
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 18 September 2024
Sec. Public Mental Health
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1463415
This article is part of the Research TopicRedefining Acute Psychiatric Care: Strategies for Improved Inpatient ExperiencesView all 6 articles
Objective: Shortening the length of hospital stay (LOS) has become a major challenge for psychiatric hospitals in reducing unnecessary costs and improving the patient healthcare experience. We investigated the key factors associated with a long psychiatric hospitalization.
Method: This was a retrospective study of 8,870 full-time psychiatric hospital stays (6,216 patients) in the Paris Psychiatry Hospital Group, with a discharge in 2022. We used machine learning tools and univariate and multivariate methods to explore the impact of demographic, pathway-related, and clinical variables on the LOS.
Results: LOS >30 days was associated with age >55 years {odds ratio [OR] =2 [95% confidence interval 1.7–2.3]}, admission from outside the sectorization zone [OR=1.2 (1.1–1.3)], admission via a psychiatric emergency unit [OR, 1.2 (1.1–1.4)], and some clinical severity markers, such as psychotic disorder diagnosis [OR, 1.5 (1.3–1.7)], mandatory care [request of a third party, OR, 2.5 (2.1–2.9); case of imminent danger, OR, 2.3 (1.9–2.7)], the presence of seclusion and mechanical restraint measures (highlighting the positive effect of restraint duration), the somatic comorbidity for female sex [OR, 1.4 (1.2–1.7)], and treatment resistance [OR, 1.4 (1.2–1.6)]. Conversely, LOS ≤30 days was associated with being in a relationship [OR, 0.6 (0.5–0.8)], admission during a travel-related psychiatric episode [OR, 0.5 (0.3–0.6)], and personality and behavior disorders [OR, 0.7 (0.6–0.9)]. We found no significant association for features such as sex and a lack of treatment compliance.
Conclusion: To our knowledge, this is the first recent study to investigate and highlight the impact of factors related to various illness severity markers, medication adherence, and patient journeys on the length of psychiatric hospital stay. A better understanding of long-stay risk factors might be helpful for optimizing the allocation of medical resources and anticipating tailored therapeutic programs.
The cost of inpatient psychiatry in France was estimated at €13.4 billion in 2007, representing 64% of the total cost of mental healthcare (1). Prolonged hospitalization is associated with an increased consumption of health resources and services in addition to a risk of exceeding hospital capacity. Hence, the cost is an important economic burden for our healthcare system. In addition to the impact on healthcare organizations and expenditure, long hospital stays also lead to a loss of quality of life because of social isolation and high dependency (2, 3). Although the results need to be confirmed, a Cochrane review (4) suggested that a short-stay policy for patients with severe mental illness did not result in a “revolving door pattern” of admission or poor or fragmented delivery of care. This study also highlighted that a short stay significantly improved social functioning (including unemployment). Similarly, international recommendations on mental healthcare have promoted the reduction of unnecessary long stay hospitalizations by improving the quality of care (2, 5, 6). In France, this objective has been included in the national plan for the reform of psychiatric financing through a financial incentive indicator (7) based on counting hospital stay days for full-time and free inpatient psychiatric admissions. It aims to encourage psychiatric institutions to minimize inappropriate long stays.
To achieve this goal, we need to better understand the clinical, social, and care pathway determinants that influence the length of psychiatric hospital stay (LOS). Knowledge of the predictors of LOS could help caregivers anticipate this event (8, 9) and thus adapt care planning for earlier discharge (10–12). The benefits are optimized and improve healthcare, reduce the risk of chronic mental illness, and reduce superfluous costs associated with inpatient care.
Reviews of the international literature (8, 10, 13, 14) have identified several factors associated with a risk of a long psychiatric hospital stay: sociodemographic (sex, age, marital status, precariousness, and unemployment), clinical [diagnosis of psychosis, addictive comorbidity, hetero-aggressive behavior, mandatory admission, severity of pathology, suicide risk, and treatment with clozapine or electroconvulsive therapy (ECT)], and organizational (hospital size and number of care coordinators). However, the same patient characteristics may have a different impact on LOS in different countries. Therefore, national studies must take into account the national and contextual complexity of the factors predicting LOS (10). The French literature has highlighted the role of characteristics such as a high level of dependency, diagnosis of psychosis, psychological development disorder, intellectual disability, mandatory admission, seclusion, and mechanical restraint during the stay, as well as territorial health and social care provision (3, 15).
There are few recent studies conducted in France that have investigated factors associated with LOS. The LOS cutoffs used in these studies, 90 (7) and 292 days (3, 15), were very high and do not seem relevant to clinical practice, according to the experience of health professionals. Furthermore, to the best of our knowledge, there is a lack of research in France on the characteristics of the patient journey. French psychiatric care organizations are characterized by a division into sectors, each providing care for approximately 70,000 inhabitants from a determined geographic area. The objective of sector organization was to provide residents from the same geodemographic area some integrated and graduated care, in accordance with the stage of their disease and available as closely as possible to their living space (16, 17). This organization was built to ensure equal access, proximity, continuity, and also multidisciplinarity for inpatient and outpatient care services. The medico-psychological center is the pivotal point of care supply, including prevention, diagnose, ambulatory care, and home-based intervention. In addition to inpatient full-time hospitalization, alternative pathways were developed, such as full-time hospitalization in rehabilitation units, therapeutic apartments, hospitalization at home, and also part-time day or night hospitalization. No previous national study has investigated the impact of admission in a ward outside the patient’s sectorization zone on LOS. Additionally, other pathway features, such as hospitalization during a travel-related psychiatric episode or after a visit to a psychiatric emergency department, have not been investigated. We also did not find any recent French work on the effect of somatic comorbidity, duration of seclusion and physical restraint, medication adherence, and treatment resistance. These characteristics might be associated with a long hospital stay.
The aim of the present exploratory study was to better understand the determinants of long hospital stay outcomes in the French context, using some already established risk factors and exploring new and unstudied candidate features. We used structured and textual data from the electronic health record database of the Paris Psychiatry Hospital Group. This was an opportunity to explore a new approach, combining state-of-the art machine learning tools and statistical methods.
