- 1Doctoral School in the Social Sciences, Jagiellonian University, Krakow, Poland
- 2Department of Crisis Intervention and Psychotherapy, Institute of Applied Psychology, Faculty of Management and Social Communication, Jagiellonian University, Krakow, Poland
Background: The clinical form of depersonalization affects approximately 1%–2% of the adult population. This study aimed to describe the symptoms of depersonalization in a non-clinical sample and to operationalize depersonalization as a regulatory mechanism. This article introduces the Depersonalization Mechanism Scale, 41-item measure developed to assess one’s tendency for depersonalization in response to overstimulation. The aim of the study is to explore how depersonalization mechanism is associated with cognitive and behavioral emotion regulation strategies, depression, and anxiety.
Method: The study included a sample of 300 Polish adults (149 men) from the general population, ranging in age from 18 to 60. Participants were administered the following questionnaires: Depersonalization Mechanism Scale (DMS), Behavioral Emotion Regulation Questionnaire (BERQ), Cognitive Emotion Regulation Questionnaire (CERQ), Occupational Depression Inventory (ODI), Patient Health Questionnaire (PHQ), and Trait Anxiety Scale (SL-C).
Results: An exploratory factor analysis revealed a two-factor structure of Depersonalization Mechanism Scale, with very high reliability coefficients for both subscales and full scale. A regression analysis revealed that depersonalization mechanism is a significant predictor of depressive symptoms. Depersonalization mechanism is strongly correlated with maladaptive regulation strategies such as withdrawal, ignoring, rumination, catastrophizing, self-blame, and blaming others. Weaker but significant connections were identified with certain adaptive strategies: acceptance, positive refocusing, putting into perspective, and seeking social support. Women were more prone to depersonalization than men.
Conclusions: Further research on depersonalization in non-clinical samples may improve understanding of this mechanism in the general population. This knowledge, combined with greater education about non-clinical forms of depersonalization, may support preventive programs against depression and professional assistance for people facing acute or chronic stressful life events.
Introduction
Difficulties in emotion regulation play an important role in the development and maintenance of psychopathology. Emotional dysregulation can be found in many mental health problems, including substance abuse, eating disorders, depression, or borderline personality disorder (1–4). Various definitions of emotion regulation can be found across literature, one of the most influential being the one proposed by Gross (5, 6). It is broadly defined as processes through which individuals monitor, evaluate, and modulate their emotions to adequately respond to environmental demands. Utilizing this framework, Folkman and Lazarus (7) introduced a distinction between problem- and emotion-focused coping, emphasizing the more adaptive value of problem-solving strategies. Gross’s model is especially useful in investigating the relationship between specific strategies and symptoms of clinical disorders (1, 4, 8, 9). Maladaptive strategies (e.g., rumination, suppression, or avoidance) are consistently found to be more strongly associated with anxiety, depression, eating disorders, and substance abuse (10, 11). To specify more precisely the subtleties among strategies, Garnefski et al. (12) and Kraij and Garnefski (13) proposed a distinction between cognitive and behavioral strategies. While catastrophizing, rumination, self-blame, and other-blame are seen as less adaptive, positive reappraisal, planning, and putting into perspective are described as more adaptive (14) and useful in dealing with life difficulties, depression, anxiety, or anger (15). Behavioral strategies also can be divided in the same way—adaptive strategies are seeking distraction, actively approaching, and seeking social support, as opposite to less adaptive withdrawal and ignoring. While some strategies are well described and studied, some remain unclear in terms of definition, functions, and adaptive value. Another problem is associated with grouping strategies in complex mechanisms such as depersonalization. We propose a different understanding of this phenomenon and investigate its relationship to specific emotion regulation strategies, anxiety, and depression.
In its clinical form, depersonalization is characterized by persistent or recurrent episodes of experiences of unreality, detachment, or being an outside observer of one’s thoughts, feelings, sensations, body, or actions (16). Two core components of depersonalization are detachment and hypoemotionality (emotional numbing or blunting) (17). An individual may feel as if in a dream or a game and may have a feeling of alienation from the reflection in the mirror. On a conscious level, a person recognizes themselves (“I know it is me”) but lacks an emotional connection to their image (“It doesn’t feel like me”), resulting in a profound sense of strangeness. Hypoemotionality refers to blunted affect: an individual remains capable of expressing emotions yet experiences them as strangely dampened.
This phenomenon can be described on a continuum, ranging from chronic, clinical form (depersonalization/derealization disorder), to transient episodes. Short-term experiences of depersonalization are mostly triggered by fatigue, anxiety, substance abuse, stress (18), or artificial induction (19) and are considered universal in the general population (20). Depersonalization appears in order to preserve adaptive behaviors (21) and allows to put off emotions and feelings that are too difficult to cope with and, therefore, tolerate the circumstances one is in (22).
We conceptualize depersonalization as an emotion regulation mechanism, broader than specific strategies. The use of word mechanism instead of strategy is not accidental—we suggest that a person can have at least some amount of control over which strategy to use in certain situation, while depersonalization is independent of the will. In the face of an overwhelming or demanding situation, depersonalization can “switch on” and provide a temporary relief. It distances an individual from their emotions and enables them to tolerate the challenges as long as needed. Despite short-term relief, it can exacerbate distress in the long run, potentially leading to emotional depletion, difficulties in maintaining relationships, and overall psychological distress. Regardless from clinical domain, we took inspiration from the burnout syndrome, where depersonalization is one of three core dimensions (23). In burnout, it is characterized as an increased mental distance to work, negativity, and work-related cynicism (24). On the one hand, clinical depersonalization withdraws a person from themselves; on the other, in burnout concept, it withdraws a person from other people and work-related context (25). We decided to merge these two ways of thinking and propose that trait-like depersonalization dampens emotional experiences and interferes with the ability to maintain personal relationships. If an individual has a problem accessing their emotions, feels distanced, it is hard to be empathetic and attentive. As a result, they have very little energy to engage in relationships and provide support or reciprocation of any kind. We believe that this type of depersonalization could be placed in the middle of the abovementioned continuum, offering a more comprehensive understanding of this phenomenon. We conceptualize it as a trait-like tendency to “activate” depersonalization in order to regulate one’s emotional state, which means certain individuals may be more prone to it than the others.
Since existing questionnaires focus on a clinical form of depersonalization, we decided to develop a new measurement tool (see Materials and methods). The aim of this paper is fourfold: (1) to propose a novel understanding of depersonalization as an emotion regulation mechanism; (2) to investigate relationships between depersonalization mechanism, cognitive and behavioral emotion regulation strategies, depression symptoms, and trait anxiety; (3) to explore behavioral and cognitive emotion regulation strategies as predictors of depersonalization mechanism; and 4) investigate whether depersonalization mechanism is a predictive factor for depression symptoms.
Materials and methods
Participants
The sample consisted of 300 Polish participants from the general population, meeting inclusion criteria: age 18–60. All participants were recruited by the Polish national research panel. Sample characteristics according to gender, age, and education are as follows: 151 women (50.3%) and 149 men (49.7%); 102 persons (34%) were between 46 and 60 years old, 86 persons (28.7%) between 36 and 45 years old, 70 persons (23.3%) were between 26 and 35 years old, and 42 persons (14%) were between 18 and 25 years old; 129 participants (43%) have received higher education, 167 persons (55.7%) finished high school or similar type of education, and four participants (1.3%) finished primary education. A total of 226 people (75.3%) were professionally active. Participants were asked to disclose any health problems; 151 participants (50.3%) had chronic illnesses (predominantly diabetes, high blood pressure, and asthma), and 146 participants (48.7%) were taking medication (mostly related to chronic illnesses). The sample was representative across all provinces of Poland.
