- 1Department of Occupational Therapy, Monash University, Melbourne, VIC, Australia
- 2Department of Nursing and Allied Health, Swinburne University of Technology, Melbourne, VIC, Australia
- 3Department of Psychiatry, The University of Melbourne, Melbourne, VIC, Australia
- 4Northern Area Mental Health Service, Melbourne, VIC, Australia
- 5Occupational Science and Therapy, Deakin University, Geelong, VIC, Australia
- 6Department of Occupational Therapy, Western Health, Melbourne, VIC, Australia
- 7School of Rehabilitation Therapy, Queens University, Kingston, ON, Canada
Introduction: Time use is an important indicator of health and well-being. Exploration of time use can provide in-depth information about individuals’ activity patterns including routines and structure, the experience of activities, personal priorities and challenges. People experiencing severe mental illness may be at particular risk for time use patterns associated with poor health and wellbeing.
Methods: This scoping review aimed to identify and map the evidence about how a time use perspective informs assessment and intervention in community mental health practice. Electronic databases and hand-searches were used to identify relevant studies involving people with severe mental illness, and focused on time use applications in practice. Twenty-nine studies were included in this review, data-extracted and synthesized with reference to the review question.
Results: Of the twenty-nine identified studies, seven described development and psychometric testing of time use assessments; twelve used time use tools to measure outcomes; and ten described or evaluated time use intervention approaches. The identified time use assessments typically involved retrospective diaries completed before or during structured interviews, and an Experience Sampling Method using smart technology to gather activity data in real time. Both psychosocial and occupational interventions used time use to measure outcomes relevant to activity engagement, social functioning, and personal recovery. The identified time use interventions originated in occupational therapy; included structured manuals and workbooks to enable reflection on daily time use; individual or group sessions to collaborate in identifying priorities, goal planning and supporting desired changes to activity patterns. These interventions were viewed favorably overall, with improved activity engagement, quality of life, and personal recovery reported.
Discussion: Time use assessments evaluate outcomes of importance to personal recovery and community inclusion. Time use interventions address activity patterns associated with poor health and wellbeing, using collaborative and supported activity engagement approaches, and contribute to emerging evidence on interventions that support personal recovery. Furthering peer involvement in developing and delivering these interventions will bring important insights to time use practice and research, while the social forces that marginalize or constrain activity participation for people with severe mental illness also need to be addressed to advance time use and other approaches that aim to support community inclusion.
1 Introduction and background
How people spend their time has long been recognized as an important indicator of health and well-being in various disciplines. Early in the 20th century, Adolf Meyer (1), a psychiatrist, espoused that the active and purposeful use of time had the potential for both restoring and maintaining health; and that the ways in which individuals used and organized their time reflect adjustments to daily living demands. Such principles informed the beginning development of the occupational therapy profession in the 1920s, and the conceptual roots of the recovery movement (2). Time use is of continuing interest in occupational therapy principally as a means to understand and address disrupted and restricted activity patterns that contribute to individuals’ risk for ill-health (3). Further, as part of their public health strategies, many nations routinely collect time use data to better understand and influence the health and well-being of the general population (4). This emphasis on time use is grounded in the belief that various features of activities – such as frequency, meaning, repetition, duration, and variety – within a temporal context can either promote or compromise health. Public health applications of time use specifically target populations at risk for poor health and well-being due to problematic time use patterns with wide-ranging social impacts (4). As illustrative examples, these include adolescents’ time use patterns associated with risk-taking, problem behaviors and mental health (5, 6); differences in time use among mothers and fathers (7); and health and well-being concerns emerging from time use patterns of unemployed youth, retirees and older adults such as a predominance of sedentary activity (8–12).
Ongoing health conditions, associated functional limitations and disability have also been linked to time use patterns that further contribute to poor health and wellbeing (13–16). For instance, a number of time use studies involving community dwelling people with severe mental illness have reported imbalanced activity patterns that show limited time spent in productive activities (such as work, parenting, education) and most time spent in sedentary or passive leisure activities (e.g. watching TV), self-care (e.g. eating and sleeping) and alone (17–20). Health and well-being concerns about such time use patterns include the limited variety of activities that individuals experience, reduced opportunities for community contributions and participation, weakened social connections and overall social marginalization (17).
Time use is an important way of conceptualizing and understanding engagement in activities and their impacts on health and wellbeing for people with severe mental illness. It provides insight into how people structure their time, their priorities, the social and spatial contexts of their lives and key barriers they face (21). Time use contributes to understanding how activity patterns are related to community inclusion and adjustment (17). Time use practice approaches offer a collaborative way to map day-to-day experiences, enabling individuals to reflect on the impacts of their daily activity experiences on their health and wellbeing (13, 22). Furthermore, opportunities to engage in personally and socially meaningful activities have consistently been identified by people living with severe mental illness as an important element of personal recovery, a process that differs individually but broadly involves creating a life of well-being and meaning with or without the continuing presence of illness (23–26). The potential of engagement in self-chosen activities to support personal recovery lies in their capacity to create conditions for building hope, meaning and purpose in life, developing social connections in communities of choice and ways of self-managing one’s health in everyday life (27–29). As such, the extent to which time use focused approaches support people in their recovery should be considered an important outcome (3).
This paper focuses on time use as a practice approach for working with people with severe mental illness to construct self-chosen, meaningful and health-enhancing activity patterns and thereby to support recovery and wellbeing. To the best of our knowledge, the available evidence to guide time use focused practice approaches to these issues in mental health care has not previously been mapped or synthesized. A scoping review approach was considered appropriate for this purpose, given the authors’ understanding that the evidence base in this area is diverse in both research methodologies and disciplinary context (30). The concept of time use has been used in public health and social sciences as an indicator of productivity, mental health, happiness and quality of life; and to understand the impact of disability at individual and population levels (4, 15). Describing the extent, range and content of the available evidence will provide a clearer basis for practices informed by a time use perspective, as well as rigorous guidance for ongoing practice developments and research directions.
1.1 Aims and objectives
The overall aim of this scoping study was to synthesize evidence on practice applications of a time use perspective to support the personal recovery of people with severe mental illness. The specific review question was: ‘How does a time use perspective inform assessment and interventions within community mental health practice?’
2 Materials and methods
This scoping study utilized the method originally developed by Arksey and O'Malley (31) and further elaborated by Levac et al. (32). It includes six steps: a) identifying the research question; b) identifying relevant studies; c) study selection; d) charting the data; e) collating and synthesizing the results; and f) consultation. While a protocol was not registered for this scoping review, the reporting of this scoping review conforms to the PRISMA Extension for Scoping Reviews (PRISMA-ScR) (33).
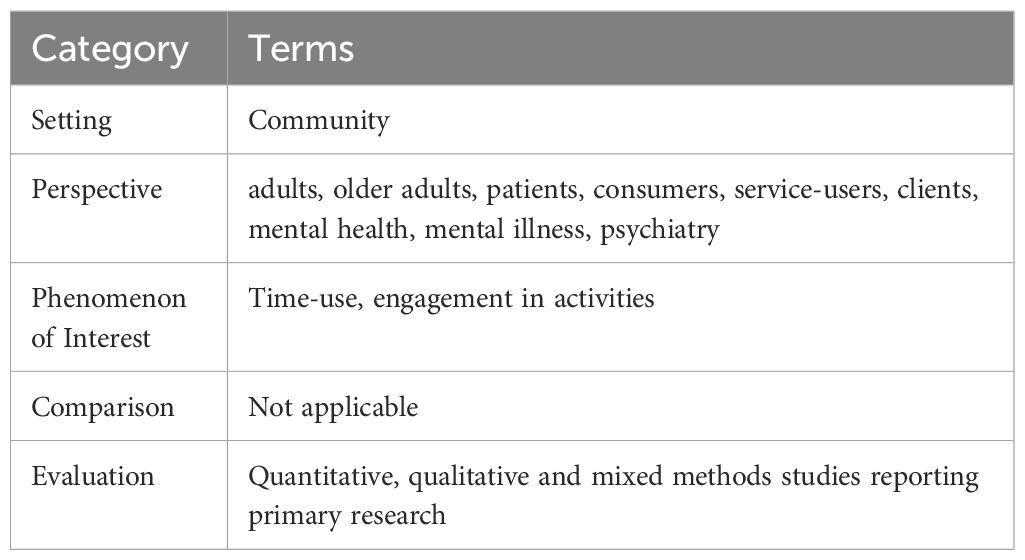
The research team consisted of senior academics and community mental health clinicians with substantial research and practice experience of time use assessment and intervention. The team identified the review question from their professional knowledge of gaps in current understanding and applications of a time use perspective in mental health practice. The review began with a preliminary search on Google Scholar guided by the SPICE framework (34) to assist in identifying the key concepts (Table 1).
