- 1Faculty of Medical and Health, The University of Sydney, Sydney, NSW, Australia
- 2South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka
Background: Approximately 70% of self-poisoning suicides occur in low- and middle-income countries (LMICs).The implementation of pesticide bans has significantly reduced the rate of pesticide self-poisoning in these regions; however, this has been accompanied by a shift toward an increased incidence of pharmaceutical poisoning, highlighting the importance of intervention strategies to prevent pharmaceutical self-poisoning in the future. This report summarizes the existing evidence on community pharmacist gatekeeper interventions aimed at reducing pharmaceutical suicide to discuss their complementary role with pesticide bans in LMICs.
Methods: The literature review identified studies published between April 2014 and April 2024 using multiple keywords related to “suicide,” “intervention,” “pharmacist” and “gatekeeper” in various library databases. Data were extracted into a table for analysis.
Results: Only eight relevant studies were found during the search period, and none quantified the impact of pharmacy gate keeper interventions. Community pharmacists became more confident and willing to intervene after pharmacist gatekeeper training. They demonstrated positive attitudes and improved knowledge and skills in responding to suicidal intent. However, the evidence supporting community pharmacy gatekeeper interventions primarily comes from developed countries. Furthermore, the role of pharmacists in preventing suicide relies on frequent contact between suicidal individuals and pharmacies in developed countries.
Conclusion: Pharmacy gatekeeper interventions can be implemented in LMICs as a complement to pesticide bans, provided they are modified and adapted to suit the specific context of these regions. Further research is essential to tailor and implement successful strategies from developed countries to address the unique challenges faced by LMICs.
1 Introduction
According to the World Health Organization, self-poisoning has become one of the most common method of suicide particularly in low- and middle-income countries (LMICs) (1). In 2019, more than 20% of suicides were attributed to self-poisoning (1). Additionally, majority of world’s suicide deaths (77%) occur in LMICs (2), with India and China alone accounting for 42% of the 703,000 annual suicides (1). However, less than 15% of studies on suicide prevention are based in LMICs (3). These facts highlight the importance of learning from the experiences of developed countries to curb self-poisoning prevention in LMICs.
A review of toxicological autopsy data shows that, in developed countries, medically prescribed drugs such as antidepressants are the primary cause of self-poisoning suicides (4). Consequently, these countries have developed suicide prevention through pharmacy regulations, with community pharmacists playing a pivotal role. Pharmacists serve as gatekeepers, regulating access to lethal medicines and act as sentinels by recognizing the signs of individuals at risk of suicide, such as changes in behavior or mood (5). At the level of behavioral prevention, pharmacists can engage with populations at risk and positively influence their mental states to help prevent suicides (6). In addition, pharmacists can also collaborate with other healthcare providers, such as physicians and mental health professionals, or make referrals to appropriate services and resources for individuals at risk of suicide (6).
Due to their critical role in suicide prevention, gatekeeping is an essential skill that supports community pharmacists in managing patients who present with warning signs. It involves recognizing signs of suicide, responding to patients with suicidal thoughts and reassuring them (7). Moreover, training is a key factor shaping the profession of pharmacists. It has an impact on their attitudes, experiences, and preparedness to participate in suicide care (6). Thus, suicide gatekeeper training programs, such as Pharm-SAVES (Signs, Ask, Validate, and Encourage) and QPR (Question, Persuade, and Refer) are designed to help increase suicide prevention rates. These programs can improve the trainees’ knowledge and self-efficacy, build their confidence in detecting signs of suicide and enable them to respond effectively to patients with suicidal thoughts (8).
Although no studies have directly identified a causal relationship between the implementation of community pharmacist gatekeeper interventions and changes in suicide rates, a study of suicide patterns in the United States (US) cited a significant decline in drug-related suicide rates (9). Following the development of the Pharm-SAVES online training program (10), the US suicide rate from drug use dropped by 6% and 7% in 2018 and 2019, respectively (9). In addition, self-poisoning suicide rates have declined since the mid-2000s (9), corresponding to the period when QPR was introduced and began to grow in popularity (11). This trend indicates that pharmacy gatekeeper interventions may be effective.
In LMICs, most suicides by self-poisoning occur through the use of lethal pesticides (4). However, the rate of pesticide self-poisoning in LMICs has declined in recent years following the ban on several highly toxic pesticides (12–14). LMICs are expected to observe trends similar to those in developed countries, with pharmaceutical poisoning becoming the main source of suicide (4). Thus, pharmacy gatekeeper training could emerge as a primary intervention strategy in these resource poor settings to prevent self-poisoning.
