- 1Graduate School, Hebei University of Chinese Medicine, Shijiazhuang, China
- 2Anorectal Surgery Department, The First Affiliated Hospital of Hebei University of Chinese Medicine, Shijiazhuang, China
Objectives: This study aimed to explore the association between bowel movement disorders and depression in adults.
Method: A cross-sectional study was conducted using data from the National Health and Nutritional Examination Survey (NHANES), 2005–2010. Depression, constipation, diarrhea, and fecal incontinence were self-reported via questionnaires. Weighted logistic regression and subgroup analyses were performed to explore the association between bowel movement disorders and the risk of depression. Restricted cubic spline (RCS) was also conducted to investigate the association between bowel movements disorder and depression.
Results: A total of 13,820 participants were collected. Compared to the participants with normal bowel movements, the full-adjusted depression model ORs for constipation and diarrhea were 2.28 (95%CI,1.78-2.92), 1.75 (95%CI,1.31-2.31), respectively. Any kind of bowel leakage were associated with depression. The RCS showed the possible nonlinear association between bowel movement frequency/stool shape and depression.
Conclusions: Constipation, diarrhea, and bowel leakage are associated with an increased risk of depression.
1 Introduction
Depression is one of the most hazardous mental disorders, rank among the most substantial causes of death worldwide (1). In 2020, the prevalence of depression was 9.2% (2), and the incidence was increasing (3). It can increase suicide ideation, attempts, and death (4). thus, depression became the leading cause of disability around the world (5).
Defecation disorders are common clinical problems that includes constipation, diarrhea and fecal incontinence. Constipation and diarrhea are changes in bowel movement frequency and stool form, and fecal incontinence refers to the involuntary leakage of gas, mucus, liquid, or solid stool. These bowel movement disorders profoundly impair the quality of life (6–9). Evidence showed that the risk of constipation in depressed people was 1.69 to 3.76 times that of non-depressed people (10, 11). Diarrhea, the eighth leading cause of death among all ages (12), was found to be commonly comorbid with depressive symptoms (13). As for fecal incontinence, which has a worldwide prevalence of 7% and 40 newonset per 1000 person a year, can markedly impair quality of life (14, 15). Moreover, the severe symptoms of depression were thought to be an identified risk factor of fecal incontinence (15). However, insufficient large population-based studies adjusting for related variables are available to assess the association between common gastrointestinal problems and depression. In this study, we aimed to determine the relation between depression and bowel movement disorders (constipation, diarrhea, and fecal incontinence) in a nationally representative sample of US adults.
2 Methods
2.1 Study design and recruitment
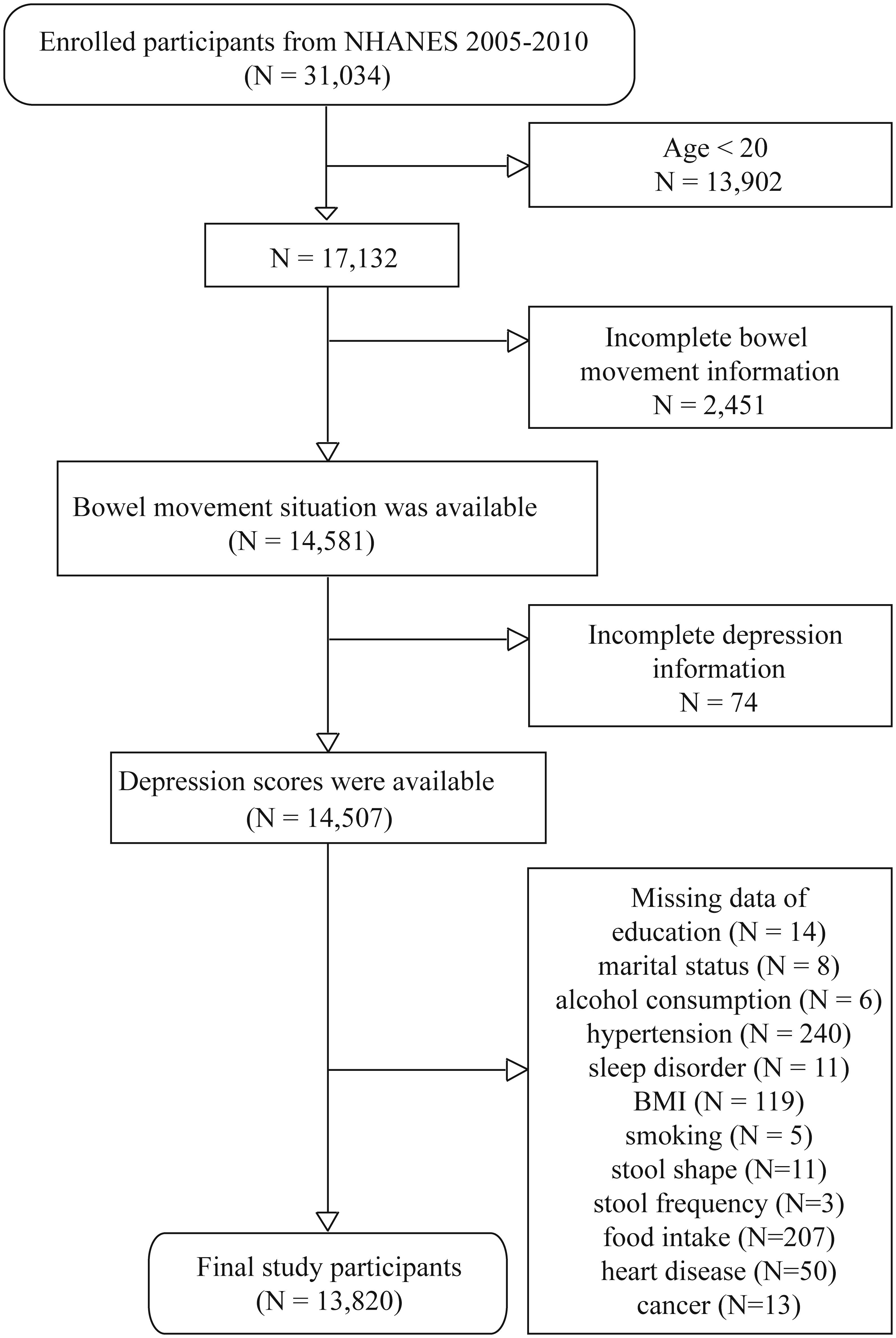
Data from the National Health and Nutrition Examination Survey (NHANES) was used to conduct this study. The NHANES is a continuous cross-sectional survey of noninstitutionalized US civilians conducted by the US National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention. Data for the NHANES was collected via household interviews, physical examinations, and laboratory data (16). For this study, bowel health data from 31,034 participants in the NHANES (2005–2010) were evaluated. The NCHS Research Ethics Review Board reviewed and approved this study. Informed consent was obtained from all subjects involved in the study.
Participants under 20 years old were excluded (N = 13,902) because they were not involved in the “bowel health” questionnaire. Participants with missing bowel health (N = 2,451), depression (N = 74) information and other covariate information (N = 687) were excluded. The specific screening process was shown in Figure 1. After the exclusion of participants, the data from 13,820 individuals were eligible for further analysis.
