- 1Wuxi School of Medicine, Jiangnan University, Wuxi, China
- 2Department of Intensive Care Unit, Wuxi No.2 People’s Hospital (Jiangnan University Medical Center), Wuxi, China
- 3Department of General Surgery, Wuxi No.2 People’s Hospital (Jiangnan University Medical Center), Wuxi, China
- 4Department of Infection Management, Wuxi No.2 People’s Hospital (Jiangnan University Medical Center), Wuxi, China
Objective: In this study, we examine the network structure of posttraumatic stress disorder (PTSD), including core symptoms and strong edges in patients undergoing chemotherapy for colorectal cancer in China, and lay the groundwork for targeted psychological interventions for these patients.
Methods: This study included 360 colorectal cancer patients receiving chemotherapy at a third-class hospital in Wuxi, China, from November 2023 to June 2024. The severity of each item of PTSD was assessed using the DSM-5 Checklist (PCL-5). A network analysis approach was conducted in R to pinpoint core symptoms and investigate notable edge connections within the network.
Results: The accuracy and stability of the PTSD network structure model were relatively good, and the results indicated that robust connections emerged between avoidance of thoughts and avoidance of reminders, hypervigilance and exaggerated startle response, and loss of interest and detachment. The most central node was emotional cue reactivity, which was more closely connected with other symptoms, while self-destructive/reckless behavior was the lowest central node.
Conclusion: Emotional cue reactivity was proved to be the most prominent symptom in the PTSD symptom network in colorectal cancer patients treated with chemotherapy, and targeting it in interventions could lead to substantial improvements.
1 Introduction
Colorectal cancer (CRC), recognized as a malignant tumor, is one of the most common cancers in the world. In 2022, the global incidence of new CRC cases accounted for 10.7% of all cancer types, making it the second most common cause of cancer-related mortality, following lung cancer (1). Moreover, CRC incidence and mortality rates in China continue to rise, surpassing the global average (2). After experiencing a series of significant stressors, including a cancer diagnosis and chemotherapy, CRC patients often encounter negative emotions (3), such as depression and anxiety. They may even develop posttraumatic stress disorder (PTSD) (4). Research has reported that the positive rate of PTSD in CRC patients ranges from 11.2% to 32.3% (5, 6). PTSD mainly manifests in intrusive traumatic experiences, avoidance, negative cognitive and emotional changes, and persistent hypervigilance (4). Under prolonged psychological stress from traumatic events, PTSD patients may experience infections (7), pain (8), somatic symptoms (9), and changes in systemic immune function, which seriously affect their quality of life and prognosis (10).
PTSD clinical symptoms are diverse, with their interactions potentially influencing the progression of the disorder (11). Previous research often treated PTSD as a whole (12, 13), assuming that all symptoms or items of PTSD are equally important. Researchers typically use the total symptom score to assess the severity and as an indicator of treatment effectiveness, ignoring the complex links and interactions among the symptoms.
Network analysis is a research approach to investigating and comprehending the symptoms (nodes)within a network and the relationships (edges)that connect them. It shifts the focus from the disease to the uniqueness of each symptom and its internal connections (14). Through network analysis, we plan to identify the most influential central symptoms and strongly associated edges, expecting that this will help to reveal the underlying structure of disease symptoms and enhance our understanding of how symptoms interact (15).
To date, network analysis has become more prevalent in examining PTSD symptoms (16–18). Individuals who have experienced similar traumatic events display specific shared response patterns, which may create a tightly linked PTSD network, increasing their vulnerability to developing PTSD (17). It is important to note that various types of trauma and demographic groups can result in differences in the features of the network framework (16, 19–21). For example, hypervigilance frequently appears as the primary symptom among adults who have suffered from sudden natural disasters like earthquakes (21). In veterans exposed to war environments, the core PTSD symptoms are flashbacks and emotional cue reactivity (19).
Currently, the network structure and core symptoms of PTSD in Chinese colorectal cancer patients in chemotherapy treatment remain unclear. Given that the network characteristics of PTSD vary by type of trauma and population, this suggests that findings from previous studies may not apply to the colorectal cancer group. Therefore, we will carry out network research on PTSD in colorectal cancer patients to explore their unique response patterns.
2 Methods
2.1 Participants
This research utilized a convenience sampling method involving CRC individuals who fulfilled the following criteria. The study occurred in the general surgery and oncology wards of a tertiary medical facility in Wuxi, Jiangsu Province, China, from November 2023 to June 2024. According to the sample size estimation of network analysis, In a twenty-node network, 210 parameters (twenty threshold parameters and 20×19/2 = 190 pairwise association parameters) need to be estimated (22). Therefore, the minimum sample size required for this study is 210 cases. This research received approval from the Ethics Committee at Wuxi No.2 People’s Hospital (Ethics number: 2023Y-172). Participation was voluntary, and consent was obtained from all participants. The criteria for inclusion were: 1) a diagnosis of colorectal cancer; 2) aged 18 years or older and sufficiently clear-minded to possess basic reading comprehension skills; 3) currently undergoing chemotherapy; 4) aware of their diagnosis and condition and willing to participate in the research. The criteria for exclusion were: 1) cancer diagnosis not exceeding one month; 2) history of mental illness; 3) presence of severe comorbidities that hinder cooperation (such as ardiac, pulmonary or renal insufficiency); 4) experience of other significant traumatic events in the past six months (such as natural disasters or loss of a close relative); 5) presence of other malignant tumors; 6) currently participating in other intervention studies.
During the study, the researcher explained the study’s objective to participants, gathered their consent, and distributed paper questionnaires. The researcher offered standardized guidance to assist participants with questions during the questionnaire’s completion. Once the questionnaire was filled out, the researcher promptly gathered and reviewed the questionnaires. A total of 378 questionnaires were distributed. After excluding 7 patients with a psychiatric history, 3 patients who had experienced other traumatic events within the past six months, and 8 patients with other malignant tumors, 360 valid responses were collected.
