- 1Mental Health Research and Treatment Center, Ruhr-University Bochum, Bochum, Germany
- 2Center of Excellence for Suicide Prevention, VA Finger Lakes Health Care System, Canandaigua, NY, United States
- 3Department of Psychiatry, University of Rochester Medical Center, Charleston, SC, United States
- 4Department for Clinical Psychology and Psychotherapy, University of Duisburg-Essen, Essen, Germany
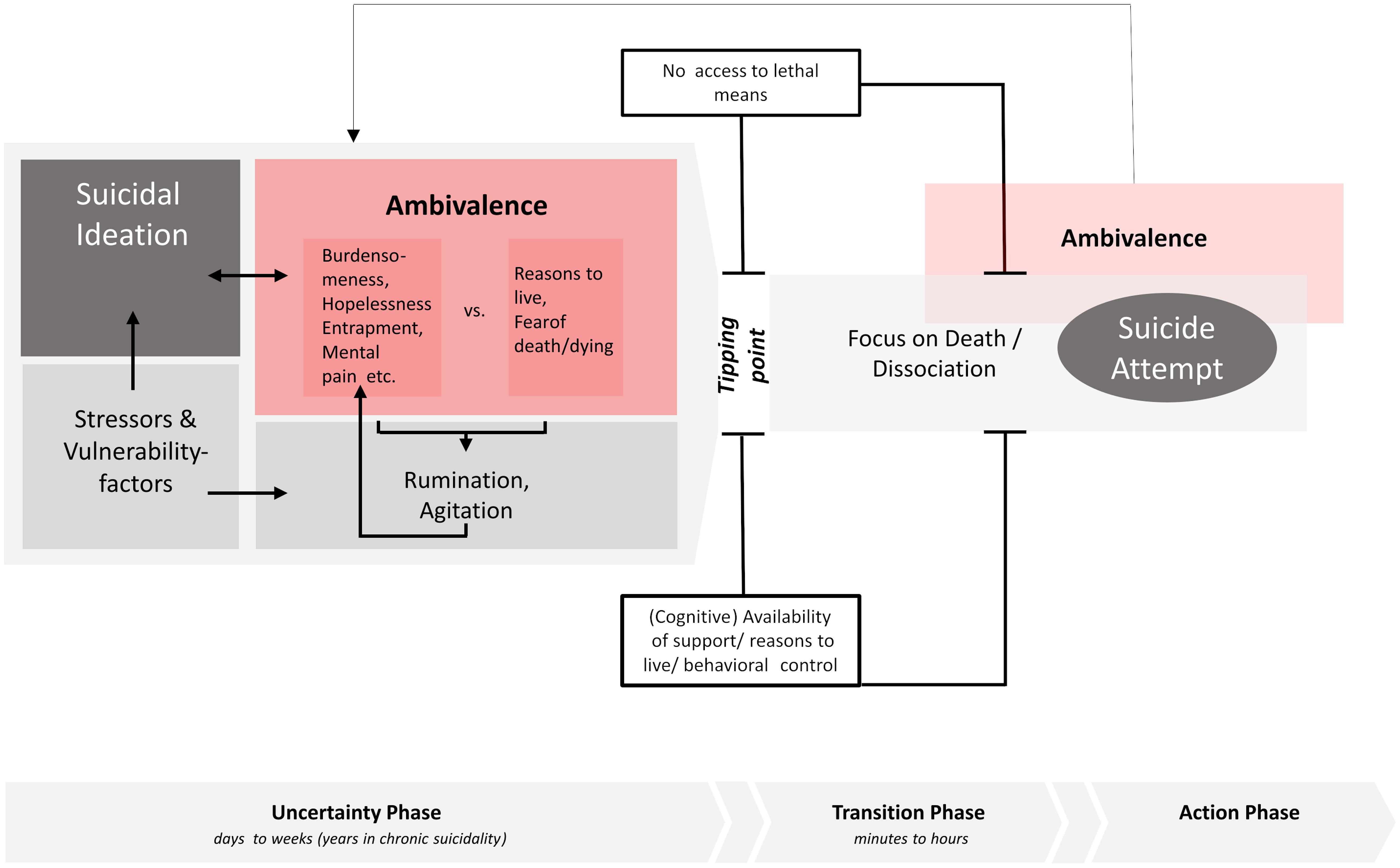
The existing models for understanding suicidal ideation and behavior do not provide satisfactory orientation for clinical-therapeutic work with suicidal clients. Based on the observation that ambivalence accompanies the entire suicidal process and building on the empirical knowledge about suicidal ambivalence, this article presents the ambivalence model of suicidality (ABS model), a new clinical working model that aims to provide a framework for risk assessment, case conceptualization and treatment planning in the treatment of suicidal individuals. The model divides the suicidal process into three phases (uncertainty phase, transition phase and action phase), describes the psychological state within the different phases, and identifies phase-specific therapeutic interventions. The ABS model is a descriptive model that can be used to structure and organize crisis intervention and psychotherapy with suicidal patients.
