- 1Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy
- 2Department of Women's and Children's Health, School of Medicine and Surgery, University of Padua, Padua, Italy
- 3Child Neuropsychiatry Unit, University Hospital of Padua, Padua, Italy
- 4Department of Developmental and Social Psychology, University of Padua, Padova, Italy
Background: Non-suicidal self-injury (NSSI) is defined as a transdiagnostic phenomenon that has well increased in the latest years, especially in the adolescent population. It has been associated with suicidality, alexithymia, emotion dysregulation, and psychosocial impairment, as well as family issues. The choice of level of care (i.e., hospitalization versus outpatient visit) depends on a number of factors that relate not only to suicidal risk but also to severity of individual’s psychosocial functioning, the ability of family environment to support treatment choices and to contain child, as well as the need for ongoing monitoring of the young patient. A scarcity of studies has compared outpatients with inpatients, both of them engaging in NSSI.
Methods: the current study aimed to further expand knowledge regarding features that characterize young self-harmers who receive different levels of care, with particular attention on psychopathological, family, and NSSI-related characteristics, as well as suicidality. The current research included 56 inpatients and 56 outpatients with NSSI, paired for gender, age, and psychiatric diagnosis. Instruments investigating psychopathology, emotion dysregulation, alexithymia, psychosocial functioning, and interactive family dynamics were administered. Descriptive statistics, parametric and non-parametric inferential statistics were applied.
Results: study findings highlighted that inpatients engaging in NSSI reported lifetime suicidality, clinical level of externalizing and internalizing problems, more severe alexithymia, emotion dysregulation, and impaired psychosocial functioning compared to outpatients engaging in self-harming. Furthermore, when compared to outpatients’ families, inpatients’ families were more capable of adhering to rules and time of the family play situation (the Lausanne Trilogue Play procedure) and fixing interactive mistakes through activities. On the contrary, in the inpatient group, global performance, role implication, parental scaffolding, child’s involvement and self regulation tend to decline, while parental conflicts tend to rise over the four part scenario of the family play.
Conclusion: these findings confirmed a more severe global picture of young inpatients engaging in self-harming, suggesting that NSSI may be the expression of this larger psychopathological picture. In addition, the study highlighted the need for a multi-informant and multimethod clinical assessment, which should include evaluation of family context and co-parenting system, especially for hospitalized young patients engaging in self-harm.
1 Introduction
Non-suicidal self-injury (NSSI) is defined as behavior of intentional harm to one’s body tissue in the absence of a suicidal purpose (1), although several studies have identified frequent coexistence between NSSI and suicidal behavior (2, 3). It is a transdiagnostic phenomenon; in fact, it is associated with a wide variety of psychiatric disorders in both outpatient and inpatient samples (4–7). Research showed a NSSI prevalence in nonclinical adolescent populations of 20% (8). This tends to rise in clinical populations to over 50% (5, 9). A further increase in NSSI among adolescents has been recorded during the Covid-19 pandemic (10, 11). The NSSI methods can be multiple (12), such as “cutting,” “scratching,” “head banging,” “burning,” and “hitting” (13, 14).
Nock and Pristein (2004) proposed a model that conceptualizes the different functions of NSSI along two axes: the positive/negative reinforcement axis and the intrapersonal/interpersonal axis (15). Subsequent research has shown that the one most reported is the intrapersonal function (16) in both inpatients (17) and outpatients (18). Unlike interpersonal function, intrapersonal function also positively predicts the severity of NSSI in terms of method versatility and NSSI frequency (19). The severity of the clinical picture has also been associated with more injured body sites or an injury in a body site other than the arms (20). Non suicidal self-injurers often reported greater psychosocial impairment (21, 22) and alexithymia, which is the difficulty in identifying and describing emotions (7, 23, 24). Moreover, Andover and Morris (2014) showed an association between NSSI and a low ability to regulate emotions adaptively (25). As a consequence, NSSI can be used as a dysfunctional coping mode that allows avoidance or reduction of negative emotions (15, 26).
The literature has also investigated the social and family context associated with NSSI, identifying dysfunctional family dynamics (27, 28), particularly in terms of the emotional dimension. A history of emotional abuse (29), a lack of parental emotional validation, a prevalence of negative affect and control (30), more rigid punitive methods, and an insecure parent-child attachment relationship (31) have been found. In addition, Halstead and colleagues (2014) reported poor family cohesion and communication issues in these families (32), whereas other authors found high family conflict (33, 34), low parental monitoring (34), and poor relationships with caregivers (33). A study conducted by Wang and colleagues (2022) showed a mediating effect of depressive symptoms on the relationship between poor family functioning and NSSI (35). Specifically, it has been suggested that the onset of depressive symptoms within a dysfunctional family context might be linked to the low development of the child’s ability to regulate emotions (36).
Emergency Department (ED) presentation for self-harm has increased in the last years, and this trend has accelerated, most of all in young females, since the Covid-19 outbreak (37). Nevertheless, a systematic review and meta-analysis conducted by Witt and colleagues (2023) showed that just one-in-five adults and young people who were referred for inpatient treatment were admitted following hospital presentation for self-harm, whereas just over half of young people referred for outpatient treatment after hospital presentation for self-harm attended at least one treatment session (38). In addition, Bridge and colleagues (2019) noted that only about one in four cases resulted in an outpatient follow-up appointment being scheduled before the patient leaves the emergency room (39), despite non-suicidal self-injury — especially if it occurs repeatedly over time — is thought to be a precursor of suicidal behavior (40). Moreover, the time after hospital discharge is considered to be the peak risk period for both non-suicidal self-harm and suicide (38). The choice regarding the level of care (hospitalization versus outpatient visit), in turn, depends on a number of factors that relate not only to suicidal risk (i.e., previous history of suicidal behaviors, depressive disorders, and high-lethality self-harm), but also to the severity of the individual’s psychosocial functioning, the ability of the family environment to adhere to and support treatment choices, and the need for ongoing monitoring of the patient (41). Family’s level of distress and the parental capacity to contain the child also play a role in the decision-making on the child’s psychiatric hospitalization (42).
Few studies have compared NSSI outpatients with NSSI inpatients. We are aware of only one study that investigated the course of suicidal and non-suicidal self-injury between the two clinical samples, identifying in the hospitalized sample a lower age of onset of such self-injurious phenomena and a significantly higher presence of suicidal ideation and suicidal planning (43). This study considered the current level of care as an inclusion criterion, such that some outpatients might have had previous hospitalizations. Further research, focusing exclusively on groups of self-harm inpatients, has identified an increased suicide risk among those with a previous hospitalization for self-harm (44) and a tendency for repeated self-harm over time, which, in turn, is influenced by traits of emotional dysregulation and internalizing symptoms (45). Moreover, other studies found that both externalizing (e.g., disruptive behavior disorder) and internalizing (e.g., anxiety and depressive disorder) problems were associated with inpatient treatment in adolescents (46, 47).
The current study aimed to further expand knowledge regarding features that characterize young self-harmers who receive different levels of care (i.e., inpatient admission vs. outpatient visits), with particular attention on psychopathological, family, and non-suicidal self-harm-related characteristics, as well as suicidality. Specifically, the objectives of the study were as follows: 1) identifying any difference between young NSSI inpatients and young NSSI outpatients in the non-suicidal self-harm-related characteristics (i.e., NSSI methods, NSSI frequency, NSSI method versatility, NSSI function, and number of injured body sites), suicidality (i.e., lifetime suicidal ideation and lifetime suicide attempts), and psychopathological features. We have considered variables that have previously been associated with NSSI, such as alexithymia, emotion dysregulation, psychosocial functioning, externalizing problems, internalizing problems, and total problems. According to the previous findings (41, 43, 48), we supposed that NSSI inpatients reported more lifetime suicidality, greater NSSI severity, and impaired psychosocial functioning than the outpatient group. Moreover, based on studies that focused on hospitalization-related psychopathological factors in psychiatric populations (46, 47, 49), we hypothesized that the inpatient group showed a greater severity of externalizing, internalizing, and total problems than the outpatient group, as well as more severe emotion dysregulation; 2) pinpointing any difference between young NSSI inpatients and young NSSI outpatients in the family interactive-relational variables and investigating any changes in family interaction dynamics in the inpatient and the outpatient groups. Plener and colleagues (2016) highlighted that inpatient treatment for youngs with NSSI was indicated when the environment is detrimental for the recovery in an outpatient setting (41), whereas other studies found that hospitalization in a Child Neuropsychiatric Unit was associated with intrafamily issues (50–52). Despite these findings, we are not aware of studies that focused on specific interactive family dynamics associated with hospitalization in NSSI cases; thus, we did not formulate any hypothesis and we decided to proceed in an explorative way.
