- 1Treatment of Disease Department, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 2Department of Pediatrics, Central Hospital of Jinan City, Jinan, Shandong, China
- 3College of Acupuncture and Massage, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
Background: Depressive symptom, a pervasive mental health disorder, has garnered increasing attention due to its intricate interconnections with various physiological processes. One emerging avenue of investigation delves into the potential association between depressive symptom and Homeostasis Model Assessment of Insulin Resistance (HOMA-IR), a parameter reflecting insulin resistance. The intricate interplay between these two domains holds promising implications for understanding the multifaceted nature of depressive symptom and its impact on metabolic health.
Methods: We used weighted multivariable logistic regression models with subgroup analysis to explore the relationship between depressive symptom and homeostasis model assessment of insulin resistance. Non-linear correlations were explored using fitted smoothing curves. Then, we constructed a two-piece linear regression model and performed a recursive algorithm to calculate the inflection point.
Results: The study included 20,282 participants in the United States. In the regression model adjusted for all confounding variables, the odds ratio (OR) for the correlation between depressive symptom and the Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) was 1.01 (95% CI: 1.00, 1.01). However, a significant discrepancy between trend tests and regression analyses suggests a potential non-linear relationship between depressive symptom and the assessment of insulin resistance using the Homeostasis Model. Constrained cubic spline analysis confirmed this non-linear relationship, identifying an inflection point at 10.47. Before the inflection point, depressive symptom exhibited a significantly positive correlation with the assessment of insulin resistance using the Homeostasis Model. However, after the inflection point, a negative correlation was observed, though it did not reach statistical significance.
Conclusion: We found a curve-like relationship between depressive symptom and homeostasis model assessment of insulin resistance.
1 Introduction
Depression is a prevalent and debilitating mental health disorder that significantly affects individuals’ quality of life worldwide. As per recent studies, it is estimated that Depression impacts over 300 million people globally, representing a substantial burden on both individual and public health systems (1). The adverse effects of Depression extend beyond psychological distress, contributing to considerable physical health risks, including a heightened likelihood of chronic illnesses such as cardiovascular disease and diabetes, thereby amplifying the overall disease burden (2, 3).
The pathogenesis of Depression involves a complex interplay of genetic, neurobiological, and environmental factors. Recent advances in genetic studies have identified specific loci associated with Depression, offering insights into its biological underpinnings (4). Concurrently, environmental factors, such as exposure to stress and adverse life events, have been closely linked to the development of Depression, highlighting the multifaceted nature of this condition (5, 6).
The Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) is a widely utilized index for assessing insulin resistance (IR), a key component in the pathophysiology of metabolic syndrome and type 2 diabetes mellitus. By integrating fasting plasma glucose and insulin levels, HOMA-IR offers a practical and efficient approach for evaluating IR in both clinical and research settings, facilitating early detection and intervention strategies for metabolic disorders (7).
In recent years, studies exploring the link between mood disorders and insulin resistance have been on the rise. Although there is a dearth of studies examining the relationship between depressive symptoms and insulin resistance, opinions among scholars vary. For example, research by Webb M et al. suggests that depressive symptoms are associated with elevated HOMA-IR levels (8). Conversely, Wu CY et al.’s study found no significant overall association between depressive symptoms and insulin resistance (9). Our objective is to leverage the NHANES database, which is both extensive and reliable, to enrich and further investigate the association between depressive symptoms and HOMA-IR.
2 Materials and methods
2.1 Study participants
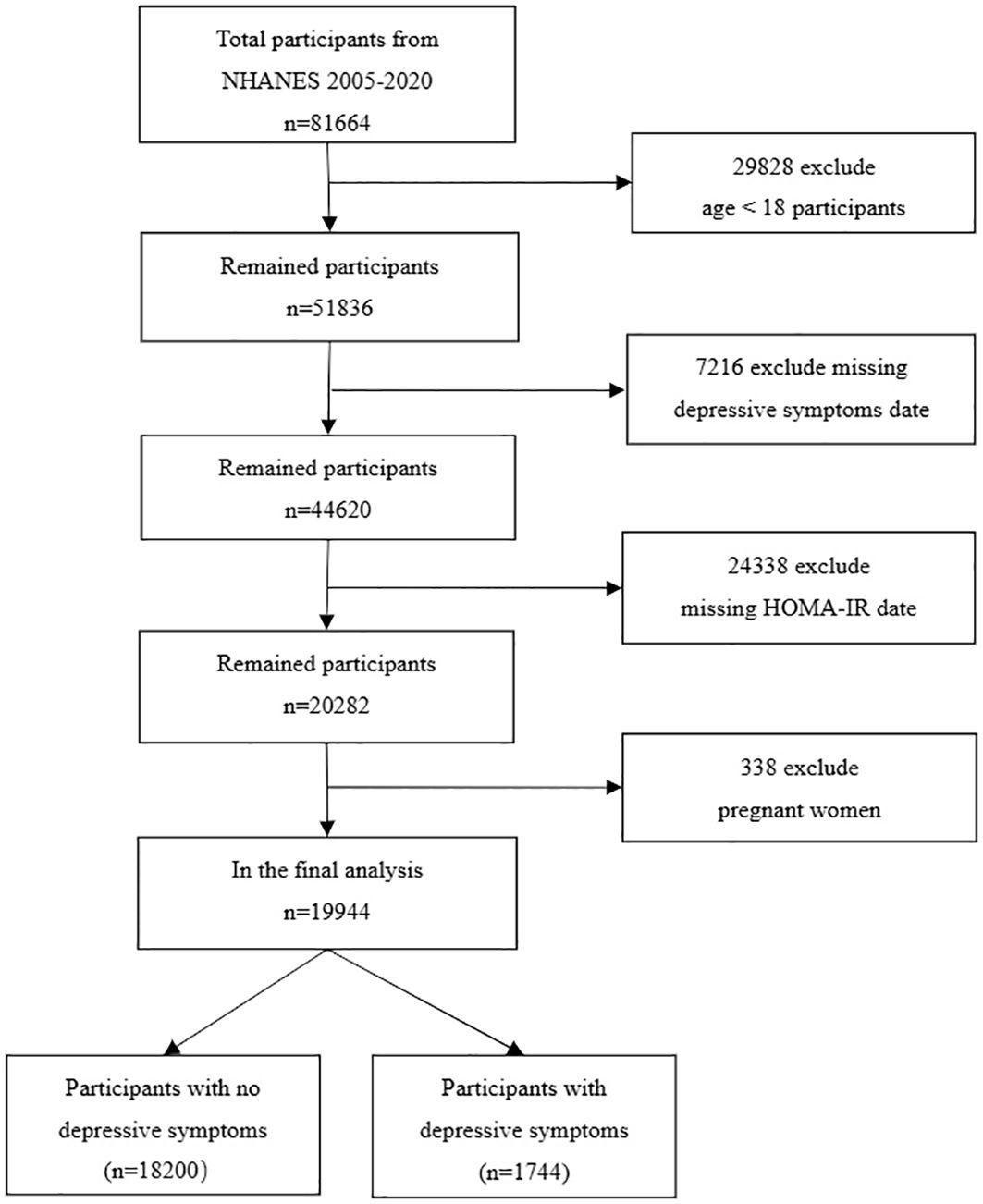
Our data was sourced from the United States’ NHANES database. We analyzed data from eight cycles between 2005 and 2020, which provided all the comprehensive information required for our study. NHANES, conducted by the National Center for Health Statistics, is a cross-sectional survey that includes a nationally representative sample of the non-institutionalized civilian U.S. population. Executed biennially, NHANES employs a stratified, multistage probability sampling approach and covers demographic, socioeconomic, health-related, and medical information. The NHANES research protocol is approved by the NCHS Research Ethics Review Board, and no additional ethical review was needed for this study. By pooling data from these eight cycles, we amassed a total of 49,461 participants. Our study’s participants were filtered based on the following exclusion criteria: 1. Age under 18; 2. Incomplete Patient Health Questionnaire-9 (PHQ-9); 3. Absence of HOMA-IR data; 4. Pregnant women. Following the exclusion of 29,828 participants under 18 years of age, 7,216 subjects lacking data on depressive symptoms, 24,338 subjects without HOMA-IR information, and 338 pregnant women, we were left with a study cohort of 19,944 subjects (Figure 1).
