younger people in particular showed more pronounced trauma-related symptoms, which the authors attribute to less life experience and fewer stress management skills (14).
A French study (15) comparing anxiety and depression symptoms in students and non-students at three points during the pandemic found that students reported more depressive symptoms during the initial nationwide lockdown, comparable levels during the relaxation phase, and a subsequent increase during the second lockdown. In addition, anxiety symptoms were generally more prevalent in students during the pandemic than in people who were not studying. These findings suggest that the governmental restrictions disproportionately affected students compared to their peers who were not in academic education (15). A meta-analysis by Jia et al. (16) further confirmed that students are more susceptible to depression and anxiety than the general population and healthcare professionals. Many studies also identify female gender as another important risk factor for pandemic-related psychological reactions including anxiety disorders, depression, and post-traumatic stress symptoms and PTSD [e.g., (17)], although the meta-analysis by Peng et al. (18) points to a certain heterogeneity in these findings.
Regardless of the discussion about whether or not the COVID-19 pandemic is formally classified as a traumatic event, preliminary research suggests that individuals with previous traumatic life events, particularly childhood trauma, may be more vulnerable to increased anxiety, depression and post-traumatic stress symptoms in the wake of the COVID-19 pandemic (19–21). It is known that individual exposure to environmental stressors during early life impairs adaptive coping strategies and thus increases vulnerability to future stressors (22). Many studies therefore emphasize the importance of considering people’s past traumas when assessing mental health during the COVID-19 pandemic (20).
A significant proportion of the population has a history of trauma (23), and students in particular frequently report childhood trauma (24, 25). A distinction is made between different types of childhood trauma, including physical and emotional abuse, sexual abuse or neglect (26). Childhood trauma is considered a risk factor that can lead to a variety of mental disorders (27), and both to decreased mental as well as physical health (28). Research shows that individuals with traumatic childhood experiences are more susceptible to increased mental health problems in later stressful situations (29).
Studies investigating the impact of childhood trauma on mental health during the COVID-19 pandemic have shown that childhood trauma and adverse childhood experiences negatively affected mental health (30, 31). According to Stanislawski et al. (32), the experience of emotional abuse in childhood was associated with higher levels of depression and PTSD in students during the pandemic. Similarly, Xie et al. (33) found a positive association between childhood trauma, pandemic-related psychological distress, and depression, anxiety and stress. Conversely, secure attachment in childhood may serve as a protective factor against the development of psychological symptoms, according to Bussone, Pesca, Tambelli, and Carola (34).
Therefore, the present cross-sectional study has two primary aims: to compare the mental health status of university students before and during the two-year pandemic, and to investigate whether students with higher levels of childhood trauma were more vulnerable to COVID-19 stressors and reported more mental health problems during the COVID-19 pandemic.
2 Materials and methods
2.1 Study procedure and participants
The sample consists of three cohorts of German-speaking students from different faculties in Austria and Germany. The students were recruited via social networks, university courses and the mailing lists of the University of Innsbruck and Graz. The pre-COVID group was surveyed between September and December 2016 and a second and third survey of students was conducted during two distinct phases of the COVID-19 pandemic. The survey for the second cohort was started in May 2020, was stopped during the semester break and was completed in mid-November 2020. This period coincided with initial experiences of restrictive measures and university closures, necessitating a transition from face-to-face to distance learning. The third cohort was surveyed in June 2022. The third survey period was characterized by a substantial easing of restrictions. Nevertheless, many university courses continued to be held online for various reasons.
This study was approved by the ethics committees of the University of Graz and the University of Innsbruck. All participants provided informed consent prior to their study inclusion.
A total of n = 747 students participated in the online surveys. Only students between the ages of 18 and 26 were included in the analyses. Students who were already working full-time and were not registered as “actively studying” at the time of the survey were excluded from the study. Participants with incomplete questionnaires were also excluded. The final sample consisted of 564 students (pre-COVID group: n = 175; COVID-Year 2020 group: n = 200; COVID-Year 2022 group: n = 189). Using the Bernstein, Fink, Handelsman, and Foote (35) cut-off scores, students in each cohort were categorized into a group with moderate/severe childhood trauma (n = 126) and a group with no/mild childhood trauma (n = 438).
2.2 Measures
2.2.1 Beck’s depression inventory
The BDI-II (36) was administered to all participants to assess the severity of depressive symptoms. Participants self-reported a variety of current depressive symptoms, rating each on a 4-point Likert scale from 0 (absent or mild) to 3 (severe). The total BDI-II score is calculated by summing all 21 item scores and thus ranges from 0 to 63. Higher scores indicate more severe depressive symptoms. A review of the psychometric properties of the BDI-II (37) reported internal consistency around 0.9 and retest reliability ranging from 0.73 to 0.96. The review also found a high overlap (0.66 to 0.86) between the construct measured by BDI-II and that of other widely used depression scales, such as the Center for Epidemiologic Studies of Depression Scale (CES-D) and, the Hamilton Depression Rating Scale (HAM-D). For the German version of the BDI-II Kühner et al. (38) reported Cronbach’s alphas of at least 0.84 across different samples, along with significant and strong correlations with similar measures (ranging from 0.72 to 0.89 across different samples). In the current study Cronbach’s alpha was also calculated to assess reliability. The internal consistency of the BDI-II in this sample is high, with α = 0.89.
2.2.2 Modified impact of events scale – COVID-19
A modified version of the IES-R (39) was used to measure the traumatic impact of the COVID-19 pandemic. The IES-R, a 22 items scale, capture the subjective distress experienced in the past seven days as a result of a traumatic event. It contains three subscales: Avoidance (8 items), Hyperarousal (7 items), and Intrusion (7 items), which correspond to DSM-IV criteria B, C, and D for PTSD. Each item is scored on a 4-point scale ranging from ‘not at all’ (0), ‘rarely’ (1), ‘sometimes’ (3) to ‘often’ (5), with higher scores indicating a greater psychological impact of the traumatic situation. The original IES-R instructions were slightly adapted to specifically address the COVID-19 situation. Items referring to the past, were changed to the present tense, as the COVID-19 pandemic was still ongoing during data collection.
The internal consistency of the modified version of the IES-R, used in the current study to measure the traumatic impact of the COVID-19 pandemic was high, with Cronbach’s α = 0.90.
2.2.3 Childhood trauma questionnaire
The CTQ [35; German version by Klinitzke, Romppel, Häuser, Brähler, and Glaesmer (40)] is a self-report measure designed to retrospectively assess the occurrence and severity of child maltreatment and abuse (childhood trauma). The 28 items cover five subscales related to childhood trauma, namely sexual abuse, emotional abuse, physical abuse, emotional neglect, and physical neglect. Three additional questions assess whether participants minimize or deny their childhood trauma. Items are rated on a 5-point Likert scale from 1 (not at all) to 5 (very often) and summed to a global score. The following cut-off scores for the presence of moderate/severe childhood trauma, taken from Bernstein et al. (35), were used: ≥13 for emotional abuse, ≥10 for physical abuse, ≥8 for sexual abuse, ≥15 for emotional neglect, and ≥10 for physical neglect. The German version of the CTQ showed high internal consistency for all scales (Cronbach’s α: 0.80 – 0.89), except for physical neglect, Cronbach’s α: 0.55), in a sample of 2500 psychiatric patients (40). The established factor structure (i.e., sexual, physical, and emotional abuse, as well as physical and emotional neglect) was replicated by means of confirmatory factor analysis. Only low to moderate correlations between the CTQ and self-report measures for anxiety and depression on the Patient Health Questionnaire-4 (PHQ-4P) could be found. In the present study, the internal consistency of the CTQ global score was high, with a Cronbach’s α = 0.91.