2 Materials and methods
2.1 Participants
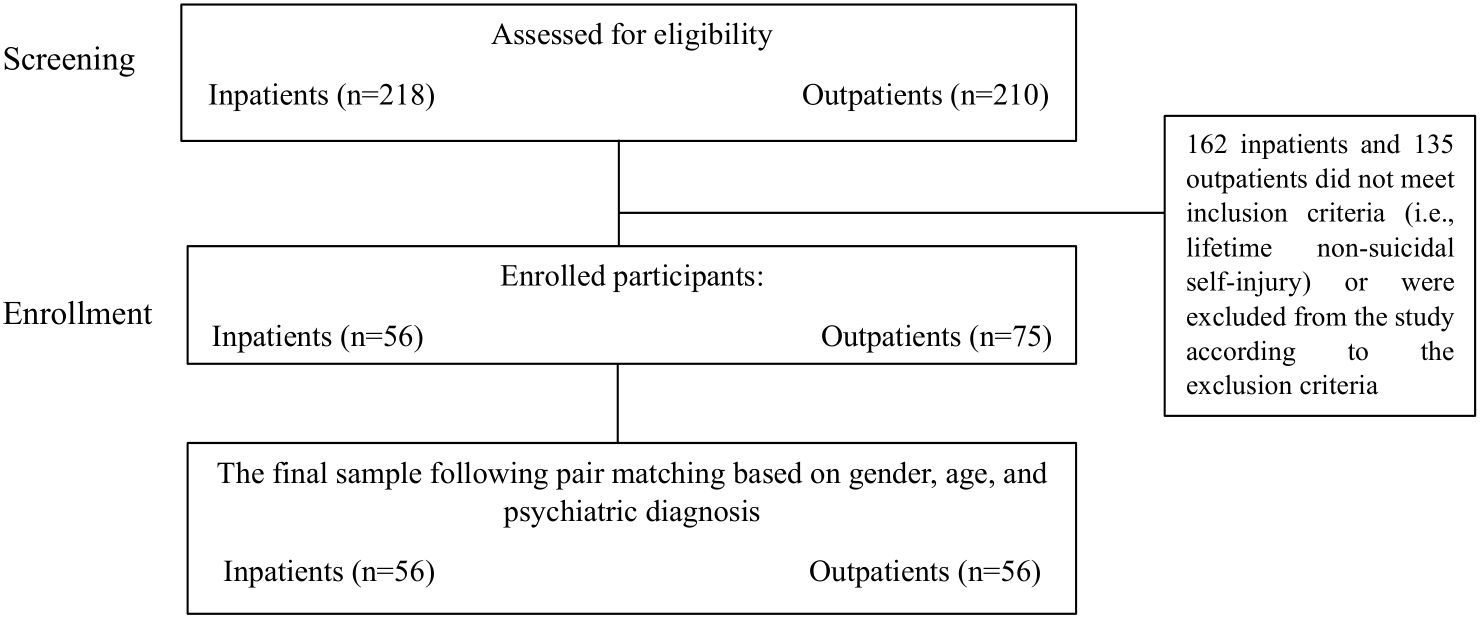
The current research is a cross-sectional observational study. It has been screened all inpatients and outpatients who consecutively approached two Child Neuropsychiatry Units in northern Italy in the period between January 2022 and December 2023. We included in the study only patients who reported lifetime non-suicidal self-injury (NSSI) either as a reason for the clinical consultation, hospital admission or emerged from clinical history. For each inpatient included, we matched an oupatient, according to age, gender, and first psychiatric diagnosis (ICD-10) in order to control for these factors. The availability of participants within the clinical settings constrained the sample size. The final sample was composed of fifty-six NSSI inpatients and fifty-six NSSI outpatients. Given the scarcity of male NSSI inpatients who were admitted to the Child Neuropsychiatric Unit, we excluded males in the final sample. Moreover, we excluded outpatients with previous psychiatric hospitalizations, inpatients and outpatients with intellectual disabilities, with autism spectrum disorders and those who did not give informed consent for research participation. Flow diagram of participants is shown in Figure 1. The patients’ age range was 11 to 17 years old (M = 14.5; SD = 1.4). Regarding the distribution of the first psychiatric diagnosis, thirty-two outpatients and thirty-two inpatients had an ongoing diagnosis of mood disorders (F30-39), seventeen outpatients and seventeen inpatients had an ongoing diagnosis of anxiety and somatoform disorders (F40-49), five outpatients and five inpatients had an ongoing diagnosis of behavioral and emotional disorders (F90-98) and two outpatients and two inpatients had an ongoing diagnosis of eating disorders (F50-59). Moreover, forty-five (80%) inpatients and twenty-two (39%) outpatients had at least one psychiatric comorbidity. Forty-three inpatients (77%) were on their first hospitalization for mental issues. All inpatients and 46.9% outpatients were on drug therapy. As regards family characteristics, 10% of outpatients and 26% of inpatients had divorced or separated parents. The parents’ ages ranged from 31 to 57 years old for the mothers (mean age of inpatients’ mothers = 46.6, SD = 6.2 and mean age of outpatients’ mothers = 45.6, SD = 6.7) and from 33 to 71 years old for the fathers (mean age of inpatients’ fathers = 51.8, SD = 7.2 and mean age of outpatients’ fathers = 48.4, SD = 7.8). 80% of inpatients and 96% of outpatients had at least one sibling.
2.2 Procedure
Data were gathered from patients and their parents during the clinical assessment that occurred in the initial clinical consultation (for outpatients) or in the hospital admission (for inpatients). In the outpatient setting, the clinical evaluation includes a clinical interview with the adolescent patient and their parents conducted by a neuropsychiatrist and a psychologist and the administration of clinical questionnaires (see section ‘Instruments’). In the absence of clinical and family limitations (e.g., family not providing consent for video-recording), multi-problem family situations, etc.), the observation of family interactions is conducted by administering the Lausanne Trilogue Play (LTP) procedure. Regarding the inpatient setting, the clinical assessment was carried out by an interdisciplinary team composed of medical doctors, psychologists, nurses, and educators. The clinical multidisciplinary evaluation includes medical examinations, clinical interviews with the inpatient and their parents, the administration of clinical questionnaires (see section ‘Instruments’), and the observation of family interactions through the use of the Lausanne Trilogue Play (LTP) procedure, administered only to patients without clinical and family limitations, as mentioned above. Both the young patients and their parents provided informed consent for research participation. The current study was conducted in accordance with the Declaration of Helsinki and was approved by the local Ethics Committee (CESC protocol code n° 0044914 of 13 July 2021)
2.3 Instruments
The Youth Self Report (YSR) (53, 54) is a standardized, widely used self-report instrument completed by adolescents for the assessment of the juvenile’s psycho-behavioral profile (55). It is composed of two parts: the first part assesses adaptive functioning (activities, social, and total competencies); the second part is characterized by 112 items evaluating emotional-behavioral problems according to eight syndrome scales, which were grouped into three broadband scales: internalizing problems (including withdrawn/depressed problems, anxious/depressed problems, somatic complaints); externalizing problems (including aggressive behavior and rule-breaking behavior); and total problems (sum of all items). Moreover, other three syndrome scales were included: social problems, attention problems, and thought problems. According to the score obtained for each scale, behaviors can be evaluated as ‘clinical’, ‘borderline’, or ‘nonclinical’. Furthermore, a Deficient Emotional Self-Regulation (DESR) profile can be obtained by summing the scores of the attention problems, anxious/depressed, and aggressive behavior scales. A score between 180 to 210 suggests poor emotional self-regulation, while 210 or more indicates severe dysregulation (56, 57). According to the purpose of the current study, we considered the scores of three broadband scales (i.e., internalizing, externalizing, and total problems), the subscale ‘activities’ (i.e., youth’s engagement in sport and non-sport related activities), and the DESR profile. Regarding psychometric properties, Frigerio and colleagues (2004) found satisfactory internal consistency of the questionnaire (Cronbach’s alpha values ranging from 0.83 to 0.91) (58).
The Children’s Global Assessment Scale (CGAS) (59) is a clinician-reported measure that assesses general psychological and social functioning in children and adolescents ages 4 to 16, but has now been extended to 23 years old (60). Based on the lowest level of functioning in the last month, the clinician evaluates a range of psychological and social aspects and gives a score between 1 and 100. Scores formed ten categories, from ‘constant supervision is required’ (1-10) to ‘superior functioning’ (91-100). Scores higher than 70 indicate good psychosocial functioning. It has been found to have adequate inter-rater reliability (ICC=0.84), satisfactory test-retest reliability (ICC range= 0.69-0.95) and good convergent and discriminant validity (59).
The Toronto Alexithymia Scale (TAS-20) (61, 62) is a 20-item, self-administered questionnaire that measures three factors: difficulty in identifying feelings, difficulty in describing feelings, and externally oriented thinking. For the purpose of this study, we calculated the total TAS score by adding the scores from the aforementioned factors. A total score of 60 or higher suggests alexithymia. Several studies have supported the application of this instrument in the juvenile population (63–65). The Italian version of TAS-20 exhibits adequate test-retest reliability and good internal consistency (Cronbach’s α range: 0.52-0.75 for the general population and 0.54-0.82 for clinical samples) (61).
