- 1Forensic Psychiatry Division, The Centre for Addiction and Mental Health, Toronto, ON, Canada
- 2Department of Psychiatry, University of Toronto, Toronto, ON, Canada
- 3General and Health Systems Psychiatry Division, Centre for Addiction and Mental Health, Toronto, ON, Canada
Introduction/Background: Aggression and violence are common problems in healthcare settings and affects both patients and healthcare staff. The Dynamic Appraisal of Situational Aggression (DASA) is an assessment tool to guide assessment for short term risk in inpatient settings. There have been no large-scale studies examining the performance of the DASA across different clinical settings. Our objective is to examine the performance of the DASA using a large longitudinal patient sample on different clinical units. A secondary objective was to examine alterative risk categories of the DASA.
Methods: All consecutive mental health hospital admissions to a large hospital in Toronto, Canada between 2016 and 2019 were included. Time-to-event analysis and Receiver Operating Characteristics Area Under the Curve (AUC) was conducted with the outcome variable being the occurrence of the first violent incident or first restraint event.
Results: We included 3819 patients, of which 17% had at least one violent incident. We analysed 88,124 DASA scores and found a significant association with violence (HR 1.79 (95% CI), AUC 0.73). We found that the AUCs were similar for subspecialized forensic, schizophrenia and acute care units (0.71, 0.73 and 0.75 respectively), and lower for geriatric units (0.66). We propose new violence risk categories based on the frequency of violence at each score.
Discussion: Higher DASA scores are associated with higher risk of violent incidents in both forensic and non-forensic inpatient psychiatric units. The proposed violence risk groups help rule out patients at low risk of violence and may help identify patients who would most benefit from interventions to reduce violence.
Introduction
Violence in healthcare settings is a widespread problem which affects both patients and staff and costs an estimated 12.7 billion dollars annually in legal and healthcare costs in Canada alone (1). Over 60% of nurses in Canada reported violence in the workplace during the previous year (2), and as many as 70% of mental health staff report having been physically assaulted within the last 12 months (3). In acute psychiatric settings, around 20% of patients engage in violent behavior (4) and in forensic settings, as many as 30% to 40% of patients commit at least one act of violence within a one-year period (5).
Efforts to reduce violence include staff training (6), organizational policy and safety procedures and environmental design (7). Structured risk assessments can be used by clinicians to identify those at high risk for violence so that appropriate steps can be taken. Several risk assessment tools such as the Historical Clinical Risk Management tool (HCR-20) (8) and the Short-Term Assessment of Risk and Treatability tool (START) (9) have been shown to have good predictive validity. However, these tools are not ideally suited for inpatient settings, for the purpose of short-term monitoring of violence risk over the next hours to days (10).
Several short-term dynamic risk assessments have been developed to predict violence within a 24-hour window (11, 12), one of which is the Dynamic Appraisal of Situational Aggression (DASA). The DASA was originally developed in a secure forensic hospital in Melbourne, Australia. The DASA is a 7-item risk assessment tool that has been developed to assess short-term risk in adult forensic inpatient settings. The presence or absence of each of the seven items within the past 24-hours are totaled to give a score between zero and seven (13). Total DASA scores more accurately predict violence in multiple settings, as compared to unstructured clinical assessments (14–18), including among youth (19, 20), female forensic inpatients (21) and in the emergency department (22). More recently, Dickens and colleagues carried out a systematic review and meta-analysis of tools to assess imminent aggression, which included 14 patient samples that employed the DASA. The overall effect size (Hedge’s g coefficient) for prediction of interpersonal aggression and for any aggression was 1.04 [0.69, 1.39] and 0.88 [0.62, 1.15], respectively (23). To improve the utility of DASA, some efforts have been undertaken to optimize the way in which the score is analysed. One study showed that averaging the DASA score over a period of three days improved its predictive validity (24). A similar study by Chu and colleagues showed that averaging the DASA score may improve predictive validity (22).
Some studies have categorized the risk of violence into “low”, “medium” and “high” risk categories depending on the total DASA score. These categories can have practical value for clinical staff, who can mitigate risk by linking a clinical intervention to a risk severity category (25). This may have utility in resource prioritization and clinical interventions but there has been little investigation of the predictive validity of such categorization. However, there have been no studies that we are aware of that have directly compared the validity of the original risk categories in other settings. Examining different inpatient units would help determine the generalizability of the DASA across clinical settings – making the DASA a more universal tool for predicting short term risk of violence. Moreover, no studies have investigated alternative cut-offs for the risk categories. One limitation in the DASA tool has been the high sensitivity and low specificity of the original DASA cut-offs. We hypothesize that different clinical settings may benefit from different cut-off scores. For example, a chronic, long-term, psychiatric unit, with rare violent incidents, may wish to adjust the cut-off score to maximize specificity and minimize the number of false positives. Investigating different cut-offs, may help clinicians in determining the optimal use of the DASA for their clinical setting.