1 Introduction
Suicidal ideation and behaviour are very common in clinical populations (1). The intensity of suicidal ideation is subject to considerable fluctuations (2). While suicidal ideation does not lead to suicidal behaviour in the vast majority of those affected (3), people who have attempted suicide generally report very rapid transitions from suicidal ideation to suicidal behaviour (4, 5). The considerable dynamics of suicidal ideation and behaviour - in addition to other factors (6) - make it incredibly difficult to reliably assess a person’s suicide risk (7, 8). In addition, a wide variety of constellations of stress factors can lead to suicidal behaviour (9) and suicidal experience and behaviour is therefore motivated very differently in individual cases (10). Treatment approaches for suicidal patients must do justice to this ‘individuality’ of suicidal ideation and behaviour (11).
In this sense, a model of suicidal ideation and behaviour is required, which on the one hand provides clinicians with a framework of understanding and orientation for the exploration and treatment of suicidal patients in clinical practice and on the other hand can be used as an explanatory model for patients in the context of psychoeducation (12). Therapy-related elaborations of common theoretical models of suicidal ideation and behaviour - such as the Interpersonal Theory of Suicidal Behaviour (ITS; 13), the Integrative Motivational-Volitional Model of Suicidal Behaviour (IMV model; 14), or the 3-Steps-Theory (3-ST; 15) - have not yet been developed. All three models can be credited with inspiring research activity and significantly expanding our knowledge of suicidal ideation and behavior. However, it can be questioned whether these models can provide a sufficient framework for individualised clinical-therapeutic work with suicidal individuals due to their focus on individual, very specific factors, that may not resonate with every suicidal person. Another concern is that these models are primarily unidirectional, representing the factors that propel an individual towards suicidal behavior, with minimal consideration of the countervailing factors that protect against it.
Against this background, this article presents a clinical working model that aims to provide a framework for risk assessment, case conceptualization and treatment planning in the treatment of suicidal individuals. At the core of the model stands the observation that ambivalence towards suicide/death accompanies the entire suicidal process of many affected individuals (16): Suicidal individuals report an internal struggle between a wish to die and a wish to live before, during and after suicidal behaviour (e.g., 17–19). Suicide ambivalence offers a therapeutic starting point in different phases of the suicidal process (20, 21) and by exploring the “internal suicide debate” (22), – with intent to “resolve” it towards living (23) –, both individually significant risk and protective factors come into view. In this sense, a focus on suicide ambivalence not only serves to motivate those affected to take a first step back from acting on a suicide wish (20, 23–26), but also informs case conceptualization and treatment planning (cf. 11).
The ambivalence model of suicidality (ABS model) divides the suicidal process into three phases: the uncertainty phase, the transition phase and the action phase (see Figure 1).
The model focuses on the process leading up to a suicide attempt (and not a suicide). This focus is due to the fact that most of our empirical knowledge about suicidal acts comes from the study of individuals who have survived a suicide attempt and are thus able to participate in research and provide insight into the suicidal process. It is unclear whether these findings can be equally applied to individuals who have died by suicide. In the following, the suicidal process is described in relation to the three phases and phase-specific information on (therapeutic) interventions are provided.
2 Uncertainty phase
The possibility of suicide usually comes into focus when individuals are exposed to significant and/or multiple stressors (separation, death, unemployment, financial loss, physical illness, trauma (27);) and/or suffer from a mental disorder (28); in the case of prolonged stress and suicidal thoughts, even minor mood changes may be sufficient to activate a more intensive preoccupation with suicidal desires (12, 29, 30). Given the significance of a suicide decision and the difficulty of enacting suicidal behavior, it is to be expected that those affected will enter a phase of ambivalence. Indeed, 94% of suicidal individuals affirmed to have ever had an internal debate about whether to live or die in a survey study (22). Accordingly, Shneidman (31) refers to ambivalence as a cognitive state “that occurs in almost every case of suicide” (p. 129), and Evans and Farberow (32) emphasize ambivalence as “perhaps the most important psychological concept in our understanding of suicide” (p. 12). Ambivalence refers to the simultaneous existence of mutually exclusive attitudes and action tendencies. The term suicidal ambivalence refers to the fact that reasons/wishes to die (e.g., “I can’t bear the pain any longer”) are experienced simultaneously with reasons/wishes to live (e.g., “I want to be there for my daughter”) or to not die (e.g., “I’m afraid of the pain involved in killing oneself”). Of course, ambivalence can vary greatly in intensity and some individuals may not explicitly express ambivalence, but ambivalence rather reveals itself through the usage of words such as “maybe”, “not now”, and “possibly” when talking about suicidal intentions (33).