2.2 Measures
2.2.1 Demographics and disease characteristics
A self-report questionnaire was used to collect sociodemographic and clinical information. (For example, gender, age, occupational status, marital status, educational level, place of residence, monthly household income, tumor type, cancer stage, enterostomy, surgery, radiotherapy, and length of diagnosis).
2.2.2 The PTSD checklist for DSM-5(PCL-5)
Consisting of 20 items, the PTSD Checklist for DSM-5 (PCL-5) is a self-report measure that evaluates PTSD symptoms based on DSM-5 criteria (23). In this study, we used the Mandarin version of the PCL-5 (24), which has a Cronbach’s α of 0.881. This tool evaluates four PTSD symptom clusters defined by the DSM-5: intrusions, avoidance, negative alterations in cognition and mood (NACM), and hyperarousal. Participants used a 5-point Likert scale, from 0 (not at all) to 4 (significantly). They rated how much specific symptoms had affected them over the past month. Scores can vary from 0 to 80, where a score of 33 or higher indicates significant PTSD and serves as a diagnostic reference.
2.3 Data analysis
We conducted descriptive statistics for demographic characteristics, clinical information, and PTSD scores using SPSS 29.0. Next, we conducted symptom network estimation, centrality measurement, and accuracy and stability assessments using R packages in R version 4.4.1.
2.3.1 Network estimation
Performed with the qgraph package in R was the estimation of the PTSD network. The Least Absolute Shrinkage and Selection Operator (LASSO) regression, combined with the Extended Bayesian Information Criterion (EBIC), was utilized to shrink the edges in the network (25). This approach aimed to remove relatively weak connections, enhancing the sparsity and clarity of the symptom network and making the results easier to interpret. Shorter and thicker edges in the network represent stronger associations between nodes. Blue edges signify positive correlations, while red edges denote negative correlations.
2.3.2 Centrality measurements
Each node’s expected influence, strength, closeness, and betweenness were computed using the qgraph package in R. Expected influence indicates the aggregate of the edge weights that connect a node to its adjacent nodes, accounting for positive and negative associations (15). Strength refers to the total absolute values of edge weights tied to that node, demonstrating the degree of direct connections. Closeness and betweenness reflect the extent of indirect connections for the node. This study will focus on the expected influence metric, the most reliable, stable, and accurate indicator compared to other centrality measures (18). Higher EI represents the node’s increased centrality, signifying its greater importance.
2.3.3 Stability and accuracy analysis
The stability and accuracy of the networks were analyzed through the bootnet package in R. First, accuracy was estimated by calculating 95% confidence intervals (CIs) using non-parametric bootstrapping (nBoots = 1000). Narrower CIs indicate more reliable edge weight estimates, while less overlap between CIs suggests greater accuracy in the network edge weights (22). Subsequently, the stability of the centrality measures was evaluated by calculating the Correlation Stability Coefficient (CS-C) through the subset bootstrap method. The CS-C reflects the highest percentage of cases that can be omitted while maintaining a correlation with 95% confidence, with a value ideally above 0.50 and not lower than 0.25 to ensure stability (26).
3 Results
3.1 Sample descriptive
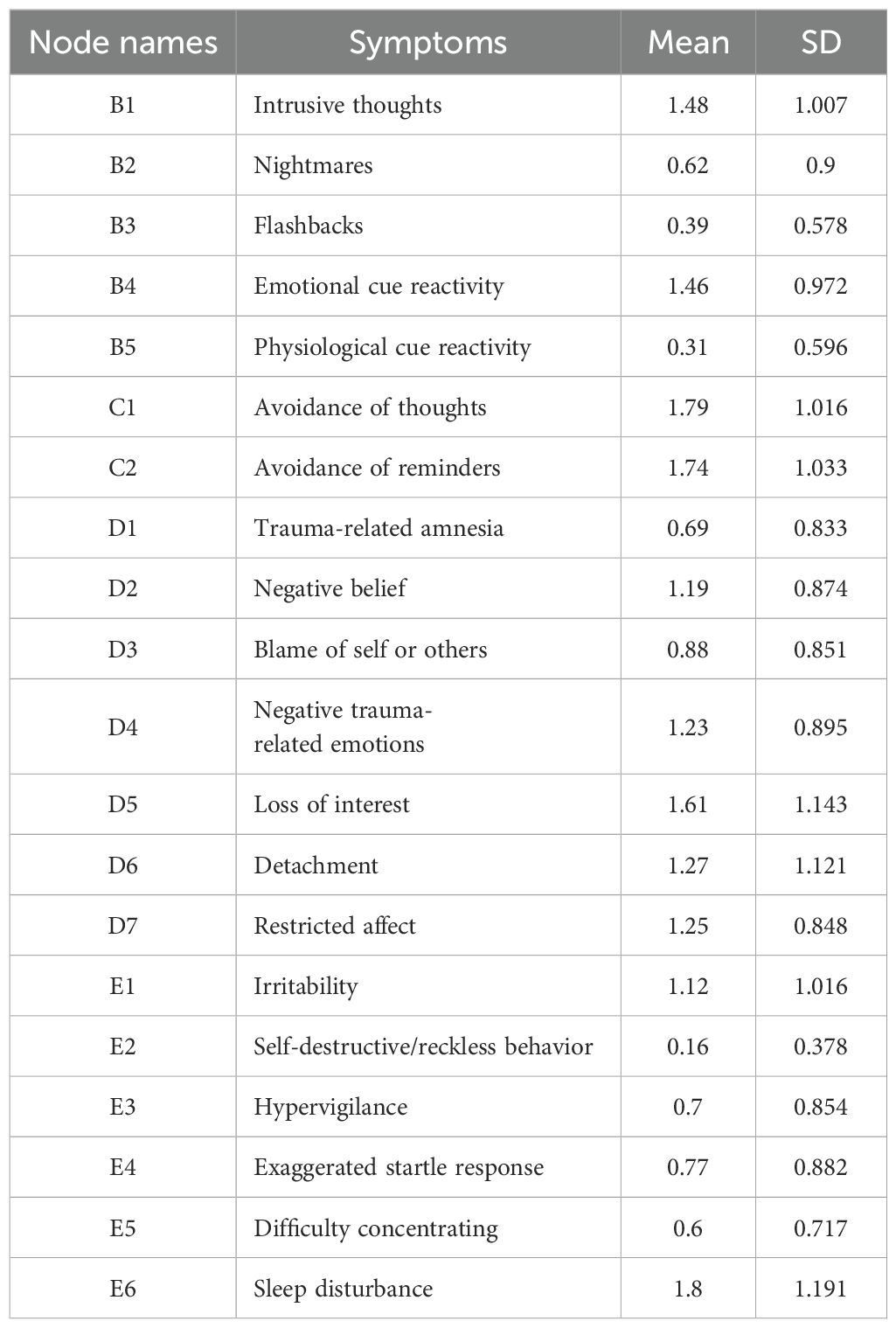
Table 1 shows the participants’ characteristics. A total of 360 colorectal cancer chemotherapy patients participated in this study, with males accounting for 55.6% (200 cases) and females for 44.4% (160 cases). The mean age of the patients was 66.39 ± 10.46 years. (see Table 1 for details). The PCL-5 score for these patients was 21.07 ± 10.15, with 52 patients (14.4%) scoring ≥33 on the PCL-5. The scores for each scale item are shown in Table 2.