2.2 Study variables
2.2.1 Definition of depressive symptom
The survey utilized the 9-Item Patient Health Questionnaire (PHQ-9) to evaluate symptoms of depression that occurred within the two weeks leading up to the assessment. Designed to align with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, the PHQ-9 targets the nine specific diagnostic indicators of major depressive disorder, which include feelings of sadness, diminished interest in activities, sleep irregularities, tiredness, reduced self-worth, changes in appetite, concentration difficulties, noticeable restlessness or slowed behavior, and thoughts of self-harm. Scores for each question were defined as 0 (none), 1 (a few days), 2 (more than half the days), or 3 (almost every day), and total scale scores ranged from 0 to 27. A person with a total score of 10 on the PHQ-9 was considered to have major depressive disorder; the sensitivity of this cut-off value was 88%, and the specificity was 88% (10).
2.2.2 Definition of HOMA-IR
A blood sample was obtained from participants who underwent a morning physical examination after fasting for at least 8 hours. The plasma glucose level was determined using the COBRAS MIRA hexokinase enzymatic reference method (Roche Diagnostics, Indianapolis, IN), while the serum insulin level was measured using a radio-immunoassay (Pharmacia Diagnostics, Uppsala, Sweden). To assess insulin resistance (IR), which is commonly evaluated in large epidemiological studies, we utilized the homeostasis model assessment of IR (HOMA-IR) formula: fasting serum insulin (μU/mL) multiplied by fasting plasma glucose (mmol/L), divided by 22.5 (7).
2.2.3 Assessment of other variables
The CDC collected demographic, lifestyle, self-reported health, physical measurement, and biochemical data systematically and comprehensively, in the form of individual interviews with computer assistance. In our study, the main demographic variables required were the participants’ age, sex, ethnicity, education, and income poverty rate; lifestyle variables we considered included the participants’ smoking status, alcohol consumption, and recreational activities; physical variables included BMI; health status: diabetes, hypertension, hyperlipidemia, heart disease, stroke. Smoking status: Never: participants had smoked less than 100 cigarettes so far; Former: participants had a history of smoking but did not currently smoke; Now: participants were still smoking (11). Recreational activities: “yes” and “no”. Stroke was determined by the question MCQ160f, which specifically asked, “Have you ever been told by a doctor or other health professional that you have had a stroke?” Cardiovascular disease was obtained from the Medical Status Questionnaire, which recorded whether participants had been informed by a doctor that they had coronary heart disease, congestive heart failure, or a heart attack (12). Diabetes diagnosis (diabetes and prediabetes): at least one of the following: 1. Fasting plasma glucose (FPG >7.0 mmol/L). 2. Glycosylated hemoglobin HbA1c (>= 6.5%). 3. Random plasma glucose (>= 11.1mmol/L). 4. 2 h OGTT plasma glucose (>= 11.1mmol/L). 5. The doctor says you have diabetes. 6. IFG (6.11mmol/L <=FPG <=7.0mmol/L). 7. IGT (7.7mmol/L <=OGTT <=11.1mmol/L). Hypertension: At least one of the following. 1. Systolic blood pressure ≥140mmhg. 2. Diastolic blood pressure ≥90mmhg. 3. Taking antihypertensive medication. 4. Self-reported hypertension. Hyperlipidemia: One of the following. 1. Triglycerides ≥150mg/dL. 2. Total cholesterol ≥200mg/dL. 3. Low-density lipoprotein (LDL) ≥130mg/dL. 4. High-density lipoprotein (HDL): ≤50mg/dL for women, ≤40mg/dL for men. 5. Taking lipid-lowering medication. Drinking status: Heavy (women: ≥3 drinks per day or ≥4 drinks in one sitting); Men: ≥4 drinks per day or ≥5 drinks in one sitting; binge drinking ≥5 days per month); Moderate (women: ≥2 drinks per day; Men: ≥3 drinks per day; binge drinking ≥2 days per month); Mild (women: 1 drink per day; Men: 2 drinks per day); Former (drank before, but no longer); Never (less than 12 drinks in a lifetime) (13).
2.3 Statistical analysis
The data analysis was conducted using weights in accordance with NCHS guidelines to ensure the sample’s representativeness. Missing variables were subjected to imputation. Missing data were imputed using predictive mean matching for numeric variables and logistic regression for binary variable. Participants were categorized into two groups based on the presence or absence of depressive symptom to assess baseline characteristics. Mean (95% CIs) depicted continuous variables, while percentages described categorical variables. To compare the baseline characteristics of continuous and categorical variables, we employed weighted linear regression for continuous variables, chi-square tests for unordered categorical variables, and Mann-Whitney U tests for ordered categorical variables. We conducted a weighted multiple logistic regression analysis to explore the association between HOMA-IR and depressive symptoms. The findings were presented through odds ratios (ORs) with 95% confidence intervals (95% CI). HOMA-IR was categorized into four equal quartiles, designated as Q1, Q2, Q3, and Q4, to assess the stability of the relationship under examination. To examine consistency and variations in the association across different population subgroups, stratified analyses along with linear trend tests were performed. The existence of a non-linear relationship between depressive symptom and HOMA-IR was evaluated using restricted cubic splines, and a recursive algorithm along with a two-piece linear regression model was employed to identify the inflection point in cases of nonlinearity. R software (version 4.2.0) and Empower Stats were utilized for statistical analyses, with statistical significance set at p < 0.05.