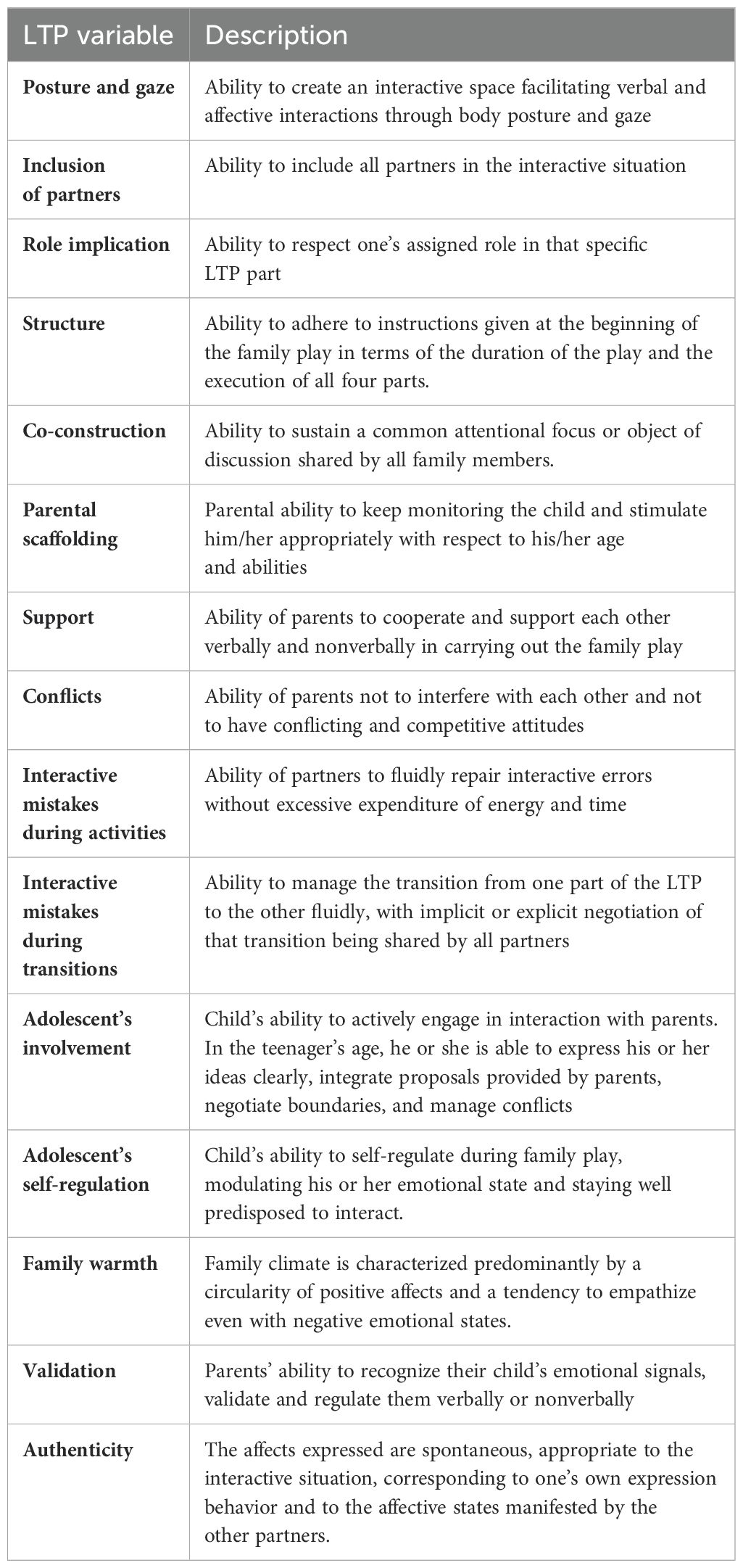
The Lausanne Trilogue Play (LTP) procedure (66) is an observational, semi-standardized, distress-free play situation that assesses the triadic family interactions. This procedure involves the adolescent and their parents together, who are requested to plan either the adolescent’s birthday or a daytrip. It requires a specific setting based on a four-part scenario characterized by four subsequent triadic interactive configurations: in the first part (2 + 1), one parent plays with the adolescent while the other parent simply stays nearby; in the second part (2 + 1), the two parents switch roles; in the third part, the parents and the adolescent play together; and in the fourth part (2 + 1), the parents play together whereas the adolescent simply stays nearby. The play situation is video-recorded and subsequently analyzed according to the guidelines provided by the FAAS manual (Family Alliance Assessment Scale 6.3) (67) tailored for adolescents (68). Fifteen interactive-relational variables were evaluated (further details about variables are described in Table 1). For each LTP’s part, the variables are evaluated on a three-point Likert scale (1=inappropriate; 2= partially appropriate; 3=appropriate). An overall score for each variable is obtained by summing the scores of the same variable for each part of the LTP. Furthermore, by adding the scores of 15 variables from the same part of the play, a global score for each LTP part is calculated. Scoring was performed by two independent assessors who underwent specific training in the LTP procedure. In the current research, the inter-rater reliability reached a Cohen’s kappa of 0.90, and the overall internal consistency was high (Cronbach’s α=0.91), ranging from 0.90 to 0.94.
2.4 Data analysis
Descriptive statistics (i.e., means, standard deviation, and percentage frequencies) were calculated in order to determine the socio-demographic and clinical characteristics of the whole sample and the subgroups of patients divided according to the level of care setting (outpatients vs. inpatients). A Chi-square test was applied in order to investigate the differences between outpatients and inpatients in categorical variables in terms of NSSI characteristics, suicidality, and YSR’s psychopathological features, including internalizing, externalizing, and total problems categorized at clinical, borderline, or non-clinical levels. To explore differences between outpatients and inpatients in continuous clinical variables, first, we controlled the assumption of normality and homoscedasticity. The TAS total scores and DESR profile scores satisfied both assumptions, thus the Student’s t-test was applied. Unlikely, CGAS scores did not show homogeneity of variance, thus Welch’s t-test was performed. LTP variable scores did not satisfy the normality assumption, thus the Mann-Whitney test was applied. In order to outline the magnitude of the differences between outpatients and inpatients in the psychopathological variables, effect size indices are reported (i.e., Cohen’s d for continuous normal variables and Cramer’s V for categorical variables). Finally, in order to investigate, separately for the outpatients and inpatients groups, the within-subjects trend of the overall scores among the four parts of the LTP and the scores of each interactive-relational variable among the four parts of the LTP scenario, Friedmann’s test was applied. For this purpose, we selected only families who had completed all four LTP parts. A Durbin-Conover post-hoc test was conducted for the pairwise comparison. Due to the exploratory nature of the study, we did not perform a formal power analysis. To handle missing data, we used Available Case Analysis in order to maximize the use of the data without excluding participants due to missing values on some variables. Data analyses were performed using the software Jamovi 2.3.18 (2022).
3 Results
3.1 NSSI characteristics and suicidality
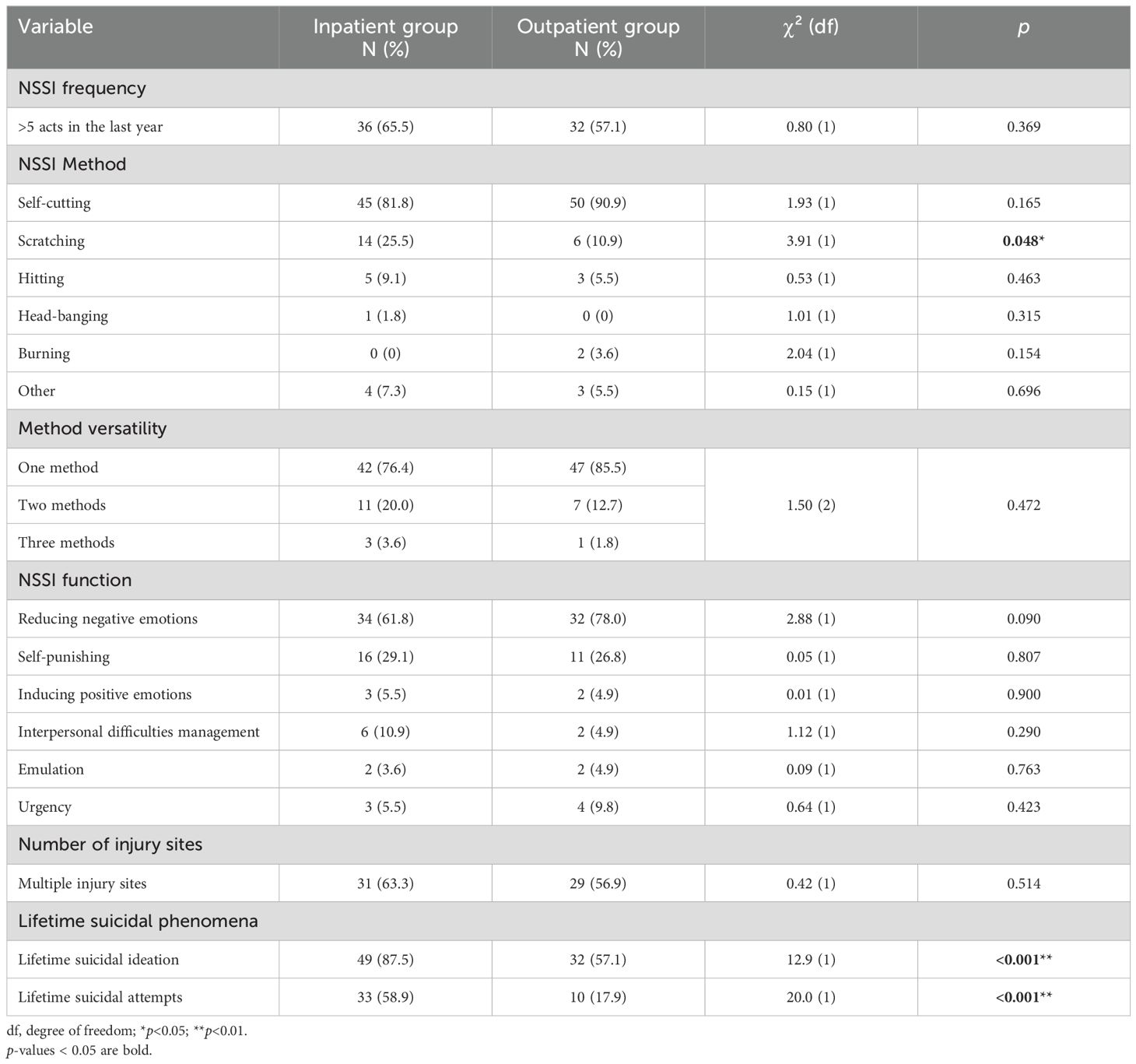
57.1% outpatients and 65.5% inpatients reported repetitive NSSI (i.e., more than five NSSI acts in the last year). Regarding the NSSI method, scratching was more likely in the inpatient group (χ²(1)=3.91; p=0.048), whereas other NSSI methods (i.e., self-cutting, hitting, head-banging, and burning) did not differ between the inpatient and outpatient groups (see Table 2). Average NSSI versatility was 1.16 (SD= 0.42; range=1-3) for the outpatient group and 1.27 (SD=0.52; range=1-3) for the inpatient group, with 85.5% outpatients and 76.4% inpatients using one method, 12.7% outpatients and 20.0% inpatients using two methods, and 1.8% outpatients and 3.6% inpatients using three methods. As regards the NSSI functions, 78.0% outpatients and 61.8% of inpatients used NSSI for reducing negative emotions; 26.8% outpatients and 29.1% inpatients used NSSI for self-punishing; 4.9% outpatients and 10.9% inpatients used NSSI for managing interpersonal difficulties; 4.9% outpatients and 5.5% inpatients used NSSI for inducing positive feelings; 4.9% outpatients and 3.6% inpatients used NSSI for emulation. In 9.8% outpatients and 5.5% inpatients, NSSI was associated with a sense of urgency. 56.9% of outpatients and 63.3% of inpatients reported multiple sites of injury. The NSSI frequency, method versatility, NSSI function, and number of injury sites did not differ between the inpatient and outpatient groups. The inpatient group was more likely to report lifetime suicidal ideation (χ²(1)=12.9; p=0.001) and lifetime suicide attempts (χ²(1)=20.0; p=0.001) than the outpatient group. However, the difference was still statistically significant for lifetime suicide attempts (χ²(1)=9.84; p=0.002) but not for suicidal ideation (χ²(1)=0.55; p=0.458) when we stratified the data based on the presence of a drug regimen.