3.2 The network estimation
Figure 1 shows the network structure diagram of PTSD in chemotherapy patients with colorectal cancer, which includes 20 nodes and a total of 85 non-zero edges (network density is 0.45) with an average edge weight of 0.044. There are 79 positive blue edges (93%) and 6 negative red edges (7%)—A more robust correlation exists when the lines connecting two network nodes are shorter and thicker. The associations of symptoms within dimensions are slightly more potent than those between dimensions. The strongest edge weights in the network structure appear between avoidance of thoughts(C1) and avoidance of reminders(C2)(edge = 0.85), hypervigilance(E3) and exaggerated startle response(E4)(edge = 0.66) and loss of interest(D5) and detachment(D6)(edge = 0.40).
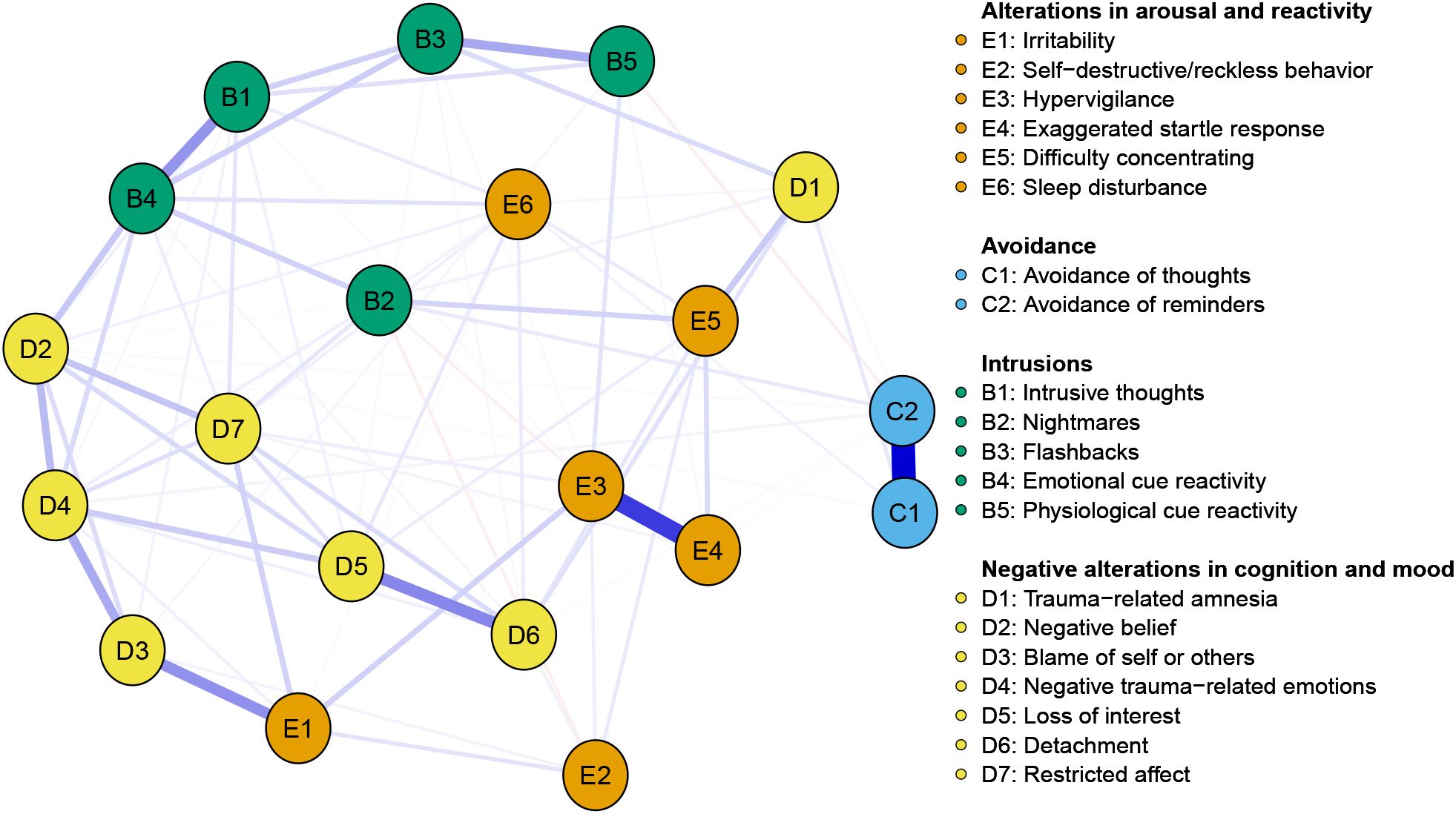
Figure 1. Network structure model of colorectal cancer patients receiving chemotherapy. The blue edges represent positive correlations, and the red represents negative correlations. Edge thickness represents the strength of the connection between symptoms.