2.2.4 Symptom checklist 90 revised
The SCL-90-R [ (41); German version (42); 90 items] is a self-report questionnaire assessing subjective impairment caused by physical and psychological symptoms within the past seven days. The frequency and intensity of the symptoms are rated on a 5-point Likert scale from 0 (“not at all”) to 4 (“very strongly”). The Global Severity Index (GSI) calculated as the mean of all items, serves as an overall measure of psychological distress. An evaluation of the psychometric properties of the German version of the SCL-90-R (43) showed high internal consistency for the Global Severity Index (Cronbach’s α = 0.97) and all original subscales (Cronbach’s α = between 0.80 -0.90). Significant correlations between the subscales of the SCL-90 and other scales, such as the General Health Questionnaire (GHQ-12), ranged from 0.45 to 0.72 and provide evidence of concurrent validity. However, the original nine-factor and subsequent two factor model could not be replicated. In the current study, Cronbach’s alpha for the GSI was high, with α = 0.97.
2.3 Statistical analysis
Descriptive data are presented as means (M) and standard deviations (SD). Pearson’s chi-square tests were used to compare the demographic characteristics (gender and childhood trauma) of the three cohorts (pre-COVID [first cohort], COVID-Year 2020 [second cohort], COVID-Year 2022 [third cohort]). A univariate analysis of variance (ANOVA) was used to examine the age differences between the three cohorts of students.
Furthermore, univariate two-factor analyses of covariance (ANCOVAs) were conducted for BDI-II, SCL-90-R, and CTQ scores, with cohort (pre-COVID, COVID-Year 2020, and COVID-Year 2022), and childhood trauma (no/mild childhood trauma vs. moderate/severe childhood trauma) as fixed factors, and age as a covariate. Similarly, an ANCOVA was used to analyze differences in the mIES-R scores between the two COVID-19 groups (COVID-Year 2020 and COVID-Year 2022), again with age as covariate. Consistent with the research questions of the present study, the relevant effects of interest in these analyses were the main effects of cohort (differences in the overall symptom level) and the two-way interaction between cohort and childhood trauma. Post-hoc pairwise comparisons with Bonferroni-corrections were conducted to explore significant interactions effects. Effect sizes in ANCOVAs are reported as partial eta-squared (ηp2). Moreover, for significant ANCOVA effects we additionally report adjusted means and 95% confidence intervals of the means (CIs). All analyses were performed using the SPSS software (version 26) with a significance level of α = .05 (two-tailed).
To determine the achieved power of the significant ANCOVA results, post-hoc power analyses were conducted using G*Power 3.1 (44). First, we converted the obtained partial eta-squared effect sizes to Cohen’s f effect sizes. For the power analyses, we specified an α-level of 0.05, a total sample size of 564, and the number of groups and covariates. The analyses demonstrated that the present study was adequately powered to detect small effects in the BDI-II, SCL-90-R GSI, and CTQ scores.
3 Results
3.1 Sample characteristics
The majority of the sample was female and reported no/mild childhood trauma. There were no significant differences in the distribution of gender (χ2(2, n = 564) =2.054, p = .358) or the number of students across the two childhood trauma groups (χ2(2, n = 564) = 4.090, p = .129) in the three cohorts. However, there was a significant difference in the age of students among the three cohorts (F(2,561) = 77.174, p <.001, ηp² = .215), with the oldest students belonging to the third cohort, followed by the second and the first cohort (all p’s <.001).
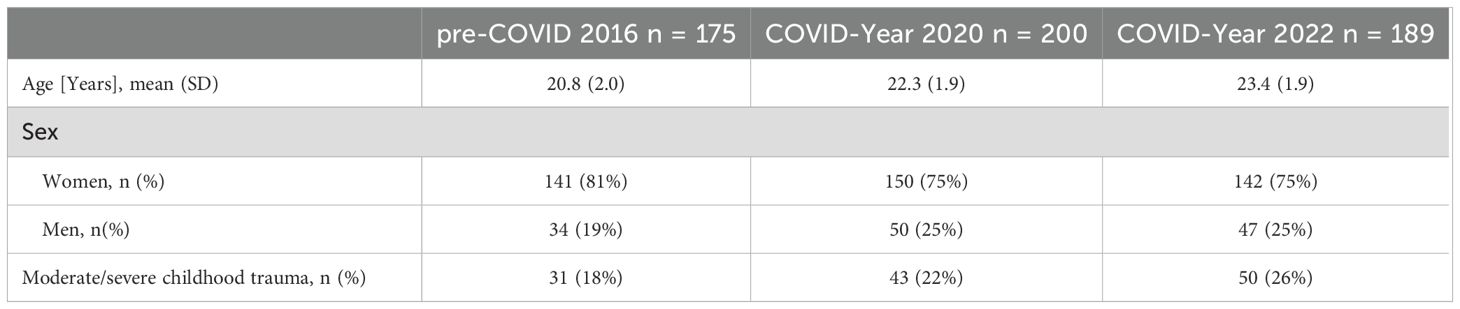
Demographic data are presented in Table 1.
Table 2 summarizes the descriptive statistics for the four clinical scales at the three measurement periods, separately for the two childhood trauma groups.
3.2 The impact of COVID-19 pandemic and childhood trauma on depression scores
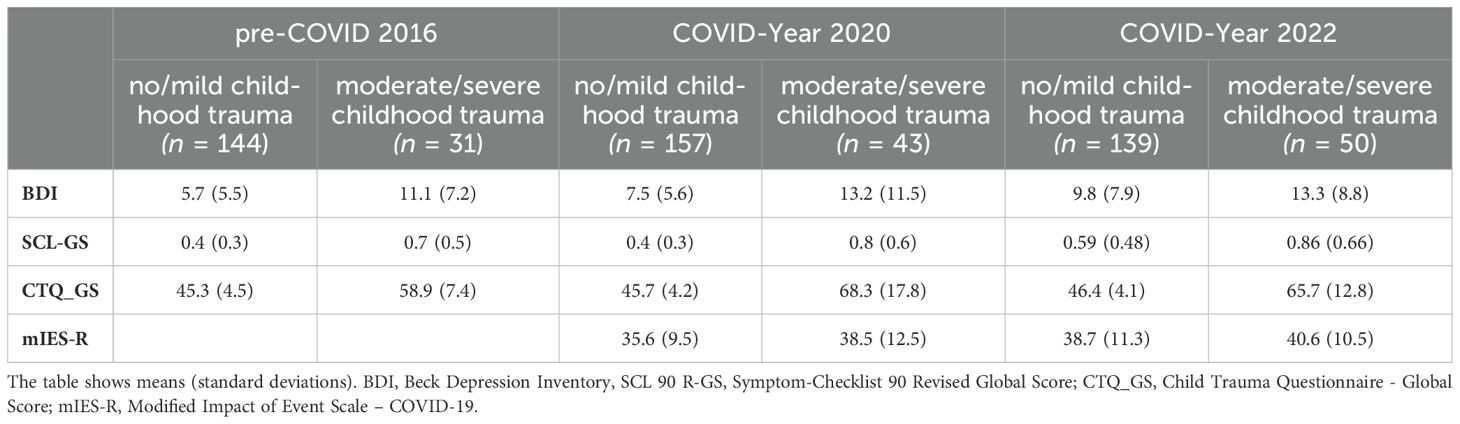
The ANCOVA using the BDI-II as the dependent variable revealed no significant interaction between the cohort and childhood trauma experiences (F(2,557) = .737, p = .479).
However, there was a significant main effect of childhood trauma (F(1,557) = 43.512, p <.001, ηp2 =.072), with individuals who experienced moderate/severe trauma exhibiting significantly higher BDI-II scores compared to those who experienced no/mild childhood trauma. Adjusted means were 7.66, 95% CI [6.99, 8.33], for the no/mild trauma group and 12.53, 95% CI [11.25, 13.82], for the moderate/severe trauma group.
