- 1Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 2Pediatrics Department, Central Hospital of Jinan City, Jinan, Shandong, China
- 3Basic Medical College, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
- 4College of Acupuncture - Moxibustion, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, China
Background: The Framingham Steatosis Index (FSI) serves as a diagnostic metric for fatty liver. While research has established a link between depression and fatty liver, the association with the Framingham Steatosis Index (FSI) remains undocumented. The aim of this study is to explore the potential correlation between FSI and depression, addressing this research void.
Methods: Our data originates from the National Health and Nutrition Examination Survey (NHANES) database. We employed the PHQ-9 questionnaire for the evaluation of depressive symptoms. We investigated the association between FSI and depression using a weighted multiple logistic regression model and stratified analysis. Non-linear associations were explored using fitted smooth curves. A recursive method was employed to identify inflection points. Subgroup analyses were conducted to examine differences in the association between FSI and depression within subgroups.
Results: Our research encompassed a total of 19,697 participants. Multivariate logistic regression analysis, adjusted for potential confounding factors, demonstrated a significant positive association between FSI and depression, with OR of 1.14 (95% CI: 1.10, 1.18). Stratified analysis indicated that a significant positive correlation exists between FSI and depression among all groups except those with BMI below 30. The non-linear relationship was further confirmed by the restricted cubic splines analysis, which revealed an inflection point at an FSI value of 29.72. Below this threshold, there was no significant correlation, while above it, a positive correlation was observed. Subgroup analysis revealed statistically significant interactions between FSI and depression within the educational attainment groups.
Conclusion: Our study’s discovery is the curvilinear relationship between FSI and depression. Factors such as inflammation, hormonal levels, and metabolic disruptions could be the underlying mechanisms driving this relationship. This finding offers valuable insights that could inform the development of comprehensive intervention strategies for managing depression in clinical settings.
1 Introduction
Depression, recognized as a pervasive mood disorder, poses a significant threat to global public health, affecting an estimated 280 million individuals around the world (1) and showing an upward trend in prevalence (2). A cross-sectional study conducted by Neyazi A et al. indicated an alarmingly high prevalence of depression in Afghanistan, reaching 72.05% (3). This condition not only erodes social, psychological, and physical well-being but also amplifies the risk of suicide (4, 5). Individuals with Major Depressive Disorder (MDD) are alarmingly prone to suicidal tendencies, with a mortality rate nearly 20 times higher than that of the broader population (6). In addition, depression is associated with a spectrum of health challenges, such as cardiovascular diseases, breast cancer, sleep disorders, and non-alcoholic fatty liver disease (7–10).
The Framingham Steatosis Index (FSI), developed by Long MT et al. in 2016, is a key diagnostic tool for hepatic steatosis (11). It was established through analysis of a cross-sectional study with 1,181 participants, incorporating factors like age, gender, BMI, triglycerides, hypertension, diabetes, and the ALT: AST ratio. The accuracy of the FSI has been confirmed through validation and it is currently being applied in clinical settings. A cohort study by Nima Motamed and colleagues has demonstrated that FSI is a potent tool for diagnosing non-alcoholic fatty liver disease (NAFLD) and has the additional capability to predict new incidences of NAFLD (12). Furthermore, a community-based evaluation of liver steatosis by Jung TY and other researchers revealed that the FSI outperformed both the Hepatic Steatosis Index (HSI) and the Fatty Liver Index (FLI) in terms of diagnostic accuracy (13). Previous research has already documented associations between liver-related markers and depression. The link between NAFLD and depression could be attributed to the disruption of inflammation, oxidative stress pathways, and mitochondrial dysfunction (14). For example, Manusov EG and colleagues have shown that the AST/ALT ratio is significantly correlated with depression (15). Furthermore, in a cohort study by Cho YK and colleagues, FSI demonstrated a significant predictive ability for cardiovascular risk (16). Considering that cardiovascular diseases, including hypertension, are significantly linked to depression (17), we have grounds to hypothesize a potential relationship between FSI and depression. Nonetheless, the relationship between FSI and depression remains largely unexplored. The National Health and Nutrition Examination Survey (NHANES) constitutes a large, meticulously collected, and extensively detailed database. Utilizing NHANES dataset, this study endeavors to investigate the association between FSI and depression. Our research endeavors to elucidate the intricate interplay among multiple factors and mental health, offering insights to inform the creation of more holistic prevention and intervention strategies.
2 Materials and methods
2.1 Study participants
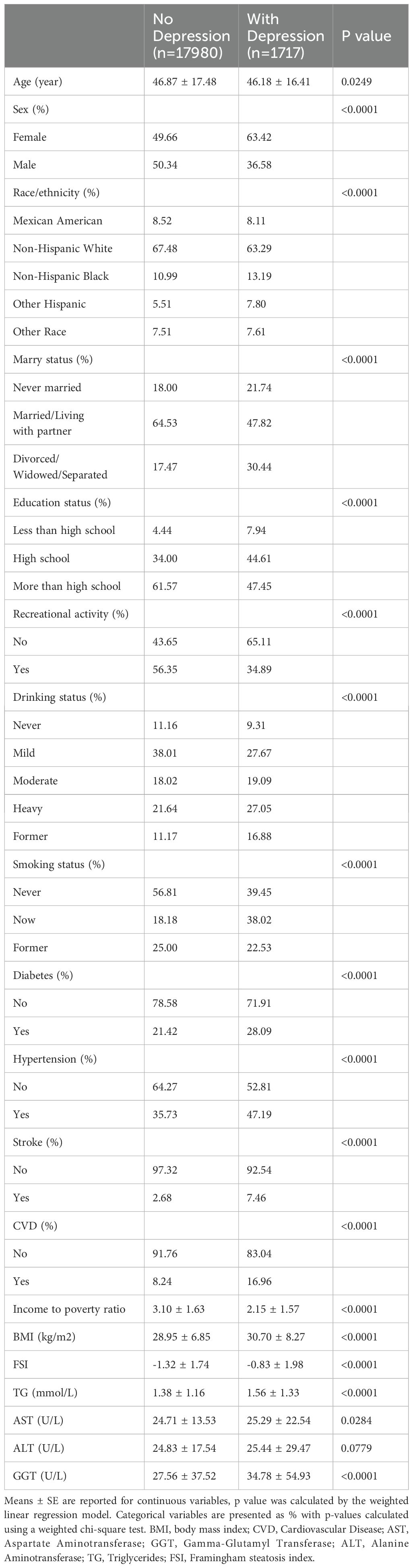
Our research drew upon data from the National Health and Nutrition Examination Survey (NHANES) in the United States, spanning nine cycles from 2003 to 2020. The NHANES database offers a rich array of information, including demographic details, lifestyle practices, self-reported health metrics, and blood biochemistry assessments. Data collection is conducted through household interviews, mobile examination centers (MECs), and laboratory tests. This resource is openly available to the research community without the need for specific permissions. The study protocol was granted approval by the National Center for Health Statistics Research Ethics Review Board, and all participants provided their informed written consent. To safeguard the privacy of the individuals involved, all personal identifiers were anonymized. In the data preparation phase of our study, we excluded participants who were under 18 years of age, accounting for 38,416 individuals. Furthermore, we omitted 33,761 individuals due to incomplete data on gender, age, BMI, diabetes status, hypertension, TG, AST, and ALT levels. An additional 3,998 individuals were excluded for lacking depression-related data. Consequently, our study encompassed a total of 19,697 participants, as depicted in Figure 1.