The final search strategy was developed in consultation with a university librarian with expertise in health databases; and tested through a trial search of the EBSCOHOST platform. Examples of the search terms included “Mental disorder*” or “Psychotic disorder*” or “Schizophreni*” or “Mental illness*” or “Psychosocial disability*” or “Psychiatric disorder*” or “Psychiatric patient*” or “Mentally ill”; AND “Time use” or “time use” or “Use of time” or “Occupational balance” or “Occupational engagement*”. Supplementary Table S1 in Supplementary Materials presents the search strategy.
The search strategy included limiters to ensure sources were peer-reviewed, published in English and included adults (age 18 or older). Book chapters, conference papers, theses, pre-prints, study protocols and letters were excluded. No time limits were set, so as to locate any studies focused on time use applications in community mental health practice. Nine databases were selected to identify studies meeting the inclusion criteria, including five databases within EBSCOHOST platform (Academic Search Complete; CINAHL Complete; Health Source – Nursing/academic; Social Work abstracts; SocINDEX) and four other databases: PsycInfo, PsycArticles, Scopus, and Web of Science. The database searches were last updated in June 2024.
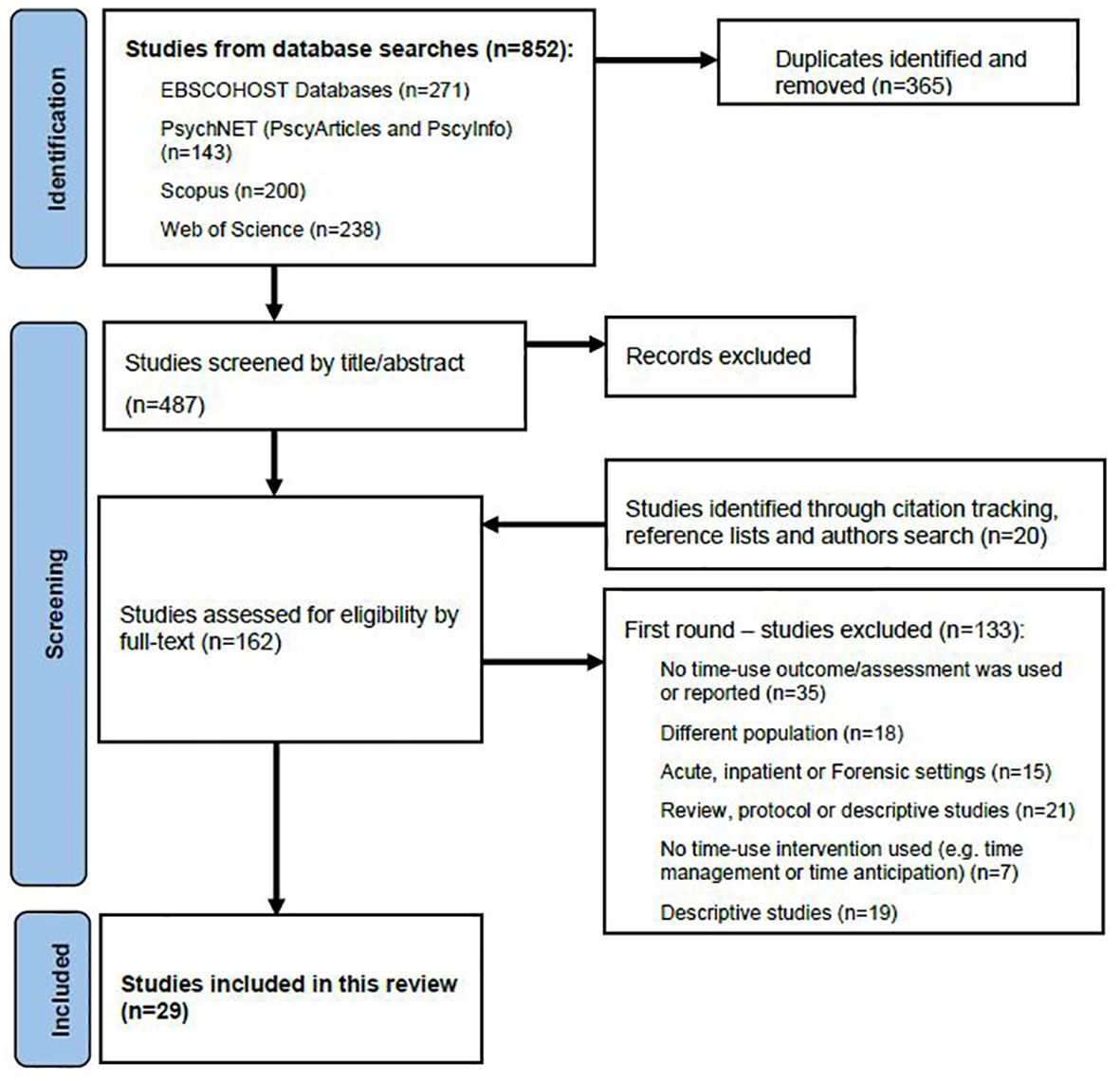
After duplicate removal, 487 studies were imported to Covidence for screening. Two authors (ND, EF) independently screened all studies, with disagreements discussed and resolved by consensus in regular meetings. Title and abstract screening excluded 345 studies, leaving 142 sources to proceed to full-text review. At this stage, the reference lists of included studies were searched for further potentially relevant sources. Google scholar was also used for citation tracking and searches of key authors or journals to retrieve studies that may have been missed in the database searches. These processes identified a further 20 potentially relevant studies for full text screening. Therefore, the full text of 162 studies were reviewed for eligibility, resulting in 29 studies being included in this review based on the following criteria:
a) studies were of time use assessments, time use as an outcome measure or time use focused interventions (i.e. studies describing time use patterns, time spent in specific activities such as employment, internet-use, or physical activity, or investigating time use associations with clinical and socio-demographic factors were excluded);
b) study participants were people with severe or persistent mental illness, defined as a primary diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, or other severe and enduring psychotic disorder (29) (i.e. studies involving people with other diagnoses such as depression and anxiety were excluded);
c) studies were conducted in community or outpatient setting (e.g. excluding studies in inpatient or secure settings); and
d) papers reported original studies (i.e. excluding reviews, protocols and secondary analyses).
Figure 1 illustrates the screening and selection processes, using a PRISMA flow diagram (35). The resulting studies were grouped into three main categories: 1) development and psychometric testing of time use assessments (n=7); 2) studies using time use as an outcome measure (n=12); and 3) studies of time use focused interventions (n=10).
Data were extracted from the 29 studies according to key fields suggested by Arksey and O'Malley (31): authors, location, study aim, methodology and design, and key findings. Additional fields relevant to our review question were used to record details about participants (e.g. diagnosis, gender), time use assessments, outcome measures and interventions, as well as other data collection methods, implications and limitations. The team developed the data extraction template, with all data extracted by a single author (ND) and presented in three separate tables based on the review question: time use assessments, time use as an outcome measure, and time use focused interventions. Within each table, similarities and differences between the studies were compared. For example, similarities between approaches to completing time use assessments, and in the development and delivery of time use interventions, were compiled by two authors (ND, EF), to synthesize the results.
3 Results
3.1 Study characteristics
The 29 included studies were published between 2006 – 2023. The majority were from Sweden (n=14), followed by the UK (n=7), Canada (n=2), Italy (n=2), Australia (n=2), Denmark (n=1) and Portugal (n=1). Most studies recruited participants from community mental health settings; three studies recruited participants from multiple settings including in-patient, residential and outpatient clinics; and two recruited from supported residential settings. Study methodologies included randomized control trials (n=14), psychometric testing (n=5), qualitative methods (n=5), pilot or feasibility studies (n=3), one correlational study, and one mixed-methods study. Most studies were designed and conducted by occupational therapists (n=20) including four studies that developed or tested time use assessments, and all studies of time use interventions. Others involved the disciplines of psychiatry, psychology and social sciences.
