- 1Centre for Youth Mental Health, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Parkville, VIC, Australia
- 2Orygen Youth Health, Parkville, VIC, Australia
Background: Since the mid-20th century, mental illness has become a leading cause of health burden, particularly among adolescents and emerging adults, with most disorders emerging before the age of 25. Over the past two decades, mental ill health has surged to alarming levels, with evidence confirming that the increase is not just due to better awareness or diagnosis but reflects a genuine public health crisis.
Study design/method: We explore the evolving landscape of youth mental health and its contributing factors, including family dynamics, educational pressures, climate change, social media, and socio-economic challenges, potentially linked to neoliberal policies. A narrative review methodology was employed to analyze these factors and their role in the trends of mental ill-health among young people.
Study results: We document mental health trends since the mid-1990s, focusing on mental and substance use disorders among young people and their current needs. Potential new explanatory factors and megatrends, potentially flowing from a paradigm shift in the global political economy which has largely passed under the radar, yet which has produced fragmentation and inequality, are identified, with the COVID-19 pandemic further intensifying these trends. We discuss methodologies to estimate the contribution of these megatrends and outline potential barriers to implementation, along with strategies to overcome them.
Conclusion: This review calls for a comprehensive global action plan, emphasizing prevention, early intervention, and improved treatment strategies. In addition to strengthening prevention, which may take time and be elusive, immediate action is needed to innovate and expand services, which are currently under-resourced and overwhelmed.
1 Introduction
1.1 The youth mental health landscape and time trends over the past 30 years
This review is anchored in Rutter and Smith (1)’s seminal monograph, which highlighted an increasing prevalence of youth psychosocial disorders since the mid-20th century. The authors examined the extended transition period from puberty to mature adulthood in the mid-twenties and explored various candidate variables to explain the rising prevalence. Despite their extensive analysis, they found it challenging to draw definitive conclusions. Ultimately, they attributed the trend more to increasing family discord and heightened expectations, particularly related to employment than to other potential factors such as mass media, migration, social disadvantages, unemployment, poor physical health, and declining moral values.
However, the trend of mental health prevenance and burden depends on many factors, e.g., geographical region, socio-demographic status of the region, gender and age group as well as how the prevenance and burden are measured. For example, according to the 2021 Global Burden of Disease Study (2), the prevalence of mental disorders remained relatively stable or decreasing in most countries except for young people 10-19 years in high and high-middle Socio-Demographic Index (SDI) countries prior to the COVID-19 pandemic, which resulted in increases in all age groups across all SDI categories, see Figure 1A. However, the percentage of the total burden attributable to mental disorders, see Figure 1B or mental disorders, self-harm and substance use combined, see Figure 1C increases gradually among those aged 10-34 across most of the SDI categories highlighting the substantial contribution of mental health disorders and self-harm to overall health loss in these populations.
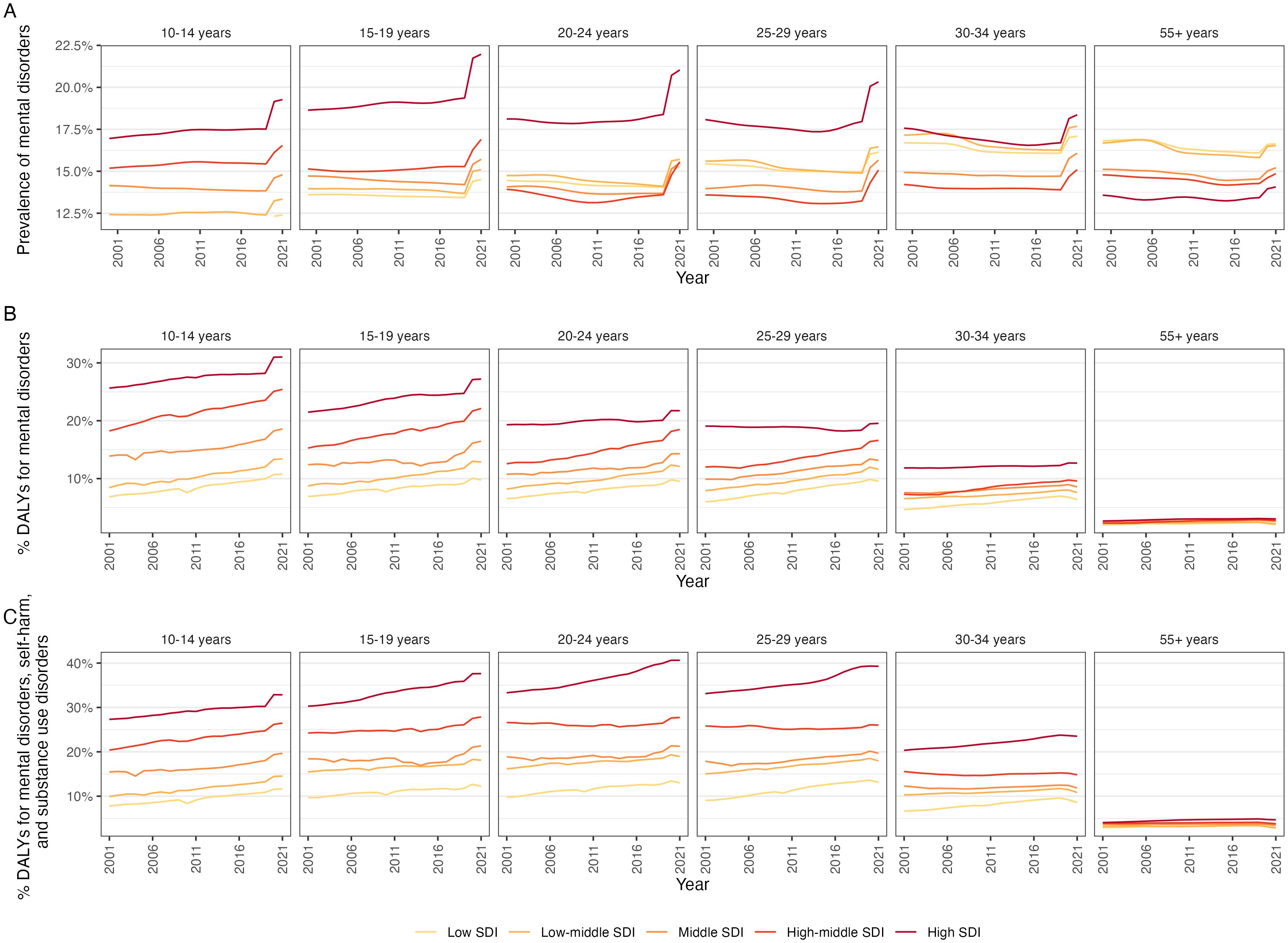
Figure 1. Trends of the burden of mental disorders by age group, country Socio-Demographic Index (SDI) estimated from Global Burden of Disease Study 2021 (2) (A) Prevalence of mental disorders; and (B) Percentage Disability-adjusted life year (DALYs) attributable to mental disorders, (C) Percentage DALYs attributable to mental disorders, self-harm and substance use disorders.
While depression and anxiety can impact people of all ages (3–5), youth aged 10–24 are at a higher risk of experiencing these and other mental disorders (6–9). The pathway to emerging adulthood, from early adolescence to young adulthood, is a time of significant biological, social and personal change that has evolved over generations (10). This period is marked by major life milestones and transitions that coincide with the peak onset of mental disorders (11). Lost productivity at this life stage due to mental illness poses a significant psychosocial and economic burden (12). The imperative to address the mental health needs of young people has been recognised and significant reforms have commenced in some high-income countries to improve mental health service provision for this population (13, 14). These efforts are modest and insufficient in proportion to the scale of need and rapidly rising rates of youth mental ill-health that have been exacerbated by the COVID-19 pandemic (15).Until recently, the evidence for a further increase in youth mental ill-health since the mid-1990s was mixed (16, 17); however, there are increasing indications that this rise is real and alarming in scale (18, 19). Australia’s national survey of mental health recently found that the 12-month prevalence of mental disorders (i.e., anxiety, affective and substance use disorders) among young people had increased by 50% over the past 15 years, disproportionately affecting females (20). The prevalence of depression among young adults in Australia has more than doubled over the past 14 years, according to data from the 2007 and 2020–21 National Survey of Mental Health and Wellbeing (21). The 12-month prevalence of affective disorders, including major depressive disorder, dysthymia, and bipolar disorder, increased significantly from 6.3% to 13.6% among those aged 16–24, and from 7.9% to 11.0% among those aged 25–34, between 2007 and 2020–21 (21). However, according to Liu et al. (22)’ s secondary data analysis of the 2019 Global Burden of Disease study, the annual incidence of anxiety disorders in children and adolescents (10-19 years) decreased by 2.2% from 1990 to 2019, a trend observed primarily before COVID-19 and largely driven by reductions in middle- to low-income countries. There were significant variations in the age-standardised incidence rate (ASIR) and trends among countries. Despite a global decrease in adolescent anxiety disorders over the past 30 years, developed countries continue to see a steady increase in both incidence and disease burden. For example, Portugal had the highest ASIR, while Mexico saw the largest increase. In 2019, Portugal reported the highest number of DALYs (1001.71 million) followed by Ireland (897.80) and Iran (873.64), and India the lowest (212.09 million) (22). Regarding eating disorders among young people, referrals to child and adolescent services in the UK have nearly doubled (23).
Mechanisms underlying this surge remain poorly understood; however, it is likely influenced by a broad range of social and economic changes or “megatrends” (e.g., increasing financial insecurity, family life, educational experiences, and rising health and social inequality) (24). In this review, we focus on the transitional life stage of youth (adolescence and young adulthood). We examine mental health trends relevant to anxiety, depression, psychological distress and wellbeing since the mid-1990s and explore potential explanatory factors associated with prevalence changes.
2 Methods
A literature search using Medline (1946), PsycINFO (806) and Embase (1947) was conducted from inception to May 2023. The search strategy included subject headings and free text terms: (anxiety OR depression OR mental disorders OR mental health OR mental illness OR psychiatric disorders OR psychopathology) AND (youth OR young people OR young person OR young adult OR adolescence OR teenage) AND (epidemiology OR prevalence OR time trends). A new search was carried in June 2024 to include new publications: Medline (262), PsycINFO (175) and Embase (281). This search strategy included the aforementioned terms as well as additional terms such as psychosis, eating disorder, and bipolar disorder. Both the search strategies were combined with additional search terms for various sections of this review: causal explanation, determinants, economy, inequality, politics, political leadership, climate change, terrorism, urbanization, globalization, education, employment, unemployment, labour market, structural change, social change, social media, internet, technology, society, trauma, victimization, development, individualism, materialism, expectations, family, culture, COVID, COVID-19, 2019-nCoV, SARS-CoV-2, coronavirus, and corona virus. Searches were augmented by Google Scholar, reviewing the reference lists of relevant studies, and by seminal publications known to the authors.
Primary or secondary studies were selected if they included young people aged 12–25 years and examined trends relevant to anxiety and depression, psychosis, suicidal behaviours/thoughts, eating disorders (ED), Schizophrenia and mood disorders, with at least one time point after 1995 (i.e., following the publication of Rutter and Smith’s monograph). These included studies reporting trends in relation to psychological distress, psychological wellbeing, and somatic, internalising and emotional symptoms. Studies using administrative or health service data were excluded. Two reviewers selected articles identified from the database searches, with one reviewer covering the period from inception to May 2023 and the other from May 2023 to June 2024. Results were summarised according to trends in youth mental health and potential explanatory factors associated with prevalence changes. The percentage of increase or decrease in prevalence is reported when these data were available.
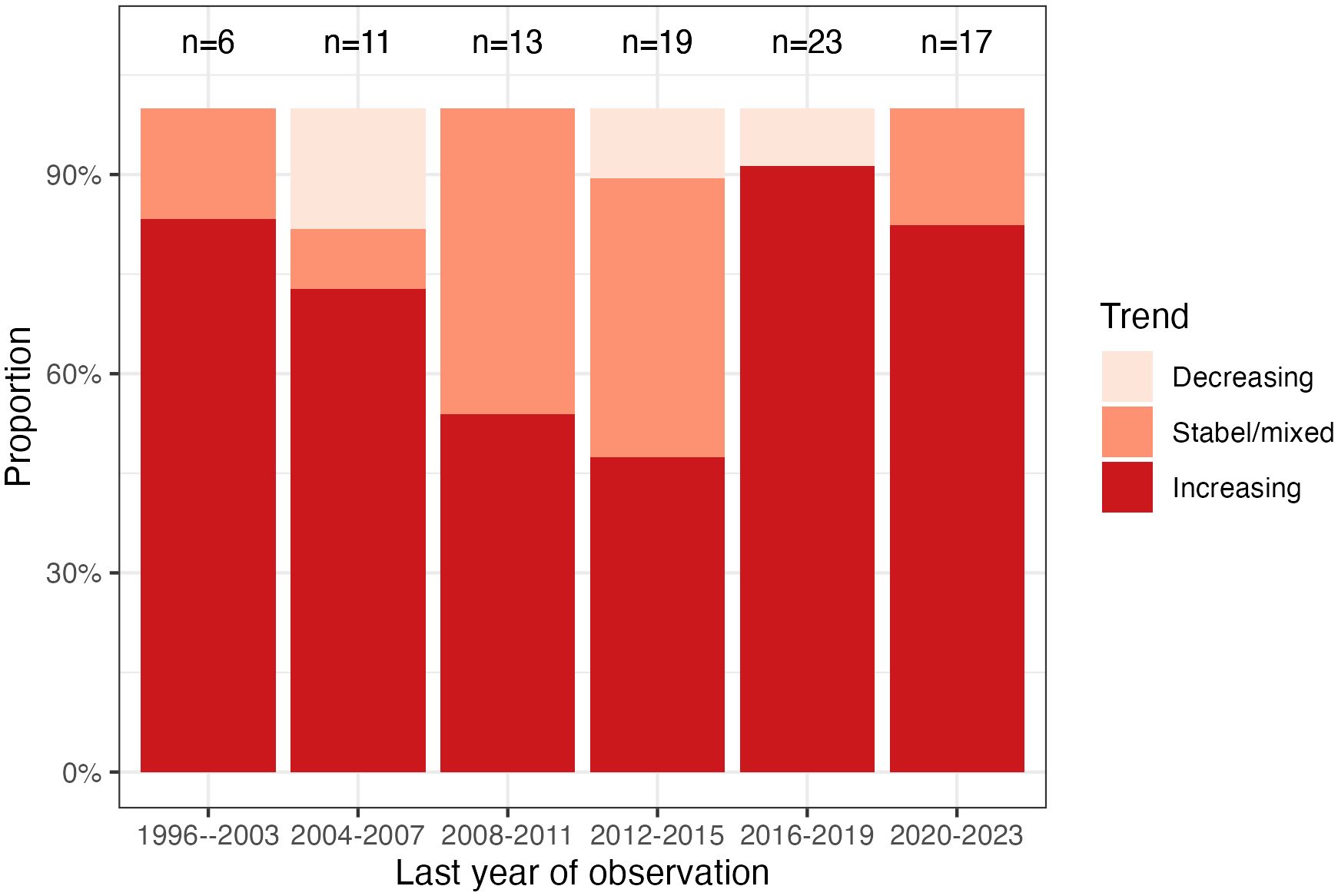
The searches up to May 2023 returned a combined total of 12,047 results after duplicates were removed. Of the 177 full-text papers retrieved, 72 met the criteria for inclusion and were included. The new search strategy yielded a combined total of 373 after duplicates were removed. Out of 122 full-text papers retrieved, 11 met the inclusion criteria, bringing the total number of included studies to 83. Six additional studies were identified following the database searches, thus a total of 89 studies. The characteristics and findings of the studies are shown in Supplementary Table S1 (See Supplementary File). A time-trends graph of overall youth mental health disorders was created using the most recent year of observation in the studies reviewed in this paper. Youth mental health trends were categorized as increasing, stable/mixed (e.g., diverging trends for different disorders/symptoms), or decreasing. Due to small sample sizes, it was not possible to further subdivide the data by disorder or by year.
3 Results
3.1 Youth mental health trends
Of the 89 studies included, 33% (n=29) were based in Europe, 29% (n=26) in North America, 13% (n=12) in the UK, 7% (n=6) in Australia, 6% (n=5) in Asia, 2% (n=2) in New Zealand, 1% (n=1) in each of South America, and Iran, and 7% (n=6) were multinational. Only 4% (n=4) were undertaken with populations from low- and middle-income countries. 79 (89%) were primary studies, of which 60 (76%) were nationally or geographically representative.