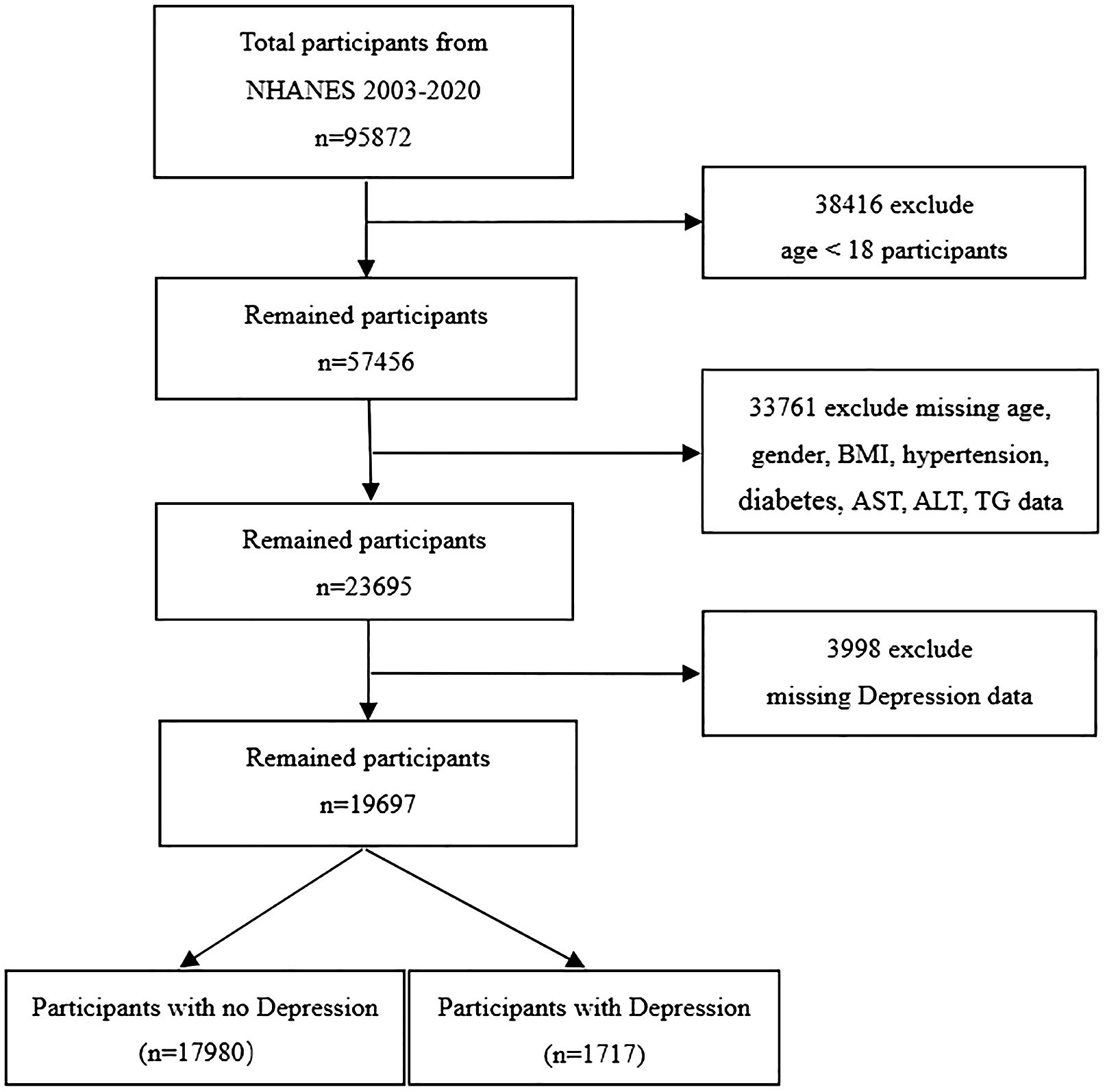
Figure 1. Flow chart of sample selection from the 2003-2020. BMI, body mass index; AST, Aspartate Aminotransferase; ALT, Alanine Aminotransferase; TG, Triglycerides.
