- 1Department of Neurology, Changhua Christian Hospital, Changhua, Taiwan
- 2Department of Neurology, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan
- 3Neuroscience Research Center, Kaohsiung Medical University, Kaohsiung, Taiwan
- 4Department of Neurology, Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung, Taiwan
- 5School of Post-Baccalaureate Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 6Department of Pharmacy, Taichung Veterans General Hospital, Taichung, Taiwan
- 7Intelligent System Laboratory, Department of Electrical Engineering, College of Electrical Engineering and Computer Science, National Kaohsiung University of Science and Technology, Kaohsiung, Taiwan
- 8National Institute of Cancer Research, National Health Research Institutes, Tainan, Taiwan
- 9Center for Big Data Research, Kaohsiung Medical University, Kaohsiung, Taiwan
- 10Dementia Center, Department of Neurology, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 11School of Medicine, College of Medicine, Chang Gung University, Taoyuan, Taiwan
Background and objectives: This study aimed to confirm the effectiveness of the virtual passport for dementia care.
Research design and methods: The virtual passport is an application (app) tool connecting healthcare professionals, dementia care sites, and people living with dementia (PLWD) and their family caregivers. This tool assists case managers in hospitals by providing individualized care plans and health education to PLWD and their caregivers. The dementia quality indicator achievement rates, care needs investigation and fulfillment, severity of behavioral and psychological symptoms of dementia (BPSD), and changes in caregiver burden and depression are measured at the initial interview and 6 and 12 months after the intervention.
Results: We enrolled 57 and 54 patients and their caregivers in the virtual passport and routine care groups, respectively. Compared to the control group, six quality indicators in the passport group showed significantly higher achievement at 6 months after using the virtual passport. Case managers addressed more care needs at 6 months (1.37 vs 0, p < 0.001) and 12 months (1.32 vs 0, p < 0.001). Improvement in severity of neuropsychiatric symptoms (neuropsychiatric inventory (NPI) irritability/lability difference: -0.58 vs 0.22, p = 0.044; NPI agitation/aggression difference =-0.78 vs 0.00, p = 0.042) were also observed. No obvious influence was found in caregiver burden and depression after using the virtual passport.
Discussion and implications: The virtual passport is an effective information technology tool in improving the quality of dementia care, assisting case management in identifying more care needs, and reducing the severity of BPSD.
Introduction
Dementia is a degenerative disease characterized by a general decline in cognitive abilities, impacting memory, judgment, language, and behavior. It also often leads to delusions, hallucinations, and disruptive behaviors, imposing a huge burden on both patients and their caregivers (1). As the prevalence and incidence of dementia increase with age, dementia care has become a crucial medical concern in developed countries with a high proportion of elderly populations (2–4).
A population-based study in Taiwan in 2011 reported that the age-adjusted prevalence of dementia among individuals aged 65–69, 70–74, 75–79, 80–84, 85–89, and 90 years was 3.40%, 3.46%, 7.19%, 13.03%, 21.92%, and 36.88%, respectively. The prevalence of dementia exhibited an upward trend with advancing age, doubling approximately every 5-year after age 70 (5). Another study utilizing Taiwan’s National Health Insurance Research Database spanning from 2004 to 2010 indicated a significant increase in the prevalence of dementia and Alzheimer’s disease (AD), rising from 4.7 to 7.6 per hundred people and 2.3 to 3.5 per hundred people over a seven-year period, respectively (6). These findings suggest that dementia care has emerged as a critical concern in Taiwan’s long-term care services owing to its rapidly aging society.
To further support people living with dementia (PLWD) and alleviate the burden of caregivers, the Taiwanese government brought people with dementia aged over 50 years within the Long-Term Care Act 2.0 since 2017. This act introduced two kinds of dementia care services centers: Dementia-integrated Care Centers and Community Service Centers for Dementia (CSCD). Dementia-integrated Care Centers are in hospitals or sites; they assist patients with suspected dementia to obtain accurate diagnoses, provide medical treatment and care management, and introduce social resources. Dementia-integrated Care Centers also provide professional health training and promote public education on dementia literacy. CSCD are community care sites offering cognitive training or stimulation programs, respite services for PLWD, and training programs and support for caregivers (7). As of September 2021, there were 103 Dementia Integrated Care Centers and 506 CSCD in Taiwan, providing care for 55,360 and 16,053 PLWD, respectively (7).
The primary mission of Dementia Integrated Care Centers is to provide case management, which involves a collaborative process of assessment, planning, facilitation, coordination, and evaluation to meet the health needs of individuals and their families. This can help promote the achievement of dementia quality indicators, facilitate the transfer of appropriate social resources, and improve the outcome for both patients and caregivers, such as reducing the severity of neuropsychiatric symptoms (8, 9). However, each care center developed its own content and offered individualized characteristic services and the actual efficacy and chilits of these services for patients and their caregivers are lacking in Taiwan. (10)
The complexity of dementia case management is further compounded by changes in household dynamics. In Taiwan, the nuclear family is the predominant household type and aging parents are often cared for by different children in rotation, and this might require movement between different countries. Thus, PLWD may need to visit various regional hospitals or dementia service stations. Despite the Taiwanese government’s promotion of a national dementia policy, there still remains a lack of exchange of individual medical information and records between different care centers which may increase the social costs and burden.
Currently, Information Technology(IT) (11–13) and mobile applications(apps) (14–16) have been used widely to improve the quality of dementia health care. A variety of innovative products were reported benefit PLWD and their informal caregivers in their daily lives. (12, 15–20) However, apps designed for health professionals or case manager were relatively few and lack relevant research verification or could not fully meet user needs as being a support tool (21).
Consequently, we propose the concept of a virtual passport as available and comprehensive apps for dementia care in Taiwan. The health professionals and case manager have to regularly assess and upload the medical information, including diagnostic evaluations, personalized health education, and care plans developed through shared decision-making with PLWD and caregivers on a secure and encrypted cloud platform. Using a webpage and app, medical information can be shared between different care centers so that the case management could be more consistent and would not be interrupted based on PLWD’s location. Also, family caregivers can access the care plan as well as communicate with healthcare professionals or staff at the CSCD readily.
The objective of this study is to demonstrate the effectiveness of the virtual passport designed to support dementia care. Our aim is to establish an evidence-based integrated information technology (IT) system that connects three stakeholders: healthcare professionals in Dementia Integrated Care Centers, staff in the CSCD, and patients and family caregivers, facilitating effective communication and resulting in a holistic and continuous approach to dementia care.