In addition to differences in choice of agents for suicide, LMICs differ from developed countries in terms of access to psychological support. Residents of developed countries are accustomed to seeking help from psychiatrists and psychologists. On the contrary, help-seeking behaviors in LMICs often heavily rely on community and family support systems (15). Furthermore, mental health services in developed countries are well-structured to provide a broader psychological support and treatment. In contrast, LMICs often have limited access to mental health services due to lack of medical resources, trained professionals, and healthcare infrastructure. Mental health facilities often unavailable in many rural areas, making it difficult for individuals to access appropriate psychiatric care (16). Therefore, there is a need to review studies on the effectiveness of pharmacy gatekeeper interventions and integrate them to the specific cultural and resource context of developing countries. Integrating these interventions with existing community-based support systems could improve their relevance and effectiveness.
This review aims to explore the effectiveness of pharmacist gatekeeper training interventions implemented in developed countries for reducing self-poisoning suicides. Moreover, it seeks to explore their feasibility for implementation in LMICs. It also evaluates whether pharmacy gatekeeper training programs can emerge as a primary intervention strategy for preventing suicide by drug use.
2 Materials and methods
In this review, we analyzed the effectiveness of community pharmacy gatekeeper training as a suicide prevention intervention based on existing evidence. Additionally, we also reviewed other existing gatekeeper interventions to explore feasible self-poisoning prevention interventions appropriate for LMICs.
2.1 Rationale behind the study design selection
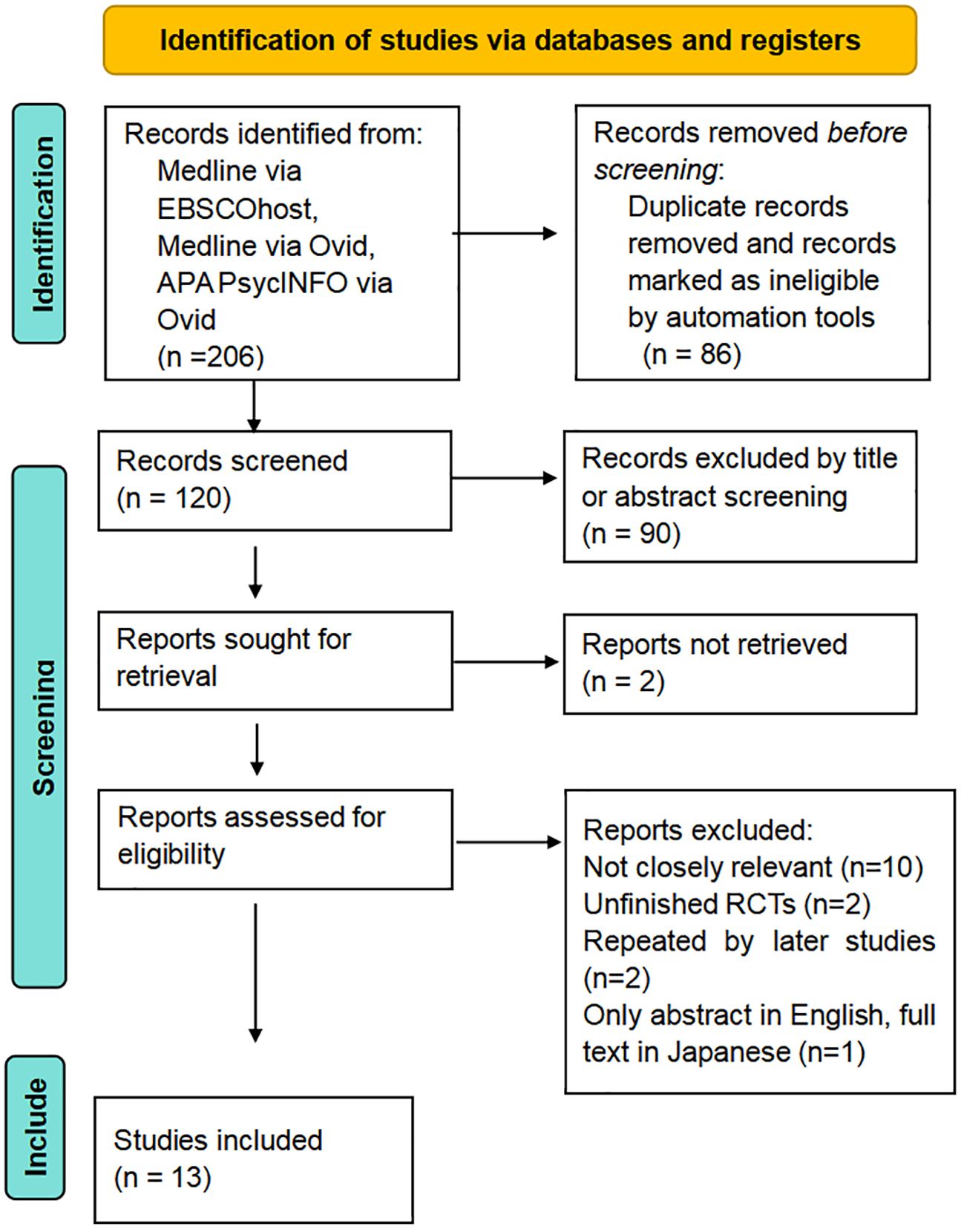
This article is a semi-systematic literature review, adopting a part of the systematic review checklist from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (17) to structure its methodological flow. Current research on the topic of “pharmacist gatekeeper interventions” has been conducted by teams of researchers from different disciplines, employing various approaches including both qualitative and quantitative. Thus, the heterogeneity in these studies limits a comprehensive systematic review and meta-analysis.