2.2 Study variables
2.2.1 Definition of depression
The 9-item Patient Health Questionnaire (PHQ-9), recognized as a prevalent self-assessment tool, is fashioned to gauge the intensity of depressive symptoms experienced within a two-week period. This instrument adheres to the criteria for major depressive episodes as detailed in the DSM-IV, the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (18). This scale is a reliable tool for diagnosing depression, exhibiting high specificity and sensitivity. The questionnaire comprises nine items that evaluate symptoms such as sadness, loss of interest, sleep disturbances, fatigue, feelings of worthlessness, appetite issues, difficulty concentrating, psychomotor agitation or retardation, and suicidal thoughts. Each item is scored from 0 to 3, with 0 indicating “not at all”, 1 reflecting “a few days”, 2 corresponding to “more than half the days”, and 3 signifying “nearly every day”. The total score ranges from 0 to 27, with a score of 10 or above indicating the presence of depression. A total score of 9 or below is considered to indicate no depressive symptoms, while a score of 10 or above is used for the diagnosis of depression, demonstrating 88% sensitivity and 88% specificity. The PHQ-9 exhibits strong internal reliability, as evidenced by a Cronbach’s alpha coefficient of 0.89.
2.2.2 Definition of FSI
We employed FSI, as formulated by Long MT and colleagues in 2016 (11), in our analysis. It is calculated using the formula:
FSI = -7.981 + 0.011 × age (years) - 0.146 × sex (female = 1, male = 0) + 0.173 × BMI (kg/m2) + 0.007× triglycerides (mg/dL) + 0.593× hypertension (yes = 1, no = 0) + 0.789× diabetes (yes = 1, no = 0) + 1.1× ALT: AST ratio>= 1.33(yes = 1, no = 0).
Assessment of TG, AST and ALT Levels: Peripheral blood samples were collected in the morning from participants who had fasted for at least eight hours. Serum alanine TG, ALT levels were assessed using an enzymatic method, while AST levels were measured in serum or plasma by a kinetic rate assay.
2.2.3 Assessment of other variables
CDC collects comprehensive participant data, including demographics, lifestyle, self-reported health status, physical measurements, and biochemical indicators, through computer-assisted personal interviews. Demographic factors encompass age, sex, ethnicity, educational attainment, marital status, and the income-to-poverty ratio. Lifestyle factors, including smoking and drinking habits as well as recreational activities, were also taken into account. Self-reported health data included diabetes, hypertension, stroke, and cardiovascular disease, while anthropometric data included BMI. Biochemical data encompassed gamma-glutamyl transferase (GGT), triglycerides (TG), ALT, and AST. Smoking status was categorized into three distinct groups: “Never” was defined as having smoked fewer than 100 cigarettes in one’s lifetime; “Former” referred to individuals with a history of smoking who had since quit; and “Now” was designated for those who continued to smoke (19). Engagement in recreational activities was binary, recorded as “Yes” or “No.” The diagnosis of diabetes, including pre-diabetes, is based on meeting at least one of the following criteria: 1. Fasting blood glucose levels above 7.0 mmol/L; 2. Hemoglobin A1c (HbA1c) levels of 6.5% or higher; 3. Random blood glucose levels of at least 11.1 mmol/L; 4. Blood glucose levels of 11.1 mmol/L or higher after a 2-hour oral glucose tolerance test (OGTT); 5. A formal diagnosis of diabetes by a healthcare provider; 6. Impaired fasting glucose ranging from 6.11 to 7.0 mmol/L or impaired glucose tolerance, with OGTT levels between 7.7 and 11.1 mmol/L. Hypertension was determined by one or more of the following conditions: 1. Systolic blood pressure readings of 140 mmHg or higher; 2. Diastolic blood pressure of 90 mmHg or higher; 3. Current use of antihypertensive medications; 4. Self-reported hypertension. Alcohol consumption levels were categorized as follows: “Heavy” drinking was characterized by women consuming three or more drinks per day or four or more drinks on a single occasion; men consuming four or more drinks per day or five or more drinks on a single occasion, with at least five heavy drinking days per month. “Moderate” drinking was defined as women consuming two drinks per day and men consuming three drinks per day, with at least two heavy drinking days per month. “Mild” drinking referred to women having one drink per day and men having two drinks per day. “Never” drinking was designated for those who had fewer than 12 drinks in their lifetime, while “Former” drinkers were individuals with a history of drinking who no longer consumed alcohol. CVD was determined through a medical history questionnaire, which recorded whether participants had been diagnosed with coronary artery disease, congestive heart failure, or had a history of a heart attack (20).
2.3 Statistical analysis
The research data were properly weighted to accurately represent a more extensive demographic profile. We managed missing data by imputation, utilizing predictive mean matching for continuous variables and logistic regression for binary variables. Participants were categorized into groups with and without depression based on their baseline characteristics. Continuous variables are displayed as the mean ± standard error, while categorical variables are shown as percentages of the overall sample. To explore the association between FSI and depression, we utilized weighted logistic regression analysis. The outcomes are expressed as odds ratios (ORs) along with their respective 95% confidence intervals (95% CI). To substantiate the stability of the association between FSI and depression, we conducted a linear trend analysis. Subsequently, generalized additive models were applied to assess any potential non-linear relationships. After establishing non-linearity, the inflection point was determined using a recursive algorithm, which was then utilized to build a two-piecewise linear regression model. Further subgroup analyses and interaction tests were conducted to identify any additional risk factors that could potentially influence the relationship between FSI and depression. Statistical analyses were performed using R (version 3.5.3) and EmpowerStats software (http://www.empowerstats.com), with a P-value < 0.05 for statistical significance.
