
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 01 November 2024
Sec. Adolescent and Young Adult Psychiatry
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1454484
 John Chee Meng Wong1,2*
John Chee Meng Wong1,2* Natalie Cheok Ling Lei1
Natalie Cheok Ling Lei1 Dennis Mun Yen Kom3
Dennis Mun Yen Kom3 Victoria Hui Fen Fee3
Victoria Hui Fen Fee3 Natalie Huijing Yap1
Natalie Huijing Yap1 Jie Yu Teoh1
Jie Yu Teoh1 Liang Shen4
Liang Shen4 Qai Ven Yap4
Qai Ven Yap4 Michelle Jing Si Wan1
Michelle Jing Si Wan1 Ruochen Du4
Ruochen Du4 Leoniek Kroneman1
Leoniek Kroneman1 Daniel Shuen Sheng Fung5
Daniel Shuen Sheng Fung5 Say How Ong5
Say How Ong5 Cheong Sing Tian2
Cheong Sing Tian2 Muhammad Nabil Syukri Bin Sachiman1
Muhammad Nabil Syukri Bin Sachiman1 Nicholas En-Ping Sii1
Nicholas En-Ping Sii1 Jia Ying Teng2
Jia Ying Teng2 Tze Pin Ng2
Tze Pin Ng2 Frank Verhulst6
Frank Verhulst6Background: Adolescence is a pivotal developmental phase, marked by a high prevalence of mental health issues. The Singapore Youth Epidemiology and Resilience (YEAR) study aims to assess the prevalence of mental health symptoms, sociodemographic risk factors, and the protective role of resilience in a multi-ethnic, Asian school-going adolescent population.
Methods: School-based adolescents aged 11-18 and their parents were invited from a stratified sample of national schools, designed to be demographically representative of the mainstream school-going population. In the screening phase, adolescents completed a battery of questionnaires including the Youth Self-Report (YSR), Child Behaviour Checklist (CBCL), and the Singapore Youth Resilience Scale (SYRESS). Thereafter, diagnostic interviews were conducted on high-risk and control participants. Data analysis was conducted to establish prevalence rates of mental health symptoms, and to examine the associations between mental health symptoms, sociodemographic factors, and resilience.
Results: The final study sample consisted of 3336 adolescents and 2475 parents. Based on adolescents’ response on the YSR, 37.3%, 13.1% and 27.7% of the YEAR Study population scored in the clinical range for internalizing, externalizing and total problems respectively. Based on parents’ reporting on their children on the CBCL, 15.9%, 4.0% and 11.2% scored in the clinical range for internalizing, externalizing and total problems respectively. Sociodemographic risk factors for specific mental health symptoms were identified, including belonging to the age category of 15-16 (OR, 1.8-2.2) and those living in either a 4-, 5-room or executive flat (OR, 0.6-0.7), or in condominiums and other apartments (OR, 0.4-0.6). Total resilience scores were moderately correlated with total [rs(3334) = -.49, p <.01] and internalizing [rs(3334) = -.50, p <.01] problem scores on the YSR.
Conclusion: This study illustrates the state of mental health of school-going adolescents aged 11-18. The greater prevalence of internalizing symptoms indicates the need for stronger attention for identifying internalizing problems and targeted interventions for those at risk of such symptoms. The association between mental health symptoms and resilience factors highlights the protective potential of resilience building for adolescents.
Adolescence is a crucial developmental phase, broadly understood as the transitory period between childhood and adulthood, during which individuals undergo their formative years of physical, socio-emotional and identity development (1).
Due to the significant changes in brain systems related to higher cognitive functions, emotional control, and risk-reward assessment during adolescence, such developmental challenges may increase the risk of developing mental health disorders if insufficiently addressed (2). According to the World Health Organisation (WHO), one in seven 10- to 19-year-olds suffer from a mental health condition globally. Furthermore, mental health conditions contribute to 16% of the global disease burden for this age group (3). Yet, mental health conditions in adolescents are often undetected and untreated, due to stigmatisation (4) and low mental health literacy (5), the latter defined as “understanding how to obtain and maintain positive mental health; understanding mental disorders and their treatments; decreasing stigma related to mental disorders; and, enhancing help-seeking efficacy” (6).
Based on a local recent web survey conducted in Singapore from April to June 2022, 11.7% and 12.8% of children and youth had depressive and anxiety symptoms respectively based on parental responses (7), indicating an urgent need to understand and address the mental health status and resilience of our adolescents. National figures on the prevalence and incidence of psychiatric disorders in adolescents are useful for the implementation of change-affecting policies, establishing research priorities, and monitoring the effect of changes in treatment or service funding. Although the Singapore Mental Health Study (SMHS) provides figures for Singaporeans aged 18 and older (8, 9), no such data is currently available for school-going Singaporean adolescents. Furthermore, although Chodavadia et al. (7)’s study provides recent national data, it leverages on proxy reports from parents, who may be more likely to report more severe cases. The current study employs self-report in addition to parent-report, building upon Chodavadia et al. (7)’s findings by increasing sensitivity of identifying cases, especially with respect to internalizing symptoms such as anxiety and depression. As noted in literature, parents are more likely to report externalizing symptoms in their child as opposed to internalizing symptoms (10).
In addition to establishing prevalence, examining resilience in relation to mental health disorders would help to provide a more holistic picture of mental health (11) and better inform both preventative measures and psychological interventions for adolescents. Resilience is defined as a dynamic process or capacity to adapt and “bounce back” from adversities or life challenges (12–14), a multi-dimensional trait that changes with different demographic factors (e.g., age, gender, socioeconomic status, and ethnicity) and the circumstances that individuals are in and subjected to (15). Being malleable, resilience can be built upon by improving resilience-based skills such as mindfulness and/or cognitive-behavioural skills (16). In recent years, resilience studies have been gaining traction in understanding the risks of developing psychopathologies – many have found resilience to be negatively associated with depression and anxiety (17–19), even exerting protective or buffering effects (20, 21).
Considering the above, the Singapore Youth Epidemiology and Resilience (YEAR) study was conceived to establish the prevalence rates of psychiatric disorders and reflect the state of resilience for school-going adolescents aged 11-18. Additionally, it aims to assess the levels of psychosocial, familial, and academic stress and their relationships to adolescent mental health, as well as examine how resilience modulates the effects of stress on mental health. Investigating adolescent identity development and impairment and its age trajectory is also a key objective. Ultimately, the study strives to accurately provide the above information for policy makers to aid in their decision-making to raise public awareness of adolescent mental health issues, and to plan, design and implement school-based interventions to detect, treat and prevent such problems.
This present article will focus on the: (i) study methodology, (ii) reporting of prevalence rates of mental health symptoms, (iii) identification of sociodemographic risk factors for five DSM-oriented mental health symptom clusters (affective problems, anxiety problems, somatic problems, attention-deficit hyperactive problems, oppositional-defiant/conduct problems) and comorbidities, as well as the (iv) association between resilience factors and mental health symptoms. The prevalence rates of mental health disorders and associated risk factors will be discussed in a subsequent manuscript.
To summarise, the research questions of this current study include:
1. What are current prevalence rates of mental health symptoms in 11- to 18-year-olds in Singapore? What are the rates of comorbidity?