For this observational study, we used administrative, sociodemographic, and clinical data from the electronic health record database of the Paris Psychiatry Hospital Group, which serves a population of approximately 1.6 million people and covers three-quarters of the city of Paris. Our source database contained 700,000 patient electronic health records. We leveraged structured and unstructured data (e.g., discharge summaries or medical observation reports). We selected patient stays corresponding to a full-time psychiatric hospitalization for patients ≥15 years old, with a discharge in 2022 (n=9,697 admissions). As detailed in Figure 1, we excluded short hospitalizations (≤2 days) and iterative hospitalizations when they were dedicated to specific therapies such as ECT in case of treatment-resistant depression or long-acting neuroleptic injection for patients with psychoses. This study was approved by the Paris Psychiatry Hospital Group Research Ethics Committee (accreditation no. 2024-CER-A-007).
LOS was the study outcome. To assess actual stay duration, we used a specific algorithm: we chained 2 consecutive stays as one stay if the time between the discharge and entry date was ≤3 days. We assumed these stays were the same healthcare period interrupted by a temporary absence. We also treated the LOS outcome as a continuous variable or binary variable by defining “short LOS” as ≤30 days and “long LOS” as >30 days (see Supplementary Material for details). This cutoff (30 days) was chosen according to the experience of health professionals. Studies in different contexts also suggest such a threshold (18–20).
The characteristics to be included in the statistical modeling were validated in the literature or hypothesized based on the experience of health professionals. The independent variables were divided into the following categories:
● Demographic variables: sex, age, marital status, social vulnerability (homelessness status, high deprivation index level, and social factors influencing health status).
● Variables characterizing the patient’s care pathway: admission (a) from outside the patient’s sectorization zone, (b) after a travel-related psychiatric episode, and/or (c) after a visit to a psychiatric emergency department.
● Clinical variables: psychiatric primary or associated diagnosis according to the International Classification of Diseases, 10th revision (ICD-10) codes (see Table 1), presence of a somatic comorbidity, suicide risk, severity of seclusion and mechanical restraint measure (assessed by the duration of restraint), mandatory admission, number of psychiatric admissions in previous years, medication discontinuation (due to lack of compliance), and treatment resistance.
The list of variables with their precise definitions is featured in Supplementary Material.
Applying the method mentioned in section 2.1, we obtained a dataset of 8,870 observations, each related to a patient stay. Because of the lack of reliability in the electronic health records for ICD-10 diagnoses related to somatic comorbidity and suicide, we calculated these predictors by combining ICD-10 diagnostic data and information extracted from medical narratives. In the same way, we mined information from textual medical observations to compute the variables medication discontinuation and treatment resistance (for the latter variable, we precisely combined information extracted from narratives with ECT data). For more details about these variables, see Supplementary Material. To compute the variables, we applied natural language processing techniques using Python v3.8.5 and the NLTK library. All other predictors were obtained by using only structured information from the electronic health record database, with R v4.3.1 or Python v3.8.5.
We performed initial descriptive and univariate analyses of the dataset (n=8,870). Because the distribution of the continuous variables LOS and age was not normal, we first described them using the median [interquartile range (IQR)]. For ease of reading, we also produced mean ± SD. For categorical variables, we described the characteristics of the study population using frequencies and percentages (%).
We first performed preliminary bivariate analysis of the dataset (n=8,870) for each of the 30 selected predictors and the LOS outcome. We transformed the continuous variable age into an ordinal variable for further analysis. We used chi-squared or Fisher’s exact tests for categorical variables and the Cochran–Armitage test for ordinal variables (e.g., age category, seclusion and mechanical restraint severity level, or history of hospitalization in the Paris Psychiatry Hospital Group before 2019; see Supplementary Material for definitions). We repeated this bivariate analysis on sex-stratified data (n=8,870).
We then found that a logistic regression with “long LOS” defined as “hospitalization >30 days” was the best model for achieving our study objective. Specifically, we checked whether there was no need for a multilevel model, accounting for a potential nested data structure at the psychiatric sector level (see Supplementary Material for more details on model selection). Logistic regression analysis was first used with the dataset for which observations with any missing values were removed (n=6,206). We implemented a model including all the predictors significant at p<0.2 on bivariate analysis and interaction terms if necessary (21). Stepwise variable selection was used to select the most relevant variables for prediction. We computed the area under the receiver operating characteristic curve metric (AUC) to evaluate our final multivariate model (see Supplementary Material for more details about model evaluation). We estimated odds ratios (ORs) and 95% confidence intervals (CIs), with p<0.05 considered statistically significant.
As a sensitivity analysis, we repeated the whole bivariate and multivariate process, testing different LOS cutoffs for the binary outcome definition, successively 20, 60, and 90 days.
We applied the same statistical steps to the initial dataset with missing values previously replaced by random imputation (n=8,870) (22). We also checked whether there was a significant difference between stays excluded versus included from the logistic regression process (n=2,664 vs. n=6,206). As a sensitivity analysis, we repeated the same multivariate analysis on a dataset (n=8,522) that filtered the variable mostly affected by missing data (marital status). Statistical analysis was carried out using R v4.3.1.
We constructed a database of 8,870 full-time hospital stays (6,216 patients) (Figure 1). The median LOS was 14 days (IQR, 5–31; mean 27 ± 47.8 days) (see distribution plot in Figure 2). The median age of patients was 38 (IQR, 27–53; mean age 41 ± 16 years); 44.9% of long stays were for female patients (Table 2). Overall, 25.5% of the stays were in a psychiatric ward that was different from the patient’s psychiatric sector of origin, 10.0% were during a travel-related psychiatric episode, and 68.9% were after a visit to a psychiatric emergency unit. We found that 25.1% of the admissions were related to mandatory care at the request of a third party, and 18.7% to imminent danger. In all, 9.1% of stays were associated with another type of mandatory care (by decision of the state representative, of detained persons, after a decision of criminal irresponsibility, or within the framework of a temporary placement order). The two most common diagnoses were schizophrenia and mood disorders, accounting for 52.4% and 40.3% of the 8,870 hospitalizations, respectively. A total of 20.9% of stays featured suicidal risk and 53.5% featured somatic comorbidity.