Most studies (80%, n=71) reported an increase in at least one outcome related to anxiety, depression, psychological distress, wellbeing or emotional, internalising or somatic symptoms, psychosis, suicidal behaviours/thoughts, eating disorders (ED), Schizophrenia and mood disorders (Supplementary Table S1). The remaining studies reported a decreasing trend (7%, n=6) or no increase (13%, n=12). Trends according to type of mental health problem suggest rising rates of anxiety (15/18 studies), depression (26/37 studies), emotional or internalising problems (20/27 studies), somatic symptoms (8/9 studies), psychological distress (9/14 studies), low mental wellbeing (7/9 studies), suicidal behaviours/thoughts (3/3 studies), Psychosis (1/2 studies), ED (1/1 studies), and Schizophrenia and mood disorders (1/1 studies) (Supplementary Table S1). Methodological differences between studies (e.g., outcome measures, sampling method and sample characteristics) are a probable explanation for the variation in trends.
The degree of increase varied within and across nations. The proportion of young people experiencing anxiety increased by 29–84% in the US (25, 26), 77–164% in Sweden (27, 28), 105% in Australia (20, 29), and 115% in Canada (30). Severe anxiety increased by 86% in the US (31) and high levels of anxiety doubled in Iceland (32). For depressive symptoms or disorder, the percentage of increase was 8%–119% in the US (33–42) and 87% in Australia (43). Severe depression rose by 145% in the US (31), while the change was modest in Finland (+18%) (44). The proportion of young people with emotional or internalising problems increased by 25–79% in the Netherlands and Nordic countries (45–48), 43% in Canada (49), 48% in New Zealand (50), 55–61% in the UK (51, 52), and 10%-64% in Poland (53, 54). For psychological distress, the percentage of increase was modest to large: 43–135% in the UK (55–58), 12–70% in the US (33, 37), and 7%-47% in Ethiopia (59). In the UK, severe psychological distress tripled (58). Somatic symptoms increased by 25–54% in the Netherlands (45, 48), while low wellbeing rose by 119% in the US (31) and 118% in Denmark (60). Rates of suicide increased from 3.6- 7.1 (per 100, 000) in Asian American and Pacific Islander (AAPI) youth in the US (61), ED increased by 5% per month from 2017-2021 (62), and Schizophrenia and mood disorders increased by 4% per month (62).
There are indications that trends have risen since 2011–2016 for psychological distress, low mental wellbeing, and depressive and anxiety symptoms (6, 31, 32, 34, 39, 41, 42, 58, 63–67). Since 2020/the COVID-19 pandemic, rates of psychological distress, anxiety and depressive symptoms have increased further, and mental wellbeing has worsened (56–58, 60, 68–70).
Increasing trends were not observed in Canada, New Zealand, England, China, Netherlands, and Chile for depression; Belgium and Japan for psychological distress; Poland for somatic symptoms; the UK for low wellbeing; and Scotland, Switzerland and Iran for internalising symptoms. However, for each of these locations (except the UK and Canada), only one study was available for the corresponding outcome. Where declining trends were reported, the percentage of decrease was 22% for depression (71) and 6–29% for distress (72, 73).
Trends in relation to gender suggest greater increases among females for anxiety, depression, distress, emotional problems, psychosis, and internalising symptoms (31, 34, 37, 39, 63, 74–78). However, some studies have reported increases for both genders in relation to anxiety, depression and emotional problems (28, 38, 49, 51, 54, 77, 79, 80) or higher increase for males for psychological distress (81), and low mental wellbeing (82). These discrepancies across similar outcomes likely reflect methodological heterogeneity, particularly in terms of outcome measure, which varied across studies. Also, outcomes of this review may not have detected non-specific symptoms (e.g., irritability, anger, and risk-taking) that may represent gender-specific markers of distress in young men (83).
Figure 2 illustrates the trends in youth mental health disorders from 1996 to 2023 (the most recent years of observation in the studies reviewed). The figure shows a declining trend from 1996 to 2015, followed by an increase starting in 2016. The effect of the COVID-19 pandemic (2020-2022) is unclear from this figure at least, and it appears that the increase from 2016 is difficult to explain on that basis.
3.2 The social, economic, and commercial determinants of mental health
Social determinants of mental health refer to the structural conditions individuals are exposed to throughout their lives, from conception to death (86). These conditions affect mental health outcomes and contribute to disparities within and between populations. Key factors include income, employment, socioeconomic status, education, food security, housing, social support, discrimination, childhood adversity, neighbourhood conditions, and access to affordable health care (87–89). The likelihood of encountering protective or harmful social determinants is influenced by the distribution of money, power, and resources at global, national, and local levels, shaped by policy choices (86).
The impact of mental health issues is particularly evident among young people. Young people have high rates of self-harm, and suicide is a leading cause of death among them (90, 91). Poor mental health is closely linked to other significant health and developmental concerns, such as educational achievements, substance use and abuse, violence, and reproductive and sexual health (37). Poor mental health can hinder life chances, impacting both lifespan and quality of life. Therefore, improving young people’s mental health by addressing modifiable social risk factors through effective prevention strategies is a critical social justice issue.
Commercial determinants of health, a relatively new area of study, highlight how corporate actions, conditions, and omissions significantly impact health (92). Young people are especially vulnerable to advertisements and celebrity endorsements. For example, marketing electronic nicotine delivery systems and cannabis to young people can activate sensitive and developing pathways in their brains (93). On the positive side, the private sector can enhance public health by providing living wages, paid parental leave, sick leave, and health insurance, all of which contribute to better health outcomes (93). However, as highlighted by critics like Pennington (94) and Monbiot (95), in the context of neoliberal political and economic settings, with minimal regulatory safeguards and weakened central government, the private sector now falls increasingly short in delivering these benefits equitably, leading to rising inequality and growing disparities in health outcomes.
A range of social, environmental, and commercial factors influence the collective life experiences and mental health of young people and their families (93, 96, 97). Ensuring that young people have a healthy environment where they can grow, participate actively in their communities, and pursue goals that honour their uniqueness and dignity is essential (98). However, this is a complex challenge, as meeting basic needs such as safety, education, financial stability, healthy caregivers, and positive life experiences is fundamental to building health and resilience (99, 100).
3.2.1 Dynamic new megatrends
The identification of mechanisms underlying trends in youth mental health is an emerging area of research. Most studies to date have examined correlation rather than causation. An exploratory review of potential proximal and distal factors associated with trends is provided in the following sections. Proximal factors reflect those within the young person’s immediate environment: developmental changes, family, education, health and lifestyle, social media, childhood trauma, and bullying (86, 98). Distal factors reflect broader societal contexts, which are often related to and mediated by proximal factors: economy, socio-economic disadvantage and inequality, politics, and climate change (86, 101). This review considers the influence of both proximal and distal factors, largely related to Western and high-income countries, structuring the discussion based on Kirkbride (86)’s framework of social determinants. This framework includes individual-level social determinants (i.e. proximal) and broader environmental determinants (i.e. distal).
3.2.1.1 Individual level social determinants
3.2.1.1.1 Developmental trends
This section explores developmental trends that influence youth mental health, including factors such as family environment, education, health and lifestyle, experiences of abuse or neglect, bullying and cyberbullying, and the role of social media.
3.2.1.1.2 Family environment
With respect to family structure, while there has been an increase in the proportion of young people not living with both biological parents, this has not been associated with increasing rates of psychological distress (72, 102), depressive symptoms or disorder (43, 79), and emotional problems (76). On the other hand, it may have retarded the maturational process of attaining independent identity and adult status. Parent-adolescent arguments have been found to explain a large proportion of the rise in self-reported adolescent psychological distress, although reverse causality could not be eliminated and the survey items used to measure arguments differed at the two time points (102). Based on two large national surveys using identical measures of adolescent and parent emotional problems over a 20-year period, increases in maternal emotional problems were found to modestly contribute to increasing rates of adolescent emotional problems (103). This was based on three key findings: maternal and adolescent emotional problems increasing at the same time; parental emotional problems prospectively predicting offspring emotional problems, beyond reverse causation and influences of shared adversity; and cohort differences in adolescent emotional problems were attenuated when controlling for trends in parental emotional problems. Armitage et al. (104) posits that these trends in family structure have not significantly impacted trends in youth mental health, as similar increases in adolescent emotional problems are observed across different family structures (103, 105, 106). While they may not account for the rise, family environment and structure are still an important influence, and equally, efforts to alleviate childhood poverty, food insecurity, and family homelessness are critical for addressing these social determinants of mental health among young people.
3.2.1.1.3 Education
Educational reforms in the UK and many other countries have led to increased grading and testing, which significantly contributes to student anxiety and stress (104). Studies report rising school-related stress, academic pressure, and burnout among adolescents, with notable variation across countries (107–111). Female adolescents are particularly affected, showing increased worry about academic performance, contributing to a widening gender gap around 50% for internalising problems (102, 112). Studies that have compared trends between students and non-students indicate variation across countries and genders. A meta-analysis across 57 nations found an overall increase in anxiety among both students and non-students between 1970 and 2010; however, when analysed according to country (US, Australia, UK, Canada), only students in the US showed a significant increase (113). Recent data from England (2000–2014) suggest that only female students have shown increases in common mental disorders, although the sample was relatively small (114). There is little experimental evidence as to why rates have increased among some students, particularly females. Hypotheses include rising tuition fees, student debt (113, 114) and increasing educational expectations or pressures that have impacted females (75, 108, 115), which when combined with other stressors (e.g., concerns about personal identity), has led to an accumulation of risk factors for mental ill-health (115). While these trends indicate increased anxiety and mental health issues among students, particularly females, the evidence is complex and varies across countries, necessitating further research to unravel the underlying causes, causal sequence, and implications.
3.2.1.1.4 Health and lifestyle
Indicators of health that are commonly associated with mental ill-health have similarly declined; however, their impact on youth mental health trends is unclear. The vaping epidemic exemplifies how social factors impact substance use, with electronic nicotine delivery systems (ENDS) popular among youth due to targeted marketing and social media influence (116, 117). Youth with mental illness may use ENDS to manage symptoms or medication side effects, contributing to conditions like depression, ADHD, and conduct disorder (93). Sleep disturbances have risen, which has been linked to electronic device usage (118). Physical activity has declined, especially since the COVID-19 pandemic (119). While obesity rates have risen, this has not been associated with increasing rates of distress (102). There has been a notable increase in the percentage of females in the clinical range for mental health and substance use among Finnish young people (120). The effect of urbanisation on anxiety and depression trends is mixed and limited by differences in measures of urbanisation and the conflation other outcomes (e.g., conduct disorders) (49, 53).
In contrast, several studies have found that some lifestyle trends have positively improved for adolescents, with signs of decreasing alcohol consumption, illicit drug use, and risky behaviour (47, 121–125). While alcohol use has declined among Generation Z, there has been a rise in the use of substances such as cannabis, which is now more potent and readily available (126, 127). An increase in depressive symptoms in Norway was partly attributed to increases in cannabis use and disordered eating (79).
3.2.1.1.5 Abuse or neglect experiences
At present there are no direct links between population changes in youth mental health and exposure to violence, abuse and neglect. While childhood maltreatment is common and remains a major public health concern, stable (128) and, in some instances, decreasing trends in exposure to violence and abuse (122, 129–131) cautiously indicate that these factors may not be likely candidates to account for the rise in prevalence of disorders. However, this requires robust investigation across the various types of maltreatment as increases in emotional abuse and neglect have been reported (132).
3.2.1.1.6 Bullying and cyberbullying
Studies indicate that the impact of being bullied surpasses the effects of other childhood adversities and adult abuse (133, 134). While bullying victimisation has shown a downward trend in most European countries (135, 136), increasing trends have been observed in the UK (135, 137). In Scotland, increasing rates of victimisation have been linked to a decline in the mental wellbeing of adolescents (137). While cyberbullying victimization has remained stable (136) or increased among adolescents (138–140), it has negatively impacted mental health. This suggests that both bullying and cyberbullying victimization are indicators of comorbid mental health problems (136). Conversely, a rise in cyberbullying in 2020 occurred in the absence of increasing anxiety and depressive symptoms (141). According to Patchin and Hinduj (142), the proportion of individuals who have experienced cyberbullying at some point in their lives has more than doubled over the years. Protecting youth from bullying and its detrimental effects is crucial, necessitating safe, respectful, and inclusive school environments that do not tolerate such behaviour.
3.2.1.1.7 Digital media/social media
The digital world offers youth avenues for connection, creativity, and support, but also carries significant risks. Smartphone usage may contribute to sleep deprivation (143), and social media addiction may further exacerbate mental health issues among young people (144). While evidence suggests a longitudinal association between social media and mental health in young people, the magnitude is likely to be small and the nature of this association is uncertain owing to bidirectional effects and the range of mediating factors (145–149). With these considerations, recent studies have suggested a link between increased social media/electronic device usage and both a decrease in psychological wellbeing and increase in depressive symptoms, occurring between 2011/2012 and 2015/2016 (63, 64). This was based on two criteria: social media/electronic device usage being correlated with higher depressive symptoms/lower wellbeing and usage significantly increasing simultaneously with depression/low wellbeing. These findings are limited by the broad categories used to measure usage (e.g., ‘almost every day’), which do not capture the variance in this variable given that the majority of young people use social media daily (150). Other studies using the same surveys analysed by Twenge et al. indicate a small correlation between social media usage and both depressive symptoms and wellbeing (150–152) and that social media explained only 4% of the increase in depressive symptoms (150). Furthermore, between 2009 and 2017, the association between social media usage and depressive symptoms was found to be weak and confined to only 2009–2010 (152).
3.2.1.2 Wider social environmental determinants
3.2.1.2.1 Economic trends
This section explores economic trends, including the labour and housing markets, socio-economic disadvantage and inequality, climate change, and political factors, all of which impact youth mental health.
3.2.1.2.2 Labour market/unemployment
The impacts of the 2008 global financial crisis on young people were substantial and included insecure employment and income (153–157). These trends have relevance to the COVID-19 pandemic (see below). In Southern Europe, cross-sectional repeated surveys spanning before and after the 2008 recession showed that symptoms of anxiety and depression increased among students (potentially due to limited employment prospects) (158) and that these symptoms among young people have become more strongly associated with insecure employment (e.g., fixed term contracts) following the recession (159). Across the working-age population, young Australians (15–24 years) have shown the largest decrease in mental health and wellbeing and increase in high/very high symptoms of psychological distress since 2010 (160). This coincided with an increase in insecure employment, inadequacy of pay, and the casualisation of the youth labour force.
In the US, no association was found between rising adolescent depressive symptoms and the overall unemployment rate immediately after the 2008 recession (63). However, when labour market trends have been measured specifically in relation to young people, an association has been found between increases in the proportion of young people not in the workforce and increases in mental health symptoms among adolescents (feeling low, headache and sleep difficulties) between 1983 and 2005 (161). This lends some support to the finding that proximal (i.e., adolescents’ worry about family finances) rather than societal level factors (i.e., overall municipality unemployment rate) are more strongly associated with increasing psychosomatic symptoms among adolescents during a period of economic downturn in Sweden (5). However, the direction of causality remains unclear. As somewhat expected, little evidence was found to support the role of economic variables (e.g., no working parent, worry about unemployment) in explaining increases in psychological distress in Scottish adolescents during a period of reduced economic hardship (102). Moreover, the pandemic seemed to have affected school engagement among young people. For instance, symptoms of anxiety decreased from pre-pandemic levels to during the first UK lockdown but increased upon the return to school for 13-14-year-olds (162). These findings underscore the complex and context-dependent relationship between economic instability, insecurity of work, youth mental health, and factors like school engagement during the pandemic, highlighting how both direct experiences of economic hardship and broader economic conditions can variably impact mental health outcomes.
3.2.1.2.3 Housing market
Housing market and economic trends have contributed to a generation of young people who frequently face residing with parents for longer or living in unaffordable and insecure rentals (154). Economic downturns negatively impact young people’s mental health, with effects comparable across different economic indicators like unemployment rates and housing prices (163). Golberstein et al. (163), found that a decline in unemployment rates (2001-2013) in the US is associated with a reduction in the severity of mental health problems in children and adolescents (4-17 years), similar to the impact on adult health outcomes. Conversely, a five-percentage point increase in unemployment during the Great Recession was linked to a 35% to 50% increase in clinically significant mental health issues among these age groups (163). Home-ownership rates among young adults have decreased (154, 164) amid stagnant wages, unstable employment conditions and dramatically increasing house prices (165). This has negatively impacted the mental health of adult renters (166). Young people who rent fear that housing security and wealth are unattainable and have reported feeling anxious, depressed and stressed due to insecure, expensive and poor-quality housing, and rising rental costs have added to this precarious situation for many (167).