Research design and methods
Design and participants
This case-control study was conducted at the Dementia Center of Changhua Christian Hospital, a medical center in Changhua, Taiwan, from October 2022 to October 2023. The study enrolled patients aged from 50 to 100 who had been diagnosed with mild cognitive impairment or dementia by neurologists or psychiatrists. All participants had a clinical dementia rating (CDR) scale of ≥ 0.5 as evaluated by clinical psychologists (22). The exclusion criteria in this study were patients residing in long-term care facilities or those lacking a family caregiver. Participants were invited to join the virtual passport group if they had access to a computer, mobile phone, or tablet and agreed to have their medical information uploaded to the cloud platform and accessed via the website or mobile app. The control group received routine dementia collaborative care, while the case group utilized the virtual passport in addition to routine dementia care.
This study received approval from the Institutional Review Board of Changhua Christian Hospital (CCH IRB 220128). All participants provided informed consent before participating in the study.
Intervention method
Dementia collaborative care model
Since October 2014, we have a dementia collaborative care model at Changhua Christian Hospital. Our team members include physicians (including neurologists, psychiatrists, gerontologists, and primary care physicians), psychologists, social workers, dieticians, occupational therapists, pharmacists, and nursing case managers. Upon diagnosing mild cognitive impairment or dementia, our care team conducts patient and caregiver interviews to assess various aspects, including the patient’s cognitive, functional, behavioral, and psychological symptoms, as well as the caregiver’s burden, care problems, and preference for utilizing care resources.
The care team addresses 26 different care needs, mostly related to quality measures and the needs of the patients and their caregivers (23–25). Detailed content regarding the assessment for each care need has been published in our previous study (26). When assessments reveal abnormalities, the care team addresses these needs and introduces corresponding education and resources. After the initial interview, the care team arranges monthly phone contacts and face-to-face evaluations every six months to review the care needs of patients and their caregivers. Case managers also examine whether each care need has been fulfilled six months after the need was chosen. For example, if PLWD are still driving or riding a motorcycle, the care need called “driving evaluation and suggestion” will be chosen (26). Any unsafe driving scenario will be discussed with the PLWD and their caregivers. The need will be considered fulfilled if the PLWD can identify more than one risk factor related to unsafe driving/riding and if they can suggest more than one alternative transportation option.
Virtual passport for dementia care
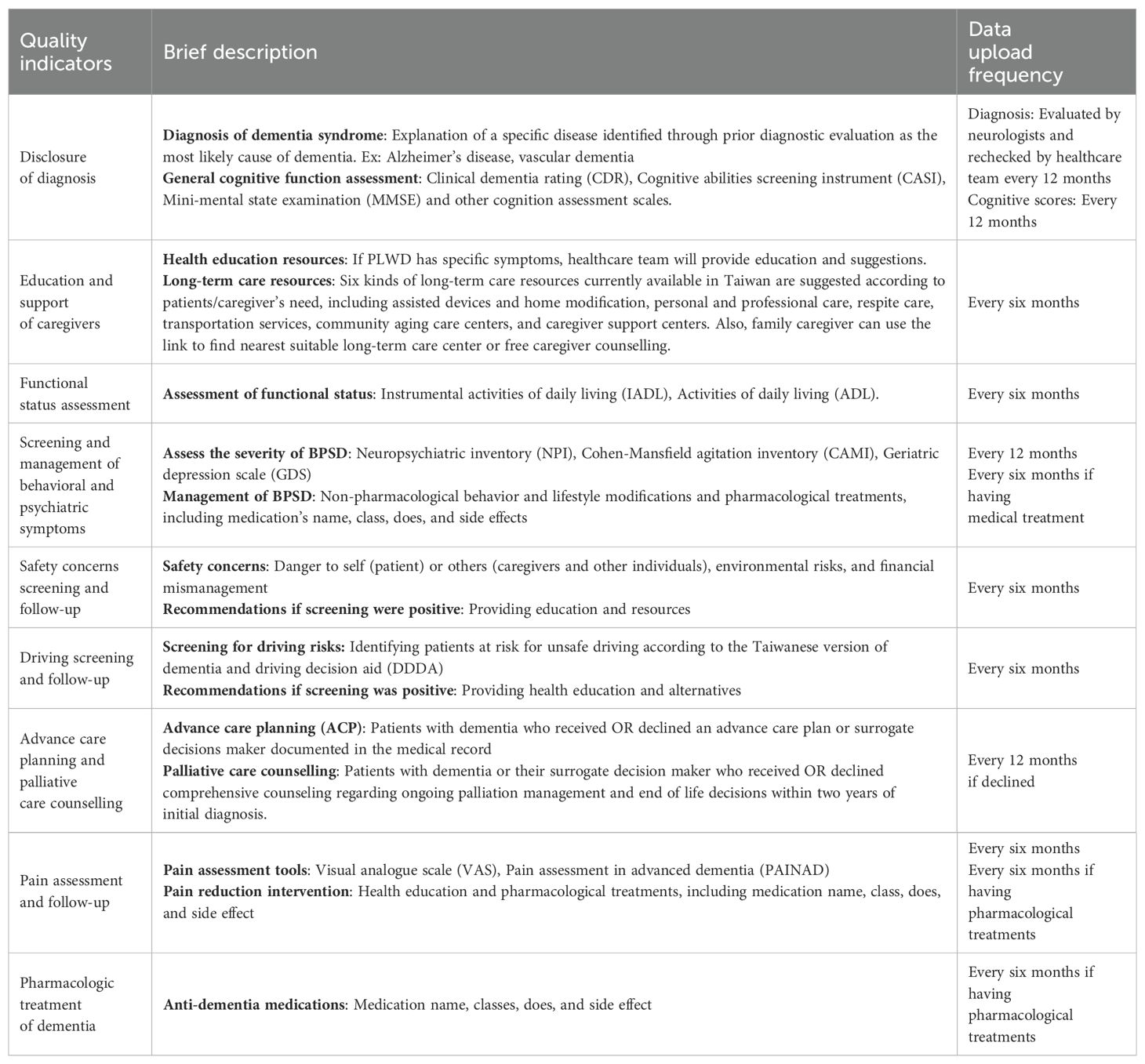
“Virtual passport for dementia” is a website/phone app. Its content refers to the 2015 Dementia Management Quality Measurement Set of the American Academy of Neurology Institute (AANI) (24) and the care needs addressed by the memory clinic of Changhua Christian Hospital (26–28). Nine dementia quality indicators are incorporated in the virtual passport (Table 1) to regularly assess the care needs of patients and their caregivers.
The virtual passport group’s medical information and individualized health education are uploaded to a cloud platform. The incorporation of information into the virtual passport enables case managers to address the care needs once again and provide relevant care plans and health education on the passport. Patients and family caregivers can view the evaluation reports, care plans, and health education by logging into the websites or app. Case managers will evaluate and upload information on the virtual passport every six to 12 months (see Table 1). Virtual passport for dementia” website/APP was created by Changhua Christian hospital, Kaohsiung Medical University, and National Kaohsiung University of Science and Technology. Android APP V1.0 and website system V1.3.27 were used for the present analysis.