3 Results
3.1 Baseline characteristics
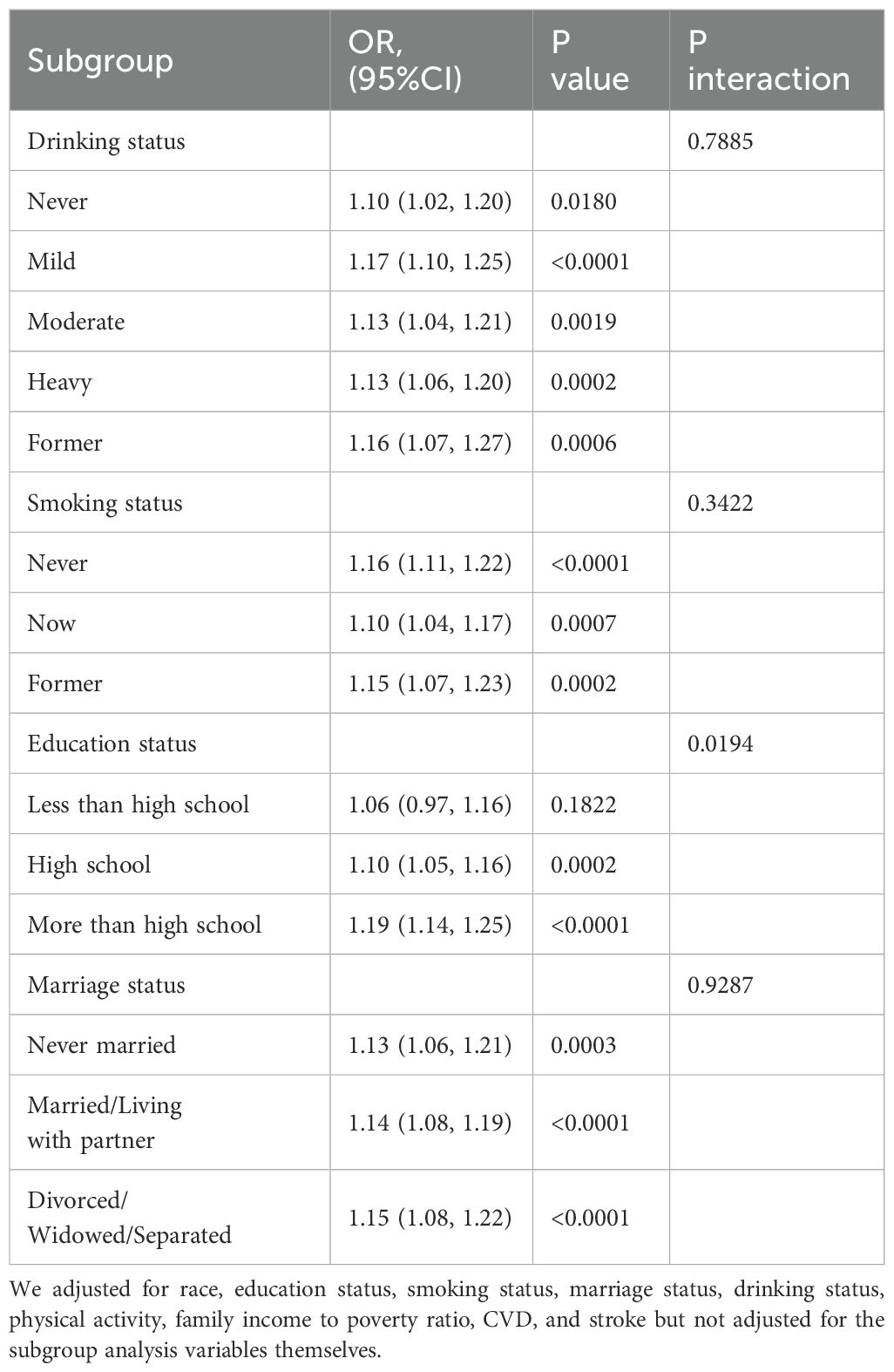
Table 1 delineates the foundational traits of participants, distinguishing those afflicted with depression from their non-depressed counterparts. Notably, the prevalence of women (63.42%) is markedly higher within the depressed cohort compared to the non-depressed group (49.66%). Individuals with depression are less likely to be married or living with a partner compared to those without depression, and are also less likely to have attained higher education, or to participate in recreational activities. They also have a higher incidence of health issues such as diabetes, hypertension, stroke, and cardiovascular disease. Moreover, they have a lower income-to-poverty ratio and are younger on average, yet they exhibit higher levels of BMI, FSI, TG, and GGT.
3.2 Association between FSI and depression
Table 2 details the correlation between FSI and depression. The unadjusted Model 1 revealed a significant positive association, with an OR of 1.17 (95% CI: 1.14, 1.20). This correlation persisted in Model 2, even after accounting for race and education status, with an OR of 1.15 (95% CI: 1.12, 1.18). Model 3, which included all covariates, still showed a positive significant association, with an OR of 1.14 (95% CI: 1.10, 1.18).In the subsequent trend test, the ORs (95% CI) for the association between FSI and depression were Q2 (OR: 0.90, 95% CI: 0.74, 1.09), Q3 (OR: 1.07, 95% CI: 0.89, 1.30), and Q4 (OR: 1.68, 95% CI: 1.41, 2.01), using Q1 as a reference, indicating a potential non-linear relationship between FSI and depression.
Sex-stratified analysis reveals that both females and males exhibit significant associations between FSI and depression, with females showing a more pronounced relationship (Female: OR 1.15, 95% CI: 1.11, 1.21; Male: OR 1.13, 95% CI: 1.07, 1.19). BMI-stratified analysis indicates that individuals with BMI >=30 demonstrate a significant association, while those with BMI <30 show no significant link. Age-stratified analysis confirms a consistent association across different age groups, with a stronger association observed in participants younger than 60 years old (<60: OR 1.12, 95% CI: 1.08, 1.16; >=60: OR 1.19, 95% CI: 1.10, 1.29).
In order to further explore the relationship between FSI and depression, we utilized a two-piecewise linear regression model enhanced by RCS analysis. The findings, after accounting for all relevant covariates, exposed a non-linear dynamic between FSI and the incidence of depression, as graphically represented in Figure 2. A pivotal point was discerned at an FSI value of -2.4. At values below this threshold, a negative correlation was observed, with OR of 0.89 (95% CI: 0.75, 1.07), which did not achieve statistical significance. Conversely, at values surpassing this threshold, a positive correlation emerged, with an OR of 1.17 (95% CI: 1.13, 1.22), signifying an enhanced probability of depression with an increase in FSI levels, as detailed in Table 3.