3.2.1.2.4 Socio-economic disadvantage and inequality
Socio-economic and intergenerational inequalities have been increasing since the 1990s in most high-income countries (168, 169). Today’s young people are not only struggling more than older generations, but they are also worse off compared to previous generations at the same age and are expected to face greater challenges as seniors than the current over-65s (170). A global study by (171), using data between 2009-2022, has shown that relative inequality in youth wellbeing has worsened, with emotional distress and life satisfaction becoming increasingly unequal between socioeconomic groups. This suggests that growing income disparities are intensifying relative inequality across generations, leaving today’s youth more disadvantaged compared to previous generations (171). In the UK, a comparison of three nationally representative cohorts with comparable data revealed a widening disparity in emotional problems according to level of family income, with a fourfold increase for adolescents in the lowest income group between 1974 and 1999/2004 (172). This was partially accounted for by the increasing impact of socio-economic adversity (e.g., insecure housing tenure), mediated by adolescents’ proximal family environment. Increasing social inequalities have similarly been observed in relation to rising rates of depression in Finland and the US (6, 44). In Japan, a nation with higher levels of equality than most others, psychological distress among adolescents decreased significantly from 10.7% to 7.6% between 2007 and 2013 (72). However, the patterns of psychological distress relative to socioeconomic status remained consistent throughout the study period. Adolescents in both lower-income and higher-income households reported more psychological distress compared to those in middle-income households. Conversely, findings from Denmark indicate that the largest increases in emotional symptoms have occurred in high and middle socio-economic classes (46); however, a substantial proportion of cases with emotional problems had missing socio-economic status data, which may have skewed findings. Data from the US suggest increasing rates of major depressive episode in adolescents between 2005 and 2017 across all income levels, although inequalities remained as those in the lowest income group experienced higher annual rates of major depressive episode than the highest income group (37).
The COVID-19 pandemic and its associated economic crisis have exacerbated inequality among vulnerable and disadvantaged groups, including young people (173). During the pandemic, young people have experienced increased rates of educational disruption, unemployment or precarious employment, financial insecurity, and housing stress (173, 174). Young people of lower socio-economic status have experienced greater economic hardship (174). This amplification of socio-economic determinants of mental health and of inequality has likely contributed to an increase in anxiety and depression that has disproportionately affected young people (15, 68, 174–176).
3.2.1.2.5 Climate change
There is increasing evidence of climate change impacts on young people’s mental health who are a priority population group in the context of climate change. These include anxiety, sadness, grief, hopelessness, powerlessness, depression, and existential worries about the future (177–180). A range of factors including government inaction on climate change, social media exposure, and social challenges such as housing instability, food insecurity, and increased conflict influence this relationship between climate change and young people’s mental health (177, 178, 181–183).
According to Sciberras & Fernando (184)’s eight-year longitudinal study which focused on climate change worry among Australian adolescents found that adolescents with high levels of worry related to climate change that are persistent over time showed higher rates of depressive symptoms in late adolescence than adolescents with moderate levels of climate change related worry. Although 50% of young people have experienced a negative emotional response to climate change (185), a causal relationship and time trends between climate-related negative emotions and mental ill-health in young people has yet to be fully established (186). There has been one study that looked at the causal relationship between climate change and mental health. Patrick et al. (183)’s systems dynamics study developed a systems map highlighting the relationships between causal factors (e.g. under theme areas of government, services and structures, personal experience of environmental disasters, and social norms, communication and taking action). While the nature of causal relationships requires further investigation, higher temperatures have been associated with increased suicide rates (187) and lower mental wellbeing (188).
3.2.1.2.6 Politics
Although anxiety surrounding political elections and decision-making is not a recent phenomenon, there is concern about the impact of recent and current political landscapes (189). Both immediate and potential future negative effects on youth mental health have been observed. This includes increased stress and anxiety during the 2016 presidential election in America (190, 191); increasing concern in the UK because of the Brexit vote and its uncertain consequences, particularly on employment and education (192); and social unrest in Hong Kong that has been independently associated with depressive symptoms (193). Gimbrone et al. (194)’s study (2005-2018) highlights a growing mental health disparity (e.g. depressive symptoms) among adolescents based on their political beliefs. The findings suggest that the ideological perspectives through which adolescents interpret the political climate can have varying impacts on their mental well-being.
4 Discussion
The findings of this review indicate a substantial rise in youth mental health issues including anxiety, psychological distress, self-harm, suicide, and depressive symptoms, contributing to a global youth mental health crisis as highlighted by a recent Lancet Commission on youth mental health (14). The magnitude of change varied within and across nations and was not observed in some studies. However, in others, it was substantial, with the percentage of increase as high as 164% for anxiety, 135% for psychological distress (increasing to 242% for severe distress), and 119% for both depression and low wellbeing (increasing to 145% for severe depression). An important consideration is whether increasing trends reflect a real population change or are an artefact arising from reduced stigma, improved mental health awareness, greater willingness to disclose mental health issues, a widening of diagnostic thresholds, and population growth (195–197). These factors might contribute to an inflation of prevalence rates by capturing individuals with transient distress that does not necessarily require clinical intervention (198). Additionally, the role of cultural and societal shifts, such as the influence of digital media and the pressures of modern life, may contribute to these trends, making it essential to consider both the real and perceived changes in mental health across generations (199). However, these factors contributing to increasing trends in youth mental health remain unclear and individually only explain a small proportion of the increasing trend and the interpretation of findings and causal inferences are limited by methodological constraints (e.g., unmeasured cofounders or co-occurring social changes, lack of harmonised measures across studies and, in some instances, timepoints) as identified in the review. Although potential shifts in respondent reporting and diagnostic approaches have been difficult to unequivocally refute, Twenge et al. (200) found that increases in psychopathology were not explained by a greater willingness to report mental health problems after controlling for socially acceptable and defensive responding. Further validation of a true rise can also be provided from related rising trends, including increased rates of suicide (28, 63), co-occurring functional impairment (36, 74), and mental health service use (28, 30, 71, 201, 202).
According to the findings of this review, over time, several social and commercial determinants have shown varying trends in their impact on youth mental health. increasing trends are observed in areas such as the instability and identity explorations associated with adolescent and emerging adulthood, homelessness and housing insecurity, cyberbullying, social media usage, and economic precarity, particularly in insecure employment. Conversely, there are decreasing trends in certain substance use, bullying victimization, and exposure to violence and abuse, though the latter also shows some stability. Mixed or stable trends are noted in areas like family structure, educational stress, urbanization, and the impact of maternal emotional problems.
Given the current context of the aftermath of the COVID-19 pandemic, many of these factors, particularly socio-economic inequality and climate change, will likely be exacerbated in the coming years (203, 204). Mental health and social services already need to be urgently expanded to meet the rising needs of young people and offset the likelihood of persistent mental health problems into later adulthood, including early parenthood (13). Hence, there are critical intergenerational consequences of inaction given parental mental health problems are predictive of offspring mental ill-health (205–208).
4.1 Determining the relative contributions (underlying forces) of these candidate causes
Adolescence and emerging adulthood have undergone two key maturational shifts: an early onset of puberty and a delayed commencement of independent adulthood (209). This has extended the period of heightened susceptibility to environmental stressors and mental ill-health. This lengthening of adolescence commenced prior to the recorded rise in youth mental ill-health in the 1990s (1). While its impact on more recent trends is unclear, it has converged with educational, labour market and economic shifts (e.g., prolonged years of education; insecure employment, income and housing; and delayed independence) that have contributed to highly precarious pathways to adulthood (113, 159, 163, 167). Emerging adulthood is a heightened period of instability and identity explorations, which have been correlated with anxiety (210). Increasing and cumulative exposure to psychosocial stressors during this period of precarity may have increased the risk of mental ill-health and contributed to deteriorating trends (13, 98, 211). However, the salience and impact of these influences are likely to vary across different cultural settings, as well as in relation to levels of wealth and development around the wealth (212, 213).
Various opinions and theories have emerged to examine and evaluate the candidate causes of negative trends in youth mental health. For example, Twenge (118, 214) and Haidt (143) argue that the rise of social media and increased screen time are the dominant contributors to the deterioration in mental health among young people, suggesting that these factors lead to heightened anxiety, depression, and social isolation. Twenge’s research points to a correlation between the advent of smartphones and a decline in adolescent mental health (215). Haidt (143)’s The Anxious Generation proposes a stronger relationship between the rise in social media use and deteriorating mental health among young people, positing that the increased screen time and social comparison are major contributors to the surge in anxiety and depression. While Haidt (143)’s work has brought significant attention to this issue, it has also been critiqued for potentially overemphasising the role of social media at the expense of other sociocultural and economic factors that may contribute to youth mental health trends. Additionally, the reliance on correlational data in Haidt (143)’s argument, limits the ability to draw definitive conclusions about causality. Thus, support for a causal link between social media usage and increasing depressive symptoms and low wellbeing is limited and requires further investigation using more robust measures of social media use. Despite this, politicians in several jurisdictions have been persuaded to implement age linked restrictions on access to the internet and social media for teenagers (216). Such action can be argued to be misdirected, lacking in nuance and to produce unintended consequences (217–219). This regulatory gap has allowed platforms to prioritize engagement and profit over the well-being of their users, particularly vulnerable populations like young people. Odgers (220) argues that age restrictions and mobile device bans may prove ineffective—or even counterproductive—considering what is known about adolescent behaviour. Regulation of the social media platforms to make them safer would be a more appropriate response.
Wilkinson and Pickett (175)’s work highlights the role of socio-economic inequality, emphasizing how growing disparities and economic stressors exacerbate mental health issues. Focusing on a deeper level, the economic doctrine of neoliberalism, which has dominated the political economy of the globe since the 1980s, can also be hypothesised to be a common force underpinning many of these trends in youth mental health and indeed wider effects on society (86, 221). Neoliberalism, with its promotion of individualism over collectivism and the common good, market deregulation, privatization, a weakened role and respect for government and even democracy, reduced government intervention erosion of the welfare state, creates an environment where young people face heightened economic pressures, social inequalities, and reduced and fragmented health and social safety nets (169, 222). These proposed contributory causes may (223) collectively contribute to the deteriorating trends in youth mental health, however their relative importance is yet to be determined scientifically. To explore whether youth mental health trends reflect surface manifestations of deeper underlying societal changes, new methodologies, including potentially illuminating cross-national comparisons could be employed (108, 224).
4.2 Methodologies required to improve clarity and guide public health and political and social measures
Further research is urgently required to understand megatrends impacting mental ill-health in order to quantify their relative effect and estimate their malleability. Subsequently the effective implementation of strategies that target such harmful forces undermining this and other related aspects of public health must be pursued. Firstly, prospective studies utilising comparable sampling methods and measurement approaches are needed to validate trends within and across specific regions and nations, including and especially need to include low- and middle-income countries. This includes using equivalent measures across repeated timepoints (225). A global focus is needed to coordinate national and harmonised surveillance efforts in monitoring trends (226). While the Global Burden of Disease studies provide essential descriptive epidemiology data on incidence, prevalence, mortality, morbidity and disability (227), large longitudinal studies of representative samples are needed to monitor trends and changes within cohorts by assessing young people’s psychosocial development prior to, during and following the developmental stage of emerging adulthood (225, 228). These studies should incorporate comparable measures of potential explanatory factors. By collecting data on a wide range of explanatory factors such as social media usage, economic precarity, and educational pressure, and performing sophisticated multivariate regression analyses, it may be possible to quantify their potential individual and combined effects on mental health outcomes (229).
Causality could be guided by criteria such as temporality, strength and consistency of association, and dose-response relation (230). How these variables interact, and their cumulative effects on mental health require exploration in addition to identifying protective factors. For example, path analysis (231, 232), systems dynamics (233), and structural equation modelling (SEM) (234, 235) model complex relationships between variables to identify direct and indirect pathways influencing mental health. Using advanced statistical software to construct SEM models that include multiple variables and pathways can provide a detailed understanding of how different factors interact to affect mental health (234). Additionally, big data and machine learning can analyze large datasets to identify patterns and predictors of mental health outcomes (236–238). Collecting and analyzing big data from sources such as social media, health records, and surveys, and using machine learning techniques, can uncover trends and predictive factors for youth mental health (237).
Conducting comprehensive literature searches, systematic reviews, and meta-analyses can summarize findings, assess the relative importance of different candidate causes, and identify overall trends and patterns (239). Qualitative research, including in-depth interviews, focus groups, and case studies, with young people, parents, and educators can be used to explore their lived experiences with economic insecurity, educational pressures, and other stressors, and how these impact young people’s mental health (240, 241).
A range of robust approaches (e.g., interrupted time series, cross-cohort comparisons) are needed that contribute to the triangulation of findings and increase confidence in inferring causality (242). This may guide the identification of new at-risk populations and can inform preventive and early intervention strategies where modifiable factors are targeted and their effect on trends are monitored (243, 244). Intervention studies can offer a starting point to implementing and evaluating interventions aimed at addressing identified risk factors and improving mental health outcomes (245, 246). Designing and testing interventions, such as school-based mental health programs or community support initiatives and measuring their effectiveness through stepped wedge, cluster and other forms of randomized controlled trials or other rigorous evaluation methods, can provide more robust evidence for effective strategies (247).
Improving the measurement of cross-sectoral impacts of mental health prevention and treatment costs requires innovative methodologies. By expanding the scope of economic evaluations to include broader cost perspectives and utilizing cost-benefit and return on investment analyses, decision makers can gain valuable insights that extend beyond the healthcare sector (14). Employing methods like Multiple Criteria Decision Analysis (MCDA) can help integrate these economic impacts with other relevant considerations, providing a comprehensive approach for informed decision-making across different government portfolios (248). Moreover, conducting policy analysis to identify key policies related to candidate causes and using statistical methods to assess their impact on youth mental health by comparing outcomes pre- and post-policy implementation, can provide valuable insights (249, 250). There is some scope for limited randomized trials, particularly stepped wedged designs as new policies are introduced sequentially across different communities (251). By integrating these methodologies, researchers can improve the clarity and robustness of their findings, providing a more comprehensive understanding of the relative contributions of different factors to trends in youth mental health. This will give political leaders the opportunity to move beyond opinion, ideology and superficial populist responses.
4.3 Solutions using the Mrazek and Haggerty (1994) spectrum of interventions for mental health
Improving mental health outcomes requires a multifaceted approach that includes prevention, early intervention, and continuing care. This holistic approach is exemplified in the Mrazek and Haggerty model (85), which highlights prevention, early intervention, and sustained treatment and recovery support (See Figure 3).
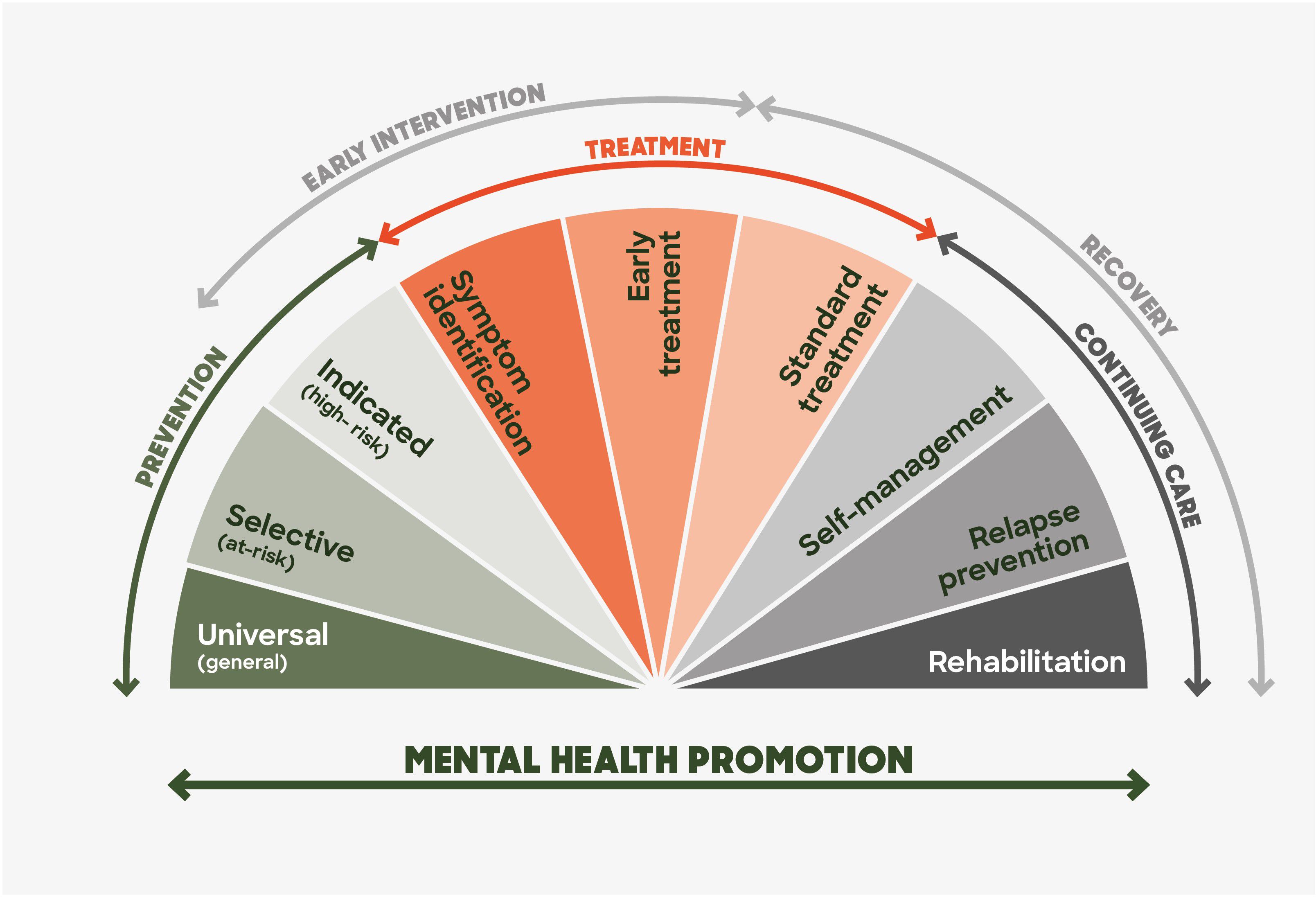
Figure 3. Model of the spectrum of interventions for mental health problems and mental health disorders: Adapted from Rickwood (84) and Mrazek & Haggerty (85).