Measurements
Measurement of patient and caregiver features
The sex, age, dementia subtype, baseline clinical dementia rating (CDR) scale, anti-dementia (cholinesterase inhibitors or memantine), perfusion drugs (such as piracetam or ginkgo biloba), psychotropic drugs (antipsychotic, antidepressant, sedative or anti-epileptic) and baseline neuropsychiatric inventory (NPI) scores of patients as well as the baseline Zarit Burden Interview instrument (ZBI) and Center for Epidemiologic Studies Depression Scale (CES-D) scores of the caregivers were collected during the initial assessment. The NPI score was used to assess the severity of dementia-related psychological and behavioral symptoms (29). The total NPI score, which encompasses 12 domains, ranged from 0 to 144, with higher scores indicating greater severity. ZBI was used to evaluate the caregiver burden (30). The total ZBI score ranged from 0 to 88, with higher ZBI scores indicating increased caregiver burden. CES-D was used to assess the caregiver’s depressive mood (31). The total CES-D score ranged from 0 to 60, with higher scores indicating greater caregiver depression.
Measurement of virtual passport efficacy
The assessment was conducted at the initial interview and six and 12 months after using the virtual passport. We analyzed the virtual passport efficacy by comparing the following outcome measures between the control and passport groups: (1) achievement rates of dementia quality indicators suggested by the American Academy of Neurology (AAN) 2015 dementia care quality indicators, (2) investigation and fulfillment of care needs, (3) severity of behavioral and psychiatric symptoms, (4) change in caregiver’s burden, and (5) change in caregiver’s depression.
In (2), investigation and fulfillment of care needs, we counted the number of care needs chosen by the case managers and the percentage of need fulfillment six months later. In (3), severity of behavioral and psychiatric symptoms, we analyzed the difference in total NPI scores and each NPI subdomain score between the initial assessment and that six or 12 months later. In (4), change in caregiver burden, we compared the ZBI score at six and 12 months with that at the initial assessment. In (5), change in caregiver depression, we tracked the changes in the CES-D scores.
Statistical analyses
All data were analyzed using R software (R Foundation for Statistical Computing). Pearson’s chi-squared test or Fisher’s exact test were employed to test for differences in categorical data. Numerical data were tested using Student’s t-test or the Kruskal-Wallis rank sum test. Differences were considered statistically significant when the p-value was less than 0.05.
Results
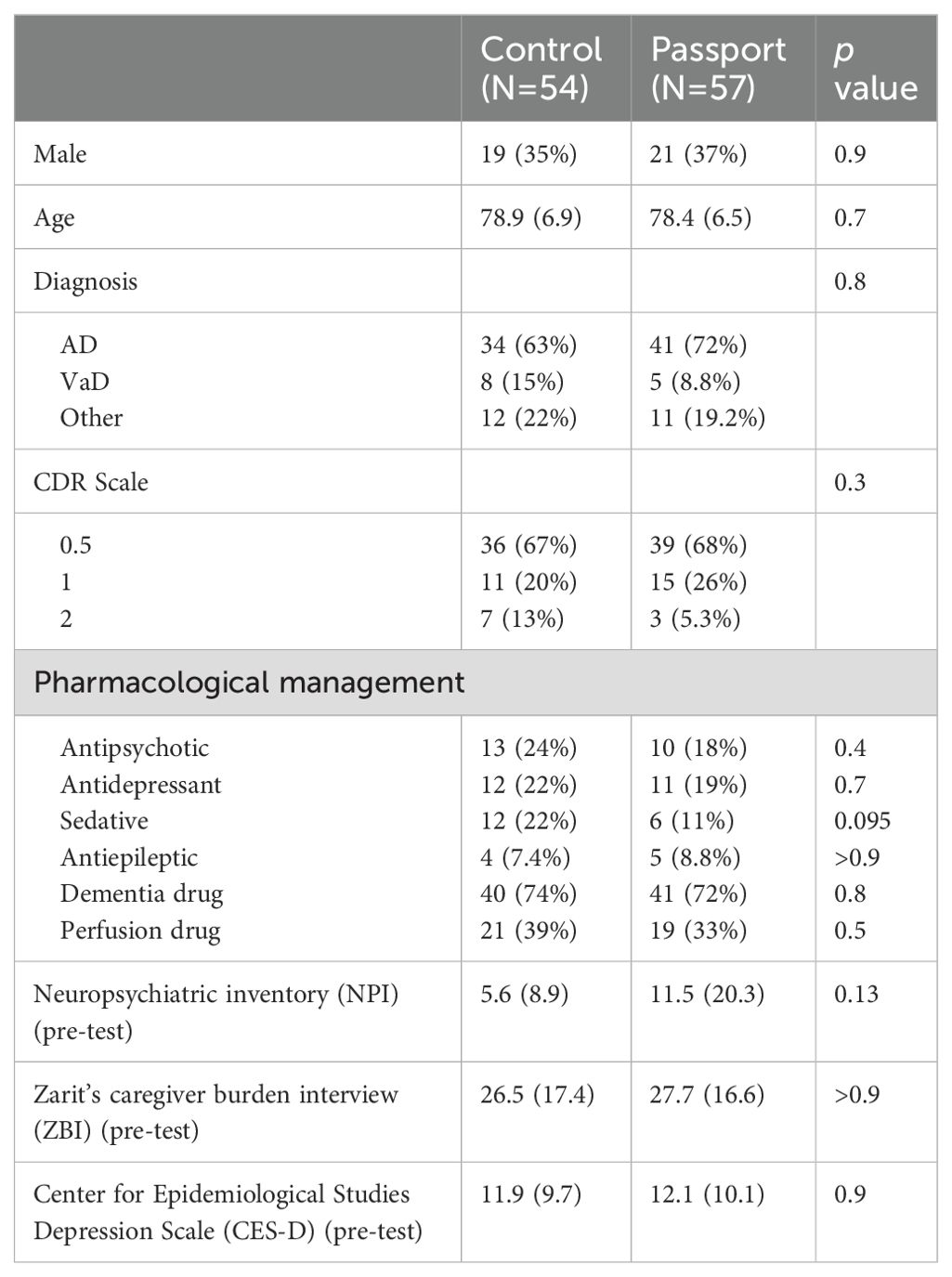
This study enrolled 111 patients newly diagnosed with dementia, comprising 54 participants who received routine dementia collaborative care and 57 who used the virtual passport in addition to routine care. Table 2 presents the baseline characteristics of the participants. There were no significant differences between the control and passport groups with regard to sex, age, diagnosis, CDR scale, medication use and baseline NPI, ZBI and CES-D scores.