3.2 Psychopathological characteristics
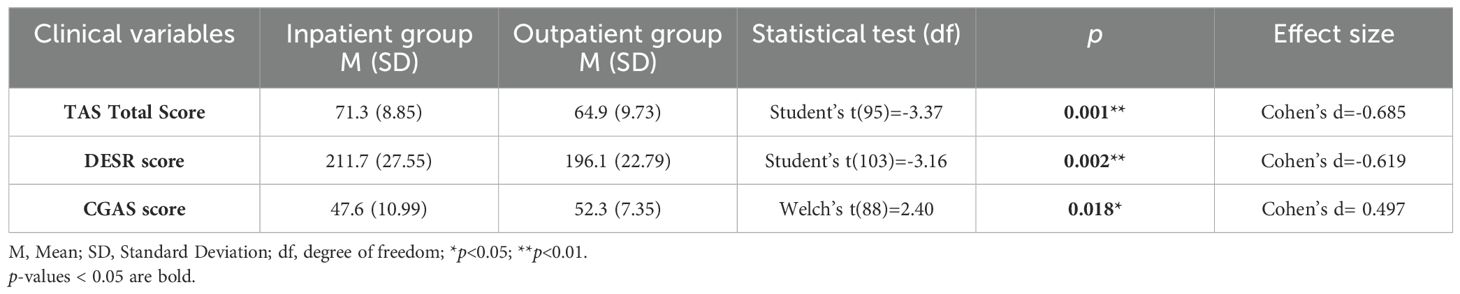
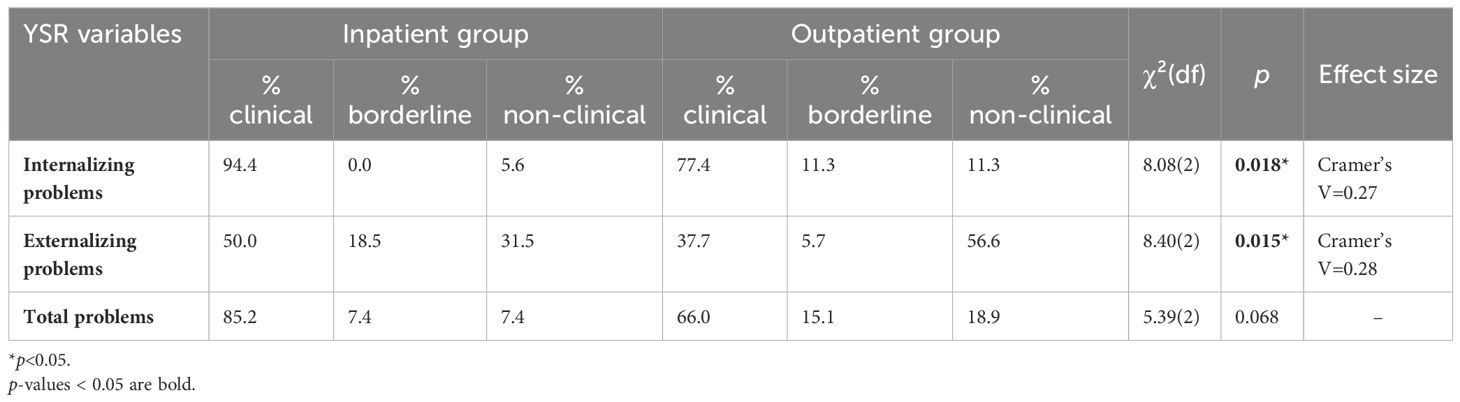
In order to determine whether the inpatient and outpatient groups of NSSI adolescents differed in some clinical variables usually associated with NSSI, the Student’s t-test was performed. It has been found that the inpatient group showed a statistically higher total TAS mean score (t(95)=-3.37; p=0.001) and a statistically higher DESR mean score (t(103)=-3.16; p= 0.002) than the outpatient group, indicating more severe alexithymic traits and more severe difficulties in emotion regulation, respectively. Moreover, the inpatient group exhibited a statistically significant lower CGAS mean score than the outpatient group (t(88)=2.40; p=0.018), indicating worse psychosocial functioning. In YSR subscale ‘activities’ 40.5% of outpatients and 59.5% of inpatients reached the clinical level, despite the absence of any statistical significant difference between groups (χ²(2)=4.26; p=0.119). Considering the YSR’s broad variables (i.e., internalizing problems, externalizing problems, and total problems), whose severity is evaluated on three categorical levels (i.e., clinical, borderline, and non-clinical), we found a statistically significant association between the level of care (inpatient vs. outpatient) and the internalizing (χ²(2)=8.08; p=0.018) and externalizing problems (χ²(2)=8.40; p=0.015), whereas no statistically significant association has been found for total problems (χ²(2)=5.39; p=0.068). Results are shown in Tables 3 and 4. By stratifying the data according to the presence of a drug regimen, the difference only remained statistically significant for TAS mean score (t(62)=-3.26; p=0.002), DESR mean score (t(66)=-2,30; p=0.024), and internalizing problems (χ²(2)=8.58; p=0.014).
3.3 The interactive family functioning
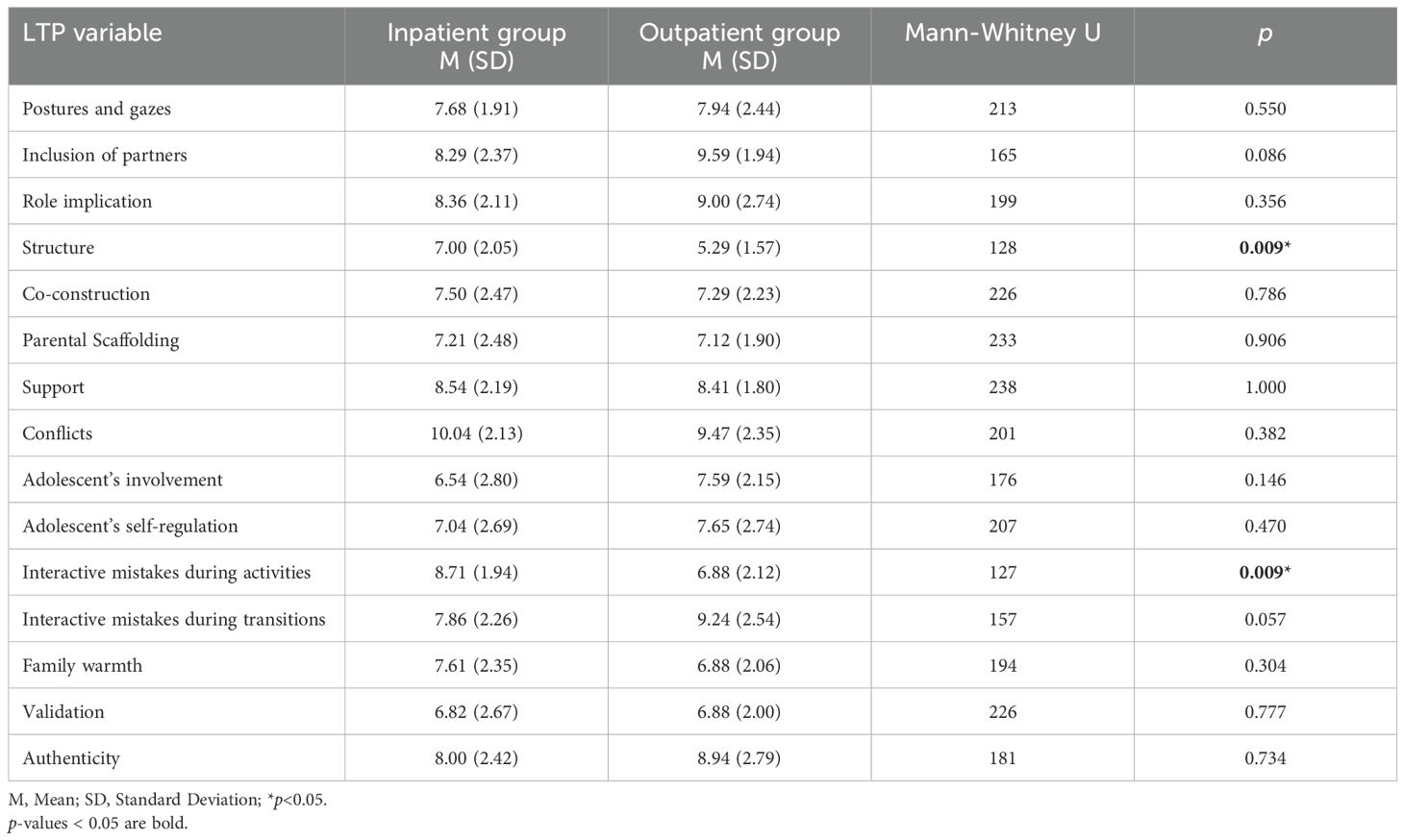
For a subgroup of inpatients (N=28) and a subgroup of outpatients (N=19) and their parents, we considered data obtained from the Lausanne Trilogue Play (LTP) procedure. In order to explore the difference in the interactive family dynamics between two groups, the Mann-Whitney test was applied to the global scores of each LTP interactive-relational variable. Higher global scores indicate a higher quality of family interactions. Statistically significant differences between the inpatient and outpatient groups have emerged in the following LTP variables: structure (U=128; p=0.009) and interactive mistakes during activities (U=127; p=0.009). Descriptive statistics and the Mann-Whitney test are shown in Table 5.