2. What are some sociodemographic risk factors of mental health symptoms?
3. How is adolescents’ resilience related to the presence (or absence) of mental health symptoms?
The YEAR Study is a cross-sectional epidemiological study (September 2018 – present). A school-based study design was chosen as most typically developing children in Singapore are in the public education system. According to data from The United Nations Educational, Scientific and Cultural Organization (UNESCO), 99.4% of all Singaporean children were enrolled in primary education in 2021 (22). The school-based approach also maximises the response rate by leveraging the organisational structure. The sampling frame consisted of 40 schools stratified by level; primary, secondary and post-secondary, zone, and type, excluding special education schools. 16,000 students aged 11-18 and their parents were randomly selected and approached to participate in the study. The sample was designed to be nationally representative of the mainstream school-going population in terms of sex, ethnicity, father’s education level, mother’s education level and housing type. Physical or Electronic Participant Information Sheets and Consent forms were distributed to the invited students, and consent from parent and assent from child was taken. 20.9% (n = 3336) of the invited students consented to the study. The consent rate is in line with other national school studies conducted during the COVID-19 pandemic.
Survey information was gathered after consent taking in two-stages: initial questionnaire assessment, and subsequent in-person diagnostic interview of screened high-risk participants and controls. In Stage 1, consented students completed the online questionnaires either in school or at home. To assure the quality of data collected, members of the research team were present during the school screenings and closely supervised the survey respondents. For respondents with clarifications on the questionnaire, study team members were present and assisted them accordingly during in-person school screenings. For online screenings, respondents were able to clarify any queries via a chatbot manned by a study team member. The questionnaire was also pilot-tested in a smaller sample of school-going adolescents of the same age range to ensure readability. 2475 consented parents and 958 consented teachers of the respective students completed a battery of questionnaires (see Appendix). To identify subjects for Stage 2, the procedure described by Verhulst & Van der Ende (23) was adapted. The average 75th percentile of the cumulative frequency distribution of the mean screening z-scores of the child’s Youth Self-Report (YSR) Total Problem score was used as a cutoff score to select participants. Individuals who scored in the top 25th percentile, as well as the first 100 of the 10% of the remaining with normal scores were selected and invited to receive the semi-structured Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime Version (K-SADS-PL) screen interview and complete a battery of questionnaires (see Appendix). The stage 2 sample comprised of 474 adolescents. Consented parents and adolescents were interviewed either face-to-face or online separately. Interviewers were trained by an external trainer from the University of Pittsburgh, where the K-SADS was developed. Interviews were audio-recorded and randomly reviewed by a senior research team member for quality assurance. This manuscript only reports findings from stage 1.
All the participants who reported either having had thoughts or intention to harm or kill themselves on the YSR were contacted and invited for the Stage 2 interview as a safety protocol. For those who were found to be at-risk during the interview, a list of counselling hotlines and resources was provided for them to seek help. This included several outpatient and community services. Interviewers also suggested approaching school counsellor/counselling services. If the parent and child had further enquiries or consented to a referral, the team would recommend other private practitioners or facilitate the referral to school counsellors or REACH services – a community-based mental healthcare service for students. For at-risk participants who declined to participate in the interview or were uncontactable, a brochure with self-care resources was provided via email.
The Youth Self-Report (YSR) and Child Behavior Checklist for Ages 6 to 18 (CBCL) are established measures of emotional and behavioural problems among adolescents. The items within the two questionnaires mirror each other; while the YSR is completed by the adolescent, the CBCL is rated by their parent. The YSR and CBCL consist of 112 and 113 items respectively, scored based on experiences in the past six months according to a 3-point Likert scale: 0 (Not True), 1 (Somewhat or Sometimes True), and 2 (Very and Often True). The ratings are summarised in three broad composite scores (total problems score, internalizing problem score, and externalizing problem score), with eight empirically-derived subscale scores (i.e., anxious/depressed, depressed/withdrawn, somatic complaints, attention problems, social problems, thought problems, aggressive behavior, and rule-breaking behavior). Separately, the data can also be presented and analysed using six DSM-oriented scales (i.e., affective, anxiety, somatic, attention-deficit hyperactive, oppositional-defiant, and conduct problems). The good validity and reliability of the YSR and CBCL are well documented by Achenbach & Rescorla (24). In this study, Cronbach’s αs for the internalizing, externalizing and total problems scales were 0.78, 0.87 and 0.73 respectively for the YSR. For the empirically-derived scales, Cronbach’s αs ranged from 0.71 to 0.87. For the DSM-oriented scales, Cronbach’s αs ranged from 0.70 to 0.83. For the CBCL, good internal consistencies for the composite scales were reported (α = 0.89; 0.89; 0.93 for internalizing, externalizing and total problems respectively). For the empirically-derived scales, Cronbach’s αs ranged from 0.69 to 0.86. For the DSM-oriented scales, Cronbach’s α ranged from 0.63 to 0.80.
The YSR and CBCL can also be categorised into three severity ranges – normal, borderline and clinical – using cut-offs based on international norms. Scores in the normal range are considered within typical range of adolescents’ functioning. Scores in the borderline category suggest a higher risk of mental health problems but are not within clinical range. Scores in the clinical range indicate mental health problems comparable to those referred for professional help within mental health services. The terminology used in this manuscript has been aligned with the instrument manual (24) for the YSR and CBCL, for purpose of consistency.
The Singapore Youth Resilience Scale (SYRESS) is a self-reported, 50-item scale that measures the multidimensional construct of resilience among Singaporean adolescents, constructed and validated based on the contextual and cultural aspects of the Singaporean adolescent population. Comprising of 10 domains – Perseverance/commitment, Positive Self-Image/Optimism, Relationship/Social Support, Humour/Positive Thinking, Emotional Regulation, Spirituality/Faith, Personal Confidence/Responsibility, Personal Control, Flexibility, and Positive Coping, the good validity and reliability of the SYRESS was documented by Lim et al. (25). In this study, the Cronbach α for the overall scale was 0.95. The Cronbach’s α for most of the subscales ranged from 0.43-0.85. The items are rated on a 5-point Likert scale: 1 (Never), 2 (Sometimes), 3 (About half the time), 4 (Most of the time) and 5 (Always).
English versions of the above scales were used in this study.
Sociodemographic factors were sex (male or female), age, ethnicity, type of housing and parent’s highest level of education, parent’s gender, presence of domestic helper (present/absent), household composition, number of siblings, and child’s medical conditions.
Age was categorised as the following: 11-12, 13-14, 15-16, 17-18. Ethnicity was categorised as: Chinese, Malay, Indian or Other (comprises ethnicities not listed in the first three categories). For type of housing, the categories are Housing and Development Board (HDB) 1-, 2-, or 3-room flat, 4-, 5-room or executive flat, condominiums or other apartments, and landed property. HDB flats are public housing flats built by the Singapore government for Singaporeans and Permanent Residents. Executive flats contain an easily convertible additional space (e.g., balcony) compared to other HDB flats. The categories of the parent’s highest education level are adapted from the Singapore Standard Educational Classification (SSEC) – Primary, Secondary, Post-secondary, Diploma and Professional Attainment, and University. Post-secondary refers to non-tertiary general and vocational education level, such as junior colleges and national Institute of Technical Education certificates (NITECs). Diploma and professional attainment may include polytechnic diplomas and qualifications awarded by professional bodies. University level refers to Bachelor’s, Master’s or Doctorate degrees or postgraduate diploma or certificates. Household composition was categorised as 2 parents + child(ren), 1 parent + child(ren), parent(s) + child(ren) + grandparent(s), and Grandparent(s) + Child(ren) or Others. Child medical conditions surveyed were asthma, diabetes, being overweight and underweight.