Reasons for dying are heterogenous and might be associated with physical health issues, relationship problems, the desire to escape, loneliness, a negative self-perception, hopelessness and financial difficulties (34). Moreover, reasons for dying cover all the perceptions that have been identified as central risk factors in the different suicide theories (cf. 10): I am a burden and others would be better off if I were dead (perceived burdensomeness; 13). I don’t really belong anywhere/I am not important to anyone (thwarted belongingness; 13). My situation will never change, it is hopeless (hopelessness; 35). I am trapped in a hopeless situation (entrapment; 14, 36). I just can’t take the thoughts/memories anymore; (unbearability; 35). The feelings are so bad; it’s like physical pain, I can’t stand them any more (mental pain/psychache; 15, 31). Within the ABS model, no weighting of the different perceptions is specified (cf. 12), allowing for suicidal individuals to share their understanding of which factors (“reasons”) they experience as particularly stressful/important and in this sense are to be understood as personally relevant “suicide drivers” (11).
Reasons to die are countered by reasons to live and/or reasons not to die. Reasons to live include themes such as family/friends (“I don’t want my husband to think I didn’t love him”), future plans (“There are still things on my bucket list”), enjoyable things (“I could never go swimming again if I were dead”), self-image (“I don’t want anyone to think I was a coward”) and religion (“My religion forbids suicide”; 37). In addition, aspects such as fear of the pain involved in dying, fear of death (13, 38), and/or fear of emerging disabled from a suicide attempt, that is reasons against dying (“I would so like to be dead, but I don’t dare”), might also have an equivalent effect on suicidal ambivalence.
The strength of the two sides of suicidal ambivalence can vary to a great deal (39). Furthermore, studies showing considerable fluctuations in suicidal thoughts throughout the day (2, 40–42) suggest that the relative importance of reasons to die and reasons to live might also be subject to rapid changes. Finally, it has to be highlighted that even though it is a good thing, if suicidal individuals are (still) ambivalent rather than leaning towards suicide, the experience of ambivalence can be an exhausting and stressful state (43) and ambivalence in itself can therefore represent internal dissonance that can be an additional stressor (“I just can’t stand this back and forth in my head anymore”). There is furthermore a risk that persistent ambivalence contributes to persistent rumination and in consequence, to symptoms of overarousal, sleep problems or agitation that may in turn be associated with increased suicidal thoughts or behavior (44, 45). In addition, persistent ambivalence might also prevent individuals from engaging with life and its challenges, resulting in long-lasting and easily activated (chronic) suicidal ideation. It is therefore important to support suicidal individuals in resolving suicidal ambivalence and/or to step out of a constant engagement with suicidal ambivalence.
The uncertainty phase can last minutes, days, weeks or – in the case of chronic suicidal ideation – even years. However, it seems that there are also people who never enter this phase, but immediately transition to the action phase: As such, Bryan, Allen (46) found that 17% of individuals who attempted suicide did so without ever having suffered from suicidal ideation or having made a suicide plan beforehand (cf. 47). Such cases cannot be understood in the sense of the uncertainty phase. Yet, for some proportion of this group, this may not matter from a therapeutic perspective, as practitioners only get to know these patients after a suicide attempt (if at all).
2.1 Therapeutic implications
Therapeutically, it follows from the understanding of the uncertainty phase that both sides of the suicidal ambivalence have to be explored in detail (see Figure 2). This pursues two goals: On the one hand, the aim is to get the person into contact with their ambivalence, to empathically validate reasons for dying and to make reasons for living emotionally salient (48). In this way, those affected should be motivated to stay alive (for the time being) and to accept therapeutic support. The literature on Motivational Interviewing with suicidal individuals, for example, gives detailed instructions on how this can be done (20, 23–26, see also 11). On the other hand, the precise exploration of the reasons for/against dying/living serves to come up with a case conceptualization and an individualized treatment plan that targets both the individuals’ personal reasons for dying and reasons for living. A person whose suicidal ideation is driven by perceptions of perceived burdensomeness, for example, possibly needs different therapeutic interventions than a person whose suicidal ideation is driven by perceptions of thwarted belongingness or entrapment (49). In conclusion, the reasons for dying specify what further treatment must focus on. Finally, significant reasons for living define the resources that can be drawn on in the context of crisis management (50).