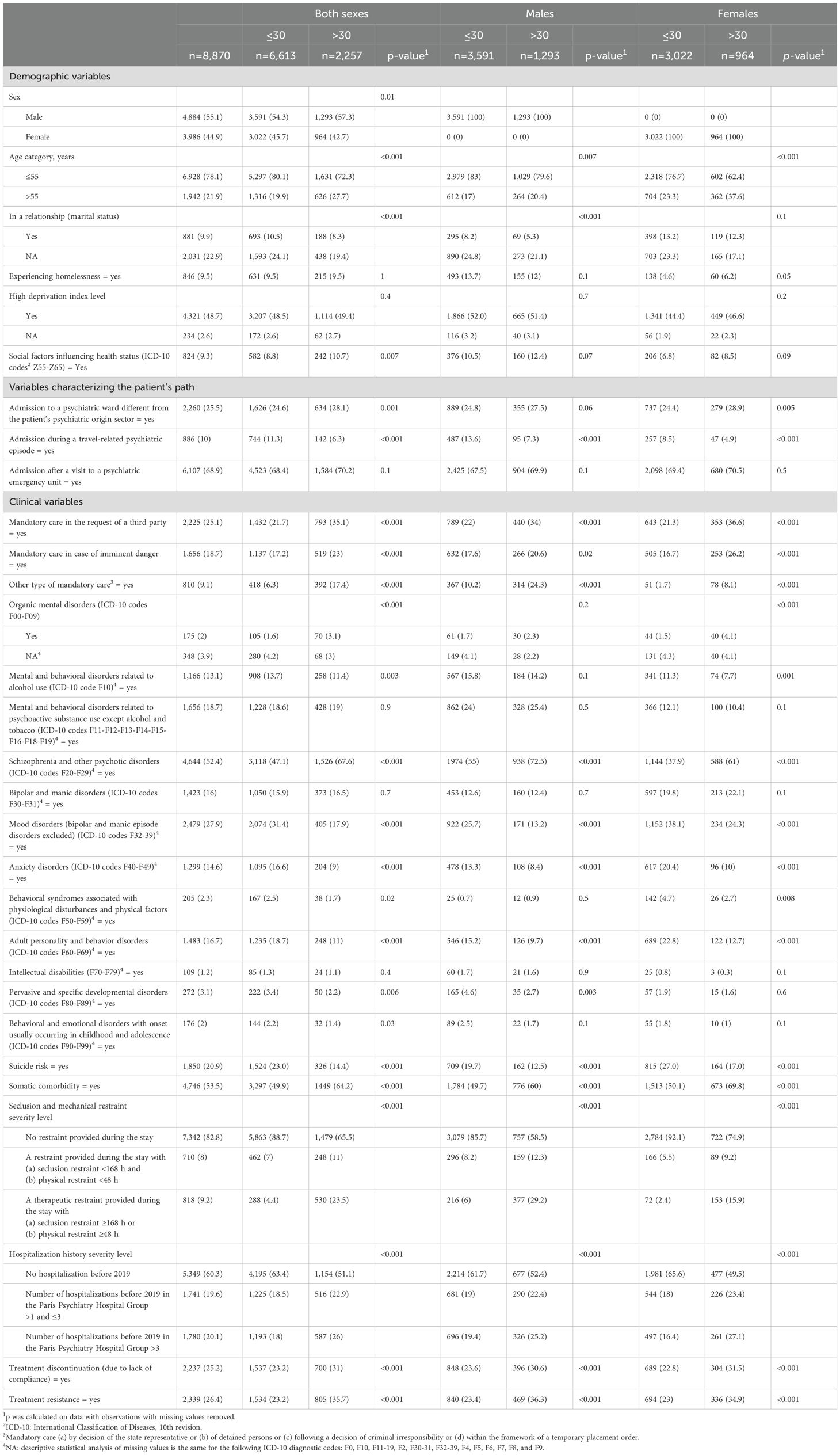
Table 2. Bivariate analysis of patients with a length of psychiatric hospital stay of ≤30 versus >30 days for both sexes and by sex.
Table 2 reports details of the results by sex and overall. A long LOS was significantly increased for male patients (p=0.01) and aged >55 years (p<0.001), persons not in a relationship (p<0.001), and a diagnosis related to social factors influencing health status (p=0.007). Long versus short LOS was less frequent with travel-related psychiatric episodes (p<0.001) but was more frequent for patients admitted outside their sectorization zone (p=0.001). Long versus short LOS was more frequent for patients under mandatory care (p<0.001 for all mandatory care predictors). The clinical diagnostic profile of patients significantly differed between the patients with long and short LOS: long LOS was associated with a diagnosis of schizophrenia (p<0.001), organic mental disorders (p<0.001), or a somatic comorbidity (p<0.001). In addition, long LOS was associated with seclusion and mechanical restraint severity level, hospitalization history severity level, medication discontinuation (because of a lack of compliance), and treatment resistance (p<0.001 for four factors). However, a long LOS was less frequent among patients with disorders related to alcohol use (p=0.003), mood disorders (excluding bipolar and manic episodes) (p<0.001), anxiety (p<0.001), behavioral syndromes associated with physiological disturbances (p=0.02), personality disorders (p<0.001), psychological developmental disorders (p=0.006), behavioral and emotional disorders with early onset (p=0.03), and suicide risk (p<0.001).
The odds of a long LOS was associated with age >55 years [OR, 2 (95% CI 1.7–2.3)], admission from outside the sectorization zone [OR, 1.2 (1.1–1.3)] and admission via a psychiatric emergency unit [OR, 1.2 (1.1–1.4)], mandatory care [request of a third party [OR, 2.5 (2.1–2.9)], in imminent danger [OR, 2.3 (1.9–2.7)], another type of mandatory care [OR, 4.3 (3.5–5.5)]], a diagnosis of schizophrenia [OR, 1.5 (1.3–1.7)], a high level of seclusion and mechanical restraint [level 1: OR, 1.6 (1.3–1.9); level 2: OR, 5 (4–6.2)], and treatment resistance [OR, 1.4 (1.2–1.6)] (Table 3). We found a significant interaction between sex and somatic comorbidity (p<0.002): a sex-stratified analysis confirmed that somatic comorbidity increased the odds of LOS for only females [OR, 1.4 (1.2–1.7), computed after taking interaction terms into account]. Conversely, protective factors for the odds of a long LOS were being in a relationship [OR, 0.6 (0.5-0.8)], admission during a travel-related psychiatric episode [OR, 0.5 (0.3–0.6)], and a diagnosis of personality disorders [OR, 0.7 (0.6,0.9)].