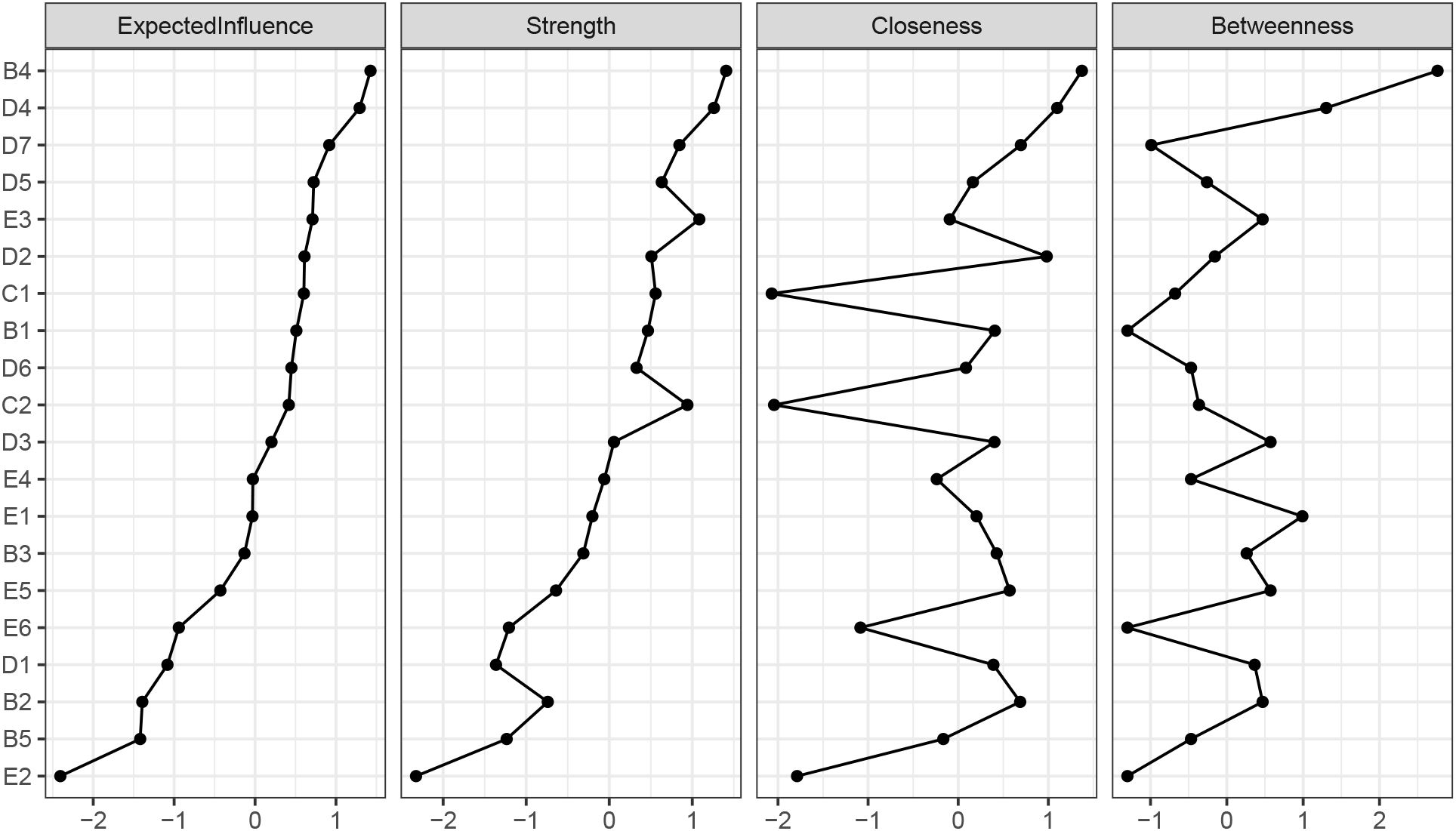
Figure 2 illustrates that emotional cue reactivity (B4) has the highest expected influence (EI =1.18), followed by negative trauma-related emotions (D4) (EI = 1.14) and restricted affect (D7) (EI = 1.05). These results indicate that these symptoms are critical components in the network, while the symptom with the lowest expected influence is self-destructive/reckless behavior (E2) (0.25).
Figure 3A demonstrates partial overlap between the 95% confidence intervals of the edge weights obtained through non-parametric bootstrapping. At the same time, the absence of overlap in the confidence intervals for some of the strongest edges indicates a relatively precise evaluation of the edge weights. Figure 3B shows that the network stability is good, with the stability of expected influence, strength, closeness, and mediation centrality being 0.672, 0.672, 0.594, and 0.283, respectively. A stability coefficient for EI greater than 0.50 indicates that the central symptoms retain stability, even with fewer samples or nodes during network re-estimation.