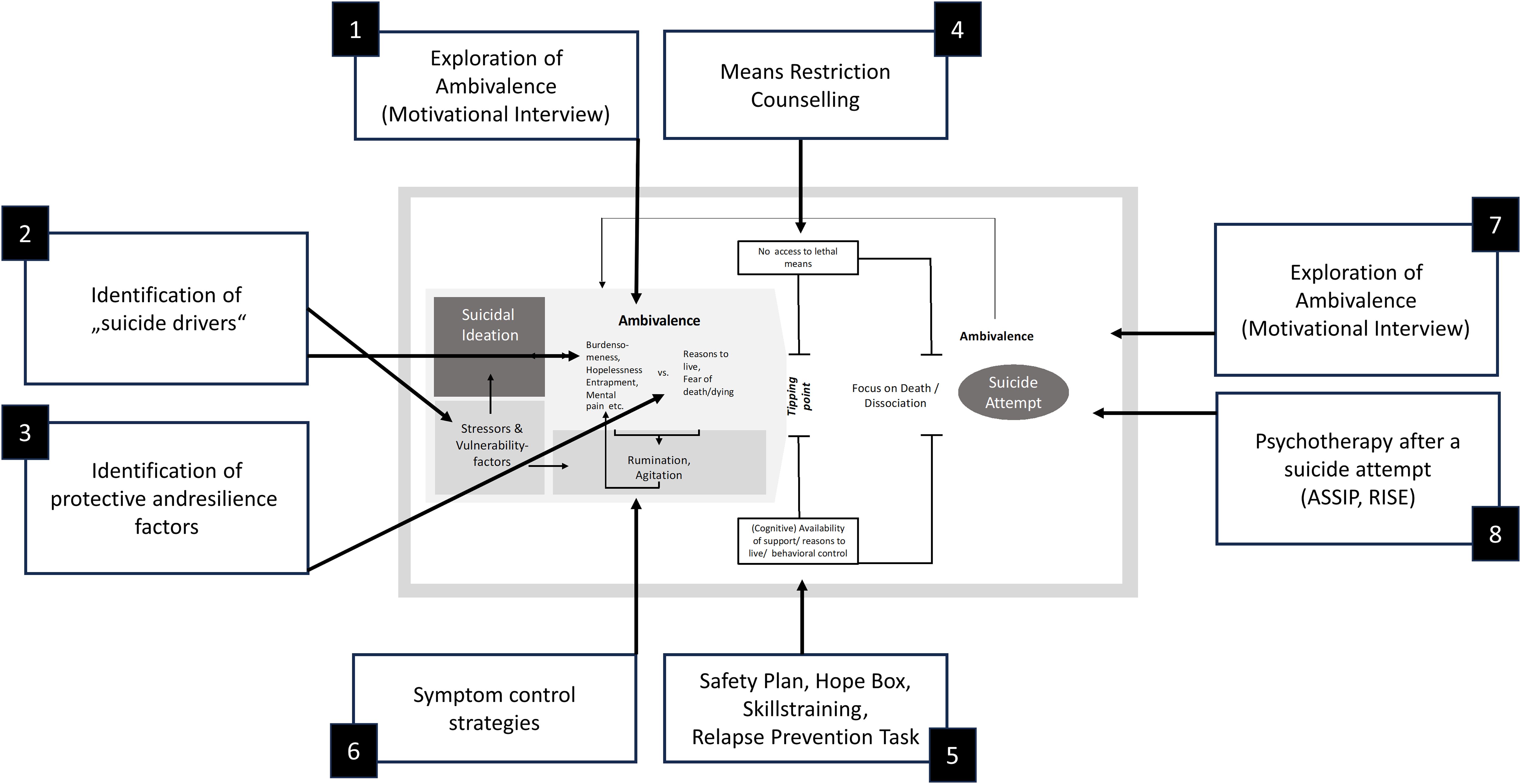
Figure 2. Therapeutic interventions. ASSIP, Attempted Suicide Short Intervention Program (Gysin-Maillart, 2021) (76); RISE, Relapse Intervention after Suicidal Event (Bahlmann et al., 2022) (75).
Ambivalence-focused interventions also aim to contribute to a reduction in (suicide-specific) rumination and, as a result, a reduction in symptoms of overarousal. However, further interventions for dealing with symptoms of rumination/dissociation/insomnia/panic may have to be integrated into a comprehensive treatment plan (12, 49, 51, 52). Finally, it should be noted that stressors and vulnerability factors underlying the individual reasons for dying may also require specific therapeutic attention. In the case of traumatization, trauma therapy may be required to support amelioration of suicidal ideation (53, 54), perfectionism may need to be addressed (55), or individuals have to be supported in making contact with specialized counselling agencies (for example regarding debt, abortion or refugee aid).
3 Transition and action phase
With the decision to die by suicide, those affected leave the uncertainty phase and enter the transition phase. The transition phase, therefore, describes suicidal individuals in a state of imminent suicide risk. Whether and when suicidal individuals enter the transition phase cannot be predicted; some authors speak of a “mental accident” in which behavioral control over suicidal impulses (suddenly) fails (56), others speak of coincidence (57) and within dynamic systems approaches (29) the term tipping points is used to characterize the sudden shift into a state of acute suicidality. From qualitative studies, it is known that ambivalence does not have to be resolved in order to enter the transition phase; rather, for some individuals, ambivalence seems to be pushed aside at these moments (58).