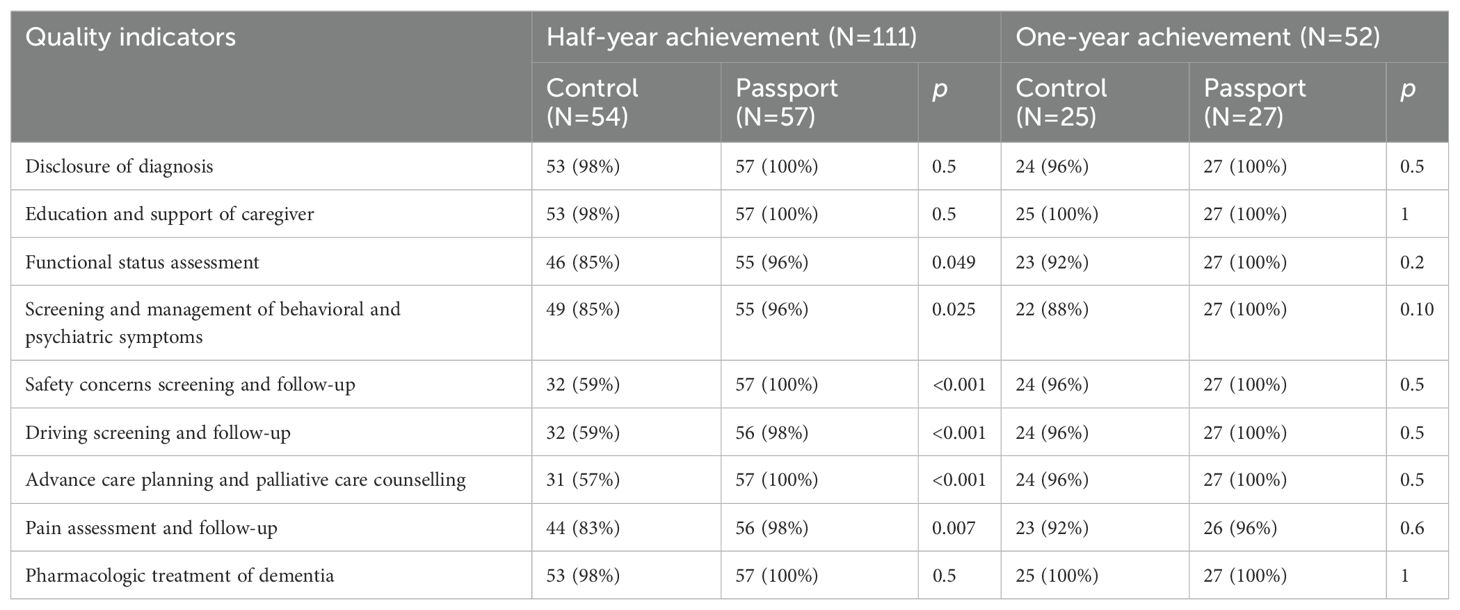
Dementia quality indicator achievement rates suggested by AAN 2015 dementia care quality indicators
Table 3 presents the dementia quality indicator achievement rates after using the virtual passport for six months and 12 months. Compared with the control group, the passport group showed significantly higher achievements six months after virtual passport intervention in six quality indicators, including functional status assessment (85% vs 96%, p=0.049), screening and management of behavioral and psychiatric symptoms (85% vs 96%, p=0.025), safety concerns screening and follow-up (59% vs 100%, p<0.001), driving screening and follow-up (59% vs 98%, p<0.001), advance care planning and palliative care counselling (57% vs 100%, p<0.001), and pain assessment and follow-up (83% vs 98%, p=0.007). Although not significant, all the quality indicators showed higher achievements 12 months after using the virtual passport.
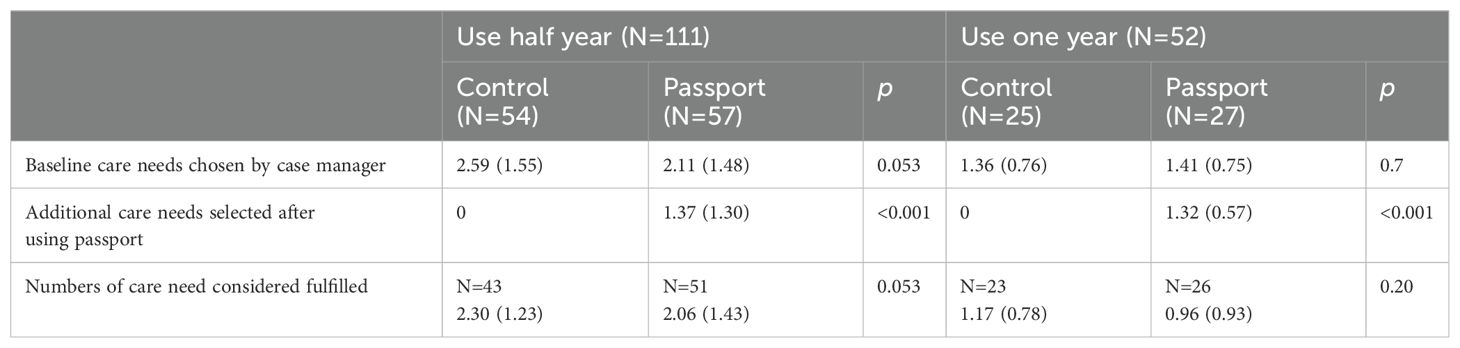
Investigation and fulfillment of care needs
Table 4 shows no significant differences in number of baseline care needs between the control and passport group by six (n=2.59 vs 2.11, p=0.053) and 12 (n=1.36 vs 1.41, p=0.7) months of intervention. However, the case manager addresses significantly more care needs after six (1.37 vs 0, p<0.001) and 12 (1.32 vs 0, p<0.001) months of virtual passport intervention. There were no significant differences in care need fulfillment percentage between the control and passport groups by six and 12 months.