Furthermore, a significant main effect of cohort was identified (F(2,557) = 8.097, p <.001, ηp2 = .028). After adjusting for age, Bonferroni-corrected post-hoc tests revealed that the pre-COVID group had the lowest BDI-II score (adjusted mean = 7.92, 95% CI [6.46, 9.37]), differing significantly from both the COVID-Year 2020 cohort (p = .033; adjusted mean = 10.38, 95% CI [9.17, 11.59]) and the COVID-Year 2022 cohort (p <.001; adjusted mean = 11.99, 95% CI [10.77, 13.21]). There was no significant difference in the BDI-II scores between the COVID-Year 2020 and COVID-Year 2022 cohorts (p = .201).
After adjusting for age, Bonferroni-corrected post-hoc tests revealed significant differences in the BDI-II scores between the three cohorts in the no/mild childhood trauma group. The pre-COVID group (adjusted mean = 5.28, 95% CI [4.04, 6.52]) had lower scores than both the COVID-19 Year 2020 cohort (p = .024; adjusted mean = 7.55, 95% CI [6.43, 8.67]) and the COVID-19 Year 2022 cohort (p <.001; adjusted mean = 10.14, 95% CI [8.90, 11.38]). Furthermore, the COVID-19 Year 2020 cohort had lower BDI-II scores than the COVID-19 Year 2022 cohort (p = .007).
No significant differences in the BDI-II scores were observed between the three cohorts in the moderate/severe childhood trauma group.
Post-hoc analyses revealed an achieved statistical power of 0.96 or higher for both significant main effects in the ANCOVA.
Figure 1 presents the means and 95% confidence intervals (CIs) of the BDI-II scores for the three cohorts and the two childhood trauma groups.
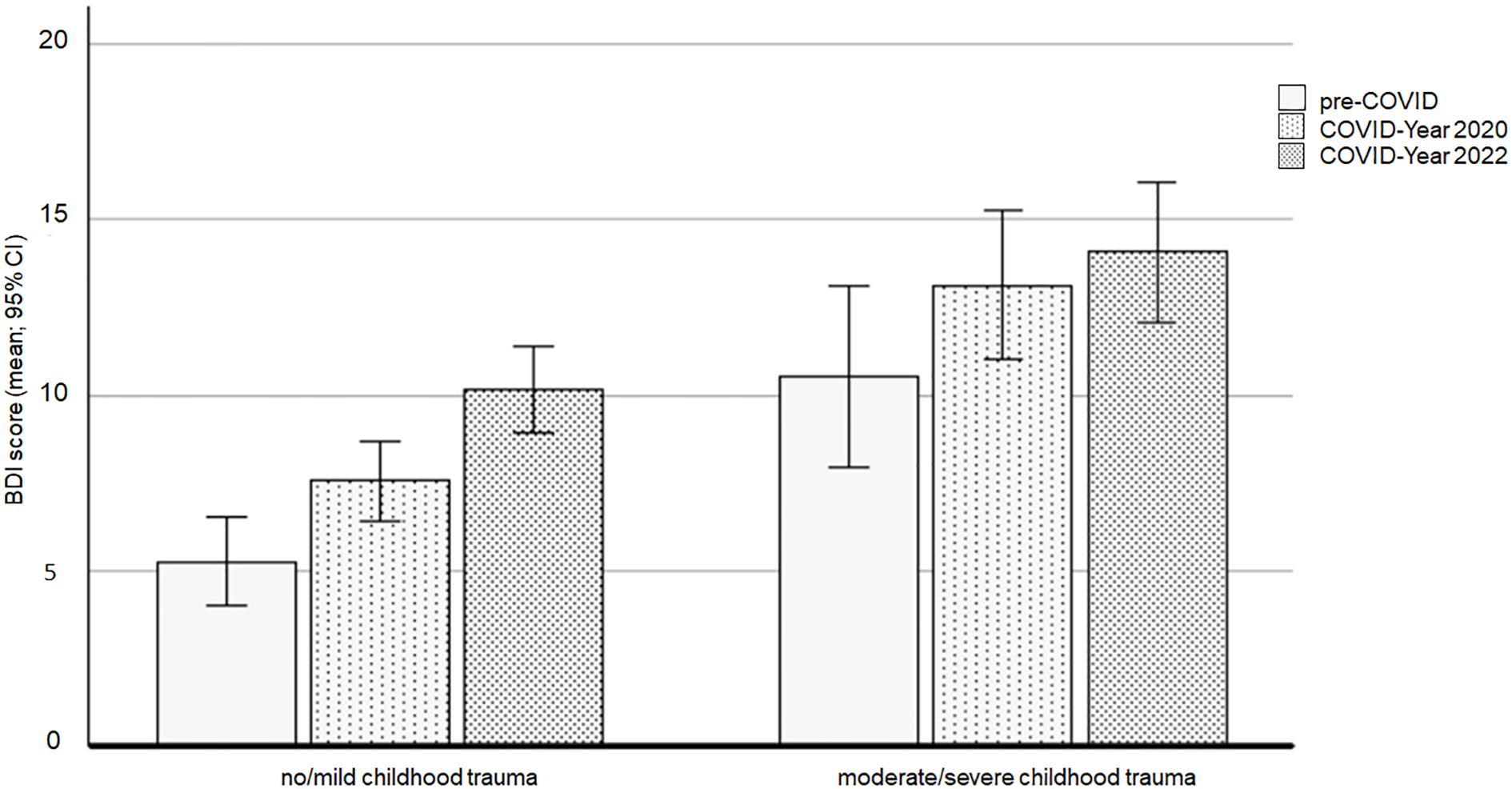
Figure 1. BDI scores affected by the COVID-19 pandemic and the experience of childhood trauma. BDI, Beck’s Depression Inventory.
3.3 The impact of COVID-19 pandemic and childhood trauma on psychological distress
The ANCOVA using the SCL-90-R Global Severity Index (GSI) showed no significant interaction between cohort and childhoodtrauma (F(2,557) = .190, p = .827). However, there was a significant main effect of trauma (F(1,557) = 44.642, p <.001, ηp2 = .074), with significantly higher GSI score in the moderate/severe childhood trauma group compared to the no/mild childhood trauma group (p <.001). Adjusted means were 0.48, 95% CI [0.44, 0.52], for the no/mild trauma group and 0.78, 95% CI [0.70, 0.86], for the moderate/severe trauma group.
A significant main effect of cohort was also found (F(2,557) = 4.965, p = .007, ηp2 = .018). Post-hoc tests indicated that the GSI score was significantly higher in the COVID-Year 2022 cohort (adjusted mean = 0.74, 95% CI [0.66, 0.81]) compared to the pre-COVID group (p = .012; adjusted mean = 0.56, 95% CI [0.47, 0.65]) and the COVID-Year 2020 cohort (p = .038; adjusted mean = 0.60, 95% CI [0.53, 0.68]). There was no significant difference in GSI scores between the pre-COVID and the COVID-Year 2020 cohorts (p = 1.000).
Further analysis within each childhood trauma group revealed significant differences in GSI scores between the three cohorts in the no/mild childhood trauma group. Specifically, the COVID-Year 2022 cohort (adjusted mean = 0.60, 95% CI [0.52, 0.68]) had higher scores than both the pre-COVID cohort (p = .002; adjusted mean = 0.40, 95% CI [0.33, 0.48]) and the COVID-Year 2020 group (p = .004; adjusted mean = 0.43, 95% CI [0.36, 0.50]). No significant differences in GSI scores were observed between the cohorts in the moderate/severe childhood trauma group.
Figure 2 presents the means and 95% confidence intervals (CIs) of the GSI scores for the three cohorts and the two childhood trauma groups.