To date, there have been no large longitudinal studies that investigated the validity of DASA in predicting violent incidents during the first few weeks of a hospital admission. The largest sample to date included 1548 patients assessed within an emergency department in a single 24-hour period (22). Moreover, there have been no studies that compared validity across specialized and general psychiatric units in both forensic and non-forensic settings. We have therefore carried out a study to investigate the predictive validity of DASA among all newly admitted adult patients in a large mental health facility comprising acute, long-stay, elderly and forensic services. Our study aims are as follows: (1) to investigate the predictive validity of the DASA among new admissions in different populations; and (2) to investigate the predictive validity of alternative cut-off scores for risk categories.
Methods
Setting
We carried out this study at The Centre for Addiction and Mental Health (CAMH) in Toronto, Ontario, Canada’s largest mental health teaching hospital. The hospital has multiple units including acute care, forensic, geriatric and chronic schizophrenia programs. This study was carried out independently of the authors of the DASA.
Patient population
We included all patients aged 18 years and over admitted to CAMH from 2016 to 2019. For those admitted more than once during that time, we included only the first admission. We excluded patients held only in the emergency department and those admitted for less than 24-hours. We also excluded those in which a violent incident occurred on the first day of admission (prior to a DASA being scored) because of the need to record DASA scores prior to a violent incident occurring and those with two or more consecutive missing DASA scores.
Measures
The DASA comprises seven items that are recorded daily for every patient by nursing staff using observational and chart data from the last 24 hours. DASA produces a maximum score of 7 with each item scoring either a 0-1 (13). Violence risk was first classified as Low, Moderate, or High based on the standard cut off scores 0-1 , 2-3 and 4-7 respectively. Based on our preliminary investigation of predictive validity at alternative cut-off scores, we defined a “high specificity” categorization as Low (0-3), Medium (4-5) and high (6-7).
The outcome measure is the occurrence of the first violent incident following admission, which is defined as verbal or physical aggression towards a person or property. This definition is consistent with previous studies examining the validity of DASA (17, 18). Outcome measure data were collected from the electronic medical record (EMR) by identifying violent incidents reported in a SCORE report (Staff and Client On-line Reporting of Events- the hospital’s incident reporting system) or by the use of incidents of seclusion, mechanical restraint or chemical restraint where the documented reason was harm to others. It is hospital policy for all violent events to be recorded in the SCORE system. The use of seclusion or restraint events was to capture any violent outcome events that were not captured in SCORE.
Clinical and demographic data
We collected clinical and demographic data including age, sex, DSM-5 diagnosis (26), legal status (voluntary, involuntary or informal) and unit type, categorized as adult acute care, geriatric, forensic and chronic schizophrenia units.
Procedure and statistical analysis
The follow-up period for each patient was a maximum of 60 days, until discharge from hospital, or the first outcome incident, whichever came first. We restricted the analysis window to 60 days from the day of admission, adopting the methods used in a previous study (14), and because of the very low incidence of violence beyond this time.
Statistical analysis was conducted using the SAS Enterprise Guide version 7.1 software. The cohort was described by summarizing demographic data, DASA scores and the outcome measure using percentages and means where appropriate. The association between DASA score and outcome over a subsequent 24-hour period was measured.
Patients had DASA scores recorded daily, and therefore each DASA score was used as the predictor for violence in each subsequent 24-hour period. We used Cox proportional hazard regression, using DASA scores and violence risk groups, as time-dependent variables to model association with violence. We calculated the area under the Curve (AUC) for each 24-hour period and report the average AUCs. A difficulty in measuring the predictive validity of a violence risk assessment instrument in clinical settings is that a high score on the risk instrument would likely prompt a clinical intervention by healthcare staff to mitigate this risk, and thereby reducing the apparent association between risk instrument scores and outcome. Unscheduled medication (often referred to as Pro re nata (PRN) medication) is often given on an “as needed” basis, in inpatient settings aimed at reducing agitation or aggression. We therefore also included administration of unscheduled antipsychotic or benzodiazepine medication in the 24 hours prior to the incident as a time-varying variable in our model, to control for the effects of this intervention in reducing violence. Other clinical interventions with nursing staff which may have been prompted by a high DASA scores were not measured and therefore could not be included in the model.
We first investigated the association between the Low, Medium and High risk categories using the original cut-off scores reported by the authors (13), then repeated that analysis using the alternative “high specificity” cut-off scores to assign new risk categories. We then carried out the analyses separately for patients in forensic, schizophrenia, acute and geriatric units to calculate hazard ratios and AUC for each.
Ethics statement
Research Ethical approval was granted by the Centre for Addictions and Mental Health Research Ethics Board (067/2020) for use of retrospective data for the purpose of research. No identifiable information was retained or is presented in this study.