2.2 Dependent variable: depression
Depression symptoms were measured with a nine-item Patient Health Questionnaire (PHQ-9). The internal and test-retest reliabilities of the PHQ-9 were both excellent, with a Cronbach’s α of 0.89 (17). The scores of the nine items were added to calculate the depressive scores. Depression was defined as PHQ-9 scores of ≥10 (17).
2.3 Independent variables
Bowel movement status was evaluated using a questionnaire about weekly bowel movement frequency and the Bristol Stool Form Scale. The Bristol Stool Form Scale uses 7 descriptions of stool shape from separate hard lumps to watery stool. Constipation was defined as less than 3 bowel movements per week or 1 and 2 types of stool from the Bristol Stool Form Scale (18). Diarrhea was defined as 21 defecations per week without 1 or 2 Bristol Stool Form Scale types or Bristol Stool Form Scale type 7 stool defecation more than 2 times per week (19).
Fecal incontinence was defined as the unintentional loss of solid or liquid stool. The Fecal Incontinence Severity Index (FISI) consists of 4 questions about the frequency of different types of bowel leakage, including gas, mucus, liquid, and solid stool. The answer choices represented the frequency of leakage and included “1” for “2 or more times a day,” “2” for “once a day,” “3” means “2 or more times a week,” “4” for “once a week,” “5” for “1 to 3 times a month,” and “6” for “never.” It assigns a cumulative subjective weighted score from 0 to 61 to each patient, where a value of ‘0’ indicates no incontinence and ‘61’ indicates incontinence to gas, liquid, mucus and solid stool at least twice daily (20). Fecal incontinence was defined as any type of leakage on the FISI (21).
2.4 Covariates
Sociodemographic information (age, gender, marital status, ethnicities, and education), lifestyles (smoking, alcohol drinking, and sleep situation), medical conditions (hypertension, heart disease, cancer), antidepressant use, food intake (energy intake, protein intake, dietary fiber, and carbohydrate consumption), and body mass index (BMI) were collected. Age was divided into four categories: 20–39, 40–59, 60–79, and 80 and above. Marital status was classified into two groups: married/live with partner and widowed/divorced/separated/never married. Educational levels were classified into two categories: high school or below and above high school. Participants were considered smokers if they chose “YES” on the questionnaire: “Have you smoked at least 100 cigarettes in your entire life?” and also chose “Every day” or “Some days” on the questionnaire: “Do you now smoke cigarettes”. Alcohol users were defined if they consumed at least 12 drinks in any one year. Sleep disorder was defined as a participant complaint to the doctor about trouble sleeping or the participant was told by a doctor that they had a sleep disorder. Hypertension was defined as a high systolic (≥130 mmHg) or diastolic (≥80 mmHg) blood pressure measured at the mobile examination center, or self-report history of hypertension, or use of antihypertension medication. Participants were considered heart disease as if they chose “YES” on the questionnaire: “Ever told had congestive heart failure?” or “Ever told you had coronary heart disease?”. Cancer participants were defined if they had ever been told having cancer or a malignancy. Antidepressants were identified by the second level codes 249 in NHANES Drug Information (RXQ_DRUG). The list of antidepressants can be found in Supplementary Table 1. The energy, protein, fiber, and carbohydrate intake data were obtained from total nutrient intakes data by taking the average of two-day-recall. BMI was calculated as weight in kilograms divided by height in meters squared and was categorized into four groups (22): under-weight (BMI<18.5), normal (18.5≤ BMI≤ 25) overweight (25<BMI<30), and obesity (BMI≥30).
2.5 Statistical analysis
All statistical analyses accounted for the complex sampling design of the NHANES database, sample weights of individuals were determined by WTDR2D/3. Categorical variables are presented as weighted percentages and analyzed with Chi-square tests. Multivariable logistic regression models were used to estimate odds ratios (ORs) and 95% confidential intervals (CIs) for associations between depression and defecation disorders. Model 1 was not adjusted for any variables; Model 2 was adjusted for age, gender, race; Model 3 was adjusted for the variables in Model 2 plus education levels, marital status, BMI, sleep status, alcohol use, smoking, hypertension, heart disease, cancer, antidepressant use, and food intake (energy intake, protein intake, dietary fiber, and carbohydrate consumption). Subgroup analyses were stratified by age, gender, BMI to assess the association of depression with defecation problems. Meanwhile, interaction analyses were conducted to assess potential interactions. Furthermore, a restricted cubic spline (RCS) curve was performed to investigate the potentially nonlinear association between depression and defecation disorders. If the RCS showed a nonlinear relation, its inflection point would be further calculated. Sensitivity assessments were performed to evaluate the robustness of the results by conducting unweighted logistic regression analysis, modifying adjusted factors, and re-run the same models with depression defined as PHQ-9 scores ≥ 8. Statistical analysis was performed using Stata software (version 16.0) and R version 4.1.1. Two-tailed tests were conducted and a P value less than 0.05 was considered statistically significant.
3 Result
3.1 Baseline characteristics of participants
The study included 13,820 participants representing 191,491,012 civilian adults in the USA. 3,212 participants whom we failed to interview were excluded. Supplementary Table 2 displayed the baseline characteristics of adults with or without depression in the 2005-2010 NHANES. There were 1,182 (weighted n =14,520,742) participants had depression. Compared to non-depression participants, they were more likely to be 40 to 59 years old non-Hispanic White females, to have lower education levels, to be current smokers and drinkers, to have a higher BMI, to have higher prevalence of hypertension and heart disease, to have lower energy and protein intake, and to have higher prevalence of fecal leakage or abnormal bowel movements (P<0.05).
3.2 Association between depression and abnormal defecation
Depression positively correlated with defecation problems (Table 1). Compared to participants with normal bowel movement habits, participants with constipation had increased odds of significant depression (OR (95% CI) = 2.78 (2.19, 3.53)) in the unadjusted model (Model 1); the OR was 2.28 (95% CI, 1.78, 2.92) after full adjustment (Model 3). Compared to participants with normal bowel movement habits, participants with diarrhea had increased odds of depression (OR (95% CI) = 1.84 (1.37, 2.47)) in the unadjusted model and after full adjustment (OR (95% CI) = 1.74 (1.31, 2.31)).