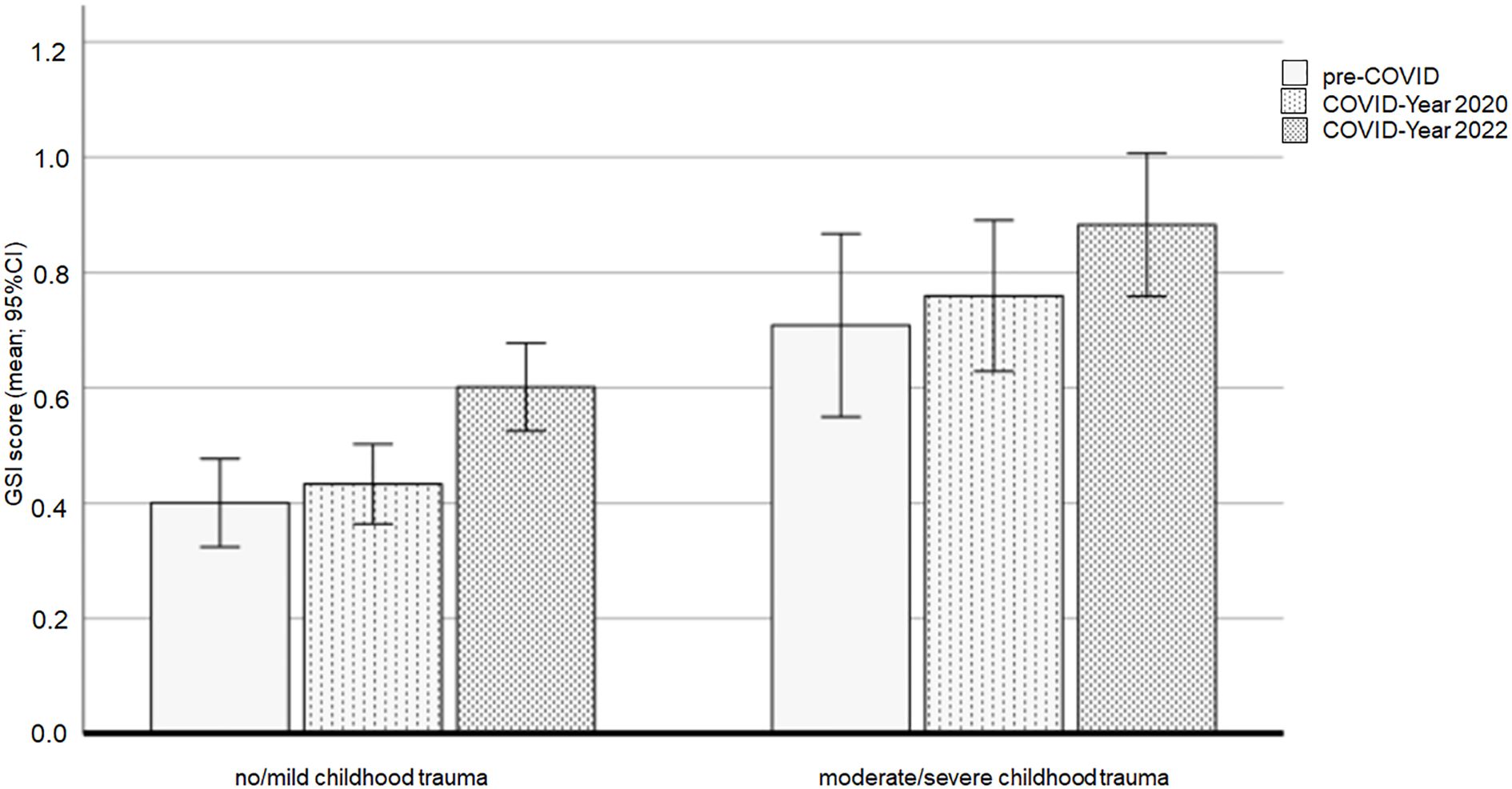
Figure 2. GSI scores affected by the COVID-19 pandemic and the experience of childhood trauma. Note: GSI = SCL-90 General Severity Index.
Post-hoc analyses revealed an achieved statistical power of at least 0.85 for both significant main effects in the ANCOVA.
3.4 Differences between the cohorts in the childhood trauma scores
The ANCOVA using the CTQ global score showed a significant main effect of cohort (F(2,557) = 11.731, p <.001, ηp2 = .040), a main effect of childhood trauma (F(1,557) = 579.060, p <.001, ηp2 = .510), and a significant interaction between cohort and childhood trauma (F(2,557) = 10.561, p <.001, ηp2 = .037).
Overall, there was a significant difference in the CTQ scores between the three cohorts. The pre-COVID cohort had the lowest CTQ global score (adjusted mean = 52.22, 95% CI [50.70, 53.73]) differing significantly from both the COVID-Year 2020 cohort (p <.001; adjusted mean = 57.01, 95% CI [55.75, 58.27]) and the COVID-Year 2022 cohort (p = .001; adjusted mean = 55.97, 95% CI [54.70, 57.24]). There was no significant difference in CTQ scores between COVID-Year 2020 and COVID-Year 2022 cohorts (p = .759).
As expected, given that childhood trauma groups were derived from CTQ scores, there was a significant difference in CTQ scores between the childhood trauma groups, with lower scores in the no/mild childhood trauma group (adjusted mean = 45.82, 95% CI [45.12, 46.52]) compared to the moderate/severe childhood trauma group (p <.001; adjusted mean = 64.31, 95% CI [62.97, 65.65]).
To further understand the interaction between cohort and childhood trauma, separate Bonferroni-corrected post-hoc analyses were conducted for each trauma group. In the moderate/severe childhood trauma group, these tests revealed significant differences in CTQ global scores between the cohorts. The pre-COVID cohort (adjusted mean = 59.04, 95% CI [56.37, 61.71]) had lower scores compared to the COVID-Year 2020 cohort (p <.001; adjusted mean = 68.31, 95% CI [66.08, 70.53]) and the COVID-Year 2022 cohort (p <.001; adjusted mean = 65.59, 95% CI [63.47, 67.70]). No difference was observed between the COVID-Year 2020 and the COVID-Year 2022 cohorts (p = .249). In the no/mild childhood trauma group, there were no significant differences in CTQ global scores between the cohorts (all p’s >.05).
Figure 3 shows the means and 95% confidence intervals (CIs) of the CTQ global scores for the three cohorts and the two childhood trauma groups.