Semi-systematic evaluations may adopt a more flexible approach to study selection, data extraction, and synthesis. While they follow a structured process similar to that of a systematic review to search and select studies, but do not strictly adhere to all the rigorous methodological criteria of a formal systematic review. Therefore, the semi-systematic method was implemented.
2.2 Search strategy
Data were collected from various online libraries including PubMed, ScienceDirect, ClinicalKey, ProQuest, and Cochrane. The databases and search engines used for searching included Medline via Ovid, APA PsycINFO via Ovid, Medline via EBSCOHost, Google Scholar, and the University of Sydney (USYD) Library’s direct on-site search. The initial search used the keyword. “gatekeeper” OR “gatekeeping” OR “gatekeep”, combined with to the term “pharmacist” OR “pharmacy” using the Boolean operator AND.
The initial search was then combined using the operator (AND) with keywords “suicide” OR “self-poisoning”, “prevention” OR “intervention” respectively. Additionally, to identify records related to the implementation of the pharmacist gatekeeper interventions in LMICs, the initial search was further refined using (AND) with keywords “LMICs” OR “low- and middle-income countries” OR “low- and middle-income countries” OR “developed countries”. The search also included more specific terms for common LMIC regions, such as “Middle East”, “Asia”, “Africa”, “South America”, along with more specific country names such as “India”, “China”, “Cambodia”, “Sri Lanka”, “Nepal”, “Pakistan”, “Bangladesh”, etc.
2.3 Inclusion criteria
This study adhered to the inclusion criteria outlined in the Joanna Briggs Institute (JBI) Manual for Evidence Synthesis (17). The inclusion criteria include that the article must be in English, published between April 1, 2014, and April 1, 2024, contain an abstract, be available in scientific databases, and evaluate community pharmacist gatekeeper interventions. As several studies reported multiple bans of lethal pesticides before 2014 in many LMICs (18–20), these studies use 2014 as the end of their study periods. We believe that the effects of banning have not been relatively fully recognized and assessed by previous studies before this time point. As a result, recent 10 years window was chosen to minimize the confounding effects of pesticide bans and to include relatively up to date studies.
2.4 Definition: low- and middle-income countries
The World Bank Group classifies the world’s economies into four income groups: low-income, lower-middle income, upper-middle income, and high-income. The countries included in each classification are updated on July 1 of each year based on the previous year’s Gross National Income (GNI) per capita (21). The term LMICs (low- and middle-income countries) includes all low-income, lower-middle-income and upper-middle-income countries.
2.5 Definition: gatekeeper intervention
Suicide prevention “gatekeepers” are people who can contact individuals at high risk of suicide and have the opportunity to prevent suicides. At the societal level, gatekeeper interventions consist of educating individuals with the knowledge, skills and confidence to identify and support those at risk (8). In community pharmacy, gatekeeper interventions can also refer to specific proactive actions taken by community pharmacy staff, including identifying, communicating with, and assisting patients who present with warning signs of suicide (10).