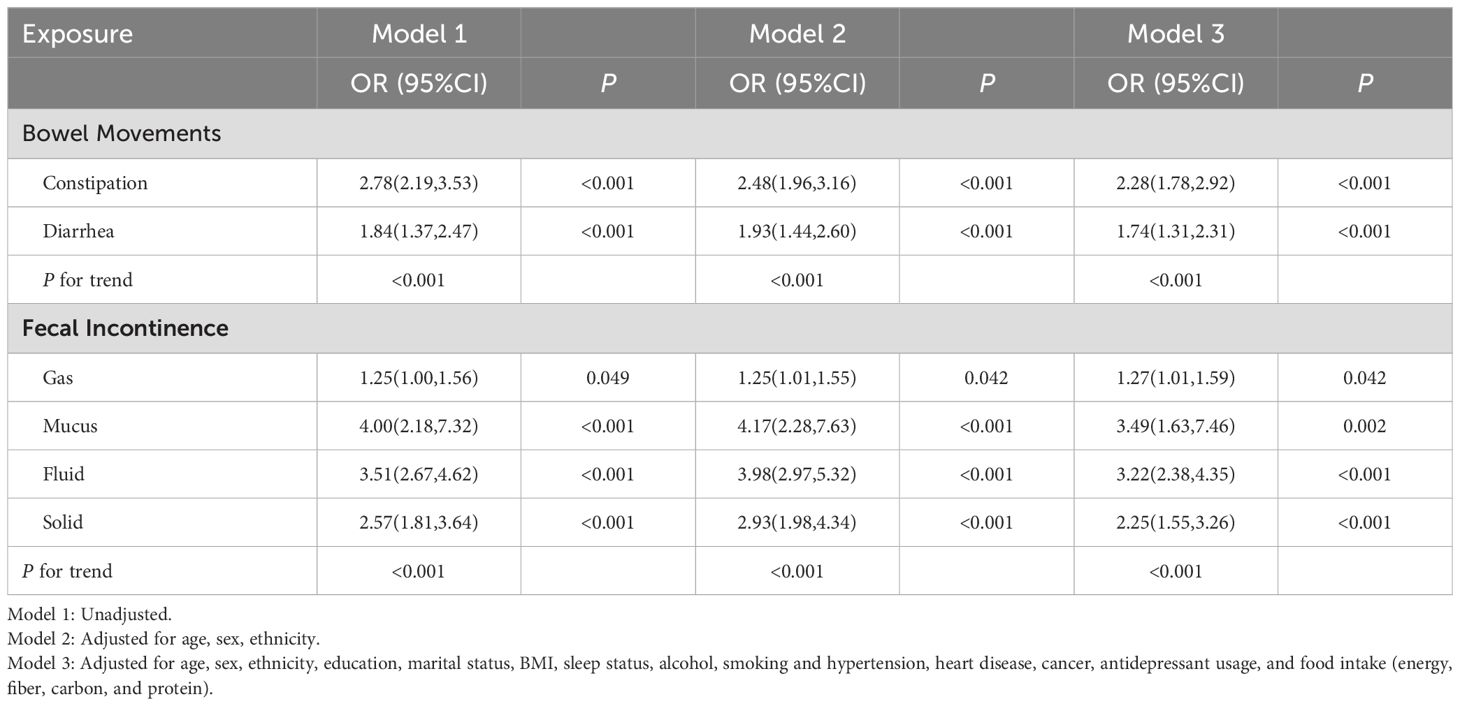
Table 1. Association of depression with bowel movement problems in a US population: NHANES, 2005–2010.
In the fully adjusted Model 3, all categories of bowel leakage showed significant positive association with the incidence of depression (OR (95% CI): 1.27 (1.01, 1.59), OR (95% CI):3.49 (1.63, 7.46), OR (95% CI): 3.22 (2.38, 4.35), and OR (95% CI): 2.25(1.55, 3.26), respectively), as presented in Table 2.
3.3 Subgroup analysis
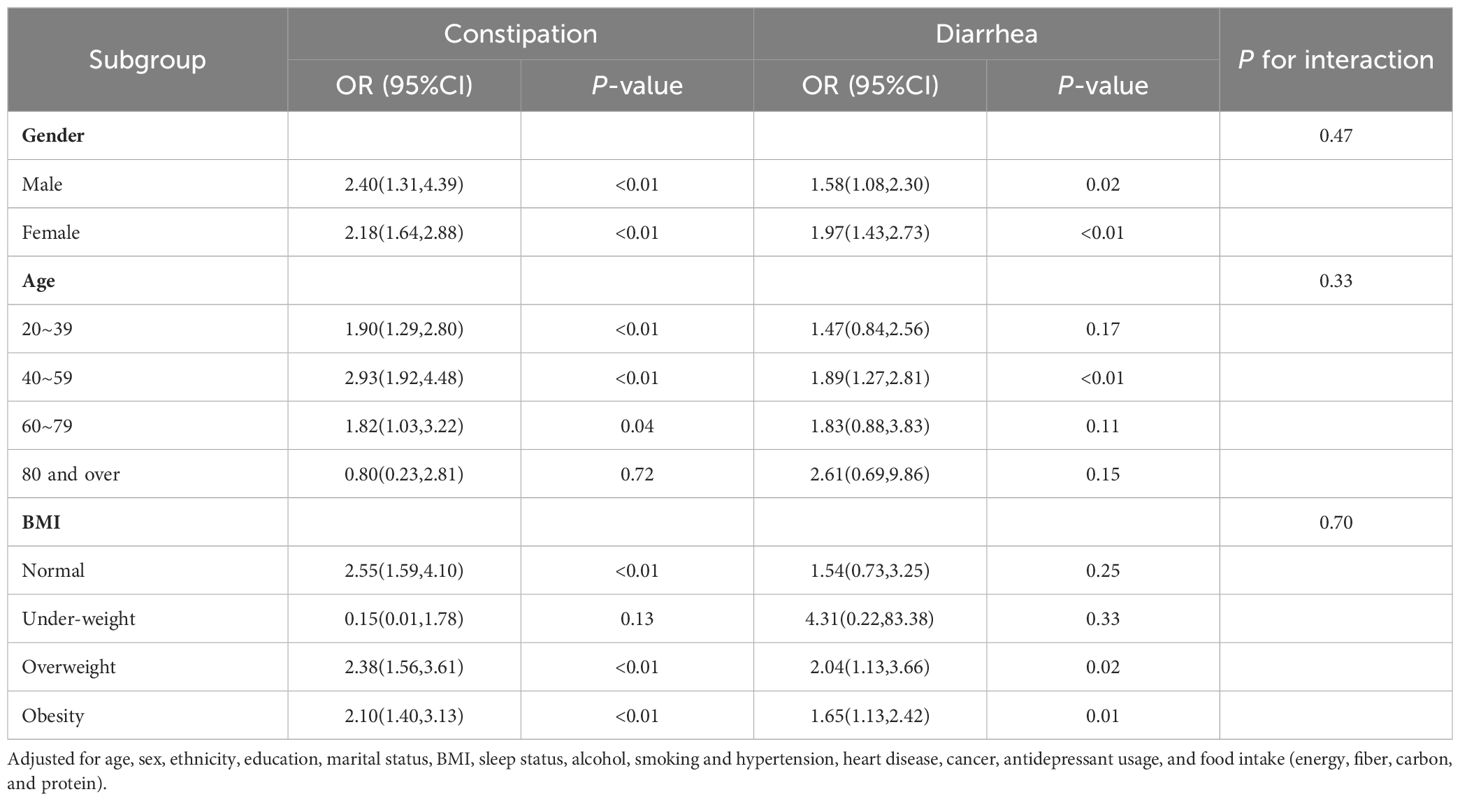
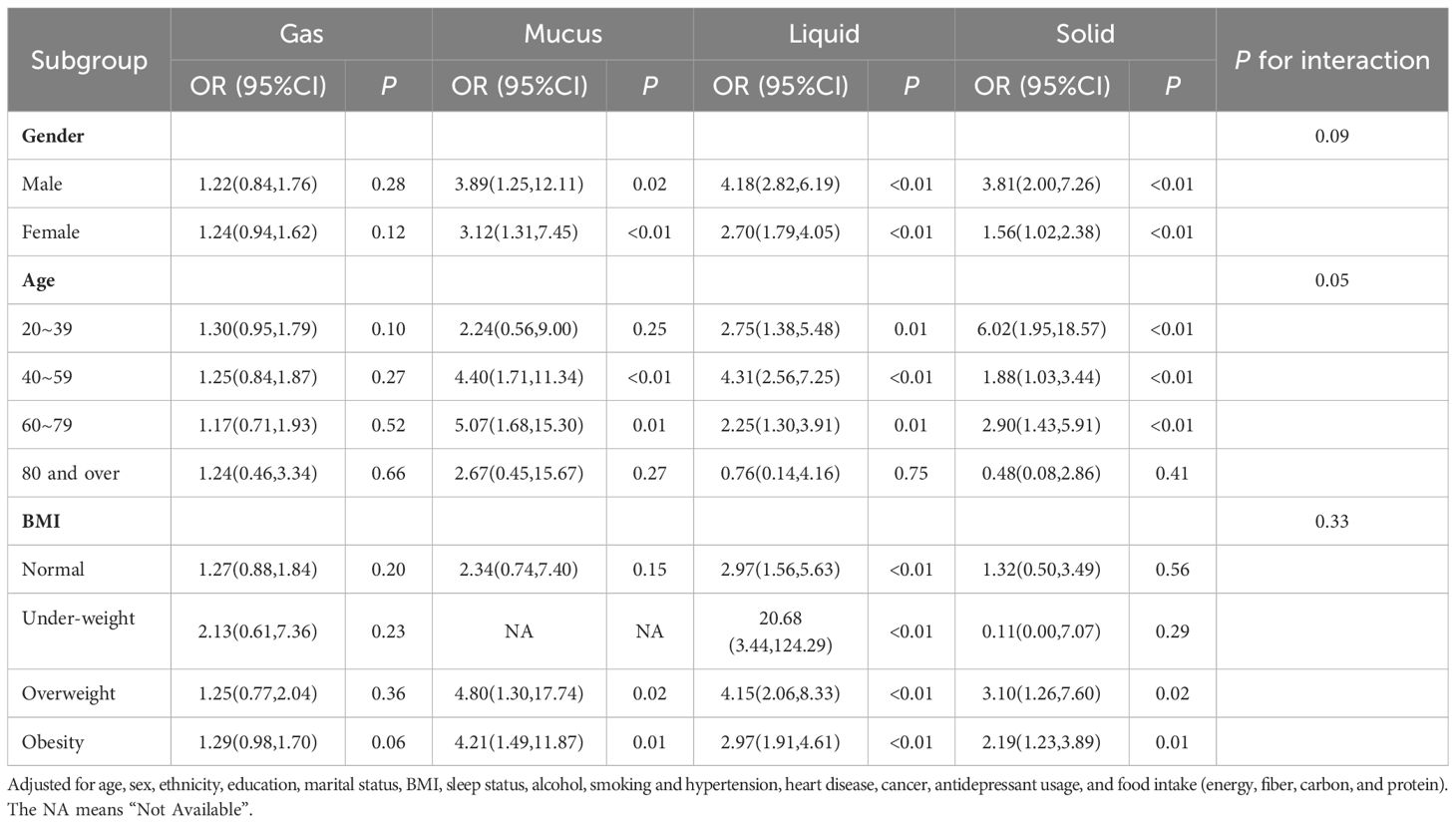
Subgroup analysis of association between bowel movements and depression was conducted according to fully adjusted multivariate logistic regression stratified by age, gender, and BMI (Table 2, Figure 