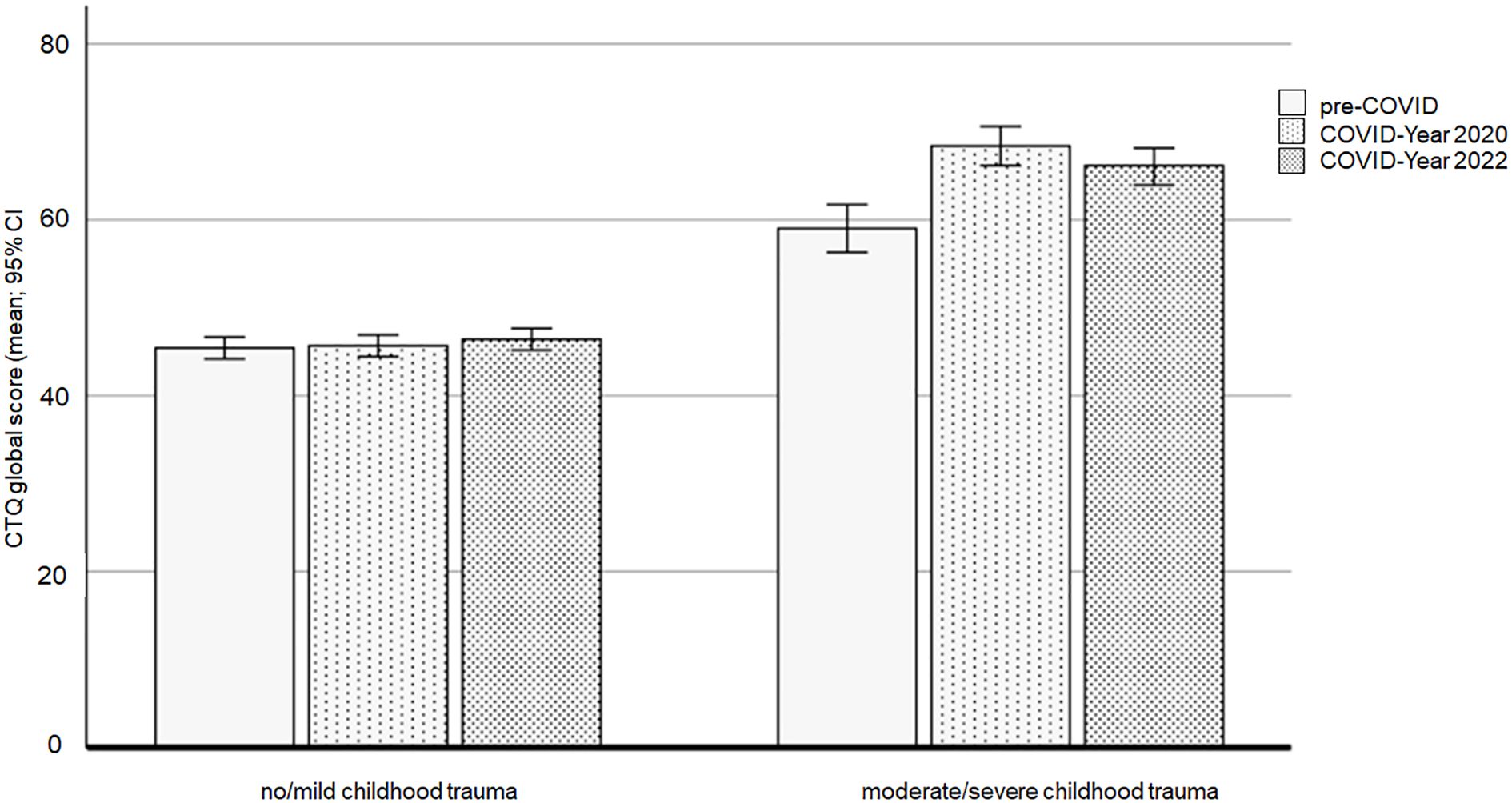
Figure 3. CTQ global scores affected by the COVID-19 pandemic and the experience of childhood trauma. Note: CTQ = Child Trauma Questionnaire.
Post-hoc analyses demonstrated an achieved statistical power of at least 0.99 for both the significant main effects and the interaction effect of CTQ scores.
3.5 The traumatic impact of the COVID-19 pandemic
The modified IES-R (mIES-R) was used to assess the traumatic impact of the COVID-19 pandemic in the two COVID-19 cohorts. The results revealed a marginal main effect of childhood trauma (F(1,384) = 3.598, p = .059, ηp2 = .009), with a trend toward higher mIES-R scores in the moderate/severe childhood trauma cohort compared to the no/mild childhood trauma cohort.
There was also a marginal effect of cohort (F(1,384) = 3.654, p = .057, ηp2 = .009), with lower mIES-R scores in the COVID-Year 2020 cohort (adjusted mean = 37.11, 95% CI [35.28, 38.94]) compared to the COVID-Year 2022 cohort (adjusted mean = 39.62, 95% CI [37.86, 41.39]). The interaction between cohort and childhood trauma did not reach significance (F(1,384) = .143, p = .705). Additionally, Bonferroni-corrected post hoc tests showed that mIES-R scores increased significantly over time only in the no/mild childhood trauma cohort (p = .019; adjusted mean for COVID-Year 2020 = 35.66, 95% CI [33.97, 37.36] and adjusted mean for COVID-Year 2022 = 38.66, 95% CI [36.86, 40.46]).
Figure 4 presents the means and 95% confidence intervals (CIs) for the mIES-R scores for the three cohorts and the two childhood trauma groups.
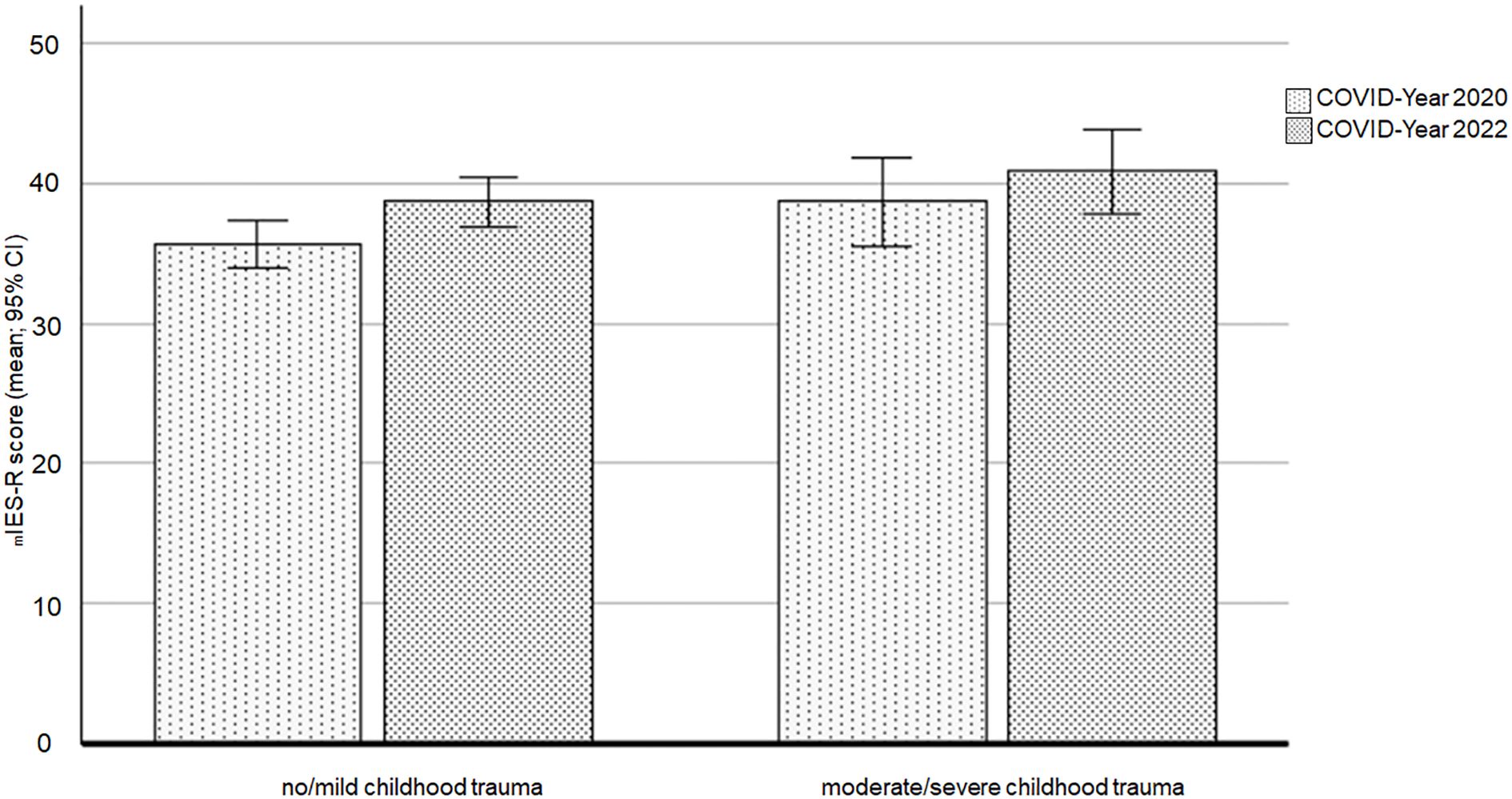
Figure 4. Impact of the COVID-19 pandemic on the two childhood trauma groups across the two COVID-19 cohorts. Note: mIES-R = Modified Impact of Event Scale – COVID-19.