Design and procedure
The research was carried out by the national research panel. At the beginning, respondents were asked about their gender, age, education, chronic illnesses, currently taken medication, and family risk factors. Then, they were provided with a set of questionnaires, described in detail in Measures. This study was carried out in accordance with the recommendations of the APA Ethics Code and Helsinki Declaration.
We constructed a new questionnaire that measures a tendency for depersonalization, named Depersonalization Mechanism Scale (DMS). During the developmental phase, we performed a pilot study, starting with an initial pool of 76 items. Items were inspired by already existing depersonalization scales, presenting satisfactory psychometric values: Dissociative Experiences Scale (26), Cambridge Depersonalization Scale (27), Depersonalization–Derealization Inventory (28), The Perceptual Alteration Scale (29), and The Dissociation Questionnaire (30). Moreover, some of the items were inspired by depersonalization subscales from burnout questionnaires: The Maslach Burnout Inventory–General Survey (MBI-GS) (23) (Cynicism subscale), Oldenburg Burnout Inventory (Disengagement subscale), and Link Burnout Questionnaire (25) (Deterioration of relations subscale). Initial 76 items were divided into three categories: 1) selected from the existing scales, for example, “I find my mind blank” from The Perceptual Alteration Scale (29); 2) items selected from the existing scales but with altered phrasing, for example, “I have the experience (…) instead of “Some people have the experience (…)” from Dissociative Experiences Scale (26); 3) created by the authors for example, “I feel that I have so little mental energy that I am able to do bare minimum when it comes to interacting with other people.” After the pilot study, redundant and weak loading items were reviewed or discarded. The 50-item version remained and was utilized during research. This version has undergone another psychometric evaluation and factor analysis (described in detail below, in Results, Factor analysis). The final version of the scale consists of 41 items (described in detail in the Measures). The scale is designed as self-report and can be administered to adults. A whole version of the scale is presented in Supplementary Materials.
As the aim of this study was to explore the relationships between depersonalization mechanism, cognitive and behavioral emotion regulation strategies, depression symptoms, and trait anxiety, several instruments were used: Cognitive Emotion Regulation Questionnaire and Behavioral Emotion Regulation Questionnaire to analyze associations with different emotion regulation strategies; Patient Health Questionnaire and Occupational Depression Inventory for employees to assess links with depression; and Trait Anxiety Scale to investigate the relationship between depersonalization mechanism and anxiety.
Measures
Depersonalization Mechanism Scale (DMS)
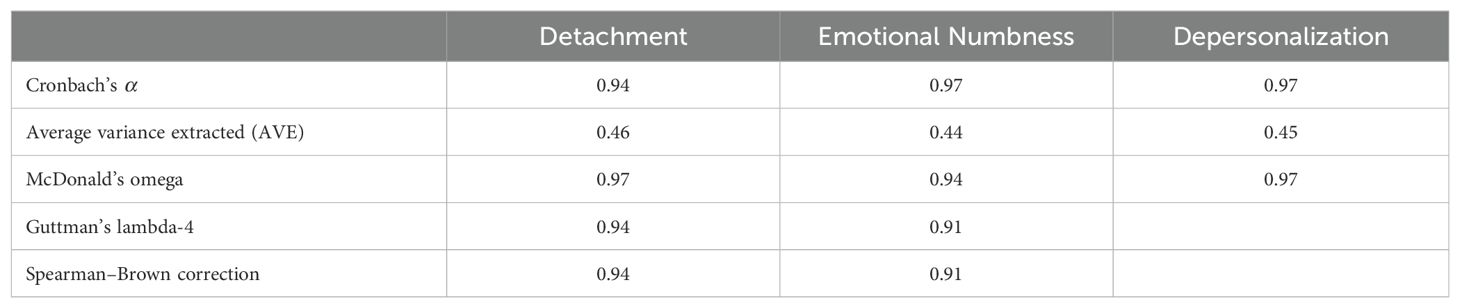
This is a 41-item, self-report measure designed to assess a tendency to depersonalization. It consists of two subscales: emotional numbness and detachment. Items are rated on 5-point Likert scale, ranging from 0 never to 4 always. A general score ranges from 0 to 164 with a higher score, indicating a higher tendency to depersonalization. The scale was originally constructed in Polish and translated into English by the authors. Reliability scores are presented in Table 1.
Cognitive Emotion Regulation Questionnaire
Cognitive Emotion Regulation Questionnaire (CERQ) (31) is a 36-item, self-report measure designed to assess nine cognitive emotion regulation strategies used in response to threatening or stressful life events. It consists of nine, four-item scales: self-blame, blaming others, acceptance, refocusing on planning, positive refocusing, rumination, positive reappraisal, putting into perspective, and catastrophizing. Items are rated on a 5-point Likert scale, ranging from 1 (almost) never to 5 (almost) always. Subscale scores range from 4 to 20 with higher scores indicating greater tendency to particular strategy. The psychometric characteristics of the original version indicate good reliability, with Cronbach’s α ranging from 0.75 to 0.86. In this study, Cronbach’s α of the Polish version of CERQ ranges from 0.73 to 0.85.
Behavioral Emotion Regulation Questionnaire
Behavioral Emotion Regulation Questionnaire (BERQ) (13) is a 20-item, self-report measure to designed to describe five behavioral coping strategies: seeking distraction, withdrawal, actively approaching, seeking social support, and ignoring. Each scale consists of four items rated on 5-point scale, ranging from 1 (almost) never to 5 (almost) always. Each subscale is scored from 4 to 20—the higher the scores, the stronger the behavioral strategy. The psychometric characteristics of the original version indicate good reliability, with Cronbach α ranging from 0.86 to 0.93 (13). In this study, Cronbach’s α of the Polish version of BERQ ranges from 0.80 to 0.94.
Occupational Depression Inventory
Occupational Depression Inventory (ODI) (32) is a nine-item, self-report measure designed to assess the severity of work-attributed depressive symptoms. It focuses on nine areas of depressive episodes (consistent with DSM-5 diagnostic criteria for major depressive disorder): anhedonia, depressed mood, sleep alterations, fatigue/loss of energy, appetite alterations, feelings of worthlessness, cognitive impairment, psychomotor alterations, and suicidal ideation. Additional question relates to work-related cause of depressive symptoms. Items are rated on a 4-point scale, ranging from 0 never or almost never to 3 nearly every day. In this study, Cronbach’s α of the Polish version is 0.94.
Patient Health Questionnaire
Patient Health Questionnaire (PHQ-9) (33) is a nine-item self-report measure to assess the depressive symptoms. Participants are asked how often they experienced described states during the last 2 weeks. Items are rated on a 4-point scale, ranging from not at all to nearly every day, and are scored from 0 to 3, respectively. The general scores range from 0 to 27 and refer to different levels of depression severity (from minimal to severe). In previous studies, Cronbach’s α revealed good reliability (e.g., 0.89) (34). In this study, Cronbach’s α is 0.92.
Trait Anxiety Scale—SL-C
Trait Anxiety Scale—SL-C (35) is a 15-item measure assessing the intensity of anxiety as a personality trait. This is an English version of a Polish scale (Skala Lęku–Cecha, SL-C). Trait anxiety is understood as a tendency to perceive a situation as threatening or to anticipate future events in terms of the danger that manifests through characteristic cognitive, emotional, and behavioral symptoms. Items are rated on a 4-point scale, from 3 (often) to 0 (never). The SL-C is a one-factor tool; the score ranges from 0 (minimum trait anxiety intensity) to 45 (maximum trait anxiety intensity). The original Cronbach’s α coefficient was 0.86. In this study, Cronbach’s α is 0.89.
Results
The analysis was carried out with IBM SPSS Statistics 25. The following analysis was performed: descriptive statistics with Kolmogorov–Smirnov test, Pearson r correlations, Student’s t-test for independent samples, Kruskal–Wallis test, and multiple regression analysis. Significance level was set at α = 0.05.
