- 1School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Shanghai Jiao Tong University of Medicine, Shanghai, China
- 3Shanghai Jing’an District Jiangning Road Community Health Service Center, Shanghai, China
- 4Department of General Practice, Yangpu Hospital, Tongji University School of Medicine, Shanghai, China
- 5Department of Social Medicine and Health Management, School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Objective: This study aims to investigate the prevalence of smartphone addiction, physical activity levels, and depressive symptoms among secondary school students, and to analyze the combined impact of smartphone addiction and physical activity on depressive symptoms.
Methods: A cluster sampling method was employed in two secondary schools in the Jing’an District of Shanghai, China. Univariate analysis was used to compare the prevalence of depressive symptoms across different demographic characteristics. Logistic regression was utilized to examine the associations between smartphone addiction, physical activity, and their combined effect on depressive symptoms.
Results: A total of 1,316 respondents participated in the study, with reported prevalence rates of depressive symptoms (36.2%), smartphone addiction (19.2%), and insufficient physical activity (23.3%). Risk factors for depressive symptoms included being a non-only child (OR=1.421, 95% CI: 1.090-1.853, P=0.009), inadequate sleep duration (OR=2.722, 95% CI: 2.070-3.578, P<0.001) and smartphone addiction (OR=2.173, 95% CI: 1.621-2.913, P < 0.001). Adolescents with smartphone addiction were significantly more likely to report depressive symptoms compared to those without (OR=2.173, 95% CI: 1.621-2.913, P < 0.001). Joint analysis indicated that combined smartphone addiction and insufficient physical activity significantly increased the risk of depressive symptoms (OR=2.781, 95% CI: 1.627-4.753, P < 0.001).
Conclusion: The study identified a high prevalence of severe smartphone addiction, insufficient physical activity, and elevated rates of depressive symptoms among secondary school students. Smartphone addiction and inadequate physical activity were associated with increased likelihood of depressive symptoms. Moreover, higher levels of physical activity appeared to mitigate the adverse impact of smartphone addiction on depressive symptoms.
1 Introduction
In recent decades, as wireless network technology has become more pervasive and smartphone functionalities have advanced, there has been a noticeable trend towards younger individuals using smartphones. This trend has brought to light the issue of smartphone addiction among adolescents. Smartphone addiction is characterized by an inability to control phone use (1), leading to physiological issues like headaches and difficulty concentrating, as well as emotional challenges such as anxiety, depression, and reduced social adaptability (2, 3).Research has indicated that the global reporting rate of smartphone addiction was 28.3%, with variations observed across different cultural backgrounds, ranging from 10% to 31% (4). Eastern cultural backgrounds tend to report higher rates of smartphone addiction compared to Western cultures (5).
Another issue associated with smartphone addiction is the insufficient physical activity observed among adolescents globally (6). This lack of activity hinders the attainment of normal growth and development standards and has emerged as a significant public health concern. Research highlighted by Hallal showed that over 80% of adolescents worldwide failed to achieve the recommended 60 minutes of moderate-to-vigorous physical activity daily (7).
These aforementioned issues may be closely related to depression among adolescents. Depression, as one of the most prevalent mental disorders, affects approximately 350 million people of various ages worldwide. It is anticipated that by 2030, depression will constitute the largest global disease burden, posing a significant public health challenge to the international community (8). Adolescent depression is often considered to be a precursor of the adult depression and can lead to enduring social and psychological harm (9). Adolescents are particularly vulnerable to depression due to genetic, social, and environmental factors, resulting in a higher incidence compared to other age groups. Recent studies indicated a strong correlation between smartphone addiction, insufficient physical activity and psychological symptoms such as anxiety and depression. Tang et al. (2018) observed that adolescents and young adults addicted to mobile phones exhibited increased mental vulnerability, heightening their risk of depression (10). Additionally, individuals in Asian countries with smartphone addiction tended to have higher rates of depression compared to those in the United States. This suggested that cultural factors and environmental context should also not be ignored when exploring the impact of smartphone addiction and physical inactivity on adolescent mental health. Research among British adolescents aged 11-14 revealed a negative association between physical activity and depressive symptoms: increasing weekly exercise by 60 minutes reduced the risk of developing depressive symptoms by 8% (11). Furthermore, Kim et al. (2020) demonstrated that moderate-to-vigorous physical activity moderates the relationship between screen time and depressive symptoms (12). Studies on Chinese college students by Feng et al. (2014) and Wu et al. (2015) similarly found that those with both smartphone addiction and insufficient physical activity had a higher likelihood and severity of depressive symptoms (13, 14). However, there remains a paucity of research investigating the combined impact of smartphone addiction and insufficient physical activity on depressive symptoms, particularly in adolescents.
This study examined the prevalence of smartphone addiction, physical activity level, and depressive symptoms among secondary school students. It analyzed how smartphone addiction and insufficient physical activity impacted depressive symptoms. Additionally, it explored whether increased physical activity could mitigate the negative effects of smartphone addiction on depressive symptoms. The aim of this study is to provide insights for effective interventions targeting adolescent depression.