4 Discussion
In general, individuals with a history of childhood trauma have an increased risk developing mental disorders including post-traumatic stress symptoms, depression, anxiety disorders, and substance use disorders (30, 32, 33). Consistent with this, the current study found that in all three cohorts, students with moderate/severe childhood trauma reported higher levels of depression (BDI-II) and greater subjective impairment due to both physical and psychological symptoms (SCL-90-R (GSI) compared to those with no/mild childhood trauma.
Remarkably, differences in mental health between the three cohorts were observed only in the no/mild childhood trauma group. Students in the Pre-Covid cohort had significantly lower levels of depressive symptoms and subjective impairment due to physical and psychological symptoms than the two cohorts surveyed during the pandemic (2020 and 2022). This suggests, that the increase in mental health problems during the COVID-19 pandemic was primarily observed in students with no/mild childhood trauma, while those with pre-existing moderate to severe childhood trauma histories showed relatively consistent high psychological distress levels regardless of the pandemic context.
Even prior to the COVID-19 pandemic, young adults, particularly students, experienced elevated levels of psychological distress (5). The pandemic introduced additional stressors, burdens, and challenges (45). Several studies have reported increased mental health symptoms and illnesses among students during the pandemic [e.g., (46, 47)]. Longitudinal studies have also demonstrated an increase in perceived psychological distress over the course of the pandemic (18, 48), or at least persistently high levels even after restriction eased (49). In this context, Goral, Lahad, and Aharonson-Daniel (50) proposed that psychological stress becomes more pronounced and severe when a traumatic experience extends over a longer period of time. Continuous exposure to stressors makes it more difficult to cope with stress, and both vulnerability and sensitivity to stress increase (50, 51). The findings of this study are consistent with those of previous research, which showed that students in the COVID-Year 2022 cohort reported more psychological distress due to the COVID-19 pandemic (mIES-R scale) than those in the COVID-Year 2020 cohort.
In contrast, no significant differences in depression (BDI-II) or SCL-90-R scores were found between the pre-Covid cohort and the two pandemic cohorts among students with moderate/severe childhood trauma. Furthermore, these students showed no change in the mIES-R scores between 2020 and 2022. These results are consistent with a study from Russo et al. (52), who found that in individuals with adverse childhood experiences (ACEs), pandemic-related stressors primarily impacted those with less emotion regulation deficits. In individuals with ACEs and higher emotion regulation deficits, the added stress caused of the COVID-19 pandemic did not result in further mental health deterioration, potentially due to a ceiling effect. Moreover, individuals with severe trauma experiences often perceive relationships as a source of threat (53). Consequently, social distancing and isolation during lockdowns may have had less impact on them. Some research on attentional bias supports this notion, suggesting that individuals with prior trauma exposure may be more avoidant of threat cues or have a higher threshold for perceiving them, leading to less fear or distress related to the pandemic [e.g., (54, 55)]. In contrast, other studies have found that past trauma exposure is associated with an attentional bias towards threat, potentially contributing to increased mental health problems during the COVID-19 pandemic (56, 57).
4.1 Limitations
A limitation of the current study is the cross-sectional cohort design, which prevents a direct examination of the trajectory of mental health problems in individuals with a history of childhood trauma. However, so far, longitudinal studies on this topic have yielded inconsistent results. Some studies suggest that individuals with pre-existing mental health diagnosis and/or a history of childhood trauma may experience worsening symptoms during the pandemic [e.g., (58, 59)], while others, particularly those involving adults receiving treatment for PTSD, show less fear, distress, and trauma reminders [e.g., (60, 61)]. This latter effect is particularly pronounced when controlling for complex PTSD symptoms (21).
In addition, the three cohorts in this study were not perfectly matched and differed in age. Moreover, the pre-COVID cohort had lower global CTQ scores than the two COVID cohorts among students with moderate/severe childhood trauma. Since participants retrospectively assessed the severity of child maltreatment and abuse, recall bias is a potential concern, potentially leading to an overestimation of the relationship between adverse childhood experiences and poorer health outcomes (62).
Furthermore, the present study focused exclusively on university students, limiting the generalizability of the findings to other populations. However, the homogenous education level within the student sample is a strength, as it eliminates potential confounding effects of education. It is also important to note that the sample has a higher proportion of female students, which may have influenced the results. Finally, the online recruitment strategy may have introduced selection bias.
4.2 Practical and clinical implications of the study
The results of this study have significant practical and clinical implications for mental health professionals, university administrators, and policy makers. Young adulthood is a high-risk period for developing mental health problems (45, 46). It is crucial to offer support, such as stress management training, to students, especially during stressful periods like the COVID-19 pandemic. Effective stress management skills that promote adaptive emotion regulation and coping strategies, and enhance a sense of control, can protect against stress-related illness, unhealthy behaviors, and the long-term physical and psychological effects of stress (63). In a recent study we could demonstrate that a 7-week app-based passive psychoeducation program for stress management significantly improved adaptive emotion regulation strategies and coping styles, even in students with low clinically relevant psychopathological symptoms (64). Since passive psychoeducation does not use elements of active psychotherapies or require homework, it is an easily accessible and cost-effective self-guided intervention.
In the current study, students with moderate to severe childhood trauma consistently reported high levels of depression and psychological distress, regardless of the pandemic context. This underscores the need for specialized mental health services tailored to trauma-affected individuals. Trauma-informed care approaches, including cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and emotion regulation training, should be integrated into university counseling services to better support these students.
5 Conclusions
This study highlights the vulnerability of students to mental health problems during the COVID-19 pandemic. It specifically examined whether students with a history of childhood trauma were more susceptible to pandemic-related stressors and mental health issues. Comparing three student cohorts before and during the pandemic, the study confirmed previous findings that individuals with moderate or severe childhood trauma reported higher levels of psychological and physical distress than those with minimal or no trauma. However, the study did not find evidence that the pandemic disproportionately impacted the mental health of students with childhood trauma compared to those without. It is possible that individuals with pre-existing trauma exposure may engage in more avoidance of potentially threatening COVID-19-related information. Further research is needed to explore the complex interplay between the COVID-19 pandemic and its long-term effects on the mental health of individuals with a history of trauma.
Data availability statement
The datasets generated and/or analysed during the current study are available from the corresponding author upon reasonable request.
Ethics statement
The studies involving humans were approved by Ethics Review Board of the University of Innsbruck and the University of Graz. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EW: Conceptualization, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. AF: Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. IP: Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. SE: Methodology, Writing – original draft, Writing – review & editing. AL: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. VD: Methodology, Writing – original draft, Writing – review & editing. MC: Formal Analysis, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors wish to thank Claudia Immisch, Ramona Mühlburger, Franziska Rieger and Anna Katharina Pfeil for their assistance in data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ahmed N, Barnett P, Greenburgh A, Pemovska T, Stefanidou T, Lyons N, et al. Mental health in Europe during the COVID-19 pandemic: a systematic review. Lancet Psychiatry. (2023) 10:537–56. doi: 10.1016/S2215-0366(23)00113-X
2. Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
3. Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J Abnormal Psychol. (2018) 127:623–38. doi: 10.1037/abn0000362
4. Rodriguez-Besteiro S, Tornero-Aguilera JF, Fernández-Lucas J, Clemente-Suárez VJ. Gender differences in the covid-19 pandemic risk perception, psychology and behaviors of spanish university students. Int J Environ Res Public Health. (2021) 18:3908. doi: 10.3390/ijerph18083908
5. Robotham D, Julian C. Stress and the higher education student: A critical review of the literature. J Further Higher Educ. (2006) 30:107–17. doi: 10.1080/03098770600617513
6. Eisenberg D, Golberstein E, Hunt J. Mental health and academic success in college. B.E J Economic Anal Policy. (2009) 9:1–37. doi: 10.2202/1935-1682.2191
7. Lee B, Krishan P, Goodwin L, Iduye D, Farfan de los Godos E, Fryer J, et al. Impact of COVID-19 mitigations on anxiety and depression amongst university students: A systematic review and meta-analysis. J Global Health. (2023) 13:6035. doi: 10.7189/jogh.13.06035
8. Quan L, Lu W, Zhen R, Zhou X. Post-traumatic stress disorders, anxiety, and depression in college students during the COVID-19 pandemic: a cross-sectional study. BMC Psychiatry. (2023) 23:228. doi: 10.1186/s12888-023-04660-9
9. Karasmanaki E, Tsantopoulos G. Impacts of social distancing during COVID-19 pandemic on the daily life of forestry students. Children Youth Serv Rev. (2021) 120:105781. doi: 10.1016/j.childyouth.2020.105781
10. Kaubisch LT, Reck C, von Tettenborn A, Woll CFJ. The COVID-19 pandemic as a traumatic event and the associated psychological impact on families - A systematic review. J Affect Disord. (2022) 319:27–39. doi: 10.1016/j.jad.2022.08.109
11. World Health Organization. ICD-11: International classification of diseases (11th Revision)(2019). Available online at: https://icd.who.int/ (Accessed June 18, 2024).