All consented participants were assigned a non-identifiable ID. Subsequently, collected data were anonymised using their non-identifiable ID to protect participant privacy and confidentiality. To minimise transcription errors in data collection and processing, an online survey platform (Qualtrics) was used to record all responses.
Data were analysed using IBM Statistical Package for the Social Sciences (SPSS, version 29.0.1.0). Descriptive analyses were conducted to derive percentages of individuals who fell in the normal, borderline, and clinical ranges on the YSR and CBCL, as well as the sociodemographic breakdown for individuals who met clinical range cut-offs for the DSM-oriented scales of the YSR and CBCL. Borderline and clinical range cut-offs used were Group 2 norms derived and advised by Achenbach & Rescorla (26) for countries who have yet to derive their own norms. To better reflect the general population distribution, prevalence estimates for the CBCL were weighted to adjust for sex, type of housing and parent’s highest education level (27). Prevalence estimates for the YSR were weighted to adjust for sex. Binary logistic regression analyses were conducted to examine the association between sociodemographic variables and the DSM-oriented YSR and CBCL scales, as well as the association between sociodemographic variables and the presence of comorbidity. Only certain sociodemographic variables were included in the logistic regression analyses due to multicollinearity, namely age, sex, ethnicity, type of housing and parent’s highest education level. For the DSM-oriented scales, oppositional-defiant and conduct problems were grouped into one variable in regression analyses, as they lie on the same diagnostic spectrum. Comorbidity was operationalised as meeting the clinical cut-off for more than one of the five DSM-oriented scales. Non-parametric correlation analyses were conducted to examine the association between adolescent problem scores on the broad-band YSR scales and resilience scores.
Table 1 depicts the sociodemographic distribution of the sample. In comparison with national data, the demographic profile of the YEAR Study is largely representative of the adolescent and the population demographic distribution in the general population in terms of age and ethnicity, in comparison with data from the Department of Statistics of Singapore. Sex, housing type and parents’ highest level of education were not proportionally representative of the local adolescents’ population profile based on comparison with Department of Statistics data.
Table 2 shows the unweighted and weighted prevalence of mental health symptoms in the population based on adolescent self-report using the YSR, and parent report using the CBCL. On the YSR, internalizing problems were most prevalent, with 37.3% adolescents meeting the clinical cut-off, compared to externalizing and total problems (13.1% and 27.7% respectively). Under the empirically-derived YSR subscales, 20.3% of adolescents had scores in the clinical range on the anxious/depressed scale, 14.5% on the withdrawn/depressed scale, and 15.1% with social problems scores in the clinical range. For the DSM-oriented scales, 41.5% of adolescents had anxiety problems scores in the clinical range, followed by 15% who had affective problems in the clinical range. On the CBCL, internalizing problems were most prevalent, with 15.9% adolescents meeting the clinical range cut-off, compared to externalizing and total problems (4.0% and 11.2% respectively). 6.5% of adolescents had scores in the clinical range on the somatic problems scale, followed by 5.0% who had anxious/depressed scores in the clinical range. For the DSM-oriented scales, 15.9% of adolescents had anxiety problems scores in the clinical range, followed by 4.8% who had affective problems scores in the clinical range.
Table 3 illustrates the distribution of the prevalence of problem scores in the clinical range (as determined by the YSR and CBCL respectively) by age, sex, ethnicity, type of housing and parent’s highest educational level attained.
Tables 4 and 5 present the results of the logistic regression analyses examining the association between sociodemographic predictors and the prevalence of adolescents’ problems. These analyses were adjusted for demographics.
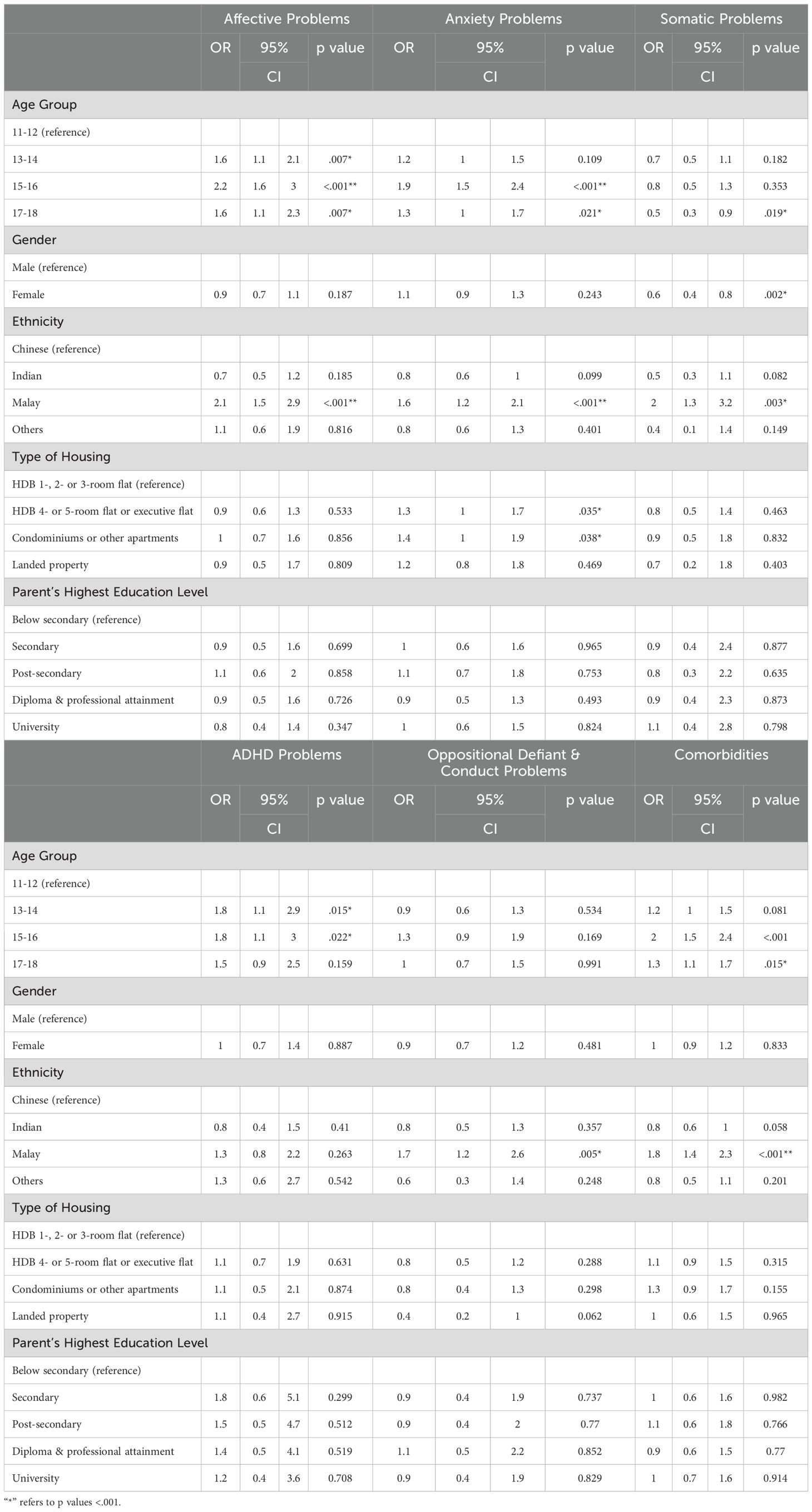
Table 4. Adjusted sociodemographic correlates for adolescents’ problems in the clinical range (YSR).
