- 1Department of Psychiatry and Psychotherapy, Charité Campus Mitte, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany
- 2College of Pharmacy, Yonsei Institute of Pharmaceutical Sciences, Yonsei University, Incheon, Republic of Korea
Background: Insomnia is a prevalent disorder that impacts quality of life and leads to significant economic costs. Treatment includes both non-medication and pharmacological interventions, with international guidelines recommending cognitive behavioral therapy for insomnia (CBT-I) as the first-line treatment.
Objective: To describe current insomnia treatment practices in South Korea, focusing on pharmacological and non-medication treatments, and to identify gaps in guideline implementation.
Methods: This cohort study used data from the Korea National Health Insurance Service-National Sample Cohort (NHIS-NSC) from 2002 to 2019 and identified 18,003 patients newly diagnosed with insomnia between 2015 and 2019. This study analyzed treatment patterns and utilization rates.
Results: Of the 18,003 patients, 16,181 (89.9%) received pharmacological treatment, resulting in 35,638 prescriptions. Zolpidem (60%) and benzodiazepines (30-40%) were the most prescribed medications. Most patients were treated in clinics, with consistent dosages and increasing treatment lengths. Psychotherapy claims rose from 3.20% in 2015 to 9.14% in 2019, particularly in general hospitals (22.06% to 48.37%), but remained low in clinics (1.26% to 2.08%).
Conclusion: Pharmacological treatments dominate insomnia management in South Korea, with CBT-I being underutilized. Future efforts should focus on integrating non-pharmacological treatment into routine practice and exploring treatment risks and effectiveness based on patient demographics.
1 Introduction
Insomnia is clinically diagnosed based on complaints of difficulty falling asleep, staying asleep, or waking up too early, coupled with resulting daytime dysfunction, despite having adequate opportunity for sleep (1, 2). This condition is prevalent, affecting approximately 10% of the general population (3, 4), with current estimates ranging up to 20% (5). In South Korea, the prevalence of sleep disorders has significantly increased, rising from 8% in 2011 to 14% in 2020, nearly doubling over a decade (6). Insomnia is a recognized risk factor for several serious health issues, including depression, anxiety disorders, substance use disorders, suicidality, hypertension, and metabolic syndrome, and it significantly impacts quality of life (7–14). The functional consequences of insomnia are considerable, leading to reduced productivity, increased absenteeism, increased use of healthcare services, and a greater risk of accidents, all of which contribute to substantial economic costs (15, 16).
When a patient is diagnosed with insomnia, treatment can be initiated with a variety of interventions categorized broadly into non-medication treatments and pharmacological therapies. General management includes addressing comorbid medical and psychiatric conditions, modifying sleep-interfering medications and substances, and optimizing the sleep environment (17, 18). International guidelines recommend cognitive behavioral therapy for insomnia (CBT-I) and insomnia medications as effective specific treatments for insomnia disorder (19–23).
Non-pharmacological treatment options for insomnia include relaxation therapy, biofeedback, and cognitive behavioral therapy for insomnia (CBT-I). Among the non-pharmacological treatment options, CBT-I is the most empirically supported and widely used. It is recommended by several clinical guidelines from South Korea, the USA, and Europe as the first-line treatment for adults with chronic insomnia (19–23). Typically delivered over four to seven sessions, it includes sleep hygiene education, cognitive restructuring, and behavioral interventions such as bedtime restriction and stimulus control (17, 24). Meta-analyses have demonstrated that CBT-I leads to significant improvements in insomnia symptoms, sleep efficiency, and sleep quality across a wide array of clinical populations (25–28). CBT-I has been shown to be equally effective in the short-term as medication-based therapies, with greater long-term maintenance of positive effects and minimal side effects (17, 27). It has been provided through various methods, such as individual and group in-person sessions, as well as digitally delivered therapy. Overall, all these approaches are effective, although some research indicates that face-to-face therapy has better outcomes (29–31). In July 2018, the South Korean Ministry of Health and Welfare implemented a policy change, expanding the national health insurance coverage to include various forms of psychotherapy, such as CBT. However, the lack of formal training, awareness among healthcare professionals, and availability of clinical staff limits the use of non-medication strategies such as CBT-I (32–35).
Pharmacological treatments for insomnia are widely accessible and often prescribed due to their immediate effect on sleep symptoms and ease of prescription (18). Commonly used medications include benzodiazepines and Z substances (36). However, these medications are associated with substantial adverse events, such as sedation, psychomotor impairment, and potential for abuse (18). Additionally, hypnotics are linked to an increased risk of falls, particularly in elderly patients, which is a significant concern given the widespread use of these medications in this population (37). Pharmacological treatments for insomnia have been evaluated primarily through short-term, placebo-controlled trials, and regulatory agencies have recently begun to require long-term data for medication approval (38, 39). As a result, pharmacological treatment is recommended mainly for the acute management of insomnia disorder and should not be the sole treatment for chronic insomnia (19–23). Furthermore, the comparative effectiveness of these medications remains unclear due to limited long-term evidence (40). An overview of the treatment guidelines for insomnia is presented in Table 1.
Despite the established guidelines, there is a significant gap in understanding how these recommendations are implemented in real-world settings in South Korea. This study aims to provide a comprehensive description of current insomnia treatment practices in South Korea, focusing on both pharmacological and non-medication treatments. This includes examining treatment patterns and utilization rates associated with different therapeutic approaches. By offering a detailed overview of existing practices, this study seeks to identify gaps in implementing clinical guidelines and highlight areas for potential improvement.
2 Methods
The study was approved by the Institutional Review Board of Yonsei University (202306-HR-3406-01) and was conducted in accordance with the Declaration of Helsinki. As the data used were deidentified and retrospective, informed consent was waived.
2.1 Study design and data source
This population-based cohort study utilized data from the Korea National Health Insurance Service-National Sample Cohort (NHIS-NSC) database from 2002 to 2019. Since the introduction of universal health coverage in 1989, approximately 97% of the population has been enrolled in the NHIS. Utilizing systemic stratified sampling based on sex, age, residential location, insurance premium, and health insurance type, the NHIS-NSC included a representative sample of 1,000,000 individuals, making up to 2.2% of the national population [39]. The NHIS-NSC database comprises sociodemographic characteristics and diagnosis codes based on the International Classification of Diseases, 10th revision (ICD-10) (41), and healthcare utilization information derived from the National Health Insurance (NHI) claims for inpatient and outpatient visits. In detail, the NHI claims data contain principal and additional diagnoses, hospitalization and outpatient treatment details, prescribed medications, and health examination data. The classification codes for psychotherapy within the dataset are based on the setting in which the therapy was provided, such as individual therapy, group therapy, and family therapy. However, the database does not include specific codes for identifying the type of psychotherapy conducted, such as CBT-I or other specific therapeutic techniques.