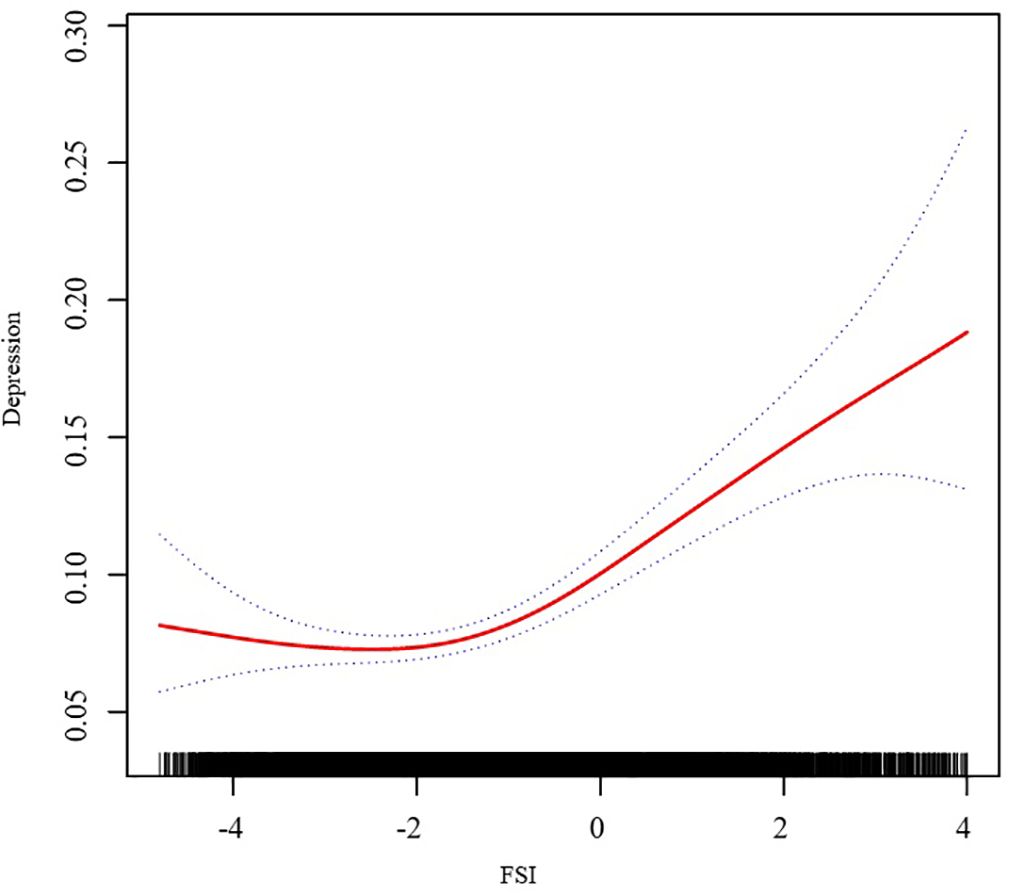
Figure 2. Association of FSI and Depression. We adjusted for race, education status, smoking status, marriage status, drinking status, physical activity, family income to poverty ratio, CVD, and stroke.
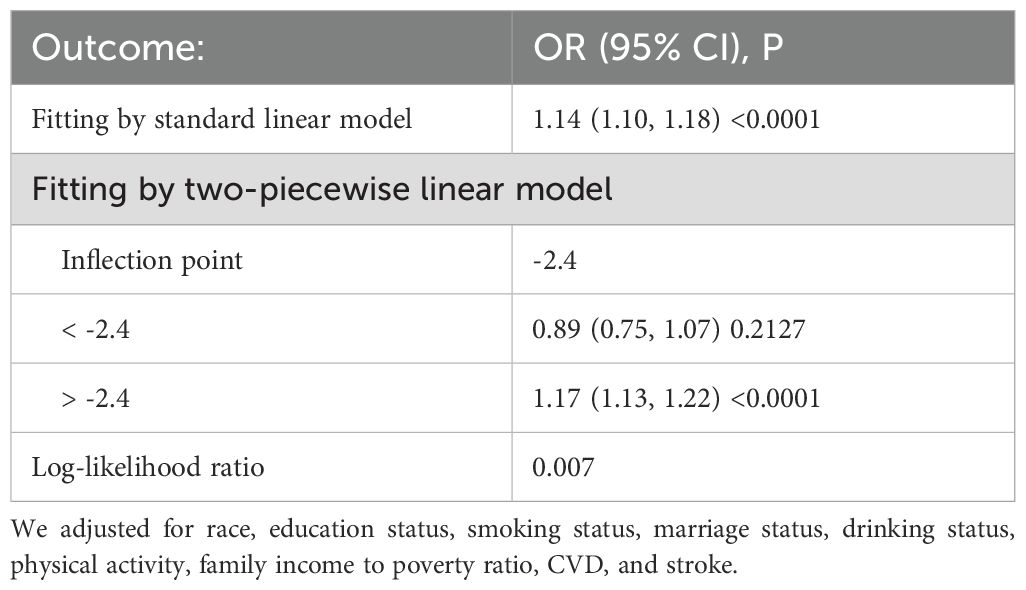
Table 3. Threshold effect analysis of FSI on depression using a two-piecewise linear regression model.
We performed subgroup analyses to investigate the potential Interaction between FSI and the risk of depression among different demographic groups, based on factors such as education level, marital status, smoking and drinking habits. The results indicate that there is a significant interaction between FSI and depression within subgroups defined by education level (Table 4). As education levels increase, the association between FSI and depression becomes more pronounced.
4 Discussion
As far as we are aware, this research pioneers the exploration of the association between FSI and the inclination toward depression. The multivariable logistic regression analysis, meticulously adjusted for a spectrum of potential confounding variables, has uncovered a notably positive correlation between FSI and depressive symptoms, with an OR of 1.14 (95% CI: 1.10, 1.18). Our sophisticated curve-fitting analysis has brought to light a nonlinear dynamic between FSI and the presence of depressive disorders, establishing an FSI threshold at -2.4. Below this threshold, no significant link is observed between FSI and the propensity for depression. Above this threshold, however, a 17% heightened risk of depression is associated with each incremental unit increase in FSI. These insights underscore the intricate interrelationship between FSI and the susceptibility to depressive tendencies. The intricate interconnection between physical and mental health is both pervasive and profound. For example, research indicates that an increase of 100μmol/L in uric acid levels is associated with a 21.7% reduction in the risk of depressive symptoms (21). Additionally, studies on the Dietary Inflammatory Index reveal that each unit increase in DII corresponds to a 12% rise in the likelihood of depression (22). These insights not only highlight the significance of the relationship between FSI and depression but also imply that a comprehensive, collaborative approach may be necessary for effective depression management.