2 Materials and methods
2.1 Participants
A cross-sectional survey was conducted in Shanghai from November to December 2023. Using a cluster sampling method, the research team collaborated with two secondary schools in Jing ‘an District, Shanghai, an economically developed area in China. Participants included students from grades 6, 7,and 8 in junior secondary school, and grades 10 and 11 in senior secondary school. Students in grades 9 and 12 were excluded due to the transition pressures associated with higher education. After obtaining the consent of all participants and their legal guardians, all eligible participants independently completed the questionnaire including demographic information. In addition, variables for student height and weight were obtained by physical examination of the students. Gender, age, type of school, type of family structure, one-child status, BMI, and sleep duration were all included as control variables in the regression of smartphone addiction, physical activity, and depressive symptoms. A total of 1,327 students participated, with 1,316 providing valid responses (effective response rate: 99.2%).
2.2 Ethical approval
The research adhered to local legislation and institutional requirements.
2.3 Measures
2.3.1 Smartphone addiction
Smartphone addiction was assessed using the Smartphone Addiction Scale Short-Version (SAS-SV) modified by Kwon, based on the Smartphone Addiction Scale (SAS) (15). Xiang et al. (16)revised this scale in Chinese in 2019, and conducted a reliability and validity test in adolescents, and the results showed that the scale had good reliability and validity in adolescents. Mu et al. also used the Chinese version of the scale to investigate smartphone addiction in their study, and verified Cronbach’s α =0.92 (17).The scale consists of 10 items rated on a 6-point Likert scale (1 = strongly disagree to 6 = strongly agree), yielding a total score ranging from 10 to 60. Scores > 32 indicated smartphone addiction. The Cronbach’s α coefficient for reliability was 0.920.
2.3.2 Physical activity level
The physical activity level was assessed using the Chinese University of Hong Kong: Physical Activity Rating for Children and Youth (CUHK-PARCY) scale. The CUHK-PARCY scale was adapted based on the Jackson Activity Coding and the Godin-Shephard Activity Questionnaire (18, 19). It encompasses a range of 11 physical activity levels, from complete inactivity (0 points) to vigorous exercise (10 points), demonstrating robust validity and aggregate reliability. In this study, scores on the CUHK-PARCY questionnaire were categorized as follows: scores of 0-2 indicated insufficient physical activity, scores of 3-6 denoted a moderate physical activity level, and scores of 7-10 represented a high physical activity level (20).