3.2 Time use assessments
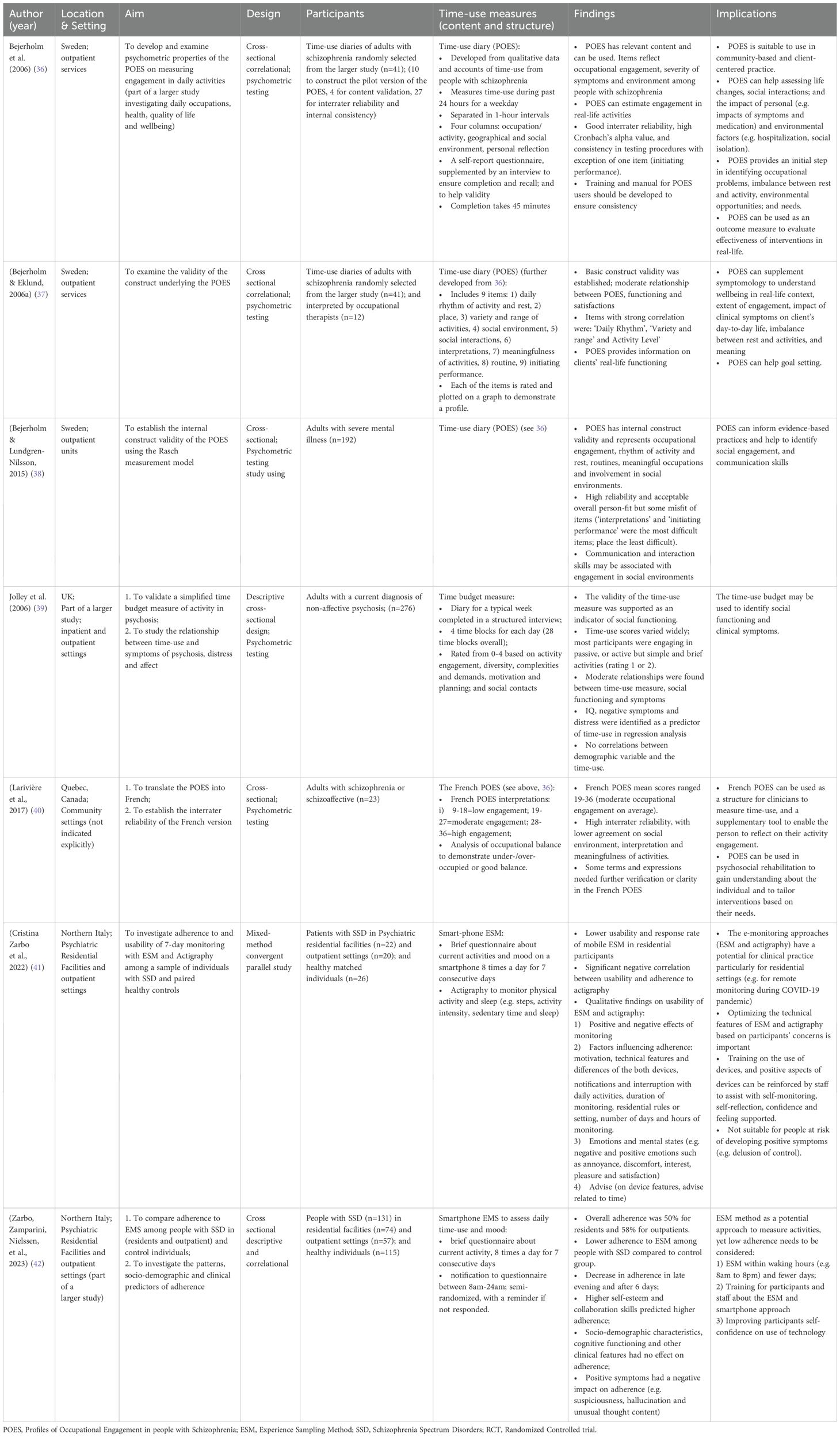
Seven studies reported on the development, psychometric testing or practice application of time use assessments (Table 2). Two of these assessment tools are based on time use diary methods and one uses the Experience Sampling Method (ESM), as described below.
3.2.1 Development of time use assessments
Four studies reported the development and psychometric testing of the Profiles of Occupational Engagement in people with schizophrenia (POES) (36–38). The POES was developed by occupational therapists drawing on accounts of time use and occupational engagement from people diagnosed with schizophrenia (43, 44), previous literature and the authors’ clinical expertise.
The POES utilizes a 24-hour time use diary designed for a person to report their activities in one-hour blocks of time for the preceding weekday. It asks the person to record their activities (i.e. what they were doing, and how long for), the place and the social context (i.e. who else was present or if on their own), and a personal reflection or comment about how the activity was experienced. This is supplemented by an interview (typically about 45 minutes) to support the person’s completion of the diary and reflection on personal experiences related to the activities recorded in it. The POES also allows the rating of activity engagement across nine key areas: 1) daily balance of activity and rest; 2) geographical location; 3) variety and range of activities; 4) social environment; 5) social interactions, 6) individuals’ experiences and interpretations; 7) meaningfulness of activities and/or contribution to wellbeing; 8) daily routines; and 9) initiating performance. Each is rated on a 4-point scale (36–38), highlighting personal and contextual factors that contribute to patterns of time use and activity engagement.
The POES was reported to have good interrater reliability, construct validity, and utility in understanding individuals’ level of engagement, wellbeing, functioning and social participation (36–38). A French version developed in Canada also demonstrated sound psychometric properties and utility as a measure of activity engagement in the mental health context (40). Bejerholm and colleagues further suggest the POES is relevant for mental health practitioners to use since it accurately reflects activity engagement in real-life settings and may aid understanding of how not only psychiatric symptoms and treatments (e.g. medication) but also available resources impact the everyday lives of individuals experiencing severe mental illnesses.
Another time diary-based activity measure intended for routine clinical use with individuals living with psychosis was developed by Jolley et al. (39). Their simplified time budget is completed in a structured interview designed to record a person’s activities over seven days in four daily blocks of time, and to support recall of activities and social contacts. Activities are then rated by the interviewer on a 0-4 scale according to their demands (e.g. whether passive, active but simple, or more complex or socially demanding activities). Jolley et al. (39) reported that this simplified time budget is able to discriminate levels of activity, showed stronger associations with symptom distress than symptom severity, and suggested its use as an indicator of social functioning.
The third identified assessment was a smartphone-based Experience Sampling Method (ESM) for assessment and monitoring of daily life experiences, such as activities, mood, sleep, and symptomatology. In a series of mixed-method studies, Cristina Zarbo et al. (20), Zarbo et al. (41) and Zarbo et al. (42) investigated the feasibility of using smartphone-based brief questionnaire to prompt sampling of experiences of current activities and mood in real time at eight intervals daily (between 8am to midnight) over a week. Their findings suggested the ESM as a useful tool for supporting people with severe mental illness to reflect on their activity engagement, and for staff to gain insights into their daily lives in community settings where regular assessment may be challenging. Some participants disliked the technical features of this approach and its interruptions to their daily activities, while the authors also acknowledged that ESM may be experienced as intrusive or distressing in the context of positive symptoms and recommended reduced sampling times, better training and technical support.
3.2.2 Application in practice
The time use assessment methods identified in this review provide varied ways to gather information on time use patterns and influencing factors in real-life contexts including, for example, resources, supports, symptoms, medication and satisfaction (20, 36, 37, 41). They also provide tangible information readily transferable to collaborative priority setting and planning (36, 37). The POES, for example, includes contextual information about places and people with whom activities are completed, from which resources to support change may be identified (36, 37). In comparison, the simplified time budget (39) may be easier to complete than the POES and less intrusive than the Experience Sampling-based approach. Since it focuses more on the level of activity involvement than on dimensions of activity engagement and experience, it may also be less useful to guide interventions. While originating in occupational therapy, the POES could be used by mental health professionals widely to guide person-centered and evidence-based community practice (40). The potential of the POES and ESM methods to support self-reflection also suggests their potential relevance for facilitating the process of personal recovery.
3.3 Time use as an outcome measure to evaluate effectiveness of interventions
Twelve studies (including three sub-studies from a larger project) measured time use as an outcome when evaluating the effectiveness of psychosocial and occupational interventions (Table 3). These interventions included staff training about activity engagement, its importance for addressing mental illness and approaches to encourage engagement (49); Individual Placement and Support (IPS) (45, 48); cognitive remediation (50); Social Recovery Therapy (SRT) (based on cognitive behavioral strategies) (52–54); a befriending program (56); lifestyle modification (51) and occupational therapy group programs (55).
Six of the intervention studies measured time use as an outcome using a Time Use Survey (TUS). Adapted from the UK 2000 Time Use Survey for general population (58), the TUS is completed via semi-structured interview and asks about time spent over the past month in activities that include work, education, volunteering, leisure, sport, hobbies, socializing, household chores, resting, childcare and sleep. To date, the TUS has been variously used to measure time spent in structured activities (excluding resting and sleep) as an indicator of overall functioning (50, 52, 53); economic and structured activity participation (55); social participation (e.g. places visited and people with whom activities were completed) (56); and time use as an indicator of social recovery (54). In two studies, cut-off scores for social disability (≤30 hours per week in structured activities) (53) and isolation (< 1 hour per day in recreational or social activities) (56) were applied to determine participants’ eligibility for the intervention, although neither reported how the cut-off scores were determined. Fowler et al. (53, 54) found that the SRT was effective in improving engagement in structured and economic activities. Fowler et al. (54) and Inman et al. (55) concluded respectively that the TUS is a relevant and sensitive measure of real-world functioning, and a suitable outcome measure for evaluating individualized occupational therapy interventions.