2.6 Data analysis
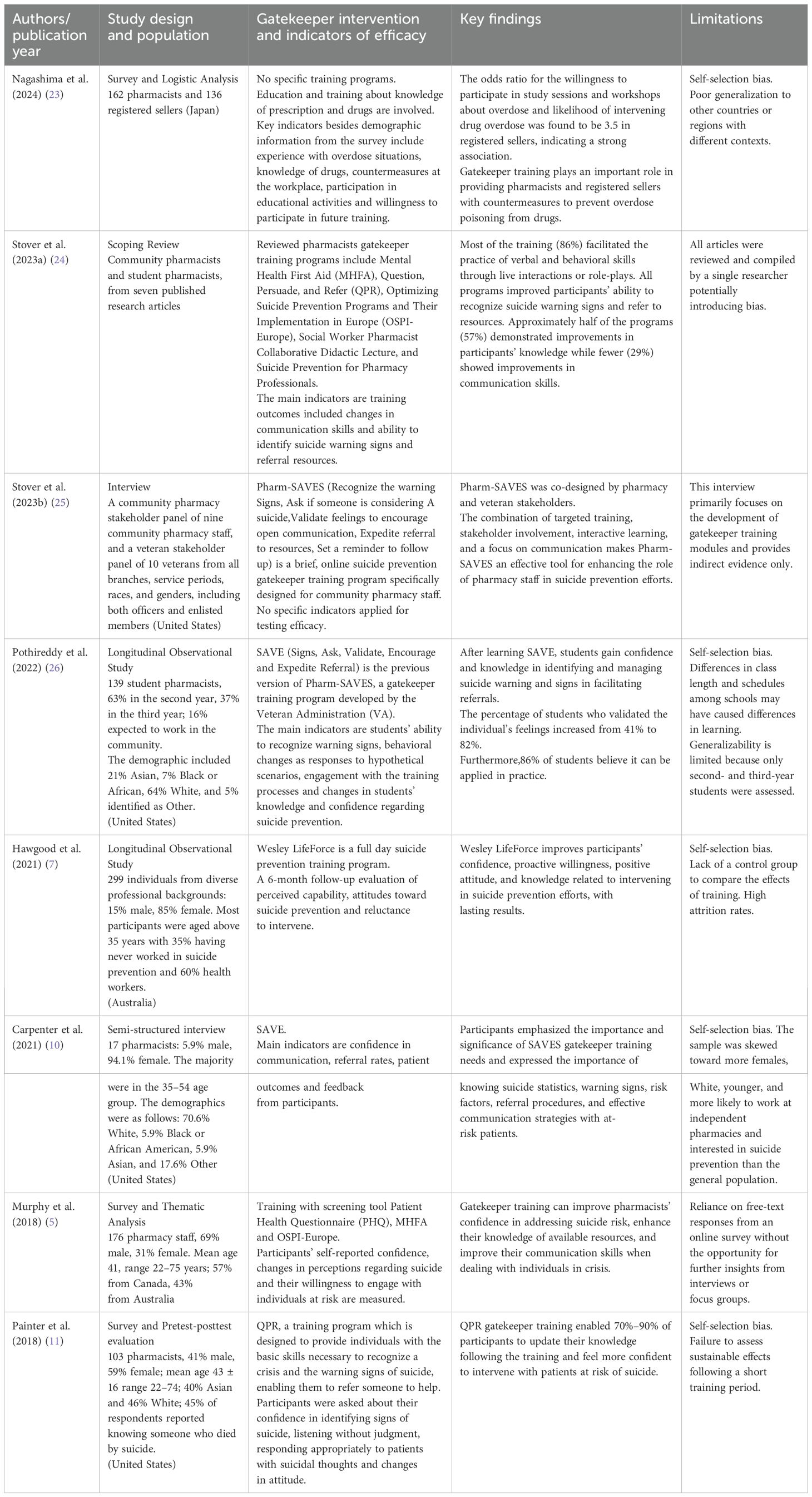
The screening of titles and abstracts was carried out by ZZ during the literature search and data analysis. Data were entered into a custom data extraction sheet (Table 1). The main information collected include participant characteristics, key concepts, primary results or conclusive outcomes, and the methodology and limitations used to evaluate the quality of the study.
In the absence of records establishing a statistical relationship between the implementation of pharmacist gatekeeper training programs and changes in suicide rates, qualitative indicators (attitude, knowledge, behaviors, etc.) were employed to assess the efficacy of these interventions in the countries where they were implemented. In this study, we focused on the narrative outcomes of the analyzed studies, for example, subjects’ perceptions of intervention strategies and changes in attitudes before and after their participation.
2.7 Ethics statement
According to ethics approval guidelines (22), the ethical review process is mandatory for designing, organizing, or conducting research that directly or indirectly involves patients. This literature review involved only the synthesis and analysis of published studies; no new research involving human subjects was conducted. Therefore, formal ethical approval was not sought. All sources of information are publicly available, and references were properly cited to respect the intellectual property rights of the original authors.
3 Results
Two hundred and six studies were identified through database searches (Figure 1). All 206 search results were integrated using the command ‘search with OR’ to remove duplicates, and some results were automatically excluded by database search engines after setting inclusion criteria. Subsequently, 120 studies were screened, and 28 of them were selected to assess their eligibility. Two sources could not be retrieved due to a lack of free online access, while 15 studies were excluded for reasons of inaccessibility, low relevance, and other factors. Ultimately, 8 studies were selected to summarize the pharmacy gatekeeper interventions (5, 7, 10, 11, 23–26), (Table 1). Five relevant studies were selected and evaluated to discuss the current profile of self-poisoning in LMICs (27–31).
Of the eight studies summarisedin Table 1, five were from the US, three from Australia, and one from Japan (two studies spanned two countries). Five studies recorded the gender and age, while three documented the ethnicity. Most participants were aged between 30 and 50 years. The participants included qualified pharmacists, student pharmacists, pharmacy technicians, registered sellers, pharmacy owners, and other pharmacy-related staff.