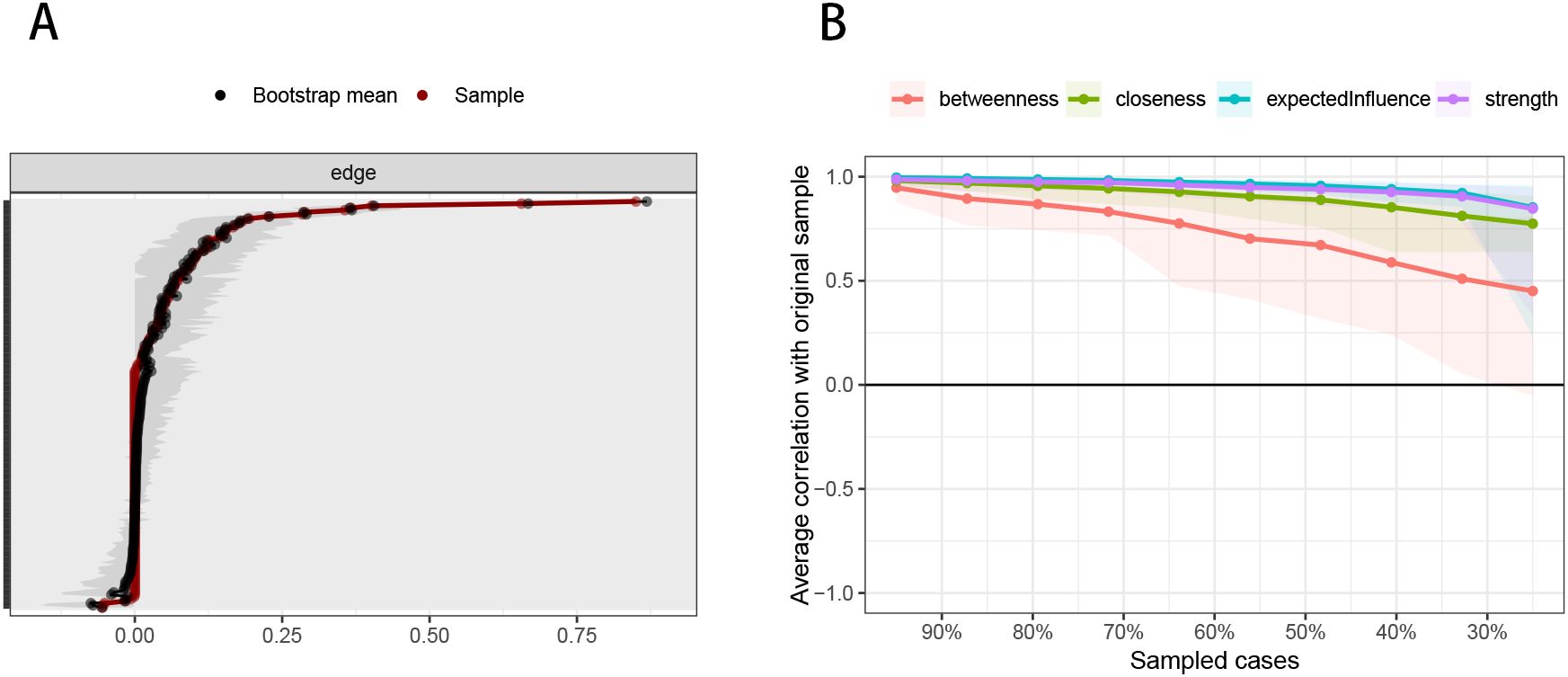
Figure 3. Accuracy and stability of network structure model. (A) Accuracy analysis of edge weights. (B) Stability analysis of centrality indicators.
4 Discussion
To our knowledge, this is the first study to conduct a PTSD network analysis among colorectal cancer patients treated with chemotherapy in China. The findings reveal a comparatively compact PTSD network, where symptoms are highly correlated. In our study, strong positive connections often occur among nodes within the same dimension (27–29), which aligns with the concept of PTSD in the DSM-5. The most central symptom is emotional cue reactivity, while the slightest central symptom is self-destructive/reckless behavior.
The results of this study’s symptom network analysis revealed the most vital edge between the symptoms of avoidance of thoughts(C1) and avoidance of reminders(C2), which is in agreement with prior studies (17, 29, 30). PTSD symptoms are often triggered by situational and environmental factors (31). To alleviate their distress, patients who have experienced trauma tend to avoid thoughts, feelings, and places that remind them of the traumatic event, such as recalling the details of the illness or hospital scenes (32). Consequently, the association between avoidance of thoughts and reminders is strengthened. Avoidance is a defense strategy against intense stimuli to temporarily ease perceived distress, accomplishing this by diminishing central nervous system activity (33). However, when avoidance is prolonged, it can lead to heightened adverse cognitive and emotional reactions, ultimately worsening mental states and hindering executive functioning (17).
The strong association between the symptoms of hypervigilance (E3) and exaggerated startle response (E4) aligns with findings from previous PTSD network research (16, 28, 31, 34). Individuals who have been through trauma tend to be more sensitive and vulnerable to triggering events or similar stimuli, a pattern that follows a sensitization model of PTSD (31, 35). As the disease advances, the physical symptoms caused by cancer and its treatment become more severe (36), and patients perceive an intensified threat from cancer (37). Therefore, hypervigilance and exaggerated startle responses reinforce each other (29). Research has shown that trauma-induced prolonged hypervigilance not only disrupts the hippocampus’s ability to function in learning and memory (38) but also impairs emotional and cognitive regulation (17), reducing the person’s ability to face trauma and contributing to the development of PTSD (16, 39).
There is also a strong connection between the symptoms of loss of interest (D5) and detachment (D6), slightly differing from previous studies (40, 41), which found only a moderate association between these symptoms. This discrepancy may relate to the types of trauma examined. For instance, Bryant et al. (41) focused on PTSD resulting from mixed trauma types, such as traffic accidents and assaults, while our research centers on the trauma of a cancer diagnosis. A cancer diagnosis may lead patients to trigger a loss of meaning and purpose in their lives (42), resulting in decreased interest in enjoyable activities, reduced social engagement, and alienation from others (43). As a result, the connection between loss of interest and detachment is strengthened. Additionally, some colorectal cancer patients who have a stoma may feel shame due to changes in their bowel movements, leading them to avoid social interactions (44).
Given the connections between the symptoms above, future healthcare professionals should focus on the associations between avoidance of thoughts and avoidance of reminders, hypervigilance and exaggerated startle response, and loss of interest and detachment. Preventive identification of these vital links can serve as a starting point, combined with early psychological interventions and pharmacotherapy, to weaken the interactions between symptoms, disrupt these strong associations, and improve intervention outcomes. Caregivers should also assist patients in understanding their illness and treatment process, explaining that symptoms such as avoidance and hypervigilance are common stress responses. Techniques like relaxation training and cognitive behavioral therapy (CBT) can alleviate the patients’ psychological stress (45). Patients should be encouraged to participate in social activities actively, rediscover new meanings and goals in life, and rebuild self-confidence, thereby effectively controlling the development of PTSD.