Access to lethal means is arguably the single most important factor within the transition to suicidal behavior: Knowledge and availability of lethal means appear to be relevant risk factors for suicidal behavior (59, 60) and restricting access to lethal means is considered one of the most effective methods of suicide prevention (61). A lack of (immediate) availability of lethal means may therefore, on the one hand, protect against entering the transition phase in the first place and, on the other hand, help to prevent a transition to the action phase, i.e., the enactment of suicidal behavior. A second factor that potentially determines whether people enter the transition phase or leave the transition phase unscathed is the (cognitive) availability of (professional/private) supporters, reasons to live and skills in dealing with emotional turmoil (62). Interventions like safety plans (63), crisis response plans (12), hope boxes (64) and skills training (51), all focus on strengthening self-management when dealing with suicidal urges.1
Michel (65) highlights the importance of a dissociative state of mind in the immediate run-up to a suicidal act (cf. 66). Suicidal individuals in the transition phase describe an all-embracing “focus on death” (31, 35, 67); to outsiders, the suicidal person may appear “zombie-like” rather than emotionally agitated (68), a “thousand yards stare” (69) seems to characterize some. In general, the transition phase seems to be rather brief: When asked about the time that passed between the decision to die by suicide and the suicidal act, up to 48% of suicide attempters reported a period of less than 10 minutes (5, 70, see also 71). This points to the considerable dynamic of a suicidal crisis.
A peaceful exit from the transition phase is nevertheless possible, however, it often depends on coincidence: the phone rings, the cats scratch at the door, one is approached by a by-stander; or, to put it differently: something happens that “bursts the bubble” (68) the suicidal individual is captured in. Unavailability of lethal means or a sudden reminder of important social partners may also help to live through the transition phase: In such cases suicidal ambivalence might kick in again and a suicide attempt is aborted before the act of killing has been initiated or even shortly after the suicidal act has been initiated. In this sense, 50% of suicide attempters reported in one study that they were still ambivalent during the suicide attempt (18); ambivalence thus seems to accompany the whole suicidal process (72). In this regard, it has to be emphasized that ambivalence does not only refer to a simultaneity of conflicting motives, but can also refer to rapid temporal changes in dominant motives (diachronic ambivalence). It should also be emphasized that the ambivalence experienced at this point in the suicidal process may focus on different questions than during the uncertainty phase. For example, for methods that take time such as overdose, cutting, or hanging individuals may ask “Should I call an ambulance?” or “Should I carry on despite the pain?”. However, the underlying ambivalence for and against dying is potentially composed in the same way as the ambivalence experienced during the uncertainty phase.
3.1 Therapeutic implications
Therapeutically, it follows from this understanding of the transition and action phases that suicidal individuals have to become prepared for dealing with strong suicidal impulses and urges: Means restriction counselling (25), safety planning (12, 63), creating a hope box (12, 48), skills training (12, 51) are suitable interventions, in that they support suicidal individuals to establish behavioral control in dealing with suicidal impulses and might prevent them from entering the transition and action phases (see Figure 2), and step back into the uncertainty phase.
Interventions in dealing with immediate suicidality are not fundamentally different from strategies used in less acute crisis intervention situations. Still, the starting point is naturally different: the person must first step back from the edge of a tower block, put down a gun, untie a rope; that means a cautious approach and an offer of conversation based on understanding and respect is required. As the conversation progresses, a gentle focus on suicidal ambivalences (21, 73) may then become possible. Initiatives such as the British Samaritans’ “Smalltalks save lives” campaign (www.samaritans.org/support-us/campaign/small-talk-saves-lives/) focus on the fact that cognitive constriction/dissociation (“focus on death”) in the transition phase can also be softened by lay people with the help of small measures – speaking up, being present and showing sympathy (68). It should be noted, that in the case of more severe dissociation, a more resolute approach in order to break this dissociation might be indicated – still, however, based on careful listening and understanding of what the individual needs and respect of his or her personhood.
4 Post-attempt phase
In the aftermath of a suicide attempt, 36% to 43% of suicide attempters report that they feel ambivalent about having survived, while 35% are glad to have survived and 14% to 22% regret having survived (17, 74); as such some, but not all individuals will re-enter the uncertainty phase after a suicide attempt. Depending on the individual reaction to survival, a different approach is needed to motivate suicide attempters to come to terms with the suicide attempt, with the prospect of continuing to live, and therefore to prevent future suicidal acts. An ambivalence-friendly approach that takes the experience of shame and stigma into account, psychoeducation and brief therapeutic interventions (75, 76) appears to be suitable for this. In this context, it should be noted that quite a few suicide attempters appear to show signs of post-traumatic stress disorder after a suicide attempt (77) – a low demand for therapeutic treatment of a suicide attempt (78) may therefore also be associated with trauma-related avoidance behavior and must be taken into account therapeutically.