Based on a similar approach to the TUS, the previously described time budget (39) was used by Cardoso et al. (49) to measure the effectiveness of a staff training program to improve the activity engagement of people with schizophrenia living in residential facilities. They reported improvements in activity engagement, although these were not statistically significant when compared with the control group. Given the time budget measures activity engagement in 4 blocks daily, it may possibly be less sensitive to activity changes than the POES that records activities at 1-hourly intervals.
Five identified intervention studies reported use of the POES (36, 37) as an outcome measure. POES has been used to measure activity engagement and community inclusion outcomes of IPS programs for people experiencing severe mental illness (45, 48), with significant improvements reported with more engagement in a range of activities and community contexts. Further, when used to measure the outcomes of a lifestyle intervention, Active in My Home (AiMH), for people living in supported housing, significant improvements in activity engagement measured by POES and personal recovery measured by QPR (59, 60) between baseline and completion of the AiMH intervention were reported (51). Further highlighting links between activity engagement and personal recovery outcomes, Argentzell et al. (46) used the POES in conjunction with the Satisfaction with Daily Occupations and Occupational Balance (SDO-OB) (61) to identify aspects of activity engagement (e.g. balance and meaning) associated with effectiveness of the manualized Balancing Everyday Life (BEL) intervention (described in the next section). They reported activity engagement, mastery, satisfaction and symptom severity as the strongest mediators of changes in personal recovery following the intervention. Lastly, Bjorkedal et al. (57) used the POES as a primacy outcome in an evaluation of the Meaningful Activities and Recovery (MA&R) intervention, which combines group and individual sessions and is co-delivered by an occupational therapist and a peer worker to encourage activity engagement and recovery through education, reflective questions, peer exchange of ideas, workbooks and creative methods. No significant improvements in activity engagement were found in the MA&R group compared to those receiving standard occupational therapy services, possibly due to similarities between MA&R and the standard service. Overall however, these five intervention studies suggest POES as a useful tool for evaluating the outcomes of interventions designed to enable changes in the nature and quality of time use patterns.
3.4 Time use focused interventions
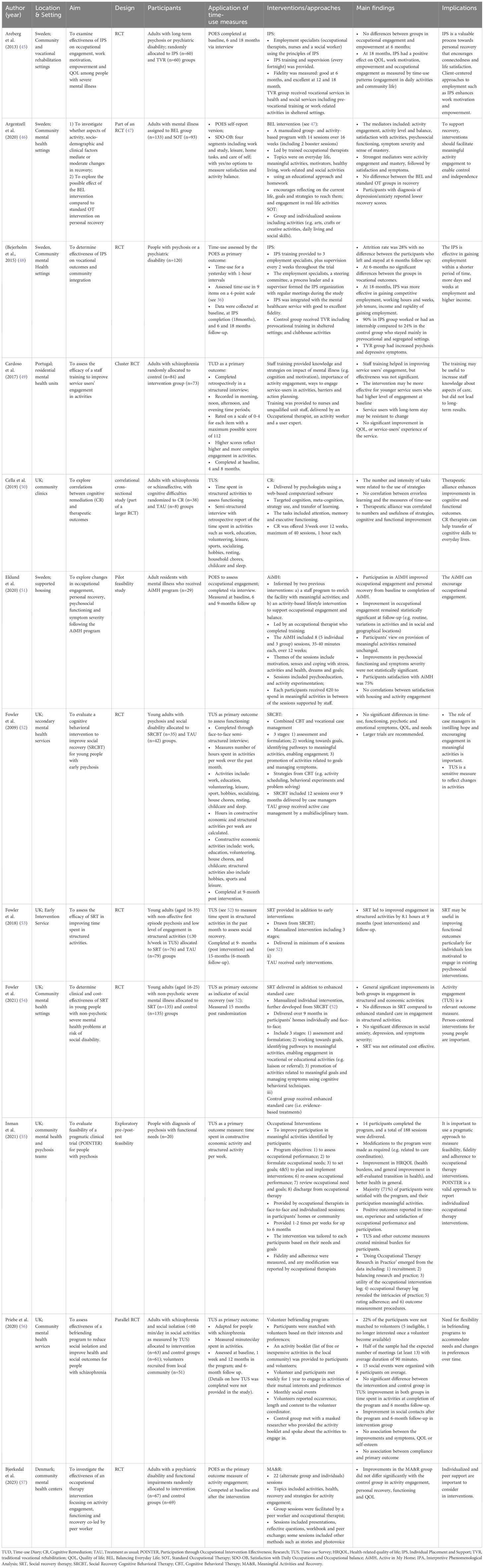
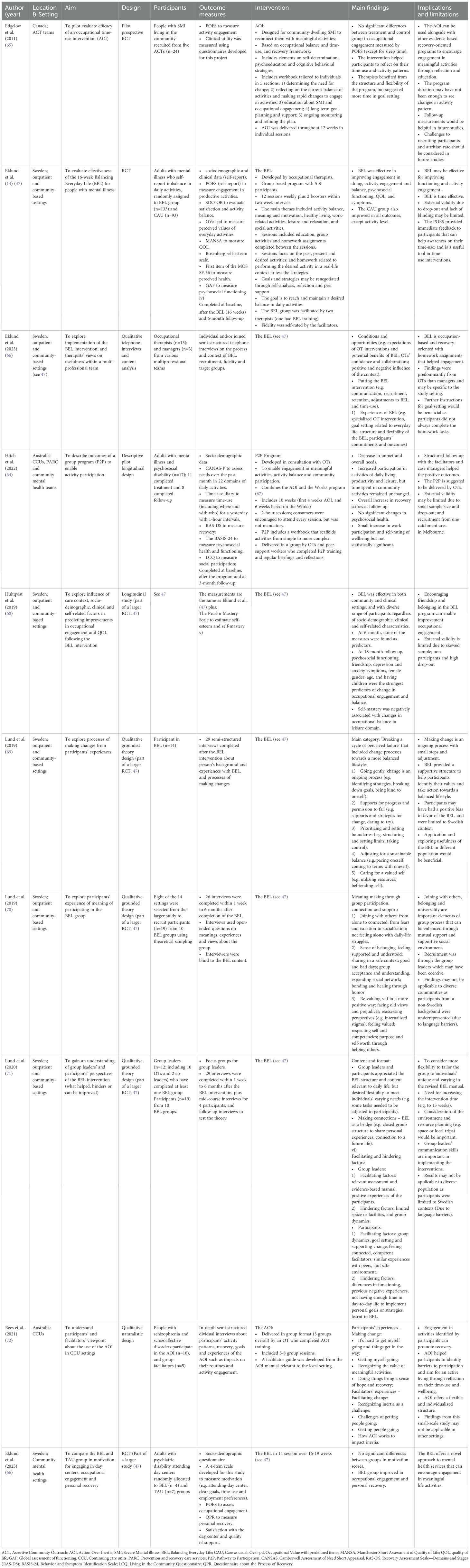
Ten studies reported the development and evaluation of time use interventions, including Action over Inertia (AOI) (62, 63), Balancing Everyday Life (BEL) (47) and the Pathway to Participation (P2P) program (64). All three interventions were developed by occupational therapists and focus on participants’ time use and developing strategies and supports to engage in desired activities (see Table 4).
3.4.1 Development, content and structure of the time use interventions
The three identified time use interventions are grounded in knowledge that what people do in everyday life matters for health and wellbeing; informed by recovery-oriented practice principles; and draw on educational and cognitive behavioral strategies (14, 62–64). Broadly, they aim to enable engagement in meaningful activities through a combination of educational, activity-based, group or individual sessions, and practice assignments related to engagement in real-world activities. Each uses a manual or participant workbook. They also each emphasize reflection on time use patterns as a means to develop understanding of health and well-being related aspects of activity engagement, and to bring about desired changes in activity patterns.
Action Over Inertia (AOI) (62, 63) was developed by Canadian occupational therapists as a person-centered, strengths-focused and flexible workbook-based approach for supporting individuals to construct activity patterns that enable fulfilling lives. The workbook provides resources, including time diaries, to support individuals to reflection on personal activity patterns and development of strategies for enabling rapid activity changes, supported planning for change, and ongoing supports for sustainable changes (65). More recently, AOI in group formats with 4-10 sessions have been described (63, 72). Integrating the AOI approach with a manualized vocational program, The Works (67), the Pathway to Participation (P2P) group program is designed to scaffold support for activity participation and build momentum for group members to engage in more complex and demanding occupations over time (64).
Balancing Everyday Life (BEL) (47) is a manualized group-based lifestyle intervention designed for people using community-based mental health services. Developed by Swedish occupational therapists, it aims to facilitate engagement in desired activities identified by participants and support for personal recovery (47). Of longer duration than AOI and P2P group programs, the BEL intervention consists of 14 group sessions over 16 weeks and addresses themes relevant to everyday life and personal recovery, including activity balance, meaning and motivation, healthy living, work-related activities, leisure and relaxation, and social activities (14, 66). Each BEL session includes an educational component, a group activity and a home assignment to try out preferred activities and strategies.