3 Results
3.1 Baseline characteristics
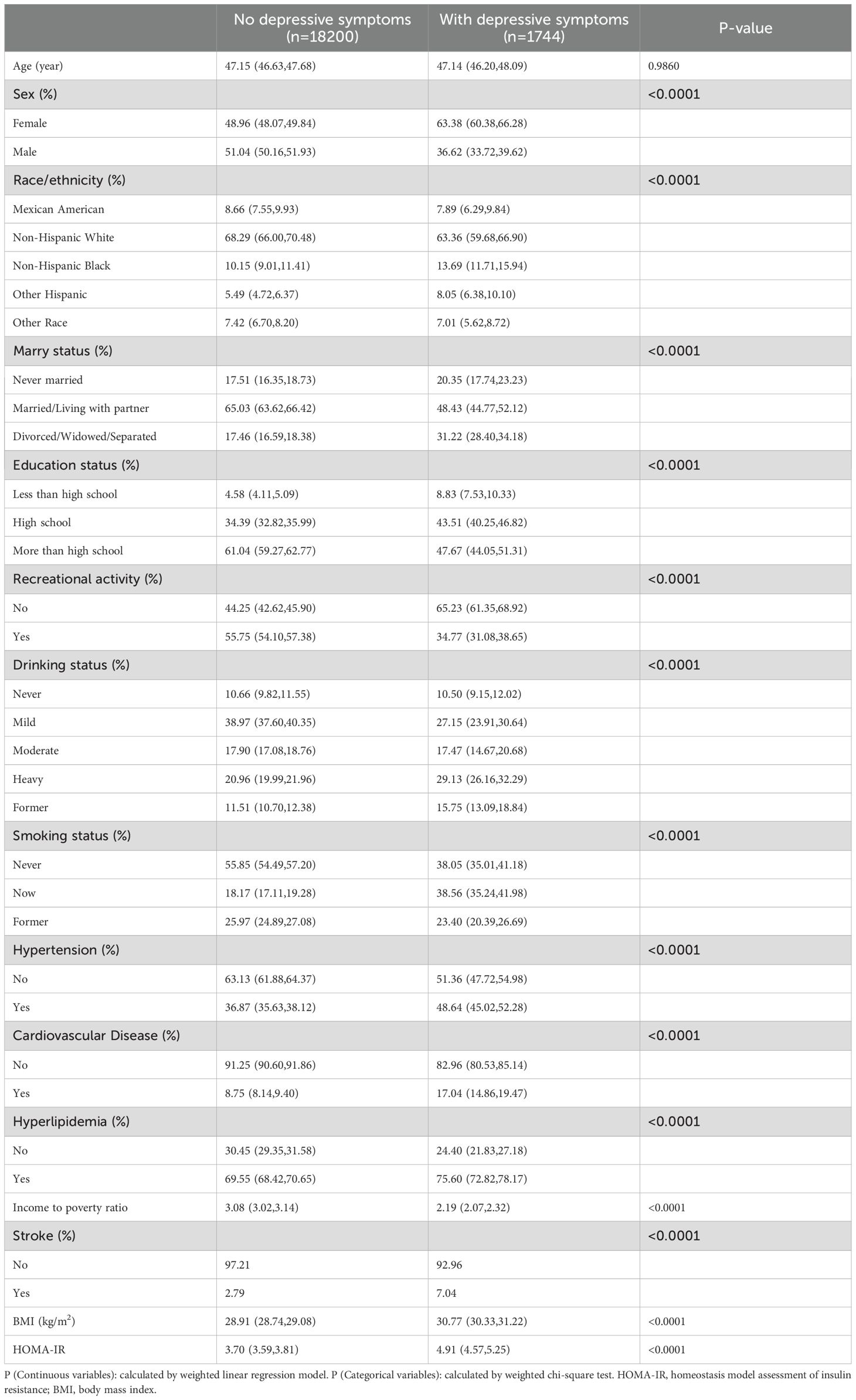
Table 1 shows the baseline characteristics of the participants. As can be seen from Table 1, in patients with depressive symptom, they have a larger BMI, HOMA-IR. Participants without depressive symptoms had an average age of 47.15 (46.63, 47.68), while those with depressive symptoms had an average age of 47.14 (46.20, 48.09). The prevalence of depressive symptom is higher among people with low education, women, hypertension, hyperlipidemia, stroke, cardiovascular and cerebrovascular diseases, and non-recreational activities.