Results
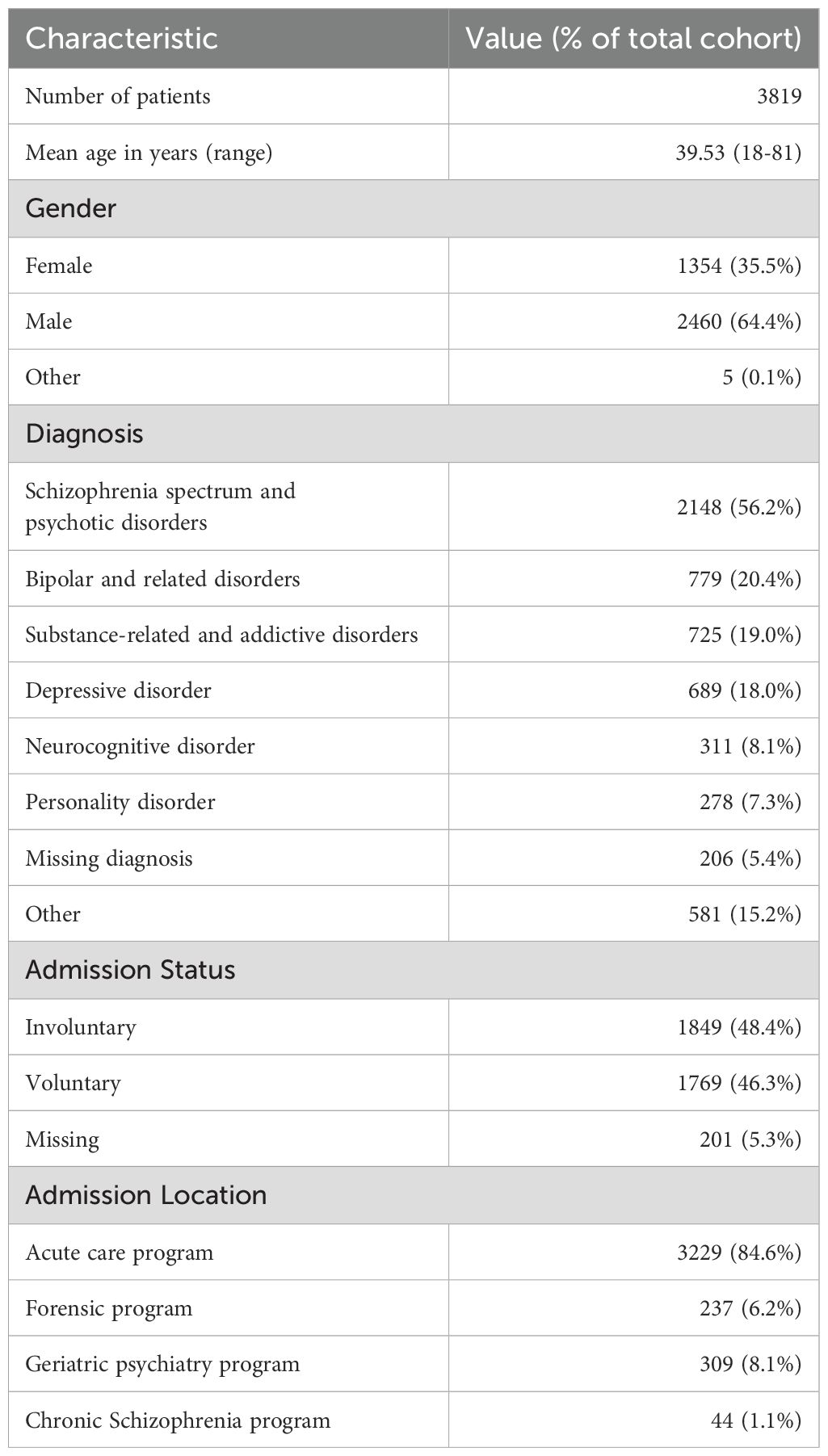
There were 4,320 admissions during the study period. We excluded 501 patients (213 patients had a length of stay in hospital of less than 1 day, 16 patients had a violent event prior to a DASA score being recorded and 272 patients had 2 or more consecutive DASA scores missing) leaving 3819 patients included in the study. There were 88,124 DASA scores recorded. Demographic data, diagnosis, admission status and admission location for the study population are summarized in Table 1. The mean age of the patients studied was 39.5 (range 16-81); approximately two thirds were male. Just over half of patients had a diagnosis of schizophrenia spectrum or psychotic disorder and approximately one fifth of patients had a diagnosis of either bipolar and related disorders, substance-related and addictive disorders and depressive disorders. Around half of the patients were involuntarily admitted with the remainder being voluntarily admitted. The majority (84.6%) were admitted to an acute care unit, 8.1% were admitted to the geriatric psychiatry program, 6.2% admitted to the forensic program and 1.1% to the chronic schizophrenia program.
The maximal DASA score reported during the study period is shown in Table 2. Almost one quarter of patients had a DASA score of zero through the period of observation, and 45% had a maximum score of 3 or more. Approximately 7-8% of patients had maximum scores of 5, 6 or 7. Table 3 summarizes the time to outcome event for the study cohort. There were 634 patients who carried out at least one violent incident, representing 16.6% of the study cohort. We found that 82% of all outcome events (519 incidents) occurred in the first two weeks following admission. We found that 59% of patients categorized with a high DASA score received a PRN medication, 39% with a medium score and 14% with a low score for aggression or agitation.