2A). According to stratified analysis results, we discovered for those who were under 80 years old, overweight or obesity, constipation and diarrhea might increase the depression risk. The interaction test did not find any statistically significant differences among all subgroups. (P for interaction > 0.05).
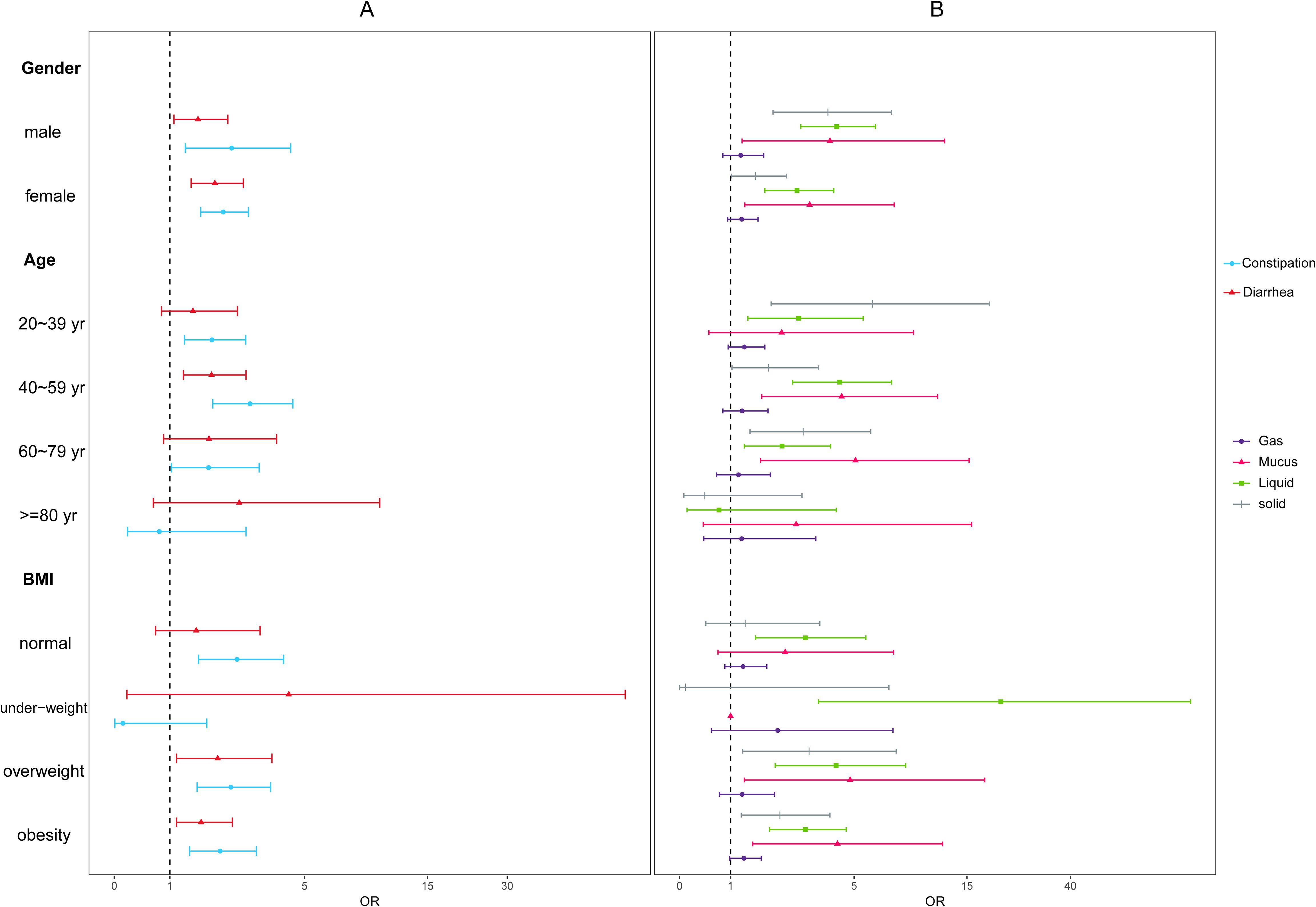
Figure 2. Subgroup analysis adjusted for age, sex, ethnicity, education, marital status, BMI, sleep status, alcohol, smoking and hypertension, heart disease, cancer, antidepressant usage, and food intake (energy, fiber, carbon, and protein) (A). Subgroup analysis of association between bowel movement and depression; (B). Subgroup analysis of association between fecal incontinence and depression.