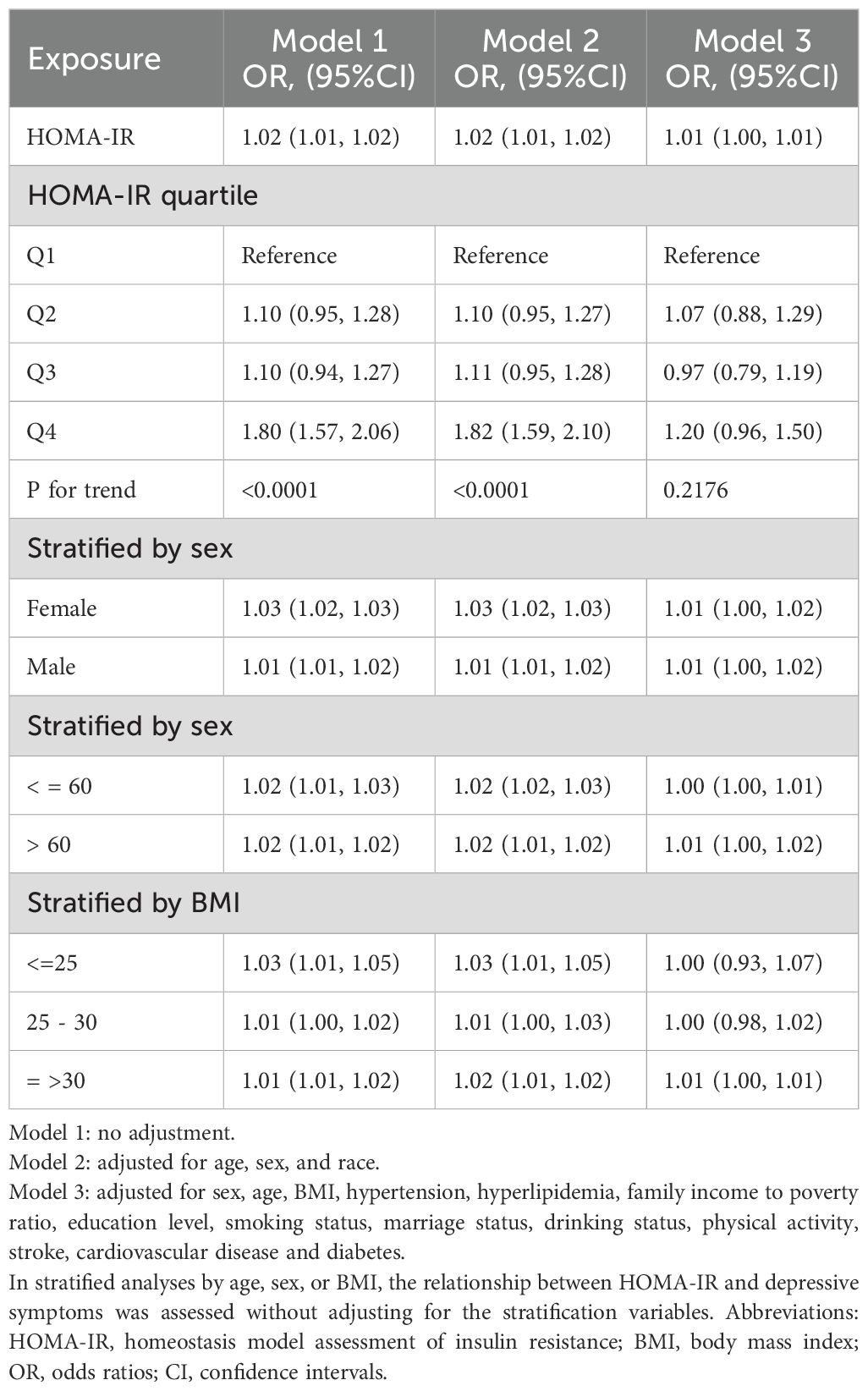
3.2 Association between depressive symptom and HOMA-IR
We used multiple logistic regression equation, sensitivity analysis and trend test to explore the relationship between depressive symptom and HOMA-IR, and the results were shown in Table 2. In model 1 (unadjusted model), OR (95%CI) was 1.02 (1.01, 1.02), indicating a significant positive correlation between depressive symptom and HOMA-IR. In model 3, We adjusted for sex, age, race, hyperlipidemia, family income to poverty ratio, education level, smoking status, marriage status, drinking status, physical activity and other covariates, OR (95%CI) is 1.01 (1.00, 1.01). It also showed that there was a significant positive correlation between depressive symptom and HOMA-IR, but the correlation was weaker than model 1. HOMA-IR was stratified into four quartiles, designated as Q1, Q2, Q3, and Q4. In Model 3, taking Q1 as the reference category, the odds ratios (OR) and 95% confidence intervals (CI) for Q2, Q3, and Q4 were 1.07 (0.88, 1.29), 0.97 (0.79, 1.19), and 1.20 (0.96, 1.50), respectively. The p-value for trend across these quartiles exceeded 0.05. This indicates that there may be a curvilinear relationship between depressive symptom and HOMA-IR. In the sex-stratified analysis, there was a significant positive correlation between depressive symptom and HOMA-IR, which was consistent with the results without stratification. When stratified by age and BMI, a significant positive association was found between depressive symptom and HOMA-IR in participants over 60 years old and obese. The association between depressive symptom and HOMA-IR was not significant in participants under 60 years of age and BMI<=30.
In further analysis, we used GAM and smoothing curve to analyze the association between Depressive symptom and HOMA-IR. We have established the curvilinear relationship between depressive symptoms and HOMA-IR, as depicted in Figure 2, and have determined the inflection point to be at 10.47, as detailed in Table 3. Before the inflection point, OR (95%CI) was 1.05 (1.02, 1.08), indicating a significant positive correlation between Depressive symptom and HOMA-IR. After the inflection point, OR (95%CI) was 0.99 (0.96, 1.01), indicating that Depressive symptom was negatively correlated with HOMA-IR, but the correlation was not significant. In subgroup analyses stratified by age or sex, this relationship remains non-linear (Figures 3, 4).
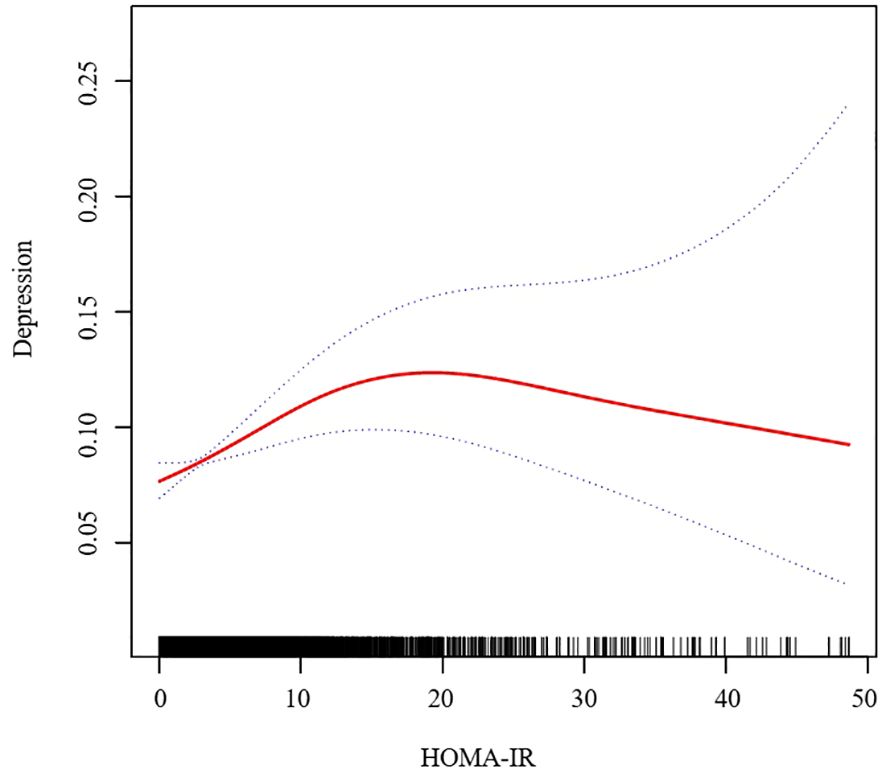
Figure 2. Association between HOMA-IR and Depressive symptom. We adjusted for sex, age, BMI, hypertension, hyperlipidemia, family income to poverty ratio, education level, smoking status, marriage status, drinking status, physical activity, cardiovascular disease and diabetes. HOMA-IR, homeostasis model assessment of insulin resistance; BMI, body mass index.