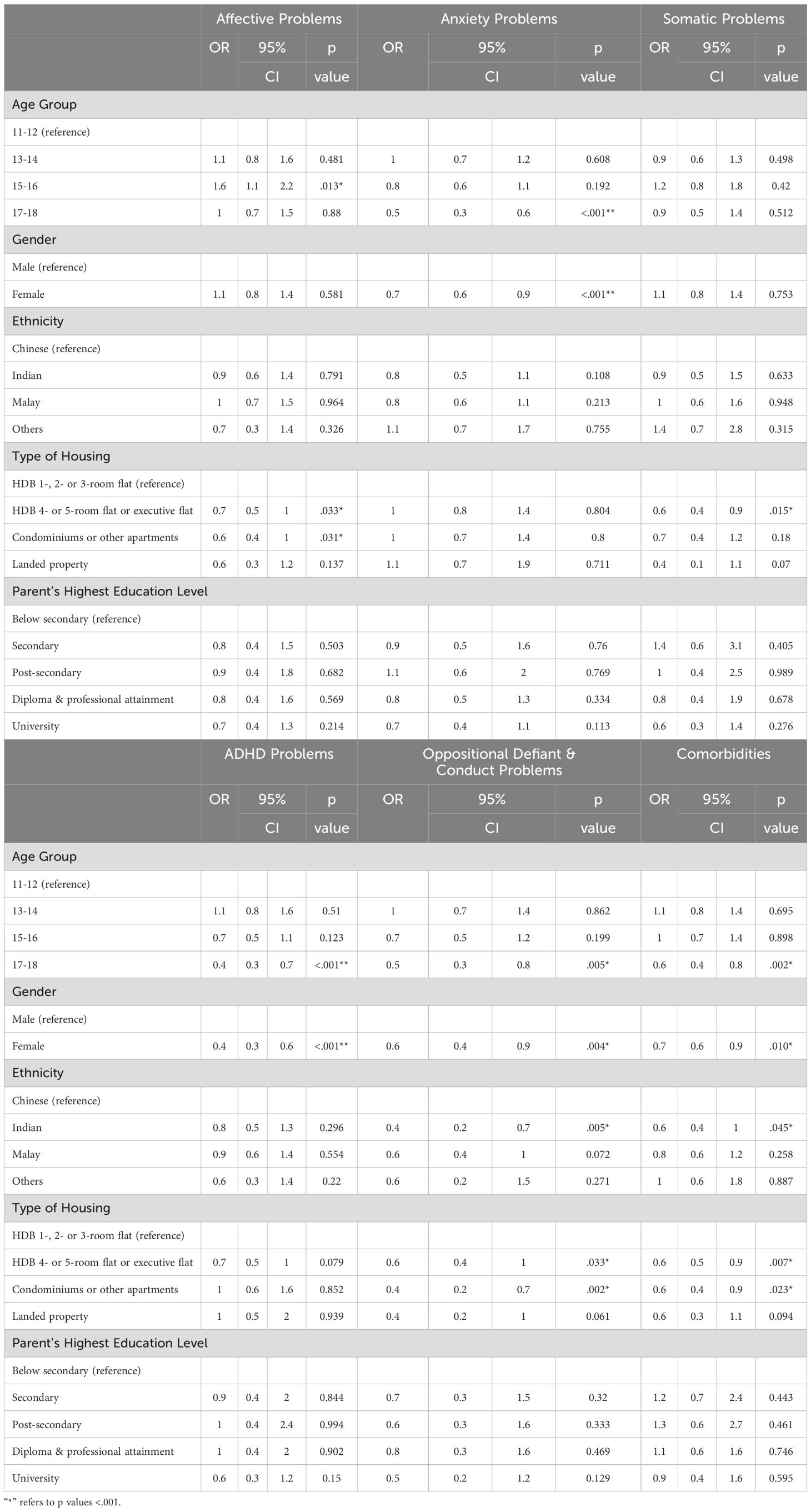
Table 5. Adjusted sociodemographic correlates for adolescents' problems in the clinical range (CBCL).
Based on the YSR, 15-16-year-olds were more likely to have affective (OR, 2.2; 95%CI, 1.6-3.0), anxiety (OR, 1.9; 95%CI, 1.5-2.4), and ADHD problems (OR, 1.8; 95%CI, 1.1-3.0) scores in the clinical range compared to 11-12-year-olds. They were also twice as likely to have comorbidities (95%CI, 1.5-2.4). 13-14-year-olds were more likely to have affective (OR, 1.6; 95%CI, 1.1-2.1) and ADHD problems scores in the clinical range (OR, 1.8; 95%CI, 1.1-2.9) compared to 11-12-year-olds. 17-18-year-olds were more likely to have affective (OR, 1.6; 95%CI, 1.1-2.3) and anxiety problems scores in the clinical range (OR, 1.3; 95%CI, 1.0–1.7) and comorbidities (OR, 1.3; 95%CI, 1.1-1.7), but less likely to have somatic problems (OR, 0.5; 95%CI, 0.3-0.9) compared to 11-12-year-olds. 15-16-year-olds had higher odds than other age groups for affective and anxiety problems, and of having comorbidities.
Females were less likely to have somatic problems than males (OR, 0.6; 95%CI, 0.4-0.8). The odds ratios for Malay adolescents were 2.1 (95%CI, 1.5-2.9) for affective problems, 1.6 (95%CI, 1.2-2.1) for anxiety problems, 2.0 (95%CI, 1.3-3.2) for somatic problems, 1.7 for oppositional defiant/conduct problems (95%CI, 1.2-2.6), and 1.8 (95%CI, 1.4-2.3) for comorbidities. Adolescents staying in a 4-5 room or executive flat (OR, 1.3; 95%CI, 1.0-1.7) and in condominiums or other apartments (OR, 1.4; 95%CI, 1.0-1.9) had higher odds of having anxiety problems in the clinical range compared to those staying in a 1-, 2- or 3-room flat.
Based on the CBCL, 17-18-year-olds had lower odds of having anxiety (OR, 0.5; 95%CI, 0.3-0.6), ADHD (OR, 0.4; 95%CI, 0.3–0.7) and oppositional defiant/conduct problems in the clinical range (OR, 0.5; 95%CI, 0.3-0.8) and comorbidities (OR, 0.6; 95%CI, 0.4-0.8) compared to 11-12-year-olds. 15-16-year-olds had higher odds of having affective problems (OR, 1.6; 95%CI, 1.1-2.2) than 11-12-year-olds.
Females had lower odds of having anxiety (OR, 0.7; 95%CI, 0.6-0.9), ADHD (OR, 0.4; 95%CI, 0.3-0.6) and oppositional defiant/conduct problems in the clinical range (OR, 0.6; 95%CI, 0.4-0.9) and comorbidities (OR, 0.7; 95%CI, 0.6-0.9) than males. Indian adolescents had lower odds of having oppositional defiant/conduct problems in the clinical range (OR, 0.4; 95%CI, 0.2-0.7) and comorbidities (OR, 0.6; 95%CI, 0.4-1.0) than Chinese adolescents. Adolescents staying in a 4-5 room or executive HDB flat had lower odds of having affective (OR, 0.7; 95%CI, 0.5-1.0), somatic (OR, 0.6; 95%CI, 0.4-0.9) or oppositional defiant/conduct problems in the clinical range (OR, 0.6; 95%CI, 0.4-1.0) and comorbidities (OR, 0.6; 95%CI, 0.5-0.9) than those staying in a 1-, 2- or 3-room flat. Adolescents staying in condominiums or other apartments also had lower odds of having affective (OR, 0.6; 95%CI, 0.4-1.0) and oppositional defiant/conduct problems (OR, 0.4; 95%CI, 0.2-0.7) in the clinical range and comorbidities (OR, 0.6; 95%CI, 0.4-0.9) than those staying in a 1-, 2- or 3-room flat.