5 Discussion
Suicidal ambivalence accompanies the entire suicidal process (31) and offers a therapeutic starting point to motivate suicidal individuals to postpone a decision to die by suicide, to engage in treatment, to establish a different way of dealing with suicidal ideation (20, 23–25) and to explore “suicide drivers” (31) as well as resilience factors. By emphasizing the significance of ambivalence, the ABS model presented here attempts to provide a framework for understanding and treating suicidal individuals. The model does not claim to be able to predict who is at particularly high risk of suicide; in this sense, the model is less explicative than descriptive. As mentioned already, the model furthermore does not assume that every person goes through the described phases in the same way. It should also be clear that the core focus of the model, the experience of ambivalence, is not experienced in the same way by every suicidal person throughout the entire process. Ambivalence is a fluid state that is characterized by inter- and intra-individual variability. Research has shown that suicidal ideation and related risks and warning signs show substantial between- and within subject variance (79). For instance, Hallensleben and colleagues (2) could demonstrate that if measured 10 times a day across seven days, 36% of the variance in active suicidal ideation is accounted for by within-person-variability (see also e.g., 41, 42). It can be inferred that the strength of protective factors may also fluctuate over time, which would mean that suicidal ambivalence (the sum of risk and protective factors) also fluctuates over time. We assume that suicidal ambivalence also shows individual trajectories. It is conceivable that these trajectories differ depending on variables such as age, gender, or cultural backgrounds. The extent to which the assumptions of the model presented here are generally valid independently of age, gender, etc. should be investigated in future studies.
It should also be noted that despite the widespread consensus that ambivalence is a core characteristic of suicidal individuals (31, 32), there is comparatively little high-quality empirical research on suicidal ambivalence (16). The same applies to the description of the mental state of suicidal persons in the transition phase (65). In view of this, various model descriptions of the ABS model must be regarded as provisional. Additional research on the topic of suicidal ambivalence appears warranted. Future studies should aim to verify central assumptions of the model, such as the positive loop between stressors and vulnerability factors, suicidal ideation, ambivalence and rumination/agitation. Prospective studies are of particular interest for this purpose. It would also be important to investigate the trajectories of protective factors and suicidal ambivalence over the course of a suicidal crisis. For all these research endeavors, the use of Ecological Momentary Assessments (EMA) seems particularly promising. EMA allows a repeated assessment of participants in their natural environment (80) and permits capturing moment-to-moment variations in psychological and behavioral variables and calculating relations between the constructs within and across sampling moments. This method has gained much interest in suicidology in recent years (81) and might help to gain a greater understanding of the complex and dynamic interrelations between the variables of the model.
Further, most clinical interventions being studied today address ambivalence in some way, but a comprehensive description of similarities and differences across these interventions, as well as potential implication of the promoted strategies is beyond the scope of this particular article. However, none of this changes the fact that the model parameters can already be used as an orientation framework for the treatment of suicidal patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
TT: Conceptualization, Visualization, Writing – original draft, Writing – review & editing. PB: Conceptualization, Writing – review & editing. TF: Conceptualization, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
- ^ Please note that a detailed description of suicide-specific interventions and treatment manuals is beyond the scope of the present article.
References
1. Teismann T, Forkmann T, Glaesmer H, Alpers GW, Brakemeier EL, Brockmeyer T. Prevalence of suicidal ideation in German psychotherapy outpatients: a large multicenter assessment. J Affect Disord. (2024) 351:971–6. doi: 10.1016/j.jad.2024.02.019
2. Hallensleben N, Glaesmer H, Forkmann T, Rath D, Strauss M, Kersting A, et al. Predicting suicidal ideation by interpersonal variables, hopelessness and depression in real-time. An ecological momentary assessment study in psychiatric inpatients with depression. Eur Psychiatry. (2019) 56:43–50. doi: 10.1016/j.eurpsy.2018.11.003
3. Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. psychol Med. (2016) 46:225–36. doi: 10.1017/S0033291715001804
4. Deisenhammer EA, Ing CM, Strauss R, Kemmler G, Hinterhuber H, Weiss EM. The duration of the suicidal process: how much time is left for intervention between consideration and accomplishment of a suicide attempt? J Clin Psychiatry. (2009) 70:19–24. doi: 10.4088/JCP.07m03904
5. Paashaus L, Forkmann T, Glaesmer H, Juckel G, Rath D, Schönfelder A, et al. From decision to action: suicidal history and time between decision to die and actual suicide attempt. Clin Psychol Psychother. (2021) 28:1427–34. doi: 10.1002/cpp.2580
6. Teismann T, Forkmann T, Glaesmer H. Suicide risk assessment: is it possible]? Verhaltenstherapie. (2019) 29:80–4. doi: 10.1159/000493887
7. Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. psychol Bull. (2017) 143:187. doi: 10.1037/bul0000084
8. Woodford R, Spittal MJ, Milner A, McGill K, Kapur N, Pirkis J, et al. Accuracy of clinician predictions of future self-harm: A systematic review and meta-analysis of predictive studies. Suicide Life-Threatening Behav. (2019) 49:23–40. doi: 10.1111/sltb.12395
9. Huang X, Ribeiro JD, Franklin JC. The differences between suicide ideators and suicide attempters: simple, complicated, or complex? J Consulting Clin Psychol. (2020) 88:554. doi: 10.1037/ccp0000498
10. May AM, Pachkowski MC, Klonsky ED. Motivations for suicide: converging evidence from clinical and community samples. J Psychiatr Res. (2020) 123:171–7. doi: 10.1016/j.jpsychires.2020.02.010