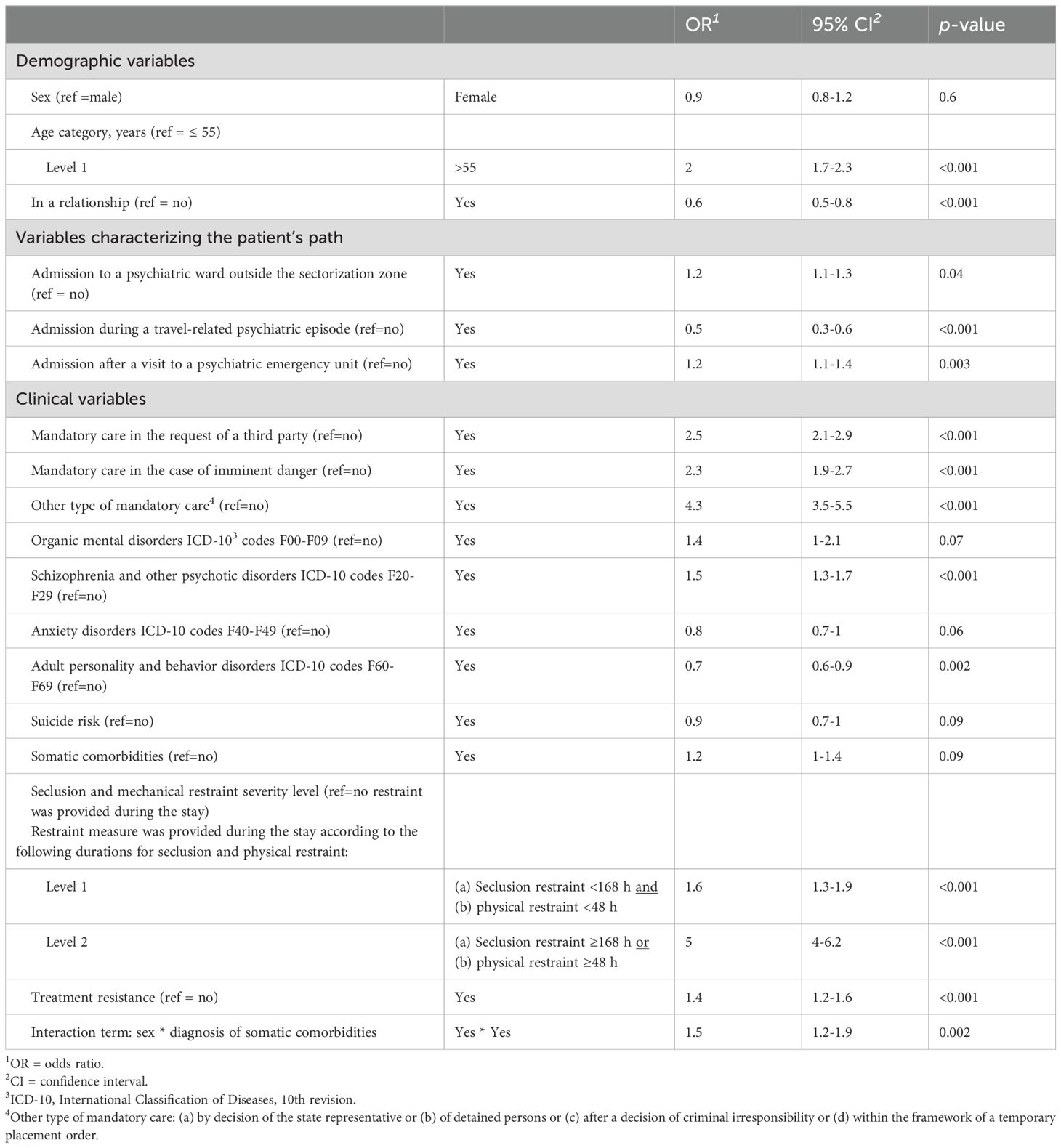
Table 3. Multivariate logistic regression analysis of factors associated with the odds of a psychiatric hospital stay of >30 days.
For receiver operating characteristic (ROC) analysis, the AUC for our final model was 65.9% (95% CI 56.3–74.9). We checked that we had acceptable results for the following tests: variance inflation factor, deviance, and Hosmer and Lemeshow (Supplementary Material).
Sensitivity analysis consisted of using different cutoff thresholds for LOS, successively 20, 60, and 90 days. This exploration showed consistent results for the final logistic regression. For the three mentioned cutoffs, the diagnosis of organic mental disorders was positively associated with a long stay. Additionally, for homelessness status, for a cutoff of 90 days, the OR was 1.9 (95% CI 1.3–2.7) (Supplementary Material).
We found consistent conclusions for the highlighted variables of interest when we performed bivariate and multivariate analyses, whether imputing or excluding missing data. On the imputed dataset, the organic mental disorders diagnosis appeared as a long-stay risk factor [OR, 1.6 (95% CI 1.1–2.2)]. Nevertheless, observations excluded because of missing values (n=2,664) were significantly associated with male sex, older age, and a long LOS as compared with observations with no missing information (n=6,206) (Supplementary Material).
Factors that increased the odds of a long LOS were age >55 years, admission from outside the patient’s sectorization zone, admission via a psychiatric emergency unit, mandatory care, seclusion and physical restraint, diagnosis of schizophrenia and psychosis, treatment resistance, and somatic comorbidity for female sex. Factors that reduced the odds of a long LOS were being in a relationship, admission during a travel-related psychiatric episode, and a diagnosis of a personality disorder.
Our results agree with the French and international literature. Among patient characteristics previously validated as risk factors, we first identified age >55 years. We found a positive association between age and a long LOS in previous studies (13, 23, 24). The positive association of outcome with a diagnosis of schizophrenia has been widely confirmed (3, 9, 13, 14, 19, 23, 25–28). We also highlighted features related to clinical severity, reported in previous studies: treatment resistance (29, 30), mandatory care (3), and seclusion and mechanical restraint (3) (25). We noted some previous contradictory findings (31) on the effect of coercive treatment on LOS (alternatively positive, negative, or null, depending on the study). However, these results were obtained in different foreign countries with their own mandatory care regulations, but our conclusions were consistent with a recent French study (3). We found another significant result for the severity of seclusion and mechanical restraint: a multiplication factor of 3 for the risk of LOS between the first and second variable level, depending on the duration of the measure. These findings suggest that the use of mandatory care and seclusion and mechanical restraint may correspond to severe and difficult-to-treat symptoms, materialized by patient aggressiveness, dangerousness, a lack of illness awareness, social withdrawal, functional impairment, and a low adherence to care. This observation could explain the need for complex treatment, difficulties in discharge, and thus a long stay (3, 9, 32). The literature suggests that particular attention should be paid to the severity of illness (13).
Another notable finding of our study was the positive association of somatic comorbidity with a long LOS for only women. Somatic illness has been described in the literature as a potential “focus of care” (33) and a risk factor for long hospital stays (13, 34, 35). However, we could not find other examples of this interaction between sex and somatic comorbidity in the literature. To interpret our result, because women are more likely to report physical symptoms than men (36), somatic symptoms may be easier to treat for women within a psychiatry unit, in contrast to men, who have to be transferred to the general medical ward and are therefore discharged from psychiatry care earlier.