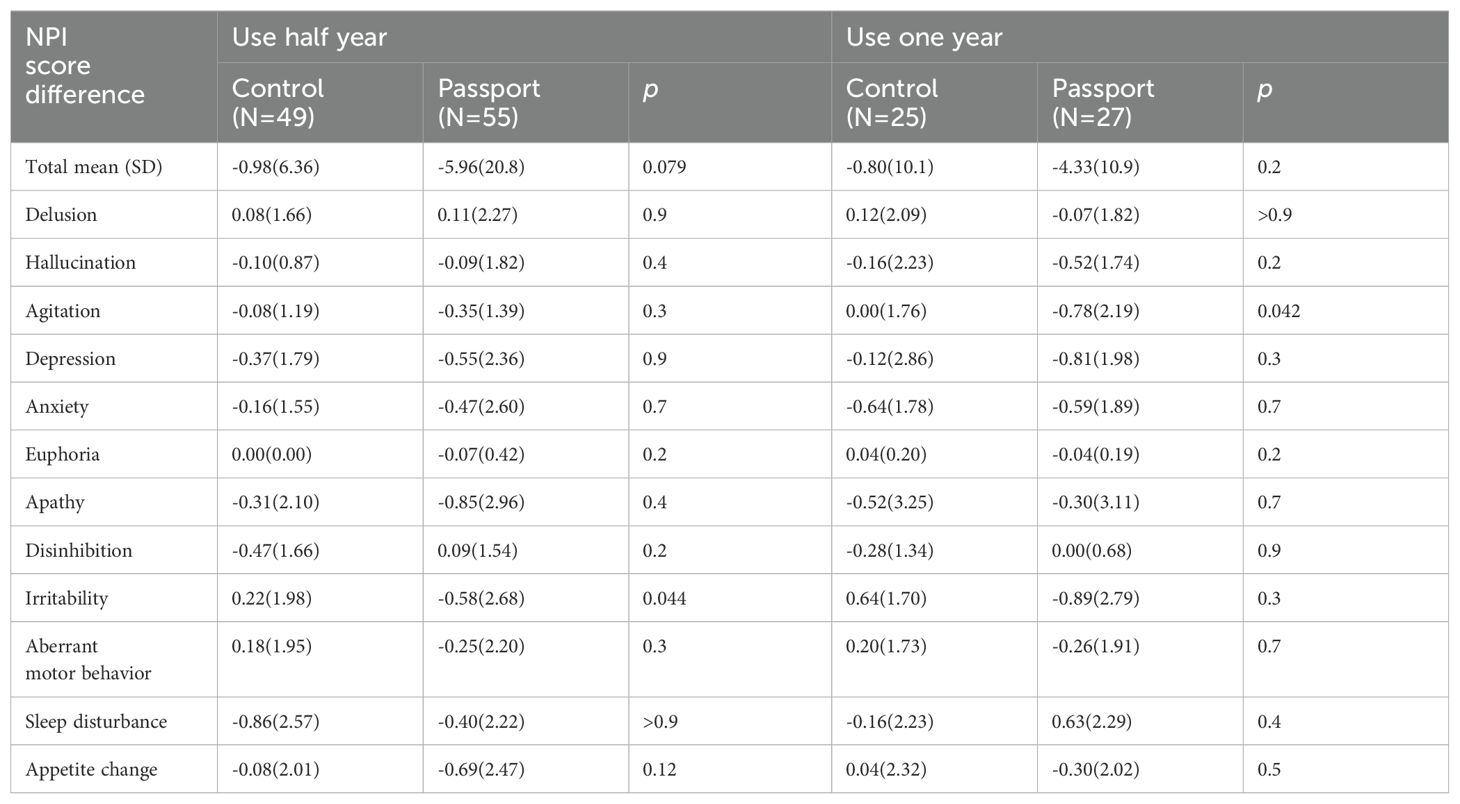
Severity of behavioral and psychiatric symptoms
Table 5 shows the change in NPI scores from the initial assessment six and 12 months after passport use. In all, 104 participants completed six months of intervention by the care team. In a comparison with the control group (n = 49), PLWD in the passport group (n = 55) showed significant improvement in irritability/liability (NPI difference =-0.58 vs 0.22, p=0.044) after the intervention. Furthermore, 52 participants completed 12 months of intervention. In a comparison with the control group (n = 25), PLWD in the passport group (n = 27) showed significant improvement in agitation/aggression after the intervention (NPI difference =-0.78 vs 0.00, p=0.042).
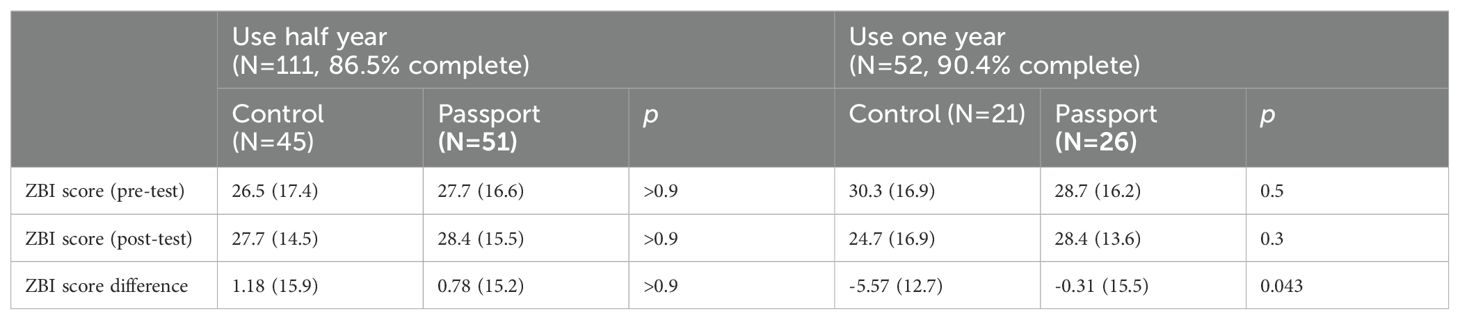
Change in caregiver burden
Table 6 shows the change in ZBI scores from the initial assessment six and 12 months after passport use. In all, 96 (86.5%) and 47 (90.4%) caregivers completed ZBI in six and 12 months, respectively. In a comparison with the passport group (n = 26), the control group (n = 21) showed significant improvement in ZBI scores after 12 months of passport use (ZBI difference =-5.57 vs -0.31, p=0.043).
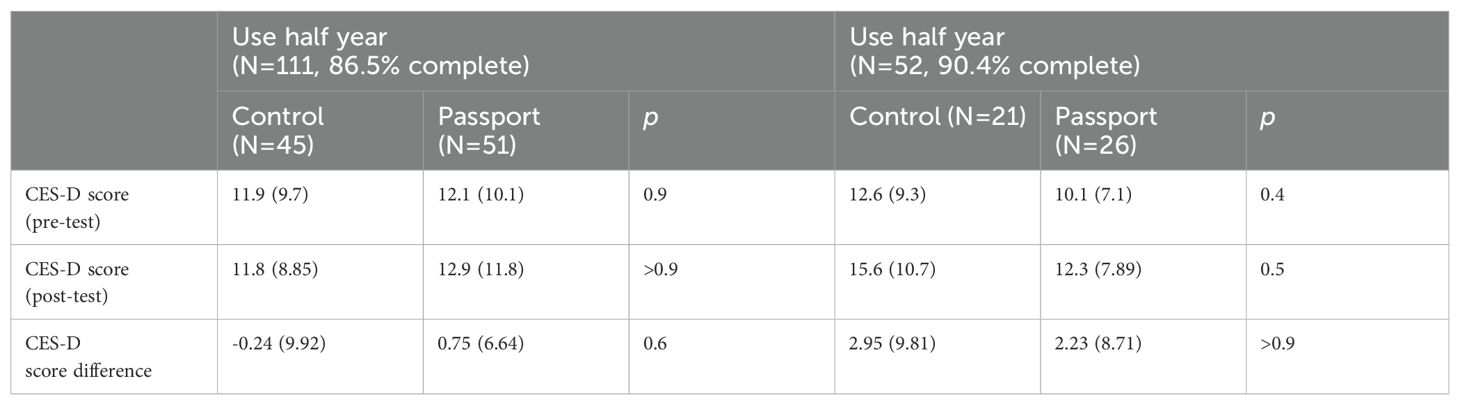
Change in caregiver depression
Table 7 shows the change in CES-D scores from the initial assessment six and 12 months after passport use. In all, 96 (86.5%) and 47 (90.4%) caregivers completed ZBI in six and 12 months, respectively. No significant difference was found in CES-D scores between the passport and control groups at both time points.