12. APA (American Psychiatric Association). Diagnostic and statistical manual of mentaldisorders (5th ed). Arlington: American Psychiatric Publishing (2013). doi: 10.1176/appi.books.9780890425596
13. Wang Y, Xu S, Chen Y, Liu H. A decline in perceived social status leads to post-traumatic stress disorder symptoms in adults half a year after the outbreak of the COVID-19 pandemic: consideration of the mediation effect of perceived vulnerability to disease. Front Psychiatry. (2023) 14:1217264. doi: 10.3389/fpsyt.2023.1217264
14. Bach M, Bitterlich W. COVID-19 und Traumafolgesymptome: repräsentative Daten aus Österreich. Psychopraxis Neuropraxis. (2021) 24:299–303. doi: 10.1007/s00739-021-00748-7
15. Macalli M, Texier N, Schück S, Côté SM, Tzourio C. A repeated cross-sectional analysis assessing mental health conditions of adults as per student status during key periods of the COVID-19 epidemic in France. Sci Rep. (2021) 11:21455. doi: 10.1038/s41598-021-00471-8
16. Jia Q, Qu Y, Sun H, Huo H, Yin H, You D. Mental health among medical students during COVID-19: A systematic review and meta-analysis. Front Psychol. (2022) 13:846789. doi: 10.3389/fpsyg.2022.846789
17. Lotzin A, Krause L, Acquarini E, Ajdukovic D, Anastassiou-Hadjicharalambous X, Ardino V, et al. Risk and protective factors for posttraumatic stress disorder in trauma-exposed individuals during the COVID-19 pandemic – findings from a pan-European study. Eur J Psychotraumatol. (2022) 13:2138099. doi: 10.1080/20008066.2022.2138099
18. Peng P, Hao Y, Liu Y, Chen S, Wang Y, Yang Q, et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. (2023) 321:167–81. doi: 10.1016/j.jad.2022.10.040
19. Gewirtz-Meydan A, Lassri D. A profile analysis of COVID-19 stress-related reactions: The importance of early childhood abuse, psychopathology, and interpersonal relationships. Child Abuse Negl. (2022) 130:105442. doi: 10.1016/j.chiabu.2021.105442
20. Goldstein E, Topitzes J, Brown RL, Jussel AB. Mental health among university employees during the COVID-19 pandemic: The role of previous life trauma and current posttraumatic stress symptoms. Psychol Trauma. (2023) 15:536–45. doi: 10.1037/tra0001332
21. Tsur N, Abu-Raiya H. COVID-19-related fear and stress among individuals who experienced child abuse: The mediating effect of complex posttraumatic stress disorder. Child Abuse Negl. (2020) 110:104694. doi: 10.1016/j.chiabu.2020.104694
22. Mayo D, Corey S, Kelly LH, Yohannes S, Youngquist AL, Stuart BK, et al. The Role of Trauma and Stressful Life Events among Individuals at Clinical High Risk for Psychosis: A Review. Front Psychiatry. (2017) 8:55. doi: 10.3389/fpsyt.2017.00055
23. Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br J Psychiatry. (2010) 197:378–85. doi: 10.1192/bjp.bp.110.080499
24. Read JP, Ouimette P, White J, Colder C, Farrow S. Rates of DSM-IV-TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychol Trauma. (2011) 3:148–56. doi: 10.1037/a0021260
25. Strand EB, Brandt J, Rogers K, Fonken L, Chun R, Conlon P, et al. Adverse childhood experiences among veterinary medical students: a multi-site study. J Vet Med Educ. (2017) 44:260–7. doi: 10.3138/jvme.0816-123R
26. Miller AB, Esposito-Smythers C, Weismoore JT, Renshaw KD. The relation between child maltreatment and adolescent suicidal behavior: a systematic review and critical examination of the literature. Clin Child Fam Psychol Rev. (2013) 16:146–72. doi: 10.1007/s10567-013-0131-5
27. van Nierop M, Viechtbauer W, Gunther N, van Zelst C, de Graaf R, Ten Have M, et al. Childhood trauma is associated with a specific admixture of affective, anxiety, and psychosis symptoms cutting across traditional diagnostic boundaries. Psychol Med. (2015) 45:1277–88. doi: 10.1017/S0033291714002372
28. Riedl D, Lampe A, Exenberger S, Nolte T, Trawöger I, Beck T. Prevalence of adverse childhood experiences (ACEs) and associated physical and mental health problems amongst hospital patients: Results from a cross-sectional study. Gen Hosp Psychiatry. (2020) 64:80–6. doi: 10.1016/j.genhosppsych.2020.03.005
29. Dykshoorn KL. Trauma-related obsessive–compulsive disorder: a review. Health Psychol Behav Med. (2014) 2:517–28. doi: 10.1080/21642850.2014.905207
30. Alradhi MA, Moore J, Patte KA, O’Leary DD, Wade TJ. Adverse childhood experiences and COVID-19 stress on changes in mental health among young adults. Int J Environ Res Public Health. (2022) 19:12874. doi: 10.3390/ijerph191912874
31. Xia J, Zhu L, Huang H, Fan P, Zhou M, Cai XL, et al. Relationships between childhood trauma and mental health during the COVID-19 pandemic: a network analysis. Front Psychiatry. (2023) 14:1251473. doi: 10.3389/fpsyt.2023.1251473
32. Stanislawski ER, Saali A, Magill EB, Deshpande R, Kumar V, Chan C, et al. Longitudinal mental health outcomes of third-year medical students rotating through the wards during COVID-19. Psychiatry Res. (2023) 320:115030. doi: 10.1016/j.psychres.2022.115030
33. Xie M, Tang Y, Zhu L, Dai M, Wu Y, Huang Y, et al. Childhood trauma and mental health status in general population: A series mediation examination of psychological distress in COVID-19 pandemic and global sleep quality. Front Psychiatry. (2021) 12:782913. doi: 10.3389/fpsyt.2021.782913
34. Bussone S, Pesca C, Tambelli R, Carola V. Psychological health issues subsequent to SARS-cov 2 restrictive measures: the role of parental bonding and attachment style. Front Psychiatry. (2020) 11:589444. doi: 10.3389/fpsyt.2020.589444
35. Bernstein DP, Fink L, Handelsman L, Foote J. Childhood trauma questionnaire. In: Assessment of family violence: A handbook for researchers and practitioners. The Psychological Corporation, TX (1998).
36. Hautzinger M, Keller F, Kühner C. Beck Depressions-Inventar (BDI-II): Deutsche Ausgabe des Beck-Depressions-Inventars nach Aaron T. Beck, Robert A. Steer und Gregory K. Brown. Pearson, Frankfurt am Main (2009).