Descriptive statistics
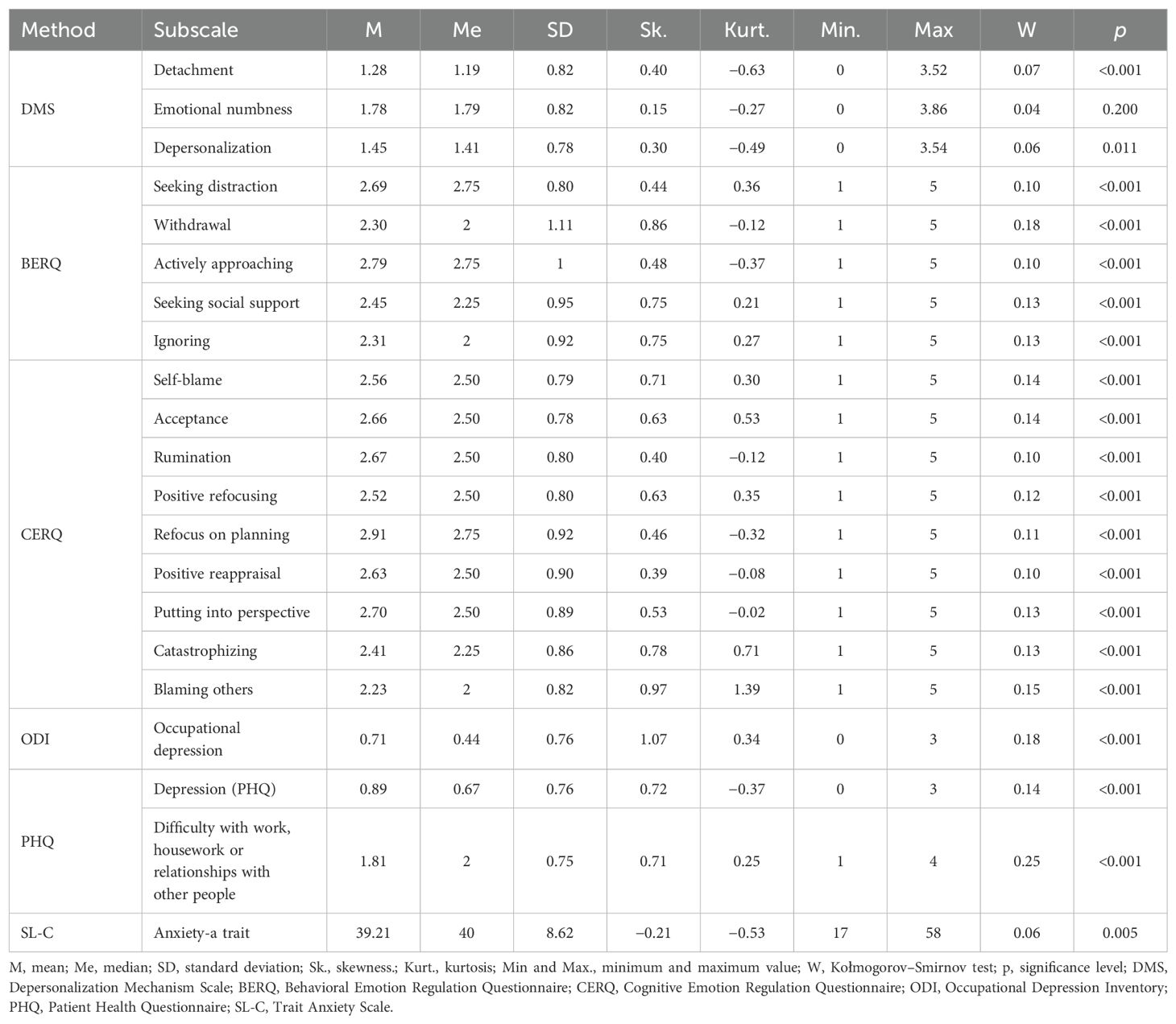
In the first step, descriptive statistics were calculated, along with Kołmogorov–Smirnov tests to determine distribution of variables. Apart from the emotional numbness subscale, all subscales significantly differed from normal distribution. Additional skewness tests were performed in order to verify whether they are between −/+2 standard deviations from the mean. In that case, it is safe to assume that the distribution is not significantly different from normal distribution (36). Based on the results presented in Table 2, it was decided to use parametric tests while fulfilling other assumptions.
Factor analysis
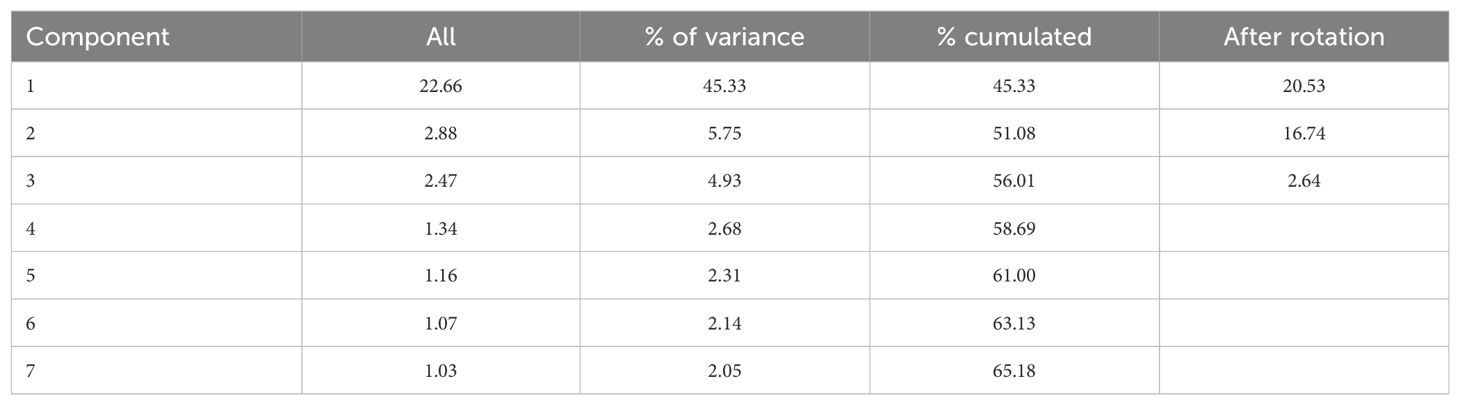
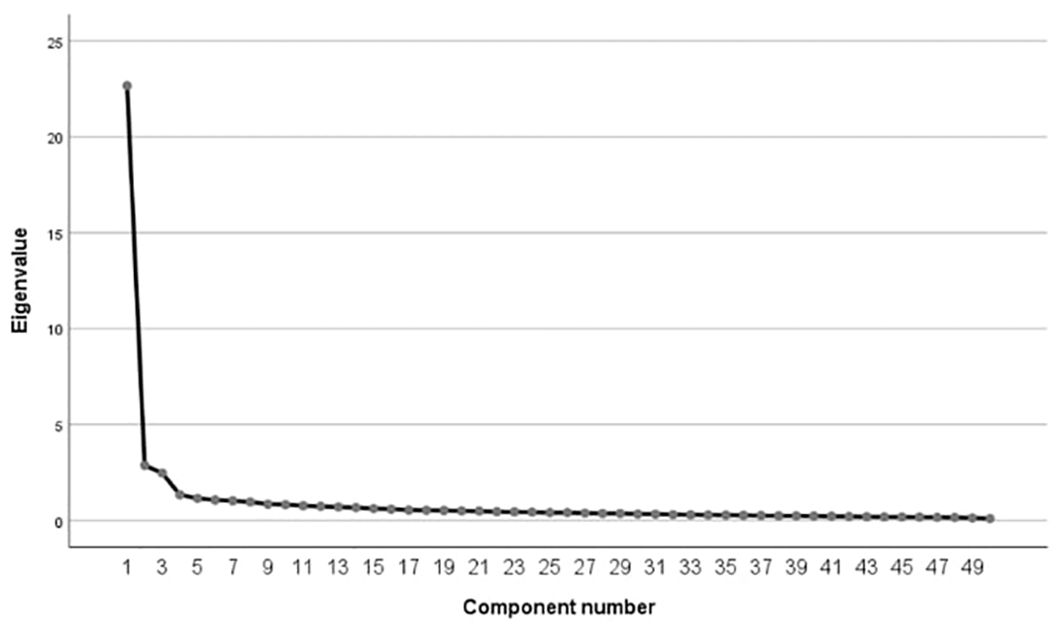
In order to determine psychometric values of the Depersonalization Mechanism Scale, principal component analysis with Oblimin rotation was performed. Sampling size was adequate—KMO = 0.96; Bartlett sphericity test [χ2(1,225) = 11,091.21; p < 0.001]. Seven factors had eigenvalue >1 (Table 3), but the scree plot showed three factors (Figure 1). Together, they explained 56.01% of variance.