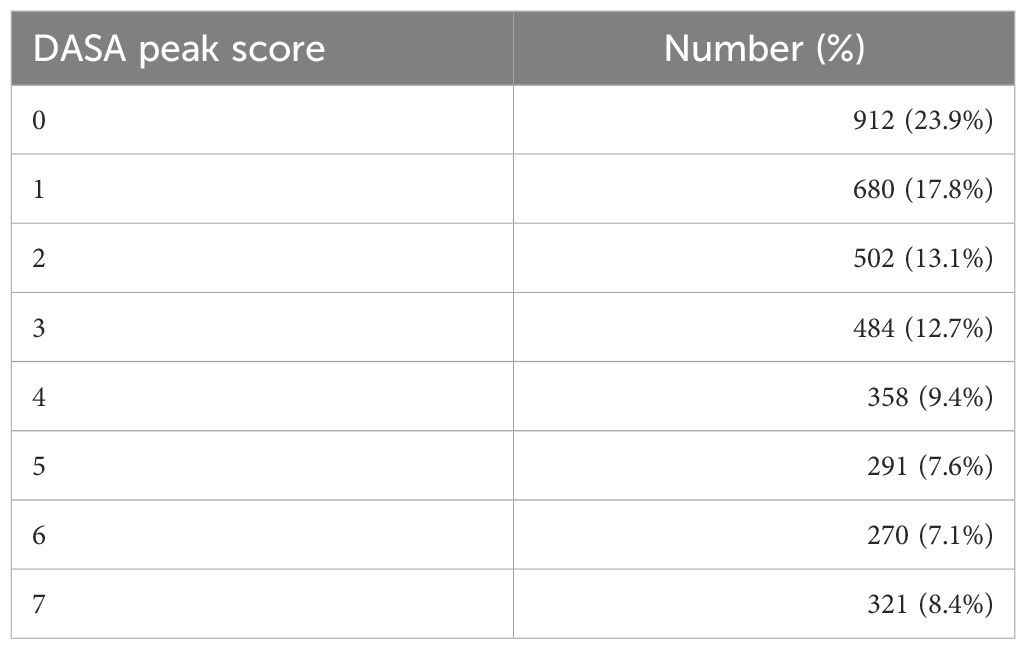
Table 2. Summary of number and percentage of patients for each DASA peak score within the follow-up period of 60 days and time to outcome event.
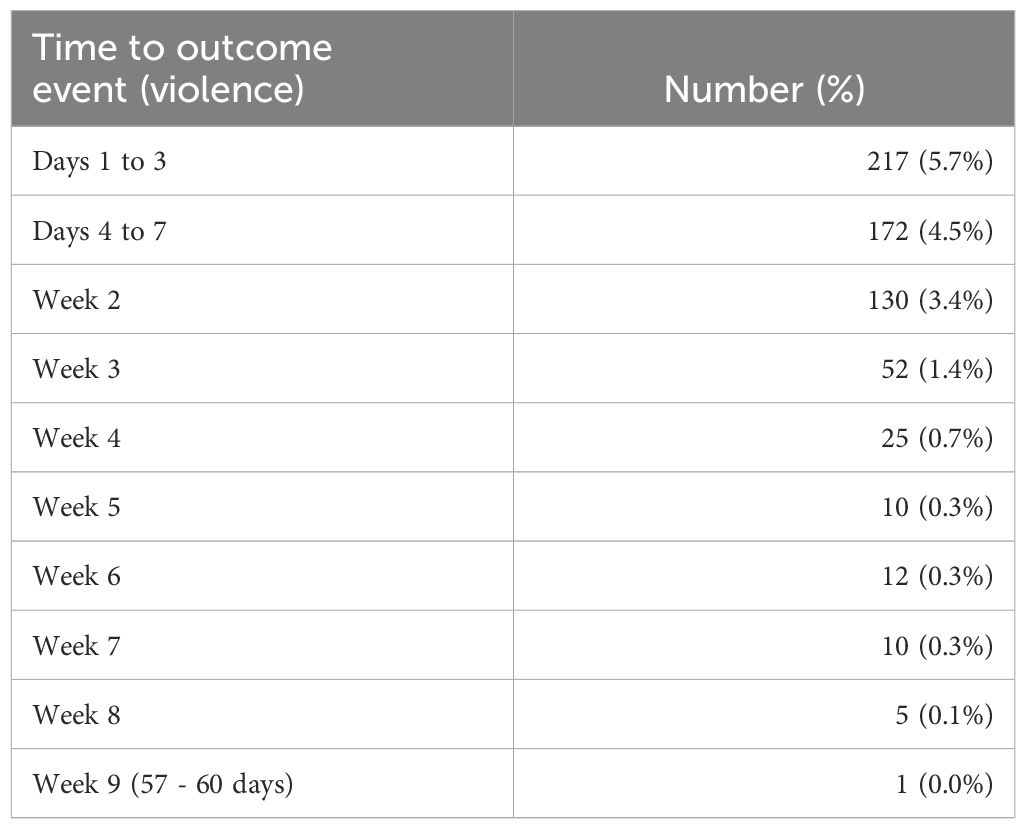
Table 3. Number and percentage of patients who were violent at each timeframe out of all patients per timeframe.