3.4 Within-subjects trend of interactive family dynamics
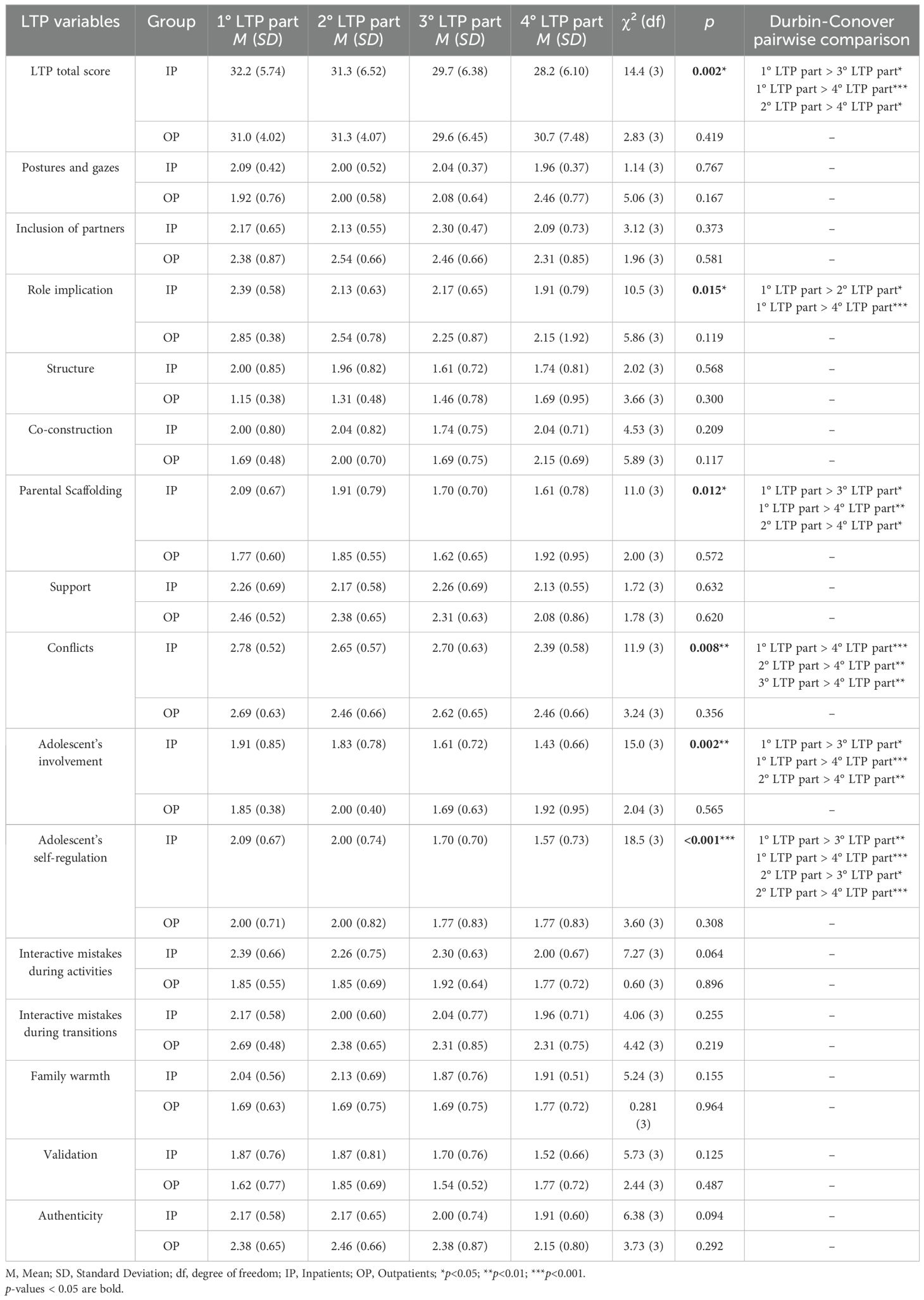
To determine whether the interactive family dynamics changed over the LTP four-part scenario, the Friedmann test was run for the inpatient and the outpatient groups, respectively. We only considered families who had completed all four LTP parts, thus including 13 families for the outpatient group and 23 families for the inpatient group. As regards the outpatient group, there has not been a statistically significant change over the LTP four-part scenario (χ²(3)=2.83; p=0.419). On the contrary, for the inpatient group, a statistically significant change from the first LTP part to the fourth LTP part has been found (χ²(3)=14.4; p=0.002). No statistically significant difference in any LTP part occurred between the inpatient and the outpatient groups (1° LTP part: U=264; p=0.974; 2° LTP part: U=217; p=0.622; 3° LTP part: U=232; p=0.730; 4° LTP part: U=167; p=0.152). Figure 2 depicts trends in interactive family dynamics over the LTP four-part scenario for both the inpatient and outpatient groups.
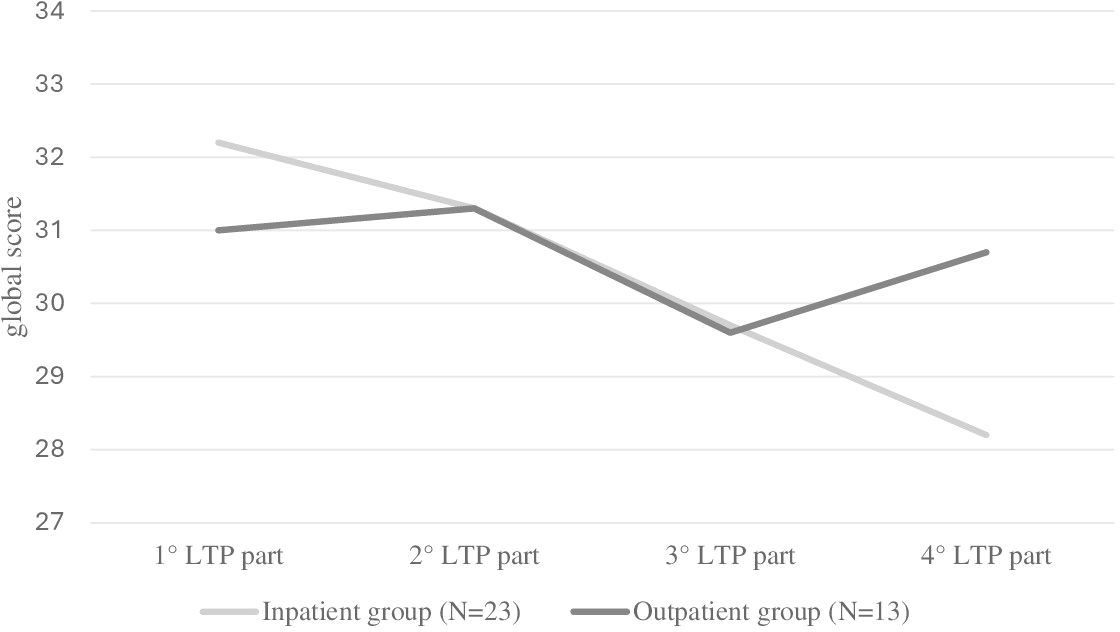
Figure 2. Within-subjects trends in interactive family dynamics in the inpatient group and the outpatient group.
Furthermore, the Friedmann test was performed on each of the LTP interactive-relational variables to determine whether specific LTP variables changed during the four-part scenario for the inpatient and outpatient groups separately. Unlike the outpatient group, in the inpatient group the following LTP variables exhibited a statistically significant change during the LTP four-part scenario: role implication (χ²(3)=10.5; p=0.015); parental scaffolding (χ²(3)=11.0; p=0.012); conflicts (χ²(3)=11.9; p=0.008); adolescent’s involvement (χ²(3)=15.0; p=0.002); adolescent’s self-regulation (χ²(3)=18.5; p<0.001). Descriptive statistics, the Friedmann Test, and the Durbin-Conover pairwise comparison are described in Table 6.