Multivariate analysis of imputed data revealed a diagnosis of organic mental disorders as a risk factor for a long LOS. Considering the specific low prevalence of positive cases for this feature, with more statistical power, this characteristic might have initially appeared among the significant predictors. This result was also confirmed with sensitivity analysis with cutoffs of 20, 60, and 90 days. In addition, homelessness became positively and significantly associated with the highest cutoff of LOS (90 days). This finding agreed with previous research reporting the impact of homelessness on LOS (21, 37).
We found a protective effect of non-single marital status on a long LOS, in line with the literature describing it as a proxy “for functional impairment” (13) and a factor “reflecting resilience” (18). This characteristic is related to human relationships and family connection providing moral support to the patient and is consistent with studies showing that family visits reduce the LOS (38). We found no association between the diagnosis of mood disorders and a long stay in our multivariate analysis. Yet, significance would have been in accordance with previous French studies (3) but not the international literature (8, 29, 37). A diagnosis of a personality disorder was a negative predictor, reported in previous research (21, 28, 39). This observation was consistent with international guidelines (40), recommending limited extended hospitalization in this case. Moreover, it was also consistent with the fact that personality disorders are more often a comorbidity rather than a primary cause of full-time hospitalization (for 2019–2022, the unpublished GHU Paris Psychiatry Hospital annual report highlights that 58% of personality disorder diagnoses related to full-time hospitalization in the Paris Psychiatry Hospital Group were “associated” and not “primary” diagnoses).
An interesting result of our exploration was the variables related to the patient pathway. We highlighted two new significant features. The first was admission after a visit via a psychiatry emergency unit: its positive effect on a long LOS could be interpreted as a marker of the clinical severity of the disease and need for more complex care. The second, the protective effect of a long LOS during a travel-related psychiatric episode, was in line with the profile of these patients (41). Such patients are mostly traveling from France (Paris suburbs or other regions) (41). They are out of their sectorization zone, psychotic, and characterized by a delusional state or disorganization of thought. Their vulnerability and lack of control justifies rapid hospitalization to protect themselves and others, but as soon as possible, health professionals organize their return to their original psychiatric sector to ensure better follow-up. In addition, we found admission from outside the sectorization zone positively associated with a long LOS. Sensitivity analysis with a lower cutoff point for LOS (20 days) confirmed this result. This finding was consistent with those from previous studies in the UK (28, 42). Out-of-area patients may be mostly new and unknown patients for psychiatric wards and thus require a long stay. In addition, out-of-area placements might penalize continuity of care and thus increase the LOS (28).
Our current results suggest that these characteristics related to the patient and the journey should be systematically assessed by healthcare professionals and taken into account during clinical decision-making. Knowledge of such determinants of LOS could help clinicians identify and focus on patients with high clinical severity and a risk of a prolonged stay. We suggest that long-stay patients require a more complex behavioral management and thus a higher level of staff in dedicated units, for specialized acute care. The aim would be to provide them tailored care with a multidisciplinary team, to optimize treatment, discharge planning, and use intensive case management for patients with disruptive behaviors (43, 44). Our results also suggested the benefits of early treatment resistance detection (45) and optimization of somatic comorbidity care. Moreover, the protective effect of non-single marital status on a long LOS emphasized the importance for health care professionals to favor any opportunity for patients to have constructive interactions with families, and also with the social environment. This confirmed the benefits of an approach integrating mental health and social care, through rehabilitation programs, assertive community treatment, and care provided in community-based settings (43).
Our findings should also be contextualized in regard to the variety of international results on the same subject. The mean LOS in this study (27 days) approximates the mean LOS highlighted in the international literature for the USA (24.9 days) (13) and Quebec (25.3 days) (43). It is above the mean LOS found for Italy (17.9 days) (10) and India (5.7 days) (46), and below the mean LOS found for other European countries (10) such as Germany (37 days), Poland (33.4 days), the United Kingdom (46.2 days), and Belgium (55.1 days). Previous studies conducted for Germany, Poland, the UK, Italy, and Belgium (10) highlighted features such as poor social functioning, psychotic disorder, and high clinical severity (in line with our findings) that predicted LOS regardless of the country. However, this study argued that the specific effect of variables might be different from one country to another, and that national context characteristics (cultural and organizational) might influence LOS and its determinants. A previous study comparing the USA and Germany (47) suggested that a greater number of social workers and private psychiatrists per inhabitant in the USA might ease a faster connection to after care, and thus partly explain a lower mean LOS in the USA. We suggest that French sectorization might also influence our LOS in the same way: our system provides specific pathways such as alternatives to full-time hospitalization (23) and rehabilitation programs (improving continuity of care, patient autonomy, and reintegration into the community) that might lower our mean LOS, compared with other European countries. A perspective of future studies would be to extend that kind of comparative study (10) to a greater number of countries, including France, with a rigorous approach that takes national healthcare system characteristics into account.
Although many studies have explored factors relating to LOS, there are few up-to-date studies conducted in France. We confirmed and broadened results from French studies related to LOS (3, 15, 23, 25). This study had several methodological assets. Our sample size (n=8,870) aligned with literature recommendations (at least 3,000 observations) (13), which ensured that our study was not underpowered, taking the number of covariables we used for modeling into account (48). We used data from the Paris Psychiatry Hospital Group electronic health records. This healthcare institution, consisting of three different hospitals, provides mental healthcare for much of the city of Paris, offering a representative target population of approximately 1.6 million people. Therefore, our sample was characterized by different types of patients with very different sociodemographic features. It was a representative sample of the Paris population and allowed us to minimize selection bias. To our knowledge, this study is the first to compute true LOS with a specific algorithm. With our computation method, we avoided a bias while evaluating LOS: we took into account the potential splitting of the healthcare period with a spurious administrative discharge, normally supposed to be a temporary absence. We performed a comprehensive analysis by including several categories of predictors (demographic, clinical, and related to care pathway) in our final model, selected after several rigorous statistical steps. As far as we know, this research was among the first in France to analyze the effect of factors related to the patient’s pathway, which are important understudied characteristics. We compensated for the lack of structured data for somatic comorbidity and suicide risk by implementing natural language processing methods on raw medical narratives and leveraged comprehensive lexical dictionaries assessed by different raters. We checked that ignoring sector effects did not bias our results significantly (see Supplementary Material). Our sensitivity multivariate analysis results were consistent in terms of age, psychotic diagnosis, and clinical severity factors, whatever the cutoff used to define a long LOS. A bivariate comparison of included versus excluded observations revealed the latter observations were significantly associated with older male patients with a long LOS. This finding suggested that removing observations with missing values (necessary before logistic regression implementation) could lead to a potential bias selection, resulting in a minimization of the effect size of predictors in logistic regression modeling. However, we ran consistent sensitivity multivariate analyses on imputed data (n=8,870) and the dataset excluding variable marital status, accountable for most of the missing information (n=8,522). The missing data exclusion did not significantly bias our main findings in multivariate models. These methodological steps strengthened the robustness of our final conclusions.