We found that DASA scores were significantly associated with violence overall (HR 1.79, CI 1.73-1.85 (per unit increase)). The overall AUC was 0.73. We investigated two alternative groupings of Low, Medium and High risk of violence with either high sensitivity or high specificity. The high sensitivity groupings are as follows: scores 0-1, 2-3 and 4-7 for Low, Moderate and High risk of violence. The high specificity grouping had the following categorization: scores of 0-3, 4-5 and 6-7 for Low, Moderate and High risk of violence. Both groupings were analysed using the Cox proportional hazard model (see Table 4). The high sensitivity grouping hazard ratio comparing medium and low risk groups was 5.38 (CI 4.38-6.61) and the hazard ratio comparing low to high-risk group was 18.98 (CI 15.69-22.97). For the high specificity groupings, the hazard ratios comparing medium and low risk groups was 8.4 (CI 6.87-10.28) and the hazard ratio comparing low to high-risk group was 20.3 (CI 16.41-25.12) (see Table 4).
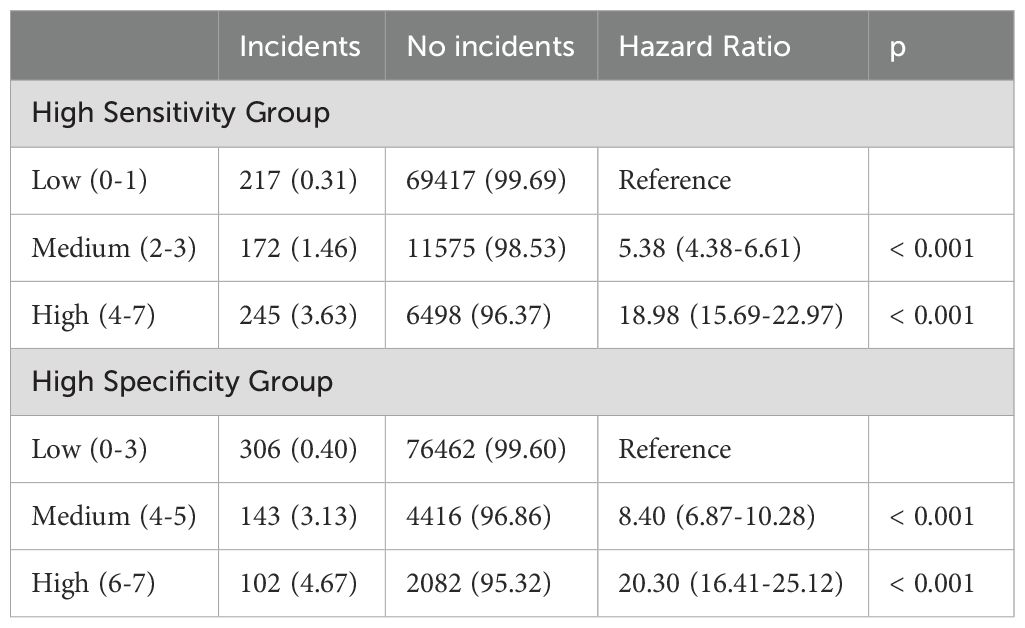
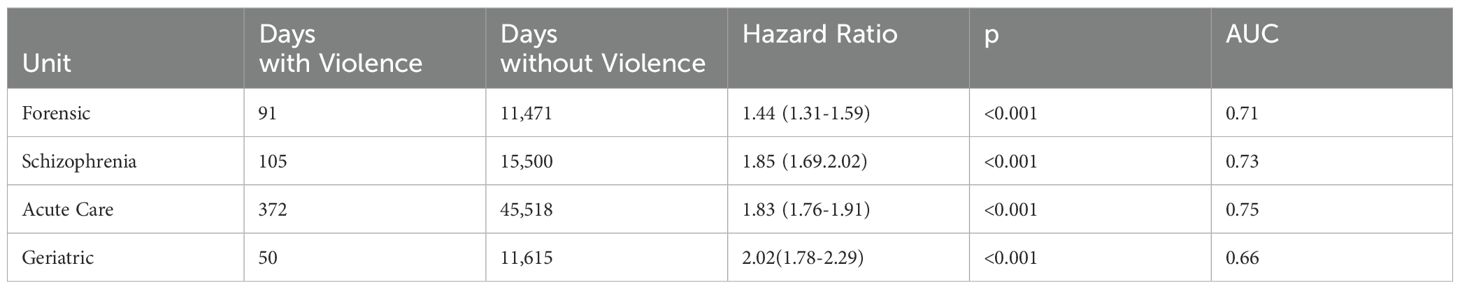
Table 4. Hazard ratios for either moderate or high violence risk categories for DASA across different inpatient psychiatric units.