Table 6 presents the results of the Spearman rank-order correlation analyses examining the association between adolescent’s clinical mental health symptoms (as measured by the YSR) and resilience levels. Moderate correlations were observed between total resilience scores and internalizing problem scores [rs(3334) = -.50, p <.01], and between total resilience scores and total problem scores [rs(3334) = -.49, p <.01], while the correlation between total resilience scores and externalizing problem scores was relatively weaker [rs(3334) = -.35, p <.01]. The resilience domains that displayed the highest negative correlations with total and internalizing problem scores were: Positive Self-Image/Optimism [rs(3334) = -.54, p <.01; rs(3334) = -.58, p <.01], Personal Control [rs(3334) = -.48, p <.01; rs(3334) = -.52, p <.01], Relationship/Social Support [rs(3334) = -.47, p <.01; rs(3334) = -.47, p <.01] and Emotional Regulation [rs(3334) = -.41, p <.01; rs(3334) = -.43, p <.01].
The YEAR Study is a school-based epidemiology study conducted in a multi-ethnic, Asian city-state that surveys mental health symptoms in school-based adolescents aged 11-18, and thus, its findings on the prevalence of mental health symptoms, the role of resilience and sociodemographic correlates bear important implications for policymaking, preventive efforts and targeted interventions.
Based on the YSR, 37.3%, 13.1% and 27.7% of the YEAR Study population scored in the clinical range for internalizing, externalizing and total problems respectively. In comparison to recent studies in Asia, a longitudinal cohort study conducted among Korean students from two middle schools’ representative of the Korean middle school youth population reported prevalence figures of 8.2% and 7.4% for internalizing and externalizing symptoms respectively on the YSR (28). Cui et al. (29)’s national study among Chinese adolescents reported that 17.6% of the study population, representative of the mainland Chinese population, had total problems in the clinical range on the CBCL. No other recent Asian studies were available for comparison. Among other national studies published within the last 10 years, such as in Kosovo (30), Kenya (31), Brazil (32), and Italy (33), the YEAR Study similarly reports the highest prevalence rate of total problem scores and internalizing problem scores in the clinical range. In contrast, the YEAR Study has the lowest prevalence rates of externalizing problems. For the problem subscales, the YEAR study similarly reports the highest prevalence rate in comparison to the studies done in Kosovo, Brazil, and Italy, apart from rule-breaking and aggressive problems, on which the YEAR study holds one of the lowest rates. It should be noted that inter-country comparisons should be interpreted in light of varying contextual factors (e.g., rural vs. urban, different social cultural contexts), and the fact that YEAR study collected data during the COVID-19 pandemic period.
Given Singapore’s unique multi-ethnic and cultural context, some possible explanations of the higher prevalence of internalizing symptoms among Singaporean adolescents may include the high value of academic excellence (from one’s parents or self) inherent in Singaporean, and more broadly, East Asian society. The positive association between academic stress and conditions such as anxiety and depression has been widely explored in past literature (34–36); especially with regards to East Asian societies such as Singapore, China, Korea, Taiwan, Hong Kong and Japan, where the Confucian values of hard work and filial piety hold greater influence (37). In such societies, academic stress often stems from the perception of academic excellence as an obligation towards one’s family, with failure of attainment resulting in familial shame (38). Moreover, when examining sociodemographic correlates, adolescents aged 15-16 had higher odds of having affective and anxiety problems than all other age groups. In Singapore, school-attending adolescents are required to sit for national examinations at age 16, which are perceived as highly crucial in determining one’s post-secondary academic track (Junior College, Polytechnic, Institute of Technical Education, etc.) and subsequent longer term career prospects. Thus, the above finding lends further weight to the role of academic stress in adolescents in predicting internalizing mental health problems.
Another contributing factor may be rooted in the historical narrative and account of Singaporean history legitimised by the Singaporean government, referred to as the ‘Singapore Story’ (39). The historical narrative underscores the vulnerability surrounding Singapore’s early days, characterised by stress and a pervasive drive for survival. Propagated via national education initiatives, this “ideology of survival” (40) – of perseverance and determination to thrive – remains embedded in Singaporean psyche, potentially influencing the Singaporean strive, including academic, and the association with high internalizing problems observed in the adolescent population.
The relatively low prevalence of externalizing problems in Singaporean adolescents compared to adolescents from other countries corroborates estimates presented in earlier studies (41, 42). This finding may be explained by the collectivistic nature of Asian societies which tends to prize behaviour that favours social harmony and interdependence, and frowns upon disruptive behaviour (43). Furthermore, the formal and informal forms of social control (e.g., stringent laws, family values, religious influence, economic stability etc.) inherent in Singaporean society likely contributes to the lower prevalence of externalizing behaviours (44).
13-14, 15-16 and 17-18-year-olds were all observed to have higher risk of affective and anxiety problems as compared to 11-12-year-olds. 15-16-year-olds had the highest risk compared to the other age groups of affective and anxiety problems, and comorbidities. As explicated above, this finding may reflect the academic stress accompanying a “high-stakes” year. However, as this trend has also been observed in other countries (30, 32), these findings may also be partially explained by the effects of pubertal development. Studies have generally observed depression levels and psychosocial stresses to increase with pubertal development (45). It was also observed that 17-18-year-olds were less likely to have somatic problems scores in the clinical range than 11-12-year-olds, in contrary to findings from previous studies, where somatic symptoms were generally found to increase with age among adolescents (46–48). A study by Feraco and Meneghetti (49) found emotional resilience skills (e.g., stress and impulse regulation) to increase with age (12–19), perhaps indicating the increased capability of older adolescents to understand and express their emotions rather than somatise. However, the Dutch TRAILS Study also reported a decline in somatic symptoms with age (50). Further research is needed to better understand these mixed findings.
In contrast to previous findings (51, 52), females were less likely than males to have somatic problems. Apart from somatic problems, males and females did not significantly differ on the likelihood of having clinical mental health symptoms. A similar finding was observed in the Singapore Mental Health Study (SMHS) – another local epidemiological study on the adult (18 and above) population, where sex was not found to be associated with mental health disorders such as Major Depressive Disorder (MDD) and Generalised Anxiety Disorder (GAD). Historically, females have demonstrated higher risk of MDD (53), but recent findings seem to demonstrate a rising trend of internalizing symptoms among males – as reported by the SMHS, the national prevalence of MDD in males was reported to have increased from 4.3% in 2010 to 5.6% in 2016, perhaps suggesting an increased awareness of mental health struggles among males (9).
Malay adolescents were found to have higher odds in reporting affective, anxiety, somatic and opposition defiant/conduct problems in the clinical range as well as comorbidities, the most pronounced difference being that of affective problems. This finding was observed even after accounting for all other predictors, namely age, sex and our proxy indicators of socioeconomic status (type of housing, parent’s highest qualification). The SMHS also observed higher odds of obsessive-compulsive disorder among Malays (9). However, Malays were also found to have the lowest lifetime risk of at least one mental health disorder (54) and suicide risk (55) compared to other ethnic groups. At this juncture, we do not have any explanation for these mixed findings, and further research is needed to identify the exact cause to further elucidate the unique needs for adolescents of this ethnic group.