In addition to the edges, emotional cue reactivity (B4) was identified as the most central symptom in the PTSD network of colorectal cancer patients in chemotherapy treatment based on our findings. The core symptom is not aligned with Peters et al. (46), which identified hypervigilance as the central symptom. This variation could stem from the different types of trauma involved, as our research concentrates on patients dealing with the threat of illness. In contrast, Peters et al. examined trauma resulting from an earthquake, a natural disaster. The conditioning theories of PTSD suggest that emotional responses to emotional cue reactivity following exposure to traumatic events are common reactions (47, 48). Individuals develop various associations due to fear, matching trauma-related cues with associated stimuli through classical conditioning (49). As a result, these cues can evoke distressing emotional responses, even in the absence of immediate danger (48). Fear of disease progression in colorectal cancer patients can undermine cognitive abilities and intensify negative beliefs (37). This fear makes it challenging for individuals to shift their attention away from cancer-related cues, leading to increased rumination about these cues (50). Therefore, interventions by healthcare providers aimed at addressing emotional cue reactivity may lead to a more significant reduction in overall PTSD levels. Additionally, future research could explore the influencing factors of this symptom to enable precise interventions, promote psychological recovery, and further reduce PTSD levels.
Interestingly, this study found that the symptom with the lowest centrality is self-destructive/reckless behavior (E2). This finding contrasts with those of most other studies (27, 31, 51), which identified trauma-related amnesia as consistently exhibiting the lowest centrality. This distinction may be attributed to variations in sample size and the interactions between symptoms. Birkeland and Heir noted that intrusive symptoms can lead patients to repeatedly recall their trauma, potentially reducing trauma-related amnesia (52). In our study, intrusive symptoms emerged as the most central symptom, which may have influenced the severity of trauma-related amnesia. Conversely, in the research conducted by Spiller et al. (53), self-destructive/reckless behavior was identified as the most significant symptom. This contradiction may be related to the smaller sample size in Spiller et al.’s study, which may affect the reliability of their findings.
5 Strengths and limitations
The advantage of this study is that it is the first to network the PTSD symptoms of colorectal cancer patients undergoing chemotherapy in China. Early identification of these central symptoms may effectively block the progression of other symptoms and reduce the severity of PTSD in patients. Furthermore, given that the PCL-5 is derived from the model of DSM-5, we also observed that the strongly associated clusters (such as C1-C2, E3-E4, D5-D6) are consistent with the conceptual framework of DSM-5, which can provide a supplementary perspective for the classification and multi-dimensional models of mental disorders. Mainly through network analysis methods, it uncovers potential causal relationships between symptoms, providing a valuable reference for promoting patients’ psychological recovery.
Of course, this study also has certain limitations. First, it is a cross-sectional study that provides a fixed view of the PTSD symptom network among chemotherapy-treated colorectal cancer patients, thus failing to capture the dynamic changes of the network over time. Second, we did not carry out subgroup analyses (such as the PTSD group and the non-PTSD group, different age groups, different gender groups, etc.). Therefore, it is difficult for us to determine whether the relationships and patterns observed in the overall sample would still hold in this potentially specific subgroup. Third, the study relied on self-reported questionnaires to assess patients’ PTSD symptoms, which may introduce recall bias. Fourth, the research was conducted solely among colorectal cancer patients in China, so the generalizability of the findings may be limited and should be applied cautiously to other cultural contexts and cancer types. We recommend that future research employ longitudinal data to track the PTSD symptom network among colorectal cancer patients undergoing chemotherapy. Moreover, subgroup analyses ought to be taken into account to offer a more refined perspective. Also, using structured clinical interviews rather than self-reported questionnaires may assist in minimizing recall bias. Subsequently, investigations should be carried out in a wide range of cultural backgrounds and cancer varieties to guarantee the wider generalizability of the results.
6 Conclusions
This study reveals the PTSD symptom network structure among colorectal cancer patients undergoing chemotherapy in China. The findings show the most substantial connection between avoidance of thoughts and avoidance of reminders. Moreover, emotional cue reactivity is the most central symptom. We suggest that clinicians should prioritize these central symptoms and their strong interconnections. Targeted interventions based on these network characteristics could improve PTSD management and promote the mental health of patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Wuxi No.2 People’s Hospital Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YZ: Data curation, Investigation, Writing – original draft, Writing – review & editing. WT: Data curation, Writing – review & editing. LL: Supervision, Writing – review & editing. PZ: Supervision, Writing – review & editing. GF: Supervision, Writing – review & editing. HL: Data curation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our deep appreciation to everyone who contributed to this study.
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest. Author Contributions
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, et al. Global cancer statistics 2022: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2024) 74:229–63. doi: 10.3322/caac.21834
2. Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, et al. Cancer incidence and mortality in China, 2022. J Natl Cancer Cent. (2024) 4:47–53. doi: 10.1016/j.jncc.2024.01.006
3. Antoniadis D, Giakoustidis A, Papadopoulos V, Fountoulakis KN, Watson M. Quality of life, distress and psychological adjustment in patients with colon cancer. Eur J Oncol Nurs. (2024) 68:102467. doi: 10.1016/j.ejon.2023.102467
4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5™, 5th ed. TX: American Psychiatric Association (2013).