4.3.1 Prevention
Preventive measures aim to reduce the incidence and severity of mental health disorders by targeting megatrends as well as traditional risk and protective factors. Key players in this effort include communities, families, schools, and digital platforms. To effectively reduce the incidence and severity of mental health disorders, it is recommended to strengthen community support by fostering social connections and providing essential resources, which can act as protective factors against mental health issues (199, 252–254). Studies have shown a positive relationship between high-quality social relationships and subjective well-being across all ages (255). These findings indicate that the quality of relationships is more crucial than the quantity. However, having a large and diverse social network also provides protection against depression (255). High social support is important for adolescents who have experienced child maltreatment or other adversities and serves as a protective factor for LGBTQ adolescents (256–258).
Youth mentoring programs, where an adult mentor provides social support and engages in shared activities without offering psychotherapeutic interventions, have been used to reduce the risk of behavioural disorders among young people (259). Evidence suggests these programs can enhance social and emotional skills and lower the risk of behavioural disorders, substance use, and criminal offending (259, 260).
Schools should implement mental health programs that include early identification and intervention services, as these can significantly improve student outcomes and address mental health challenges (261). Additionally, leveraging digital platforms to offer accessible resources, psychoeducation, peer support, and connections to mental health professionals can reduce symptoms of anxiety and depression among young people (262). These strategies can be integrated across different levels of prevention:
Universal prevention targets broad risk factors, protective factors, and megatrends for an entire population without regard to individual risk factors. For example, integrating mental health education into school curricula helps to normalize discussions about mental health and provide students with tools for managing stress and emotional challenges (261, 263). This may also include school-based behavioral interventions to minimize risk of bullying and peer rejection (264) as well as substance abuse (265). Conversely, the literature also suggests that universal interventions may be ineffective and, in some cases, potentially harmful (266, 267). For example, a systematic review of studies conducted in UK mainstream schools found that school-based universal interventions targeting the promotion of emotional or mental wellbeing, or the prevention of mental health difficulties demonstrated neutral to small effects (268).
The identification of potent harmful megatrends strengthens the momentum for and emphasis upon both universal and selective preventive strategies (14). However, even if the relative contribution of these megatrends and new risk factors can be clarified, how malleable they will be is quite another question. It is likely to be not merely a scientific one but a political and economic one which, when posed, is likely to provoke controversy and resistance. It took forty years for neoliberalism to displace Keynsian economic theory and although there is an emerging case being mounted within the field of progressive economics for a reengineering and humanization of capitalism in the service of the common good (269, 270), this will be resisted and would in any case take time. One only needs to reflect on how “science” has been misused to oppose efforts to counter efforts to decrease smoking and exposure to asbestos, and to respond to the climate crisis to anticipate how “merchants of doubt” would be mobilized to whitewash and defend harmful policies which threaten vested interests (271).
Selective prevention targets on at-risk groups. Selective interventions are aimed at individuals who are at a significantly higher risk of developing a mental disorder compared to the general population, despite being asymptomatic. For instance, targeted interventions for LGBTIQA+ youth can address unique stressors and reduce the risk of mental health issues (272). One might even assert that a substantial proportion of young people are an at-risk segment of society and are already showing serious warning signs ahead of the remainder of society.
Indicated prevention transitions into early intervention, providing support for individuals showing early signs of mental health issues. Programs that identify, treat and support young people with emerging mental health problems can prevent the escalation of symptoms (90, 273–275). Research suggests that indicated interventions have successfully achieved their goals by strengthening service engagement, shortening the duration of untreated illness, and coordinating with secondary prevention efforts (273, 276). This is potentially a “sweet spot” for most potential health and economic gain and cost-effectiveness.
A balanced approach that integrates universal, selective, and indicated prevention research and interventions is essential for addressing the mental, physical and social needs of young people (277).
4.3.2 Early intervention
Early intervention is considered a “best buy” in healthcare due to its cost-effectiveness and the substantial evidence supporting its benefits (274). Integrated and enhanced primary care youth services offer comprehensive support, addressing a range of mental health issues before they become severe (278). The “Integrated Behavioural Health in Primary Care” (IBHPC) model is an example, where behavioural health providers are embedded in primary care practices to offer immediate support and referrals (279). These services are designed to provide comprehensive, accessible, and coordinated care for young people, integrating mental health services into primary care settings. For instance, headspace serves as a model of Early Intervention, offering stigma-free, integrated support for mental health, substance use, and vocational needs while ensuring all help-seeking youth have access to care (14). This approach aims to address mental health issues early and effectively, leveraging the strengths of both primary care and specialized mental health services. For example, early psychosis intervention has been a focus for several decades, providing specialized care for young people experiencing their first episode of psychosis. This has now expanded to include transdiagnostic platforms of care, which address various mental health conditions within a unified framework (13).
4.3.3 Treatment, continuing care and recovery support
Holistic, evidence-based treatment approaches are essential for sustained mental health and well-being. Once people remit with the benefit of early treatment it is crucial as with cancer to keep them well or also intervene early should relapse occurs. Recovery-oriented approaches recognize the importance of peer support networks and community resources (280). Group-based psychosocial interventions for children and adolescents exposed to traumatic events in humanitarian settings have been found to be effective in low- and middle-income countries. For example, Alzaghoul et al. (281) found that a skills-based trauma-focused CBT program significantly reduced PTSD and depression scores compared to waitlist groups. On the other hand, another study showed a small beneficial effect of psychosocial support on PTSD symptoms at four weeks post-intervention, but no difference in depressive and anxiety symptoms between treatment and control groups (282). Community resources, including support groups and local mental health services, play a vital role in continuing care. These resources help individuals maintain their mental health gains post-treatment and provide ongoing support to prevent relapse (283).
While there has been a real, yet modest and piecemeal, expansion of treatment availability and uptake for some young people, thanks to model innovation, the prevalence and impact of mental health conditions have not decreased in almost 25 years and are rising among young people (14). There is a need for a radical change and decisive action which will involve a major boost to prevention, early intervention and innovative youth focused treatment systems (14, 263, 284).
4.4 Barriers, strategies and opportunities, including economic and political considerations
Prevention, early diagnosis and intervention, and sustained access to evidence-based care have catalysed progress for other non-communicable diseases, leading to significant reductions in the prevalence and impact of conditions such as cardiovascular disease and some forms of cancer (285–287). These fundamental components of health care have not received the same recognition, urgency for deployment, and investment in mental health (288–290). This explains the lack of reduction in the prevalence and burden of mental disorders over the past 25 years (291). Worse still there has been a parallel rise in rates of youth mental ill-health, increased help-seeking and greater need for accessible and safe mental health services among young people (30, 201). However mental health services for young people continue to be all too poorly designed, sparse in coverage and depth, and under-resourced, even in countries that have led youth mental health reform (13). Contributing to these shortcomings are a range of personal and structural barriers. Young people may face personal barriers such as a lack of awareness about available services, mistrust of those services, stigma, misconceptions surrounding mental health, and fears around seeking help (292). Structural barriers include the absence of supportive initiatives within young people’s circles of support (such as family, community, and educational settings), limited-service capacity, and inadequate funding (292). Economic and political factors also present significant barriers to improving the mental health landscape for young people. Unaccountable government policies, harmful and hidden economic orthodoxy, and the impact of unrestrained and unregulated commercial and business activity can be extremely harmful and result in large cohorts of the population being exposed to iatrogenic effects and commercial drivers of mental ill health (293, 294). This is partially recognized but often overlooked in political and economic decision-making. There is a need for mental health impact analyses or statements (295), similar to environmental impact assessments, to be conducted before policies and projects are approved. Privatisation of health care and other economic barriers limit access to mental health services, exacerbate health inequity, and constitute frank discrimination against the mentally ill (296, 297). This scandal results in underfunded mental health programs and insufficient insurance coverage (298).
Strategic investment in both prevention, early intervention, and recovery and improved public health approaches could enable countries to achieve much greater improvements in mental health, save a lot of money and future proof their societies as a result. This includes increased preventive efforts targeting risk factors and determinants of mental illness (e.g., social, economic and environmental), as well as improved provision of evidence-based early intervention that has the capacity to meet the volume of demand (14). Additionally, as discussed in the previous sections, a range of methodological approaches should be utilized to understand the megatrends related to young people’s mental health.
Political will is essential for enacting policies that deliver mental health equity, such as increased funding for mental health research proportional to its share of the burden of disease and its impact on society, implementation of school-based mental health programs, and the establishment of accessible mental health services (294, 299). Political will is directly proportional in a democracy to the level of public activism and demand for reform, which needs to be energised and mobilised (300). Economic stability and growth can also indirectly impact mental health by reducing socio-economic adversity, one of the key contributors to mental health issues particularly among young people (68, 171, 175, 176). Policies aimed at reducing income inequality, improving education systems, and providing health and social safety nets can have positive effects on young people’s mental health (301, 302).
The mounting evidence of increasing youth mental ill-health combined with the persistent neglect of mental health care globally highlights the urgent need for increased action on prevention and early intervention of mental disorders. The scale of this crisis extends beyond the disorders that have been the main focus of this review, as other potentially serious mental illnesses that typically emerge during adolescence and young adulthood, such as eating disorders, have also increased in incidence (303). An immediate call to action was recently declared, with a whole of society approach invited to address growing rates of youth mental ill-health (18). To support this global endeavour, core principles to guide youth mental health care in low-, middle- and high-income countries are available (304) and a global blueprint to transform prevention and early intervention in youth mental health has been developed (305, 306). An urgent and serious public health response to the rising mental health needs of young people is required. This has the capacity to yield massive personal, social, and economic returns. If implemented effectively, major gains seen in other areas of health such as cancer and cardiovascular disease are also possible for youth mental health, and the mental health field and community globally.
5 Limitations
It is possible that factors not examined here, such as poor access to and quality of mental health care, have led to an increased prevalence, rather than incidence, of mental health issues among youth, as untreated or inadequately treated conditions may worsen and persist over time. Another limitation of this paper is the generalizability of findings. This lack of generalizability could be problematic as it overlooks some of the unique socio-economic, cultural, and environmental factors that influence youth mental health in diverse global contexts. Furthermore, trends and contributing factors in low- and middle-income countries remain unclear owing to the dominant focus on high-income countries, stemming from the fact that most data and literature comes from the latter. Another limitation of this review is the exclusion of neurodevelopmental disorders (NDDs), such as autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD), from the primary analysis. While these conditions have seen a significant rise in diagnoses over the past century and an increase in diagnosis-seeking behaviour post-pandemic, their prevalence and trends remain uncertain due to the lack of robust community surveys. This gap in data also applies to evidence regarding the time trends of several youth mental health disorders, including bipolar disorder, schizophrenia, and eating disorders, which tend to be absent from many of the surveys of mental health. Future research should aim to address these gaps to provide a more comprehensive understanding of mental health trends.
6 Conclusion
The increasing evidence of deteriorating mental health among young people highlights a significant global public health crisis. The substantial rise in anxiety, psychological distress, and depression since the mid-1990s is alarming and deeply concerning. Factors such as climate change, family environment, educational pressures, socio-economic precarity, intergenerational inequality and the rise of social media contribute to this trend, though each only partially explains the increase and many of them may stem from a deeper malaise with political and economic roots. Methodological constraints and unexamined risk factors and trends further complicate our understanding. The COVID-19 pandemic is likely to have exacerbated the crisis but, in a way, fully accounts for it, emphasizing the urgent need for dynamic research, prevention and a new wave of innovation in youth mental health and social care. Facing these challenges can mitigate and reverse the harm, reduce the prevalence and impact of mental illness and deliver vital and essential benefits to our societies and economies globally.
Author contributions
PM: Conceptualization, Writing – original draft, Writing – review & editing. HG: Formal analysis, Writing – original draft, Writing – review & editing. CM: Formal analysis, Writing – original draft, Writing – review & editing. SR: Writing – original draft, Writing – review & editing. CG: Formal analysis, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1517533/full#supplementary-material
References
1. Rutter M, Smith DJ. Psychosocial disorders in young people: time trends and their causes. Chichester, West Sussex: John Wiley & Sons Ltd (1995).
2. GBD 2019 Adolescent Mortality Collaborators. Global, regional, and national mortality among young people aged 10-24 years, 1950-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2021) 398:1593–618. doi: 10.1016/S0140-6736(21)01546-4
3. Canuto A, Weber K, Baertschi M, Andreas S, Volkert J, Dehoust MC, et al. Anxiety disorders in old age: psychiatric comorbidities, quality of life, and prevalence according to age, gender, and country. Am J Geriatric Psychiatry. (2018) 26:174–85. doi: 10.1016/j.jagp.2017.08.015
4. Gautam M, Tripathi A, Deshmukh D, Gaur M. Cognitive behavioral therapy for depression. Indian J Psychiatry. (2020) 62:S223–S9. doi: 10.4103/psychiatry.IndianJPsychiatry_772_19
5. Kim Y, Hagquist C. Trends in adolescent mental health during economic upturns and downturns: a multilevel analysis of Swedish data 1988-2008. J Epidemiol Community Health. (2018) 72:101–8. doi: 10.1136/jech-2017-209784
6. Coley RL, O’Brien M, Spielvogel B. Secular trends in adolescent depressive symptoms: growing disparities between advantaged and disadvantaged schools. J Youth Adolesc. (2019) 48:2087–98. doi: 10.1007/s10964-019-01084-1
7. Hafstad GS, Sætren SS, Wentzel-Larsen T, Augusti E-M. Adolescents’ symptoms of anxiety and depression before and during the Covid-19 outbreak - a prospective population-based study of teenagers in Norway. Lancet Regional Health Europe. (2021) 5:100093. doi: 10.1016/j.lanepe.2021.100093
8. Martin J, Hadwin JA. The roles of sex and gender in child and adolescent mental health. JCPP Adv. (2022) 2:e12059. doi: 10.1002/jcv2.12059
9. Shim R, Szilagyi M, Perrin JM. Epidemic rates of child and adolescent mental health disorders require an urgent response. Pediatrics. (2022) 149:e2022056611. doi: 10.1542/peds.2022-056611
10. Worthman CM, Trang K. Dynamics of body time, social time and life history at adolescence. Nature. (2018) 554:451–7. doi: 10.1038/nature25750
11. Caspi A, Houts RM, Ambler A, Danese A, Elliott ML, Hariri A, et al. Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the Dunedin birth cohort study. JAMA Network Open. (2020) 3:e203221. doi: 10.1001/jamanetworkopen.2020.3221
12. Productivity Commission. Mental health, Report no. 95. Canberra: Productivity Commission (2020).
13. McGorry PD, Mei C, Chanen A, Hodges C, Alvarez-Jimenez M, Killackey E. Designing and scaling up integrated youth mental health care. World Psychiatry. (2022) 21:61–76. doi: 10.1002/wps.20938
14. McGorry PD, Mei C, Dalal N, Alvarez-Jimenez M, Blakemore S-J, Browne V, et al. The Lancet Psychiatry Commission on youth mental health. Lancet Psychiatry. (2024) 11:731–74. doi: 10.1016/S2215-0366(24)00163-9
15. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12.