Finally, we compared the performance of the DASA in predicting violent events between the different specialized units at CAMH (See Table 5). We found that the AUCs were similar for forensic, schizophrenia and acute care units (0.71, 0.73 and 0.75 respectively), and lower for geriatric units (0.66). We found that hazard ratios were similar across units with lowest on forensic units (HR 1.44, CI 1.31-1.59) and highest on geriatric units (HR 2.02, CI 1.78-2.29).
Discussion
In our study of 3819 patients admitted to a large mental health facility, we found that the DASA was a moderately good predictor of violent incidents overall. We also found that although the DASA performed well in all settings, the predictive accuracy was lower on geriatric units in comparison to acute, schizophrenia and forensic units, and we found that alternative risk categories to those originally defined may have better performance. This has clinical implications for aligning resources with predicted need in efforts to reduce violence on in-patient settings.
Our results are consistent with previous literature that has validated the DASA (13–15, 17, 18). Our study similarly found that higher DASA scores are significantly associated with higher likelihood of violence, and additionally found that this held across a diverse patient population.
The main objective of our study was to examine the validity of the DASA instrument in a large inpatient population across different units. The original DASA authors proposed risk categories that were compared to unit staff’s clinical judgement (13). We explored alternative cut-off scores for categorizing Low, Moderate and High risk groups that may have practical and clinical implications in healthcare settings.
We found that 82% of first violent incidents occur in the first two weeks of admission. Patients are likely more acutely ill at the start of their admission and are more likely to be involved in violent incidents. Patients that are at a low risk of violence based on the DASA score in these first two weeks are unlikely to have a violent incident during their admission. This finding, based on our high specificity risk categories, can allow psychiatric units to identify patients in need of more intensive risk management strategies and to intervene early in the course of an admission. Although there is a significant association between higher DASA scores and violence, the AUCs are moderate which are consistent with other tools that assess short term risk such as the Broset Violence Checklist (AUC = 0.69) (27). In our study, even the highest scores on the DASA resulted in a violent incident in only around 5% of occasions.
The DASA score has been incorporated into an aggression prevention protocol to better help staff manage risk of violence (28) and provide guidance around situations requiring staff intervention such as verbal de-escalation or pharmacotherapy (29). Given limited healthcare resources and low proportion of violent incidents, a strategy directing resources to high-risk individuals is ideal, where the need is greatest (30). We selected violence risk categories that result in high specificity to identify more individuals that are of low risk of violence where fewer resources are needed. This comparison was ideally suited for our large sample size where we were able to ensure DASA remains valid across multiple violence risk categories and across multiple inpatient units.
Overall there was little difference in the performance of the DASA across different units, however the predictive accuracy was slightly lower on geriatric units. The majority of the patients on geriatic units had neurocognitive disorders, and therefore the items of the DASA may not be as relevant in predicting aggression compared with those on other units, where the primary diagnoses are psychotic illnesses.
A major strength of our study is the large sample, gathering an almost complete cohort of new admissions over a two-year period, which to our knowledge is the largest study analyzing the DASA to date. This allowed our study to investigate the performance of the DASA across multiple specialized inpatient units in both forensic and non-forensic settings making our findings applicable across a broad setting. We were also able to offer clinical implications while analyzing different violence risk categories.
There are however a number of limitations of our study. First, our study only included the first violent incident, and therefore our findings may not apply to the predictive validity of DASA score in the context of repeat violent incidents during a single admission. This does however eliminate previous violent incidents as a confounder which has been shown to be a significant variable in predicting violence (31). Second, we did not have any data to assess clinical interventions that may be differentially applied to those identified as high risk, other than PRN medication administration. The association between higher DASA scores and violence is therefore underestimated due to likely clinical interventions to mitigate risk of violence that are not captured by our study. Third, our study is retrospective, and it is difficult to control for all potential biases in our cohort, such as the reliability of DASA scores recorded by all staff.
For future research it will be important to address the question of whether our findings can guide intervention for violence prevention and how this may impact the incidence of violence in the inpatient setting. It also remains unclear how a violent incident during an admission changes the validity of the DASA. Multiple risk factors that correlate with risk of violence have been identified in previous literature (4, 31, 32) but it remains unknown whether a comprehensive model that includes clinical data, risk factors and the DASA may improve violence prediction.