Our results should be interpreted in light of several methodological limitations. The first are those related to observational and retrospective studies (49, 50). We could not assess any causal relationship between explanatory variables and long-stay outcome. Our results were at the association level only. Future research on a national level will be needed to ensure better generalizability and address these questions about sector-level LOS determinants more accurately. For instance, it would be relevant to take hospital and ward policies about coercive measures into account, specifically when we investigate the impact of seclusion and restraint on length of stay. There is important literature about programs for reducing seclusion and restraint (51, 52). De-escalation techniques for psychosis-induced aggression or agitation (53), crisis prevention plans (54), tools like advanced directives in psychiatry (55), the use of “sensory rooms” (55), and a focus on a secure therapeutic relationship (56, 57) can help limit tension and the frequency of conflict. It would be interesting in a future study to investigate how these hospital-level and ward-level strategies might contribute to reducing length of stay.
Another limitation was the lack of data availability for some patient characteristics. We were not able to include, among explanatory variables, unemployment, a “proxy for current functional impairment” (21, 58), dependency (3, 25), symptom measurements, which could be used to assess clinical severity more accurately (9, 18, 28, 31), and biochemical markers obtained at the beginning of hospitalization (18). Nor could we evaluate the effect of the treatments received. To deal with polypharmacy impact, suggested strategies might be to stratify patients starting a treatment at the point of inclusion in the study and those already receiving treatment (59), grouping patients depending on the kind of treatment they receive (18). For future research, the medical record could include a traceability of precise reasons preventing patient discharge, whether clinical or organizational (e.g., no place available in a medico-social institution, a lack of rehabilitative programs at discharge, and no possibility of rehousing) (3). Future studies need to include all these factors. Our exploration was a proof of concept for other studies based on extended and national-level data.
LOS is an increasing focus for psychiatric hospitals, related to the need to reduce unnecessary healthcare costs. In this study, we used statistical and innovative machine learning tools to explore factors related to a long hospitalization. To the best of our knowledge, our study is the first in recent French literature to define a long stay with a clinically relevant duration threshold and focus on under-investigated variables such as the patient’s path characteristics, a somatic comorbidity, seclusion and mechanical restraint duration, and treatment compliance and resistance. Statistical modeling underlined the factors age >55 years, out-of-area hospitalization, and features relevant to illness severity as related to a long LOS. Our results also revealed the protective effect of variables such as admission during a travel-related psychiatric episode, being in a relationship, and a diagnosis of a personality disorder. The risk factors we highlighted should alert and encourage healthcare professionals to anticipate tailored coordinated action for early discharge. Our results are encouraging but we are cautious to generalize them to the French population. To achieve this, supplementary investigation should be carried out on a national scale. Such a study would also better highlight the role of regional characteristics such as healthcare organizations, social care, and housing policies. Future studies should also take factors related to medication patterns and biological analysis results into account. The use of symptom assessment data would also be justified to better reflect illness severity and its evolution during the stay.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the Paris Psychiatry Hospital Group Research Ethics Committee (accreditation no. 2024-CER-A-007). Written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
DB: Writing – original draft, Software, Methodology, Formal analysis, Data curation, Conceptualization. AP: Writing – review & editing, Validation, Methodology. HL: Writing – review & editing, Validation, Methodology, Conceptualization. AM: Writing – review & editing, Validation. CL: Writing – review & editing, Validation. VD-L: Writing – review & editing, Validation, Supervision, Methodology, Formal analysis, Conceptualization.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1463415/full#supplementary-material
1. Chevreul K, Prigent A, Bourmaud A, Leboyer M, Durand-Zaleski I. The cost of mental disorders in France. Eur Neuropsychopharmacol. (2013) 23:879–86. doi: 10.1016/j.euroneuro.2012.08.012
2. World Health Organization. WHO QualityRights Tool Kit - Assessing and improving quality and human rights in mental health and social care facilities. (Avenue Appia, 1211 Geneva 27, Switzerland: WHO Press, World Health Organization) (2012), 20.
3. Plancke L, Amariei A. Les hospitalisations longues en psychiatrie. Rev d’Épidémiologie Santé Publique. (2017) 65:9–16. doi: 10.1016/j.respe.2016.10.058
4. Babalola O, Gormez V, Alwan NA, Johnstone P, Sampson S. Length of hospitalisation for people with severe mental illness. Cochrane Database Syst Rev. (2014) 2014:CD000384. doi: 10.1002/14651858.CD000384.pub3
5. Cour des comptes. Rapport les parcours dans l’organisation des soins de psychiatrie. (13 rue Cambon 75001 PARIS: Cour des comptes) (2021).
6. Department of National Health Service UK. Modern standards and service model. (7 and 8 Wellington Place Leeds West Yorkshire LS1 4AP: National Health Service (NHS) England Digital) (1999).
7. ATIH (Agence Technique de l’Information sur l’Hospitalisation. IFAQ - Fiche descriptive Indicateur : Mesure des hospitalisations de longue durée à temps plein en soins libres. (117 boulevard Marius Vivier Merle 69329 Lyon Cedex 03: Agence technique de l'information sur l'hospitalisation) (2022).