16. Levin KA, Currie C, Muldoon J. Mental well-being and subjective health of 11- to 15-year-old boys and girls in Scotland, 1994-2006. Eur J Public Health. (2009) 19:605–10. doi: 10.1093/eurpub/ckp046
17. Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. (2015) 56:345–65. doi: 10.1111/jcpp.2015.56.issue-3
18. Office of the Surgeon General. Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory. Washington, D.C: The U.S. Surgeon General’s Advisory (2021). Available at: https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf (Accessed September 20, 2024).
20. Australian Bureau of Statistics. National Study of Mental Health and Wellbeing (2022). Available online at: https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/2020-21 (Accessed September 15, 2024).
21. Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings. ABS (2021). Available at: https://www.abs.gov.au/statistics/health/health-services/patient-experiences/2020-21 (Accessed August 13, 2024).
22. Liu X, Yang F, Huang N, Zhang S, Guo J. Thirty-year trends of anxiety disorders among adolescents based on the 2019 Global Burden of Disease Study. Gen Psychiatr. (2024) 37:e101288. doi: 10.1136/gpsych-2023-101288
23. England N. Mental health: children and young people with an eating disorder waiting times (2015). Available online at: https://www.england.nhs.uk/statistics/statistical-work-areas/cyped-waiting-times/ (Accessed September 28, 2024).
24. Collishaw S. Annual research review: secular trends in child and adolescent mental health. J Child Psychol Psychiatry. (2015) 56:370–93. doi: 10.1111/jcpp.2015.56.issue-3
25. Goodwin RD, Weinberger AH, Kim JH, Wu M, Galea S. Trends in anxiety among adults in the United States, 2008-2018: rapid increases among young adults. J Psychiatr Res. (2020) 130:441–6. doi: 10.1016/j.jpsychires.2020.08.014
26. Parodi KB, Holt MK, Green JG, Porche MV, Koenig B, Xuan Z. Time trends and disparities in anxiety among adolescents, 2012–2018. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:127–37. doi: 10.1007/s00127-021-02122-9
27. Calling S, Midlov P, Johansson SE, Sundquist K, Sundquist J. Longitudinal trends in self-reported anxiety. Effects of age and birth cohort during 25 years. BMC Psychiatry. (2017) 17:119. doi: 10.1186/s12888-017-1277-3
28. Kosidou K, Magnusson C, Mittendorfer-Rutz E, Hallqvist J, Hellner Gumpert C, Idrizbegovic S, et al. Recent time trends in levels of self-reported anxiety, mental health service use and suicidal behaviour in Stockholm. Acta Psychiatr Scand. (2010) 122:47–55. doi: 10.1111/j.1600-0447.2009.01487.x
29. Australian Institute of Health and Welfare. Young Australians: their health and wellbeing 2011. Cat. no. PHE 140. Canberra: Australian Institute of Health and Welfare (2011).
30. Wiens K, Bhattarai A, Pedram P, Dores A, Williams J, Bulloch A, et al. A growing need for youth mental health services in Canada: examining trends in youth mental health from 2011 to 2018. Epidemiol Psychiatr Sci. (2020) 29:e115. doi: 10.1017/S2045796020000281
31. Duffy ME, Twenge JM, Joiner TE. Trends in mood and anxiety symptoms and suicide-related outcomes among U.S. undergraduates, 2007–2018: evidence from two national surveys. J Adolesc Health. (2019) 65:590–8. doi: 10.1016/j.jadohealth.2019.04.033
32. Thorisdottir IE, Asgeirsdottir BB, Sigurvinsdottir R, Allegrante JP, Sigfusdottir ID. The increase in symptoms of anxiety and depressed mood among Icelandic adolescents: time trend between 2006 and 2016. Eur J Public Health. (2017) 27:856–61. doi: 10.1093/eurpub/ckx111
33. Wang C, Li K, Kim M, Lee S, Seo DC. Association between psychological distress and elevated use of electronic devices among U.S. adolescents: results from the youth risk behavior surveillance 2009-2017. Addict Behav. (2019) 90:112–8. doi: 10.1016/j.addbeh.2018.10.037
34. Keyes KM, Gary D, O’Malley PM, Hamilton A, Schulenberg J. Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:987–96. doi: 10.1007/s00127-019-01697-8
35. Mehta K, Kramer H, Durazo-Arvizu R, Cao G, Tong L, Rao M. Depression in the US population during the time periods surrounding the great recession. J Clin Psychiatry. (2015) 76:e499–504. doi: 10.4088/JCP.14m09637
36. Lu W. Adolescent depression: national trends, risk factors, and healthcare disparities. Am J Health Behav. (2019) 43:181–94. doi: 10.5993/AJHB.43.1.15
37. Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. (2019) 128:185–99. doi: 10.1037/abn0000410
38. Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. (2018) 48:1308–15. doi: 10.1017/S0033291717002781
39. Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. (2016) 138:e20161878. doi: 10.1542/peds.2016-1878
40. Lipson SK, Lattie EG, Eisenberg D. Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007-2017). Psychiatr Serv. (2019) 70:60–3. doi: 10.1176/appi.ps.201800332
41. Lu W, Kim JC, Yoon AS, Yun KK, Solomon P. Trends and disparities in unmet treatment needs for co-occurring depression and alcohol use disorders among young adults in the U.S. Am J Orthopsychiatry. (2022) 92:268–79. doi: 10.1037/ort0000608
42. Sutcliffe K, Ball J, Clark TC, Archer D, Peiris-John R, Crengle S, et al. Rapid and unequal decline in adolescent mental health and well-being 2012–2019: Findings from New Zealand cross-sectional surveys. Aust N Z J Psychiatry. (2022) 57:264–82. doi: 10.1177/00048674221138503
43. Sawyer MG, Reece CE, Sawyer ACP, Johnson SE, Lawrence D. Has the prevalence of child and adolescent mental disorders in Australia changed between 1998 and 2013 to 2014? J Am Acad Child Adolesc Psychiatry. (2018) 57:343–50. doi: 10.1016/j.jaac.2018.02.012
44. Torikka A, Kaltiala-Heino R, Rimpelä A, Marttunen M, Luukkaala T, Rimpelä M. Self-reported depression is increasing among socio-economically disadvantaged adolescents - repeated cross-sectional surveys from Finland from 2000 to 2011. BMC Public Health. (2014) 14:408. doi: 10.1186/1471-2458-14-408
45. Tick NT, van der Ende J, Verhulst FC. Ten-year trends in self-reported emotional and behavioral problems of Dutch adolescents. Soc Psychiatry Psychiatr Epidemiol. (2008) 43:349–55. doi: 10.1007/s00127-008-0315-3
46. Due P, Damsgaard MT, Madsen KR, Nielsen L, Rayce SB, Holstein BE. Increasing prevalence of emotional symptoms in higher socioeconomic strata: trend study among Danish schoolchildren 1991–2014. Scandinavian J Public Health. (2019) 47:690–4. doi: 10.1177/1403494817752520
47. Mishina K, Tiiri E, Lempinen L, Sillanmäki L, Kronström K, Sourander A. Time trends of Finnish adolescents’ mental health and use of alcohol and cigarettes from 1998 to 2014. Eur Child Adolesc Psychiatry. (2018) 27:1633–43. doi: 10.1007/s00787-018-1158-4
48. Tick NT, van der Ende J, Verhulst FC. Twenty-year trends in emotional and behavioral problems in Dutch children in a changing society. Acta Psychiatr Scand. (2007) 116:473–82. doi: 10.1111/j.1600-0447.2007.01068.x
49. Comeau J, Georgiades K, Duncan L, Wang L, Boyle MH. Changes in the prevalence of child and youth mental disorders and perceived need for professional help between 1983 and 2014: evidence from the Ontario Child Health Study. Can J Psychiatry. (2019) 64:256–64. doi: 10.1177/0706743719830035
50. Fleming TM, Clark T, Denny S, Bullen P, Crengle S, Peiris-John R, et al. Stability and change in the mental health of New Zealand secondary school students 2007-2012: results from the national adolescent health surveys. Aust N Z J Psychiatry. (2014) 48:472–80. doi: 10.1177/0004867413514489
51. Collishaw S, Maughan B, Goodman R, Pickles A. Time trends in adolescent mental health. J Child Psychol Psychiatry. (2004) 45:1350–62. doi: 10.1111/j.1469-7610.2004.00335.x
52. Fink E, Patalay P, Sharpe H, Holley S, Deighton J, Wolpert M. Mental health difficulties in early adolescence: a comparison of two cross-sectional studies in England from 2009 to 2014. J Adolesc Health. (2015) 56:502–7. doi: 10.1016/j.jadohealth.2015.01.023
53. Konowałek Ł, Wolanczyk T. Changes in emotional and behavioral problems between 2000 and 2011 among 16-year-old Polish children: a cross-sectional study. Child Psychiatry Hum Dev. (2018) 49:757–65. doi: 10.1007/s10578-018-0791-y
54. Bobrowski K, Ostaszewski K, Pisarska A. Mental health of Warsaw middle school students. Mokotow Study 2004-2016. Psychiatr Pol. (2019) 55 1:127–43. doi: 10.12740/PP/OnlineFirst/112215
55. Sweeting H, Young R, West P. GHQ increases among Scottish 15 year olds 1987-2006. Soc Psychiatry Psychiatr Epidemiol. (2009) 44:579–86. doi: 10.1007/s00127-008-0462-6
56. Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health. (2021) 75:224–31. doi: 10.1136/jech-2020-215060
57. Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. (2020) 7:883–92. doi: 10.1016/S2215-0366(20)30308-4
58. Gagné T, Schoon I, McMunn A, Sacker A. Mental distress among young adults in Great Britain: long-term trends and early changes during the COVID-19 pandemic. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1261–72. doi: 10.1007/s00127-021-02194-7
59. Mitiku KW, Tegegne E, Amsalu M, Habtegiorgis SD, Melaku B. Mental illness in children and its determinants in Ethiopia: A systematic review and meta-analysis, 2023. Clin Child Psychol Psychiatry. (2024) 29:168–86. doi: 10.1177/13591045231209078
60. Jensen HAR, Davidsen M, Møller SR, Román JEI, Kragelund K, Christensen AI, et al. The health of the Danes: The national health profile 2021 [Danskernes sundhed – Den Nationale Sundhedsprofil 2021]. Copenhagen: Sundhedsstyrelsen (2022).
61. Reyes MP, Song I, Bhatt A. Breaking the silence: an epidemiological report on asian american and pacific islander youth mental health and suicide (1999–2021). Child Adolesc Ment Health. (2024) 29:136–44. doi: 10.1111/camh.12708
62. Matsumoto N, Kadowaki T, Takanaga S, Shigeyasu Y, Okada A, Yorifuji T. Longitudinal impact of the COVID-19 pandemic on the development of mental disorders in preadolescents and adolescents. BMC Public Health. (2023) 23:1308. doi: 10.1186/s12889-023-16228-z
63. Twenge JM, Joiner TE, Rogers ML, Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among U.S. adolescents after 2010 and links to increased new media screen time. Clin psychol Sci. (2018) 6:3–17. doi: 10.1177/2167702617723376
64. Twenge JM, Martin GN, Campbell WK. Decreases in psychological well-being among American adolescents after 2012 and links to screen time during the rise of smartphone technology. Emotion. (2018) 18:765–80. doi: 10.1037/emo0000403
65. Pitchforth J, Fahy K, Ford T, Wolpert M, Viner RM, Hargreaves DS. Mental health and well-being trends among children and young people in the UK, 1995-2014: analysis of repeated cross-sectional national health surveys. Psychol Med. (2019) 49:1275–85. doi: 10.1017/S0033291718001757
66. Wong SMY, Chen EYH, Suen YN, Wong CSM, Chang WC, Chan SKW, et al. Prevalence, time trends, and correlates of major depressive episode and other psychiatric conditions among young people amid major social unrest and COVID-19 in Hong Kong: a representative epidemiological study from 2019 to 2022. Lancet Reg Health West Pac. (2023) 40:100881. doi: 10.1016/j.lanwpc.2023.100881
67. Parks MJ, Roesler J, Menanteau B, Raguet M, Eisenberg ME. The intersection of depressive symptoms, adverse childhood experiences, and protective factors among adolescents: epidemiological evidence from minnesota, 2016 and 2019. Advers Resil Sci. (2022) 3:21–36. doi: 10.1007/s42844-022-00052-2
68. Thorisdottir IE, Asgeirsdottir BB, Kristjansson AL, Valdimarsdottir HB, Jonsdottir Tolgyes EM, Sigfusson J, et al. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: a longitudinal, population-based study. Lancet Psychiatry. (2021) 8:663–72. doi: 10.1016/S2215-0366(21)00156-5
69. Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 52:3222–30. doi: 10.1017/S0033291720005358
70. Prichett LM, Yolken RH, Severance EG, Carmichael D, Zeng Y, Lu Y, et al. COVID-19 and youth mental health disparities: intersectional trends in depression, anxiety and suicide risk-related diagnoses. Acad Pediatr. (2024) 24:837–47. doi: 10.1016/j.acap.2024.01.021
71. Twenge JM. Time period and birth cohort differences in depressive symptoms in the U.S., 1982–2013. Soc Indic Res. (2015) 121:437–54. doi: 10.1007/s11205-014-0647-1
72. Kachi Y, Abe A, Ando E, Kawada T. Socioeconomic disparities in psychological distress in a nationally representative sample of Japanese adolescents: a time trend study. Aust N Z J Psychiatry. (2017) 51:278–86. doi: 10.1177/0004867416664142
73. Harvey SB, Deady M, Wang MJ, Mykletun A, Butterworth P, Christensen H, et al. Is the prevalence of mental illness increasing in Australia? Evidence from national health surveys and administrative data, 2001-2014. Med J Aust. (2017) 206:490–3. doi: 10.5694/mja2.2017.206.issue-11
74. van Geelen SM, Hagquist C. Are the time trends in adolescent psychosomatic problems related to functional impairment in daily life? A 23-year study among 20,000 15-16 year olds in Sweden. J Psychosom Res. (2016) 87:50–6. doi: 10.1016/j.jpsychores.2016.06.003
75. Ross A, Kelly Y, Sacker A. Time trends in mental well-being: the polarisation of young people’s psychological distress. Soc Psychiatry Psychiatr Epidemiol. (2017) 52:1147–58. doi: 10.1007/s00127-017-1419-4
76. Collishaw S, Maughan B, Natarajan L, Pickles A. Trends in adolescent emotional problems in England: a comparison of two national cohorts twenty years apart. J Child Psychol Psychiatry. (2010) 51:885–94. doi: 10.1111/j.1469-7610.2010.02252.x
77. Sigfusdottir ID, Asgeirsdottir BB, Sigurdsson JF, Gudjonsson GH. Trends in depressive symptoms, anxiety symptoms and visits to healthcare specialists: a national study among Icelandic adolescents. Scandinavian J Public Health. (2008) 36:361–8. doi: 10.1177/1403494807088457
78. Buli BG, Larm P, Nilsson KW, Hellström-Olsson C, Giannotta F. Trends in mental health problems among Swedish adolescents: Do school-related factors play a role? PloS One. (2024) 19:e0300294. doi: 10.1371/journal.pone.0300294
79. von Soest T, Wichstrom L. Secular trends in depressive symptoms among Norwegian adolescents from 1992 to 2010. J Abnorm Child Psychol. (2014) 42:403–15. doi: 10.1007/s10802-013-9785-1
80. Cerniglia L, Cimino S. Eating Disorders and Internalizing/Externalizing Symptoms in Adolescents before and during the COVID-19 Pandemic. J Am Nutr Assoc. (2023) 42:445–51. doi: 10.1080/07315724.2022.2063206
81. Jorm AF, Butterworth P. Changes in psychological distress in Australia over an 8-year period: evidence for worsening in young men. Aust N Z J Psychiatry. (2006) 40:47–50. doi: 10.1080/j.1440-1614.2006.01740.x
82. Ahn-Horst RY, Bourgeois FT. Mental health-related outpatient visits among adolescents and young adults, 2006-2019. JAMA Netw Open. (2024) 7:e241468. doi: 10.1001/jamanetworkopen.2024.1468
83. Rice SM, Kealy D, Oliffe JL, Ogrodniczuk JS. Externalizing depression symptoms among Canadian males with recent suicidal ideation: a focus on young men. Early Intervention Psychiatry. (2019) 13:308–13. doi: 10.1111/eip.2019.13.issue-2
84. Rickwood D. Pathways of Recovery: Preventing Further Episodes of Mental Illness (Monograph). Australia: Commonwealth of Australia (2006).