5. Lin YH, Kao CC, Pan IJ, Liu YH. Lower urinary symptoms, resilience, and post-traumatic stress symptoms among rectal cancer patients after surgery. Jpn J Nurs Sci. (2020) 17:e12320. doi: 10.1111/jjns.12320
6. Acevedo-Ibarra JN, Juárez-García DM, Espinoza-Velazco A, Buenaventura-Cisneros S, Téllez A. Post-traumatic stress symptoms, distress, and optimism in mexican colorectal cancer patients. Psychol Russ. (2022) 15:127–39. doi: 10.11621/pir.2022.0408
7. Song H, Fall K, Fang F, Erlendsdóttir H, Lu D, Mataix-Cols D, et al. Stress related disorders and subsequent risk of life threatening infections: Population based sibling controlled cohort study. BMJ. (2019) 367:l5784. doi: 10.1136/bmj.l5784
8. Siqveland J, Hussain A, Lindstrøm JC, Ruud T, Hauff E. Prevalence of posttraumatic stress disorder in persons with chronic pain: A meta-analysis. Front Psychiatry. (2017) 8:164. doi: 10.3389/fpsyt.2017.00164
9. Astill Wright L, Roberts NP, Barawi K, Simon N, Zammit S, McElroy E, et al. Disturbed sleep connects symptoms of posttraumatic stress disorder and somatization: A network analysis approach. J Trauma Stress. (2021) 34:375–83. doi: 10.1002/jts.22619
10. Zhao YJ, Zhang C, Guo T, Sha S, Su Z, Cheung T, et al. Associations between post-traumatic stress symptoms and quality of life among psychiatric healthcare personnel in China during the covid-19 pandemic: A network approach. Front Psychiatry. (2023) 14:975443. doi: 10.3389/fpsyt.2023.975443
11. Borsboom D, Cramer AO. Network analysis: An integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. (2013) 9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608
12. Amonoo HL, LeBlanc TW, Kavanaugh AR, Webb JA, Traeger LN, Jagielo AD, et al. Posttraumatic stress disorder symptoms in patients with acute myeloid leukemia. Cancer. (2021) 127:2500–6. doi: 10.1002/cncr.33524
13. Vance MC, Mash HBH, Ursano RJ, Zhao Z, Miller JT, Clarion MJD, et al. Exposure to workplace trauma and posttraumatic stress disorder among intern physicians. JAMA Netw Open. (2021) 4:e2112837. doi: 10.1001/jamanetworkopen.2021.12837
14. McNally RJ. Network analysis of psychopathology: Controversies and challenges. Annu Rev Clin Psychol. (2021) 17:31–53. doi: 10.1146/annurev-clinpsy-081219-092850
15. Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol. (2016) 125:747–57. doi: 10.1037/abn0000181
16. Eli B, Liang Y, Chen Y, Huang X, Liu Z. Symptom structure of posttraumatic stress disorder after parental bereavement - a network analysis of chinese parents who have lost their only child. J Affect Disord. (2021) 295:673–80. doi: 10.1016/j.jad.2021.08.123
17. Zhu Z, Eli B, Chen Y, Liu Z. Symptom structure of posttraumatic stress disorder in workplace trauma: A "distraction-avoidance" pattern. J Clin Psychol. (2024) 80:490–502. doi: 10.1002/jclp.23626
18. Fried EI, Eidhof MB, Palic S, Costantini G, Huisman-van Dijk HM, Bockting CLH, et al. Replicability and generalizability of posttraumatic stress disorder (ptsd) networks: A cross-cultural multisite study of ptsd symptoms in four trauma patient samples. Clin Psychol Sci. (2018) 6:335–51. doi: 10.1177/2167702617745092
19. Lazarov A, Suarez-Jimenez B, Levi O, Coppersmith DDL, Lubin G, Pine DS, et al. Symptom structure of ptsd and co-morbid depressive symptoms - a network analysis of combat veteran patients. Psychol Med. (2020) 50:2154–70. doi: 10.1017/s0033291719002034
20. Ouyang H, Wu L, Yan W, Si K, Lv H, Zhan J, et al. Network analysis of the comorbidity between post-traumatic stress, depression and anxiety symptoms among frontline healthcare workers during the covid-19 pandemic. Ther Adv Psychopharmacol. (2024) 14:20451253241243292. doi: 10.1177/20451253241243292
21. McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK, Borsboom D. Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clin psychol Sci. (2015) 3:836–49. doi: 10.1177/2167702614553230
22. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
23. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for dsm-5 (pcl-5): Development and initial psychometric evaluation. J Trauma Stress. (2015) 28:489–98. doi: 10.1002/jts.22059
24. Zhou X, Wu X, Zhen R. Assessing the latent structure of dsm-5 ptsd among chinese adolescents after the ya'an earthquake. Psychiatry Res. (2017) 254:33–9. doi: 10.1016/j.psychres.2017.04.029
25. Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. Qgraph: Network visualizations of relationships in psychometric data. J Stat Software. (2012) 48:1–18. doi: 10.18637/jss.v048.i04
26. Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. (2018) 23:617–34. doi: 10.1037/met0000167
27. Graziano RC, Brown WJ, Strasshofer DR, Yetter MA, Berfield JB, Haven SE, et al. Posttraumatic stress symptoms, posttraumatic growth, and personality factors: A network analysis. J Affect Disord. (2023) 338:207–19. doi: 10.1016/j.jad.2023.06.011
28. Birkeland MS, Greene T, Spiller TR. The network approach to posttraumatic stress disorder: A systematic review. Eur J Psychotraumatol. (2020) 11:1700614. doi: 10.1080/20008198.2019.1700614
29. Yang F, Huang N, Mu J, Guo J. The similarities and differences of network structures of posttraumatic stress symptoms among chinese adolescents exposed to three different types of trauma. Psychol Trauma. (2024). doi: 10.1037/tra0001705
30. Moshier SJ, Bovin MJ, Gay NG, Wisco BE, Mitchell KS, Lee DJ, et al. Examination of posttraumatic stress disorder symptom networks using clinician-rated and patient-rated data. J Abnorm Psychol. (2018) 127:541–7. doi: 10.1037/abn0000368
31. Stefanovic M, Takano K, Wittekind CE, Ehring T. Dynamic symptom associations in posttraumatic stress disorder: A network approach. Eur J Psychotraumatol. (2024) 15:2317675. doi: 10.1080/20008066.2024.2317675