While current evidence on the effectiveness of pharmacist training programs originated primarily from developed countries, a significant gap remains in the literature with respect to adaptation and implementation of pharmacist gatekeeper training in the LMIC context. No relevant results found when combining the topic of pharmacist gatekeeper with any keywords referring to LMICs. However, we retained five studies that, although not directly addressing pharmacy gatekeeper interventions, examine drug-related suicide or explored appropriate methods of suicide prevention strategies in LMICs (27–31).
Pharmacy gatekeeper intervention strategies were consistently perceived as effective by the majority (86%) of participants across eight studies (24, 26). Training programs such as QPR, SAVE, Pharm-SAVES, and Wesley LifeForce enhanced participants’ ability to recognize warning signs, communicate effectively, and refer at-risk individuals (Table 1). For instance, SAVE increased validation of individuals’ feelings from 41% to 82% (26), and QPR achieved 70% to 90% confidence improvements among participants (11). Indicators for measuring the efficacy of interventions are mainly based on pharmacists’ subjective feelings such as changes in attitudes, increased self-confidence, and readiness to respond to suicidal intent. Other relatively objective ability indicators included expanded knowledge and improving pharmacists’ skills.
Only Nagashima et al. emphasized that pharmacists play a gatekeeper role in drug overdose situations, highlighting the need for both theoretical and practical education regarding lethal doses of pharmaceutical drugs and dangerous drug interactions (23). In other literature, the rationale for pharmacist gatekeeper training is not centered on withholding access to medicines but rather on their interactions with individuals at risk of suicide, as pharmacists are the most accessible health professionals to the public (24).
4 Discussion
4.1 Implications of the evidence for pharmacist gatekeeper interventions
Pharmacists did not play a role as a barrier to prevent pharmaceutical overdoses; rather, they assume on a role resembling that of a psychiatrist working in a pharmacy. It is noted that 80% of suicides in the US had contact with a healthcare provider in the year prior to death (30). Although we were unable to confirm whether such contacts were made to seek support for psychological problems or for other health problems, this data at least proves that there is frequent and close contact between health workers and individuals at-risk in developed countries, which presents the opportunity for prevention. This finding also suggests that the effectiveness of pharmacist gatekeeper interventions is highly dependent on the context of developed countries, where pharmacists have close contact individuals with suicidal risks. In LMICs, however, individuals at risk of suicide often do not receive adequate mental health support from pharmacy or healthcare system (15). Despite the broader role pharmacists have to play by positioning themselves as champions in suicide prevention interventions, implementing such interventions through community pharmacies may be limited in some rural and suburban areas of LMICs, where pharmacies are not widely available (31). Therefore, recommendations for applying the pharmacist gatekeeper training in LMICs must consider unique context and the current trends in self-poisoning in these countries.
Furthermore, although studies have demonstrated the efficacy of pharmacist gatekeeper interventions, “efficacy” reflects an increase in pharmacists’ ability to prevent patient suicides as a result of training, rather than a direct reduction in the number of suicides attributable to this strategy. The direct statistical effect of all gatekeeper keeper training programs on reducing suicide rates, however, remain (32). At the same time, many confounding factors, such as the impact of shifts in the economic environment, likely influence overall suicide rates (3). Thus, even in the context of studies conducted in developed countries, health economics data, such as the cost-effectiveness of pharmacy gatekeeper interventions, remain difficult to measure (33). Nonetheless, pharmacists still have a pivotal role to play in suicide prevention interventions.
4.2 The current role of pesticides bans in LMICs
For most countries globally, the most effective suicide prevention strategy involves prohibiting the use of lethal methods at the legislative level (27). Among all these approaches, restricting pesticides is generally considered the optimal option for LMICs. Banning highly hazardous pesticides could reduce suicide deaths by approximately 28,000 per year, at a cost of only 0.007 US dollars per capita annually (34). Current evidence indicates that safe storage methods were ineffective on the incidence of pesticide self-poisoning. In contrast, banning of highly toxic pesticides resulted in reduction in suicides without impacting agricultural output (35).
Due to the recent successful implementation of bans on lethal pesticides in some LMICs (12), researchers have predicted that the primary method of self-poisoning will shift from the use of lethal pesticides to medication overdoses, thereby highlighting the importance of community pharmacies. However, pesticide bans have not completely blocked access to toxic pesticides due to strong resistance from the industry (13, 35). Highly toxic pesticides, such as organophosphates and carbamates, rather than pharmaceuticals, remain the primary method of self-poisoning in LMICs (4). Most victims of poisoning used pesticides because they are not only more lethal but also more widely available, often stored in most households in both urban and rural areas (31). However, emerging trends in LMICs indicate a shift towards pharmaceutical self-poisoning as a result of restricted access to pesticides, highlighting a changing landscape of suicide methods that requires targeted interventions. At this stage, pharmacy gatekeeper interventions should serve as a complement pesticide bans rather than replacing them as the primary focus of suicide prevention intervention in developing countries.