Table 3 and Figure 2B showed the stratified analysis of association between fecal incontinence and depression. The result indicated that for those who were 40 to 59 year-old overweight or obesity participants, mucus, liquid and solid bowel leakage might increase the depression risk. For those with normal BMI, only liquid leakage would increase the depression risk (OR (95% CI): 2.97(1.56,5.63)). In addition, the interaction test did not find any statistically significant differences among all subgroups. (P for interaction > 0.05).
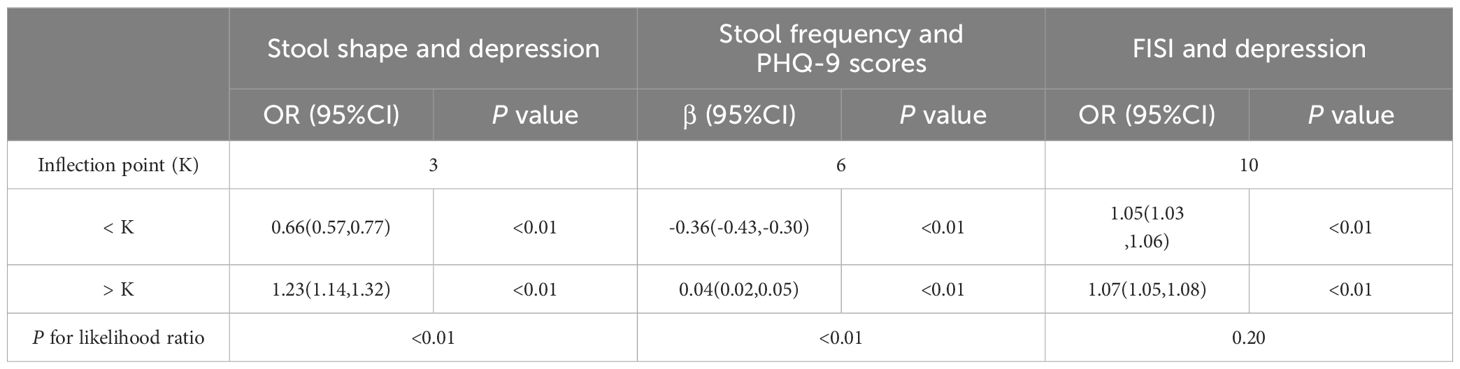
3.4 Non-linearity analysis between abnormal defecation and depression
We used restricted cubic spline (RCS) plots to explore the non-linear association of defecation disorders and depression (Figure 3). We built three RCS plots according to Model 3 by gender stratification. Figure 3A showed a ‘U-shape’ curve between the stool shape and depression (P for non-linear <0.05). Only when the stool shape represented as “like a sausage or snake, smooth and soft” (23), the odd ratio of depression was not increased. Furthermore, we found that overall inflection point was 3. Significant associations were found with the ORs (95% CI) of 0.66 (0.57, 0.77) after the inflection point and with the ORs (95% CI) of 1.23 (0.14, 1.32) before the inflection point (Table 4).
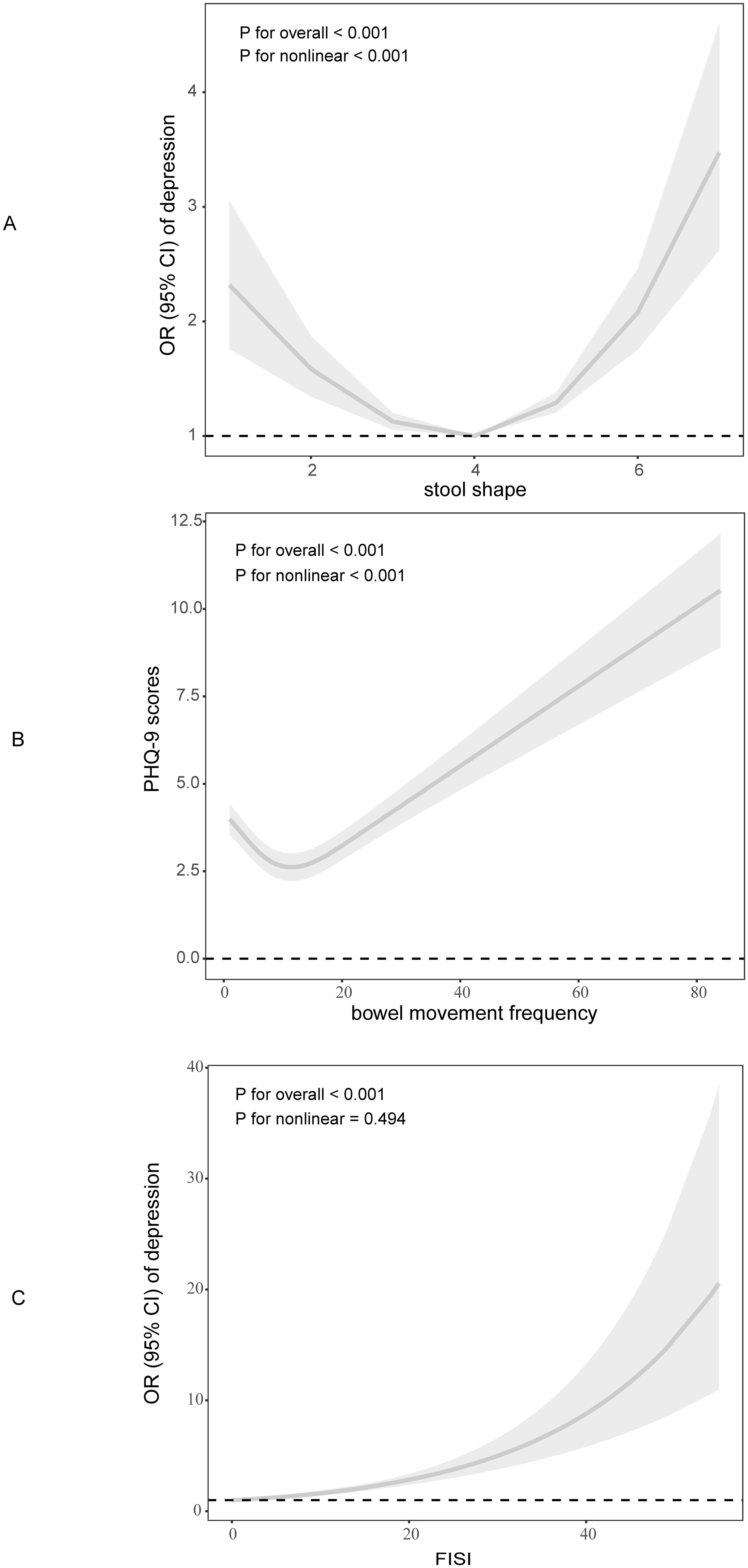
Figure 3. Dose-response connection of defecation disorders with depression based on full adjusted model. (A). Stool shape and depression; (B). Bowel movements frequency and PHQ-9 scores; (C). FISI and depression.