Adolescents who lived in a 4-, 5-room or executive flat as well as those who lived in condominiums or other apartments were more likely to have anxiety problems in the clinical range on the YSR. In 2022, the average monthly household income ranged from $9,200-19,936 for those that lived in the above household types (56), representing the middle to higher income categories in Singapore. Although higher socioeconomic status has historically been associated with positive mental health outcomes (57), past literature suggests that parents of a higher socioeconomic status tend to have higher educational expectations of their children (58, 59), which as explicated previously, likely translates to higher academic stress and higher anxiety. Furthermore, relatively affluent children who experience overbearing demands to achieve and parental neglect are thought to be at higher risk of developing anxiety, depression or substance abuse issues (60).
The prevalence rates of mental health symptoms reported by adolescents and their parents using the YSR and CBCL respectively showed differences across the different problems. For instance, 11.2% of parents reported mental health distress of clinical levels in their adolescents, compared to 27.7% based on adolescent report. Similarly, for other scales, prevalence rates derived from parent report were consistently observed to be lower than adolescent-reported rates, this being especially pronounced for depressive and anxiety symptoms. Further analysis such as correlation analyses need to be conducted to interrogate the extent of the discrepancy in reporting.
Differences in reporting between parent and child have been observed in other studies (61–63); studies have identified the quality of the parent-child relationship – parental engagement, communication and acceptance – as one of the stronger predictors of parent-child discrepancies (64, 65). In addition, low mental health literacy among parents may be a contributing factor – a meta-analysis of local studies by Tonsing et al. (66) found the younger generation to possess a greater understanding of mental health conditions, as compared to older generations. Thus, parents could benefit from mental health literacy programs that increase their sensitivity in identifying mental health issues in their children. Moreover, the discrepancies may be the product of certain sociocultural experiences, which colour parental reports. For instance, parents of 17-18-year-olds may be less attuned to the emotional states of their older, more independent adolescents (as compared to 11-12-year-olds).
Consistent with the extant literature (18, 19, 67), higher resilience scores were observed in this study to be negatively correlated with higher psychopathology score – in a meta-analysis of 60 studies that examined the relationship between resilience and mental health indicators, the mean correlation between resilience and negative mental health indicators was r = -.36 (68). In addition to verifying existing findings on the inextricable link between resilience and mental health, this study identified four pertinent resilience facets: Positive Self-Image/Optimism, Personal Control, Relationship/Social Support and Emotional Regulation, which inversely correlate with YSR scores and could serve as protective factors against mental health symptoms measured by YSR. Further exploration into the protective, moderating effects of these resilience factors and how they can inform intervention targets will be discussed in a subsequent manuscript. For instance, resilience-based parent and teacher interventions were offered to parents and teachers in this current study. Using the theoretical framework underlying the Singapore Youth Resilience Scale (SYRESS), parenting and classroom management tips were shared in the form of a parenting guide and workshops for teachers based on the 10 resilience facets, to inculcate and bolster resilience in adolescents.
The YEAR study population is reflective of school-going age students in a multi-ethnic Asian population. With its stratified sampling design based on the national student database, its findings on mental health symptoms serve as a reflective benchmark of student mental health in a city-state. Internalizing symptoms are observed to be a key feature of mental health distress in this study population.
This study was conducted in the context of the COVID-19 pandemic, during which social distancing measures was implemented nationwide, and classes were suspended for three months. The pandemic disrupted daily routines and could have amplified the prevalence of anxiety and mood symptoms. The data collection was also suspended when the social distancing measures were enforced, and only resumed after the schools resumed classroom lessons.
The 20.9% response rate of a stratified representative sample may contribute towards a selection bias, as consenting participants may have been more willing to share about their mental health, while those with mental health difficulties may also avoid participating due to perceived stigmatisation from mental health difficulties. This was mitigated by confidentiality and anonymity of responses being explained to participants during the consent-taking process. The consent rate is also in line with other national studies conducted in schools during the COVID-19 pandemic.
Importantly, the respondent population is similar in demographic and educational profile to the national youth population of equivalent age range, though the study population tends to reflect a slightly higher parent’s highest educational level and housing type, which may be protective factors for mental health disorders as found in other studies (57).
Lastly, this study’s cross-sectional design provides a good time-in-point prevalence, but is unable to illustrate cause-effect relationships between study factors.
The present study illustrates the state of mental health and resilience of Singaporean school-going adolescents aged 11-18, against the backdrop of the COVID-19 pandemic. The relatively high prevalence of internalizing symptoms in Singaporean adolescents, coupled with the reported lower prevalence by parents, warrants greater efforts in increasing literacy among both adolescents and their parents. Furthermore, there exists a need for targeted interventions aimed at those with higher risk of clinical mental health symptoms, such as those belonging to the age category of 15-16. It would be helpful for future prevalence studies to be conducted, so as to determine whether the current prevalence estimates are unique as a result of the pandemic context, or whether they are representative baseline estimates. At the same time, its examination of the associations of mental health symptoms with resilience factors highlights the protective potential of resilience building for children and adolescents.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by National University of Singapore Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
JW: Conceptualization, Methodology, Supervision, Project Administration, Funding Acquisition, Writing – original draft, Writing – review & editing. NL: Investigation, Data Curation, Formal analysis, Writing - original draft, Writing – review & editing. DK: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. VF: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. NY: Investigation, Data Curation, Writing – original draft, Writing – review & editing. JT: Investigation, Data Curation, Writing – original draft, Writing – review & editing. LS: Formal analysis, Data Curation, Writing – original draft, Writing – review & editing. QY: Formal analysis, Data Curation, Writing – original draft, Writing – review & editing. MW: Investigation, Data Curation, Writing – original draft, Writing – review & editing. RD: Formal analysis, Data Curation, Writing – original draft, Writing – review & editing. LK: Conceptualization, Methodology, Funding Acquisition, Writing – original draft, Writing – review & editing. DF: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing. SO: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. CT: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. MB: Investigation, Data Curation, Writing – original draft, Writing – review & editing. NS: Investigation, Data Curation, Writing – original draft, Writing – review & editing. JT: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. TN: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. FV: Conceptualization, Methodology, Writing – original draft, Writing – review & editing
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Mind-Science Centre Seed Grant and the Singapore Tote Board.
The study team would like to acknowledge the efforts of the Ministry of Education, Singapore in contributing to the successful conduct of the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. (2018) 2:223–8. doi: 10.1016/S2352-4642(18)30022-1
2. Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. (2008) 9:947–57. doi: 10.1038/nrn2513
3. World Health Organisation (WHO). Mental health of adolescents (2021). World Health Organisation. Available online at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (Accessed 5 Sep 2023).