37. Wang YP, Gorenstein C. Psychometric properties of the Beck Depression Inverntory-II: a comprehensive review. Rev Bras Psiquiatria. (2013) 35:416–43. doi: 10.1590/1516-4446-2012-10418
38. Kühner C, Bürger C, Keller F, Hautzinger M. Reliabilität und Validität des revidierten Beck-Depressionsinventars (BDI-II) Befunde aus deutschsprachigen Stichproben. Nervenarzt. (2007) 78:651–6. doi: 10.1007/s00115-006-2098-7
39. Weiss DS. The impact of event scale: revised. In: Wilson JP, Tang CS, editors. Cross-Cultural Assessment of Psychological Trauma and PTSD. International and cultural psychology series. Springer, Boston (2007). p. 219–38. doi: 10.1007/978-0-387-70990-1_10
40. Klinitzke G, Romppel M, Häuser W, Brähler E, Glaesmer H. The German Version of the Childhood Trauma Questionnaire (CTQ): psychometric characteristics in a representative sample of the general population. Psychotherapie Psychosomatik medizinische Psychol. (2012) 62:47–51. doi: 10.1055/s-0031-1295495
41. Derogatis LR, Rickels K, Rock AF. The SCL-90-R and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. (1976) 128:280–9. doi: 10.1192/bjp.128.3.280
42. Franke GH. Die Symptom-Checkliste von Derogatis (SCL-90-R) - Deutsche Version. Göttingen: Beltz (2002).
43. Schmitz N, Hartkamp N, Kiuse J, Franke GH, Reister G, Tress W. The Symptom Check-List-90-R (SCL-90-R): A German validation study. Qual Life Res. (2000) 9:185–93. doi: 10.1023/a:1008931926181
44. Faul F, Erdfelder E, Buchner A, Lang AG. GPower 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91. doi: 10.3758/bf03193146
45. Elharake JA, Akbar F, Malik AA, Gilliam W, Omer SB. Mental health impact of COVID-19 among children and college students: A systematic review. Child Psychiatry Hum Dev. (2022) 54:913–25. doi: 10.1007/s10578-021-01297-1
46. Kohls E, Guenthner L, Baldofski S, Brock T, Schuhr J, Rummel-Kluge C. Two years COVID-19 pandemic: Development of university students’ mental health 2020–2022. Front Psychiatry. (2023) 14:1122256. doi: 10.3389/fpsyt.2023.1122256
47. Zurlo MC, Cattaneo Della Volta MF, Vallone F. Psychological health conditions and COVID-19-related stressors among university students: A repeated cross-sectional survey. Front Psychol. (2022) 12:741332. doi: 10.3389/fpsyg.2021.741332
48. Ausín B, González-Sanguino C, Castellanos MA, Sáiz J, Zamorano S, Vaquero C, et al. The psychological impact of the COVID-19 pandemic in Spain: A longitudinal study. Psicothema. (2022) 34:66–73. doi: 10.7334/psicothema2021.290
49. Kaltschik S, Pieh C, Dale R, Probst T, Pammer B, Humer E. Assessment of the long-term mental health effects on Austrian students after COVID-19 restrictions. Int J Environ Res Public Health. (2022) 19:13110. doi: 10.3390/ijerph192013110
50. Goral A, Lahad M, Aharonson-Daniel L. Differences in posttraumatic stress characteristics by duration of exposure to trauma. Psychiatry Res. (2017) 258:101–7. doi: 10.1016/j.psychres.2017.09.079
51. Lanius RA, Rabellino D, Boyd JE, Harricharan S, Frewen PA, McKinnon MC. The innate alarm system in PTSD: conscious and subconscious processing of threat. Curr Opin Psychol. (2017) 14:109–15. doi: 10.1016/j.copsyc.2016.11.006
52. Russo JE, Dhruve DM, Oliveros AD. Coping with COVID-19: Testing the stress sensitization hypothesis among adults with and without a history of adverse childhood experiences. J Affect Disord Rep. (2022) 10:100379. doi: 10.1016/j.jadr.2022.100379
53. Charuvastra A, Cloitre M. Social bonds and posttraumatic stress disorder. Annu Rev Psychol. (2008) 59:301–28. doi: 10.1146/annurev.psych.58.110405.085650
54. Beevers CG, Lee HJ, Wells TT, Ellis AJ, Telch MJ. Association of predeployment gaze bias for emotion stimuli with later symptoms of PTSD and depression in soldiers deployed in Iraq. Am J Psychiatry. (2011) 168:735–41. doi: 10.1176/appi.ajp.2011.10091309
55. Sipos ML, Bar-Haim Y, Abend R, Adler AB, Bliese PD. Postdeployment threat-related attention bias interacts with combat exposure to account for PTSD and anxiety symptoms in soldiers. Depression Anxiety. (2014) 31:124–9. doi: 10.1002/da.22157
56. Cisler JM, Koster EHW. Mechanisms of attentional biases towards threat in anxiety disorders: An integrative review. Clin Psychol Rev. (2010) 30:203–16. doi: 10.1016/j.cpr.2009.11.003
57. Depierro J, D’Andrea W, Pole N. Attention biases in female survivors of chronic interpersonal violence: Relationship to traumarelated symptoms and physiology. Eur J Psychotraumatol. (2013) 4:1–10. doi: 10.3402/ejpt.v4i0.19135
58. Hafstad GS, Saetren SS, Wentzel-Larsen T, Augusti EM. Adolescents’ symptoms of anxiety and depression before and during the Covid-19 outbreak–A prospective population based study of teenagers in Norway. Lancet Regional Health Europe. (2021) 5:1–8. doi: 10.1016/j.lanepe.2021.100093
59. Seitz KI, Bertsch K, Herpertz SC. A prospective study of mental health during the COVID-19 pandemic in childhood trauma-exposed individuals: social support matters. J Traumatic Stress. (2021) 34:477–86. doi: 10.1002/jts.22660
60. Buttanshaw LE, Purnell LR, El-Leithy SM, Pain AS. Understanding the experiences of people with posttrau matic stress disorder (PTSD) during the COVID-19 pandemic: A qualitative study. psychol Trauma: Theory Research Practice Policy. (2022) 14:1347–55. doi: 10.1037/tra0001198
61. Sprang G, Eslinger J, Whitt-Woosley A, Gusler S, Clemans T. Child traumatic stress and COVID 19: the impact of the pandemic on a clinical sample of children in trauma treatment. J Child Adolesc Trauma. (2023) 16:659–70. doi: 10.1007/s40653-023-00531-3
62. Reuben A, Moftt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry. (2016) 57:1103–12. doi: 10.1111/jcpp.12621
63. Kato T. Frequently used coping scales: A meta-analysis. Stress Health J Int Soc Invest Stress. (2015) 31:315–23. doi: 10.1002/smi.2557
Keywords: childhood trauma, mental health, COVID-19, depression, psychological distress
Citation: Weiss EM, Fink A, Papousek I, Exenberger-Vanham S, Lampe A, Dresen V and Canazei M (2025) No particularly negative impact of the Covid-19 pandemic on the mental health of individuals with higher levels of childhood trauma. Front. Psychiatry 16:1452732. doi: 10.3389/fpsyt.2025.1452732
Received: 21 June 2024; Accepted: 14 March 2025;
Published: 04 April 2025.
Edited by:
Oliver Tüscher, Johannes Gutenberg University Mainz, GermanyReviewed by:
Smriti Nepal, The University of Sydney, AustraliaMiguel Landa-Blanco, National Autonomous University of Honduras, Honduras
Copyright © 2025 Weiss, Fink, Papousek, Exenberger-Vanham, Lampe, Dresen and Canazei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisabeth M. Weiss, ZWxpc2FiZXRoLndlaXNzQHVpYmsuYWMuYXQ=
 Elisabeth M. Weiss
Elisabeth M. Weiss Andreas Fink
Andreas Fink Ilona Papousek
Ilona Papousek Silvia Exenberger-Vanham
Silvia Exenberger-Vanham Astrid Lampe
Astrid Lampe Verena Dresen
Verena Dresen Markus Canazei
Markus Canazei