All ten studies reported the time use interventions were facilitated by at least one occupational therapist; only P2P groups were co-facilitated with peer or lived experience workers. All reported facilitator training and regular briefings (47, 64, 65).
3.4.2 Experiences and effectiveness of the time use interventions
All ten studies of time use interventions reported positive outcomes. The BEL has been evaluated in rigorous RCT studies that demonstrate it is effective in improving activity engagement, as represented in increased activity levels and more optimal activity balance, and improving personal recovery, clinical symptoms, psychosocial functioning and general quality of life (47, 68). Eklund et al. (47) also reported significant improvements in the control group in activity engagement, satisfaction with activities, symptoms, functioning and general quality of life. The authors suggest this may be attributed to the use of the POES as an outcome measure since it encourages reflection on current activity patterns and their impact on wellbeing, which may itself be a strong agent for change and promote activity engagement independent of the intervention.
A pilot RCT of AOI delivered individually over 12 weeks also showed small but not statistically significant activity changes: decreased time spent sleeping and increased general activity compared to a control group (65). The 10-week P2P group program was evaluated using a non-randomized, longitudinal study design. It too reported improvements in self-rated recovery scores and reduction of unmet needs through activity engagement, but no changes were detected in time use or psychosocial health measured using the Behavior and Symptom Identification Scale (BASIS-32) (64).
Five qualitative studies explored participants’ and facilitators’ experiences of the time use interventions; four of which related to the BEL (Table 4). Overall, participants reported the BEL program structure and content tailored to their skills and interests were helpful, along with opportunities to connect with peers and share life experiences in a supportive environment (69–71) This suggests connectedness and belonging were central to participants’ experiences of the BEL intervention (70). The group components also encouraged reflection, envisioning and connecting to a more positive future, and sustaining change (69–71). However, participants suggested more flexibility to tailor the program to their needs, and more time and support for goal setting and implementing strategies in daily life would be helpful (71). The BEL group facilitators also perceived the program structure of the program as beneficial, along with its alignment to occupational therapy through activity engagement and promotion of collaboration within multidisciplinary teams (71). From their experience, the main barriers in implementing BEL were variation in individual needs and challenges, limited space or information technology issues (71).
Regarding AOI groups, Rees et al. (72) also reported participants’ experiences of time use were changed by reconnecting with the value of meaningful activities and addressing barriers to sustaining activity engagement. The facilitators reported the concept of ‘inertia’, as conceptualized in the AOI, helped to identify restricted time use patterns and participation barriers as potential drivers for change. Rees et al. (72) also highlighted the value of peer learning and support when addressing time use, and recommended peer worker involvement in AOI group facilitation.
4 Discussion
This scoping review aimed to synthesize evidence addressing the review question: ‘How does a time use perspective inform assessment and interventions in community mental health practice?’
The findings identified applications of a time use perspective to develop methods of assessment, to measure the effectiveness of interventions, and as a basis for structured interventions in community mental health practice. Here considerations for their further use are discussed.
4.1 Time use assessment and outcome measures
Measuring time use is complex given the diversity of human activity and how multiple simultaneous activities or activities with intermittent interruptions occur across time (73). This review identified three approaches to time use assessment and evaluation currently being used: 1) measures collecting data at fixed intervals using pre-determined activity categories (e.g. TUS); 2) measures collecting data at fixed intervals with activities defined by people with severe mental illness themselves (e.g. POES); and 3) multiple daily spot sampling methods for capturing activity data in real time (e.g. ESM) (73, 74), as explored using smart phone technology (e.g. 41, 42).
Categorizing time use according to predetermined categories of activities has a long history in public health and social sciences for understanding human behavior in a temporal context; determining activity patterns and balance; identifying time use trends in structured or economically valued activity; and as an indicator of wellbeing or quality of life (4, 74). This approach is reflected in Time Use Survey (TUS) instruments, originally developed for population studies, and used to evaluate outcomes in six intervention studies identified in this review. These studies evaluated differing psychosocial and occupational interventions and indicate that the TUS is a relevant and sensitive measure, suitable for evaluating interventions designed to provide individualized support for activity engagement broadly or for participation in specific domains such as employment or socialization. The use of TUS offers advantages of well-understood language for reporting activity categories to enable communication of study results and comparability between studies (74). It also offers opportunities to consider the time use of people with severe mental illness in relation to that of the general population (74) and also specific groups within the general population (e.g. those not in the workforce, retirees, carers), as part of a more nuanced approach to analysis of activity patterns and disruptions (62, 63).
There are drawbacks to the application of TUS for time use assessment and evaluation in mental health practice. For instance, pre-determined activity categories have limited use to understand aspects of activity experiences, like their variety, meaningfulness, satisfaction and social aspects (e.g. where and with whom activities were undertaken). These aspects contribute to a holistic understanding of person’s time use, including activity experiences within temporal and social contexts, that is necessary to illuminate the interacting biological, psychological and social forces in which many activity disruptions experienced by people with severe mental illness are situated (63). An alternative approach to time use assessment, such as the POES (36), focuses on activities as defined by people with severe mental illness themselves and is more able to evaluate a range of health and well-being aspects of activity engagement that are sensitive to the influence of complex factors like capacities, experiences, and the course of recovery (36, 37, 48, 51). In so doing, POES highlights the extent to which a person’s activities are aligned with their values, capabilities and resources (14). As indicated by the studies in this review, this means POES is a useful tool for assessment and evaluating outcomes of importance to both personal recovery and community inclusion.
The time use assessments identified in this review also appear to be valuable and inexpensive tools for reflection on one’s time use, health and well-being through activity, developing awareness of personal needs and issues, describing the frequency and experiences of related behaviors, identifying the impacts of symptoms, treatments and resources in daily life, and informing goal planning (36, 37, 39). However, further evidence of the potential of time use based reflective tools to support self-determination, and to enable individuals to self-monitor their time use in relation to health and wellbeing, as part of recovery oriented and self-management approaches needs development (75). With activity-related on-line information and resources, tracking devices and other applications continuing to advance, the ESM approaches are particularly well suited for integrating time use information into person-centered recovery-oriented care and self-management tools, such as the Wellness Recovery Action Plan (WRAP) (76). Yet, the needs of people with severe mental illness for sustainable and equitable access require further consideration to overcome the ‘digital divide’ posed by socioeconomic circumstances (77).
Some limitations of time diary-based assessments, such as POES (36) and the simplified time budget (39), should be noted. While they typically include a retrospective interview that offers opportunities for practitioners to explore perceptions of activity engagement and time use, difficulties related to recall may be more pronounced for individuals with severe mental illnesses due to cognitive issues, lack of daily prompts or routines, or issues related to reporting particular activities. The most recent version of Action over Inertia (63) prompts practitioners to consider unreported daily activities, such as work for informal payments, using or selling drugs, begging, and other forms of activities that may have personal value but can also adversely impact health and wellbeing. Spot sampling methods with multiple daily reminders (e.g. ESM) can overcome recall challenges and offers more flexibility in measuring activity duration (73, 74), but issues with low adherence and accuracy of responses over an extended period (over 5-6 days), technical difficulties with devices, and potential exacerbation of positive symptoms are also reported (20, 41, 42). These are important issues for which engaging lived experience and professional perspectives in co-designing solutions will benefit future developments.
4.2 Interventions
While daily time use is a highly personal experience, influenced by various factors embedded in larger environmental contexts (e.g. culture, income, neighborhood structures, family expectations), the interventions identified in this review explicate the knowledge base and standardized processes underlying practice for addressing health and well-being aspects of time use collaboratively with people with severe mental illness. They contribute to emerging evidence on interventions supporting personal recovery (78–80). The effectiveness and external validity of these intervention may be limited. For example, most studies reported small number of participants, issues with retention and work conducted in specific contexts (e.g. Swedish mental health services). The authors of the Randomized Control Trial studies acknowledged that lack of blinding may have also impacted the findings (14, 65).
Ongoing advancements in the field are leading to the inclusion of a broader range of factors that influence implementation of interventions in practice. The BEL, AOI and P2P interventions utilize either group or individual session formats that can be modified or adapted to individuals’ needs and preferences. They also all include homework or activity experimentation based on personal goals, aligned with current knowledge regarding the transference of choices made in therapeutic settings to the real-world, including the importance of ongoing support, evaluation and adaptation (81). While peer learning and support were also identified as beneficial aspects of the group programs (70, 72), only P2P involved lived experience co-facilitators. Given emerging evidence that peer involvement in developing and delivering social interventions contributes to positive outcomes (82), this is an important avenue for further development of time use focused interventions.