Examining the FSI calculation formula reveals that the Framingham Steatosis Index is a composite indicator associated with sex, age, BMI, diabetes, hypertension, ALT/AST, and TG levels. While no research has yet investigated the link between FSI and depression, the relationships between depression and the individual components of the FSI formula have been previously explored in existing studies. Research indicates that women are roughly twice as likely as men to experience depression, a disparity that may stem from differences in sex hormones (23). Among the elderly, a study has found that individuals aged 70 and above who suffer from high blood pressure are at a higher risk of developing depression compared to those aged between 60 and 69 (24). Moreover, it’s been established that an individual’s BMI during adulthood, not during childhood, is causally linked to an increased risk of major depressive disorder (25). This underscores the significant role that age plays in the development of depression. A substantial link has been established between BMI and psychological well-being. Studies have demonstrated that obesity is associated with a 55% increased risk of depression, and individuals with depression are 58% more likely to become obese (26). Additionally, there is a correlation between depression and triglyceride levels; research by Segoviano-Mendoza M et al. has demonstrated that lower cholesterol levels are associated with mood disorders and suicidal behaviors, including Major Depressive Disorder (27). Furthermore, a robust association exists between depression and diabetes, hinting at a potential two-way causality (28). Hypertension, a condition that can severely impact the well-being of older adults, has also been linked to depression (29). There is also evidence to suggest that depression can influence the expression of genetic factors in liver enzymes, particularly the ratio of AST to ALT (30).
The precise mechanisms underlying the interaction between FSI and depression remain unclear. However, evidence suggests that inflammation, hormonal imbalances, and metabolic disruptions may be pivotal in this relationship. Obesity could trigger immune-inflammatory pathways (31), causing adipose tissue to release inflammatory cytokines like tumor necrosis factor-α and interleukin-6, which can impair brain function and precipitate depressive symptoms (32). Moreover, depression might intensify inflammatory responses by affecting the serotonin system and the hypothalamic-pituitary-adrenal axis (33). Research indicates that inflammatory markers such as AST/ALT are significantly involved in the pathophysiology of depression in individuals with diabetes (34). Fluctuations in sex hormone levels could also influence the development of depression by altering immune responses and inflammatory markers like C-reactive protein (35). Depression may further stimulate the hypothalamic axis, leading to increased cortisol secretion and subsequent insulin resistance (36). This insulin resistance could hasten liver fat accumulation and result in the overproduction of very-low-density lipoprotein-triglycerides, causing abnormal triglyceride levels (37). Conditions linked to metabolic disorders, such as hypertension and diabetes, may also contribute to the onset of depression (24). Studies suggest that obesity might elevate the risk of mental health issues through stress responses mediated by the hypothalamic-pituitary-adrenal axis (38). The progression of late-life depression is multifaceted and associated with cognitive decline (24). Educational level also impacts the prevalence of depression, largely due to its influence on memory capacity and, consequently, the expression of depressive symptoms (39). Overall, the interplay between FSI and depression appears to be a complex dynamic involving the dysregulation of multiple physiological systems.
Our data is sourced from the NHANES database, recognized for its stringent and expert-driven data collection, as well as its large sample size, thereby providing robust credibility and reliability to our research findings. Employing stratified and subgroup analyses, we thoroughly investigated the link between FSI and depression, examining its variation across different population subsets. Nonetheless, our study has inherent limitations. As a cross-sectional observational study, it does not establish a causal relationship between FSI and depression. Moreover, unadjusted residual confounders or potential unknown factors may still affect our results. There is currently a gap in research elucidating the relationship and underlying mechanisms between FSI and depression.
Further longitudinal and experimental studies are required to delve into the biological mechanisms in detail. We hope that through our collective efforts, we can improve the understanding of the etiology and pathophysiological mechanisms of depression related to FSI, potentially refining comprehensive prevention and treatment strategies for depression.
5 Conclusion
Drawing from the NHANES database spanning 2003 to 2020, our research delineated a non-linear association between FSI and depression, pinpointing a critical inflection point at an FSI value of 29.72, as identified by restricted cubic spline analysis. Below this threshold, no significant correlation was observed, but an affirmative link materialized above it. Stratified analysis consistently showed a positive correlation between FSI and depression across all groups, with the exception of those with BMI below 30. Subgroup analysis further disclosed significant interactions between FSI and depression within educational attainment cohorts, underscoring the influence of demographic factors on this nexus. These findings accentuate the critical role of demographic and clinical parameters, along with tailored management strategies, in the evaluation of depression risk. The observed relationship between FSI and depression implies that interventions such as lifestyle adjustments and specific medical treatments for correlated chronic conditions may be crucial in preventing or alleviating the advancement of depressive symptoms. It is imperative that further clinical and foundational research be conducted to elucidate the mechanisms at play in this association and to devise more effective strategies for the prevention and treatment of depression.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: www.cdc.gov/nchs/nhanes/Default.aspx.
Ethics statement
The study was approved by the Ethics Review Committee of the National Center for Health Statistics. These studies were conducted in accordance with local legislation and institutional requirements. Written informed consent was obtained from participants or their legal guardians/next of kin as required by national legislation and institutional mandates.