8. Carranza Navarro F, Álvarez Villalobos NA, Contreras Muñoz AM, Guerrero Medrano AF, Tamayo Rodríguez NS, Saucedo Uribe E. Predictors of the length of stay of psychiatric inpatients: protocol for a systematic review and meta-analysis. Syst Rev. (2021) 10:65. doi: 10.1186/s13643-021-01616-6
9. Baeza FL, da Rocha NS, Fleck MP. Predictors of length of stay in an acute psychiatric inpatient facility in a general hospital: a prospective study. Braz J Psychiatry. (2018) 40:89–96. doi: 10.1590/1516-4446-2016-2155
10. Dimitri G, Giacco D, Bauer M, Bird VJ, Greenberg L, Lasalvia A, et al. Predictors of length of stay in psychiatric inpatient units: Does their effect vary across countries? Eur Psychiatry. (2018) 48:6–12. doi: 10.1016/j.eurpsy.2017.11.001
11. Wolff J, McCrone P, Patel A, Kaier K, Normann C. Predictors of length of stay in psychiatry: analyses of electronic medical records. BMC Psychiatry. (2015) 15:238. doi: 10.1186/s12888-015-0623-6
12. Gopalakrishna G, Ithman M, Malwitz K. Predictors of length of stay in a psychiatric hospital. Int J Psychiatry Clin Pract. (2015) 19:238–44. doi: 10.3109/13651501.2015.1062522
13. Tulloch AD, Fearon P, David AS. Length of stay of general psychiatric inpatients in the United States: systematic review. Adm Policy Ment Health. (2011) 38:155–68. doi: 10.1007/s10488-010-0310-3
14. Tulloch AD, Fearon P, David AS. The determinants and outcomes of long-stay psychiatric admissions: a case-control study. Soc Psychiatry Psychiatr Epidemiol. (2008) 43:569–74. doi: 10.1007/s00127-008-0332-2
15. Coldefy M, Nestrigue C. Long-stay psychiatric hospitalisation: analysis and determinants of territorial variability. (2014). Available at: https://www.irdes.fr/english/issues-in-health-economics/202-long-stay-psychiatric-hospitalisation.pdf.
16. Coldefy M. Les soins en psychiatrie: organisation et évolutions législatives récentes. Rev française Des affaires sociales. (2016) 2):21–30. doi: 10.3917/rfas.162.0021
17. Hirsch V, Strizyk A. Du secteur au territoire: l’offre de soins ambulatoire au sein de la Communauté hospitalière de territoire pour la psychiatrie parisienne. Rev française Des affaires sociales. (2016) 2):275–80. doi: 10.3917/rfas.162.0275
18. Cheng P, Wang L, Xu L, Zhou Y, Zhang L, Li W. Factors related to the length of stay for patients with schizophrenia: A retrospective study. Front Psychiatry. (2022) 12:818254. doi: 10.3389/fpsyt.2021.818254
19. Ismail H. Duration of hospital admission in severe mental illness: is longer better? BJPsych Adv. (2021) 27:213–8. doi: 10.1192/bja.2021.15
20. Addisu F, Wondafrash M, Chemali Z, Demissie T, Tesfaye M. Length of stay of psychiatric admissions in a general hospital in Ethiopia: A retrospective study. Int J Ment Health Syst. (2015) 9. doi: 10.1186/s13033-015-0006-x
21. Newman L, Harris V, Evans LJ, Beck A. Factors associated with length of stay in psychiatric inpatient services in london, UK. Psychiatr Q. (2018) 89:33–43. doi: 10.1007/s11126-017-9498-7
22. Stekhoven DJ, Bühlmann P. MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics. (2012) 28:112–8. doi: 10.1093/bioinformatics/btr597
23. Gandré C, Gervaix J, Thillard J, Macé J-M, Roelandt J-L, Chevreul K, et al. The development of psychiatric services providing an alternative to full-time hospitalization is associated with shorter length of stay in french public psychiatry. Int J Environ Res Public Health. (2017). doi: 10.3390/ijerph14030325
24. Jacobs R, Gutacker N, Mason A, Goddard M, Gravelle H, Kendrick T, et al. Determinants of hospital length of stay for people with serious mental illness in England and implications for payment systems: a regression analysis. BMC Health Serv Res. (2015) 15:439. doi: 10.1186/s12913-015-1107-6
25. Pariente P, Labarte S, Ménard F, Marcel E. Facteurs associés à la durée de séjour dans un établissement de santé en psychiatrie (2006). Available online at: https://www.semanticscholar.org/paper/Facteurs-associ%C3%A9s-%C3%A0-la-dur%C3%A9e-de-s%C3%A9jour-dans-un-de-Pariente-Labarte/61f48d9c60dc7db04be4263ff49ffb034619c38c. Accessed date: 01/05/2024.
26. Páv M, Vňuková M, Sebalo I. Factors affecting length of inpatient forensic stay: retrospective study from Czechia. Front Psychiatry. (2022) 13:825615. doi: 10.3389/fpsyt.2022.825615
27. Hitman MH, Gopalakrishna G. Predictors of length of stay in an acute psychiatric hospital . Available online at: https://www.semanticscholar.org/paper/Predictors-of-Length-of-Stay-in-an-Acute-Hospital-Ithman-Gopalakrishna/69c300946d336af4406b47125c28a692eb52b3e0. Accessed date: 01/05/2024.
28. Crossley N, Sweeney B. Patient and service-level factors affecting length of inpatient stay in an acute mental health service: a retrospective case cohort study. BMC Psychiatry. (2020) 20:438. doi: 10.1186/s12888-020-02846-z
29. Blais MA, Matthews J, Lipkis-Orlando R, Lechner E, Jacobo M, Lincoln R, et al. Predicting length of stay on an acute care medical psychiatric inpatient service. Adm Policy Ment Health. (2003) 31:15–29. doi: 10.1023/A:1026044106172
30. Gosek P, Kotowska J, Rowińska-Garbień E, Bartczak D, Heitzman J. Treatment resistance and prolonged length of stay among schizophrenia inpatients in forensic institutions. Psychiatry Res. (2021) 298:113771. doi: 10.1016/j.psychres.2021.113771
31. Joubert F. Hospitalisations au long cours en psychiatrie - Etude de l’hétérogénéité des pratiques entre établissements à partir de l’analyse de données médico-administratives et d’entretiens semi-directifs. Université Lyon, 143 Bd du 11 Novembre 1918, 69100 Villeurbanne (2015).
32. Di Lorenzo R. Retrospective analysis of factors associated with long-stay hospitalizations in an acute psychiatric ward. Risk Manage Healthcare Policy. (2020) n°13:433–42.