4 Discussion
The main purpose of the current study was to investigate psychopathological, family, and self-harm- related features that distinguish young NSSI inpatients from young non-suicidal self-injurers who received outpatient treatment. According to Glenn and colleagues (2017) (43), we found that inpatient self-harmers reported higher rates of lifetime suicidal ideation and lifetime suicidal attempts than the outpatient group. Differently from Glenn and colleagues (2017) (43), we did not include outpatients with a previous history of psychiatric hospitalization; thus, this highlighted that the two groups differ from the intensity of level of care received in their lifetime for mental health issues. Our findings were consistent with the fact that hospitalization is often the treatment of choice for individuals with high suicidal risk (69). Contrary to our expectations, the inpatient group did not show more severe NSSI in terms of method versatility and NSSI frequency, even though the inpatient group reported higher rates of scratching, which was associated in the previous studies with a more severe risk profile (70) and with interpersonal conflict management and regulation of negative emotions (71). Consistently, we found that the inpatient group showed a more severe emotion dysregulation profile, higher alexithymic traits, and worse psychosocial functioning than the outpatient group. In addition, clinical levels of externalizing and internalizing problems were more associated with the inpatient treatment. Overall, these findings supported a more severe global clinical picture of self-harmers who were required to have a more intensive level of care. Although the association between the level of care and certain variables (such as lifetime suicidal ideation, externalizing problems, and psychosocial functioning) was lessened when a drug regimen was taken into account, the degree of underlying psychopathology — rather than the severity of the NSSI characteristics — seems to be what distinguishes the inpatient sample from the outpatient sample. This suggests that NSSI should not be viewed as a symptom in and of itself, but rather as an expression of a larger psychopathological picture that requires thorough investigation.
The evaluation of interactive family dynamics through the LTP procedure highlighted that the inpatient group showed better scores in the variables ‘structure’ and ‘interactive mistakes during activities’ than the outpatient group. In fact, hospitalization at a Child Neuropsychiatric Unit requires that all family members define new roles and responsibilities together, adjust their daily routines and adapt themselves to the strict rules and routines imposed by the admission (72–74). As a result, our findings may be understood in view of the fact that the inpatient group’s families have become accustomed to changing their activities as part of an adaptation process in response to external circumstances (e.g., the hospital admission) and strictly adhering to explicit hospital rules. Moreover, these findings emphasize the role of hospitalization as a structural framework within which the young patient and family can get care and containment at a time when the family setting alone cannot provide a safe and conflict-free environment for the child’s growth.
In addition, unlike the outpatient group’s families, the inpatient group’s families showed a decrease in the overall interactive-relational performance during the course of the LTP four-part scenario, reaching the global lowest score in the fourth part, in which the play situation is mostly managed by the co-parenting system. This decreasing trend has also been found in some of the specific LTP interactive-relational variables, such as ‘role implication’, ‘parental scaffolding’, ‘conflicts’, ‘adolescent’s involvement’, and ‘adolescent’s self-regulation’. A two-way process emerged: both the parents’ ability to monitor and stimulate appropriately the child and the child’s ability to self-regulate and appropriately involve in family interactions collapsed into the fourth part of the family play situation, when the co-parenting system was left to manage the family interactions and the adolescent simply had to stay nearby. At this stage, conflicting and interfering parental interactions peaked.
A further contribution of our research consists of showing that the adolescent’s self-dysregulation is not a fixed dimension but changes across the LTP four-part scenario, according to different triadic configurations. It reached its maximum peak when the adolescent should act as a simple observer within a family context characterized by lowered parental scaffolding and high conflicts. These findings were consistent with the biopsychosocial model of mental health (75), which emphasizes the role of the family and social environment for the child’s development (28). Previous studies highlighted the role of the co-parenting system in the child’s mental health issues (76, 77). In fact, it has been demonstrated that families of hospitalized children were often characterized by high interparental conflicts (50, 51) and low parental capacity to contain the child (42), which, in turn, were associated with a low child’s ability to regulate own emotions (78, 79). To the best of our knowledge, the current study is the first to report findings on the changes in interactive family dynamics using an observational semi-standardized tool in hospitalized adolescents with self-harming, while also disentangling family, psychopathological, and NSSI-related features from an adolescent NSSI outpatient sample. Overall, our results highlighted the relevance of evaluating the co-parental system during the hospitalization process of young self-harmers using multi-informant and multi-method instruments, given that the quality of interparental interactions may have a role in the child’s self-regulation.
The current study presents some limitations. First, because of the current study’s small sample size and the sample enrollment occurring only at two Child Neuropsychiatry Units in northern Italy, it is necessary to be cautious in generalizing the results. Particularly, we were able to obtain data on interactive family dynamics just for a small subgroup of self-harmers due to the presence of family limitations (e.g., problematic family situations). Future research involving multisite sampling across different areas of Italy are needed. Moreover, all patients were females; thus, it did not allow us to extend the findings to the male population of self-harmers. Further studies should enroll larger samples, including male self-harmers, to conduct subgroup analysis according to gender and increase the external validity of study results. Given the cross-sectional nature of this study, it poses a challenge to determine whether the findings pertaining to clinical data and family functioning also serve as a predictor for the type of psychiatric treatment that follows. Hence, prospective longitudinal studies are needed for further research in this field. Although similar inclusion and exclusion criteria between groups have been chosen (with the exception of the variable ‘previous psychiatric hospitalizations’), it is possible that other sources of selection bias acted during the sample enrollment, given the several factors that influence the choice of the outpatient level of care vs. hospitalization. We only controlled the effect of gender, age, and psychiatric diagnosis on results by using pair matching without considering other potential confounding variables such as psychiatric comorbidity, physical illness, psychiatric familiarity, intrafamily issues, and traumatic events, which should be included in future research. The absence of assessment of the influence of other family factors (such as the number of family members, family income, and family beliefs) on interactive family dynamics is an additional limitation of the study. Finally, we did not consider other environmental factors such as negative peer relationships or school-related problems, which could contribute to mental health issues. The multi-informant and multi-method approach used in this study allows to overcome limitations connected to the exclusive use of self-report instruments, which may be influenced by individual biases such as social desirability or failure to understand questions. In conclusion, disentangling throughout multi-informant and multimethod evaluation the psychopathological, family, and NSSI-related characteristics of young patients with self-harm who required different levels of care (hospitalization vs. outpatient visits) is a promising research field with high clinical relevance for the advancement of the diagnostic and therapeutic process that characterizes daily clinical practice.
5 Conclusion
The current study highlighted that NSSI inpatients showed a more severe global clinical picture, confirming the need for a more severe level of care for this group. In fact, hospitalization represents a structural framework that works as a source of containment and support for young patients and their families that show greater difficulties for sustaining the child’s development at a certain time. The absence of group difference in NSSI-related characteristics suggested that NSSI should be considered an expression of a larger psychopathological picture, in which contextual factors such as family dynamics could play a role. Therefore, the need for a multi-informant and multi-method clinical assessment, which includes the investigation of environmental factors (e.g., family system and co-parenting system), is highlighted. Future research should further investigate the characteristics of family relationships of NSSI inpatients, using longitudinal studies that allow us to understand the changes of family dynamics over time.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by CESC protocol code n°0044914 of 13 July 2021. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