Author contributions
CJ: Data curation, Formal analysis, Methodology, Software, Validation, Visualization, Writing – original draft. BW: Data curation, Formal analysis, Methodology, Software, Validation, Visualization, Writing – original draft. NW: Data curation, Formal analysis, Methodology, Software, Validation, Visualization, Writing – original draft. JW: Data curation, Methodology, Software, Validation, Visualization, Writing – original draft. YQ: Data curation, Methodology, Software, Validation, Visualization, Writing – original draft. GZ: Conceptualization, Methodology, Writing – review & editing. XZ: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors are grateful for the time and effort put in by participants during the NHANES data collection period.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
FSI, Framingham Steatosis Index; ALT, Alanine Aminotransferase; AST, Aspartate Aminotransferase; BMI, Body Mass Index; GGT, Gamma-Glutamyl Transferase; TG, Triglycerides; CVD, Cardiovascular Disease; CV, Cardiovascular; OGTT, Oral Glucose Tolerance Test; NHANES, National Health and Nutrition Examination Survey; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; RCS, Restricted Cubic Spline; CDC, Centers for Disease Control and Prevention; NCHS, National Center for Health Statistics; MECs, Mobile Examination Centers; OR, Odds Ratios; CI, Confidence Intervals.
References
1. World Health Organization Fact sheets. Depressive disorder (depression)(2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/depression (Accessed October 5, 2024).
2. Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J Psychiatr Res. (2020) 126:134–40. doi: 10.1016/j.jpsychires.2019.08.002
3. Neyazi A, Mohammadi AQ, Razaqi N, Rahimi BA, Sifat S, Rahimy N, et al. Health survey on anxiety, depression, and stress in Afghanistan: A large-scale cross-sectional study amid ongoing challenges. Discovery Ment Health. (2024) 4:38. doi: 10.1007/s44192-024-00090-5
4. Hao Y, Yuan Z, Zhu Y, Li S, Gou J, Dong S, et al. Association between tooth loss and depression mediated by lifestyle and Inflammation- a cross-sectional investigation. BMC Public Health. (2024) 24:2627. doi: 10.1186/s12889-024-20065-z
5. Baldessarini RJ, Innamorati M, Erbuto D, Serafini G, Fiorillo A, Amore M, et al. Differential associations of affective temperaments and diagnosis of major affective disorders with suicidal behavior. J Affect Disord. (2017) 210:19–21. doi: 10.1016/j.jad.2016.12.003
6. Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. (2014) 13:153–60. doi: 10.1002/wps.20128
7. Hua J, Shen R, Guo X, Yu L, Qiu M, Ma L, et al. The mediating role of depression in the association between socioeconomic status and cardiovascular disease: A nationwide cross-sectional study from NHANES 2005-2018. J Affect Disord. (2024) 366:466–73. doi: 10.1016/j.jad.2024.08.145
8. Cai Y, Zhaoxiong Y, Zhu W, Wang H. Association between sleep duration, depression and breast cancer in the United States: a national health and nutrition examination survey analysis 2009-2018. Ann Med. (2024) 56:2314235. doi: 10.1080/07853890.2024.2314235
9. Li Y, Yan J, Li Y. Association between allostatic load and depression in patients with sleep disorders: Evidence from the National Health and Nutrition Examination Survey (NHANES). Int J Psychiatry Med. (2024) 59:670–84. doi: 10.1177/00912174241244479
10. Lv D, Han N, Yuan M, Huang W, Yan L, Tang H. Depression and the risk of non-alcohol fatty liver disease: Results from a cross-sectional study and a Mendelian randomization analysis. J Affect Disord. (2024) 366:300–7. doi: 10.1016/j.jad.2024.08.189
11. Long MT, Pedley A, Colantonio LD, Massaro JM, Hoffmann U, Muntner P, et al. Development and validation of the Framingham steatosis index to identify persons with hepatic steatosis. Clin Gastroenterol Hepatol. (2016) 14:1172–80.e2. doi: 10.1016/j.cgh.2016.03.034
12. Motamed N, Nikkhah M, Karbalaie, Niya MH, Khoonsari M, Perumal D, et al. The ability of the Framingham steatosis index (FSI) to predict non-alcoholic fatty liver disease (NAFLD): A cohort study. Clin Res Hepatol Gastroenterol. (2021) 45:101567. doi: 10.1016/j.clinre.2020.10.011
13. Jung TY, Kim MS, Hong HP, Kang KA, Jun DW. Comparative assessment and external validation of hepatic steatosis formulae in a community-based setting. J Clin Med. (2020) 9:2851. doi: 10.3390/jcm9092851
14. Soto-Angona Ó, Anmella G, Valdés-Florido MJ, De Uribe-Viloria N, Carvalho AF, Penninx B, et al. Non-alcoholic fatty liver disease (NAFLD) as a neglected metabolic companion of psychiatric disorders: common pathways and future approaches. BMC Med. (2020) 18:261. doi: 10.1186/s12916-020-01713-8
15. Chan KL, Cathomas F, Russo SJ. Central and peripheral inflammation link metabolic syndrome and major depressive disorder. Physiol (Bethesda). (2019) 34:123–33. doi: 10.1152/physiol.00047.2018
16. Cho YK, Kim M, Kim YJ, Jung CH, Lee WJ, Park JY. Predictive value of the Framingham steatosis index for cardiovascular risk: a nationwide population-based cohort study. Front Cardiovasc Med. (2023) 10:1163052. doi: 10.3389/fcvm.2023.1163052
17. Neyazi A, Mohammadi AQ, Neyazi M, Timilsina S, Padhi BK, Griffiths MD. Hypertension, depression, and health-related quality of life among hospitalized patients in Afghanistan. J Hum Hypertens. (2024) 38:529–37. doi: 10.1038/s41371-024-00914-5
18. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
19. Chambers DM, Ocariz JM, McGuirk MF, Blount BC. Impact of cigarette smoking on volatile organic compound (VOC) blood levels in the U.S. population: NHANES 2003–2004. Environ Int. (2011) 37:1321–8. doi: 10.1016/j.envint.2011.05.01