2.3.3 Depressive symptoms
Depressive symptoms were assessed by using the Self-rating Depression Scale (SDS) developed by Zung, consisting of 20 items rated on a 4-point scale (1 = none or rare to 4 = most or all the time) (21). The scale includes both positive and reverse-scored items, with the total scores summed to obtain the raw score. The standard score is derived by multiplying the total raw score by 1.25, resulting in an integer score. A standard score higher than 53 indicates the presence of depressive symptoms. In this study, the Cronbach’s α coefficient for the SDS was calculated to be 0.886.
2.4 Statistical analysis
Statistical analysis was performed using IBM SPSS 26.0 software. Differences in depressive symptoms among adolescents with various characteristics were assessed using the χ2 test. Binary logistic regression was employed for both univariate and multivariate analyses to investigate the independent effects of smartphone addiction and physical activity on adolescent depressive symptoms, calculating Odds Ratios (OR) across different groups. To explore the combined effects of smartphone addiction and physical activity on depressive symptoms, the two behaviors were categorized into 6 groups (2 smartphone addiction groups × 3 physical activity level groups). The non-smartphone addiction, high physical activity group served as the reference to compare the risk of depressive symptoms across different groups of smartphone addiction and physical activity level.
3 Results
3.1 Basic information of study subjects
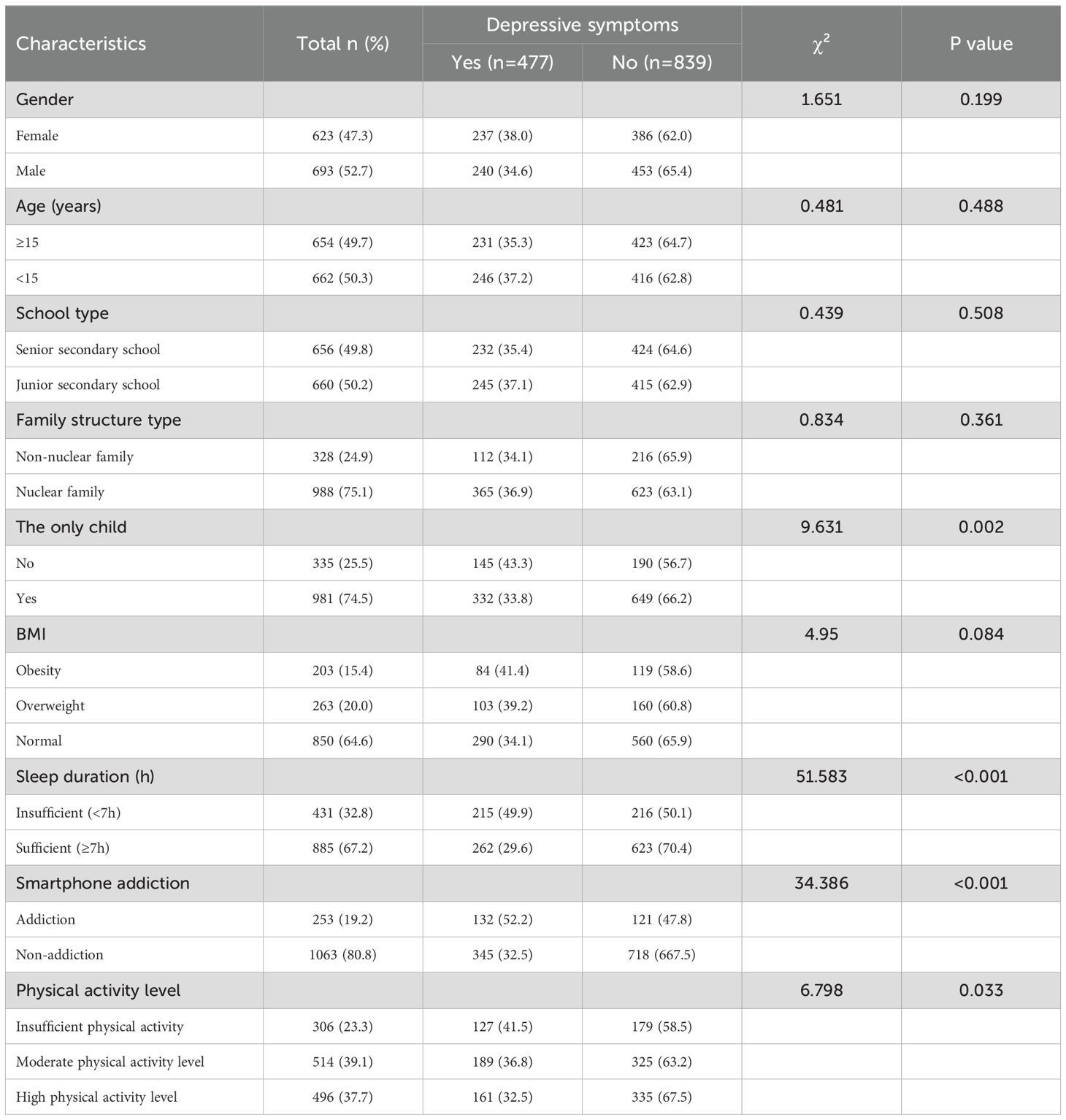
Table 1 presented data on the 1,316 participants, with 623 (47.3%) identified as female and 693 (52.7%) as male. Depressive symptoms were reported in 477 participants, constituting 36.2% of the total sample. Smartphone addiction was observed in 253 participants (19.2%). Regarding physical activity levels, the distribution from highest to lowest was moderate (39.1%), high (37.7%), and insufficient (23.3%) physical activity groups.
3.2 Influencing factors of depressive symptoms in secondary school students
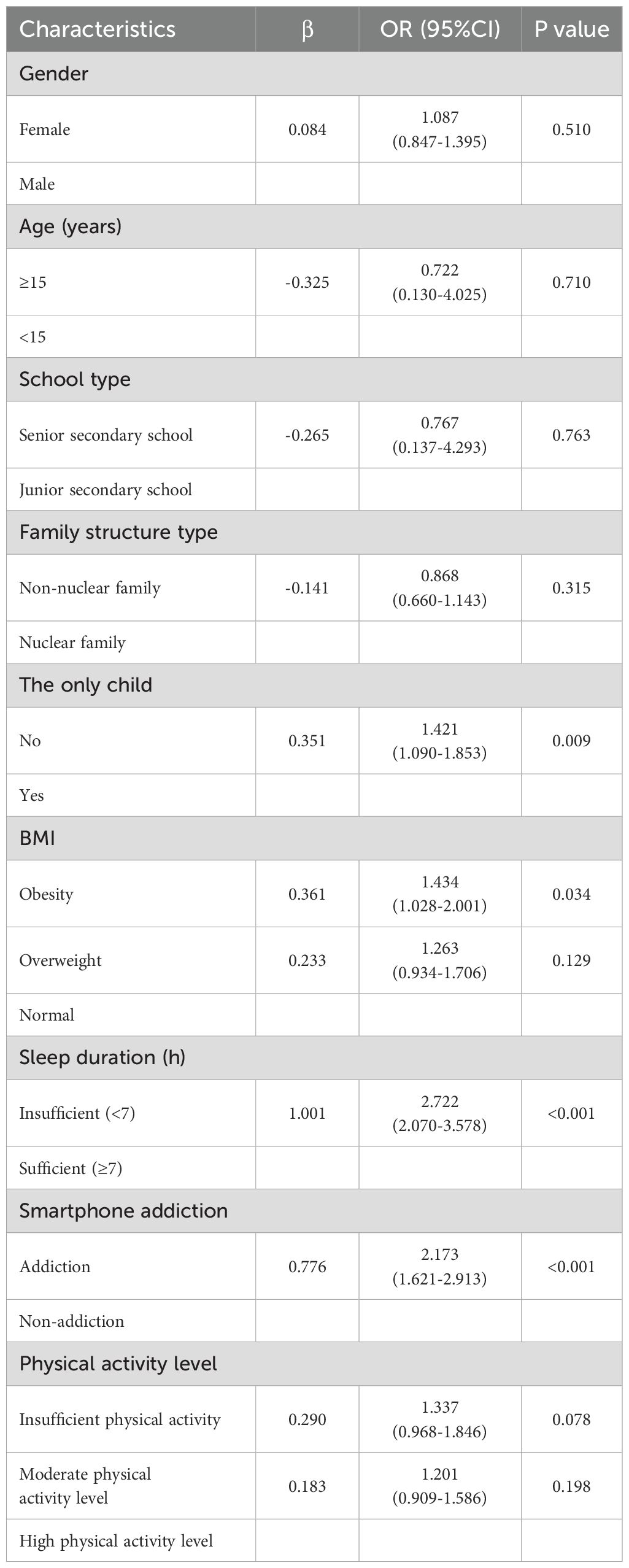
Table 2 illustrated that as obesity levels increase, so did the risk of developing depressive symptoms. Participants in the overweight group (OR=1.263, 95% CI: 0.934-1.706, P=0.129) and obesity group (OR=1.434, 95% CI: 1.028-2.001, P=0.034) showed a higher likelihood of depressive symptoms compared to the normal weight group. Smartphone addiction (OR=2.173, 95%CI: 1.621-2.913, P<0.001), non-only child status (OR=1.421, 95%CI:1.090-1.853, P=0.009), and insufficient sleep duration (OR=2.722, 95%CI:2.070-3.578, P<0.001) were identified as risk factors for depressive symptoms in secondary school students.