Conclusions
Our large-scale longitudinal patient dataset confirmed that the DASA has moderate predictive validity for predicting risk of violence in inpatient units. The DASA is valid across both forensic and non-forensic units, though further work is needed to establish the utility on geriatric units. We have proposed new violence risk categories for low, moderate, and high risk of violence, which may help improve the clinical utility of the DASA score in directing intervention to those most at risk. Our study also found that patients who are consistently at low risk of violence based on the DASA score, for the first two weeks of admission, are likely to remain at a low risk and unlikely to be involved in a violent incident. Further research is needed to look at how DASA can guide interventions and whether combining risk factors and clinical data with the DASA score improves its predictive power.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Centre for Addictions and Mental Health Research Ethics Board (067/2020). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because retrospective deidentified data was analyzed.
Author contributions
MM: Writing – original draft, Writing – review & editing. FF: Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing. LV: Formal analysis, Methodology, Writing – review & editing. AS: Writing – review & editing. PK: Conceptualization, Methodology, Writing – review & editing. RJ: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hoddenbagh J, McDonald SE, Zhang T. An estimation of the Economic Impact of Violent Victimization in Canada, 2009: Research and Statistics Division. Department of Justice Canada (2014) 2014.
3. Kelly EL, Subica AM, Fulginiti A, Brekke JS, Novaco RW. A cross-sectional survey of factors related to inpatient assault of staff in a forensic psychiatric hospital. J Adv Nurs. (2015) 71:1110–22. doi: 10.1111/jan.2015.71.issue-5
4. Iozzino L, Ferrari C, Large M, Nielssen O, de Girolamo G. Prevalence and risk factors of violence by psychiatric acute inpatients: A systematic review and meta-analysis. PloS One. (2015) 10:e0128536. doi: 10.1371/journal.pone.0128536
5. Broderick C, Azizian A, Kornbluh R, Warburton K. Prevalence of physical violence in a forensic psychiatric hospital system during 2011-2013: Patient assaults, staff assaults, and repeatedly violent patients. CNS Spectr. (2015), 20:319–30. doi: 10.1017/S1092852915000188
6. Arbury S, Hodgson M, Zankowski D, Lipscomb J. Workplace violence training programs for health care workers: an analysis of program elements. Workplace Health Saf. (2017) 65:266–72. doi: 10.1177/2165079916671534
7. Papa A, Venella J. Workplace violence in healthcare: strategies for advocacy. Online J Issues Nurs. (2013) 18:5. doi: 10.3912/OJIN.Vol18No01Man05
8. Douglas KS, Hart SD, Webster CD, Belfrage H, Guy LS, Wilson CM. Historical-clinical-risk management-20, version 3 (HCR-20V3): development and overview. Int J Forensic Ment Health. (2014) 13:93–108. doi: 10.1080/14999013.2014.906519
9. Webster CD, Nicholls TL, Martin ML, Desmarais SL, Brink J. Short-Term Assessment of Risk and Treatability (START): The case for a new structured professional judgment scheme. Behav Sci Law. (2006) 24:747–66. doi: 10.1002/bsl.v24:6
10. Chu CM, Daffern M, Ogloff JRP. Predicting aggression in acute inpatient psychiatric setting using BVC, DASA, and HCR-20 Clinical scale. J Forens Psychiatry Psychol. (2013) 24:269–85. doi: 10.1080/14789949.2013.773456
11. Mullally K, Mamak M, Chaimowitz GA. The next generation of risk assessment and management. Int J Risk Recover. (2018) 1:21–6. doi: 10.15173/ijrr.v1i1.3365
12. Vaaler AE, Iversen VC, Morken G, Fløvig JC, Palmstierna T, Linaker OM. Short-term prediction of threatening and violent behaviour in an Acute Psychiatric Intensive Care Unit based on patient and environment characteristics. BMC Psychiatry. (2011) 11:44. doi: 10.1186/1471-244X-11-44
13. Ogloff JRP, Daffern M. The dynamic appraisal of situational aggression: an instrument to assess risk for imminent aggression in psychiatric inpatients. Behav Sci Law. (2006) 24:799–813. doi: 10.1002/bsl.v24:6
14. Maguire T, Daffern M, Bowe SJ, McKenna B. Predicting aggressive behaviour in acute forensic mental health units: a re-examination of the dynamic appraisal of situational aggression's predictive validity. Int J Ment Health Nurs. (2017) 26:472–81. doi: 10.1111/inm.2017.26.issue-5
15. Lantta T, Kontio R, Daffern M, Adams CE, Välimäki M. Using the Dynamic Appraisal of Situational Aggression with mental health inpatients: a feasibility study. Patient Prefer Adherence. (2016) 10:691–701. doi: 10.2147/PPA.S103840
16. Griffith JJ, Daffern M, Godber T. Examination of the predictive validity of the Dynamic Appraisal of Situational Aggression in two mental health units. Int J Ment Health Nurs. (2013) 22:485–92. doi: 10.1111/inm.2013.22.issue-6