Thinking ahead, the field may benefit from advancing and implementing conceptual frameworks to systematically link time use activity patterns with personal recovery, health and well-being for people with severe mental illness. This would ensure shared definitions, demonstrate the links between activity patterns and health and well-being, support the evidence base, and serve as a foundation for comparing measurement tools and intervention approaches. For example, the Do-Live-Well Framework (DLW) (83–85), a conceptual framework from Canada, identifies eight activity experiences and five activity patterns previously shown to impact health and well-being. Integrating such a framework in the mental health field depends on further study of its relevance to people with severe mental illness living in the community, such as aligning to their goals and preferences.
Ensuring that the complex factors influencing time use are systematically considered in intervention approaches depends on integrating theory and conceptual models into their design, as well as lived experience and professional perspectives. The International Classification of Functioning, Disability and Health (ICF, 86), recovery frameworks (80, 87, 88), and understandings of cognition and motivation provided the foundation of time use scholarship and practice in the mental health field. With the growing understanding of the social forces that marginalize or constrain activity participation for people with severe mental illness, these must be addressed in any intervention approach that purports to focus on supporting community inclusion and quality of life (89). Hence, the updated version of AOI (63) includes identification of transportation, stigma, discrimination and personal safety related barriers. However, to consider environmental, social and other contextual factors more seriously, other theories and perspectives are needed. For example, perspectives such as Occupational Justice (90) and the Capabilities Framework (91, 92) ground an understanding of what people can do and be in the structural and contextual conditions that support or restrict possibilities for doing, and thereby could locate time use scholarship and practice in the realm of social justice.
4.3 Limitations
This scoping review focused on applications of a time use perspective in community mental health practice involving people with severe mental illness. Hence, the reviewed time use measures and interventions may not be applicable to other populations or in inpatient settings. Since the time use studies of people with mood or anxiety disorders and/or high prevalence mental illness were excluded from this scoping review, these warrant further exploration (93). Most reviewed studies were conducted in North America, Europe or Australia, so that the findings may not be generalizable to other cultural or geographical contexts. The heterogeneity of study methodologies, limited longitudinal data and flexibility of intervention formats and delivery were barriers to consolidating this evidence and commenting on the sustained impact of interventions. Inclusion of stakeholder consultation is recommended to enhance methodological rigor (32). While this scoping review was informed by a team with perspectives as researchers, educators and mental health clinicians, consultation with other stakeholders, such as people with severe mental illness or peer workers in mental health services may have enhanced synthesis of this research.
5 Conclusions
This scoping review described practice applications of a time use perspective in community mental health practice. It identified time use assessments that evaluate outcomes of importance to personal recovery and community inclusion; and time use interventions designed to address activity patterns associated with poor health and well-being. These approaches emphasize reflection, collaborative goal planning and supported activity engagement, and contribute to emerging evidence on interventions that support self-management and personal recovery. While most time use assessments and interventions originate in occupational therapy, other mental health disciplines have begun to measure time use as a means to evaluate psychosocial intervention outcomes. This is an important step in raising the profile of time use perspectives across the mental health field and integrating time use approaches into evidence informed practices within community mental health services.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
EF: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. ND: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. CH: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Conceptualization. CD: Writing – review & editing, Visualization, Validation, Formal analysis, Conceptualization. DH: Writing – review & editing, Writing – original draft, Visualization, Validation, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. LF: Writing – review & editing, Visualization, Validation, Methodology, Formal analysis, Conceptualization. TK: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We wish to thank Rachel Stefaniak, an occupational therapist with extensive experience in the mental health and community sectors who assisted with reviewing papers in the early stages of developing this scoping review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1461705/full#supplementary-material
References
1. Meyer A. The philosophy of occupation therapy. Reprinted from the Archives of Occupational Therapy, Volume 1, pp. 1-10, 1922. Am J Occup Ther. (1977) 31:639–42.
2. Davidson L, Rakfeldt J, Strauss J. The roots of the recovery movement in psychiatry: Lessons learned. Chicester, UK: John Wiley & Sons (2011).
3. Fossey E, Krupa T. Patterns of participation: Time use and occupational balance. In: Bruce MA, Borg B, Krupa T, Pitts D, Kirsh B, Fossey E, editors. Bruce and Borg's Psychosocial frames of reference: theories, models, and approaches for occupation-based practice, 4th ed. SLACK Incorporated, Thorofare (2015).
4. Bauman A, Bittman M, Gershuny J. A short history of time use research; implications for public health. BMC Public Health. (2019) 19:1–7. doi: 10.1186/s12889-019-6760-y
5. Barnes GM, Hoffman JH, Welte JW, Farrell MP, Dintcheff BA. Adolescents’ time use: Effects on substance use, delinquency and sexual activity. J Youth Adolescence. (2007) 36:697–710. doi: 10.1007/s10964-006-9075-0
6. Pulver A, Davison C, Pickett W. Time-use patterns and the recreational use of prescription medications among rural and small town youth. J Rural Health. (2015) 31:217–28. doi: 10.1111/jrh.12103
7. Offer S, Schneider B. Revisiting the gender gap in time-use patterns: Multitasking and well-being among mothers and fathers in dual-earner families. Am Sociol Rev. (2011) 76:809–33. doi: 10.1177/0003122411425170
8. Scanlan JN, Bundy AC, Matthews LR. Promoting wellbeing in young unemployed adults: The importance of identifying meaningful patterns of time use. Aust Occup Ther J. (2011) 58:111–9. doi: 10.1111/j.1440-1630.2010.00879.x
9. Sprod J, Olds T, Brown W, Burton N, van Uffelen J, Ferrar K, et al. Changes in use of time across retirement: A longitudinal study. Maturitas. (2017) 100:70–6. doi: 10.1016/j.maturitas.2017.02.018
10. Stanley M, Richard A, Williams S. Older peoples’ perspectives on time spent alone. Aust Occup Ther J. (2017) 64:235–42. doi: 10.1111/1440-1630.12353
11. Olds T, Burton NW, Sprod J, Maher C, Ferrar K, Brown WJ, et al. One day you'll wake up and won't have to go to work: the impact of changes in time use on mental health following retirement. PloS One. (2018) 13:e0199605. doi: 10.1371/journal.pone.0199605
12. Foong HF, Lim SY, Koris R, Haron SA. Time-use and mental health in older adults: A scoping review. Int J Environ Res Public Health. (2021) 18:4459. doi: 10.3390/ijerph18094459
13. Eklund M, Leufstadius C, Bejerholm U. Time use among people with psychiatric disabilities: implications for practice. Psychiatr Rehabil J. (2009) 32:177–91. doi: 10.2975/32.3.2009.177.191
14. Eklund M, Orban K, Argentzell E, Bejerholm U, Tjornstrand C, Erlandsson LK, et al. The linkage between patterns of daily occupations and occupational balance: Applications within occupational science and occupational therapy practice. Scandinavian J Occup Ther. (2017) 24:41–56. doi: 10.1080/11038128.2016.1224271
15. Pagán R. Time allocation of disabled individuals. Soc Sci Med. (2013) 84:80–93. doi: 10.1016/j.socscimed.2013.02.014
16. Hunt E, McKay EA. A scoping review of time-use research in occupational therapy and occupational science. Scandinavian J Occup Ther. (2015) 22:1–12. doi: 10.3109/11038128.2014.934918
17. Krupa T, McLean H, Eastabrook S, Bonham A, Baksh L. Daily time use as a measure of community adjustment for persons served by assertive community treatment teams. Am J Occup Ther. (2003) 57:558–65. doi: 10.5014/ajot.57.5.558
18. Pongsaksri M. Time use for occupation and the expectations of people with schizophrenia and their relatives from the perspective of themselves and their relatives. Asian J Occup Ther. (2018) 14:1–7. doi: 10.11596/asiajot.14.1
19. Hoshino A, Asakura T, Cho K, Murata N, Kogata T, Kawamura M, et al. Preliminary study of time estimation of daily activities in patients with chronic schizophrenia by questionnaire survey. Br J Occup Ther. (2020) 83:752–60. doi: 10.1177/0308022620922420