3.3 Combined effect of smartphone addiction and physical activity on depressive symptoms
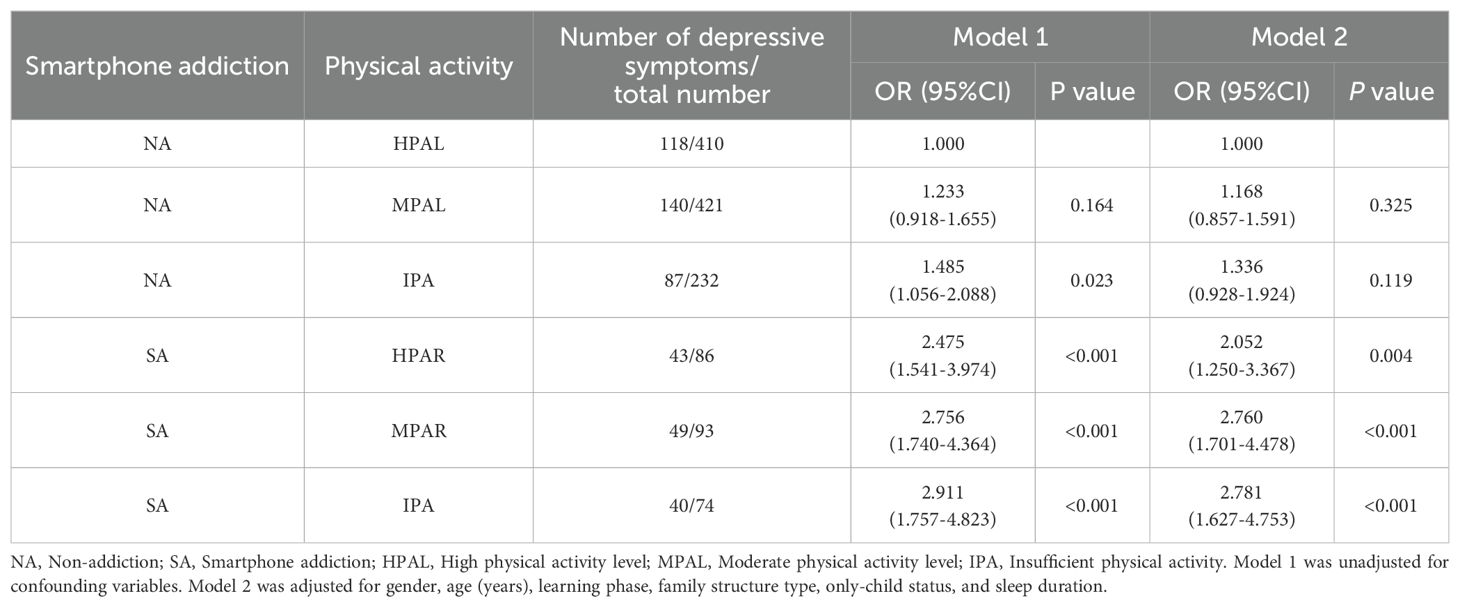
Table 3 revealed differences in reporting rates of depressive symptoms across various levels of physical activity and smartphone addiction groups. Using the non-smartphone addiction and high physical activity level group as references: Non-smartphone addiction, moderate physical activity level group: OR=1.168, 95%CI: 0.857-1.591, P=0.325; Non-smartphone addiction, insufficient physical activity group: OR=1.336, 95%CI: 0.928-1.924, P=0.119; Smartphone addiction, high physical activity level group: OR=2.052, 95%CI: 1.250-3.367, P=0.004; Smartphone addiction, moderate physical activity level group: OR=2.760, 95%CI: 1.701-4.478, P <0.001; Smartphone addiction, insufficient physical activity group: OR=2.781, 95%CI: 1.627-4.753, P <0.001. When no smartphone addiction was present, there were no statistically significant differences in the reporting rates of depressive symptoms among any physical activity level groups (P > 0.05, Figure 1).