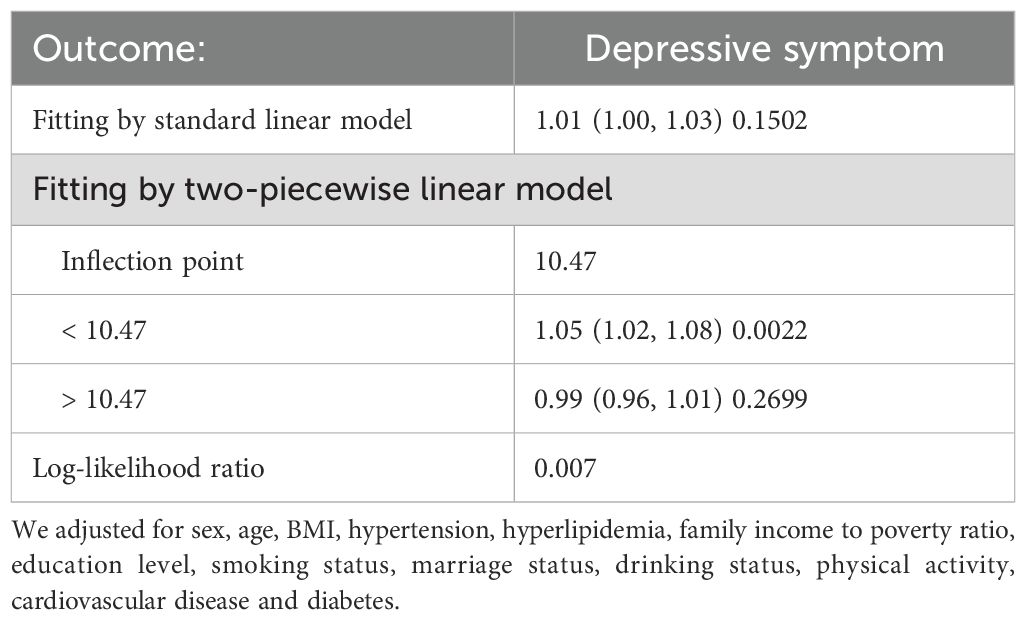
Table 3. Threshold effect analysis of HOMA-IR on Depressive symptom using a two-piecewise linear regression model.
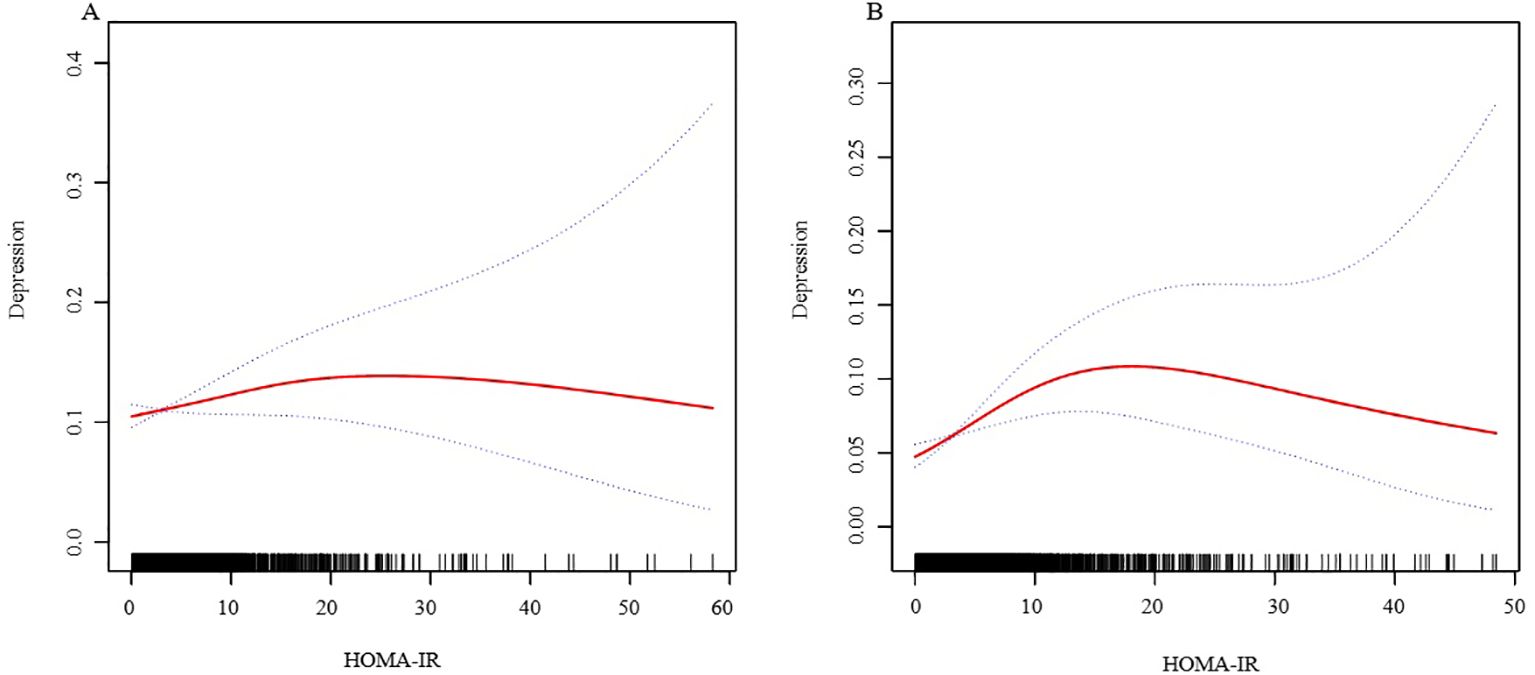
Figure 3. The association between HOMA-IR and depressive symptoms, analyzed with stratification by sex. (A: Female; B: Male). We adjusted for sex, age, BMI, hypertension, hyperlipidemia, family income to poverty ratio, education level, smoking status, marriage status, drinking status, physical activity, cardiovascular disease and diabetes. HOMA-IR, homeostasis model assessment of insulin resistance; BMI, body mass index.