85. Mrazek PH. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. US: National Academies Press (1994).
86. Kirkbride JB, Dykxhoorn J, Pitman A, Wright T, Anglin DM, Colman I, et al. The social determinants of mental health and disorder: evidence, prevention and recommendations. World Psychiatry. (2024) 23:58–90. doi: 10.1002/wps.21160
87. Acri MC. The intersection of extreme poverty and familial mental health in the United States. Soc Work Ment Health. (2017) 15:689–77. doi: 10.1080/15332985.2017.1319893
88. Yoshikawa H, Aber JL, Beardslee WR. The effects of poverty on the mental, emotional, and behavioral health of children and youth: implications for prevention. Am Psychol. (2012) 67:272–84. doi: 10.1037/a0028015
89. Duong MT, Bruns EJ, Lee K, Cox S, Coifman J, Mayworm A, et al. Rates of mental health service utilization by children and adolescents in schools and other common service settings: A systematic review and meta-analysis. Administration Policy Ment Health Ment Health Serv Res. (2021) 48:420–39. doi: 10.1007/s10488-020-01080-9
90. Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. (2007) 369:1302–13. doi: 10.1016/S0140-6736(07)60368-7
91. Abi-Jaoude E, Naylor KT, Pignatiello A. Smartphones, social media use and youth mental health. CMAJ. (2020) 192:E136–e41. doi: 10.1503/cmaj.190434
92. Gilmore AB, Fabbri A, Baum F, Bertscher A, Bondy K, Ha-Joon C, et al. Defining and conceptualising the commercial determinants of health. Lancet. (2023) 401:1194–213. doi: 10.1016/S0140-6736(23)00013-2
93. Velez G, Gibbs T, Fortuna L, Adam B, De Faria L, Elmaghraby R, et al. APA Resource Document: Social Determinants of Mental Health in Children and Youth. Washington DC: APA (2022).
94. Pennington A, Stanford J. Rebuilding after COVID-19 will need a sustained national reconstruction plan. J Aust Political Economy. (2020) 85:164.
96. Basu S, Banerjee B. Impact of environmental factors on mental health of children and adolescents: A systematic review. Children Youth Serv Review. (2020) 119:105515. doi: 10.1016/j.childyouth.2020.105515
97. Stepanous J, Munford L, Qualter P, Banaschewski T, Nees F, Elliott R. Social environment and brain structure in adolescent mental health: A cross-sectional structural equation modelling study using IMAGEN data. PloS One. (2023) 18:e0280062. doi: 10.1371/journal.pone.0280062
98. Slimmen S, Timmermans O, Lechner L, Oenema A. A socio-ecological approach of evidence on associations between social environmental factors and mental health outcomes of young adults: A systematic review. Soc Sci Humanities Open. (2024) 10:101068. doi: 10.1016/j.ssaho.2024.101068
99. Cameranesi M, Theron L, Höltge J, Jefferies P, Ungar M. Understanding the mechanisms through which family risk affects adolescent mental health: A model of multisystemic resilience in context. Children. (2022) 9:546. doi: 10.3390/children9040546
100. Andrews JL, Ahmed SP, Blakemore S-J. Navigating the social environment in adolescence: the role of social brain development. Biol Psychiatry. (2021) 89:109–18. doi: 10.1016/j.biopsych.2020.09.012
101. McAllister A, Fritzell S, Almroth M, Harber-Aschan L, Larsson S, Burström B. How do macro-level structural determinants affect inequalities in mental health? – a systematic review of the literature. Int J Equity Health. (2018) 17:180. doi: 10.1186/s12939-018-0879-9
102. Sweeting H, West P, Young R, Der G. Can we explain increases in young people’s psychological distress over time? Soc Sci Med. (2010) 71:1819–30. doi: 10.1016/j.socscimed.2010.08.012
103. Schepman K, Collishaw S, Gardner F, Maughan B, Scott J, Pickles A. Do changes in parent mental health explain trends in youth emotional problems? Soc Sci Med. (2011) 73:293–300. doi: 10.1016/j.socscimed.2011.05.015
104. Armitage JM, Collishaw S, Sellers R. Explaining long-term trends in adolescent emotional problems: what we know from population-based studies. Discover Soc Sci Health: Springer. (2024) 4:1–17. doi: 10.1007/s44155-024-00076-2
105. Collishaw S, Goodman R, Pickles A, Maughan B. Modelling the contribution of changes in family life to time trends in adolescent conduct problems. Soc Sci Med. (2007) 65:2576–87. doi: 10.1016/j.socscimed.2007.06.010
106. Seltzer JA. Family change and changing family demography. Demography. (2019) 56:405–26. doi: 10.1007/s13524-019-00766-6
107. Bersia M, Berchialla P, Charrier L, Lemma P, Borraccino A, Nardone P, et al. Mental well-being: 2010-2018 trends among italian adolescents. Int J Environ Res Public Health Switzerland: MDPI. (2022) 9:863. doi: 10.3390/ijerph19020863
108. Cosma A, Stevens G, Martin G, Duinhof EL, Walsh SD, Garcia-Moya I, et al. Cross-national time trends in adolescent mental well-being from 2002 to 2018 and the explanatory role of schoolwork pressure. J Adolesc Health. (2020) 66:S50–S8. doi: 10.1016/j.jadohealth.2020.02.010
109. Högberg B. Educational stressors and secular trends in school stress and mental health problems in adolescents. Soc Sci Med. (2021) 270. doi: 10.1016/j.socscimed.2020.113616
110. Read S, Hietajärvi L, Salmela-Aro K. School burnout trends and sociodemographic factors in Finland 2006-2019. Soc Psychiatry Psychiatr Epidemiol Germany: Springer International. (2022) 57:1659–69. doi: 10.1007/s00127-022-02268-0
111. Cosma A, Stevens GWJM, Vollebergh WAM, De Looze M. Time trends in schoolwork pressure among Dutch adolescents, 2001–2017: Gender and educational differences. Scandinavian J Public Health. (2021) 50:538–41. doi: 10.1177/14034948211018388
112. Högberg B, Strandh M, Hagquist C. Gender and secular trends in adolescent mental health over 24 years: The role of school-related stress. Soc Sci Med. (2020) 250:1–9. doi: 10.1016/j.socscimed.2020.112890
113. Booth RW, Sharma D, Leader TI. The age of anxiety? It depends where you look: changes in STAI trait anxiety, 1970-2010. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:193–202. doi: 10.1007/s00127-015-1096-0
114. McManus S, Gunnell D. Trends in mental health, non-suicidal self-harm and suicide attempts in 16–24-year old students and non-students in England, 2000–2014. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:125–8. doi: 10.1007/s00127-019-01797-5
115. West P, Sweeting H. Fifteen, female and stressed: changing patterns of psychological distress over time. J Child Psychol Psychiatry. (2003) 44:399–411. doi: 10.1111/jcpp.2003.44.issue-3
116. Massey ZB, Brockenberry LO, Harrell PT. Vaping, smartphones, and social media use among young adults: Snapchat is the platform of choice for young adult vapers. Addict Behav. (2021) 112:106576. doi: 10.1016/j.addbeh.2020.106576
117. Loukas A, Paddock EM, Li X, Harrell MB, Pasch KE, Perry CL. Electronic nicotine delivery systems marketing and initiation among youth and young adults. Pediatrics. (2019) 144. doi: 10.1542/peds.2018-3601
118. Twenge JM, Krizan Z, Hisler G. Decreases in self-reported sleep duration among U.S. adolescents 2009-2015 and association with new media screen time. Sleep Med. (2017) 39:47–53. doi: 10.1016/j.sleep.2017.08.013
119. Neville RD, Lakes KD, Hopkins WG, Tarantino G, Draper CE, Beck R, et al. Global changes in child and adolescent physical activity during the COVID-19 pandemic: A systematic review and meta-analysis. JAMA Pediatrics. (2022) 176:886–94. doi: 10.1001/jamapediatrics.2022.2313
120. Mishina K, Heinonen E, Lempinen L, Sourander A. Twenty-year changes of adolescent mental health and substance use: a Finnish population-based time-trend study. Eur Child Adolesc Psychiatry. (2024), 1–10. doi: 10.1007/s00787-024-02512-9
121. Sourander A, Koskelainen M, Niemela S, Rihko M, Ristkari T, Lindroos J. Changes in adolescents mental health and use of alcohol and tobacco: a 10-year time-trend study of Finnish adolescents. Eur Child Adolesc Psychiatry. (2012) 21:665–71. doi: 10.1007/s00787-012-0303-8
122. Clark T, Fleming T, Bullen P, Crengle S, Denny S, Dyson B, et al. Health and well-being of secondary school students in New Zealand: trends between 2001, 2007 and 2012. J Paediatr Child Health. (2013) 49:925–34. doi: 10.1111/jpc.2013.49.issue-11
123. Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2016: detailed findings. Drug Statistics series no. 31. Cat. no. PHE 214. Canberra: Australian Institute of Health and Welfare (2017).
124. Han B, Compton WM, Blanco C, DuPont RL. National trends in substance use and use disorders among youth. J Am Acad Child Adolesc Psychiatry. (2017) 56:747–54.e3. doi: 10.1016/j.jaac.2017.06.011
125. Ball J, Grucza R, Livingston M, ter Bogt T, Currie C, de Looze M. The great decline in adolescent risk behaviours: Unitary trend, separate trends, or cascade? Soc Sci Med. (2023) 317. doi: 10.1016/j.socscimed.2022.115616
126. AIHW. Young people’s use of alcohol, tobacco, e-cigarettes and other drugs. Australian Institute of Health and Welfare (2024). Available at: https://www.aihw.gov.au/reports/children-youth/young-people-alcohol-smoking-drugs (Accessed October 02, 2024).
127. M H-K. Drug and alcohol addiction by generation: Facts and statistics: American Addiction Centers (2024). Available online at: https://americanaddictioncenters.org/addiction-statistics/by-generation (Accessed August 16, 2024).
128. van Berkel SR, Prevoo MJL, Linting M, Pannebakker FD, Alink LRA. Prevalence of child maltreatment in the Netherlands: An update and cross-time comparison. Child Abuse Negl. (2020) 103:104439. doi: 10.1016/j.chiabu.2020.104439
129. Finkelhor D, Shattuck A, Turner HA, Hamby SL. Trends in children’s exposure to violence, 2003 to 2011. JAMA Pediatrics. (2014) 168:540–6. doi: 10.1001/jamapediatrics.2013.5296
130. Gonzalez-Izquierdo A, Cortina-Borja M, Woodman J, Mok J, McGhee J, Taylor J, et al. Maltreatment or violence-related injury in children and adolescents admitted to the NHS: comparison of trends in England and Scotland between 2005 and 2011. BMJ Open. (2014) 4:e004474. doi: 10.1136/bmjopen-2013-004474
131. Salas-Wright CP, Nelson EJ, Vaughn MG, Reingle Gonzalez JM, Córdova D. Trends in fighting and violence among adolescents in the United States, 2002-2014. Am J Public Health. (2017) 107:977–82. doi: 10.2105/AJPH.2017.303743
132. Degli Esposti M, Humphreys DK, Jenkins BM, Gasparrini A, Pooley S, Eisner M, et al. Long-term trends in child maltreatment in England and Wales, 1858–2016: an observational, time-series analysis. Lancet Public Health. (2019) 4:e148–e58. doi: 10.1016/S2468-2667(19)30002-7
133. Wolke D, Lereya ST. Long-term effects of bullying. Arch Dis Child. (2015) 100:879–85. doi: 10.1136/archdischild-2014-306667
134. Copeland WE, Wolke D, Angold A, Costello EJ. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA Psychiatry. (2013) 70:419–26. doi: 10.1001/jamapsychiatry.2013.504
135. Molcho M, Craig W, Due P, Pickett W, Harel-Fisch Y, Overpeck M, et al. Cross-national time trends in bullying behaviour 1994-2006: findings from Europe and North America. Int J Public Health. (2009) 54:S225–S34. doi: 10.1007/s00038-009-5414-8
136. Tiiri E, Luntamo T, Mishina K, Sillanmäki L, Brunstein Klomek A, Sourander A. Did bullying victimization decrease after nationwide school-based antibullying program? A time-trend study. J Am Acad Child Adolesc Psychiatry. (2020) 59:531–40. doi: 10.1016/j.jaac.2019.03.023
137. Cosma A, Whitehead R, Neville F, Currie D, Inchley J. Trends in bullying victimization in Scottish adolescents 1994–2014: changing associations with mental well-being. Int J Public Health. (2017) 62:639–46. doi: 10.1007/s00038-017-0965-6
138. Kennedy RS. Bullying trends in the United States: A meta-regression. Trauma Violence Abuse. (2019) 22:914–27. doi: 10.1177/1524838019888555
139. Kessel Schneider S, O’Donnell L, Smith E. Trends in cyberbullying and school bullying victimization in a regional census of high school students, 2006-2012. J Sch Health. (2015) 85:611–20. doi: 10.1111/josh.2015.85.issue-9
140. Jones L, Mitchell K, Finkelhor D. Online harassment in context: Trends from three youth internet safety surveys (2000, 2005, 2010). Psychol Violence. (2013) 3:53–69. doi: 10.1037/a0030309
141. Trompeter N, Jackson E, Sheanoda V, Luo A, Allison K, Bussey K. Cyberbullying prevalence in Australian adolescents: Time trends 2015-2020. J School Violence. (2022) 21:252–65. doi: 10.1080/15388220.2022.2075881
142. Patchin JWH S. 2019 Cyberbullying Data: Cyberbullying Research Center (2020). Available online at: https://cyberbullying.org/2019-cyberbullying-data (Accessed September 03, 2024).
143. Haidt J. The anxious generation: how the great rewiring of childhood is causing an epidemic of mental illness. Br J Gen Pract. (2024) 74:322–3. doi: 10.3399/bjgp24X738693
144. Haidt J, Allen N. Scrutinizing the effects of digital technology on mental health. Nature: Int Weekly J Sci. (2020) 578:226–7. doi: 10.1038/d41586-020-00296-x
145. Odgers CL, Jensen MR. Annual Research Review: Adolescent mental health in the digital age: facts, fears, and future directions. J Child Psychol Psychiatry. (2020) 61:336–48. doi: 10.1111/jcpp.13190
146. Viner RM, Aswathikutty-Gireesh A, Stiglic N, Hudson LD, Goddings A-L, Ward JL, et al. Roles of cyberbullying, sleep, and physical activity in mediating the effects of social media use on mental health and wellbeing among young people in England: a secondary analysis of longitudinal data. Lancet Child Adolesc Health. (2019) 3:685–96. doi: 10.1016/S2352-4642(19)30186-5
147. Orben A. Teenagers, screens and social media: a narrative review of reviews and key studies. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:407–14. doi: 10.1007/s00127-019-01825-4
148. Padmanathan P, Bould H, Winstone L, Moran P, Gunnell D. Social media use, economic recession and income inequality in relation to trends in youth suicide in high-income countries: a time trends analysis. J Affect Disord. (2020) 275:58–65. doi: 10.1016/j.jad.2020.05.057
149. Betul K, Niall M, Annmarie G. A systematic review: the influence of social media on depression, anxiety and psychological distress in adolescents. Int J Adolescence Youth: Taylor Francis Group. (2020) 25:79–93. doi: 10.1080/02673843.2019.1590851
150. Daly M. Social-media use may explain little of the recent rise in depressive symptoms among adolescent girls. Clin psychol Sci. (2018) 6:295–. doi: 10.1177/2167702617750869
151. Orben A, Przybylski AK. The association between adolescent well-being and digital technology use. Nat Hum Behav. (2019) 3:173–82. doi: 10.1038/s41562-018-0506-1
152. Kreski N, Platt J, Rutherford C, Olfson M, Odgers C, Schulenberg J, et al. Social media use and depressive symptoms among United States adolescents. J Adolesc Health. (2021) 68:572–9. doi: 10.1016/j.jadohealth.2020.07.006
153. Healy J. The Australian labour market in 2014: still ill? J Ind Relations. (2015) 57:348–65. doi: 10.1177/0022185615571981
154. Lennartz C, Arundel R, Ronald R. Younger adults and homeownership in Europe through the Global Financial Crisis. Population Space Place. (2016) 22:823–35. doi: 10.1002/psp.v22.8
155. Oreopoulos P, von Wachter T, Heisz A. The short- and long-term career effects of graduating in a recession. Am Economic J: Appl Economics. (2012) 4:1–29. doi: 10.1257/app.4.1.1
156. Bartelink VHM, Ya KZ, Guldbrandsson K, Bremberg S. Unemployment among young people and mental health: A systematic review. Scandinavian J Public Health. (2020) 48:544–58. doi: 10.1177/1403494819852847
157. Rathmann K, Pförtner T-K, Hurrelmann K, Osorio AM, Bosakova L, Elgar FJ, et al. The great recession, youth unemployment and inequalities in psychological health complaints in adolescents: a multilevel study in 31 countries. Int J Public Health: Int J Public Health. (2016) 61:809–19. doi: 10.1007/s00038-016-0866-0
158. Bacigalupe A, Esnaola S, Martín U. The impact of the Great Recession on mental health and its inequalities: the case of a Southern European region, 1997-2013. Int J Equity Health. (2016) 15:17. doi: 10.1186/s12939-015-0283-7
159. Fiori F, Rinesi F, Spizzichino D, Di Giorgio G. Employment insecurity and mental health during the economic recession: an analysis of the young adult labour force in Italy. Soc Sci Med. (2016) 153:90–8. doi: 10.1016/j.socscimed.2016.02.010
160. Black Dog Institute. Modern work: how changes to the way we work are impacting Australians’ mental health. Sydney, Australia. (2021).