2.2 Study population and cohort selection
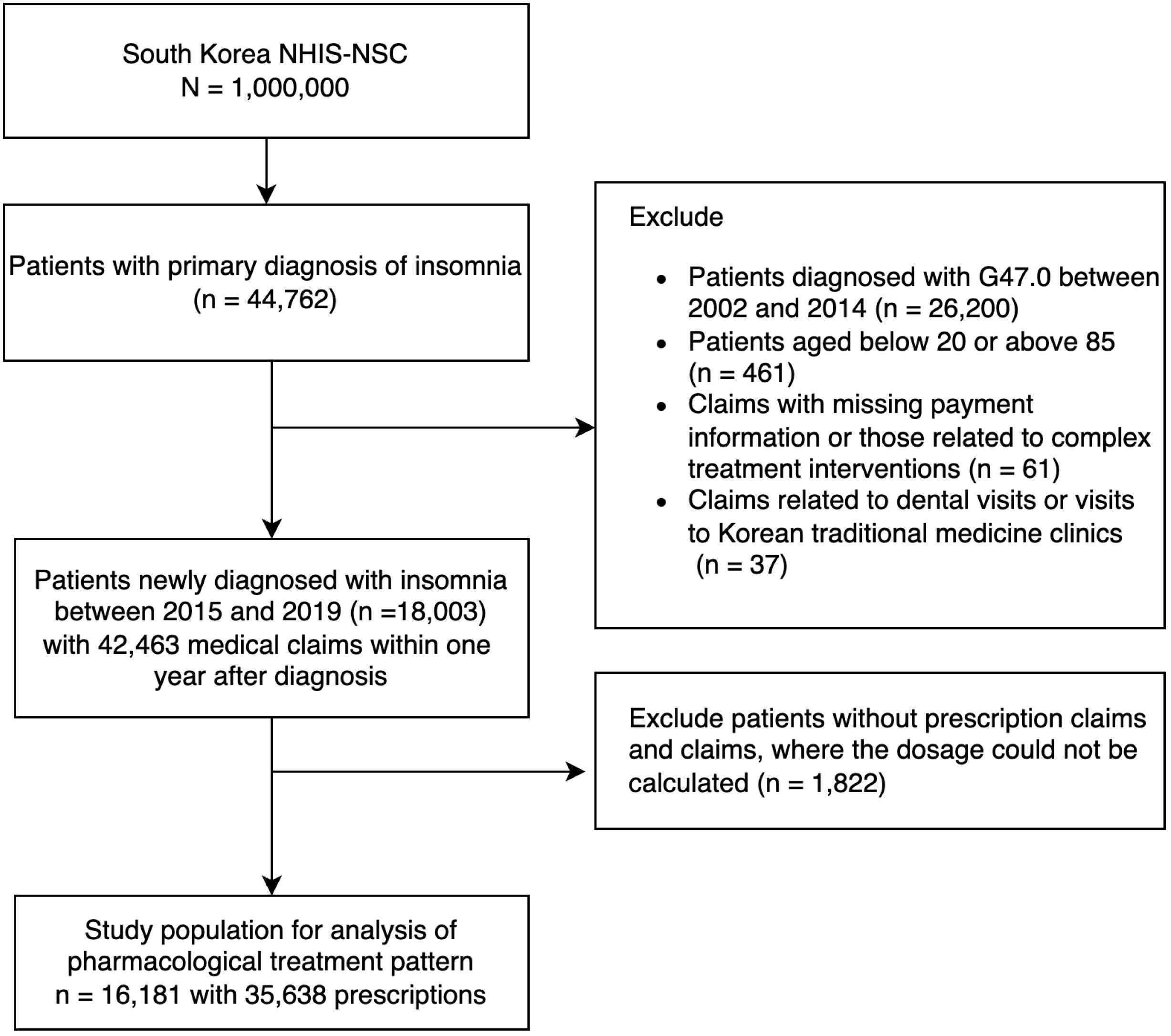
We identified 44,762 patients with a primary diagnosis of insomnia (ICD-10 code G47.0) during outpatient visits, excluding those with primary diagnoses under ICD-10 ‘F codes’ to avoid confounding variables from psychiatric comorbidities. To focus on new cases of insomnia, we excluded patients diagnosed with G47.0 between 2002 and 2014 (n = 26,200). Additionally, we excluded patients aged younger than 20 years or older than 85 years (n = 461), those with missing payment information or those related to complex treatment interventions (n = 61), and those with claims related to dental visits or visits to Korean traditional medicine clinics (n = 37). This resulted in a cohort of 18,003 patients newly diagnosed with insomnia between 2015 and 2019, accounting for 42,463 medical claims within one year after diagnosis. To analyze pharmacological treatment patterns, we excluded 1,822 patients without prescription claims or for whom the dosage could not be calculated. The final study population comprised 16,181 patients with 35,638 prescriptions for insomnia medications. The selection process and exclusions are detailed in Figure 1.
2.3 Analysis
Patients were followed for one year after the diagnosis of insomnia. General characteristics are presented as frequencies (n) and percentages (%). Clinical outcomes within this period included the number of patients and claims, frequency of outpatient visits, and number of patients receiving psychotherapy. Under Korean medical law, medical institutions were classified based on bed count: clinics had fewer than 100 beds, and general hospitals had more than 100 beds (42).