We further analyzed non-linear association between the bowel movement frequency and depression PHQ-9 scores (Figure 3B). The result indicated that there was a ‘J-shape’ curve between them (P for non-linear <0.05). The inflection point was 6 (Table 4). For those who have less than 6 bowel movements per week, the frequency of bowel movements was negatively associated with PHQ-9 scores, and positively associated with more than six bowel movements per week.
In Figure 3C, we illustrated the linear association between FISI scores and depression (P for non-linear > 0.05). High FISI scores are accompanied by a higher risk of depression.
3.5 Sensitivity assessments
Using unweighted logistic analysis indicated the similar results with previous analysis. Constipation, diarrhea, and fecal incontinence were all associated with depression (details in Supplementary Table 3). Then, we modified the adjusted factors to evaluate the robustness of the results. After adjusted for age, sex, ethnicity, education, marital status, BMI, sleep status, alcohol, smoking, antidepressant usage, and food intake in Model 3, the association between depression and bowel movement disorders remained (details in Supplementary Table 4). Furthermore, the Supplementary Table 5 showed the sensitivity analysis by re-defined depression as PHQ-9 score ≥8. The bowel movements were still related with depression. All the sensitivity analysis results represented that the association between bowel movement disorders and depression was stable.
4 Discussion
This study investigated the association between defecation disorders and the risk of depression in adults based on data from 2005 to 2010 NHANES. The results showed that constipation, diarrhea, and fecal incontinence had positive relations with the risk of depression after adjusting for potential factors. Of all the types of fecal incontinence, that of mucus is most likely to be combined with the presence of depression(OR (95%CI): 3.49 (1.63, 7.46)). The interaction test did not find any statistically significant differences among gender, age and BMI subgroups. Moreover, there was a significant “U-shaped” dose–response relation between the stool shape and the risk of depression. When the stool shape representing “sausage-like” with cracks on its surface or smooth and soft shape, the risk of depression was the lowest. A “J-shaped” dose–response relation between the stool frequency and the PHQ-9 scores was founded. Six bowel movements per week was considered to be the optimal frequency for lower PHQ-9 scores, in which case the risk of depression is lower. Our results indicated that the abnormal defecation was positively associated with the risk of depression.
Several studies have highlighted the link between constipation and depression. On one hand, a study showed that high anxiety level was the independent factors for predicting the perception of constipation (24). On the other hand, constipation might lead to a high risk of depressive symptoms. Shatri (25) found chronic functional constipation patients were commonly companied with depressive symptoms. Another study of a total of 1870 sample showed that constipation severely altered the participants’ quality of life (26). In addition, research showed the suicide mortality of acutely admitted patients was related to gastrointestinal disorders, especially constipation (27). Although there were previous studies from NHANES data illustrating that people with constipation and diarrhea were more likely to be found in depressed populations (7, 11), the data included was only one cycle of data from 2009-2010, whereas the present study included data from three cycles to make the results more convincing. Last year, Wang P et al. (28) published a study to illustrate the constipation was significantly associated with depression through NHANES 2005-2010. Of his results, the association between constipation and depression was not affected by age in both layers (<65 years old and ≥65 years old). However, our study divided age into four levels, and the results showed that the association was not significant in people aged 80 years and above. Besides, Wang P et al.’s study showed that there was no statistically significant association between constipation and depression in male, whereas our findings showed that both male and female, constipation and depression was associated. The discrepancy between the two studies may be due to different definitions of constipation and different adjustment factors. In addition, we consolidated data on fecal incontinence. Patients with fecal incontinence and concurrent constipation had poor overall quality of life (29) due to the stigma associated with fecal incontinence (30), which was consistent with our findings. In our study, diarrhea also increased the risk of depression for patients under 80 years old with BMI over 25 kg/m2, which was similar to Lu’s study (31).
To the best of our knowledge, this was the first study to explore the non-linear association between bowel movement and depression in a sizeable and complex cohort of American adults. Long L (32) found bowel movements frequency indicated the prognosis of hepatocellular carcinoma. Compared to those with daily bowel movements, participants with bowel movement more than once per day had a hazard ratio of 1.93. Another study illustrated the relationship between bowel frequency and cardiovascular disease and mortality of female. The result showed that compared with daily bowel movement, having bowel movements more than once daily was significantly associated with increased risk of cardiovascular disease (hazard ratio: 1.13) and total mortality (hazard ratio: 1.17) (33). Our study showed six times bowel movements per week corresponded to the lowest risk of depression, which was generally in line with the findings of the above studies. The non-linear association between stool shape and depression risk indicated type 3 of stool shape had the lowest risk of depression, in accordance with previous studies, fecal types 3, 4 and 5 were considered the most ‘normal’ stool shape (34).
The potential mechanisms behind the association between defecation problems and depression are unknown. However, the brain-gut axis may be involved in the association of diarrhea and constipation with depressive symptoms. Serotonin (5-HT) is an important modulator of microbiota-gut-brain axis. Zhou et al. found significant differences in gut microbiota between depressed patients and healthy controls. Transplanting fecal microbiota from healthy participants into depressed mice alleviated depressive symptoms by increasing 5-HT levels in the brain and colon of the mice (35). 5-HT interacts with receptors on the intestinal nervous system to modulate gut motility and to induce further signaling on emotion-regulating brain networks (36). Defects in the neural production of 5-HT might result in both mood disorders and intestinal dysfunction (37). Evidence showed that modulating the gut microbiome can alleviate depressive symptoms by regulating 5-HT metabolism (38). The correlations of behaviors and common metabolites showed that choline, betaine, and glycine metabolites were significantly associated with constipation and depression (39). In addition, patients with diarrhea-predominant irritable bowel syndrome were found have similar alterations in fecal microbiota with depression (40). Altogether, these studies suggest that the cooccurrence of depression and bowel disorders disturbs the gut microbiome. The peripheral signals from the microbiota may modulate the central processes causing depressive symptoms. Recent studies showed that probiotics could relieve the bowel movements (9, 41) and improve depressive symptoms (42–45), which is consistent with the point above. As for individuals with fecal incontinence, Cichowski et al. (46) found that women with fecal incontinence experienced more dyspareunia and fear than women without fecal incontinence. The unconscious bowel leakage might produce a feeling of being isolated, resulting in psychological and depressive symptoms (47, 48).
Several shortcomings of this study should be considered. First, the effects of medications were not considered in this study. Some antidepressants can lead to constipation (49) or diarrhea (50). Secondly, constipation and diarrhea are two general symptoms. Although the criteria for constipation and diarrhea were credible, the subtypes (for example, slow transit constipation or obstructive constipation) were not considered. Thirdly, bias was inevitable in cross-sectional studies, a large cohort study for further accurate evidence is still needed.