12. Bryan CJ, Rudd MD. Brief cognitive-behavioral therapy for suicide prevention. New York: Guilford Press (2018).
14. O’Connor RC, Kirtley OJ. The integrated motivational–volitional model of suicidal behaviour. Philos Trans R Soc B: Biol Sci. (2018) 373:20170268. doi: 10.1098/rstb.2017.0268
15. Klonsky ED, May AM. The three-step theory (3st): A new theory of suicide rooted in the “Ideation-to-action” Framework. Int J Cogn Ther. (2015) 8:114–29. doi: 10.1521/ijct.2015.8.2.114
16. Teismann T, Siebert AM, Forkmann T. Suicidal ambivalence: A scoping review. Suicide Life-Threatening Behav. (2024) 54:802–13. doi: 10.1111/sltb.13092
17. Henriques G, Wenzel A, Brown GK, Beck AT. Suicide attempters’ Reaction to survival as a risk factor for eventual suicide. Am J Psychiatry. (2005) 162:2180–2. doi: 10.1176/appi.ajp.162.11.2180
18. Kovacs M, Beck AT. The wish to die and the wish to live in attempted suicides. J Clin Psychol. (1977) 33:361–5. doi: 10.1002/1097-4679(197704)33:2<361::AID-JCLP2270330207>3.0.CO;2-H
19. Oakey-Frost N, Moscardini EH, Cowan T, Cohen A, Tucker RP. The temporal dynamics of wish to live, wish to die, and their short-term prospective relationships with suicidal desire. Behav Ther. (2023) 54:584–94. doi: 10.1016/j.beth.2022.12.011
20. Britton PC, Patrick H, Wenzel A, Williams GC. Integrating motivational interviewing and self-determination theory with cognitive behavioral therapy to prevent suicide. Cogn Behav Pract. (2011) 18:16–27. doi: 10.1016/j.cbpra.2009.06.004
21. Omer H, Elitzur A. What would you say to the person on the roof? A suicide prevention text. Suicide Life Threat Behav. (2001) 31:129–39. doi: 10.1521/suli.31.2.129.21509
22. Harris KM, McLean JP, Sheffield J, Jobes D. The internal suicide debate hypothesis: exploring the life versus death struggle. Suicide Life-Threatening Behav. (2010) 40:181–92. doi: 10.1521/suli.2010.40.2.181
23. Britton PC, Conner KR, Chapman BP, Maisto SA. Motivational interviewing to address suicidal ideation: A randomized controlled trial in veterans. Suicide Life-Threatening Behav. (2020) 50:233–48. doi: 10.1111/sltb.12581
24. Britton PC, Williams GC, Conner KR. Self-determination theory, motivational interviewing, and the treatment of clients with acute suicidal ideation. J Clin Psychol. (2008) 64:52–66. doi: 10.1002/jclp.20430
25. Britton PC, Bryan CJ, Valenstein M. Motivational interviewing for means restriction counseling with patients at risk for suicide. Cogn Behav Pract. (2016) 23:51–61. doi: 10.1016/j.cbpra.2014.09.004
26. Koban C, Teismann T. Psychotherapy with suicidal patients: understanding and improving the motivational starting point. Psychotherapie Aktuell. (2017) 9:24–31.