4. Pang S, Liu J, Mahesh M, Chua BY, Shahwan S, Lee SP, et al. Stigma among Singaporean youth: a cross-sectional study on adolescent attitudes towards serious mental illness and social tolerance in a multiethnic population. BMJ Open. (2017) 7:e016432. doi: 10.1136/2Fbmjopen-2017-016432
5. Aguirre Velasco A, Cruz IS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. (2020) 20:1–22. doi: 10.1186/s12888-020-02659-0
6. Kutcher S, Wei Y, Coniglio C. Mental health literacy: Past, present, and future. Can J Psychiatry. (2016) 61:154–8. doi: 10.1177/0706743715616609
7. Chodavadia P, Teo I, Poremski D, Fung DS, Finkelstein EA. Prevalence and economic burden of depression and anxiety symptoms among Singaporean adults: results from a 2022 web panel. BMC Psychiatry. (2023) 14:104. doi: 10.1002/mpr.281
8. Subramaniam M, Vaingankar J, Heng D, Kwok KW, Lim YW, Yap M, et al. The Singapore Mental Health Study: an overview of the methodology. Intl J Methods Psychiatr Res. (2012) 21:149–57. doi: 10.1002/mpr.1351
9. Subramaniam M, Abdin E, Vaingankar JA, Shafie S, Chua BY, Sambasivam R, et al. Tracking the mental health of a nation: prevalence and correlates of mental disorders in the second Singapore mental health study. Epidemiol Psychiatr Sci. (2019) 29:e29. doi: 10.1017/S2045796019000179
10. Rothen S, Vandeleur CL, Lustenberger Y, Jeanprêtre N, Ayer EV, Gamma F, et al. Parent–child agreement and prevalence estimates of diagnoses in childhood: direct interview versus family history method. Int J Methods Psychiatr Res. (2009) 18:96–109. doi: 10.1002/mpr.281
11. Patel V, Goodman A. Researching protective and promotive factors in mental health. Int J Epidemiol. (2007) 36:703–7. doi: 10.1093/ije/dym147
12. Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
13. Brooks JE. Strengthening resilience in children and youths: Maximizing opportunities through the schools. Child Sch. (2006) 28:69–76. doi: 10.1093/cs/28.2.69
14. Masten AS. Ordinary magic: Resilience processes in development. Am Psychol. (2001) 56:227–38. doi: 10.1037//0003-066x.56.3.227
15. Masten AS, Barnes AJ. Resilience in children: developmental perspectives. Children (Basel). (2018) 5:98. doi: 10.3390/children5070098
16. Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. (2018) 8:e017858. doi: 10.1136/2Fbmjopen-2017-017858
17. Mesman E, Vreeker A, Manon H. Resilience and mental health in children and adolescents: an update of the recent literature and future directions. Curr Opin Pyschiatry. (2021) 34:586–92. doi: 10.1097/2FYCO.0000000000000741
18. Hjemdal O, Vogel PA, Solem S, Hagen K, Stiles TC. The relationship between resilience and levels of anxiety, depression, and obsessive-compulsive symptoms in adolescents. Clin Psychol Psychother. (2011) 18:314–21. doi: 10.1002/cpp.719
19. Haddadi P, Besharat MA. Resilience, vulnerability and mental health. Proc Soc Behav Sci. (2010) 5:639–42. doi: 10.1016/j.sbspro.2010.07.157
20. Song S, Yang X, Yang H, Zhou P, Ma H, Teng C, et al. Psychological resilience as a protective factor for depression and anxiety among the public during the outbreak of COVID-19. Front Psychol. (2021) 11:618509. doi: 10.3389/fpsyg.2020.618509
21. Johnson J, Wood AM, Gooding P, Taylor PJ, Tarrier N. Resilience to suicidality: The buffering hypothesis. Clin Psychol Rev. (2011) 31:563–91. doi: 10.1016/j.cpr.2010.12.007
22. The UNESCO Institute for Statistics (UIS), The United Nations Educational, Scientific and Cultural Organization (UNESCO). Other policy relevant indicators: Total net enrolment rate by level of education (n.). Available online at: http://data.uis.unesco.org/index.aspx?queryid=3813. (Accessed September 5, 2023)
23. Verhulst FC, van der Ende J. Factors associated with child mental health service use in the community. J Am Acad Child Adolesc Psychiatry. (1997) 36:901–9. doi: 10.1097/00004583-199707000-00011
24. Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families (2001).
25. Lim ML, Broekman BF, Wong JC, Wong ST, Ng TP. The development and validation of the Singapore Youth Resilience Scale (SYRESS). In: Broekman BF, editor. Stress, vulnerability and resilience: a developmental approach. Dissertation, University of Amsterdam Amsterdam, Netherlands: University of Amsterdam (2007).
26. Achenbach TM, Rescorla LA. Multicultural Supplement to the Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families (2007).
27. Kalsbeek W, Heiss G. Building bridges between populations and samples in epidemiological studies. Annu Rev Public Health. (2000) 21:147–69. doi: 10.1146/annurev.publhealth.21.1.147
28. Kim DH, Kim YS, Koh YJ, Leventhal BL. Relationship between behaviour problems and perceived parenting practices in Korean youth. Child Care Health Dev. (2013) 39:194–201. doi: 10.1111/j.1365-2214.2011.01343.x
29. Cui Y, Li F, Leckman JF, Guo L, Ke X, Liu J, et al. The prevalence of behavioral and emotional problems among Chinese school children and adolescents aged 6–16: a national survey. Euro Child Adolesc Psychiatry. (2015) 30:233–41. doi: 10.1007/s00787-020-01507-6
30. Shahini M, Rescorla L, Wancata J, Ahmeti A. Mental health problems in Kosovar adolescents: results from a national mental health survey. Neuropsychiatr. (2015) 29:125–32. doi: 10.1007/s40211-015-0155-9
31. Ndetei DM, Mutiso V, Gitonga I, Agudile E, Tele A, Birech L, et al. World Health Organization life-skills training is efficacious in reducing youth self-report scores in primary school going children in Kenya. Early Interv Psychiatry. (2019) 13:1146–54. doi: 10.1111/eip.12745
32. da Silva Cristovam MA, Muzzolon SR, dos Santos LH. Application of youth self-report for age 11-18 for screening of mental disorders in the adolescence. Mathews J Pediatr. (2019) 4:1–9. doi: 10.30654/MJP.10019
33. Lisi G, Rossi R, Ribolsi M, Di Lorenzo G, Parisi C, Siracusano M, et al. [amp]]lsquo;Too many BeEPs in our teens!’ Behavioral and emotional problems in a large group of Italian adolescents. Psychol Med. (2022) 52:1040–9. doi: 10.1017/s0033291720002767
34. Jayanthi P, Thirunavukarasu M, Rajkumar R. Academic stress and depression among adolescents: A cross-sectional study. Indian Pediatr. (2015) 52:217–9. doi: 10.1007/s13312-015-0609-y
35. Ang RP, Huan VS. Relationship between academic stress and suicidal ideation: Testing for depression as a mediator using multiple regression. Child Psychiatry Hum Dev. (2006) 37:133–43. doi: 10.1007/s10578-006-0023-8
36. Stankov L. Unforgiving Confucian culture: A breeding ground for high academic achievement, test anxiety and self-doubt? Learn Individ Differ. (2010) 20:555–63. doi: 10.1016/j.lindif.2010.05.003
37. Tan JB, Yates S. Academic expectations as sources of stress in Asian students. Soc Psychol Educ. (2011) 14:389–407. doi: 10.1007/s11218-010-9146-7
38. Wong J, Salili F, Ho SY, Mak KH, Lai MK, Lam TH. The perceptions of adolescents, parents and teachers on the same adolescent health issues. Sch Psychol Int. (2005) 26:371–84. doi: 10.1177/0143034305055980
40. Seng LK. Within the Singapore story: The use and narrative of history in Singapore (1998) Crossroads: An Interdisciplinary Journal of Southeast Asian Studies, (1998) 1:1–21.
41. Woo BS, Ng TP, Fung DS, Chan YH, Lee YP, Koh JB, et al. Emotional and behavioural problems in Singaporean children based on parent, teacher and child reports. Singapore Med J. (2007) 48:1100.