20. Xu C, Liang J, Xu S, Liu Q, Xu J, Gu A. Increased serum levels of aldehydes are associated with cardiovascular disease and cardiovascular risk factors in adults. J Hazard Mater. (2020) 400:123134. doi: 10.1016/j.jhazmat.2020.123134
21. Wang J, Yang M, Lin H, Wang J. Association between uric acid and the risk of depressive symptoms in US adults: results from NHANES 2005-2018. Sci Rep. (2024) 14:24097. doi: 10.1038/s41598-024-74869-5
22. Zhai Y, Hu F, Yuan L, Wang L, Ye X, Cao Y, et al. Associations between an energy-adjusted inflammatory diet index and incident depression: a cohort study. Br J Nutr. (2024) 6:1–10. doi: 10.1017/S0007114524002253
23. Slavich GM, Sacher J. Stress, sex hormones, inflammation, and major depressive disorder: extending social signal transduction theory of depression to account for sex differences in mood disorders. Psychopharmacology. (2019) 236:3063–79. doi: 10.1007/s00213-019-05326-9
24. Niu Y, Sun Y, Xie Y, Yu S. Association between weight-adjusted waist circumference index and depression in older patients with hypertension: a study based on NHANES 2007-2016. Front Public Health. (2024) 12:1461300. doi: 10.3389/fpubh.2024.1461300
25. Xiao P, Li C, Mi J, Wu J. Evaluating the distinct effects of body mass index at childhood and adulthood on adult major psychiatric disorders. Sci Adv. (2024) 10:eadq2452. doi: 10.1126/sciadv.Adq2452
26. Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. (2010) 67:220–9. doi: 10.1001/archgenpsychiatry.2010.2
27. Segoviano-Mendoza M, Cárdenas-de la Cruz M, Salas-Pacheco J, Vázquez-Alaniz F, La Llave-León O, Castellanos-Juárez F, et al. Hypocholesterolemia is an independent risk factor for depression disorder and suicide attempt in Northern Mexican population. BMC Psychiatry. (2018) 18:7. doi: 10.1186/s12888-018-1596-z
28. Khawagi WY, Al-Kuraishy HM, Hussein NR, Al-Gareeb AI, Atef E, Elhussieny, et al. Depression and type 2 diabetes: A causal relationship and mechanistic pathway. Diabetes Obes Metab. (2024) 26:3031–44. doi: 10.1111/dom.15630
29. Kong L, Zhang H. Latent profile analysis of depression in non-hospitalized elderly patients with hypertension and its influencing factors. J Affect Disord. (2023) 341:67–76. doi: 10.1016/j.jad.2023.08.114
30. Manusov EG, Diego VP, Abrego E, Herklotz K, Almeida M, Mao X, et al. Gene-by-environment interaction in non-alcoholic fatty liver disease and depression: the role of hepatic transaminases. Med Res Arch. (2023) 11:10.18103/mra.v11i9.4408. doi: 10.18103/mra.v11i9.4408
31. Shelton RC, Miller AH. Inflammation in depression: is adiposity a cause? Dialogues Clin Neurosci. (2011) 13:41–53. doi: 10.31887/DCNS.2011.13.1/rshelton
32. Schachter J, Martel J, Lin CS, Chang CJ, Wu TR, Lu CC, et al. Effects of obesity on depression: A role for inflammation and the gut microbiota. Brain Behav Immun. (2018) 69:1–8. doi: 10.1016/j.bbi.2017.08.026
33. Catena-Dell’Osso M, Bellantuono C, Consoli G, Baroni S, Rotella F, Marazziti D. Inflammatory and neurodegenerative pathways in depression: a new avenue for antidepressant development? Curr Med Chem. (2011) 18:245–55. doi: 10.2174/092986711794088353
34. Song X, Zheng Q, Zhang R, Wang M, Deng W, Wang Q, et al. Potential biomarkers for predicting depression in diabetes mellitus. Front Psychiatry. (2021) 12:731220. doi: 10.3389/fpsyt.2021.731220
35. Chen B, Dong J, Guo W, Li T. Sex-specific associations between levels of high-sensitivity C-reactive protein and severity of depression: retrospective cross-sectional analysis of inpatients in China. BMC Psychiatry. (2024) 24:667. doi: 10.1186/s12888-024-06123-1
36. Wang S, Gao H, Lin P, Qian T, Xu L. Causal relationships between neuropsychiatric disorders and nonalcoholic fatty liver disease: A bidirectional Mendelian randomization study. BMC Gastroenterol. (2024) 24:03386–6. doi: 10.1186/s12876-024-03386-6
37. Kamagate A, Dong HH. FoxO1 integrates insulin signaling to VLDL production. Cell Cycle. (2008) 7:3162–70. doi: 10.4161/cc.7.20.6882
38. Russell G, Lightman S. The human stress response. Nat Rev Endocrinol. (2019) 15:525–34. doi: 10.1038/s41574-019-0228-0
39. Loss K, Fandino W, Almarie B, Bazan-Perkins B, Minetto J, Aranis N, et al. The impact of education level and socioeconomic status on the association between depressive symptoms and memory in an older population in Latin America: An exploratory analysis from the Brazilian Longitudinal Study of Aging (ELSI-BRAZIL). Dialogues Health. (2024) 5:100183. doi: 10.1016/j.dialog.2024.100183
Keywords: Framingham Steatosis Index, depression, curvilinear, NHANES, cross-sectional study
Citation: Jiang C, Wang B, Wang N, Wang J, Qu Y, Zhao G and Zhang X (2025) The curvilinear relationship between Framingham Steatosis Index and depression: insights from a nationwide study. Front. Psychiatry 15:1510327. doi: 10.3389/fpsyt.2024.1510327
Received: 12 October 2024; Accepted: 09 December 2024;
Published: 31 January 2025.
Edited by:
Daniel T. Christian, Des Moines University, United StatesReviewed by:
Mohsen Khosravi, Zahedan University of Medical Sciences, IranAhmad Neyazi, Afghanistan Center for Epidemiological Studies, Afghanistan
Copyright © 2025 Jiang, Wang, Wang, Wang, Qu, Zhao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Zhang, ZG9jdG9yemhhbmd4aW5AMTYzLmNvbQ==
†These authors share first authorship
 Chunqi Jiang
Chunqi Jiang Bo Wang
Bo Wang Ning Wang3†
Ning Wang3† Yinuo Qu
Yinuo Qu Xin Zhang
Xin Zhang