33. Lyketsos CG, Dunn G, Kaminsky MJ, Breakey WR. Medical comorbidity in psychiatric inpatients: relation to clinical outcomes and hospital length of stay. Psychosomatics. (2002) 43:24–30. doi: 10.1176/appi.psy.43.1.24
34. Honey A, Arblaster K, Nguyen J, Heard R. Predicting housing related delayed discharge from mental health inpatient units: A case control study. Adm Policy Ment Health. (2022) 49:962–72. doi: 10.1007/s10488-022-01209-y
35. Douzenis A, Seretis D, Nika S, Nikolaidou P, Papadopoulou A, Rizos EN, et al. Factors affecting hospital stay in psychiatric patients: the role of active comorbidity. BMC Health Serv Res. (2012) 12:166. doi: 10.1186/1472-6963-12-166
36. Barsky AJ, Peekna HM, Borus JF. Somatic symptom reporting in women and men. J Gen Intern Med. (2001) 16:266–75. doi: 10.1046/j.1525-1497.2001.016004266.x
37. Tulloch AD, Khondoker MR, Fearon P, David AS. Associations of homelessness and residential mobility with length of stay after acute psychiatric admission. BMC Psychiatry. (2012) 12:121. doi: 10.1186/1471-244X-12-121
38. Sharma SD, Kurien C. The length of stay of psychiatric inpatients. Indian J Psychiatry. (1987) 29:315–23.
39. Zhang J, Harvey C, Andrew C. Factors associated with length of stay and the risk of readmission in an acute psychiatric inpatient facility: a retrospective study. Aust N Z J Psychiatry. (2011) 45:578–85. doi: 10.3109/00048674.2011.585452
40. Yaniv-Rosenfeld A, Savchenko E, Netzer M, Elalouf A, Nitzan U. Socio-demographic predictors of hospitalization duration among patients with borderline personality disorder. Adm Policy Ment Health. (2024). doi: 10.1007/s10488-024-01388-w
41. Charre M, Phanm-Scottez A, Gourevitch R. Pathological trip: Concept news and cohort characteristics in a psychiatric emergencies unit . Available online at: https://www.em-consulte.com/article/1518662/voyages-pathologiques-actualites-du-concept-et-ca. Accessed date: 01/05/2024.
42. Galante J, Humphreys R, Molodynski A. Out-of-area placements in acute mental health care: the outcomes. Prog Neurol Psychiatry. (2019) 23:28–30. doi: 10.1002/pnp.528
43. Gentil L, Grenier G, Vasiliadis HM, Fleury MJ. Predictors of length of hospitalization and impact on early readmission for mental disorders. Int J Environ Res Public Health. (2022) 19:15127. doi: 10.3390/ijerph192215127
44. Wong HH, Yong YH, Shahwan S, Cetty L, Vaingankar J, Hon C, et al. Case management in early psychosis intervention programme: Perspectives of clients and caregivers. Early Interv Psychiatry. (2019) 13:598–603. doi: 10.1111/eip.12534
45. Barruel D, Hilbey J, Charlet J, Chaumette B, Krebs MO, Dauriac-Le-Masson V. Predicting treatment resistance in schizophrenia patients: Machine learning highlights the role of early pathophysiologic features. Schizophr Res. (2024) 270:1–10. doi: 10.1016/j.schres.2024.05.011
46. Vranda MN, Ranjith PJ, Aadi S, Gunasekaran DM, Thirthalli J, Naveen Kumar C, et al. Predictors of long-stay in a tertiary care psychiatry hospital in India. Int J Soc Psychiatry. (2023) 69:1979–85. doi: 10.1177/00207640231183916
47. Auffarth I, Busse R, Dietrich D, Emrich H. Length of psychiatric inpatient stay: Comparison of mental health care outlining a case mix from a hospital in Germany and the United States of America. German J Psychiatry. (2008) 11.
48. Peduzzi P, Concato J, Kemper E, Holford T, Feinstein A. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. (1997) 49:1373–9. doi: 10.1016/S0895-4356(96)00236-3
49. Talari K, Goyal M. Retrospective studies - utility and caveats. J R Coll Physicians Edinb. (2020) 50:398–402. doi: 10.4997/jrcpe.2020.409
51. Goulet MH, Larue C, Dumais A. Evaluation of seclusion and restraint reduction programs in mental health: A systematic review. Aggression Violent Behavior. (2017) 34:139–46. doi: 10.1016/j.avb.2017.01.019
52. Hirsch S, Steinert T. Measures to avoid coercion in psychiatry and their efficacy. Dtsch Arztebl Int. (2019) 116:336–43. doi: 10.3238/arztebl.2019.0336
53. Du M, Wang X, Yin S, Shu W, Hao R, Zhao S, et al. De-escalation techniques for psychosis-induced aggression or agitation. Cochrane Database Systematic Rev. (2017) 2017. doi: 10.1002/14651858.cd009922.pub2
54. O'Hagan M. Best practice in the reduction and elimination of seclusion and restraint; Seclusion: time for change. (PO Box 108 244, Symonds St, Auckland 1150, New Zealand: The National Centre of Mental Health Research, Information and Workforce Development) (2008).
55. Dauriac-Le Masson V, El-Khoury Lesueur F, Lahaye J, Launay C, Christodoulou A, Boiteux C, et al. Characteristics and correlates of seclusion and mechanical restraint measures in a Parisian psychiatric hospital group. Front Psychiatry. (2024) 15:1296356. doi: 10.3389/fpsyt.2024.1296356
56. Chieze M, Hurst S, Kaiser S, Sentissi O. Effects of seclusion and restraint in adult psychiatry: A systematic review. Front Psychiatry. (2019) 10:491. doi: 10.3389/fpsyt.2019.00491
57. Bowers L, James K, Quirk A, Simpson A, Sugar, Stewart D, et al. Reducing conflict and containment rates on acute psychiatric wards: The Safewards cluster randomised controlled trial. Int J Nurs Stud. (2015) 52:1412–22. doi: 10.1016/j.ijnurstu.2015.05.001
58. Glick ID, Sharfstein SS, Schwartz HI. Inpatient psychiatric care in the 21st century: the need for reform. PS. (2011) 62:206–9. doi: 10.1176/ps.62.2.pss6202_0206
Keywords: long stay, patient’s pathway, clinical severity, treatment compliance, treatment resistance, machine learning
Citation: Barruel D, Perozziello A, Lefèvre H, Msellati A, Launay C and Dauriac-Le Masson V (2024) Predictors of the length of stay in psychiatric inpatient units: a retrospective study for the Paris Psychiatry Hospital Group. Front. Psychiatry 15:1463415. doi: 10.3389/fpsyt.2024.1463415
Received: 11 July 2024; Accepted: 14 August 2024;
Published: 18 September 2024.
Edited by:
Panteleimon Giannakopoulos, Geneva University Hospitals, SwitzerlandReviewed by:
Stefan Kaiser, University Hospitals Geneva Medical Center, United StatesCopyright © 2024 Barruel, Perozziello, Lefèvre, Msellati, Launay and Dauriac-Le Masson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David Barruel, ZC5iYXJydWVsQGdodS1wYXJpcy5mcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.