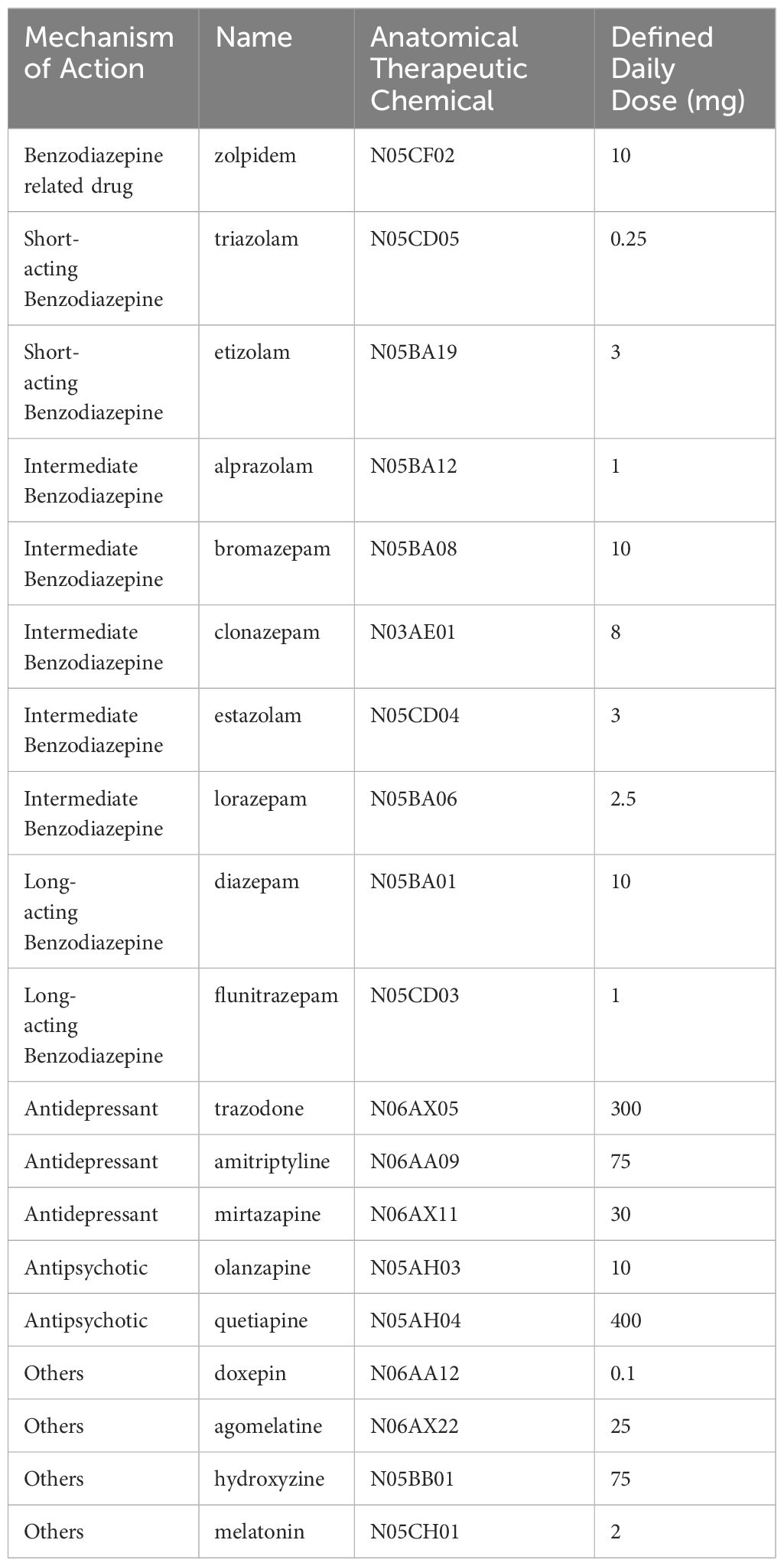
For the pharmacological treatment analysis, we included medications prescribed or judged to be administered to improve insomnia symptoms. According to the clinical practice guidelines for insomnia published by the Korean Neuropsychiatric Association, 19 drugs listed as sleep medications registered in South Korea were included in this analysis (22). These medications were classified based on their mechanism of action into the following categories: short-acting benzodiazepines, intermediate-acting benzodiazepines, long-acting benzodiazepines, zolpidem (benzodiazepine-related drug, or “z-drugs”), antidepressants, melatonin and others (Table 2). The types of prescribed medications, duration of prescriptions, dosage and regimen of sleep medications, and patterns of dosage increases or decreases were analyzed. The defined daily dose (DDD) was calculated for each medication, following the World Health Organization (WHO) guidelines, representing the average maintenance dose per day for a drug used for its main indication in adults weighing 70 kg (43). Changes in DDD patterns were analyzed to identify shifts in prescribing practices, assess the impact of clinical guidelines, and evaluate trends over time.
3 Results
3.1 Baseline characteristics
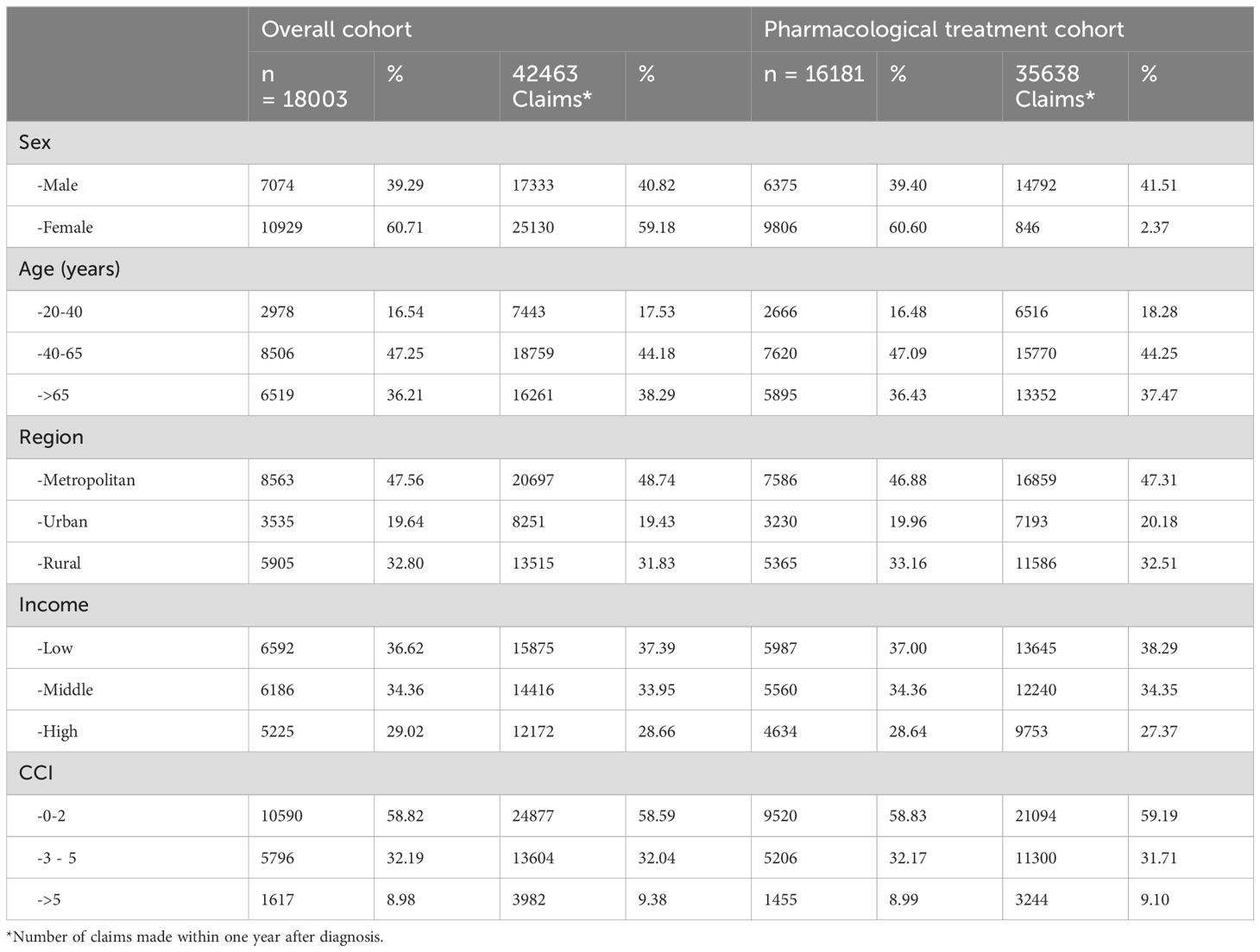
The study included 18,003 patients newly diagnosed with insomnia, generating 42,463 medical claims within one year. Of these, 16,181 patients received pharmacological treatment, resulting in 35,638 prescriptions. The majority were female (60.7% of the overall cohort and 60.6% of the pharmacological treatment cohort) and aged 40-65 years (47.3% and 47.1%, respectively), followed by those over 65 years (36.2% and 36.4%). Nearly half of the patients resided in metropolitan areas (47.6% and 46.9%). Low-income patients comprised 36.6% of the study population and 37.0% of the pharmacological treatment cohort. Most had a Charlson Comorbidity Index (CCI) of 0-2 (58.8% and 58.8%), indicating a low level of comorbid conditions (Table 3).