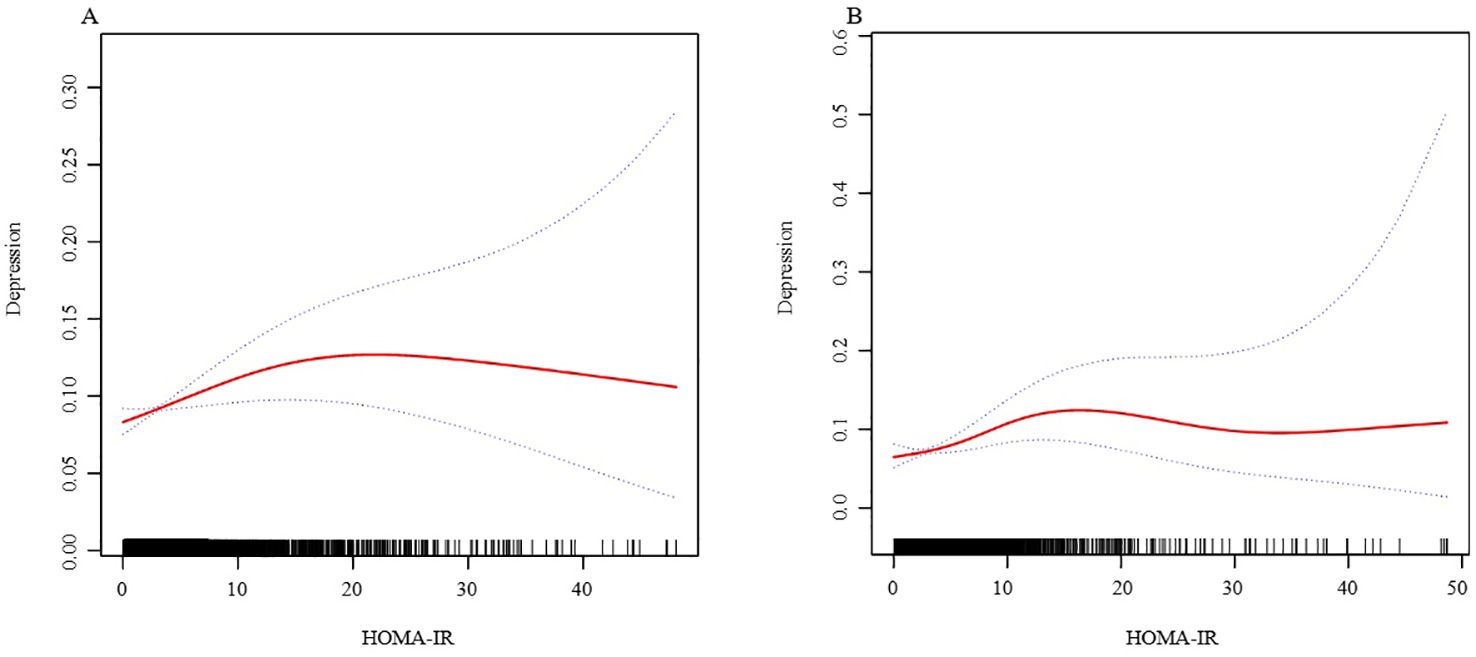
Figure 4. The association between HOMA-IR and depressive symptoms, analyzed with stratification by age. (A: age<=60; B: age>60). We adjusted for sex, BMI, hypertension, hyperlipidemia, family income to poverty ratio, education level, smoking status, marriage status, drinking status, physical activity, cardiovascular disease and diabetes. HOMA-IR, homeostasis model assessment of insulin resistance; BMI, body mass index.
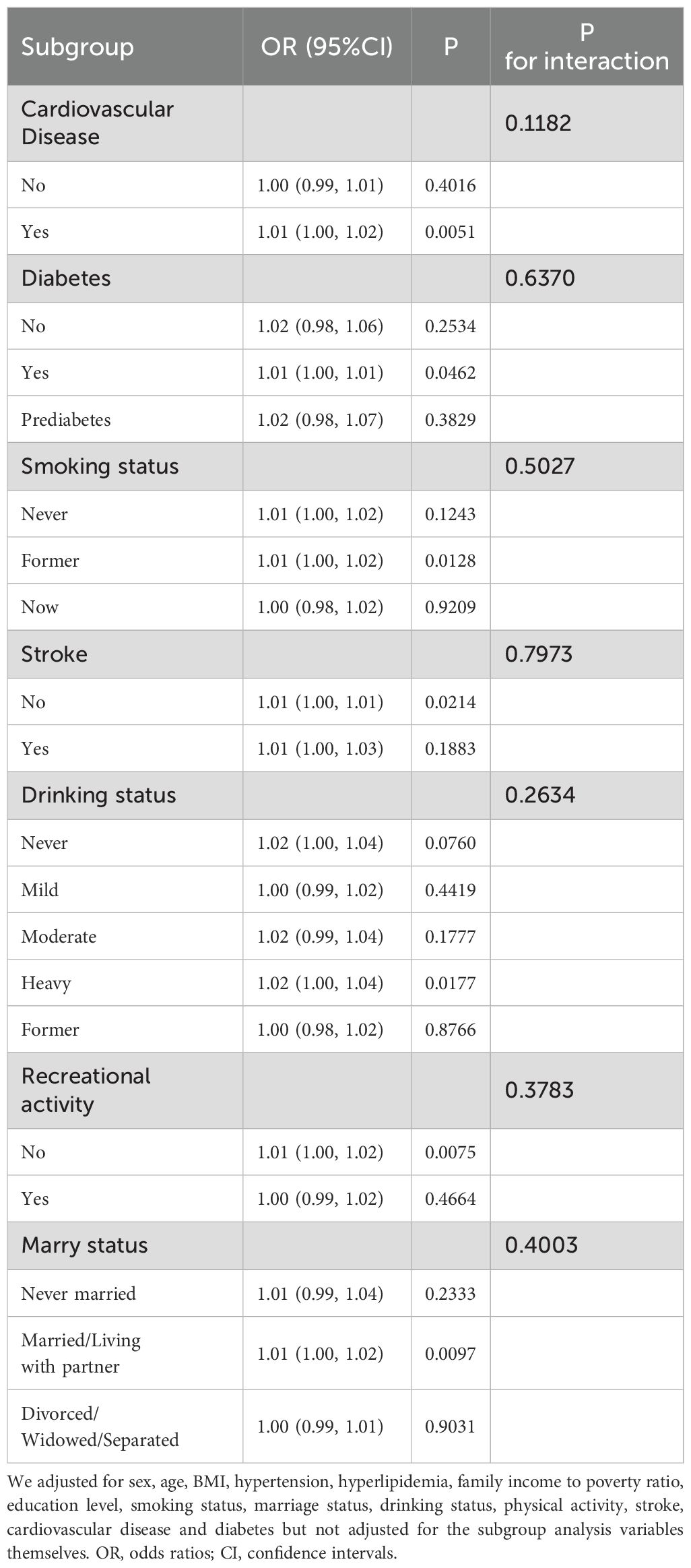
In subgroup analyses (Table 4), we found consistent interactions across all variables, suggesting a positive association between Depressive symptom and HOMA-IR in these subgroup analyses.