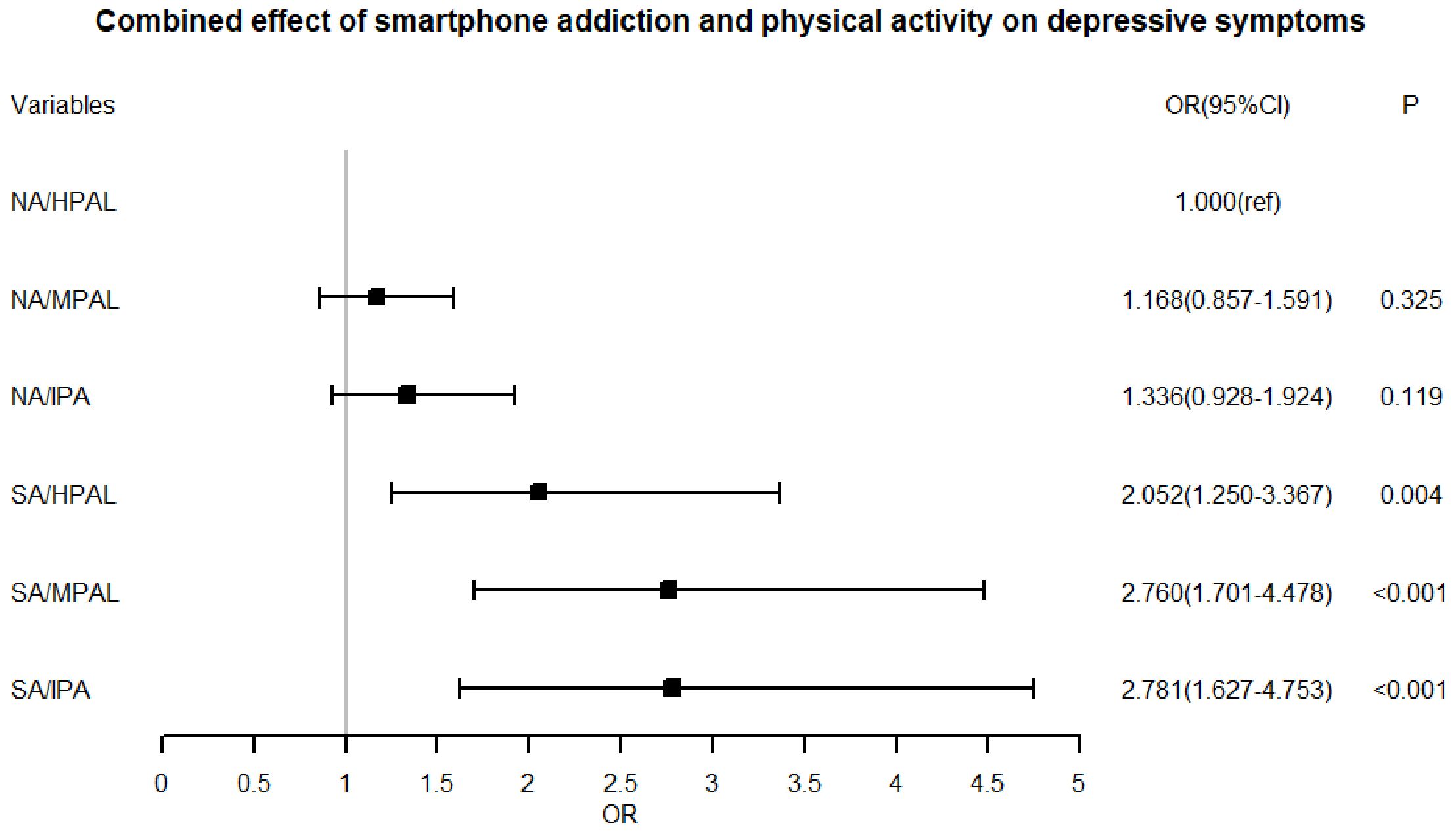
Figure 1. Combined effect of smartphone addiction and physical activity on depressive symptoms. Corresponding to Model 2 in Table 3, adjustments were made for gender, age (years), school type, family structure type, only-child status, and sleep duration.
4 Discussion
During adolescence, individuals undergo rapid psychological development, making them particularly susceptible to external influences that can result in various degrees of psychological issues. In this study, the prevalence of depressive symptoms among participants was 36.2%, significantly higher than both the 8% reported globally in previous studies on adolescent depression and the 26.3% prevalence observed among Chinese adolescents (22, 23). Despite potential influences from factors such as questionnaire tools, economic development, and social culture, this study consistently highlighted a high incidence of depressive symptoms among adolescents, underscoring the critical need for enhanced mental health interventions and improved adolescent mental health care. In addition, the study further revealed that adolescents who were non-only children or experience insufficient sleep duration demonstrated notably higher reporting rates of depressive symptoms, corroborating findings from prior research (24, 25).Future attention should prioritize the mental health needs of non-only children and adolescents with inadequate sleep duration, recognizing these factors as significant predictors of depression.