3.2 Insomnia patient distribution and psychotherapy utilization trends
Most insomnia patients were treated in clinics, with approximately 3,500 patients treated annually from 2015 to 2019. In 2015, 3,549 patients were treated, with 90.3% in clinics and 9.7% in general hospitals. By 2019, 3,762 patients were treated, 87.1% in clinics and 12.9% in general hospitals. The number of claims per person varied slightly over the years, peaking at 2.6 in 2018. Figure 2 illustrates the distribution of the number of patients between clinics and general hospitals, as well as the number of claims per person each year.

Figure 2. Number of insomnia patients and claims per person by year. Distribution of insomnia patients treated in clinics and general hospitals from 2015 to 2019, along with the average number of claims per person each year.
The number of visits for psychotherapy in the first year after insomnia diagnosis was analyzed from 2015 to 2019. Psychotherapy claims included individual psychotherapy, group psychotherapy, and family therapy. The overall proportion of psychotherapy claims relative to all medical claims increased steadily during this period. In 2015, 3.2% of all medical claims were for psychotherapy, which rose to 9.1% by 2019. In general hospitals, psychotherapy claims constituted 22.1% of the total claims in 2015, increasing to 48.4% in 2019. In clinics, however, the proportion of psychotherapy claims was low, starting at 1.3% in 2015 and rising to 2.1% in 2019 (Figure 3).
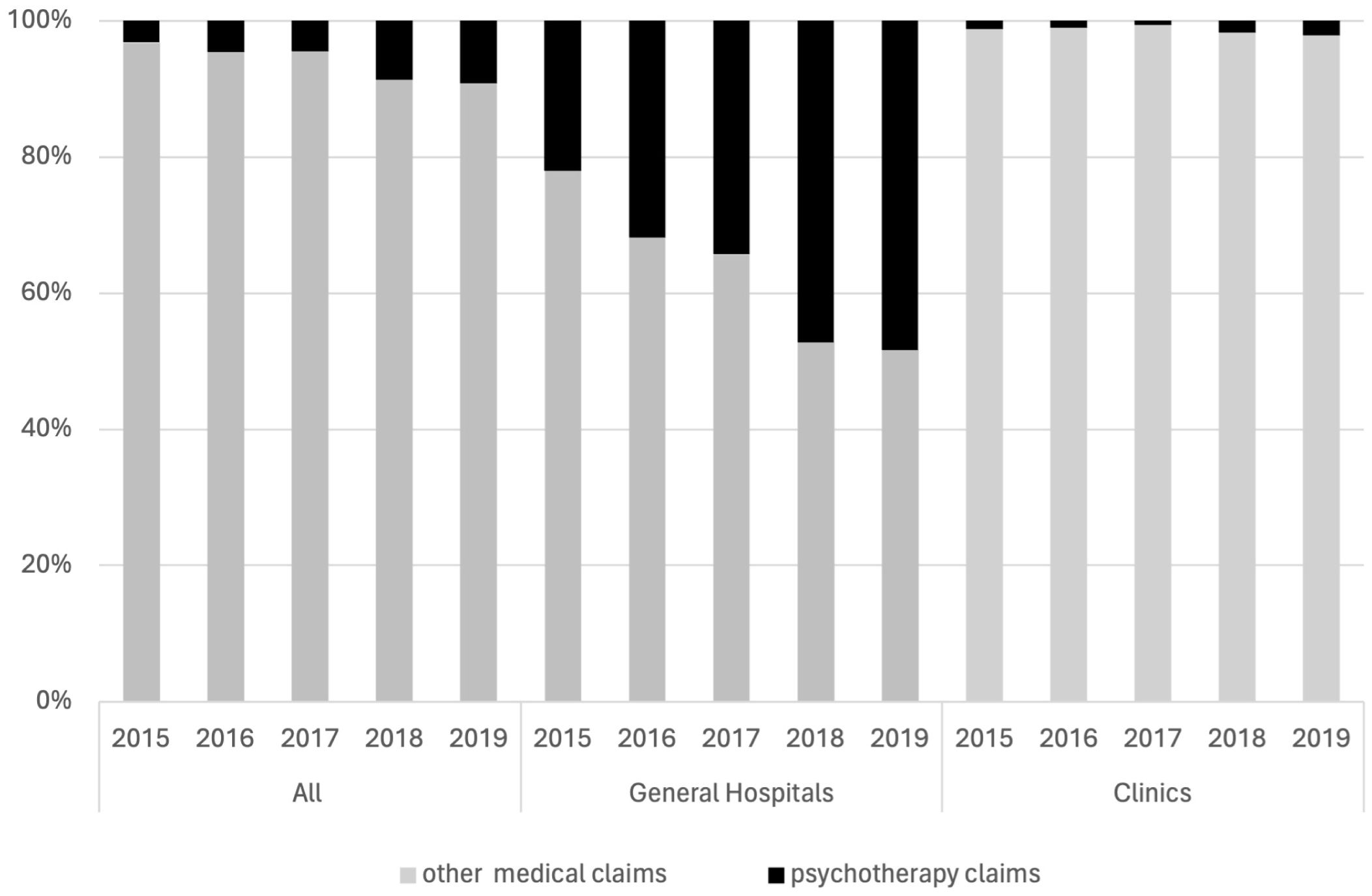
Figure 3. Psychotherapy claims for insomnia by year and setting. Percentage of psychotherapy claims relative to all medical claims for insomnia patients from 2015 to 2019, differentiated by general hospitals and clinics.