4.3 Other gatekeeper interventions for suicide prevention in LMICs
Although LMICs do not have pharmacy gatekeeper interventions equivalent to those in developed countries, other existing gatekeeper interventions in developing countries may be able to serve as a reference for the localization of pharmacy gatekeeper interventions.
The school gatekeeper interventions in China are school education strategies aim to equip teachers, school staff, parents and peers with the skills to recognize the warning signs of students at risk of suicide, based on the idea that recognising suicide risk is key to suicide prevention (36). Because Chinese student population comes into contact with schools on a daily basis, school gatekeepers have an inherent advantage in preventing youth suicide, being able to recognize and deal with suicide risk signals at the first opportunity (37). This is similar to the advantage that pharmacies in developed countries of having frequent access to people at risk of suicide, which suggests that the application of pharmacy gatekeeper interventions in LMICs should first ensure that pharmacy services are able to radiate to living areas of targeted population.
In rural areas, pesticide sellers, rather than community pharmacy staff, often serve as gatekeepers in blocking access to chemical suicide (31, 38), thus a gatekeeper training intervention tailored for pesticide vendors may be applicable in these regions. Trained suppliers can serve as gatekeepers by limiting access to pesticides and by identifying and responding to high-risk individuals among customers (29). The two vendor-based interventions for restricting pesticide sales include selling pesticides only to farmers with identity cards or to customers with pesticide “prescriptions,” and selling low-toxicity products while providing counseling and asking customers to return the next day (28, 39). This is a combination of the pharmacy gatekeeper model and pesticide restriction policies. What we can learn from this is that the “pharmacist gatekeeper” who block lethal drugs do not necessarily have to be pharmacy staff, and that intervention strategies can also consider the channels through where drugs are actually sold in LMICs.
4.4 Limitations and strength
This literature review is semi-systematic due to its more flexible structure has some advantages of systematic reviews such as methodological rigor and transparency (40, 41). However, this study is prone to source selection bias and has limited comprehensiveness, as most studies are arbitrarily selected during the process. In addition, the results of studies evaluating the effectiveness of gatekeeper interventions have tend to rely on subjective indicators of attitude, knowledge, and confidence. As a narrative outcome, the efficacy observed is likely influenced by factors such as the placebo effect, measurement errors, and the social dynamics of attending training with peers rather than the course content itself, which can increase participants’ self-confidence. These confounding factors need to be considered when interpreting the results.
This literature review summarizes existing literature on pharmacy gatekeeper intervention strategies worldwide, providing a theoretical framework and preliminary background for future research in drug suicide prevention area. It explores the key role of pharmacists in community suicide prevention interventions and compares the requirements for suicide interventions in developed and developing countries. This study also provides key insights into how community pharmacy gatekeeper interventions can be appropriately modified to achieve effective and feasible outcomes in LMICs.
5 Conclusion
Pharmacist gatekeeper training programs offer a proactive approach and are effective in enhancing confidence, willingness, positive attitudes, knowledge, and readiness of pharmacists to identify and assist patients at risk of suicide. The value of pharmacists as suicide gatekeepers lies not only in controlling access to pharmaceuticals, but in their frequent interaction with individuals who may be at risk. Therefore, tailoring gatekeeper training programs to meet these specific needs of LMICs, rather than directly transferring models from high-income countries, is essential. However, significant gaps remain in quantitative research on the efficacy of gatekeeper training programs in LMICs where pharmacist led gatekeeper interventions studies are scarce. At this stage, there is a pressing need for holistic suicide prevention strategies in LMICs, combining effective measures such as pesticide bans with adaptable pharmacist gatekeeper training programs tailored to the local social context. Effective suicide prevention in LMICs requires integrating gatekeeper training and pesticide bans, conducting pilot studies on pharmacist interventions, and addressing broader social and systemic causes.
Author contributions
ZZ: Formal analysis, Methodology, Writing – original draft, Investigation, Visualization. FM: Project administration, Supervision, Validation, Writing – review & editing, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our gratitude to the School of Public Health, the University of Sydney for their support.
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could be perceived as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Suicide. Geneva, Switzerland: World Health Organization (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/suicide (Accessed March 20, 2024).
2. Dattani S R-GL, Ritchie H, Roser M, Ortiz-Ospina E. Suicides Online at OurWorldinData.org.: Our World in Data (2023). Available online at: https://ourworldindata.org/suicide (Accessed March 20, 2024).