32. Wang N, Chung MC, Zhang J, Fang S. Network analysis on the relationship between posttraumatic stress disorder, psychiatric co-morbidity and posttraumatic growth among chinese adolescents. J Affect Disord. (2022) 309:461–70. doi: 10.1016/j.jad.2022.04.148
33. Liu A, Ren Y, Yang S, Li Z, Zhu Z, Zhang LM, et al. Contemporaneous and temporal network analysis of complex posttraumatic stress disorder among chinese college students with childhood adversity: A longitudinal study. Psychiatry Res. (2024) 336:115872. doi: 10.1016/j.psychres.2024.115872
34. von Stockert SHH, Fried EI, Armour C, Pietrzak RH. Evaluating the stability of dsm-5 ptsd symptom network structure in a national sample of u.S. Military veterans. J Affect Disord. (2018) 229:63–8. doi: 10.1016/j.jad.2017.12.043
35. Stam R. Ptsd and stress sensitisation: A tale of brain and body part 1: Human studies. Neurosci Biobehav Rev. (2007) 31:530–57. doi: 10.1016/j.neubiorev.2006.11.010
36. Demb J, Kolb JM, Dounel J, Fritz CDL, Advani SM, Cao Y, et al. Red flag signs and symptoms for patients with early-onset colorectal cancer: A systematic review and meta-analysis. JAMA Netw Open. (2024) 7:e2413157. doi: 10.1001/jamanetworkopen.2024.13157
37. van de Wal M, Thewes B, Gielissen M, Speckens A, Prins J. Efficacy of blended cognitive behavior therapy for high fear of recurrence in breast, prostate, and colorectal cancer survivors: The sword study, a randomized controlled trial. J Clin Oncol. (2017) 35:2173–83. doi: 10.1200/jco.2016.70.5301
38. Wang Z, Neylan TC, Mueller SG, Lenoci M, Truran D, Marmar CR, et al. Magnetic resonance imaging of hippocampal subfields in posttraumatic stress disorder. Arch Gen Psychiatry. (2010) 67:296–303. doi: 10.1001/archgenpsychiatry.2009.205
39. Hayes JP, Vanelzakker MB, Shin LM. Emotion and cognition interactions in ptsd: A review of neurocognitive and neuroimaging studies. Front Integr Neurosci. (2012) 6:89. doi: 10.3389/fnint.2012.00089
40. McNally RJ, Heeren A, Robinaugh DJ. A bayesian network analysis of posttraumatic stress disorder symptoms in adults reporting childhood sexual abuse. Eur J Psychotraumatol. (2017) 8:1341276. doi: 10.1080/20008198.2017.1341276
41. Bryant RA, Creamer M, O'Donnell M, Forbes D, McFarlane AC, Silove D, et al. Acute and chronic posttraumatic stress symptoms in the emergence of posttraumatic stress disorder: A network analysis. JAMA Psychiatry. (2017) 74:135–42. doi: 10.1001/jamapsychiatry.2016.3470
42. Martinez-Calderon J, García-Muñoz C, Heredia-Rizo AM, Cano-García FJ. Meaning and purpose in life, happiness, and life satisfaction in cancer: Systematic review with meta-analysis. Psychooncology. (2023) 32:846–61. doi: 10.1002/pon.6135
43. Ross J, Murphy D, Armour C. A network analysis of dsm-5 posttraumatic stress disorder and functional impairment in uk treatment-seeking veterans. J Anxiety Disord. (2018) 57:7–15. doi: 10.1016/j.janxdis.2018.05.007
44. Stavropoulou A, Vlamakis D, Kaba E, Kalemikerakis I, Polikandrioti M, Fasoi G, et al. Living with a stoma": Exploring the lived experience of patients with permanent colostomy. Int J Environ Res Public Health. (2021) 18:8512. doi: 10.3390/ijerph18168512
45. Asselbergs J, van Bentum J, Riper H, Cuijpers P, Holmes E, Sijbrandij M. A systematic review and meta-analysis of the effect of cognitive interventions to prevent intrusive memories using the trauma film paradigm. J Psychiatr Res. (2023) 159:116–29. doi: 10.1016/j.jpsychires.2023.01.028
46. Peters J, Bellet BW, Jones PJ, Wu GWY, Wang L, McNally RJ. Posttraumatic stress or posttraumatic growth? Using network analysis to explore the relationships between coping styles and trauma outcomes. J Anxiety Disord. (2021) 78:102359. doi: 10.1016/j.janxdis.2021.102359
47. Badour CL, Feldner MT. Trauma-related reactivity and regulation of emotion: Associations with posttraumatic stress symptoms. J Behav Ther Exp Psychiatry. (2013) 44:69–76. doi: 10.1016/j.jbtep.2012.07.007
48. Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychol Bull. (1986) 99:20–35. doi: 10.1037/0033-2909.99.1.20
49. Foa EB, Zinbarg R, Rothbaum BO. Uncontrollability and unpredictability in post-traumatic stress disorder: An animal model. Psychol Bull. (1992) 112:218–38. doi: 10.1037/0033-2909.112.2.218
50. Ehlers A, Steil R. Maintenance of intrusive memories in posttraumatic stress disorder: A cognitive approach. Behav Cognit Psychother. (1995) 23:217–49. doi: 10.1017/s135246580001585x
51. Snoek A, Edens R, van Ballegooijen W, Dekker J, Beekman AT, Thomaes K. A network perspective on posttraumatic stress disorder and comorbid borderline personality disorder symptoms. Eur J Psychotraumatol. (2024) 15:2367815. doi: 10.1080/20008066.2024.2367815
52. Birkeland MS, Heir T. Making connections: Exploring the centrality of posttraumatic stress symptoms and covariates after a terrorist attack. Eur J Psychotraumatol. (2017) 8:1333387. doi: 10.1080/20008198.2017.1333387
Keywords: colorectal cancer, chemotherapy, PTSD, network analysis, symptom structure
Citation: Zhou Y, Teng W, Luo L, Zhou P, Fan G and Liu H (2025) Network analysis of the symptoms of posttraumatic stress disorder in patients undergoing chemotherapy for colorectal cancer. Front. Psychiatry 15:1505518. doi: 10.3389/fpsyt.2024.1505518
Received: 03 October 2024; Accepted: 16 December 2024;
Published: 08 January 2025.
Edited by:
Saraswati Dhungana, Institute of Medicine (Nepal), NepalCopyright © 2025 Zhou, Teng, Luo, Zhou, Fan and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haiying Liu, NDM3MjI1NzE1QHFxLmNvbQ==
 Yi Zhou
Yi Zhou Wen Teng1
Wen Teng1 Liang Luo
Liang Luo