3.3 Pharmacological treatment of insomnia
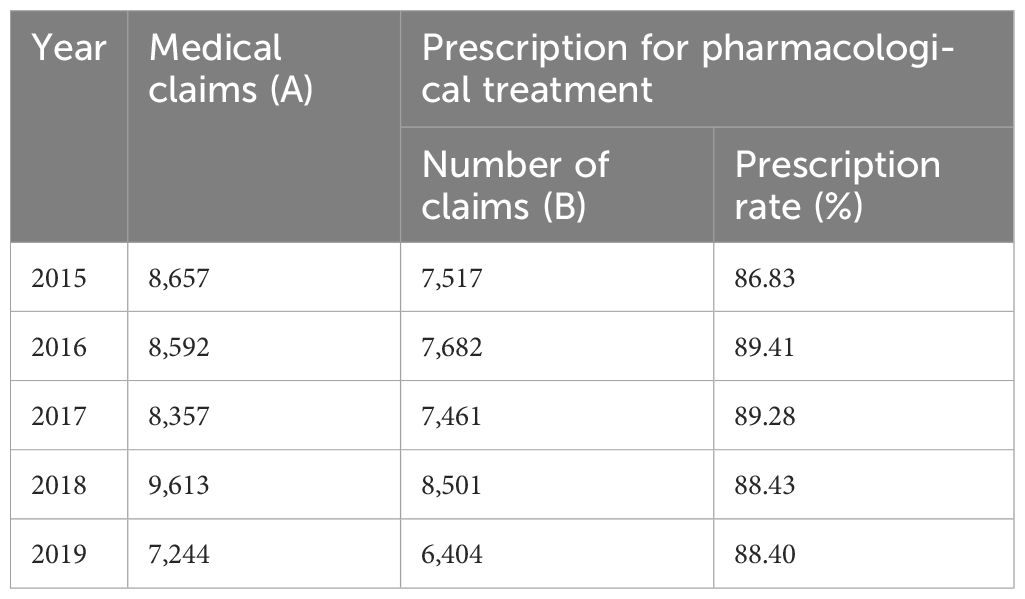
The number of medical claims, prescriptions for pharmacological treatment, and prescription rates from 2015 to 2019 are summarized in Table 4. The prescription rate remained consistently high, from 86.8% to 89.4% over the years.
The analysis of pharmacological treatments for insomnia from 2015 to 2019 revealed the distribution of various medication classes prescribed. Zolpidem was the most prescribed class of medication, accounting for more than 60% of prescriptions each year. Benzodiazepines were the second most frequently prescribed, with their usage ranging between approximately 30% and 40%. The use of antidepressants slightly increased over time, while the use of antipsychotics and other medications remained at relatively low and stable levels (Figure 4).
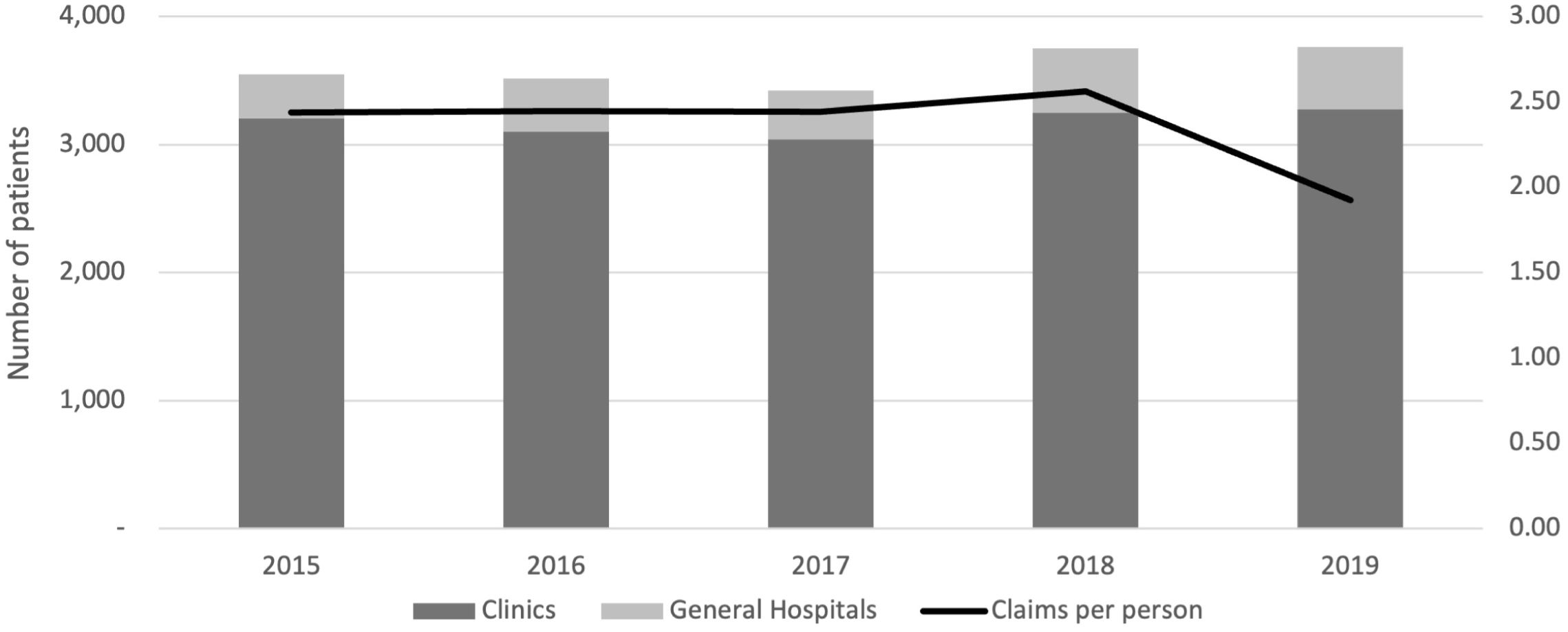
Figure 4. Distribution of medication classes prescribed to insomnia patients from 2015 to 2019. The graph shows the percentage of patients with zolpidem, benzodiazepines, antidepressants, antipsychotics, and other medications each year.