17. Chan O, Chow KK-W. Assessment and determinants of aggression in a forensic psychiatric institution in Hong Kong, China. Psychiatry Res. (2014) 220:623–30. doi: 10.1016/j.psychres.2014.08.008
18. Barry-Walsh J, Daffern M, Duncan S, Duncan S, Ogloff J. The prediction of imminent aggression in patients with mental illness and/or intellectual disability using the Dynamic Appraisal of Situational Aggression instrument. Australas Psychiatry. (2009) 17:493–6. doi: 10.1080/10398560903289975
19. Kasinathan J, Marsland C, Batterham P, Gaskin C, Adams J, Daffern M. The DASA : YV assists the appraisal of imminent aggression risk in young patients. Australas Psychiatry. (2015) 23:314–5. doi: 10.1177/1039856215584526
20. Chu CM, Hoo E, Daffern M, Tan J. Assessing the risk of imminent aggression in institutionalized youth offenders using the dynamic appraisal of situational aggression. J Forens Psychiatry Psychol. (2012) 23:168–83. doi: 10.1080/14789949.2012.668207
21. Riordan D, Browne C, Korobanova D, Kariuki M, Daffern M, Dean K. Imminent aggression in female forensic inpatients: A study assessing the predictive validity of the dynamic appraisal of situational aggression: women’s version (DASA: WV). Int J Forensic Ment Health. (2019) 18:326–35. doi: 10.1080/14999013.2019.1577315
22. Connor M, Armbruster M, Hurley K, Lee E, Chen B, Doering L. Diagnostic sensitivity of the dynamic appraisal of situational aggression to predict violence and aggression by behavioral health patients in the emergency department. J Emerg Nurs. (2020) 46:302–9. doi: 10.1016/j.jen.2019.12.006
23. Dickens GL, O'Shea LE, Christensen M. Structured assessments for imminent aggression in mental health and correctional settings: systematic review and meta-analysis. Int J Nurs Stud. (2020) 104:103526. doi: 10.1016/j.ijnurstu.2020.103526
24. Nqwaku M, Draycott S, Aldridge-Waddon L, Bush E-L, Tsirimokou A, Jones D, et al. Predictive power of the DASA-IV: variations in rating method and timescales. Int J Ment Health Nurs. (2018) 27:1661–72. doi: 10.1111/inm.2018.27.issue-6
25. Griffiths R, Dawber A, McDougall T, Midgley S, Baker J. Non-restrictive interventions to reduce self-harm amongst children in mental health inpatient settings: Systematic review and narrative synthesis. Int J Ment Health Nurs. (2022) 31:35–50. doi: 10.1111/inm.12940
26. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington DC: american Psychiatric Association (2013).
27. van der Laan B, Verstegen N, de Vogel V. The use of the Brøset Violence Checklist within forensic psychiatry. Tijdschr Psychiatr. (2023) 65:253–8.
28. Maguire T, Daffern M, Bowe SJ, McKenna B. Evaluating the impact of an electronic application of the Dynamic Appraisal of Situational Aggression with an embedded Aggression Prevention Protocol on aggression and restrictive interventions on a forensic mental health unit. Int J Ment Health Nurs. (2019) 28:1186–97. doi: 10.1111/inm.12630
29. Kaunomäki J, Jokela M, Kontio R, Laiho T, Sailas E, Lindberg N. Interventions following a high violence risk assessment score: a naturalistic study on a Finnish psychiatric admission ward. BMC Health Serv Res. (2017) 17:26. doi: 10.1186/s12913-016-1942-0
31. Dack C, Ross J, Papadopoulos C, Stewart D, Bowers L. A review and meta-analysis of the patient factors associated with psychiatric in-patient aggression. Acta Psychiatrica Scandinavica. (2013) 127:255–68. doi: 10.1111/acps.2013.127.issue-4
Keywords: aggression, inpatient violence, risk assessment, prevention, forensic-psychiatric practice, acute psychiatric admission, old age psychiatry, schizophrenia
Citation: Moscovici M, Farrokhi F, Vangala L, Simpson AIF, Kurdyak P and Jones RM (2024) Violence risk prediction in mental health inpatient settings using the Dynamic Appraisal of Situational Aggression. Front. Psychiatry 15:1460332. doi: 10.3389/fpsyt.2024.1460332
Received: 05 July 2024; Accepted: 08 November 2024;
Published: 10 December 2024.
Edited by:
Yasin Hasan Balcioglu, Bakirkoy Prof Mazhar Osman Training and Research Hospital for Psychiatry, Neurology, and Neurosurgery, TürkiyeReviewed by:
Heather Moulden, McMaster University, CanadaHoward Ryland, University of Oxford, United Kingdom
Copyright © 2024 Moscovici, Farrokhi, Vangala, Simpson, Kurdyak and Jones. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Roland M. Jones, cm9sYW5kLmpvbmVzQGNhbWguY2E=
†Present address: Mario Moscovici, Department of Psychiatry, University of British Columbia, Vancouver, BC, Canada
Forensic Psychiatric Hospital, Coquitlam, BC, Canada
 Mario Moscovici1†
Mario Moscovici1† Alexander I. F. Simpson
Alexander I. F. Simpson Roland M. Jones
Roland M. Jones