With the proliferation of smartphone technology, adolescents increasingly engage in activities such as communication, studying, and entertainment via smartphones. However, due to their ongoing development of self-control mechanisms, adolescents often struggle with smartphone addiction. This study found a 19.2% prevalence of smartphone addiction among participants. Smartphone addiction not only negatively impacts physical health, such as reduced vision and poorer sleep quality, but it can also contribute to various psychological issues including anxiety, depression, and reduced social adaptability (2, 26). This phenomenon poses significant public health challenges globally (27). Moreover, the study identified smartphone addiction as an independent risk factor for depressive symptoms, with significantly higher reporting rates among those addicted compared to non-addicted peers, aligning with previous research by Park et al. (2018) (28). The social replacement hypothesis posits that excessive smartphone use displaces real social interactions, potentially leading to negative emotions like depression (26, 29). Additionally, disruptions to circadian rhythms caused by smartphone use can impair neuroendocrine function, further predisposing adolescents to depressive symptoms (30). These findings highlight the urgent need for interventions targeting adolescent smartphone addiction. Strategies may include promoting face-to-face social interactions and offering educational resources to cultivate healthy smartphone use habits (31–33).
Notably, smartphone addiction often coexists with insufficient physical activity. The study reported prevalence rates of 37.7% for high physical activity, 39.1% for moderate physical activity, and 23.3% for insufficient physical activity among participants, reflecting a significant deviation from the UN’s recommended standards for adolescent physical activity. Prolonged physical inactivity not only contributes to physical ailments such as overweight and obesity but also serves as a key factor in the development of psychological disorders, including depressive symptoms (11). Thus, enhancing adolescent physical activity levels holds considerable importance for promoting both physical and mental well-being. Therefore, we recommend that physical activity promotion be included in public health strategies for adolescents. Schools and communities can work together to provide more accessible opportunities for sports and outdoor activities, which can both prevent physical health problems and improve mental health (34, 35).
This study also examined the combined effect of smartphone addiction and physical activity on the incidence of depressive symptoms. Compared to the students experiencing either smartphone addiction or insufficient physical activity alone, those affected by both conditions reported a higher prevalence of depressive symptoms. This finding was supported by previous research conducted by Liu et al. (2019) and Xie et al. (2019) (36, 37). When adolescents exhibited smartphone addiction, their likelihood of experiencing depressive symptoms was markedly elevated irrespective of their level of physical activity. This suggests that smartphone addiction exerts a more pronounced negative influence than insufficient physical activity, although higher levels of physical activity may partially mitigate the detrimental effects of smartphone addiction on adolescents’ depressive symptoms. The underlying rationale may stem from the possibility that smartphone addiction contributes to reduced physical activity levels, thereby nullifying the protective benefits of physical activity on mental health (38). In sight of this, interventions should not target smartphone addiction or physical inactivity in isolation, but also address both factors simultaneously, and policymakers and educators should develop comprehensive interventions to encourage reduced smartphone use and increased physical activity, providing practical solutions for incorporating healthy behaviors into adolescents’ daily lives. For example, schools and healthcare providers should implement targeted programs to educate adolescents about the importance of balancing smartphone use and physical activity, while encouraging daily physical activity, such as team sports or outdoor recreation, to help adolescents adopt a healthier daily lifestyle. In addition, parents should be educated about the signs of smartphone addiction and its impact on mental health, and provided with strategies regarding setting healthy boundaries in balancing smartphone use. By combining these strategies in both school and home environments, it is hoped that a more supportive environment can be created for adolescents to reduce their risk of developing or exacerbating depressive symptoms.
This study not only addresses a theoretical gap by providing a comprehensive analysis of smartphone addiction and physical activity, but also offers significant practical implications. The analysis of the combined effects of smartphone addiction and physical activity on depressive symptoms provides new insights for policymakers, urging the integration of support from all sectors of society to develop more effective, multifaceted intervention strategies aimed at addressing the increasing prevalence of adolescent depression. Furthermore, this study identifies additional key factors contributing to adolescent depression, including being a non-only child and sleep deprivation. These findings underscore the necessity for individualized interventions targeting these specific risk factors. Policymakers and mental health professionals can utilize these insights to design more targeted, evidence-based strategies to better mitigate the onset of adolescent depression. Additionally, the exploration of the interaction between various behavioral and demographic factors in the development of depression emphasizes the importance of a holistic approach to adolescent mental health. Several limitations of this study also need to be addressed. Firstly, the data were cross-sectional, precluding definitive conclusions regarding the causal relationships among smartphone addiction, physical activity, and depressive symptoms. Secondly, the study sample was confined to two secondary schools selected through cluster sampling, potentially limiting its generalizability to the broader adolescent population. Lastly, apart from height and weight, all variables were self-reported, which introduces the possibility of recall bias and reporting inaccuracies. Future studies should incorporate more objective assessment tools and adopt prospective methodologies to enhance data accuracy.
5 Conclusion
In summary, the prevalence of depressive symptoms among adolescents is substantial, with both smartphone addiction and insufficient physical activity posing significant challenges. A combined effect of smartphone addiction and insufficient physical activity on depressive symptoms was observed. Controlling smartphone addiction was found to be crucial in reducing the occurrence and progression of depressive symptoms in adolescents. Increasing levels of physical activity could partially mitigate the adverse effects of smartphone addiction on depressive symptoms. Therefore, comprehensive interventions targeting both smartphone addiction and physical activity are crucial for effectively managing the incidence and progression of depressive symptoms in adolescents.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Public Health and Nursing Research Ethics Committees affiliated with Shanghai Jiao Tong University School of Medicine (ref: SJUPN-20211). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
RY: Data curation, Formal analysis, Writing – original draft. ST: Data curation, Writing – original draft. GA: Data curation, Writing – review & editing. TL: Data curation, Writing – review & editing. CC: Investigation, Writing – review & editing. LS: Investigation, Writing – review & editing. BJ: Investigation, Writing – review & editing. YL: Investigation, Project administration, Resources, Writing – review & editing. JS: Funding acquisition, Investigation, Project administration, Resources, Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Natural Science Foundation of China (grant number 71603182); Shanghai Jing’an District to Strengthen the Public Health System Construction 3-year Action Plan (grant number:JAGW2023102-2); Soft Science Project of the Shanghai Municipal Science and Technology Commission (24692113600); National Natural Science Foundation of China (72204156) and Shanghai Higher Education Institutions' Faculty Industry-Academia-Research Practice Program.