3.4 Outpatient visit-based prescription duration and DDD
The analysis of outpatient visit-based prescription duration DDD was conducted for zolpidem, triazolam, diazepam, and alprazolam. Figure 5 illustrates the mean duration of prescription and DDD across different outpatient visits for these medications. The figure shows the average duration of prescriptions (in days) and the mean DDD for zolpidem (A), triazolam (B), diazepam (C), and alprazolam (D) across different outpatient visits. Zolpidem had an initial prescription duration of 12.8 days, which increased to 20.8 days by the seventh visit, with a stable mean DDD close to 1.0, indicating consistent dosing practices despite longer prescription durations. Triazolam exhibited a similar trend, with the duration increasing from 11.9 days at the first visit to 18.4 days by the seventh visit. The mean DDD remained relatively stable, around 0.9, with slight fluctuations observed across visits. Diazepam showed an increase in prescription duration from 9.0 days to 20.5 days over seven visits. The mean DDD for diazepam was the lowest among the four medications, starting at approximately 0.7 and gradually increasing to 0.9 by the seventh visit, reflecting consistent but gradually increasing dosing. Alprazolam shows increasing durations from around 11.4 to 19.0 days, with a consistent mean DDD of around 0.4. Overall, the analysis indicates that while the duration of prescriptions for these medications increases with successive outpatient visits, the mean DDD for each drug remains relatively stable, with minor variations. This stability in DDD suggests consistent dosing practices across different patient visits, even as the duration of treatment extends over time.

Figure 5. Duration of prescriptions and mean DDD by outpatient visit for (A) Zolpidem, (B) Triazolam, (C) Diazepam, and (D) Alprazolam.
4 Discussion
This study analyzed the treatment patterns and utilizations of patients newly diagnosed with insomnia using data from the Korea National Health Insurance Service-National Sample Cohort (NHIS-NSC) from 2015 to 2019.
Our analysis indicated that the majority of insomnia patients in South Korea were treated in clinics, with pharmacological treatment being the predominant management strategy. Zolpidem and benzodiazepines were the most frequently prescribed medications, accounting for a substantial portion of all prescriptions. The analysis of prescription patterns revealed consistent dosages with increasing treatment lengths across outpatient visits. Specifically, the DDD for commonly used insomnia medications such as zolpidem, triazolam, diazepam, and alprazolam remained stable, even as the duration of prescriptions increased with each subsequent outpatient visit. This pattern suggests that while clinicians are extending the duration of treatment, they are maintaining consistent dosing practices. However, it Is Important to note that current clinical guidelines recommend that both Z-drugs and benzodiazepines be used only for short-term treatment of insomnia, typically limited to two to four weeks (18, 20, 44). Prolonged use of these medications carries significant risks, including the development of dependence, cognitive impairment, and psychomotor impairment, which can lead to falls and fractures, particularly in elderly patients (36, 37). These findings are consistent with international trends despite the recommendations of clinical guidelines (18, 45). The observed extension of prescription durations in our study indicates a potential deviation from recommended practices. This highlights the need for clinicians to carefully assess the benefits and risks of continued use of Z-drugs and benzodiazepines, ensure that treatment duration is minimized, and follow appropriate tapering protocols to mitigate the risks associated with long-term use (44, 46).
Among the “Z-drugs,” eszopiclone has been shown to have the best efficacy and acceptability profiles for both short-term and long-term use (18). However, it was not included in our analysis due to its late market entry (at the end of 2019) in South Korea. Novel pharmacological treatments that are not yet available in South Korea include medications targeting new mechanisms, such as ramelteon (facilitating melatonin activity), and orexin receptor antagonists, such as daridorexant, lemborexant, seltorexant, and suvorexant (47). Lemborexant has demonstrated strong efficacy for both short-term and long-term treatment of insomnia (18). These advancements represent potential future options for insomnia management in South Korea.
Our findings indicate that despite international guidelines recommending CBT-I as the first-line treatment for insomnia, its utilization, as inferred from general psychotherapy claims, remains low, particularly in clinics. This observation is consistent with previous research, which has shown that the adoption of CBT-I in routine practice is limited despite its proven efficacy (24, 26, 32). In July 2018, the Ministry of Health and Welfare in South Korea included psychotherapy under the coverage of NHIS as part of efforts to diversify the payment system for psychiatric treatments. This policy change may account for the increased psychotherapy claims observed in 2018 and 2019, mainly in general hospitals. However, despite this expansion in coverage, the overall utilization of psychotherapy, and by extension, CBT-I, continues to be limited, suggesting that further efforts are necessary to promote its adoption. Barriers to the broader use of CBT-I include a shortage of trained professionals, time constraints, and patient preferences for quicker, medication-based solutions (35, 45, 48). New modalities, such as digital CBT-I, show promise in enhancing accessibility and utilization by offering a convenient alternative to traditional therapy (31).
The comprehensive data from the NHIS-NSC allowed for an analysis of prescription patterns and healthcare utilization, providing an analysis of insomnia management in South Korea. However, this study has several limitations. A key limitation of this study is the NHIS-NSC database’s lack of a specific code for CBT-I, which prevents precise identification of this treatment within psychotherapy claims. This means that while we observe a general increase in psychotherapy utilization, we cannot ascertain the extent to which evidence-based therapies like CBT-I are being implemented. Additionally, as a descriptive analysis, no associations were made between specific groups of patients and their utilization of treatment methods. The reliance on insurance claims data may lead to underreporting specific treatments, particularly non-pharmacological interventions such as psychotherapy, which can be conducted outside the medical setting. These sessions are not included in insurance claims data. Furthermore, the exclusion criteria, particularly for patients with psychiatric comorbidities, limit the generalizability of the findings to all insomnia patients. Also, the presence of comorbid sleep disorders, such as obstructive sleep apnea (OSA), was not analyzed, although comorbid insomnia and sleep apnea (COMISA) is prevalent and complicates insomnia management, affecting up to 35% of insomnia patients (49, 50).
Future research should aim to explore the risks based on demographics and investigate the relationships with therapy utilization. Additionally, comparisons between the psychotherapy and pharmacological treatment groups could help identify potential referral biases and predictors for psychotherapy treatment. Studies focusing on the barriers to psychotherapy utilization could provide insights into improving adherence to clinical guidelines. Moreover, research incorporating a broader range of comorbid conditions would offer a more comprehensive view of insomnia management in diverse patient populations.