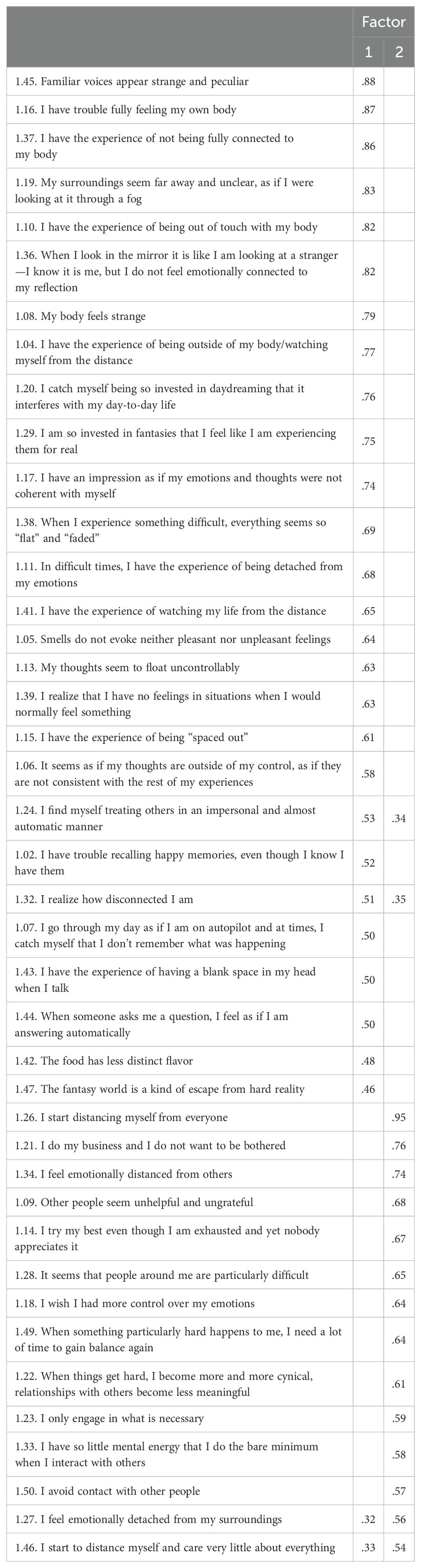
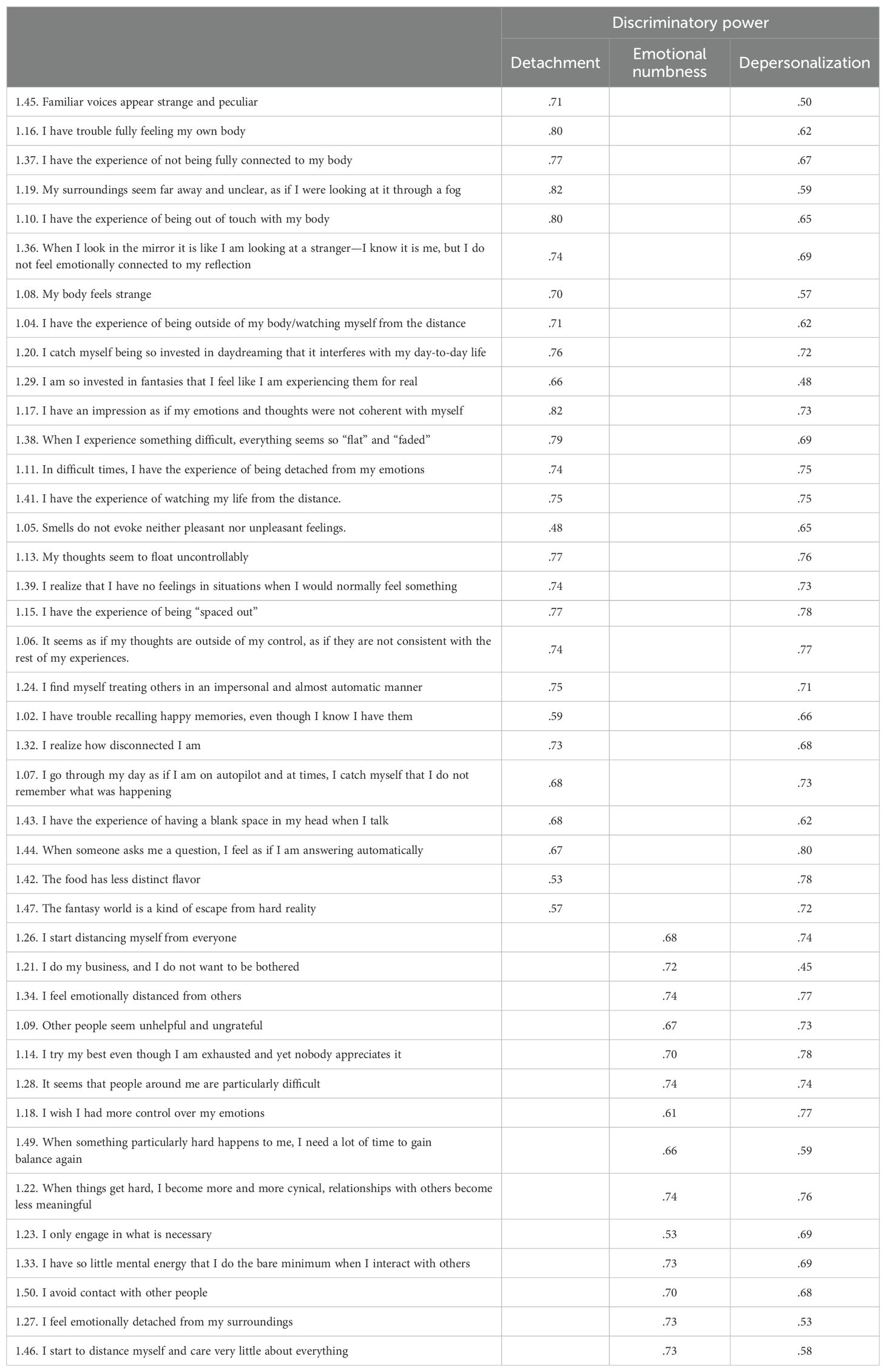
Factors 1 and 2 were strongly, positively correlated (r = 0.61), and Factor 3 was not correlated either with Factor 1 (r = −0.04) or Factor 2 (r = 0.03). We decided to remove items from Factor 3 along with five other items loading two factors at the same time. The final version of the scale consists of 41 items, organized into two subscales: detachment and emotional numbness (factor loadings are presented in Table 4). Discriminatory power of the items is presented in Table 5.