20. Zarbo C, Zamparini M, Killaspy H, Baldini V, Patrono A, Malvezzi M, et al. Daily time use among individuals with schizophrenia spectrum disorders and unaffected controls: Results from the DiAPAson multicentric project. Psychiatr Rehabil J. (2023) 46:322–34. doi: 10.1037/prj0000576
21. Eklund M, Brunt D. Measuring opportunities for engaging in meaningful home-based activities in housing services for people with psychiatric disabilities: Development of the perceived meaning of activity in housing (PMA-H). Eval Health professions. (2019) 42:131–47. doi: 10.1177/0163278717727333
22. Nordaunet Ole M. How meaningful activities influence the recovery process. Adv Dual Diagn. (2018) 11:114–25. doi: 10.1108/ADD-01-2018-0002
23. Davidson L, Shaw J, Welborn S, Mahon B, Sirota M, Gilbo P, et al. I don't know how to find my way in the world": contributions of user-led research to transforming mental health practice. Psychiatry. (2010) 73:101–13. doi: 10.1521/psyc.2010.73.2.101
24. Doroud N, Fossey E, Fortune T. Recovery as an occupational journey: A scoping review exploring the links between occupational engagement and recovery for people with enduring mental health issues. Aust Occup Ther J. (2015) 62:378–92. doi: 10.1111/1440-1630.12238
25. Piat M, Seida K, Sabetti J. Understanding everyday life and mental health recovery through CHIME. Ment Health Soc Inclusion. (2017) 21:271–9. doi: 10.1108/MHSI-08-2017-0034
26. Waks S, Scanlan JN, Berry B, Schweizer R, Hancock N, Honey A. Outcomes identified and prioritised by consumers of Partners in Recovery: a consumer-led study. BMC Psychiatry. (2017) 17:338. doi: 10.1186/s12888-017-1498-5
27. Hitch D, Pepin G, Stagnitti K. Engagement in activities and occupations by people who have experienced psychosis: A metasynthesis of lived experience. Br J Occup Ther. (2013) 76:77–86. doi: 10.4276/030802213X13603244419194
28. Doroud N, Fossey E, Fortune T, Brophy L, Mountford L. A journey of living well: a participatory photovoice study exploring recovery and everyday activities with people experiencing mental illness. J Ment Health. (2022) 31:246–54. doi: 10.1080/09638237.2021.1952950
29. Harvey C, Zirnsak T-M, Brasier C, Ennals P, Fletcher J, Hamilton B, et al. Community-based models of care facilitating the recovery of people living with persistent and complex mental health needs: a systematic review and narrative synthesis. Front Psychiatry. (2023) 14:1259944. doi: 10.3389/fpsyt.2023.1259944
30. Tricco AC, Lillie E, Zarin W, O’brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Method. (2016) 16:1–10. doi: 10.1186/s12874-016-0116-4
31. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. (2005) 8:19–32. doi: 10.1080/1364557032000119616
32. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
33. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Internal Med. (2018) 169:467–73. doi: 10.7326/M18-0850
34. Booth A. Clear and present questions: formulating questions for evidence based practice. Libr. Hi Tech (2006) 24(3):355–368. doi: 10.1108/07378830610692127
35. Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed.) (2021) 372:n71. doi: 10.1136/bmj.n71
36. Bejerholm U, Hansson L, Eklund M. Profiles of occupational engagement in people with schizophrenia (POES): the development of a new instrument based on time-use diaries. Br J Occup Ther. (2006) 69:58–68. doi: 10.1177/030802260606900203
37. Bejerholm U, Eklund M. Construct validity of a newly developed instrument: Profile of Occupational Engagement in people with Schizophrenia, POES. Nordic J Psychiatry. (2006) 60:200–6. doi: 10.1080/08039480600636239
38. Bejerholm U, Lundgren-Nilsson Å. Rasch Analysis of the Profiles of Occupational Engagement in people with Severe mental illness (POES) instrument. Health Qual Life Outcomes. (2015) 13:1–8. doi: 10.1186/s12955-015-0327-0
39. Jolley S, Garety PA, Ellett L, Kuipers E, Freeman D, Bebbington PE, et al. A validation of a new measure of activity in psychosis. Schizophr Res. (2006) 85:288–95. doi: 10.1016/j.schres.2006.03.012
40. Larivière N, Aubin G, Pépin M-È, Maurice V, Lavertu F, Tardif C, et al. French version of the profiles of occupational engagement in people with severe mental illness: Translation, adaptation, and validation. Int J Ment Health. (2017) 46:346–57. doi: 10.1080/00207411.2017.1368308
41. Zarbo C, Agosta S, Casiraghi L, De Novellis A, Leuci E, Paulillo G, et al. Assessing adherence to and usability of Experience Sampling Method (ESM) and actigraph in patients with Schizophrenia Spectrum Disorder: A mixed-method study. Psychiatry Res. (2022) 314:114675. doi: 10.1016/j.psychres.2022.114675
42. Zarbo C, Zamparini M, Nielssen O, Casiraghi L, Rocchetti M, Starace F, et al. Comparing adherence to the experience sampling method among patients with schizophrenia spectrum disorder and unaffected individuals: observational study from the multicentric diAPAson project. J Med Internet Res. (2023) 25:e42093. doi: 10.2196/42093
43. Bejerholm U, Eklund M. Time use and occupational performance among persons with schizophrenia. Occup Ther Ment Health. (2004) 20:27–47. doi: 10.1300/J004v20n01_02
44. Bejerholm U, Eklund M. Engagement in occupations among men and women with schizophrenia. Occup Ther Int. (2006) 13:100–21. doi: 10.1002/oti.210
45. Areberg C, Bejerholm U. The effect of IPS on participants' engagement, quality of life, empowerment, and motivation: a randomized controlled trial. Scandinavian J Occup Ther. (2013) 20:420–8. doi: 10.3109/11038128.2013.765911
46. Argentzell E, Bäckström M, Lund K, Eklund M. Exploring mediators of the recovery process over time among mental health service users, using a mixed model regression analysis based on cluster RCT data. BMC Psychiatry. (2020) 20:520. doi: 10.1186/s12888-020-02924-2
47. Eklund M, Tjörnstrand C, Sandlund M, Argentzell E. Effectiveness of Balancing Everyday Life (BEL) versus standard occupational therapy for activity engagement and functioning among people with mental illness – a cluster RCT study. BMC Psychiatry. (2017) 17:363. doi: 10.1186/s12888-017-1524-7
48. Bejerholm U, Areberg C, Hofgren C, Sandlund M, Rinaldi M. Individual placement and support in Sweden—A randomized controlled trial. Nordic J Psychiatry. (2015) 69:57–66. doi: 10.3109/08039488.2014.929739
49. Cardoso G, Papoila A, Tomé G, Killaspy H, King M, Caldas-de-Almeida J, et al. A cluster randomised controlled trial of a staff-training intervention in residential units for people with long-term mental illness in Portugal: the PromQual trial. Soc Psychiatry Psychiatr Epidemiol. (2017) 52:1435–45. doi: 10.1007/s00127-017-1416-7
50. Cella M, Edwards C, Swan S, Elliot K, Reeder C, Wykes T. Exploring the effects of cognitive remediation on metacognition in people with schizophrenia. J Exp Psychopathol. (2019) 10. doi: 10.1177/2043808719826846
51. Eklund M, Argentzell E, Bejerholm U, Brunt D, Tjörnstrand C. Outcomes of the Active in My Home (AiMH) intervention for people with psychiatric disabilities in supported housing: A longitudinal pilot and feasibility study. Br J Occup Ther. (2020) 83:6–14. doi: 10.1177/0308022619888872
52. Fowler D, Hodgekins J, Painter M, Reilly T, Crane C, Macmillan I, et al. Cognitive behaviour therapy for improving social recovery in psychosis: A report from the ISREP MRC trial platform study (Improving Social Recovery in Early Psychosis). psychol Med. (2009) 39:1627–36. doi: 10.1017/S0033291709005467
53. Fowler D, Hodgekins J, French P, Marshall M, Freemantle N, McCrone P, et al. Social recovery therapy in combination with early intervention services for enhancement of social recovery in patients with first-episode psychosis (SUPEREDEN3): A single-blind, randomised controlled trial. Lancet Psychiatry. (2018) 5:41–50. doi: 10.1016/s2215-0366(17)30476-5
54. Fowler D, Berry C, Hodgekins J, Banerjee R, Barton G, Byrne R, et al. Social recovery therapy for young people with emerging severe mental illness: the Prodigy RCT. Health Technol Assess. (2021) 25:1. doi: 10.3310/hta25700
55. Inman J, Bannigan K, Akhurst J. Occupational therapy and psychosis: POINTER feasibility study for a pragmatic clinical trial. Br J Occup Ther. (2021) 84:541–9. doi: 10.1177/03080226211000257
56. Priebe S, Chevalier A, Hamborg T, Golden E, King M, Pistrang N. Effectiveness of a volunteer befriending programme for patients with schizophrenia: randomised controlled trial. Br J Psychiatry. (2020) 217:477–83. doi: 10.1192/bjp.2019.42
57. Bjorkedal STB, Bejerholm U, Hjorthoj C, Moller T, Eplov LF. Meaningful Activities and Recovery (MA&R): a co-led peer occupational therapy intervention for people with psychiatric disabilities. Results from a randomized controlled trial. BMC Psychiatry. (2023) 23:406. doi: 10.1186/s12888-023-04875-w
59. Neil ST, Kilbride M, Pitt L, Nothard S, Welford M, Sellwood W, et al. The questionnaire about the process of recovery (QPR): a measurement tool developed in collaboration with service users. Psychosis. (2009) 1:145–55. doi: 10.1080/17522430902913450
60. Law H, Neil ST, Dunn G, Morrison AP. Psychometric properties of the Questionnaire about the Process of Recovery (QPR). Schizophr Res. (2014) 156:184–9. doi: 10.1016/j.schres.2014.04.011
61. Eklund M, Bäckström M, Eakman AM. Psychometric properties and factor structure of the 13-item satisfaction with daily occupations scale when used with people with mental health problems. Health Qual Life outcomes. (2014) 12:1–9. doi: 10.1186/s12955-014-0191-3
62. Krupa T. Action over inertia: addressing the activity-health needs of individuals with serious mental illness. Ottawa: CAOT Publications ACE (2010).