Discussion
This study found that the virtual passport improves the achievement rates of dementia quality indicators, especially for patients newly diagnosed with dementia within six months. Moreover, the virtual passport can help case managers address additional care needs and alleviate the severity of BPSD, particularly irritability and agitation. However, use of the virtual passport showed no obvious influence on the caregiver’s burden or depression.
Case management in dementia care presents significant challenges due to the variability in clinical symptoms, functional status, and home environment of the individual patients. Identifying potential care needs for each case and providing appropriate health education requires substantial effort and time from case managers. In the field of IT use for dementia care, most studies primarily focused on supporting both PLWD and their informal caregivers in their daily lives. A systematic review indicated that most apps developed for PLWD as end users primarily featured reminders/prompts, safety devices and reminiscence/entertainment (16, 32). Another review of dementia-related apps in Australia found the majority of them designed for caregivers with focus on dementia information, practical caregiving, and communication tips (15). However, few studies have considered IT system support case management.
Our earlier study found that a computer-assisted assessment system for dementia case management could improve the quality indicator completion rates for dementia (33). A cluster randomized trial showed that the IT tool may support case managers who are new on the job and emphasize the importance of user-friendliness (34). Moreover, a qualitative study by Thoma-Lürken et al. (21) suggested that a decision support app could aid case managers in clinical judgment, problem assessment, and providing advice on possible solutions. The present study further confirmed the effectiveness of the virtual passport in assisting case managers to identify more care needs and efficiently achieve dementia quality indicators.
Currently, most dementia-related apps designed for PLWD with BPSD focus on non-pharmacological interventions (12, 18, 35). For example, they include music therapy (36), reminiscence therapy (37, 38), and brain games. An open-label study demonstrated that tablet-based mHealth apps can serve as a non-pharmacological management tool for agitation of PLWD with varying severity (39). Some apps have been developed for caregivers or case managers as users, but with little or no significant effect noted in improving BPSD. For example, these apps can advise caregivers on monitoring BPSD severity (40), delivers psychoeducation and caregiver support with the focus on management of BPSD (20) and assist physicians in monitoring the appropriateness of psychotropic drug prescriptions (41).
The present study has confirmed the effectiveness of the virtual passport in reducing the severity of BPSD, particularly in addressing irritability and agitation. The most likely explanation for this is that the dementia collaborative care model was found beneficial for BPSD management in our previous study (9). The virtual passport facilitated close contact between healthcare professionals and caregivers, providing them with more information about non-pharmacological behavior interventions and lifestyle modifications for BPSD.
There is inconsistency on whether mobile applications can improve caregiver fatigue, burden, and depression. Three systematic reviews indicated that technology-based interventions have little or no significant effect on caregiver burden and depression (42–44). These may be attributed to that self-report which is subject to bias from over- and under-reporting of affective responses, a clinical heterogeneity in the interventions and the use of different outcomes made it difficult to compare the effects of different interventions directly. However, some case-control studies have shown that mobile apps can significantly improve family caregivers’ fatigue, burden and depression (17, 19, 20). These apps highlight the importance of caregiver support with focus on aiding management and offering insight into dementia. Also, in a qualitative study, most of enrolled family caregivers prefer easy-to-understand apps and favor concrete intervention strategies (45). Given these findings, our virtual passport can consider providing more health education and practical suggestions for specific symptoms and linking more medical resources with dementia families in the future.
As regards the outcome of the effect on caregiver burden, the control group showed significant improvement in ZBI scores after 12 months of intervention. This observation may be attributed to non-response bias. The response rate in the control group (84%) was lower than that in the passenger group (96.3%), probably because caregivers in the control group experienced increased care burden, leading to withdrawal or loss of follow-up.
The strength of this study lies in its focus on case management. Only a few studies have investigated the effect of IT on case management in dementia care. This study provides this perspective. However, this study has some limitations. First, the study population was relatively small and confined to a single hospital, limiting the generalizability of the findings. Second, the participants in the virtual passport group were invited rather than randomly assigned, leading to the possibility of subject selection bias. Fortunately, the baseline characteristics of the participants showed no significant differences between the control and passport group.
In clinical practice, more evidence-based research studies should be conducted to prove the effectiveness of the virtual passport on the ability to achieve better quality of case management, improve outcomes, and lower society costs. The virtual passport currently supports multiple dementia care sites to use simultaneously. We sincerely hope that virtual passport can cooperate with Taiwan’s government long-term care policies, and more dementia care center and more PLWD and their caregivers can participate in and benefited from it. Besides, the experience and feedback from the end users should be adopted for usability and acceptability evaluation. Safety and security for personal medical information is also an important issue we should focus more. (16, 21, 45). Also, we should consider how to deal with the challenge that these IT tool may be too complex and costly to kept updating, maintain and widespread use (13).