Acknowledgments
The authors gratefully acknowledge the Jiangning Road Community Health Service Center in Jing’an District, Shanghai for organizing and coordinating this study. Special appreciation is extended to Shanghai East Middle High School and Shanghai First High School for their valuable support and cooperation. Sincere thanks are also due to all participants and investigators involved in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Toda M, Ezoe S, Nishi A, Mukai T, Goto M, Morimoto K. Mobile phone dependence of female students and perceived parental rearing attitudes. Soc Behav Personality. (2008) 36:765–70. doi: 10.2224/sbp.2008.36.6.765
2. Yang X, Zhou Z, Liu Q, Fan C. Mobile phone addiction and adolescents’ anxiety and depression: The moderating role of mindfulness. J Child Family Stud. (2019) 28:822–30. doi: 10.1007/s10826-018-01323-2
3. Salehan M, Negahban A. Social networking on smartphones: When mobile phones become addictive. Comput Hum Behavior. (2013) 29:2632–9. doi: 10.1016/j.chb.2013.07.003
4. Wang J-L, Rost DH, Qiao R-J, Monk R. Academic stress and smartphone dependence among Chinese adolescents: A moderated mediation model. Children Youth Serv Rev. (2020) 118:105029. doi: 10.1016/j.childyouth.2020.105029
5. Sicheng X, Bin Z, Yongzhi J, Huaibin J, Yun C. Global prevalence of mobile phone addiction: A meta-analysis. Stud Psychol Behavior. (2021) 19:802–8.
6. Nilsson A, Brage S, Riddoch C, Anderssen SA, Sardinha LB, Wedderkopp N, et al. Comparison of equations for predicting energy expenditure from accelerometer counts in children. Scand J Med Sci Sports. (2008) 18:643–50. doi: 10.1111/j.1600-0838.2007.00694.x
7. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. (2012) 380:247–57. doi: 10.1016/S0140-6736(12)60646-1
9. Kisch J, Leino EV, Silverman MM. Aspects of suicidal behavior, depression, and treatment in college students: results from the spring 2000 national college health assessment survey. Suicide life-threatening behavior. (2005) 35 1:3–13. doi: 10.1521/suli.35.1.3.59263
10. Tang CSK, Wu AMS, Yan ECW, Ko JHC, Kwon JH, Yogo M, et al. Relative risks of Internet-related addictions and mood disturbances among college students: a 7-country/region comparison. Public Health. (2018) 165:16–25. doi: 10.1016/j.puhe.2018.09.010
11. Rothon C, Edwards P, Bhui K, Viner RM, Taylor S, Stansfeld SA. Physical activity and depressive symptoms in adolescents: a prospective study. BMC Med. (2010) 8:32. doi: 10.1186/1741-7015-8-32
12. Kim S, Favotto L, Halladay J, Wang L, Boyle MH, Georgiades K. Differential associations between passive and active forms of screen time and adolescent mood and anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:1469–78. doi: 10.1007/s00127-020-01833-9
13. Feng Q, Zhang QL, Du Y, Ye YL, He QQ. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One. (2014) 9:e100914. doi: 10.1371/journal.pone.0100914
14. Wu X, Tao S, Zhang Y, Zhang S, Tao F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS One. (2015) 10:e0119607. doi: 10.1371/journal.pone.0119607
15. Kwon M, Kim DJ, Cho H, Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS One. (2013) 8:e83558. doi: 10.1371/journal.pone.0083558
16. Ben XMWZM. Reliability and validity of Chinese version of the smartphone addiction scale in adolescents. Chin J Clin Psychol. (2019) 27:959–64.
17. Mu Ziwei RF, Yu W, Xiao W, Wan Y. Relationship among bullying, mobile phone addiction and depressive symptoms in college students. Chin Ment Health J. (2024) 38:820–6.
18. Baumgartner TA, Jackson AS eds. Measurement for Evaluation in Physical Education and Exercise Science (1987) Boston, MA: WCB McGrawHill.
19. Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. (1985) 10:141–6.