161. Lager AC, Bremberg SG. Association between labour market trends and trends in young people’s mental health in ten European countries 1983-2005. BMC Public Health. (2009) 9:325. doi: 10.1186/1471-2458-9-325
162. Widnall E, Winstone L, Plackett R, Adams EA, Haworth CMA, Mars B, et al. Impact of school and peer connectedness on adolescent mental health and well-being outcomes during the COVID-19 pandemic: A longitudinal panel survey. Int J Environ Res Public Health. (2022) 19. doi: 10.3390/ijerph19116768
163. Golberstein E, Gonzales G, Meara E. How do economic downturns affect the mental health of children? Evidence from the national health interview survey. Health Econ. (2019) 28:955–70. doi: 10.1002/hec.v28.8
164. Wilkins R. The Household, Income and Labour Dynamics in Australia Survey: selected findings from waves 1 to 15. In: The 12th Annual Statistical Report of the HILDA Survey. Melbourne, Australia. (2017).
165. Wilkins R, Laß I, Butterworth P, Vera-Toscano E. The Household, Income and Labour Dynamics in Australia Survey: selected findings from waves 1 to 17. In: The 14th Annual Statistical Report of the HILDA Survey. Melbourne, Australia. (2019).
166. Atalay K, Edwards R, Liu BYJ. Effects of house prices on health: new evidence from Australia. Soc Sci Med. (2017) 192:36–48. doi: 10.1016/j.socscimed.2017.09.008
167. McKee K, Soaita AM. The ‘frustrated’ housing aspirations of generation rent. Glasgow: UK Collaborative Centre for Housing Evidence. (2018).
168. United Nations. World Social Report 2020: Inequality in a rapidly changing world. In: Department of Economic and Social Affairs, United Nations. (2020). Available at: https://www.un.org/development/desa/dspd/world-social-report/2020-2.html (Accessed October 16, 2024).
169. Bessant J. The precarious generation: a political economy of young people. Taylor & Francis Group: Routledge (2017).
170. Coram V. Perceptions of intergenerational inequality in policymaking and possible responses: the case of Australia. Youth. (2022) 2:515–25. doi: 10.3390/youth2040037
171. Elgar FJ, Pförtner T-K, Rothwell D. Socioeconomic differences and global trends in youth wellbeing and emotional distress in 165 countries and territories. Health Place. (2024) 89:103322. doi: 10.1016/j.healthplace.2024.103322
172. Gore Langton E, Collishaw S, Goodman R, Pickles A, Maughan B. An emerging income differential for adolescent emotional problems. J Child Psychol Psychiatry. (2011) 52:1081–8. doi: 10.1111/j.1469-7610.2011.02447.x
173. Perry BL, Aronson B, Pescosolido BA. Pandemic precarity: COVID-19 is exposing and exacerbating inequalities in the American heartland. Proc Natl Acad Sci U S A. (2021) 118:e2020685118. doi: 10.1073/pnas.2020685118
174. OECD. Young people’s concerns during COVID-19: results from Risks That Matter 2020. Paris: OECD (2021).
175. Wilkinson R, Pickett K. The spirit level: why more equal societies almost always do better. London: Penguin (2009).
176. Pickett KE, Wilkinson RG. Income inequality and health: A causal review. Soc Sci Med. (2015) 128:316–26. doi: 10.1016/j.socscimed.2014.12.031
177. Gunasiri H, Patrick R, Snell T, Garad R, Enticott J, Meadows G, et al. Young people’s mental health in a changing climate. Lancet Planetary Health. (2022) 6:S1. doi: 10.1016/S2542-5196(22)00263-7
178. Gunasiri H, Wang Y, Watkins E-M, Capetola T, Henderson-Wilson C, Patrick R. Hope, coping and eco-anxiety: young people’s mental health in a climate-impacted Australia. Int J Environ Res Public Health. (2022) 19. doi: 10.3390/ijerph19095528
179. Patrick R, Snell T, Gunasiri H, Garad R, Meadows G, Enticott J. Prevalence and determinants of mental health related to climate change in Australia. Aust N Z J Psychiatry. (2022) 57:710–24. doi: 10.1177/00048674221107872
180. Teo SM, Gao CX, Brennan N, Fava N, Simmons MB, Baker D, et al. Climate change concerns impact on young Australians’ psychological distress and outlook for the future. J Environ Psychol. (2024) 93:102209. doi: 10.1016/j.jenvp.2023.102209
181. Charlson F, Ali S, Benmarhnia T, Pearl M, Massazza A, Augustinavicius J, et al. Climate change and mental health: A scoping review. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18094486
182. Oswald TK, Langmaid GR. Considering ecological determinants of youth mental health in the era of COVID-19 and the Anthropocene: A call to action from young public health professionals. Health Promot J Aust. (2022) 33:324–8. doi: 10.1002/hpja.v33.2
183. Patrick R, Noy S, Henderson-Wilson C, Hayward J, Allender S, Gunasiri H, et al. Minding our futures: Understanding climate-related mental wellbeing using systems science. Health Place. (2023) 84:103134. doi: 10.1016/j.healthplace.2023.103134
184. Sciberras E, Fernando JW. Climate change-related worry among Australian adolescents: an eight-year longitudinal study. Child Adolesc Ment Health. (2022) 27:22–9. doi: 10.1111/camh.12521
185. Hickman C, Marks E, Pihkala P, Clayton S, Lewandowski RE, Mayall EE, et al. Climate anxiety in children and young people and their beliefs about government responses to climate change: a global survey. Lancet Planet Health. (2021) 5:e863–e73. doi: 10.1016/S2542-5196(21)00278-3
186. Ramadan R, Randell A, Lavoie S, Gao CX, Cruz Manrique PC, Anderson R, et al. Understanding the evidence for climate concerns, negative emotions and climate related mental ill-health in young people: a scoping review. medRxiv. (2021) [Preprint]. doi: 10.1101/2021.09.27.21264151
187. Burke M, González F, Baylis P, Heft-Neal S, Baysan C, Basu S, et al. Higher temperatures increase suicide rates in the United States and Mexico. Nat Climate Change. (2018) 8:723–9. doi: 10.1038/s41558-018-0222-x
188. Romanello M, McGushin A, Di Napoli C, Drummond P, Hughes N, Jamart L, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. (2021) 398:1619–62. doi: 10.1016/S0140-6736(21)01787-6
189. (APA) American Psychological Association. Stress in America 2024 Survey. Washington DC: APA (2024).
190. (APA) American Psychological Association. Stress in America: coping with change. Stress in America™ survey. Washington DC: APA (2017).
191. Hoyt LT, Zeiders KH, Chaku N, Toomey RB, Nair RL. Young adults’ psychological and physiological reactions to the 2016 U.S. presidential election. Psychoneuroendocrinology. (2018) 92:162–9. doi: 10.1016/j.psyneuen.2018.03.011
193. Wong SMY, Hui CLM, Suen YN, Wong CSM, Chan SKW, Lee EHM, et al. The impact of social unrest and pandemic on mental health of young people in Hong Kong: the transdiagnostic role of event-based rumination. Aust N Z J Psychiatry. (2022) 56:376–84. doi: 10.1177/00048674211025710
194. Gimbrone C, Bates LM, Prins SJ, Keyes KM. The politics of depression: Diverging trends in internalizing symptoms among US adolescents by political beliefs. SSM Ment Health. (2022) 2:100043. doi: 10.1016/j.ssmmh.2021.100043
195. Ahad AA, Sanchez-Gonzalez M, Junquera P. Understanding and addressing mental health stigma across cultures for improving psychiatric care: A narrative review. Cureus. (2023) 15:e39549. doi: 10.7759/cureus.39549
196. Skinner A, Occhipinti JA, Song YJC, Hickie IB. Population mental health improves with increasing access to treatment: evidence from a dynamic modelling analysis. BMC Psychiatry. (2022) 22:692. doi: 10.1186/s12888-022-04352-w
197. Jorm AF, Patten SB, Brugha TS, Mojtabai R. Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry. (2017) 16:90–9. doi: 10.1002/wps.20388
198. Foulkes L, Andrews JL. Are mental health awareness efforts contributing to the rise in reported mental health problems? A call to test the prevalence inflation hypothesis. New Ideas Psychol. (2023) 69:101010. doi: 10.1016/j.newideapsych.2023.101010
199. Baker D, Wang M, Filia KM, Teo SM, Morgan R, Ziou M, et al. The changing impacts of social determinants on youth mental health in Australia. Preprint (2024). doi: 10.1177/00207640241280910
200. Twenge JM, Gentile B, DeWall C, Ma D, Lacefield K, Schurtz DR. Birth cohort increases in psychopathology among young Americans, 1938-2007: a cross-temporal meta-analysis of the MMPI. Clin Psychol Rev. (2010) 30:145–54. doi: 10.1016/j.cpr.2009.10.005
201. Mojtabai R, Olfson M. National trends in mental health care for US adolescents. JAMA Psychiatry. (2020) 77:703–14. doi: 10.1001/jamapsychiatry.2020.0279
202. Burke T, Thompson A, Mifsud N, Yung AR, Nelson B, McGorry P, et al. Proportion and characteristics of young people in a first-episode psychosis clinic who first attended an at-risk mental state service or other specialist youth mental health service. Schizophr Res. (2022) 241:94–101. doi: 10.1016/j.schres.2021.12.035
203. IPCC. Climate change 2023: synthesis report. In: Contribution of Working Groups I, II and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change IPCC. Geneva, Switzerland: IPCC (2023).
204. Cross K, Evans J, MacLeavy J, Manley D. Analysing the socio-economic impacts of COVID-19: a new regional geography or pandemic enhanced inequalities? Regional Studies Regional Sci. (2022) 9:461–85. doi: 10.1080/21681376.2022.2084447
205. McLaughlin KA, Gadermann AM, Hwang I, Sampson NA, Al-Hamzawi A, Andrade LH, et al. Parent psychopathology and offspring mental disorders: results from the WHO World Mental Health Surveys. Br J Psychiatry. (2012) 200:290–9. doi: 10.1192/bjp.bp.111.101253
206. Jami ES, Hammerschlag AR, Bartels M, Middeldorp CM. Parental characteristics and offspring mental health and related outcomes: a systematic review of genetically informative literature. Trans Psychiatry. (2021) 11:197. doi: 10.1038/s41398-021-01300-2
207. van Houtum LAEM, Baaré WFC, Beckmann CF, Castro-Fornieles J, Cecil CAM, Dittrich J, et al. Running in the FAMILY: understanding and predicting the intergenerational transmission of mental illness. Eur Child Adolesc Psychiatry. (2024) 33:3885–98. doi: 10.1007/s00787-024-02423-9
208. Kamis C. The long-term impact of parental mental health on children’s distress trajectories in adulthood. Soc Ment Health. (2021) 11:54–68. doi: 10.1177/2156869320912520
209. Arnett JJ, Zukauskiene R, Sugimura K. The new life stage of emerging adulthood at ages 18-29 years: implications for mental health. Lancet Psychiatry. (2014) 1:569–76. doi: 10.1016/S2215-0366(14)00080-7
210. Arnett JJ, Mitra D. Are the features of emerging adulthood developmentally distinctive? A comparison of ages 18–60 in the United States. Emerging Adulthood. (2018) 8:412–9. doi: 10.1177/2167696818810073
211. McGorry PD, Coghill D, Berk M. Mental health of young Australians: dealing with a public health crisis. Med J Aust. (2023) 219:246–9. doi: 10.5694/mja2.v219.6
212. Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. (2014) 26:392–407. doi: 10.3109/09540261.2014.928270
213. Alegría M, NeMoyer A, Falgàs Bagué I, Wang Y, Alvarez K. Social determinants of mental health: where we are and where we need to go. Curr Psychiatry Rep. (2018) 20:95. doi: 10.1007/s11920-018-0969-9
214. Twenge J. Generations: the real differences between gen Z, millennials, gen X, boomers, and silents—and what they mean for America’s future. Perspect Sci Christian Faith. (2023) 75:212–4. doi: 10.56315/PSCF12-23Twenge
215. Twenge JM, Haidt J, Lozano J, Cummins KM. Specification curve analysis shows that social media use is linked to poor mental health, especially among girls. Acta Psychol (Amst). (2022) 224. doi: 10.1016/j.actpsy.2022.103512
216. Firstpost. Australia, France and more: How countries are trying to regulate social media for children (2024). Available online at: https://www.firstpost.com/explainers/countries-regulating-social-media-for-children-13839900.html (Accessed October 12, 2024).
217. Commission AHR. Proposed Social Media Ban for Under-16s in Australia (2024). Available online at: https://humanrights.gov.au/about/news/proposed-social-media-ban-under-16s-Australia (Accessed October 05, 2024).
218. Vuorre M, Przybylski AK. Global well-being and mental health in the internet age. Clin psychol Sci. (2023) 12:917–35. doi: 10.1177/21677026231207791
219. Geurts SM, Koning IM, Van den Eijnden RJJM, Vossen HGM. Predicting adolescents’ Problematic social media use from profiles of internet-specific parenting practices and general parenting dimensions. J Youth Adolesc. (2023) 52:1829–43. doi: 10.1007/s10964-023-01816-4
220. Odgers C. The great rewiring: is social media really behind an epidemic of teenage mental illness? Nature. (2024) 628:29–30. doi: 10.1038/d41586-024-00902-2
221. Patel V. The right to mental health. Lancet (London England) England: Elsevier. (2023) 402:1412–3. doi: 10.1016/S0140-6736(23)02241-9
222. Gariépy G, Danna SM, Hawke L, Henderson J, Iyer SN. The mental health of young people who are not in education, employment, or training: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol: Int J Res Soc Genet Epidemiol Ment Health Services. (2022) 57:1107–21. doi: 10.1007/s00127-021-02212-8
223. Fava N, Gao CX, Baker D. Climate of distress: responding to the youth mental health impacts of climate change. Climate of distress: responding to the youth mental health impacts of climate change. Melbourne: Orygen (2023).