Average variance extracted (AVE) and composite reliability (CR)/McDonald’s omega (37) scores were calculated for both subscales and the whole scale—are presented in Table 1. Average variance extracted in all of all three measures falls under the acceptable level of 0.50. However, according to Fornell and Larcker (38), AVE may be a more conservative estimate of the validity and “on the basis of pn (composite reliability) alone, the researcher may conclude that the convergent validity of the construct is adequate, even though more than 50% of the variance is due to error” (p. 46). The composite reliability of all of the three constructs is above 0.90, so the internal reliability is deemed acceptable.
Correlations
Table 6 presents correlations between BERQ/CERQ and subscales of DMS (first and second column) and a whole scale (third column). Behavioral strategies positively correlated with depersonalization, except for actively approaching. Correlations ranged between 0.12 (seeking social support and depersonalization) and 0.70 (withdrawal and emotional numbness). The strongest correlations were found between all dimensions of depersonalization and withdrawal.
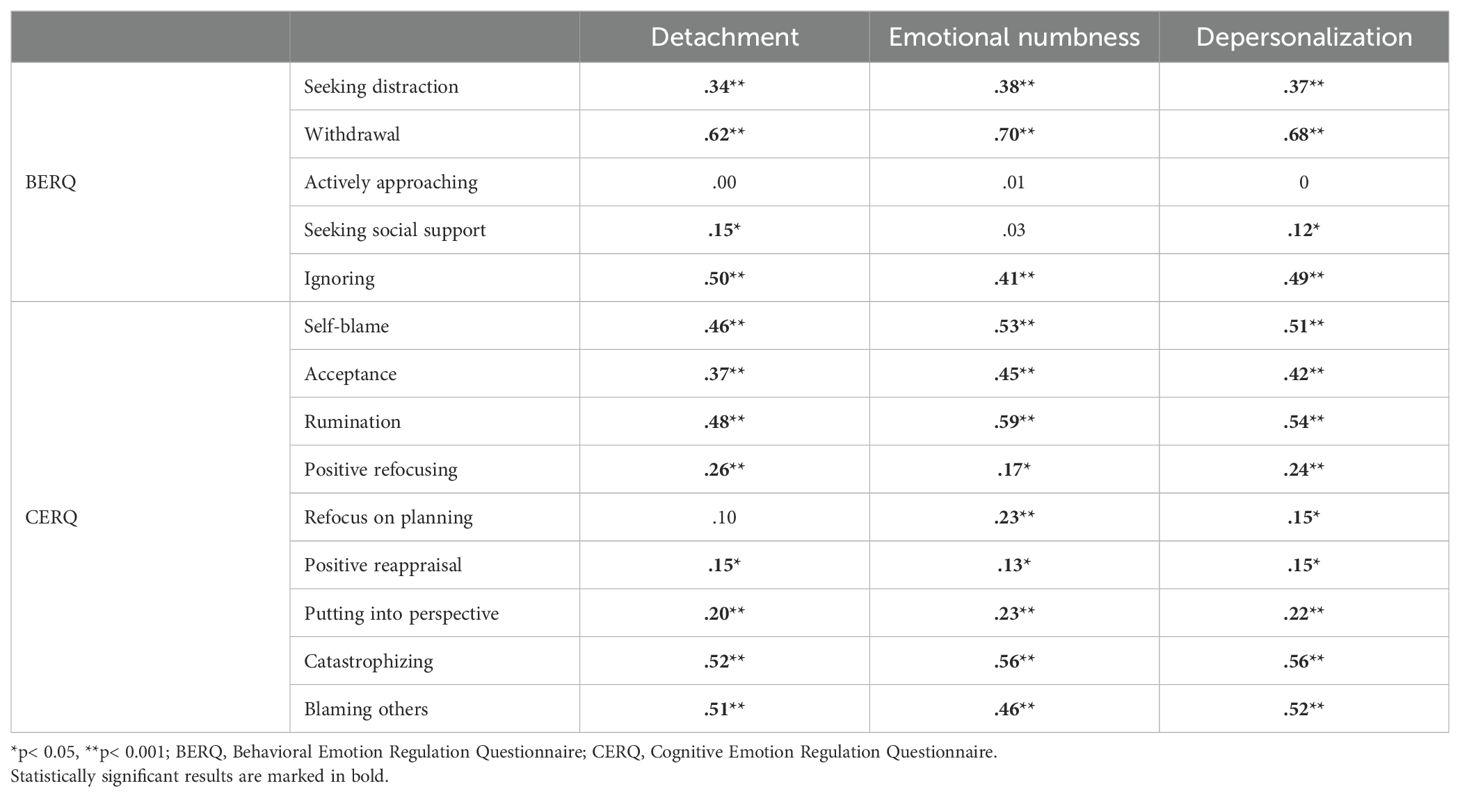
Table 6. Pearson correlations between depersonalization and cognitive and behavioral emotion regulation strategies.
All relationships between depersonalization and cognitive strategies were significant, except the one between refocus on planning and detachment. Correlations ranged between 0.13 (positive reappraisal and emotional numbness) and 0.59 (rumination and emotional numbness). The strongest correlations were found between all dimensions of depersonalization and two subscales of CERQ—rumination and catastrophizing.
Table 7 presents correlations between depersonalization and occupational depression, depressive symptoms, and trait anxiety. Correlations ranged between 0.47 (detachment and anxiety—trait) and 0.69 (depressive symptoms and depersonalization). All the correlations were significant; the strongest relationship was found between all aspects of depersonalization and depressive symptoms.
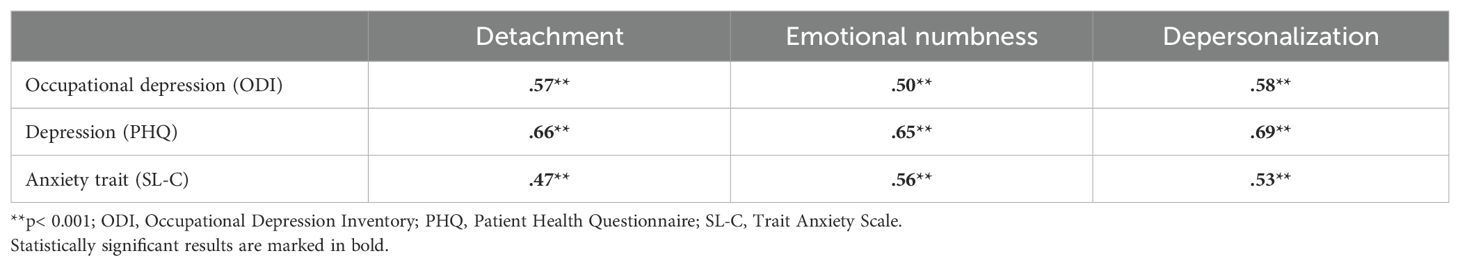
Table 7. Pearson correlations between depersonalization and depression (measured by ODI and PHQ) and anxiety trait.
Gender differences in depersonalization and emotion regulation strategies
Student’s t-test was performed in order to determine whether men and women differ in severity of depersonalization and emotion regulation strategies. Differences in the aspect of emotional numbness (t = 3.12; p = 0.002) and depersonalization (t = 2.04; p = 0.043) were found to be significant, with women being more prone than men to both. However, the effect size was small (d = 0.36 and d = 0.24, respectively). There were no differences in the aspect of detachment.
Behavioral and cognitive emotion regulation strategies were also considered. In our sample, women were more likely than men to use the following behavioral strategies: withdrawal (t = 2.37; p = 0.019), actively approaching (t = 2.48; p = 0.014), and seeking social support (t = 2.72; p = 0.007); other differences were insignificant. However, the effect size was small (d = 0.27, d = 0.29, d = 0.31, respectively). Regarding cognitive strategies, in our sample, women were more likely to use the following strategies: self-blame (t = 2.36; p = 0.019), acceptance (t = 2.65; p = 0.009), rumination (t = 4.73; p< 0.001), and refocus on planning (t = 2.20; p = 0.029 and catastrophizing (t = 3.33; p = 0.001); other differences were insignificant. Effect sizes were small (d = 0.27, d = 0.31, d = 0.25, d = 0.38, respectively), except for rumination, where the effect was medium (d = 0.50).