In conclusion, our study highlights the predominant use of pharmacological treatments for insomnia and the underutilization of psychotherapy despite its clinical recommendations. These findings suggest a need for enhanced efforts to integrate psychotherapy into routine clinical practice and further research to optimize insomnia management strategies.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://nhiss.nhis.or.kr/.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Yonsei University. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because it involved retrospective analyses of de-identified data.
Author contributions
DM: Conceptualization, Writing – original draft, Writing – review & editing. ZP: Formal analysis, Methodology, Writing – review & editing. DL: Visualization, Writing – review & editing. EH: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was conducted at the request of and supported by WELT Corp. Ltd. to understand the current therapy management of insomnia in South Korea. The funder was not involved in the study design, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Acknowledgments
We would like to extend our sincere thanks to Yea Jin Youn (Graduate Program of Industrial Pharmaceutical Science, Yonsei University, Incheon, Republic of Korea) for her valuable assistance in the revision of this manuscript.
Conflict of interest
Authors DM and DL were employed by the company WELT Corp. Ltd.The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BZRA, Benzodiazepine Receptor Agonist; CBT, Cognitive Behavioral Therapy; CBT-I, Cognitive Behavioral Therapy for Insomnia; CCI, Charlson Comorbidity Index; COMISA, Comorbid Insomnia and Sleep Apnea; CONSORT, Consolidated Standards of Reporting Trials; DDD, Defined Daily Dose; FDA, Food and Drug Administration; ICD-10, International Classification of Diseases, 10th Revision; NHIS, National Health Insurance Service; NHIS-NSC, National Health Insurance Service-National Sample Cohort; NHI, National Health Insurance; OSA, Obstructive Sleep Apnea; PR, Prolonged Release; WHO, World Health Organization.
References
1. American Psychiatric Association. DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Washington, DC: American Psychiatric Publishing, Inc (2013).
2. Sateia MJ. International classification of sleep disorders. Chest. (2014) 146:1387–94. doi: 10.1378/chest.14-0970
3. Roth T, Coulouvrat C, Hajak G, Lakoma MD, Sampson NA, Shahly V, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; international statistical classification of diseases and related health problems, tenth revision; and research diagnostic criteria/international classification of sleep disorders, criteria: results from the America insomnia survey. Biol Psychiatry. (2011) 69:592–600. doi: 10.1016/j.biopsych.2010.10.023
4. Ohayon MM, Reynolds CF III. Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD). Sleep Med. (2009) 10:952–60. doi: 10.1016/j.sleep.2009.07.008
5. Morin CM, Vézina-Im L-A, Ivers H, Micoulaud-Franchi J-A, Philip P, Lamy M, et al. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep. (2022) 45:zsab258. doi: 10.1093/sleep/zsab258
6. Ahn E, Baek Y, Park J-E, Lee S, Jin H-J. Elevated prevalence and treatment of sleep disorders from 2011 to 2020: a nationwide population-based retrospective cohort study in Korea. BMJ Open. (2024) 14:e075809. doi: 10.1136/bmjopen-2023-075809
7. Léger D, Morin CM, Uchiyama M, Hakimi Z, Cure S, Walsh JK. Chronic insomnia, quality-of-life, and utility scores: comparison with good sleepers in a cross-sectional international survey. Sleep Med. (2012) 13:43–51. doi: 10.1016/j.sleep.2011.03.020
8. Zhang Y, Jiang X, Liu J, Lang Y, Liu Y. The association between insomnia and the risk of metabolic syndrome: A systematic review and meta-analysis. J Clin Neurosci. (2021) 89:430–6. doi: 10.1016/j.jocn.2021.05.039
9. Markwald RR, Melanson EL, Smith MR, Higgins J, Perreault L, Eckel RH, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci. (2013) 110:5695–700. doi: 10.1073/pnas.1216951110
10. Malik S, Kanwar A, Sim LA, Prokop LJ, Wang Z, Benkhadra K, et al. The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: a systematic review and meta-analysis. Systematic Rev. (2014) 3:18. doi: 10.1186/2046-4053-3-18
11. Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
12. Drake CL, Pillai V, Roth T. Stress and sleep reactivity: a prospective investigation of the stress-diathesis model of insomnia. Sleep. (2014) 37:1295–304. doi: 10.5665/sleep.3916
13. Parthasarathy S, Vasquez MM, Halonen M, Bootzin R, Quan SF, Martinez FD, et al. Persistent insomnia is associated with mortality risk. Am J Med. (2015) 128:268–275.e2. doi: 10.1016/j.amjmed.2014.10.015
14. Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. (1996) 39:411–8. doi: 10.1016/0006-3223(95)00188-3
15. Wickwire EM, Shaya FT, Scharf SM. Health economics of insomnia treatments: the return on investment for a good night’s sleep. Sleep Med Rev. (2016) 30:72–82. doi: 10.1016/j.smrv.2015.11.004
16. Daley M, Morin CM, LeBlanc M, Grégoire J-P, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. (2009) 32:55–64.
17. Krystal AD, Prather AA, Ashbrook LH. The assessment and management of insomnia: an update. World Psychiatry. (2019) 18:337–52. doi: 10.1002/wps.20674
18. De Crescenzo F, D’Alò GL, Ostinelli EG, Ciabattini M, Di Franco V, Watanabe N, et al. Comparative effects of pharmacological interventions for the acute and long-term management of insomnia disorder in adults: a systematic review and network meta-analysis. Lancet. (2022) 400:170–84. doi: 10.1016/S0140-6736(22)00878-9
19. Chung S. Korean clinical practice guideline for management of insomnia in adults. Korean Neuropsychiatr Assoc. (2019) 10.
20. Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. (2017) 13:307–49. doi: 10.5664/jcsm.6470
21. Riemann D, Espie CA, Altena E, Arnardottir ES, Baglioni C, Bassetti CL, et al. The European Insomnia Guideline: An update on the diagnosis and treatment of insomnia 2023. J Sleep Res. (2023) 32:e14035. doi: 10.1111/jsr.14035
22. Choi H, Youn S, Um YH, Kim TW, Ju G, Lee HJ, et al. Korean clinical practice guideline for the diagnosis and treatment of insomnia in adults. Psychiatry Invest. (2020) 17:1048. doi: 10.30773/pi.2020.0146
23. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD, Physicians* CGCotACo. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Internal Med. (2016) 165:125–33. doi: 10.7326/M15-2175
24. Van Straten A, van der Zweerde T, Kleiboer A, Cuijpers P, Morin CM, Lancee J. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. (2018) 38:3–16. doi: 10.1016/j.smrv.2017.02.001
25. Koffel EA, Koffel JB, Gehrman PR. A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Med Rev. (2015) 19:6–16. doi: 10.1016/j.smrv.2014.05.001
26. Wu JQ, Appleman ER, Salazar RD, Ong JC. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: a meta-analysis. JAMA Internal Med. (2015) 175:1461–72. doi: 10.1001/jamainternmed.2015.3006
27. Smith MT, Perlis ML, Park A, Smith MS, Pennington J, Giles DE, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. (2002) 159:5–11. doi: 10.1176/appi.ajp.159.1.5
28. Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive behavioral therapy for treatment of chronic primary insomnia: a randomized controlled trial. JAMA. (2001) 285:1856–64. doi: 10.1001/jama.285.14.1856
29. Ye Y-y, Zhang Y-f, Chen J, Liu J, Li X-j, Liu Y-z, et al. Internet-based cognitive behavioral therapy for insomnia (ICBT-i) improves comorbid anxiety and depression—a meta-analysis of randomized controlled trials. PloS One. (2015) 10:e0142258. doi: 10.1371/journal.pone.0142258
30. Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, et al. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiatry. (2019) 76:21–30. doi: 10.1001/jamapsychiatry.2018.2745
31. Krystal AD, Prather AA. Should internet cognitive behavioral therapy for insomnia be the primary treatment option for insomnia?: Toward getting more SHUTi. JAMA Psychiatry. (2017) 74:15–6. doi: 10.1001/jamapsychiatry.2016.3431
32. Rossman J. Cognitive-behavioral therapy for insomnia: an effective and underutilized treatment for insomnia. Am J Lifestyle Med. (2019) 13:544–7. doi: 10.1177/1559827619867677
33. Jang CH, Kim SH, Oh DH. Cognitive behavioral therapy of insomnia. Hanyang Med Rev. (2013) 33:210. doi: 10.7599/hmr.2013.33.4.210
34. Fields BG, Schutte-Rodin S, Perlis ML, Myers M. Master’s-level practitioners as cognitive behavioral therapy for insomnia providers: an underutilized resource. J Clin Sleep Med. (2013) 09:1093–6. doi: 10.5664/jcsm.3096
35. Dewa LH, Hassan L, Shaw J, Senior J. Insomnia management in prisons in england and wales: A mixed-methods study. J Sleep Res. (2017) 26:322–9. doi: 10.1111/jsr.12503
36. Riemann D, Perlis ML. The treatments of chronic insomnia: A review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med Rev. (2009) 13:205–14. doi: 10.1016/j.smrv.2008.06.001
37. Andrade C. Sedative hypnotics and the risk of falls and fractures in the elderly. J Clin Psychiatry. (2018) 79. doi: 10.4088/JCP.18f12340
38. Morin CM, Benca R. Chronic insomnia. Lancet. (9821) 2012:379. doi: 10.1016/S0140-6736(11)60750-2
39. Muehlan C, Vaillant C, Zenklusen I, Kraehenbuehl S, Dingemanse J. Clinical pharmacology, efficacy, and safety of orexin receptor antagonists for the treatment of insomnia disorders. Expert Opin Drug Metab Toxicology. (2020) 16:1063–78. doi: 10.1080/17425255.2020.1817380
40. Zheng X, He Y, Xu L, Li Y, Yin F, Li H, et al. Quantitative analysis of the placebo response in pharmacotherapy of insomnia and its application in clinical trials. Sleep. (2020) 43:zsz286. doi: 10.1093/sleep/zsz286
41. World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization (1992).
42. Korean Medical Service Act. Korea legislation research institute. Sejong-Si, South Korea: Korea Legislation Research Institute (2024), Act No. 20105.
43. World Health Organization. Anatomic therapeutic chemical (ATC) and defined daily dose (DDD) toolkit (2024). Available online at: https://www.who.int/tools/atc-ddd-toolkit (Accessed May 06, 2024).
44. Brandt J, Bressi J, Lê M-L, Neal D, Cadogan C, Witt-Doerring J, et al. Prescribing and deprescribing guidance for benzodiazepine and benzodiazepine receptor agonist use in adults with depression, anxiety, and insomnia: an international scoping review. eClinicalMedicine. (2024) 70. doi: 10.1016/j.eclinm.2024.102507
45. Medalie L, Cifu AS. Management of chronic insomnia disorder in adults. JAMA. (2017) 317:762. doi: 10.1001/jama.2016.19004
46. Hirschtritt ME, Olfson M, Kroenke K. Balancing the risks and benefits of benzodiazepines. JAMA. (2021) 325:347–8. doi: 10.1001/jama.2020.22106
47. Wilson S, Anderson K, Baldwin D, Dijk D-J, Espie A, Espie C, et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders: an update. J Psychopharmacology. (2019) 33:923–47. doi: 10.1177/0269881119855343
48. Landy MSH, Newman L, Carney AE, Donkin V, Nicholls J, Krol S, et al. Therapist-assisted internet-delivered cognitive behavioral therapy for insomnia: A case report. Clin Case Stud. (2023) 22:383–402. doi: 10.1177/15346501221145944
49. Sweetman A, Lack L, Bastien C. Co-morbid insomnia and sleep apnea (COMISA): prevalence, consequences, methodological considerations, and recent randomized controlled trials. Brain Sci. (2019) 9. doi: 10.3390/brainsci9120371
Keywords: insomnia, sleep disorder, cognitive behavioral therapy for insomnia, CBT-I, NHIS-NSC, nationwide cohort study
Citation: Moon DU, Piao Z, Lee DH and Han E (2024) From guidelines to bedside - insomnia treatment practices in South Korea: a nationwide cohort study. Front. Psychiatry 15:1453550. doi: 10.3389/fpsyt.2024.1453550
Received: 23 June 2024; Accepted: 22 August 2024;
Published: 13 September 2024.
Edited by:
Kittisak Sawanyawisuth, Khon Kaen University, ThailandReviewed by:
David Neubauer, Johns Hopkins University, United StatesDing Zou, University of Gothenburg, Sweden
Copyright © 2024 Moon, Piao, Lee and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Euna Han, ZXVuYWhhbkB5b25zZWkuYWMua3I=
†These authors share first authorship
 Daa Un Moon
Daa Un Moon Zhaoyan Piao2†
Zhaoyan Piao2† Do Hyun Lee
Do Hyun Lee Euna Han
Euna Han