In summary, this study suggests that constipation, diarrhea, and fecal incontinence predict a higher risk of depression among adults. Further studies with bowel movement management and a prospective study design are warranted to confirm our observations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by NCHS Research Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LW: Writing – review & editing, Writing – original draft, Visualization, Software, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. MT: Writing – review & editing, Writing – original draft, Supervision, Resources, Methodology, Conceptualization. HS: Writing – review & editing, Supervision, Resources, Methodology, Conceptualization. JG: Writing – review & editing, Supervision, Investigation, Funding acquisition. WQ: Writing – review & editing, Visualization, Software. JX: Writing – review & editing, Methodology, Conceptualization. YA: Writing – review & editing, Methodology. WX: Writing – review & editing, Data curation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Hebei Provincial Administration of Traditional Chinese Medicine Scientific Research Programme (grant number, 2024015) and Hebei University of Chinese Medicine (grant number, XCXZZBS2023021).
Acknowledgments
We thank all participants and the NHANES research team for providing the data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1449948/full#supplementary-material
References
1. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502
2. Goodwin RD, Dierker LC, Wu M, Galea S, Hoven CW, Weinberger AH. Trends in U.S. Depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. (2022) 63:726–33. doi: 10.1016/j.amepre.2022.05.014
3. Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J Psychiatr Res. (2020) 126:134–40. doi: 10.1016/j.jpsychires.2019.08.002
4. Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry: J Ment Sci. (2018) 212:279–86. doi: 10.1192/bjp.2018.27
5. Friedrich MJ. Depression is the leading cause of disability around the world. Jama. (2017) 317:1517. doi: 10.1001/jama.2017.3826
6. Miner PB Jr. Economic and personal impact of fecal and urinary incontinence. Gastroenterology. (2004) 126:S8–13. doi: 10.1053/j.gastro.2003.10.056
7. Ballou S, Katon J, Singh P, Rangan V, Lee HN, McMahon C, et al. Chronic diarrhea and constipation are more common in depressed individuals. Clin Gastroenterol Hepatol: Off Clin Pract J Am Gastroenterological Assoc. (2019) 17:2696–703. doi: 10.1016/j.cgh.2019.03.046
8. Dennison C, Prasad M, Lloyd A, Bhattacharyya SK, Dhawan R, Coyne K. The health-related quality of life and economic burden of constipation. PharmacoEconomics. (2005) 23:461–76. doi: 10.2165/00019053-200523050-00006
9. Zhang X, Chen S, Zhang M, Ren F, Ren Y, Li Y, et al. Effects of fermented milk containing lacticaseibacillus paracasei strain shirota on constipation in patients with depression: A randomized, double-blind, placebo-controlled trial. Nutrients. (2021) 13:2238. doi: 10.3390/nu13072238
10. Adibi P, Abdoli M, Daghaghzadeh H, Keshteli AH, Afshar H, Roohafza H, et al. Relationship between depression and constipation: results from a large cross-sectional study in adults. Korean J Gastroenterol. (2022) 80:77–84. doi: 10.4166/kjg.2022.038
11. Wang Y, Shen X, Wang P. Constipation is associated with depression of any severity, but not with suicidal ideation: insights from a large cross-sectional study. Int J Colorectal Dis. (2023) 38:231. doi: 10.1007/s00384-023-04520-8
12. GBD 2016 Diarrhoeal Disease Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. (2018) 18:1211–28. doi: 10.1016/S1473-3099(18)30362-1
13. Wei Y, Fan Y, Huang S, Lv J, Zhang Y, Hao Z. Baizhu shaoyao decoction restores the intestinal barrier and brain-gut axis balance to alleviate diarrhea-predominant irritable bowel syndrome via FoxO1/FoxO3a. Phytomed: Int J Phytother Phytopharmacol. (2024) 122:155163. doi: 10.1016/j.phymed.2023.155163
14. Tamanini JTN, Franceschi Júnior O, Santos JLF, Duarte YAO, Sartori MGF, Girão M, et al. Fecal incontinence: incidence and risk factors from the SABE (Health, Wellbeing and Aging) study. Int Urogynecol J. (2022) 33:2993–3004. doi: 10.1007/s00192-021-04914-8
15. Bharucha AE, Knowles CH, Mack I, Malcolm A, Oblizajek N, Rao S, et al. Faecal incontinence in adults. Nat Rev Dis Primers. (2022) 8:53. doi: 10.1038/s41572-022-00381-7
16. NHANES. The National Health and Nutrition Examination Survey (2024). Available online at: https://www.cdc.gov/nchs/nhanes/index.htm (Accessed April 10, 2024).
17. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Internal Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
18. Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust. (2018) 209:86–91. doi: 10.5694/mja18.00241
19. Schiller LR, Pardi DS, Sellin JH. Chronic diarrhea: diagnosis and management. Clin Gastroenterol Hepatol. (2017) 15:182–93.e3. doi: 10.1016/j.cgh.2016.07.028
20. Bordeianou L, Rockwood T, Baxter N, Lowry A, Mellgren A, Parker S. Does incontinence severity correlate with quality of life? Prospective analysis of 502 consecutive patients. Colorectal Dis: Off J Assoc Coloproctol Great Britain Ireland. (2008) 10:273–9. doi: 10.1111/j.1463-1318.2007.01288.x
21. Kunduru L, Kim SM, Heymen S, Whitehead WE. Factors that affect consultation and screening for fecal incontinence. Clin Gastroenterol Hepatol. (2015) 13:709–16. doi: 10.1016/j.cgh.2014.08.015
22. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Jama. (2013) 309:71–82. doi: 10.1001/jama.2012.113905
23. Chumpitazi BP, Self MM, Czyzewski DI, Cejka S, Swank PR, Shulman RJ. Bristol Stool Form Scale reliability and agreement decreases when determining Rome III stool form designations. Neurogastroenterol Motility. (2016) 28:443–8. doi: 10.1111/nmo.12738
24. Cheng C, Chan AO, Hui WM, Lam SK. Coping strategies, illness perception, anxiety and depression of patients with idiopathic constipation: a population-based study. Alimentary Pharmacol Ther. (2003) 18:319–26. doi: 10.1046/j.1365-2036.2003.01663.x
25. Shatri H, Faisal E, Abdullah M, Syam AF, Utari AP, Muzellina VN, et al. Depression symptoms and inflammation in chronic functional constipation patients. Acta Med Indonesiana. (2023) 55:33–9.