4 Discussion
In the research, after adjusting for all potential covariates, we observed a positive association between HOMA-IR and depressive symptom. With the increase in HOMA-IR, the incidence rate of depressive symptom also increased. Furthermore, upon conducting spline curve fitting, we discovered this positive correlation to be nonlinear, with a turning point at 10.47. Before this turning point, for every unit increase in HOMA-IR, the risk of depressive symptom increased by 5%. After the turning point, each unit increase in HOMA-IR was associated with a 1% decrease in depressive symptom risk, although this was not statistically significant. To our knowledge, this is the first large-scale study to explore the relationship between HOMA-IR levels and the odds of depressive symptom.
The relationship between HOMA-IR and depressive symptoms is a subject of debate, with studies presenting divergent findings. Consistent with our results, a study by Diniz BS et al. on Mexican-American elderly individuals discovered an association between depressive symptoms and insulin resistance (14). Similarly, research by He Y et al. demonstrated that the risk of IR escalates with increasing levels of depressive status among obese women (15). However, some studies have contradicted these findings. Geraets AFJ et al.’s research indicated that HOMA-IR is not associated with the risk of developing depressive symptoms (16). Landucci Bonifácio K et al. also arrived at a similar conclusion, stating that mood disorders, including major depression, are not linked to an increased risk of IR (17).
The pathogenesis of depression is complex, integrating genetic, neurobiological, and environmental factors. Recent research underscores the significance of inflammation, neurotransmitter dysfunction, and neuroendocrine disturbances in depression. Inflammation, marked by elevated levels of cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), has been directly associated with depression, suggesting an inflammatory component to the disorder (18, 19). Neuroendocrine dysregulation, particularly within the hypothalamic-pituitary-adrenal (HPA) axis, manifests in altered cortisol levels, further contributing to depression’s etiology (20, 21). Additionally, imbalances in neurotransmitters such as serotonin and dopamine are pivotal in mood regulation disturbances characteristic of depression (22, 23). Insulin exerts a direct influence on serotonergic and dopaminergic neurotransmission, and IR affects these neurotransmitter systems, thereby impacting depressive symptoms (24). Moreover, IR promotes the accumulation of fatty acids and triglycerides within cells, which triggers inflammation and raises the levels of pro-inflammatory cytokines, including TNF-α and IL-6 (25). Furthermore, IR increases the metabolic demands on individuals with mood disorders, potentially leading to more significant neurofunctional deficits and cognitive impairments, such as difficulties in verbal communication, numerical reasoning, and mental processing speed (26). According to Bruce S McEwen (27), the body may trigger compensatory biological responses when it is in a state of high insulin resistance and inflammation, regulating this adverse condition. This could be the reason for the existence of a saturation threshold between HOMA-IR and depression.
To better explore the underlying truths, we conducted subgroup analyses. In the stratified analysis by sex and age, we found no significant sex differences in the relationship between HOMA-IR and depression. However, an independent association was observed within the obese population. Upon performing stratified smooth curve fitting, we discovered that the relationships across sex and age groups were nonlinear. Furthermore, there was no significant interaction between HOMA-IR and other related risk factors, indicating that no additional factors were found to significantly influence the association between HOMA-IR and depression. Obesity is a significant risk factor for the development of insulin resistance. The excessive adipose tissue in obesity leads to chronic inflammation and the release of pro-inflammatory cytokines, thereby impairing insulin signaling and leading to insulin resistance (28). Concurrently, obesity-related inflammation is also associated with the development of depression. Pro-inflammatory cytokines can cross the blood-brain barrier, affecting brain function and leading to mood disorders (29, 30). Additionally, adipokines released by adipose tissue, such as leptin and adiponectin, play roles in both metabolic regulation and mood regulation. The dysregulation of these adipokines in obesity may contribute to the pathophysiology of both insulin resistance and depression (31, 32).
Our study presents several significant strengths that enhance the robustness and applicability of its conclusions. Firstly, the large volume of data collected has increased the reliability of our findings across diverse populations. Secondly, the strict standards applied during the data collection process ensure high data integrity and accuracy, substantially reducing the risk of biases that could distort the study’s outcomes. Despite these advantages, our research is not without its limitations. The temporal span of the data, while beneficial for capturing a broad range of information, may also introduce variability and systematic errors that could impact the observed associations. Relying solely on the PHQ-9 scale to assess depressive symptoms, our results may be susceptible to biases arising from patient self-reporting, such as misunderstandings or deliberate omissions. The inherent limitations of a cross-sectional study design restrict our ability to establish causal relationships between HOMA-IR levels and depression. Although we can observe associations between them, determining whether increased insulin resistance leads to depression, whether depression contributes to changes in insulin sensitivity, or if a bidirectional relationship exists, remains challenging.