20. Kong AP, Choi KC, Li AM, Hui SS, Chan MH, Wing YK, et al. Association between physical activity and cardiovascular risk in Chinese youth independent of age and pubertal stage. BMC Public Health. (2010) 10:303. doi: 10.1186/1471-2458-10-303
21. Zung WW. A self-rating depression scale. Arch Gen Psychiatry. (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
22. Shorey S, Ng ED, Wong CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: A systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:287–305. doi: 10.1111/bjc.12333
23. Li JY, Li J, Liang JH, Qian S, Jia RX, Wang YQ, et al. Depressive symptoms among children and adolescents in China: A systematic review and meta-analysis. Med Sci Monit. (2019) 25:7459–70. doi: 10.12659/MSM.916774
24. Khan A, Ahmed R, Burton NW. Prevalence and correlates of depressive symptoms in secondary school children in Dhaka city, Bangladesh. Ethn Health. (2020) 25:34–46. doi: 10.1080/13557858.2017.1398313
25. Cao Y, Huang L, Si T, Wang NQ, Qu M, Zhang XY. The role of only-child status in the psychological impact of COVID-19 on mental health of Chinese adolescents. J Affect Disord. (2021) 282:316–21. doi: 10.1016/j.jad.2020.12.113
26. Kraut R, Patterson M, Lundmark V, Kiesler S, Mukopadhyay T, Scherlis W. Internet paradox. A social technology that reduces social involvement and psychological well-being? Am Psychol. (1998) 53:1017–31. doi: 10.1037//0003-066x.53.9.1017
27. Sohn SY, Rees P, Wildridge B, Kalk NJ, Carter B. Prevalence of problematic smartphone usage and associated mental health outcomes amongst children and young people: a systematic review, meta-analysis and GRADE of the evidence. BMC Psychiatry. (2019) 19:356. doi: 10.1186/s12888-019-2350-x
28. Park S, Kim H, Lee E, Lea E. Relationship between mobile phone dependence and depression of adolescents using autoregressive cross-lagged model. Forum For Youth Culture. (2018) 55:53–75. doi: 10.17854/ffyc.2018.07.55.53
29. Mendt S, Gunga H-C, Felsenberg D, Belavy DL, Steinach M, Stahn AC. Regular exercise counteracts circadian shifts in core body temperature during long-duration bed rest. NPJ Microgravity. (2021) 7:1. doi: 10.1038/s41526-020-00129-1
30. Vrshek-Schallhorn S, Doane LD, Mineka S, Zinbarg RE, Craske MG, Adam EK. The cortisol awakening response predicts major depression: predictive stability over a 4-year follow-up and effect of depression history. psychol Med. (2012) 43:483–93. doi: 10.1017/S0033291712001213
31. Shek DT, Yu L, Leung H, Wu FK, Law MY. Development, implementation, and evaluation of a multi-addiction prevention program for primary school students in Hong Kong: the B.E.S.T. Teen Program. Asian J Gambl Issues Public Health. (2016) 6:5. doi: 10.1186/s40405-016-0014-z
32. Turel O, Mouttapa M, Donato E. Preventing problematic Internet use through video-based interventions: a theoretical model and empirical test. Behav Inf Technol. (2015) 34:349–362. doi: 10.1080/0144929X.2014.936041
33. Sul S. Determinants of internet game addiction and therapeutic role of family leisure participation. J Inclusion Phenomena Macrocyclic Chem. (2015) 82:271–8. doi: 10.1007/s10847-015-0508-9
34. McKenzie TL, Sallis JF, Rosengard P, Ballard K. The SPARK programs: A public health model of physical education research and dissemination. J Teach Phys Education. (2016) 35:381–9. doi: 10.1123/jtpe.2016-0100
35. Bulger S, Illg K, Jones E. Achieving alignment in the preparation of CSPAP leaders in PETE programs. J Phys Education Recreation Dance. (2017) 88:37–42. doi: 10.1080/07303084.2017.1260982
36. Liu M, Zhang J, Hu E, Yang H, Cheng C, Yao S. Combined patterns of physical activity and screen-related sedentary behavior among Chinese adolescents and their correlations with depression, anxiety and self-injurious behaviors. Psychol Res Behav Manage. (2019) 12:1041–50. doi: 10.2147/PRBM.S220075
37. Xie H, Tao S, Zhang Y, Tao F, Wu X. Impact of problematic mobile phone use and insufficient physical activity on depression symptoms: a college-based follow-up study. BMC Public Health. (2019) 19:1640. doi: 10.1186/s12889-019-7873-z
Keywords: depressive symptoms, smartphone addiction, physical activity, adolescents, China
Citation: Yang R, Tan S, Abdukerima G, Lu T, Chen C, Song L, Ji B, Lv Y and Shi J (2025) Combined effect of the smartphone addiction and physical activity on the depressive symptoms in secondary school students: a cross sectional study in Shanghai, China. Front. Psychiatry 15:1473752. doi: 10.3389/fpsyt.2024.1473752
Received: 07 August 2024; Accepted: 03 December 2024;
Published: 03 January 2025.
Edited by:
Soumitra Das, Western Health, AustraliaReviewed by:
Kshitij Karki, G.T.A. Foundation, NepalShahabedin Rahmatizadeh, Shahid Beheshti University of Medical Sciences, Iran
ShuQiao Meng, Yangzhou University, China
Copyright © 2025 Yang, Tan, Abdukerima, Lu, Chen, Song, Ji, Lv and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianwei Shi, c2hpamlhbndlaV9hbXlAMTI2LmNvbQ==; Yipeng Lv, ZXBlbmdsQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Rui Yang
Rui Yang Shuoyuan Tan
Shuoyuan Tan Gulqihra Abdukerima
Gulqihra Abdukerima Ting Lu2
Ting Lu2 Chen Chen
Chen Chen Bing Ji
Bing Ji Yipeng Lv
Yipeng Lv Jianwei Shi
Jianwei Shi