224. Wright M, Reitegger F, Veldin M, Vidmar M, Borzucka-Sitkiewicz K, Gierczyk M, et al. What makes me happy and what worries me? A cross-national comparison of stressors and resources for stress relief among youth. Child Indic Res. (2024). doi: 10.1007/s12187-024-10194-7
225. Bogdan T, Xie W, Talaat H, Mir H, Venkataraman B, Banfield LE, et al. Longitudinal studies of child mental disorders in the general population: A systematic review of study characteristics. JCPP Advances. (2023) 3:e12186. doi: 10.1002/jcv2.12186
226. Mei C, Fitzsimons J, Allen N, Alvarez-Jimenez M, Amminger GP, Browne B, et al. Global research priorities for youth mental health. Early Intervention Psychiatry. (2020) 14:3–13. doi: 10.1111/eip.12878
227. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
228. Harris KM, Halpern CT, Whitsel EA, Hussey JM, Killeya-Jones LA, Tabor J, et al. Cohort profile: the national longitudinal study of adolescent to adult health (Add health). Int J Epidemiol. (2019) 48:1415–k. doi: 10.1093/ije/dyz115
229. Bonnini S, Borghesi M. Relationship between mental health and socio-economic, demographic and environmental factors in the COVID-19 lockdown period—A multivariate regression analysis. Mathematics. (2022) 10. doi: 10.3390/math10183237
230. Grimes DA, Schulz KF. Bias and causal associations in observational research. Lancet. (2002) 359:248–52. doi: 10.1016/S0140-6736(02)07451-2
231. Yang J, Li X, Mao L, Dong J, Fan R, Zhang L. Path analysis of influencing factors of depression in middle-aged and elderly patients with diabetes. Patient Preference Adherence. (2023) 17:273–80. doi: 10.2147/PPA.S392508
232. Derrick S, Mohammed M, Louis K, Natalino De Jesus T, Mark D, Valsamma E, et al. Longitudinal path analysis of depressive symptoms and functioning among women of child-rearing age in postconflict Timor-Leste. BMJ Global Health: BMJ Publishing Group. (2020) 5:e002039. doi: 10.1136/bmjgh-2019-002039
233. Graham E, Gariépy G, Orpana H. System dynamics models of depression at the population level: a scoping review. Health Res Policy Syst. (2023) 21. doi: 10.1186/s12961-023-00995-7
234. Kang H, Ahn JW. Model setting and interpretation of results in research using structural equation modeling: A checklist with guiding questions for reporting. Asian Nurs Res (Korean Soc Nurs Sci). (2021) 15:157–62. doi: 10.1016/j.anr.2021.06.001
235. Minoura A, Sugiyama T, Koyama T, Yoshioka T, Tabuchi T. Structural equation modeling of the effects of psychological distress and a fear of coronavirus disease 2019 on diabetes care in Japan: a cross-sectional study. Sci Rep. (2022) 12. doi: 10.1038/s41598-022-20716-4
236. Islam MM, Hassan S, Akter S, Jibon FA, Sahidullah M. A comprehensive review of predictive analytics models for mental illness using machine learning algorithms. Healthcare Analytics. (2024) 6:100350. doi: 10.1016/j.health.2024.100350
237. Iyortsuun NK, Kim S-H, Jhon M, Yang H-J, Pant S. A review of machine learning and deep learning approaches on mental health diagnosis. Healthcare. (2023) 11:285. doi: 10.3390/healthcare11030285
238. Ahmed A, Agus M, Alzubaidi M, Aziz S, Abd-Alrazaq A, Giannicchi A, et al. Overview of the role of big data in mental health: A scoping review. Comput Methods Programs Biomed Update. (2022) 2:100076. doi: 10.1016/j.cmpbup.2022.100076
239. Steel Z, Marnane C, Iranpour C, Chey T, Jackson J, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. (2014) 43:476–93. doi: 10.1093/ije/dyu038
240. Braun V, Clarke V. Conceptual and design thinking for thematic analysis. Qual Psychol. (2021) 9:3–26. doi: 10.1037/qup0000196
241. Clarke V, Braun V. Thematic analysis. J Posit Psychol Oxfordshire: Routledge. (2017) 12:297–8. doi: 10.1080/17439760.2016.1262613
242. Thapar A, Rutter M. Do natural experiments have an important future in the study of mental disorders? Psychol Med. (2019) 49:1079–88. doi: 10.1136/bmjgh-2019-002039
243. O’Connor M, Spry E, Patton G, Moreno-Betancur M, Arnup S, Downes M, et al. Better together: Advancing life course research through multi-cohort analytic approaches. Adv Life Course Res. (2022) 53:100499. doi: 10.1016/j.alcr.2022.100499
244. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. (2017) 46:348–55. doi: 10.1093/ije/dyw098
245. Smout S, Champion KE, O’Dean S, Teesson M, Gardner LA, Newton NC. Anxiety, depression and distress outcomes from the Health4Life intervention for adolescent mental health: a cluster-randomized controlled trial. Nat Ment Health. (2024) 2:818–27. doi: 10.1038/s44220-024-00246-w
246. Das JK, Salam RA, Lassi ZS, Khan MN, Mahmood W, Patel V, et al. Interventions for adolescent mental health: an overview of systematic reviews. J Adolesc Health. (2016) 59:S49–s60. doi: 10.1016/j.jadohealth.2016.06.020
247. Shahraki-Sanavi F, Ansari-Moghaddam A, Mohammadi M, Bakhshani N-M, Salehiniya H. Effectiveness of school-based mental health programs on mental health among adolescents. J Educ Health Promotion. (2020) 9:142. doi: 10.4103/jehp.jehp_421_19
248. Thokala P, Devlin N, Marsh K, Baltussen R, Boysen M, Kalo Z, et al. Multiple criteria decision analysis for health care decision making—An introduction: report 1 of the ISPOR MCDA emerging good practices task force. Value Health. (2016) 19:1–13. doi: 10.1016/j.jval.2015.12.003
249. Sapkota S, Rushton S, van Teijlingen E, Subedi M, Balen J, Gautam S, et al. Participatory policy analysis in health policy and systems research: reflections from a study in Nepal. Health Res Policy Systems. (2024) 22:1–15. doi: 10.1186/s12961-023-01092-5
250. Dopp AR, Lantz PM. Moving upstream to improve children’s mental health through community and policy change. Adm Policy Ment Health. (2020) 47:779–87. doi: 10.1007/s10488-019-01001-5
251. Iyer SN, Shah J, Boksa P, Lal S, Joober R, Andersson N, et al. A minimum evaluation protocol and stepped-wedge cluster randomized trial of ACCESS Open Minds, a large Canadian youth mental health services transformation project. BMC Psychiatry. (2019) 19:273. doi: 10.1186/s12888-019-2232-2
252. Santini ZI, Koyanagi A, Tyrovolas S, Mason C, Haro JM. The association between social relationships and depression: A systematic review. J Affect Disord. (2015) 175:53–65. doi: 10.1016/j.jad.2014.12.049
253. Filia K, Menssink J, Gao CX, Rickwood D, Hamilton M, Hetrick SE, et al. Social inclusion, intersectionality, and profiles of vulnerable groups of young people seeking mental health support. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:245–54. doi: 10.1007/s00127-021-02123-8
254. Gardner A, Filia K, Killackey E, Cotton S. The social inclusion of young people with serious mental illness: A narrative review of the literature and suggested future directions. Aust N Z J Psychiatry. (2018) 53:15–26. doi: 10.1177/0004867418804065
255. Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. (2017) 152:157–71. doi: 10.1016/j.puhe.2017.07.035
256. Meng X, Fleury M-J, Xiang Y-T, Li M, D’Arcy C. Resilience and protective factors among people with a history of child maltreatment: a systematic review. Soc Psychiatry Psychiatr Epidemiol: Int J Res Soc Genet Epidemiol Ment Health Services. (2018) 53:453–75. doi: 10.1007/s00127-018-1485-2
257. Fritz J, de Graaff AM, Caisley H, van Harmelen AL, Wilkinson PO. A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Front Psychiatry. (2018) 9:230. doi: 10.3389/fpsyt.2018.00230
258. McDonald K. Social Support and Mental Health in LGBTQ Adolescents: A review of the literature. Issues Ment Health Nurs. (2018) 39:16–29. doi: 10.1080/01612840.2017.1398283
259. Tolan PH, Henry DB, Schoeny MS, Lovegrove P, Nichols E. Mentoring programs to affect delinquency and associated outcomes of youth at risk: A comprehensive meta-analytic review. J Exp Criminol. (2014) 10:179–206. doi: 10.1007/s11292-013-9181-4
260. Barry MM, Clarke AM, Morreale SE, Field CA. A review of the evidence on the effects of community-based programs on young people’s social and emotional skills development. Adolesc Res Review. (2018) 3:13–27. doi: 10.1007/s40894-017-0055-2
261. Weare K, Nind M. Mental health promotion and problem prevention in schools: what does the evidence say? Health Promot Int. (2011) 26:i29–69. doi: 10.1093/heapro/dar075
262. Best P, Manktelow R, Taylor B. Online communication, social media and adolescent wellbeing: A systematic narrative review. Children Youth Serv Review. (2014) 41:27–36. doi: 10.1016/j.childyouth.2014.03.001
263. Colizzi M, Lasalvia A, Ruggeri M. Prevention and early intervention in youth mental health: is it time for a multidisciplinary and trans-diagnostic model for care? Int J Ment Health Syst. (2020) 14:23. doi: 10.1186/s13033-020-00356-9
264. Nocentini A, Menesini E. KiVa anti-bullying program in Italy: evidence of effectiveness in a randomized control trial. Prev Sci. (2016) 17:1012–23. doi: 10.1007/s11121-016-0690-z
265. Patnode CD, O’Connor E, Rowland M, Burda BU, Perdue LA, Whitlock EP. Primary care behavioral interventions to prevent or reduce illicit drug use and nonmedical pharmaceutical use in children and adolescents: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med United States: Am Coll Physicians–American Soc Internal Med. (2014) p:612–20. doi: 10.7326/M13-2064
266. Caldwell DM, Davies SR, Hetrick SE, Palmer JC, Caro P, López-López JA, et al. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry. (2019) 6:1011–20. doi: 10.1016/S2215-0366(19)30403-1
267. Foulkes L, Stringaris A. Do no harm: can school mental health interventions cause iatrogenic harm? BJPsych Bull. (2023) 47:267–9. doi: 10.1192/bjb.2023.9
268. Mackenzie K, Williams C. Universal, school-based interventions to promote mental and emotional well-being: what is being done in the UK and does it work? A systematic review. BMJ Open. (2018) 8:e022560. doi: 10.1136/bmjopen-2018-022560
269. Mazzucato M. Governing the economics of the common good: from correcting market failures to shaping collective goals. J Economic Policy Reform. (2024) 27:1–24. doi: 10.1080/17487870.2023.2280969
270. Piketty T. Capital in the twenty-first century. The Belknap Press of Harvard University Press (2014).
271. Oreskes N, Conway EM. Merchants of doubt: How a handful of scientists obscured the truth on issues from tobacco smoke to global warming. USA: Bloomsbury Publishing (2011).
272. Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, et al. Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. J Adolesc Health. (2011) 49:115–23. doi: 10.1016/j.jadohealth.2011.02.005
273. Mei C, van der Gaag M, Nelson B, Smit F, Yuen HP, Berger M, et al. Preventive interventions for individuals at ultra high risk for psychosis: An updated and extended meta-analysis. Clin Psychol Rev. (2021) 86:102005. doi: 10.1016/j.cpr.2021.102005
274. McGorry P, Bates T, Birchwood M. Designing youth mental health services for the 21st century: examples from Australia, Ireland and the UK. Br J Psychiatry. (2013) 202:s30–s5. doi: 10.1192/bjp.bp.112.119214
275. McGorry PD, Hartmann JA, Spooner R, Nelson B. Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry. (2018) 17:133–42. doi: 10.1002/wps.20514
276. WHO. Prevention of mental disorders: Effective interventions and policy options. Geneva: WHO (2004).
277. Warner KE, Boat T, O’Connell ME. Preventing Mental, Emotional, and Behavioral Disorders among Young People: Progress and Possibilities. Washington, D.C., United States: National Academies Press (2009).
278. Hickie IB, Scott EM, Cross SP, Iorfino F, Davenport TA, Guastella AJ, et al. Right care, first time: a highly personalised and measurement-based care model to manage youth mental health. Med J Aust. (2019) 211:S3–S46. doi: 10.5694/mja2.v211.s9
279. Kwan BM, Valeras AB, Levey SB, Nease DE, Talen ME. An evidence roadmap for implementation of integrated behavioral health under the affordable care act. AIMS Public Health. (2015) 2:691–717. doi: 10.3934/publichealth.2015.4.691
280. Grbic DS, Simetin IP, Istvanovic A. The importance of peer support in the recovery process of persons with mental disorders. Eur J Public Health. (2020) 30. doi: 10.1093/eurpub/ckaa166.1025
281. Aseel FA, Alison RM, Marc A. Post-traumatic stress disorder interventions for children and adolescents affected by war in low- and middle-income countries in the Middle East: systematic review. BJPsych Open: Cambridge Univ Press. (2022) 8(5):e153. doi: 10.1192/bjo.2022.552
282. Purgato M, Gross AL, Betancourt T, Bolton P, Bonetto C, Gastaldon C, et al. Focused psychosocial interventions for children in low-resource humanitarian settings: a systematic review and individual participant data meta-analysis. Lancet Global Health. (2018) 6:e390–400. doi: 10.1016/S2214-109X(18)30046-9
283. Slade M, Amering M, Farkas M, Hamilton B, O’Hagan M, Panther G, et al. Uses and abuses of recovery: Implementing recovery-oriented practices in mental health systems. World Psychiatry. (2014) 13:12–20. doi: 10.1002/wps.20084
284. McGorry PD, Mei C. Early intervention in youth mental health: progress and future directions. Evid Based Ment Health. (2018) 21:182–4. doi: 10.1136/ebmental-2018-300060
285. Mensah GA, Wei GS, Sorlie PD, Fine LJ, Rosenberg Y, Kaufmann PG, et al. Decline in cardiovascular mortality: possible causes and implications. Circ Res. (2017) 120:366–80. doi: 10.1161/CIRCRESAHA.116.309115
286. (AIHW) Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. Australia: AIHW (2024).
287. American Association for Cancer Research (AACR). Cancer progress report. Am Assoc Cancer Res. (2024).
288. Mahomed F. Addressing the problem of severe underinvestment in mental health and well-being from a human rights perspective. Health Hum Rights. (2020) 22:35–49.
289. Becker Anne E, Kleinman A. Mental health and the global agenda. N Engl J Med. (2013) 369:66–73. doi: 10.1056/NEJMra1110827
290. Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. eClinicalMedicine. (2022) 54. doi: 10.1016/j.eclinm.2022.101675
291. Kassebaum N, Kyu HH, Zoeckler L, Olsen HE, Thomas K, Pinho C, et al. Child and adolescent health from 1990 to 2015: findings from the global burden of diseases, injuries, and risk factors 2015 study. JAMA Pediatrics. (2017) 171:573–92. doi: 10.1001/jamapediatrics.2017.0250
293. Dun-Campbell K, Hartwell G, Maani N, Tompson A, van Schalkwyk MCI, Petticrew M. Commercial determinants of mental ill health: An umbrella review. PloS Global Public Health. (2024) 4:e0003605. doi: 10.1371/journal.pgph.0003605
294. Jenkins R, Baingana F, Ahmad R, McDaid D, Atun R. Social, economic, human rights and political challenges to global mental health. Ment Health Family Med. (2011) 8:87–96.
295. Cresswell-Smith J, Kauppinen T, Laaksoharju T, Rotko T, Solin P, Suvisaari J, et al. Mental health and mental wellbeing impact assessment frameworks-A systematic review. Int J Environ Res Public Health. (2022) 19. doi: 10.3390/ijerph192113985
296. Alayed TM, Alrumeh AS, Alkanhal IA, Alhuthil RT. Impact of privatization on healthcare system: A systematic review. Saudi J Med Med Sci. (2024) 12:125–33. doi: 10.4103/sjmms.sjmms_510_23
297. Anaf J, Freeman T, Baum F. Privatisation of government services in Australia: what is known about health and equity impacts. Globalization Health. (2024) 20:32. doi: 10.1186/s12992-024-01036-w
298. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
299. Carbone SR. The language, framework, system enablers, and political commitment that a country needs to promote and protect the mental health of its citizens. Ment Health Prev. (2024) 33:200324. doi: 10.1016/j.mhp.2024.200324
300. Baum F, Townsend B, Fisher M, Browne-Yung K, Freeman T, Ziersch A, et al. Creating political will for action on health equity: practical lessons for public health policy actors. Int J Health Policy Manage. (2022) 11:947–60. doi: 10.34172/ijhpm.2020.233
301. Verhulst F, Tiemeier H. Socioeconomic inequalities and mental health problems in children and adolescents. In: Taylor E, Verhulst F, Wong JCM, Yoshida K, editors. Mental Health and Illness of Children and Adolescents. Springer Singapore, Singapore (2020). p. 257–74.
302. Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Soc Sci Med. (2013) 90:24–31. doi: 10.1016/j.socscimed.2013.04.026
303. Agostino H, Burstein B, Moubayed D, Taddeo D, Grady R, Vyver E, et al. Trends in the incidence of new-onset anorexia nervosa and atypical anorexia nervosa among youth during the COVID-19 pandemic in Canada. JAMA Network Open. (2021) 4:e2137395. doi: 10.1001/jamanetworkopen.2021.37395
304. Killackey E, Hodges C, Browne V, Gow E, Varnum P, McGorry P, et al. A global framework for youth mental health: investing in future mental capital for individuals, communities and economies. Geneva: World Economic Forum (2020).
305. McGorry P. Building the momentum and blueprint for reform in youth mental health. Lancet Psychiatry. (2019) 6:459–61. doi: 10.1016/S2215-0366(19)30050-1
Keywords: youth mental health, anxiety, depression, time trends, prevalence, risk factors
Citation: McGorry P, Gunasiri H, Mei C, Rice S and Gao CX (2025) The youth mental health crisis: analysis and solutions. Front. Psychiatry 15:1517533. doi: 10.3389/fpsyt.2024.1517533
Received: 26 October 2024; Accepted: 09 December 2024;
Published: 21 January 2025.
Edited by:
Soumitra Das, Western Health, AustraliaCopyright © 2025 McGorry, Gunasiri, Mei, Rice and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Patrick McGorry, cGF0Lm1jZ29ycnlAb3J5Z2VuLm9yZy5hdQ==; Hasini Gunasiri, aGFzaW5pLmd1bmFzaXJpQHVuaW1lbGIuZWR1LmF1
 Patrick McGorry1,2*
Patrick McGorry1,2* Hasini Gunasiri
Hasini Gunasiri Caroline X. Gao
Caroline X. Gao