63. Krupa T, Edgelow M, Chen S-P, Mieras C. Promoting Activity and Participation in Individuals with Serious Mental Illness: The Action over Inertia Approach. New York: Taylor & Francis Group (2022).
64. Hitch D, Vernon L, Collins R, Dun C, Palexas S, Lhuede K. ). The pathways to participation (P2P) program: A pilot outcomes study. Int J Environ Res Public Health. (2022) 19:6088. doi: 10.3390/ijerph19106088
65. Edgelow M, Krupa T. Randomized controlled pilot study of an occupational time-use intervention for people with serious mental illness. Am J Occup Ther. (2011) 65:267–76. doi: 10.5014/ajot.2011.001313
66. Eklund M, Lund K, Argentzell E. The impact of the BEL intervention on levels of motivation, engagement and recovery in people who attend community mental health services. Scandinavian J Occup Ther. (2023) 30:862–72. doi: 10.1080/11038128.2023.2184717
67. Bramley S, Mayne N. The WORKS A resource to support you in achieving your employment ambitions. Sheffield, UK: Sheffield Health and Social Care NHS Foundation Trust (2010).
68. Hultqvist J, Lund K, Argentzell E, Eklund M. Predictors of clinically important improvements in occupational and quality of life outcomes among mental health service users after completion and follow-up of a lifestyle intervention: Multiple regression modelling based on longitudinal data. BMC Psychol. (2019) 7:83. doi: 10.1186/s40359-019-0359-z
69. Lund K, Argentzell E, Bejerholm U, Eklund M. Breaking a cycle of perceived failure: The process of making changes toward a more balanced lifestyle. Aust Occup Ther J. (2019) 66:627–36. doi: 10.1111/1440-1630.12604
70. Lund K, Argentzell E, Leufstadius C, Tjörnstrand C, Eklund M. Joining, belonging, and re-valuing: A process of meaning-making through group participation in a mental health lifestyle intervention. Scandinavian J Occup Ther. (2019) 26:55–68. doi: 10.1080/11038128.2017.1409266
71. Lund K, Hultqvist J, Bejerholm U, Argentzell E, Eklund M. Group leader and participant perceptions of Balancing Everyday Life, a group-based lifestyle intervention for mental health service users. Scandinavian J Occup Ther. (2020) 27:462–73. doi: 10.1080/11038128.2018.1551419
72. Rees EF, Ennals P, Fossey E. Implementing an action over inertia group program in community residential rehabilitation services: group participant and facilitator perspectives. Front Psychiatry. (2021) 12:624803. doi: 10.3389/fpsyt.2021.624803
73. Aas D. Studies of time-use: problems and prospects. Acta Sociol. (1978) 21:125–41. doi: 10.1177/000169937802100203
74. Farnworth L. Time use, tempo and temporality: Occupational therapy's core business or someone else's business. Aust Occup Ther J. (2003) 50:116–26. doi: 10.1046/j.1440-1630.2003.00391.x
75. Lean M, Fornells-Ambrojo M, Milton A, Lloyd-Evans B, Harrison-Stewart B, Yesufu-Udechuku A, et al. Self-management interventions for people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. (2019) 214:260–8. doi: 10.1192/bjp.2019.54
76. Jameel L, Valmaggia L, Barnes G, Cella M. mHealth technology to assess, monitor and treat daily functioning difficulties in people with severe mental illness: A systematic review. J Psychiatr Res. (2022) 145:35–49. doi: 10.1016/j.jpsychires.2021.11.033
77. Cruz-Jesus F, Oliveira T, Bacao F. The global digital divide: evidence and drivers. J Global Inf Manage. (2018) 26:1–26. doi: 10.4018/JGIM.2018040101
78. D’Amico ML, Jaffe LE, Gardner JA. Evidence for interventions to improve and maintain occupational performance and participation for people with serious mental illness: A systematic review. Am J Occup Ther. (2018) 72:7205190020p1–7205190020p11. doi: 10.5014/ajot.2018.033332
79. Kirsh B, Martin L, Hultqvist J, Eklund M. Occupational therapy interventions in mental health: A literature review in search of evidence. Occup Ther Ment Health. (2019) 35:109–56. doi: 10.1080/0164212X.2019.1588832
80. Winsper C, Crawford-Docherty A, Weich S, Fenton S-J, Singh SP. How do recovery-oriented interventions contribute to personal mental health recovery? A systematic review and logic model. Clin Psychol Rev. (2020) 76:101815. doi: 10.1016/j.cpr.2020.101815
81. Stewart V, McMillan SS, Hu J, Ng R, El-Den S, O’Reilly C, et al. Goal planning in mental health service delivery: A systematic integrative review. Front Psychiatry. (2022) 13:1057915. doi: 10.3389/fpsyt.2022.1057915
82. Killaspy H, Harvey C, Brasier C, Brophy L, Ennals P, Fletcher J, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry. (2022) 21:96–123. doi: 10.1002/wps.20940
83. Moll SE, Gewurtz RE, Krupa TM, Law MC, Lariviere N, Levasseur M. Do-Live-Well”: A Canadian framework for promoting occupation, health, and well-being: «Vivez-Bien-Votre Vie»: un cadre de référence canadien pour promouvoir l’occupation, la santé et le bien-être. Can J Occup Ther. (2015) 82:9–23. doi: 10.1177/0008417414545981
84. Gewurtz RE, Moll SE, Letts LJ, Larivière N, Levasseur M, Krupa TM. What you do every day matters: A new direction for health promotion. Can J Public Health. (2016) 107:e205–8. doi: 10.17269/cjph.107.5317
85. Hamilton KA, Letts LJ, Larivière N, Moll SE. Revisiting the do-live-well health promotion framework: A citation content analysis. Can J Occup Ther. (2023) 90:297–302. doi: 10.1177/00084174221149268
86. World Health Organization. ICF: International Classification of Functioning, Disability and Health. Geneva. (2001).
87. Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. (2011) 199:445–52. doi: 10.1192/bjp.bp.110.083733
88. Drake RE, Whitley R. Recovery and severe mental illness: description and analysis. Can J Psychiatry. (2014) 59:236–42. doi: 10.1177/070674371405900502
89. Carr ER. A history of the community mental health movement and individuals with serious mental illness: A vision for the future. . Am J Orthopsych. (2024) 94:380–91. doi: 10.1037/ort0000737
90. Townsend EA. Boundaries and bridges to adult mental health: Critical occupational and capabilities perspectives of justice. J Occup Sci. (2012) 19:8–24. doi: 10.1080/14427591.2011.639723
91. Sen A. Human rights and capabilities. J Hum Dev. (2005) 6:151–66. doi: 10.1080/14649880500120491
92. Nussbaum MC. Creating capabilities: The human development approach. Cambridge, Massachusetts: Harvard University Press (2011).
Keywords: time use, participation, recovery, occupational therapy, mental illness
Citation: Fossey E, Doroud N, Harvey CA, Dun C, Hitch D, Farnworth L and Krupa T (2024) Contributions of a time use perspective in community mental health practice: a scoping review. Front. Psychiatry 15:1461705. doi: 10.3389/fpsyt.2024.1461705
Received: 09 July 2024; Accepted: 04 September 2024;
Published: 11 October 2024.
Edited by:
Bhing-Leet Tan, Singapore Institute of Technology, SingaporeReviewed by:
Elizabeth McKay, Edinburgh Napier University, United KingdomAiko Hoshino, Nagoya University, Japan
Copyright © 2024 Fossey, Doroud, Harvey, Dun, Hitch, Farnworth and Krupa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ellie Fossey, ZWxsaWUuZm9zc2V5QG1vbmFzaC5lZHU=
 Ellie Fossey
Ellie Fossey Nastaran Doroud
Nastaran Doroud Carol Ann Harvey
Carol Ann Harvey Carolyn Dun4
Carolyn Dun4 Danielle Hitch
Danielle Hitch Terry Krupa
Terry Krupa