Conclusion
This study demonstrated that the virtual passport for dementia improved the quality of dementia care, assisting case management in identifying more care needs and attenuating the severity of BPSD. The virtual passport supports dementia care center case managers in providing more efficient and qualitative care to PLWD. It could be a suitable IT tool in clinical practice of healthcare systems in Taiwan. Future studies should consider a larger sample in investigating the effectiveness of the virtual passport on dementia care such as changes of cognition, caregiver’s quality of life, and cost-effectiveness.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Changhua Christian Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
QH: Writing – original draft, Writing – review & editing. WW: Methodology, Supervision, Writing – review & editing. YY: Investigation, Project administration, Supervision, Writing – review & editing. YT: Methodology, Supervision, Writing – review & editing. HD: Methodology, Supervision, Writing – review & editing. WH: Methodology, Supervision, Writing – review & editing. LH: Methodology, Supervision, Writing – review & editing. KJ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Health Research Institutes (NHRI-11A1-CG-CO-06-2225-1, NHRI-12A1-CG-CO-06-2225-1, NHRI-13A1-CG-CO-06-2225-1) and Kaohsiung Medical University Research Center (KMU-TC112B02).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Springate BA, Tremont G. Dimensions of caregiver burden in dementia: Impact of demographic, mood, and care recipient variables. Am J Geriatric Psychiatry. (2014) 22:294–300. doi: 10.1016/j.jagp.2012.09.006
2. Jorm AF, Jolley D. The incidence of dementia: A meta-analysis. Neurology. (1998) 51:728–33. doi: 10.1212/WNL.51.3.728
3. Fratiglioni L, De RD, Agüero-Torres H. Worldwide prevalence and incidence of dementia. Drugs Aging. (1999) 15:365–75. doi: 10.2165/00002512-199915050-00004
4. Reitz C, Tang MX, Schupf N, Manly JJ, Mayeux R, Luchsinger JA. A summary risk score for the prediction of Alzheimer disease in elderly persons. Arch Neurol. (2010) 67(7):835–41. doi: 10.1001/archneurol.2010.136
5. Sun Y, Lee HJ, Yang SC, Chen T-F, Lin K-N, Lin C-C, et al. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. Bayer A, ed. PloS One. (2014) 9:e100303. doi: 10.1371/journal.pone.0100303
6. Liu CC, Li CY, Sun Y, Hu SC. Gender and age differences and the trend in the Incidence and prevalence of dementia and Alzheimer’s disease in Taiwan: A 7-year national population-based study. BioMed Res Int. (2019) 2019:1–12. doi: 10.1155/2019/5378540
7. Lai PY, Wang WF, Chang MC, Jhang KM. The effectiveness of community aging care centers on global function for people living with dementia. JAD. (2022) 89:553–62. doi: 10.3233/JAD-220372
8. Chen YJ, Jhang KM, Wang WF, Lin GC, Yen SW, Wu HH. Applying apriori algorithm to explore long-term care services usage status—Variables based on the combination of patients with dementia and their caregivers. Front Psychol. (2022) 13:1022860. doi: 10.3389/fpsyg.2022.1022860
9. Hung YH, Wang WF, Chang MC, Jhang KM. Case management-based collaborative care model associated with improvement in neuropsychiatric outcomes in community-dwelling people living with dementia. BMC Geriatrics. (2023) 23:339. doi: 10.1186/s12877-023-04024-8
10. Ministry of Health and Welfare. Long-term care services (1966). Available online at: https://.gov.tw/LTC/lp-6485-207.html (Accessed 2024/02/26).
11. Lee KH, Lee JY, Kim B. Information and communication technology for physical activity in persons living with dementia: A systematic review with implications for evidence-based practice. Worldviews Evidence-Based Nurs. (2022) 19:275–81. doi: 10.1111/wvn.12591
12. Cho E, Shin J, Seok JW, Lee H, Lee KH, Jang J, et al. The effectiveness of non-pharmacological interventions using information and communication technologies for behavioral and psychological symptoms of dementia: A systematic review and meta-analysis. Int J Nurs Stud. (2023) 138:104392. doi: 10.1016/j.ijnurstu.2022.104392
13. Wolff JL, DesRoches CM, Amjad H, Burgdorf JG, Caffrey M, Fabius CD, et al. Catalyzing dementia care through the learning health system and consumer health information technology. Alzheimer’s Dementia. (2023) 19:2197–207. doi: 10.1002/alz.12918
14. Klimova B, Bouckova Z, Toman J. Mobile Phone Apps as Support Tools for People with Dementia. In: Advanced Multimedia and Ubiquitous Engineering: MUE/FutureTech 2018 (Lecture Notes in Electrical Engineering). (Singapore: Springer) (2019) vol. 518, 7–12. doi: 10.1007/978-981-13-1328-8_2
15. Chelberg GR, Neuhaus M, Mothershaw A, Mahoney R, Caffery LJ. Mobile apps for dementia awareness, support, and prevention – Review and evaluation. Disabil Rehabil. (2022) 44:4909–20. doi: 10.1080/09638288.2021.1914755
16. Ye B, Chu CH, Bayat S, Babineau J, How TV, Mihailidis A. Researched apps used in dementia care for people living with dementia and their informal caregivers: Systematic review on app features, security, and usability. J Med Internet Res. (2023) 25:e46188. doi: 10.2196/46188
17. Eisdorfer C, Czaja SJ, Loewenstein DA, Rubert MP, Argüelles S, Mitrani VB, et al. The effect of a family therapy and technology-based intervention on caregiver depression. Gerontol. (2003) 43:521–31. doi: 10.1093/geront/43.4.52
18. Varshney SU, Varshney JU, Tampi RR, McCall WV, Varshney U. AlzhaTV: A nonpharmacological intervention to manage behavioral and psychological symptoms in nursing home dementia patients. Ann Clin Psychiatry. (2018) 30:122–32.