3. Knipe D, Padmanathan P, Newton-Howes G, Chan LF, Kapur N. Suicide and self-harm. Lancet. (2022) 399:1903–16. doi: 10.1016/S0140-6736(22)00173-8
4. Albano GD, Malta G, La Spina C, Rifiorito A, Provenzano V, Triolo V, et al. Toxicological findings of self-poisoning suicidal deaths: A systematic review by countries. Toxics. (2022) 10:654. doi: 10.3390/toxics10110654
5. Murphy AL, Ataya R, Himmelman D, O’Reilly C, Rosen A, Salvador-Carulla L, et al. Community pharmacists’ Experiences and people at risk of suicide in Canada and Australia: A thematic analysis. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:1173–84. doi: 10.1007/s00127-018-1553-7
6. Kamal L, Jacob SA. Pharmacists’ Experiences, perceptions, and attitudes towards suicide and suicide prevention: A scoping review. Pharm (Basel). (2023) 11:25. doi: 10.3390/pharmacy11010025
7. Hawgood J, Koo YW, Sveticic J, De Leo D, Kolves K. Wesley lifeforce suicide prevention gatekeeper training in Australia: 6 month follow-up evaluation of full and half day community programs. Front Psychiatry. (2020) 11:614191. doi: 10.3389/fpsyt.2020.614191
8. Holmes G, Clacy A, Hermens DF, Lagopoulos J. The long-term efficacy of suicide prevention gatekeeper training: A systematic review. Arch Suicide Res. (2021) 25:177–207. doi: 10.1080/13811118.2019.1690608
9. Choi NG, Marti CN, Choi BY. Three leading suicide methods in the United States, 2017-2019: associations with decedents’ Demographic and clinical characteristics. Front Public Health. (2022) 10:955008. doi: 10.3389/fpubh.2022.955008
10. Carpenter DM, Roberts CA, Lavigne JE, Cross WF. Gatekeeper training needs of community pharmacy staff. Suicide Life Threat Behav. (2021) 51:220–8. doi: 10.1111/sltb.12697
11. Painter NA, Kuo GM, Collins SP, Palomino YL, Lee KC. Pharmacist training in suicide prevention. J Am Pharm Assoc (2003). (2018) 58:199–204.e2. doi: 10.1016/j.japh.2017.12.007
12. Eddleston M. Banning toxic pesticides is effective at preventing suicides in south asia. BMJ. (2023) 382:1838. doi: 10.1136/bmj.p1838
13. Bonvoisin T, Utyasheva L, Knipe D, Gunnell D, Eddleston M. Suicide by pesticide poisoning in India: A review of pesticide regulations and their impact on suicide trends. BMC Public Health. (2020) 20:251. doi: 10.1186/s12889-020-8339-z
14. Scholin L, Knipe D, Bandara P, Eddleston M, Sethi A. Banning highly hazardous pesticides saves the lives of young people, particularly females, in low- and middle-income countries. BMC Public Health. (2023) 23:2249. doi: 10.1186/s12889-023-17071-y
15. Tibebe A, Tesfay K. Public knowledge and beliefs about mental disorders in developing countries: A review. J Depression Anxiety. (2015) s3. doi: 10.4172/2167-1044.S3-004
16. Kopinak JK. Mental health in developing countries: challenges and opportunities in introducing western mental health system in Uganda. Int J MCH AIDS. (2015) 3:22–30.
17. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
18. Sarkar S. Despite historic bans, south asia still struggles with pesticide suicides. BMJ. (2023) 381:678. doi: 10.1136/bmj.p678
19. Weerasinghe M, Pearson M, Konradsen F, Agampodi S, Sumith JA, Jayamanne S, et al. Emerging pesticides responsible for suicide in rural Sri Lanka following the 2008-2014 pesticide bans. BMC Public Health. (2020) 20:780. doi: 10.1186/s12889-020-08871-7
20. Chowdhury FR, Dewan G, Verma VR, Knipe DW, Isha IT, Faiz MA, et al. Bans of who class I pesticides in Bangladesh-suicide prevention without hampering agricultural output. Int J Epidemiol. (2018) 47:175–84. doi: 10.1093/ije/dyx157
21. World Bank. How Does the World Bank Classify Countries? Washington, DC, USA: World Bank Data Help Desk (2019). Available at: https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries (Accessed August 21, 2024).