42. Weisz JR, Sigman M, Weiss B, Mosk J. Parent reports of behavioral and emotional problems among children in Kenya, Thailand, and the United States. Child Dev. (1993) 64:98–109. doi: 10.1111/j.1467-8624.1993.tb02897.x
43. Stevenson HW. The development of prosocial behavior in large-scale collective societies: China and Japan. In R. A. Hinde & J. Grovel (Eds.), Cooperation Prosocial Behav. Cambridge, England: Cambridge University Press. (1991), 89–105.
44. Austin WT. Crime and custom in an orderly society: The Singapore prototype. Criminol. (1987) 25:279–94. doi: 10.1111/j.1745-9125.1987.tb00798.x
45. Jiang L, Yang D, Li Y, Yuan J. The influence of pubertal development on adolescent depression: the mediating effects of negative physical self and interpersonal stress. Front Psychiatry. (2018) 18:786386. doi: 10.3389/fpsyt.2021.786386
46. Ginsburg GS, Riddle MA, Davies M. Somatic symptoms in children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. (2006) 45:1179–87. doi: 10.1097/01.chi.0000231974.43966.6e
47. Campo JV. Annual Research Review: Functional somatic symptoms and associated anxiety and depression–developmental psychopathology in pediatric practice. J Child Psychol Psychiatry. (2012) 53:575–92. doi: 10.1111/j.1469-7610.2012.02535.x
48. Romero-Acosta K, Canals J, Hernández-Martínez C, Penelo E, Zolog TC, Domènech-Llaberia E. Age and gender differences of somatic symptoms in children and adolescents. J Ment Health. (2013) 22:33–41. doi: 10.3109/09638237.2012.734655
49. Feraco T, Meneghetti C. Social, emotional, and behavioral skills: age and gender differences at 12 to 19 years old (2023). J Intell. (2023) 11:118. doi: 10.1016/j.adolescence.2010.01.010
50. Oldehinkel AJ, Verhulst FC, Ormel J. Mental health problems during puberty: Tanner stage-related differences in specific symptoms. The TRAILS study. J Adolesc. (2011) 34:73–85. doi: 10.1016/j.adolescence.2010.01.010
51. Rehna T, Hanif R, Ali SZ. Life stress and somatic symptoms among adolescents: gender as moderator. J Pak Med Assoc. (2016) 66:1448–51.
52. van Geelen SM, Rydelius PA, Hagquist C. Somatic symptoms and psychological concerns in a general adolescent population: Exploring the relevance of DSM-5 somatic symptom disorder. J Psychosom Res. (2015) 79:251–8. doi: 10.1016/j.jpsychores.2015.07.012
53. Picco L, Subramaniam M, Abdin E, Vaingankar JA, Chong SA. Gender differences in major depressive disorder: findings from the Singapore Mental Health Study. Singapore Med J. (2017) 58:649. doi: 10.11622/smedj.2016144
54. Chong SA, Abdin E, Vaingankar JA, Heng D, Sherbourne C, Yap M, et al. A population-based survey of mental disorders in Singapore. Ann Acad Medicine-Singapore. (2012) 41:49. doi: 10.47102/annals-acadmedsg.
55. Mak KK, Ho CS, Chua V, Ho RC. Ethnic differences in suicide behavior in Singapore. Transcult Psychiatry. (2015) 52:3–17. doi: 10.1177/1363461514543545
56. Singapore Department of Statistics. Average Monthly Household Income from Work (Excluding Employer CPF Contributions) Among Resident Employed Households (2023). Available online at: https://tablebuilder.singstat.gov.sg/table/CT/17814 (Accessed 5 Sep 2023).
57. McLaughlin KA, Costello EJ, Leblanc W, Sampson NA, Kessler RC. Socioeconomic status and adolescent mental disorders. Am J Public Health. (2012) 102:1742–50. doi: 10.2105/2FAJPH.2011.300477
58. Zhang M, Hu Y, Hu Y. The influences of socioeconomic status on parental educational expectations: mediating and moderating effects. Sustainability. (2023) 15:12308. doi: 10.3390/su151612308
59. Renzulli L, Barr AB. Adapting to family setbacks: Malleability of students and parents’ educational expectations. Soc Probl. (2017) 64:351–72. doi: 10.1093/socpro/spw052
60. Luthar SS. The culture of affluence: Psychological costs of material wealth. Child Dev. (2003) 74:1581–93. doi: 10.1046/2Fj.1467-8624.2003.00625.x
61. Weissman MM, Wickramaratne P, Warner V, John K, Prusoff BA, Merikangas KR, et al. Assessing psychiatric disorders in children: Discrepancies between mothers’ and children’s reports. Arch Gen Psychiatry. (1987) 44:747–53. doi: 10.1001/archpsyc.1987.01800200075011
62. Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull. (1987) 101:213. doi: 10.1037/0033-2909.101.2.213
63. Salbach-Andrae H, Klinkowski N, Lenz K, Lehmkuhl U. Agreement between youth-reported and parent-reported psychopathology in a referred sample. Euro Child Adolesc Psychiatry. (2009) 18:136–43. doi: 10.1037/0033-2909.101.2.213
64. Van Roy B, Groholt B, Heyerdahl S, Clench-Aas J. Understanding discrepancies in parent-child reporting of emotional and behavioural problems: Effects of relational and socio-demographic factors. BMC Psychiatry. (2010) 10:1–2. doi: 10.1186/1471-244x-10-56
65. Bajeux E, Klemanski DH, Husky M, Leray E, Chan Chee C, Shojaei T, et al. Factors associated with parent–child discrepancies in reports of mental health disorders in young children. Child Psychiatry Hum Dev. (2018) 49:1003–10. doi: 10.1007/s10578-018-0815-
66. Tonsing KN. A review of mental health literacy in Singapore. Soc Work Health Care. (2018) 57:27–47. doi: 10.1080/00981389.2017.1383335
67. Eisman AB, Stoddard SA, Heinze J, Caldwell CH, Zimmerman MA. Depressive symptoms, social support, and violence exposure among urban youth: A longitudinal study of resilience. Dev Psychol. (2015) 51:1307. doi: 10.1037/2Fa0039501
68. Hu T, Zhang D, Wang J. A meta-analysis of the trait resilience and mental health. Pers Individ. (2015) 1:18–27. doi: 10.1016/j.paid.2014.11.039
Keywords: mental health, resilience, adolescence, epidemiology, demographics
Citation: Wong JCM, Lei NCL, Kom DMY, Fee VHF, Yap NH, Teoh JY, Shen L, Yap QV, Wan MJS, Du R, Kroneman L, Fung DSS, Ong SH, Tian CS, Bin Sachiman MNS, Sii NE-P, Teng JY, Ng TP and Verhulst F (2024) Youth Epidemiology and Resilience (YEAR) in a student population: prevalence and predictors of mental health symptoms. Front. Psychiatry 15:1454484. doi: 10.3389/fpsyt.2024.1454484
Received: 25 June 2024; Accepted: 03 October 2024;
Published: 01 November 2024.
Edited by:
Xinqiao Liu, Tianjin University, ChinaReviewed by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranCopyright © 2024 Wong, Lei, Kom, Fee, Yap, Teoh, Shen, Yap, Wan, Du, Kroneman, Fung, Ong, Tian, Bin Sachiman, Sii, Teng, Ng and Verhulst. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: John Chee Meng Wong, pcmwcmj@nus.edu.sg
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.