RF: Conceptualization, Data curation, Formal analysis, Writing – original draft. AR: Conceptualization, Data curation, Investigation, Writing – review & editing. MM: Investigation, Methodology, Writing – review & editing. MG: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Dotazione Ordinaria Ricerca dipartimentale Università di Padova: DOR. Open Access funding provided by Università degli Studi di Padova | University of Padua, Open Science Committee.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nock MK, Joiner TE Jr, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. (2006) 144:65–72. doi: 10.1016/j.psychres.2006.05.010
2. Poudel A, Lamichhane A, Magar KR, Khanal GP. Non suicidal self injury and suicidal behavior among adolescents: co-occurrence and associated risk factors. BMC Psychiatry. (2022) 22:96. doi: 10.1186/s12888-022-03763-z
3. Grandclerc S, De Labrouhe D, Spodenkiewicz M, Lachal J, Moro MR. Relations between nonsuicidal self-injury and suicidal behavior in adolescence: A systematic review. PLoS One. (2016) 11:e0153760. doi: 10.1371/journal.pone.0153760
4. Meszaros G, Horvath LO, Balazs J. Self-injury and externalizing pathology: a systematic literature review. BMC Psychiatry. (2017) 17:160. doi: 10.1186/s12888-017-1326-y
5. Sevecke K, Bock A, Fenzel L, Gander M, Fuchs M. Nonsuicidal self-injury in a naturalistic sample of adolescents undergoing inpatient psychiatric treatment: prevalence, gender distribution and comorbidities. Psychiatr Danub. (2017) 4:522–8. doi: 10.24869/psyd.2017.522
6. Cassels M, Wilkinson P. Non-suicidal self-injury in adolescence. J Paediatr Child Health. (2016) 26:554–8. doi: 10.1016/j.paed.2016.08.006
7. Gatta M, Dal Santo F, Rago A, Spoto A, Battistella PA. Alexithymia, impulsiveness, and psychopathology in nonsuicidal self-injured adolescents. Neuropsychiatr Dis Treat. (2016) 12:2307–17. doi: 10.2147/NDT.S106433
8. Giletta M, Scholte RH, Engels RC, Ciairano S, Prinstein MJ. Adolescent non-suicidal self-injury: a cross-national study of community samples from Italy, the Netherlands and the United States. Psychiatry Res. (2012) 197:66–72. doi: 10.1016/j.psychres.2012.02.009
9. Hauber K, Boon A, Vermeiren R. Non-suicidal self-injury in clinical practice. Front Psychol. (2019) 10:502. doi: 10.3389/fpsyg.2019.00502
10. Wang LJZ, Lan Y, Liu SJ, Yan WS. Impact of the COVID-19 and psychological risk factors on non-suicidal self-injury behavior among high school students: a one-year follow-up study. BMC Psychiatry. (2023) 23:512. doi: 10.1186/s12888-023-05021-2
11. Zetterqvist M, Jonsson LS, Landberg Å, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: A comparison of data from three different time points during 2011 - 2021. Psychiatry Res. (2021) 305:114208. doi: 10.1016/j.psychres.2021.114208
12. Sornberger MJ, Heath NL, Toste JR, McLouth R. Nonsuicidal self-injury and gender: patterns of prevalence, methods, and locations among adolescents. Suicide Life Threat Behav. (2012) 42:266–78. doi: 10.1111/j.1943-278X.2012.0088.x
13. Kukielka E. An analysis of nonsuicidal self-injury among children and adolescents in inpatient psychiatric hospitals and units in pennsylvania. Patient Saf (2689-0143). (2020) 2:30. doi: 10.33940/data/2020.9.3
14. Victor SE, Klonsky ED. Understanding the social context of adolescent nonsuicidal self-injury. J Clin Psychol. (2018) 74:2107–16. doi: 10.1002/jclp.22657
15. Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol. (2004) 72:885–90. doi: 10.1037/0022-006X.72.5.885
16. Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, Dickson JM. A meta-analysis of the prevalence of different functions of non-suicidal self-injury. J Affect Disord. (2018) 227:759–69. doi: 10.1016/j.jad.2017.11.073
17. Pollak OH, D'Angelo EJ, Cha CB. Does function predict persistence? Nonsuicidal self-injury among adolescents during and after hospitalization. Psychiatry Res. (2020) 286:112839. doi: 10.1016/j.psychres.2020.112839
18. García-Nieto R, Carballo JJ, Díaz de Neira Hernando M, de León-Martinez V, Baca-García E. Clinical correlates of non-suicidal self-injury (NSSI) in an outpatient sample of adolescents. Arch Suicide Res. (2015) 19:218–30. doi: 10.1080/13811118.2014.957447
19. Brausch AM, Muehlenkamp JJ. Perceived effectiveness of NSSI in achieving functions on severity and suicide risk. Psychiatry Res. (2018) 265:144–50. doi: 10.1016/j.psychres.2018.04.038
20. Laukkanen E, Rissanen ML, Tolmunen T, Kylmä J, Hintikka J. Adolescent self-cutting elsewhere than on the arms reveals more serious psychiatric symptoms. Eur Child Adolesc. Psychiatry. (2013) 22:501–10. doi: 10.1007/s00787-013-0390-1
21. Raffagnato A, Iannattone S, Fasolato R, Rossaro MP, Spoto A, Gatta M. Psycho-behavioral profiles of pediatric inpatients with past and recent onset of nonsuicidal self-injury: A cluster analysis approach. J Clin Med. (2022) 11:4602. doi: 10.3390/jcm11154602
22. In-Albon T, Bürli M, Ruf C, Schmid M. Non-suicidal self-injury and emotion regulation: a review on facial emotion recognition and facial mimicry. Child Adolesc Psychiatry Ment Health. (2013) 7:5. doi: 10.1186/1753-2000-7-5
23. Raffagnato A, Miscioscia M, Fasolato R, Iannattone S, Valentini P, Sale E, et al. Symptomatic, alexithymic, and suicidality-related features in groups of adolescent self-harmers: A case-control study. Eur J Investig Health Psychol Educ. (2023) 13:883–96. doi: 10.3390/ejihpe13050067
24. Greene D, Boyes M, Hasking P. The associations between alexithymia and both non-suicidal self-injury and risky drinking: A systematic review and meta-analysis. J Affect Disord. (2020) 260:140–66. doi: 10.1016/j.jad.2019.08.088
25. Andover MS, Morris BW. Expanding and clarifying the role of emotion regulation in nonsuicidal self-injury. Can J Psychiatry. (2014) 59:569–75. doi: 10.1177/070674371405901102
26. Rodav O, Levy S, Hamdan S. Clinical characteristics and functions of non-suicide self-injury in youth. Eur Psychiatry. (2014) 29:503–8. doi: 10.1016/j.eurpsy.2014.02.008
27. Zhou SC, Zhou Z, Tang Q, Yu P, Zou H, Liu Q, et al. Prediction of non-suicidal self-injury in adolescents at the family level using regression methods and machine learning. J Affect Disord. (2024) 352:67–75. doi: 10.1016/j.jad.2024.02.039
28. Miscioscia M, Angelico C, Raffagnato A, Gatta M. Psychopathological and interactive-relational characteristics in non-suicidal self-injury adolescent outpatients. J Clin Med. (2022) 11:1218. doi: 10.3390/jcm11051218
29. Thomassin K, Shaffer A, Madden A, Londino DL. Specificity of childhood maltreatment and emotion deficit in nonsuicidal self-injury in an inpatient sample of youth. Psychiatry Res. (2016) 244:103–8. doi: 10.1016/j.psychres.2016.07.050
30. Gatta M, Miscioscia M, Sisti M, Comis I, Battistella PA. Interactive family dynamics and non-suicidal self-injury in psychiatric adolescent patients: A single case study. Front Psychol. (2017) 8:46. doi: 10.3389/fpsyg.2017.00046
31. Victor SE, Hipwell AE, Stepp SD, Scott LN. Parent and peer relationships as longitudinal predictors of adolescent non-suicidal self-injury onset. Child Adolesc Psychiatry Ment Health. (2019) 13:1. doi: 10.1186/s13034-018-0261-0
32. Halstead RO, Pavkov TW, Hecker LL, Seliner MM. Family dynamics and self-injury behaviors: a correlation analysis. J Marital Fam Ther. (2014) 40:246–59. doi: 10.1111/j.1752-0606.2012.00336.x
33. Liang K, Zhao L, Lei Y, Zou K, Ji S, Wang R, et al. Nonsuicidal self-injury behaviour in a city of China and its association with family environment, media use and psychopathology. Compr Psychiatry. (2022) 115:152311. doi: 10.1016/j.comppsych.2022.152311
34. DeVille DC, Whalen D, Breslin FJ, Morris AS, Khalsa SS, Paulus MP, et al. Prevalence and family-related factors associated with suicidal ideation, suicide attempts, and self-injury in children aged 9 to 10 years. JAMA Netw Open. (2020) 3:e1920956. doi: 10.1001/jamanetworkopen.2019.20956
35. Wang Y, Luo B, Hong B, Yang M, Zhao L, Jia P. The relationship between family functioning and non-suicidal self-injury in adolescents: A structural equation modeling analysis. J Affect Disord. (2022) 309:193–200. doi: 10.1016/j.jad.2022.04.124
36. Freed RD, Rubenstein LM, Daryanani I, Olino TM, Alloy LB. The relationship between family functioning and adolescent depressive symptoms: the role of emotional clarity. J Youth Adolesc. (2016) 45:505–19. doi: 10.1007/s10964-016-0429-y
37. Sara G, Wu J, Uesi J, Jong N, Perkes I, Knight K, et al. Growth in emergency department self-harm or suicidal ideation presentations in young people: Comparing trends before and since the COVID-19 first wave in New South Wales, Australia. Aust N Z J Psychiatry. (2023) 57:58–68. doi: 10.1177/00048674221082518
38. Witt K, McGill K, Leckning B, Hill NTM, Davies BM, Robinson J, et al. Global prevalence of psychiatric in- and out-patient treatment following hospital-presenting self-harm: a systematic review and meta-analysis. EClinicalMedicine. (2023) 65:102295. doi: 10.1016/j.eclinm.2023.102295
39. Bridge JA, Olfson M, Caterino JM, Cullen SW, Diana A, Frankel M, et al. Emergency department management of deliberate self-harm: A national survey. JAMA Psychiatry. (2019) 76:652–4. doi: 10.1001/jamapsychiatry.2019.0063
40. Pompili M, Goracci A, Giordano G, Erbuto D, Girardi P, Klonsky ED, et al. Relationship of non-suicidal self-injury and suicide attempt: a psychopathological perspective. J Psychopathol. (2015) 21:348–53.