23. Nagashima K, Hiruma K, Nakamura E, Watanabe M, Sekine Y. Identification of factors necessary for gatekeeper of overdose. Biol Pharm Bull. (2024) 47:112–9. doi: 10.1248/bpb.b23-00530
24. Stover AN, Lavigne JE, Carpenter DM. A scoping review of suicide prevention training programs for pharmacists and student pharmacists. Am J Pharm Educ. (2023) 87:ajpe8917. doi: 10.5688/ajpe8917
25. Stover AN, Lavigne JE, Shook A, MacAllister C, Cross WF, Carpenter DM. Development of the pharm-saves educational module for gatekeeper suicide prevention training for community pharmacy staff. Health Expect. (2023) 26:1246–54. doi: 10.1111/hex.13741
26. Pothireddy N, Lavigne JE, Groman AS, Carpenter DM. Developing and evaluating a module to teach suicide prevention communication skills to student pharmacists. Curr Pharm Teach Learn. (2022) 14:449–56. doi: 10.1016/j.cptl.2022.02.002
27. Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. (2016) 3:646–59. doi: 10.1016/S2215-0366(16)30030-X
28. Weerasinghe M, Konradsen F, Eddleston M, Pearson M, Jayamanne S, Gunnell D, et al. Vendor-based restrictions on pesticide sales to prevent pesticide self-poisoning - a pilot study. BMC Public Health. (2018) 18:272. doi: 10.1186/s12889-018-5178-2
29. Weerasinghe M, Pearson M, Turner N, Metcalfe C, Gunnell DJ, Agampodi S, et al. Gatekeeper training for vendors to reduce pesticide self-poisoning in rural south asia: A study protocol for a stepped-wedge cluster randomised controlled trial. BMJ Open. (2022) 12:e054061. doi: 10.1136/bmjopen-2021-054061
30. Lavigne JE, Stover AN, Gamble A, Tudor G, Cross WF, Carpenter DM. A randomized controlled trial protocol for a virtual, scalable suicide prevention gatekeeper training program for community pharmacy staff (Pharm-saves). Contemp Clin Trials Commun. (2024) 38:101268. doi: 10.1016/j.conctc.2024.101268
31. Shekhani SS, Perveen S, Hashmi DE, Akbar K, Bachani S, Khan MM. Suicide and deliberate self-harm in Pakistan: A scoping review. BMC Psychiatry. (2018) 18:44. doi: 10.1186/s12888-017-1586-6
32. Yonemoto N, Kawashima Y, Endo K, Yamada M. Gatekeeper training for suicidal behaviors: A systematic review. J Affect Disord. (2019) 246:506–14. doi: 10.1016/j.jad.2018.12.052
33. Ahern S, Burke LA, McElroy B, Corcoran P, McMahon EM, Keeley H, et al. A cost-effectiveness analysis of school-based suicide prevention programmes. Eur Child Adolesc Psychiatry. (2018) 27:1295–304. doi: 10.1007/s00787-018-1120-5
34. Lee YY, Chisholm D, Eddleston M, Gunnell D, Fleischmann A, Konradsen F, et al. The cost-effectiveness of banning highly hazardous pesticides to prevent suicides due to pesticide self-ingestion across 14 countries: an economic modelling study. Lancet Glob Health. (2021) 9:e291–300. doi: 10.1016/S2214-109X(20)30493-9
35. Eddleston M, Gunnell D. Preventing suicide through pesticide regulation. Lancet Psychiatry. (2020) 7:9–11. doi: 10.1016/S2215-0366(19)30478-X
36. Cai C, Yin C, Tong Y, Qu D, Ding Y, Ren D, et al. Development of the life gatekeeper suicide prevention training programme in China: A delphi study. Gen Psychiatr. (2023) 36:e101133. doi: 10.1136/gpsych-2023-101133
37. Cai C, Qu D, Liu D, Liu B, Zhang X, Chen P, et al. Effectiveness of a localised and systematically developed gatekeeper training program in preventing suicide among chinese adolescents. Asian J Psychiatr. (2023) 89:103755. doi: 10.1016/j.ajp.2023.103755
38. Weerasinghe M, Jobe L, Konradsen F, Eddleston M, Pearson M, Jayamanne S, et al. Differences in the characteristics of people who purchase pesticides from shops for self-harm versus those who use pesticides available in the domestic environment in Sri Lanka. Trop Med Int Health. (2023) 28:901–11. doi: 10.1111/tmi.13941
39. Weerasinghe M, Konradsen F, Eddleston M, Pearson M, Jayamanne S, Gunnell D, et al. Potential interventions for preventing pesticide self-poisoning by restricting access through vendors in Sri Lanka. Crisis. (2018) 39:479–88. doi: 10.1027/0227-5910/a000525
40. Snyder H. Literature review as a research methodology: an overview and guidelines. J Business Res. (2019) 104:333–9. doi: 10.1016/j.jbusres.2019.07.039
Keywords: suicide prevention, gatekeeper training, community pharmacist, self-poisoning, LMICs
Citation: Zhou Z and Mohamed F (2025) Pharmacist gatekeeper interventions for suicide prevention: how evidence from developed countries support their role in low- and middle-income countries. Front. Psychiatry 15:1508621. doi: 10.3389/fpsyt.2024.1508621
Received: 09 October 2024; Accepted: 26 December 2024;
Published: 28 January 2025.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Samuel McKay, The University of Melbourne, AustraliaCopyright © 2025 Zhou and Mohamed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fahim Mohamed, ZmFoaW0uY2FkZXJAc3lkbmV5LmVkdS5hdQ==
 Zixiao Zhou
Zixiao Zhou Fahim Mohamed
Fahim Mohamed