19. Park E, Park H, Kim EK. The effect of a comprehensive mobile application program (CMAP) for family caregivers of home-dwelling patients with dementia: A preliminary research. Japan J Nurs Sci. (2020) 17:e12343. doi: 10.1111/jjns.12343
20. Rodriguez MJ, Kercher VM, Jordan EJ, Savoy A, Hill JR, Werner N, et al. Technology caregiver intervention for Alzheimer’s disease (I-CARE): Feasibility and preliminary efficacy of Brain CareNotes. J Am Geriatrics Soc. (2023) 71:3836–47. doi: 10.1111/jgs.18591
21. Thoma-Lürken T, Lexis MAS, Bleijlevens MHC, Hamers JPH. Perceived added value of a decision support app for formal caregivers in community-based dementia care. J Clin Nurs. (2019) 28:173–81. doi: 10.1111/jocn.14647
22. Morris JC. Clinical dementia rating: A reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatrics. (1997) 9:173–6. doi: 10.1017/S1041610297004870
23. Khanassov V, Vedel I. Family physician–Case manager collaboration and needs of patients with dementia and their caregivers: A systematic mixed studies review. Ann Family Med. (2016) 14:166–77. doi: 10.1370/afm.1898
24. Sanders AE, Nininger J, Absher J, Bennett A, Shugarman S, Roca R. Quality improvement in neurology: Dementia management quality measurement set update. Neurology. (2017) 88:1951–7. doi: 10.1212/WNL.0000000000003917
25. Molony SL, Kolanowski A, Van HK, Rooney KE. Person-centered assessment and care planning. Gerontol. (2018) 58:S32–47. doi: 10.1093/geront/gnx173
26. Jhang KM, Wang WF, Cheng YC, Tung YC, Yen SW, Wu HH. Care need combinations for dementia patients with multiple chronic diseases. Psychol Res Behav Manage. (2023) 16:179–95. doi: 10.2147/PRBM.S388394
27. Jhang KM, Chang MC, Lo TY, Lin CW, Wang WF, Wu HH. Using the apriori algorithm to classify the care needs of patients with different types of dementia. Patient prefer adherence. (2019) 13:1899–912. doi: 10.2147/PPA.S223816
28. Jhang KM, Wang WF, Chang HF, Liu YH, Chang MC, Wu HH. Care needs of community-residing male patients with vascular cognitive impairment. Neuropsychiatr Dis Treat. (2020) 16:2613–21. doi: 10.2147/NDT.S277303
29. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The neuropsychiatric inventory: Comprehensive assessment of psychopathology in dementia. Neurology. (1994) 44:2308–8. doi: 10.1212/WNL.44.12.2308
30. Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M. The Zarit burden interview. Gerontol. (2001) 41:652–7. doi: 10.1093/geront/41.5.652
31. Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. (1997) 12:277–87. doi: 10.1037/0882-7974.12.2.277
32. Rostill H, Nilforooshan R, Morgan A, Barnaghi P, Ream E, Chrysanthaki T. Technology integrated health management for dementia. Br J Community Nurs. (2018) 23:502–8. doi: 10.12968/bjcn.2018.23.10.502
33. Chen YJ, Wang WF, Chang MC, Jhang KM. The effectiveness of the case manager-centered collaborative care model with computer-assisted assessment on quality indicators for the care of dementia. Dementia Geriatric Cogn Disord. (2024) 5:1–8. doi: 10.1159/000536646
34. Van Mierlo LD, Meiland FJM, Van De Ven PM, Van Hout HPJ, Dröes R-M. Evaluation of DEM-DISC, customized e-advice on health and social support services for informal carers and case managers of people with dementia; a cluster randomized trial. Int Psychogeriatrics. (2015) 27:1365–78. doi: 10.1017/S1041610215000423
35. Seok JW, Shin J, Kang B, Lee H, Cho E, Lee KH. Non-pharmacological interventions using information and communication technology for behavioral and psychological symptoms of dementia: A systematic review and meta-analysis protocol. J Adv Nurs. (2022) 78:282–93. doi: 10.1016/j.ijnurstu.2022.104392
36. Kondo E, Tabei K, Okuno R, Akazawa K. Case report: Accessible digital musical instrument can be used for active music therapy in a person with severe dementia and worsening behavioral and psychological symptoms: A case study over a year and a half. Front Neurol. (2022) 13:831523. doi: 10.3389/fneur.2022.831523
37. Imtiaz D, Khan A, Seelye A. A mobile multimedia reminiscence therapy application to reduce behavioral and psychological symptoms in persons with Alzheimer’s. J Healthc Eng. (2018) 2018:1536316. doi: 10.1155/2018/1536316
38. Moon S, Park K. The effect of digital reminiscence therapy on people with dementia: A pilot randomized controlled trial. BMC Geriatrics. (2020) 20:166. doi: 10.1186/s12877-020-01563-2
39. Vahia IV, Kamat R, Vang C, Posada C, Ross L, Oreck S, et al. Use of tablet devices in the management of agitation among inpatients with dementia: An open-label study. Am J Geriatric Psychiatry. (2017) 25:860–4. doi: 10.1016/j.jagp.2016.07.011
40. Rangseekajee P, Aphisitphinyo S, Paholpak P, Piyavhatkul N, Vadhanavikkit P, Kaenampornpan M, et al. Mobile application for monitoring behavioral and psychological symptoms of dementia in patients with moderate to severe dementia. Geriatrics Gerontol Int. (2021) 21:472–7. doi: 10.1111/ggi.14164
41. Rasing N, Janus S, Smalbrugge M, Koopmans R, Zuidema S. Usability of an app-based clinical decision support system to monitor psychotropic drug prescribing appropriateness in dementia. Int J Med Inf. (2023) 177:105132. doi: 10.1016/j.ijmedinf.2023.105132
42. Lucero RJ, Fehlberg EA, Patel AGM, Bjarnardottir RI, Williams R, Lee K, et al. The effects of information and communication technologies on informal caregivers of persons living with dementia: A systematic review. Alzheimer’s Dementia: Trans Res Clin Interventions. (2019) 5:1–12. doi: 10.1016/j.trci.2018.11.003
43. Bauernschmidt D, Hirt J, Langer G, Meyer G, Unverzagt S, Wilde F, et al. Technology-based counselling for people with dementia and their informal carers: A systematic review and meta-analysis. J Alzheimer’s disease: JAD. (2023) 93:891–906. doi: 10.3233/JAD-221194
44. Scerbe A, O’Connell ME, Astell A, Morgan D, Kosteniuk J, Panyavin I, et al. Digital tools for delivery of dementia education for caregivers of persons with dementia: A systematic review and meta-analysis of impact on caregiver distress and depressive symptoms. Metwally AM, ed. PloS One. (2023) 18:e0283600. doi: 10.1371/journal.pone.0283600
45. Désormeaux-Moreau M, Michel C-M, Vallières M, Racine M, Poulin-Paquet M, Lacasse D, et al. Mobile apps to support family caregivers of people with Alzheimer disease and related dementias in managing disruptive behaviors: qualitative study with users embedded in a scoping review. JMIR Aging. (2021) 4:e21808. doi: 10.2196/21808
Keywords: dementia, information technology, mobile applications, case management, behavioral and psychological symptoms of dementia (BPSD)
Citation: Hong Q-X, Wang W-F, Yang Y-H, Tung Y-C, Dai H-J, Hsu W-C, Huang L-C and Jhang K-M (2024) The effectiveness of virtual passport, an app-based intervention, for dementia care. Front. Psychiatry 15:1457923. doi: 10.3389/fpsyt.2024.1457923
Received: 03 July 2024; Accepted: 09 September 2024;
Published: 26 September 2024.
Edited by:
Hector Wing Hong Tsang, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Chi Man Tsui, Hong Kong Polytechnic University, Hong Kong SAR, ChinaAtanu Biswas, Institute of Post Graduate Medical Education And Research (IPGMER), India
Copyright © 2024 Hong, Wang, Yang, Tung, Dai, Hsu, Huang and Jhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai-Ming Jhang, a21qaGFuZ0BnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
 Qian-Xi Hong
Qian-Xi Hong Wen-Fu Wang
Wen-Fu Wang Yuan-Han Yang
Yuan-Han Yang Yu-Chun Tung
Yu-Chun Tung Hong-Jie Dai
Hong-Jie Dai Wen-Chuin Hsu
Wen-Chuin Hsu Ling-Chun Huang
Ling-Chun Huang Kai-Ming Jhang
Kai-Ming Jhang