Multiple regression
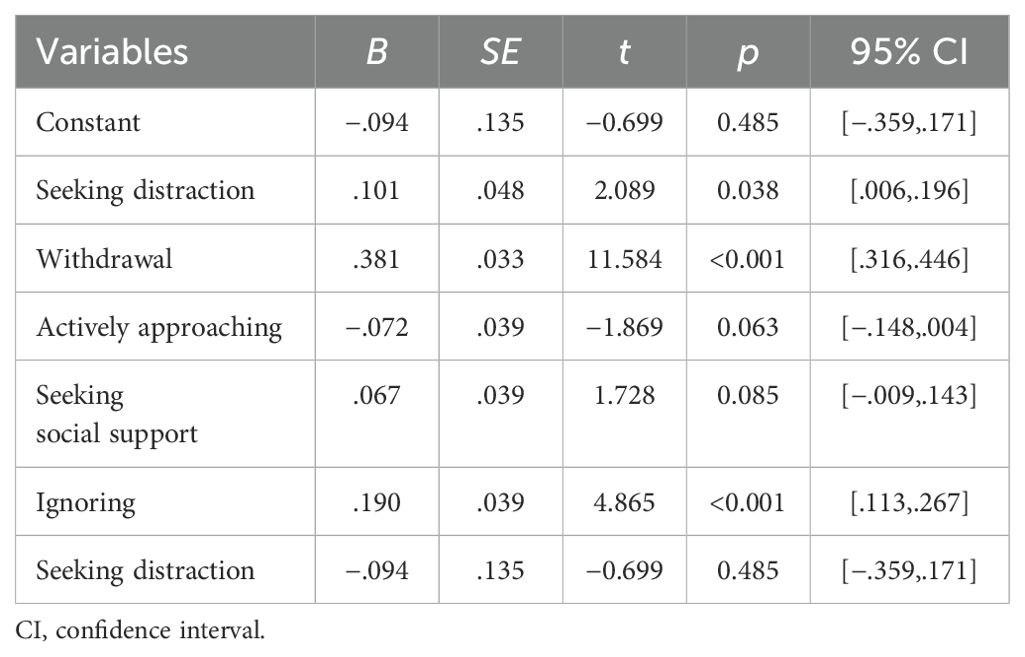
Multiple regression analyses were conducted to test if behavioral and cognitive emotion regulation strategies significantly predicted depersonalization. The results of the regression indicated that behavioral emotion regulation strategies explained 52% of the variance in depersonalization [R2Adjusted = .52, F(5,294) = 65.75, p < 0.001]. It was found that withdrawal (β = .38, p < 0.001), ignoring (β = .19, p < 0.001), and seeking distraction (β = .10, p = 0.038) significantly predicted depersonalization (Table 8).
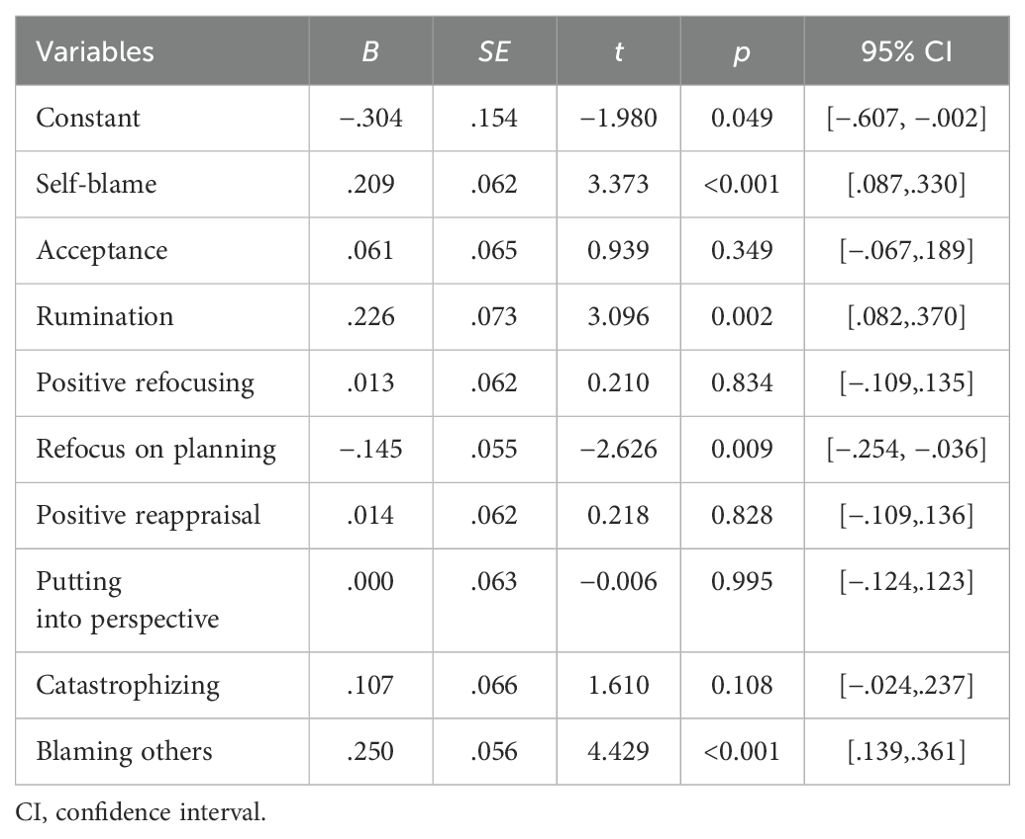
Further analysis revealed that cognitive emotion regulation strategies are significant predictors of depersonalization and explained 42% of the variance [R2Adjusted = .42, F(9,290) = 25.45, p < 0.001]. It was found that self-blame (β = .21, p < 0.001), blaming others (β = .25, p < 0.001), rumination (β = .23, p = 0.002), and refocus on planning (β = −.15, p = 0.009) were significant predictors of depersonalization (Table 9).
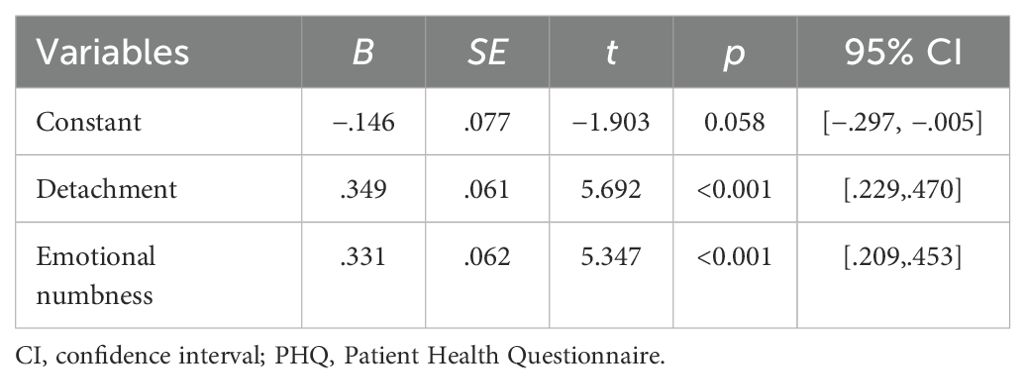
Subsequently, the two factors of depersonalization, i.e., detachment and emotional numbness, were tested to evaluate the extent to which depersonalization could predict symptoms of depression. The results of the regression analysis indicated that symptoms of depersonalization explained 48% of the variance [R2Adjusted = .48, F(2,297) = 137.37, p < 0.001]. It was found that both detachment (β = .35, p < 0.001) and emotional numbness (β = .33, p < 0.001) significantly predicted depression (Table 10).