5 Conclusion
Our study, analyzing NHANE database data from 2003 to 2020, discovered a non-linear positive correlation between HOMA-IR and depressive symptom in the US adult population, even after controlling for confounders. We identified a saturation threshold, indicating a limit to how insulin resistance impacts depressive symptom severity. This highlights the complex relationship between metabolic health and mental well-being, emphasizing the need for holistic approaches in managing both insulin resistance and depressive symptom. This research contributes to understanding the nuanced interactions between physical and mental health, advocating for integrated treatment strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CJ: Methodology, Project administration, Writing – original draft, Writing – review & editing. BW: Methodology, Project administration, Writing – original draft, Writing – review & editing. YQ: Data curation, Formal analysis, Visualization, Writing – review & editing. JW: Data curation, Methodology, Validation, Writing – review & editing. XZ: Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1393782/full#supplementary-material
References
1. Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. (2017) 317:1517. doi: 10.1001/jama.2017.3826
2. Penninx BW, Milaneschi Y, Lamers F, Vogelzangs N. Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Med. (2013) 11:129. doi: 10.1186/1741-7015-11-129
3. Vancampfort D, Correll CU, Galling B, Probst M, De Hert M, Ward PB, et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and largescale meta-analysis. World Psychiatry. (2016) 15:166–74. doi: 10.1002/wps.20309
4. Howard DM, Adams MJ, Clarke TK, Hafferty JD, Gibson J, Shirali M, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci. (2019) 22:343–52. doi: 10.1038/s41593-018-0326-7
5. Kendler KS, Gardner CO. Depressive vulnerability, stressful life events and episode onset of major depression: a longitudinal model. Psychol Med. (2016) 46:1865–74. doi: 10.1017/S0033291716000349
6. Liu RT, Hernandez EM, Trout ZM, Kleiman EM, Bozzay ML. Depression, social support, and long-term risk for coronary heart disease in a 13-year longitudinal epidemiological study. Psychiatry Res. (2017) 251:36–40. doi: 10.1016/j.psychres.2017.02.010
7. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. (1985) 28:412–9. doi: 10.1007/BF00280883
8. Webb M, Davies M, Ashra N, Bodicoat D, Brady E, Webb D, et al. The association between depressive symptoms and insulin resistance, inflammation and adiposity in men and women. PloS One. (2017) 12:e0187448. doi: 10.1371/journal.pone.0187448
9. Wu CY, Cogo-Moreira H, MacIntosh BJ, Edwards JD, Krance SH, Eid M, et al. Dynamic relationships between depressive symptoms and insulin resistance over 20 years of adulthood. Psychol Med. (2023) 53:1458–67. doi: 10.1017/S0033291721003032
10. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
11. Chambers DM, Ocariz JM, McGuirk MF, Blount BC. Impact of cigarette smoking on volatile organic compound (VOC) blood levels in the U.S. population: NHANES 2003–2004. Environ Int. (2011) 37:1321–8. doi: 10.1016/j.envint.2011.05.016
12. Xu C, Liang J, Xu S, Liu Q, Xu J, Gu A. Increased serum levels of aldehydes are associated with cardiovascular disease and cardiovascular risk factors in adults. J Hazard Mater. (2020) 400:123134. doi: 10.1016/j.jhazmat.2020.123134
13. Yang Y, Chen Y, Jia X, Huang X. Association of dietary flavonoid intake with the prevalence and all-cause mortality of depressive symptoms: Findings from analysis of NHANES. J Affect Disord. (2024) 366:44–58. doi: 10.1016/j.jad.2024.08.150
14. Diniz BS, Fisher-Hoch S, McCormick J. The association between insulin resistance, metabolic variables, and depressive symptoms in Mexican-American elderly: A population-based study. Int J Geriatr Psychiatry. (2018) 33:e294-e299. doi: 10.1002/gps.4792
15. He Y, Tong L, Guo F, Zhao S, Zhang J, Guo X, et al. Depression status and insulin resistance in adults with obesity: A cross-sectional study. J Psychosom Res. (2022) 163:111049. doi: 10.1016/j.jpsychores.2022.111049
16. Geraets AFJ, Köhler S, Muzambi R, Schalkwijk CG, Oenema A, Eussen SJPM, et al. The association of hyperglycaemia and insulin resistance with incident depressive symptoms over 4 years of follow-up: The Maastricht Study. Diabetologia. (2020) 63:2315–28. doi: 10.1007/s00125-020-05247-9
17. Landucci Bonifácio K, Sabbatini Barbosa D, Gastaldello Moreira E, de Farias CC, Higachi L, Camargo AEI, et al. Indices of insulin resistance and glucotoxicity are not associated with bipolar disorder or major depressive disorder, but are differently associated with inflammatory, oxidative and nitrosative biomarkers. J Affect Disord. (2017) 222:185–94. doi: 10.1016/j.jad.2017.07.010
18. Valkanova V, Ebmeier KP, Allan CL. CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. (2013) 150:736–44. doi: 10.1016/j.jad.2013.06.004
19. Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimäki M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav Immun. (2015) 49:206–15. doi: 10.1016/j.bbi.2015.06.001
20. Belvederi Murri M, Pariante C, Mondelli V, Masotti M, Atti AR, Mellacqua Z, et al. HPA axis and aging in depression: systematic review and meta-analysis. Psychoneuroendocrinology. (2014) 41:46–62. doi: 10.1016/j.psyneuen.2013.12.004
21. Stetler C, Miller GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med. (2011) 73:114–26. doi: 10.1097/PSY.0b013e31820ad12b
22. Ruhé HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry. (2007) 12:331–59. doi: 10.1038/sj.mp.4001949
23. Belujon P, Grace AA. Dopamine system dysregulation in major depressive disorders. Int J Neuropsychopharmacol. (2017) 20:1036–46. doi: 10.1093/ijnp/pyx056
24. Martin H, Bullich S, Martinat M, Chataigner M, Di Miceli M, Simon V, et al. Insulin modulates emotional behavior through a serotonin-dependent mechanism. Mol Psychiatry. (2024) 29(6):1610–19. doi: 10.1038/s41380-022-01812-3
25. Li M, Ji R, Liu X, Wu Y. Associations of metabolic syndrome and its components with sarcopenia, and the mediating role of insulin resistance: Findings from NHANES database. BMC Endocr Disord. (2024) 24:203. doi: 10.1186/s12902-024-01736-9
26. Brietzke E, Kapczinski F, Grassi-Oliveira R, Grande I, Vieta E, McIntyre RS. Insulin dysfunction and allostatic load in bipolar disorder. Expert Rev Neurother. (2011) 11:1017–28. doi: 10.1586/ern.10.185
27. McEwen BS. Neurobiological and systemic effects of chronic stress. Chronic Stress (Thousand Oaks). (2017) 1:2470547017692328. doi: 10.1177/2470547017692328
28. Gregor MF, Hotamisligil GS. Inflammatory mechanisms in obesity. Annu Rev Immunol. (2011) 29:415–45. doi: 10.1146/annurev-immunol-031210-101322
29. Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. (2009) 65:732–41. doi: 10.1016/j.biopsych.2008.11.029
30. Raison CL, Capuron L, Miller AH. Cytokines sing the blues: Inflammation and the pathogenesis of major depression. Trend Immunol. (2006) 27:24–31. doi: 10.1016/j.it.2005.11.006
31. Lu XY. The leptin hypothesis of depression: a potential link between mood disorders and obesity? Curr Opin Pharmacol. (2007) 7:648–52. doi: 10.1016/j.coph.2007.10.010
Keywords: non-linear, cross-sectional study, NHANES, depressive symptom, homeostasis model assessment of insulin resistance
Citation: Jiang C, Wang B, Qu Y, Wang J and Zhang X (2025) Nonlinear association between depressive symptoms and homeostasis model assessment of insulin resistance: a cross-sectional analysis in the American population. Front. Psychiatry 16:1393782. doi: 10.3389/fpsyt.2025.1393782
Received: 27 March 2024; Accepted: 06 January 2025;
Published: 22 January 2025.
Edited by:
Marcin Siwek, Jagiellonian University Medical College, PolandReviewed by:
Adrian Andrzej Chrobak, Jagiellonian University Medical College, PolandLianlian Du, Rush University Medical Center, United States
Copyright © 2025 Jiang, Wang, Qu, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Zhang, ZG9jdG9yemhhbmd4aW5AMTYzLmNvbQ==
†These authors share first authorship
 Chunqi Jiang
Chunqi Jiang Bo Wang
Bo Wang Yinuo Qu
Yinuo Qu Jun Wang1
Jun Wang1 Xin Zhang
Xin Zhang