26. Brochard C, Chambaz M, Ropert A, l’Héritier AM, Wallenhorst T, Bouguen G, et al. Quality of life in 1870 patients with constipation and/or fecal incontinence: Constipation should not be underestimated. Clinics Res Hepatol Gastroenterol. (2019) 43:682–7. doi: 10.1016/j.clinre.2019.02.011
27. Roberts SE, John A, Kandalama U, Williams JG, Lyons RA, Lloyd K. Suicide following acute admissions for physical illnesses across England and Wales. psychol Med. (2018) 48:578–91. doi: 10.1017/S0033291717001787
28. Wang P, Shen X, Wang Y, Jia X. Association between constipation and major depression in adult Americans: evidence from NHANES 2005-2010. Front Psychiatry. (2023) 14:1152435. doi: 10.3389/fpsyt.2023.1152435
29. Cauley CE, Savitt LR, Weinstein M, Wakamatsu MM, Kunitake H, Ricciardi R, et al. A quality-of-life comparison of two fecal incontinence phenotypes: isolated fecal incontinence versus concurrent fecal incontinence with constipation. Dis Colon Rectum. (2019) 62:63–70. doi: 10.1097/DCR.0000000000001242
30. McKenna C, Bartlett L, Ho YH. Fecal incontinence reduces quality of life more than you may think. Dis Colon Rectum. (2017) 60:e597–e8. doi: 10.1097/DCR.0000000000000832
31. Lu J, Shi L, Huang D, Fan W, Li X, Zhu L, et al. Depression and structural factors are associated with symptoms in patients of irritable bowel syndrome with diarrhea. J Neurogastroenterol Motility. (2020) 26:505–13. doi: 10.5056/jnm19166
32. Long L, Liu X, Jin L, Simon T, Ma W, Kim MN, et al. Association of bowel movement frequency and laxative use with risk of hepatocellular carcinoma in US women and men. Int J Cancer. (2021) 149:1529–35. doi: 10.1002/ijc.33699
33. Ma W, Li Y, Heianza Y, Staller KD, Chan AT, Rimm EB, et al. Associations of bowel movement frequency with risk of cardiovascular disease and mortality among US women. Sci Rep. (2016) 6:33005. doi: 10.1038/srep33005
34. Blake MR, Raker JM, Whelan K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Alimentary Pharmacol Ther. (2016) 44:693–703. doi: 10.1111/apt.13746
35. Zhou M, Fan Y, Xu L, Yu Z, Wang S, Xu H, et al. Microbiome and tryptophan metabolomics analysis in adolescent depression: roles of the gut microbiota in the regulation of tryptophan-derived neurotransmitters and behaviors in human and mice. Microbiome. (2023) 11:145. doi: 10.1186/s40168-023-01589-9
36. Aaldijk E, Vermeiren Y. The role of serotonin within the microbiota-gut-brain axis in the development of Alzheimer’s disease: A narrative review. Ageing Res Rev. (2022) 75:101556. doi: 10.1016/j.arr.2021.101556
37. Israelyan N, Del Colle A, Li Z, Park Y, Xing A, Jacobsen JPR, et al. Effects of serotonin and slow-release 5-hydroxytryptophan on gastrointestinal motility in a mouse model of depression. Gastroenterology. (2019) 157:507–21.e4. doi: 10.1053/j.gastro.2019.04.022
38. Ma J, Wang R, Chen Y, Wang Z, Dong Y. 5-HT attenuates chronic stress-induced cognitive impairment in mice through intestinal flora disruption. J Neuroinflammation. (2023) 20:23. doi: 10.1186/s12974-023-02693-1
39. Liu X, Liu H, Wei F, Zhao D, Wang Y, Lv M, et al. Fecal metabolomics and network pharmacology reveal the correlations between constipation and depression. J Proteome Res. (2021) 20:4771–86. doi: 10.1021/acs.jproteome.1c00435
40. Liu Y, Zhang L, Wang X, Wang Z, Zhang J, Jiang R, et al. Similar fecal microbiota signatures in patients with diarrhea-predominant irritable bowel syndrome and patients with depression. Clin Gastroenterol Hepatol. (2016) 14:1602–11.e5. doi: 10.1016/j.cgh.2016.05.033
41. Shang X, FF E, Guo KL, Li YF, Zhao HL, Wang Y, et al. Effectiveness and safety of probiotics for patients with constipation-predominant irritable bowel syndrome: A systematic review and meta-analysis of 10 randomized controlled trials. Nutrients. (2022) 14:2482. doi: 10.3390/nu14122482
42. Kim CS, Cha L, Sim M, Jung S, Chun WY, Baik HW, et al. Probiotic supplementation improves cognitive function and mood with changes in gut microbiota in community-dwelling older adults: A randomized, double-blind, placebo-controlled, multicenter trial. J Gerontol Ser A Biol Sci Med Sci. (2021) 76:32–40. doi: 10.1093/gerona/glaa090
43. Liu RT, Walsh RFL, Sheehan AE. Prebiotics and probiotics for depression and anxiety: A systematic review and meta-analysis of controlled clinical trials. Neurosci Biobehav Rev. (2019) 102:13–23. doi: 10.1016/j.neubiorev.2019.03.023
44. Pinto-Sanchez MI, Hall GB, Ghajar K, Nardelli A, Bolino C, Lau JT, et al. Probiotic bifidobacterium longum NCC3001 reduces depression scores and alters brain activity: A pilot study in patients with irritable bowel syndrome. Gastroenterology. (2017) 153:448–59.e8. doi: 10.1053/j.gastro.2017.05.003
45. Tian P, Chen Y, Zhu H, Wang L, Qian X, Zou R, et al. Bifidobacterium breve CCFM1025 attenuates major depression disorder via regulating gut microbiome and tryptophan metabolism: A randomized clinical trial. Brain Behav Immun. (2022) 100:233–41. doi: 10.1016/j.bbi.2021.11.023
46. Cichowski SB, Komesu YM, Dunivan GC, Rogers RG. The association between fecal incontinence and sexual activity and function in women attending a tertiary referral center. Int Urogynecol J. (2013) 24:1489–94. doi: 10.1007/s00192-013-2044-8
47. Yip SO, Dick MA, McPencow AM, Martin DK, Ciarleglio MM, Erekson EA. The association between urinary and fecal incontinence and social isolation in older women. Am J Obstetrics Gynecol. (2013) 208:146.e1–7. doi: 10.1016/j.ajog.2012.11.010
48. Kemp K, Griffiths J, Lovell K. Understanding the health and social care needs of people living with IBD: a meta-synthesis of the evidence. World J Gastroenterol. (2012) 18:6240–9. doi: 10.3748/wjg.v18.i43.6240
49. Oliva V, Lippi M, Paci R, Del Fabro L, Delvecchio G, Brambilla P, et al. Gastrointestinal side effects associated with antidepressant treatments in patients with major depressive disorder: A systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 109:110266. doi: 10.1016/j.pnpbp.2021.110266
Keywords: NHANES, depression, constipation, diarrhea, fecal incontinence
Citation: Wang L, Tian M, Sun H, Gao J, Qi W, Xu J, An Y and Xu W (2024) Association between bowel movement disorders and depressive symptoms: a cross-sectional study. Front. Psychiatry 15:1449948. doi: 10.3389/fpsyt.2024.1449948
Received: 16 June 2024; Accepted: 28 August 2024;
Published: 17 September 2024.
Edited by:
Luca Steardo, University Magna Graecia of Catanzaro, ItalyReviewed by:
Peijun Ju, Shanghai Mental Health Center, ChinaHongcheng Lin, The Sixth Affiliated Hospital of Sun Yat-sen University, China
Copyright © 2024 Wang, Tian, Sun, Gao, Qi, Xu, An and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jihua Gao, emhzdmRkc0BzaW5hLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Linyue Wang
Linyue Wang Maosheng Tian
Maosheng Tian Hongyuan Sun1,2†
Hongyuan Sun1,2† Jihua Gao
Jihua Gao