A significant regression was also found in the context of occupational depression [R2Adjusted = .33, F(2,223) = 56.34, p < 0.001], indicating that depersonalization explained 33% of the variance (Table 11). In this analysis, only detachment was found as a significant predictor for occupational depression (β = .44, p < 0.001).
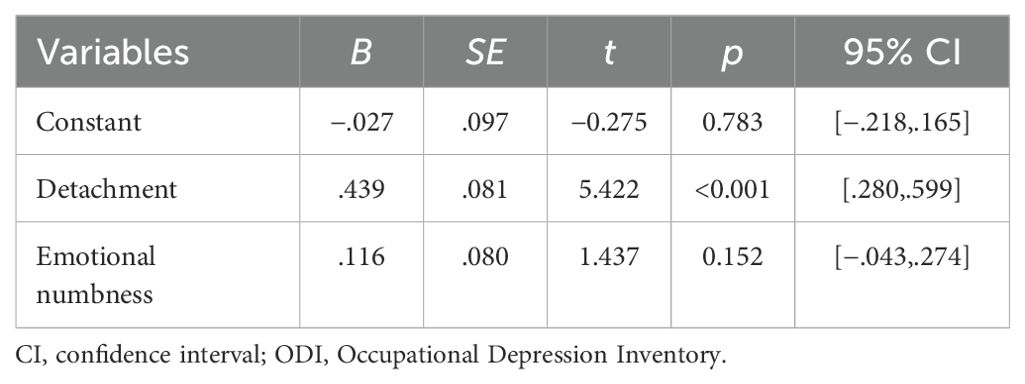
Table 11. Regression coefficients of symptoms of depersonalization on occupational depression (ODI).
Discussion
The aim of this paper was to introduce our understanding of depersonalization mechanism and its relationship with selected emotion regulation depression and anxiety. Moreover, our purpose was to investigate whether depersonalization acts as a predictive factor for depressive symptoms.
This work proposes a new measure that offers a deeper understanding of this complex phenomenon. The constructed method, the Depersonalization Mechanism Scale (DMS), comprises two subscales, namely, detachment and emotional numbness, both of high reliability (α = 0.97 and α = 0.94, respectively). The whole scale was also found to be highly reliable (α = 0.97) and applicable to adults in non-clinical population.
We aimed to shed light on depersonalization outside of strictly clinical context and normalize it as one of the possible mechanisms of emotional regulation. We propose that depersonalization mechanism is a non-voluntary, complex reaction that entails specific cognitive and behavioral strategies. The maladaptive function of depersonalization may be suggested by stronger correlation with less functional cognitive strategies, namely, self-blame, blaming others, rumination, and catastrophizing, and behavioral ones, namely, withdrawal and ignoring. However, due to significant correlations with more adaptive strategies (acceptance, positive refocusing, putting into perspective, positive reappraisal, seeking distraction and seeking social support), we may conclude that there are some positive aspects of depersonalization indicating adaptive characteristics of this mechanism. Depersonalization may provide short-term relief, especially important when we do not have the ability to change the situation that we must endure. The most important aspect of determining the adaptability of a given mechanism is determined by flexibility and adequacy of use.
It is worth noting that depersonalization cannot be reduced to avoidance only, which is confirmed by correlations with various emotion regulation strategies. This leads us to the conclusion that depersonalization is a complex mechanism of emotional regulation. Additionally, causes and motivation distinguish depersonalization from avoidance. Avoidant personality disorder is driven by feelings of inadequacy and intense fear of rejection (16), avoidance-based emotion regulation strategies are used to escape from unpleasant experiences (13), while depersonalization could be understood as a kind of “energy conservation” mechanism. We believe that adaptivity of such strategies is dependable on flexibility of use, the amount of control over it, the severity of consequences, among others.
Such perspective on depersonalization may lead to normalization of this specific response and help to better understand seemingly inadequate behaviors and attitudes. Furthermore, it may influence support and psychoeducation in the therapeutic interventions in patients who experience acute or chronic stress. The need to raise awareness among practitioners and the general population is particularly important in the light of the apparent rise in depersonalization symptoms (39, 40). Alterations in the sense of self with all of its consequences may constrain people’s ability to be more present and engaged in their lives. One of the possible results could be gradual drainage of social support network, essential for maintaining a sense of self (40).
Multiple regression analyses showed that behavioral and cognitive strategies play an important role in explaining depersonalization mechanism. The behavioral strategies explained a greater percentage of variance in depersonalization than cognitive ones. Among behavioral strategies, withdrawal, ignoring, and seeking distraction were significant predictors of depersonalization—the greater the level of these strategies, the stronger the symptoms of depersonalization. Cognitive strategies in regulating emotions revealed the similar pattern in relation to maladaptive strategies, namely, self-blame, blaming others, and rumination; the only one adaptive strategy that predicted the depersonalization was refocus on planning, which was negatively associated with depersonalization. It seems that planning may be more available in depersonalization than other adaptive cognitive strategies, like positive refocusing or positive reappraisal. This analysis helps to indicate specific emotion regulation strategies that may have a particular influence on strengthening depersonalization mechanism (i.e., withdrawal, ignoring, seeking distraction, self-blame, blaming others, and rumination), increasing the tendency to react in line with depersonalization characteristics and one cognitive strategy (i.e., refocus on planning) that may be crucial in limiting the tendency to depersonalization.
Another inspiring outcome of our analysis refers to the symptoms of depersonalization as predictors of depression. Gathered data indicate that, in a general context, both detachment and emotional numbness increase the symptoms of depression. Considering work-related context, it seems that detachment may play a crucial role in the development of occupational depression. Interestingly, “detachment” has stronger cognitive and behavioral connotations and is more prone to change than the “emotional numbness,” which is related stronger to emotions and the states caused by them. Expanding research on depersonalization in non-clinical groups could be beneficial for our understanding of this phenomenon. Combining this knowledge with increased awareness of non-clinical depersonalization could help in the development of preventive actions against depression and provide better professional support for those experiencing acute or prolonged stressful life situations.
There are several limitations to our study. We focused primarily on the description and characteristics of depersonalization in non-clinical population. Further studies should incorporate clinical samples analyzing the problem of depersonalization mechanism in different disorders. It is very important to identify individual dispositions (e.g., temperament, personality, sensory processing sensitivity) and contextual factors (e.g., family ties, traumas, social support) as possible predictors of depersonalization mechanism. In this study, basic correlations with anxiety and depression are reported; however, cause-and-effect relationships need to be studied to describe possible functions and consequences. Finally, further research on neurophysiological correlates of depersonalization can bring insight into the fundamental brain mechanisms. It would be especially valuable to use an experimental model to study different aspects of the depersonalization mechanism, like information processing in different conditions and stimuli characteristics.
The results of this study may be used in intervening programs, which could focus on developing skills in reducing strategies such as withdrawal, ignoring, distraction, blaming oneself or others, rumination on the one hand, and intensifying planning strategies on the other. It seems that precise selection of these strategies may allow for more accurate therapeutic interventions to reduce the tendency to depersonalization. It is particularly important in the light of the strong association between depersonalization and depression symptoms, both in non-professional and occupational contexts. Understanding the mechanisms of depersonalization may benefit in weakening this tendency with regard to strength and duration of being detached and emotionally numbed. The consciousness of potential depressive consequences seems to be a sufficient reason to deepen knowledge about the mechanisms of depersonalization.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
DF: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. KG: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The publication has been supported by a grant from the Faculty of Management and Social Communication under the Strategic Programme Excellence Initiative at Jagiellonian University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1481439/full#supplementary-material
References
1. Aldao A. Emotion regulation strategies as transdiagnostic processes: A closer look at the invariance of their form and function. Rev Psicol Patol Psicol Clin. (2012) 17:261–78. doi: 10.5944/rppc.vol.17.num
2. Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. (2010) 30:217–37. doi: 10.1016/j.cpr.2009.11.004
3. Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clin Psychol Rev. (2015) 40:111–22. doi: 10.1016/j.cpr.2015.05.010
4. Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clin Psychol Rev. (2017) 57:141–63. doi: 10.1016/j.cpr.2017.09.002
5. Gross JJ. Antecedent- and response-focused emotion regulation: Divergent consequences for experience, expression, and physiology. J Pers Soc Psychol. (1998) 74:224–37. doi: 10.1037//0022-3514.74.1.224
6. Gross JJ. The emerging field of emotion regulation: An integrative review. Rev Gen Psychol. (1998) 2:271–99. doi: 10.1037//1089-2680.2.3.271
7. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer Publishing Company (1984).
8. Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behav Res Ther. (2010) 48:974–83. doi: 10.1016/j.brat.2010.06.002
9. D’Avanzato C, Joormann J, Siemer M, Gotlib IH. Emotion regulation in depression and anxiety: Examining diagnostic specificity and stability of strategy use. Cognit Ther Res. (2013) 37:968–80. doi: 10.1007/s10608-013-9537-0
10. Aldao A, Nolen-Hoeksema S. When are adaptive strategies most predictive of psychopathology? J Abnorm Psychol. (2012) 121:276–81. doi: 10.1037/a0023598
11. Garnefski N, Hossain S. Relationships between maladaptive cognitive emotion regulation strategies and psychopathology in adolescents from Bangladesh. Arch Depress Anxiety. (2017) 3:23–9. doi: 10.17352/2455-5460.000019
12. Garnefski N, van den Kommer T, Kraaij V, Teerds J, Legerstee J, Onstein E. The relationship between cognitive emotion regulation strategies and emotional problems. Eur J Pers. (2002) 16:403–20. doi: 10.1002/per.458
13. Kraaij V, Garnefski N. The Behavioral Emotion Regulation Questionnaire: Development, psychometric properties and relationships with emotional problems and the Cognitive Emotion Regulation Questionnaire. Pers Individ Dif. (2019) 137:56–61. doi: 10.1016/j.paid.2018.07.036
14. Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Pers Individ Dif. (2006) 40:1659–69. doi: 10.1016/j.paid.2005.12.009
15. Kraaij V, Garnefski N, de Wilde EJ, Dijkstra A, Gebhardt W, Maes S, et al. Negative life events and depressive symptoms in late adolescence: bonding and cognitive coping as vulnerability factors? J Youth Adolesc. (2003) 32:185–93. doi: 10.1023/a:1022543419747
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013).
17. Simeon D. Depersonalisation disorder: A contemporary overview. CNS Drugs. (2004) 18:343–54. doi: 10.2165/00023210-200418060-00002
18. Hunter EC, Salkovskis PM, David AS. Attributions, appraisals and attention for symptoms in depersonalisation disorder. Behav Res Ther. (2014) 53:20–9. doi: 10.1016/j.brat.2013.11.005
19. Dewe H, Watson DG, Kessler K, Braithwaite JJ. The depersonalized brain: New evidence supporting a distinction between depersonalization and derealization from discrete patterns of autonomic suppression observed in a non-clinical sample. Conscious Cogn. (2018) 63:29–46. doi: 10.1016/j.concog.2018.06.008
20. Hunter EC, Sierra M, David AS. The epidemiology of depersonalisation and derealisation. A systematic review. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:9–18. doi: 10.1007/s00127-004-0701-4
21. Sierra M, Berrios GE. Depersonalization: neurobiological perspectives. Biol Psychiatry. (1998) 44:898–908. doi: 10.1016/s0006-3223(98)00015-8
23. Maslach C, Jackson SE, Leiter MP. The Maslach Burnout Inventory – General Survey Manual. 3rd ed. Palo Alto, CA: Consulting Psychologist Press (1996).
24. World Health Organization. Burn-out an “occupational phenomenon”: International Classification of Diseases (2019). Available online at: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (Accesed May 15, 2024).
25. Golonka K, Mojsa-Kaja J, Blukacz M, Gawłowska M, Marek T. Occupational burnout and its overlapping effect with depression and anxiety. Int J Occup Med Environ Health. (2019) 32:229–44. doi: 10.13075/ijomeh.1896.01323
26. Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J nervous Ment disease. (1986) 174:727–35. doi: 10.1097/00005053-198612000-00004
27. Sierra M, Berrios GE. The Cambridge Depersonalisation Scale: A new instrument for the measurement of depersonalisation. Psychiatry Res. (2000) 93:153–64. doi: 10.1016/s0165-1781(00)00100-1
28. Cox BJ, Swinson RP. Instrument to assess depersonalization-derealization in panic disorder. Depress Anxiety. (2002) 15:172–5. doi: 10.1002/da.10051
29. Sanders S. The Perceptual Alteration Scale: A scale measuring dissociation. Am J Clin Hypn. (1986) 29:95–102. doi: 10.1080/00029157.1986.10402691
30. Vanderlinden J, Van Dyck R, Vandereycken W, Vertommen H, Verkes JR. The dissociation questionnaire (DIS-Q): Development and characteristics of a new self-report questionnaire. Clin Psychol Psychother. (1993) 1:21–7. doi: 10.1002/cpp.5640010105
31. Garnefski N, Kraaij V, Spinhoven P. Negative life events, cognitive emotion regulation and emotional problems. Pers Individ Dif. (2001) 30:1311–27. doi: 10.1016/S0191-8869(00)00113-6
32. Bianchi R, Schonfeld IS. The Occupational Depression Inventory: A new tool for clinicians and epidemiologists. J Psychosom Res. (2020) 138:110249. doi: 10.1016/j.jpsychores.2020.110249
33. Spitzer RL. Utility of a new procedure for diagnosing mental disorders in primary care. JAMA. (1994) 272:1749. doi: 10.1001/jama.1994.03520220043029
34. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
35. Piksa M, Kosiorowska E, Golonka K. Skala Lęku - Cecha (SL-C). ResearchGate (2020). doi: 10.13140/RG.2.2.17148.36484/3
36. George D, Mallery P. IBM SPSS Statistics 25 Step by Step: A Simple Guide and Reference. 15th ed. New York (NY): Routledge (2019).
37. Cheung GW, Cooper-Thomas HD, Lau RS, Wang LC. Reporting reliability, convergent and discriminant validity with structural equation modeling: A review and best-practice recommendations. Asia Pac J Manage. (2024) 41:745–83. doi: 10.1007/s10490-023-09871-y
38. Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Market Res. (1981) 18:39–50. doi: 10.2307/3151312
39. Escolà-Gascón Á, Marín FX, Rusiñol J, Gallifa J. Pseudoscientific beliefs and psychopathological risks increase after COVID-19 social quarantine. Global Health. (2020) 16. doi: 10.1186/s12992-020-00603-1
Keywords: depersonalization, depression, emotions, regulation strategies, non-clinical sample, measurement of depersonalization
Citation: Fortuna D and Golonka K (2024) When you avoid your feelings, you may feel even worse: how depersonalization puts you at risk of depression. Front. Psychiatry 15:1481439. doi: 10.3389/fpsyt.2024.1481439
Received: 15 August 2024; Accepted: 20 September 2024;
Published: 17 October 2024.
Edited by:
Ali Saffet Gonul, Ege University, TürkiyeReviewed by:
Wahyu Rahardjo, Gunadarma University, IndonesiaWilliam Barbosa Gomes, Federal University of Rio Grande do Sul, Brazil
Copyright © 2024 Fortuna and Golonka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Krystyna Golonka, a3J5c3R5bmEuZ29sb25rYUB1ai5lZHUucGw=
 Dominika Fortuna
Dominika Fortuna Krystyna Golonka
Krystyna Golonka