41. Plener PL, Brunner R, Fegert JM, Groschwitz RC, In-Albon T, Kaess M, et al. Treating nonsuicidal self-injury (NSSI) in adolescents: consensus based German guidelines. Child Adolesc Psychiatry Ment Health. (2016) 10:46. doi: 10.1186/s13034-016-0134-3
42. Golubchik P, Server J, Finzi-Dottan R, Kosov I, Weizman A. The factors influencing decision making on children's psychiatric hospitalization: a retrospective chart review. Community Ment Health J. (2013) 49:73–8. doi: 10.1007/s10597-012-9487-0
43. Glenn CR, Lanzillo EC, Esposito EC, Santee AC, Nock MK, Auerbach RP. Examining the course of suicidal and nonsuicidal self-injurious thoughts and behaviors in outpatient and inpatient adolescents. J Abnorm Child Psychol. (2017) 45:971–83. doi: 10.1007/s10802-016-0214-0
44. Conner KR, Langley J, Tomaszewski KJ, Conwell Y. Injury hospitalization and risks for subsequent self-injury and suicide: a national study from New Zealand. Am J Public Health. (2003) 93:1128–31. doi: 10.2105/ajph.93.7.1128
45. Adrian M, Zeman J, Erdley C, Whitlock K, Sim L. Trajectories of non-suicidal self-injury in adolescent girls following inpatient hospitalization. Clin Child Psychol Psychiatry. (2019) 24:831–46. doi: 10.1177/1359104519839732
46. Lalayants M, Kim M, Prince JD. Psychiatric hospitalization among adolescents. J Behav Health Ser R. (2018) 45:292–9. doi: 10.1007/s11414-017-9567-6
47. Wright DR, Katon WJ, Ludman E, McCauley E, Oliver M, Lindenbaum J, et al. Association of adolescent depressive symptoms with health care utilization and payer-incurred expenditures. Acad Pediatr. (2016) 16:82–9. doi: 10.1016/j.acap.2015.08.013
48. Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: findings from the TORDIA study. J Am Acad Child Adolesc Psychiatry. (2011) 50:772–81. doi: 10.1016/j.jaac.2011.04.003
49. Wolff JC, Davis S, Liu RT, Cha CB, Cheek SM, Nestor BA, et al. Trajectories of suicidal ideation among adolescents following psychiatric hospitalization. J Abnorm Child Psychol. (2018) 46:355–63. doi: 10.1007/s10802-017-0293-6
50. Gatta M, Raffagnato A, Iannattone S, Mistrorigo C, Fasolato R, Traverso A, et al. Hospitalisation in child neuropsychiatry: A case study along a five-year epidemiological-clinical trend. Clin Neuropsychiatry. (2022) 19:72–83. doi: 10.36131/cnfioritieditore20220201
51. Zanato S, Miscioscia M, Traverso A, Gatto M, Poli M, Raffagnato A, et al. A retrospective study on the factors associated with long-stay hospitalization in a child neuropsychiatry unit. Healthcare. (2021) 9:1241. doi: 10.3390/healthcare9091241
52. Rice JL, Tan TX. Youth psychiatrically hospitalized for suicidality: Changes in familial structure, exposure to familial trauma, family conflict, and parental instability as precipitating factors. Child Youth Serv Rev. (2017) 73:79–87. doi: 10.1016/j.childyouth.2016.12.006
53. Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families (2001).
54. Frigerio A, Vanzin L, Pastore V, Nobile M, Giorda R, Marino C, et al. The italian preadolescent mental health project (PrISMA): rationale and methods. Int J Methods Psychiatr Res. (2006) 15:22–35. doi: 10.1002/mpr.25
55. Pace CS, Muzi S, Frigerio A, Morganti W, Bianchi V, Rogier G. Twenty years of emotional-behavioral problems of community adolescents living in Italy measured through the Achenbach system of empirically based assessment (ASEBA): a systematic review and meta-analysis. Front Psychiatry. (2023) 14:1161917. doi: 10.3389/fpsyt.2023.1161917
56. Biederman J, Petty CR, Monuteaux MC, Evans M, Parcell T, Faraone SV, et al. The child behavior checklist-pediatric bipolar disorder profile predicts a subsequent diagnosis of bipolar disorder and associated impairments in ADHD youth growing up: a longitudinal analysis. J Clin Psychiatry. (2009) 70:732–40. doi: 10.4088/JCP.08m04821
57. Biederman J, Spencer T, Lomedico A, Day H, Petty CR, Faraone SV. Deficient emotional self-regulation and pediatric attention deficit hyperactivity disorder: a family risk analysis. Psychol Med. (2012) 42:639–46. doi: 10.1017/S0033291711001644
58. Frigerio A, Cattaneo C, Cataldo MG, Schiatti A, Molteni M, Battaglia M. Behavioral and emotional problems among italian children aged 4 to 18 years as reported by parents and teachers. Eur J Psychol Assess. (2004) 20:124–33. doi: 10.1027/1015-5759.20.2.124
59. Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children's global assessment scale (CGAS). Arch Gen Psychiatry. (1983) 40:1228–31. doi: 10.1001/archpsyc.1983.01790100074010
60. Schorre BEH, Vandvik IH. Global assessment of psychosocial functioning in child and adolescent psychiatry: A review of three unidimensional scales (CGAS, GAP, GAPD). Eur Child Adolesc Psychiatry. (2004) 13:273–86. doi: 10.1007/s00787-004-0390-2
61. Bressi C, Taylor G, Parker J, Bressi S, Brambilla V, Aguglia E, et al. Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: an Italian multicenter study. J Psychosom Res. (1996) 41:551–9. doi: 10.1016/s0022-3999(96)00228-0
62. Rieffe C, Oosterveld P, Terwogt MM. An alexithymia questionnaire for children: Factorial and concurrent validation results. Pers Individ Differ. (2006) 40:123–33. doi: 10.1016/j.paid.2005.05.013
63. Loas G, Braun S, Delhaye M, Linkowski P. The measurement of alexithymia in children and adolescents: Psychometric properties of the Alexithymia Questionnaire for Children and the twenty-item Toronto Alexithymia Scale in different non-clinical and clinical samples of children and adolescents. PLoS One. (2017) 12:e0177982. doi: 10.1371/journal.pone.0177982
64. Craparo G, Faraci P, Gori A. Psychometric properties of the 20-item toronto alexithymia scale in a group of italian younger adolescents. Psychiatry Investig. (2015) 12:500–7. doi: 10.4306/pi.2015.12.4.500
65. La Ferlita V, Bonadies M, Solano L, De Gennaro L, Gonini P. Alessitimia e adolescenza: studio preliminare di validazione della TAS-20 su un campione di 360 adolescenti italiani. Infanzia e adolescenza. (2007) 6:131–44.
67. Favez N, Scaiola CL, Tissot H, Darwiche J, Frascarolo F. The Family Alliance Assessment Scales: Steps toward validity and reliability of an observational assessment tool for early family interactions. J Child Fam Stud. (2011) 20:23–37. doi: 10.1007/s10826-010-9374-7
68. Parolin M, Sudati L, Gatta M, Simonelli A. L’Osservazione delle interazioni familiari in adolescenza: Studio preliminare sull’applicazione della procedura del Lausanne Trilogue Play. Psicol Clin Dello Svilupp. (2018) 22:269–98.
69. Ward-Ciesielski EF, Rizvi SL. The potential iatrogenic effects of psychiatric hospitalization for suicidal behavior: A critical review and recommendations for research. Clin Psychol (New York). (2021) 28:60–71. doi: 10.1111/cpsp.12332
70. Peterson AL, Chen JI, Karver MS, Labouliere CD. Frustration with feeling: Latent classes of non-suicidal self-injury and emotion regulation difficulties. Psychiatry Res. (2019) 275:61–70. doi: 10.1016/j.psychres.2019.03.014
71. You J, Ma C, Lin MP, Leung F. Comparing among the experiences of self-cutting, hitting, and scratching in Chinese adolescents attending secondary schools: An interview study. Behav Disord. (2015) 40:122–37. doi: 10.17988/BD-14-9.1
72. Stragliotto Bazzan J, Milbrath VM, Gabatz RIB, Cordeiro FR, Freitag VL, Schwartz E. The family's adaptation process to their child's hospitalization in an Intensive Care Unit. Rev Esc Enferm USP. (2020) 54:e03614. doi: 10.1590/S1980-220X2018056203614
73. Baird J, Davies B, Hinds PS, Baggott C, Rehm RS. What impact do hospital and unit-based rules have upon patient and family-centered care in the pediatric intensive care unit? J Pediatr Nurs. (2015) 30:133–42. doi: 10.1016/j.pedn.2014.10.001
74. Passos SDSS, Pereira Á, Nitschke RG. Routine of the family companion during hospitalization of a family member. Acta Paul Enferm. (2015) 28:539–45. doi: 10.1590/1982-0194201500090
75. Calkins SD, Propper C, Mills-Koonce WR. A biopsychosocial perspective on parenting and developmental psychopathology. Dev Psychopathol. (2013) 25:1399–414. doi: 10.1017/S0954579413000680
76. Criscuolo M, Marchetto C, Chianello I, Cereser L, Castiglioni MC, Salvo P, et al. Family functioning, coparenting, and parents' ability to manage conflict in adolescent anorexia nervosa subtypes. Fam Syst Health. (2020) 38:151–61. doi: 10.1037/fsh0000483
77. Gatta M, Sudati L, Sisti M, Miscioscia M, Calloni V, Simonelli A. Il ruolo delle interazioni familiari nell'espressione del disagio psichico in adolescenza: uno studio preliminare. Psicol Clin Dello Svilupp. (2017) 21:397–418. doi: 10.1449/88500
78. Hameed M, Hassan MA, Zafar S, Nazir S, Rehman RAU, Omayer A. The relationship between interparental conflict, distress tolerance and emotional dysregulation among adolescents. Am J Life Sci. (2023) 11:36–41. doi: 10.11648/j.ajls.20231103.11
Keywords: non-suicidal self-injury, psychopathology, adolescents, inpatients, outpatients, family dynamics
Citation: Fasolato R, Raffagnato A, Miscioscia M and Gatta M (2025) Non-suicidal self-injury in inpatient and outpatient adolescents: disentangling psychopathology and interactive family dynamics. Front. Psychiatry 15:1483745. doi: 10.3389/fpsyt.2024.1483745
Received: 20 August 2024; Accepted: 17 December 2024;
Published: 10 January 2025.
Edited by:
Yudong Shi, Chaohu Hospital of Anhui Medical University, ChinaReviewed by:
Zhensong Lan, Guangxi Medical University, ChinaRui Zhou, Guangzhou Red Cross Hospital, China
Qiuyu Yuan, Anhui Veterans Hospital, China
Copyright © 2025 Fasolato, Raffagnato, Miscioscia and Gatta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessia Raffagnato, YWxlc3NpYS5yYWZmYWduYXRvQHVuaXBkLml0
 Rachele Fasolato
Rachele Fasolato Alessia Raffagnato
Alessia Raffagnato Marina Miscioscia
Marina Miscioscia Michela Gatta
Michela Gatta