27. Liu RT, Miller I. Life events and suicidal ideation and behavior: A systematic review. Clin Psychol Rev. (2014) 34:181–92. doi: 10.1016/j.cpr.2014.01.006
28. Favril L, Yu R, Uyar A, Sharpe M, Fazel S. Risk factors for suicide in adults: systematic review and meta-analysis of psychological autopsy studies. BMJ Ment Health. (2022) 25:148–55. doi: 10.1136/ebmental-2022-300549
29. De Beurs D, Bockting C, Kerkhof A, Scheepers F, O’Connor R, Penninx B, et al. A network perspective on suicidal behavior: understanding suicidality as a complex system. Suicide Life-Threatening Behav. (2021) 51:115–26. doi: 10.1111/sltb.12676
30. Williams J, van der Does A, Barnhofer T, Crane C, Segal Z. Cognitive reactivity, suicidal ideation and future fluency: preliminary investigation of a differential activation theory of hopelessness/suicidality. Cogn Ther Res. (2008) 32:83–104. doi: 10.1007/s10608-006-9105-y
33. Van Wyk J, Gibson K. An analysis of young clients’ Communications about their suicidality on a text message helpline:”I’m scared of what I might do to myself. Front Psychiatry. (2022) 13:925830. doi: 10.3389/fpsyt.2022.925830
34. Madsen J, Harris KM. Negative self-appraisal: Personal reasons for dying as indicators of suicidality. PloS One. (2021) 16:e0246341. doi: 10.1371/journal.pone.0246341
35. Wenzel A, Beck AT. A cognitive model of suicidal behavior: theory and treatment. Appl Prev Psychol. (2008) 12:189–201. doi: 10.1016/j.appsy.2008.05.001
37. Jobes DA, Mann RE. Reasons for living versus reasons for dying: examining the internal debate of suicide. Suicide Life-Threatening Behav. (1999) 29:97–104. doi: 10.1111/j.1943-278X.1999.tb01048.x
38. Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. Reasons for staying alive when you are thinking of killing yourself: the reasons for living inventory. J consulting Clin Psychol. (1983) 51:276. doi: 10.1037/0022-006X.51.2.276
39. Brown GK, Steer RA, Henriques GR, Beck AT. The internal struggle between the wish to die and the wish to live: A risk factor for suicide. Am J Psychiatry. (2005) 162:1977–9. doi: 10.1176/appi.ajp.162.10.1977
40. Hallensleben N, Spangenberg L, Forkmann T, Rath D, Hegerl U, Kersting A, et al. Investigating the dynamics of suicidal ideation. Crisis. (2017). doi: 10.1027/0227-5910/a000464
41. Kleiman EM, Nock MK. Real-time assessment of suicidal thoughts and behaviors. Curr Opin Psychol. (2018) 22:33–7. doi: 10.1016/j.copsyc.2017.07.026
42. Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J Abnormal Psychol. (2017) 126:726–38. doi: 10.1037/abn0000273
43. Bergmans Y, Gordon E, Eynan R. Surviving moment to moment: the experience of living in a state of ambivalence for those with recurrent suicide attempts. Psychol Psychotherapy: Theory Res Pract. (2017) 90:633–48. doi: 10.1111/papt.12130
45. Selby EA, Anestis MD, Bender TW, Joiner TE Jr. An exploration of the emotional cascade model in borderline personality disorder. J Abnormal Psychol. (2009) 118:375. doi: 10.1037/a0015711
46. Bryan CJ, Allen MH, Wastler HM, Bryan AO, Baker JC, May AM, et al. Rapid intensification of suicide risk preceding suicidal behavior among primary care patients. Suicide Life-Threatening Behav. (2023) 53:352–61. doi: 10.1111/sltb.12948
47. Wastler HM, Bryan AO, Bryan CJ. Suicide attempts among adults denying active suicidal ideation: an examination of the relationship between suicidal thought content and suicidal behavior. J Clin Psychol. (2022) 78:1103–17. doi: 10.1002/jclp.23268
49. Teismann T, Friedrich S. Therapie-Tools: Suizidalität Und Krisenintervention. Weinheim: Beltz (2022).
51. Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press (1993).
52. Williams JMG, Fennell M, Crane R, Silverton S. Mindfulness-Based Cognitive Therapy with People at Risk of Suicide. New York: Guilford Press (2017).
53. Bryan CJ. Treating ptsd within the context of heightened suicide risk. Curr Psychiatry Rep. (2016) 18:1–7. doi: 10.1007/s11920-016-0708-z
54. Bryan CJ, Bryan AO, Khazem LR, Aase DM, Moreno JL, Ammendola E, et al. Crisis response planning rapidly reduces suicidal ideation among us military veterans receiving massed cognitive processing therapy for ptsd. J Anxiety Disord. (2024) 102:102824. doi: 10.1016/j.janxdis.2023.102824
55. Flett GL, Hewitt PL. The need to focus on perfectionism in suicide assessment, treatment and prevention. World Psychiatry. (2024) 23:152. doi: 10.1002/wps.21157
56. Ajdacic-Gross V, Hepp U, Seifritz E, Bopp M. Rethinking suicides as mental accidents: towards a new paradigm. J Affect Disord. (2019) 252:141–51. doi: 10.1016/j.jad.2019.04.022
57. Soper CA, Malo Ocejo P, Large M. On the Randomness of Suicide: An Evolutionary, Clinical Call to Transcend Suicide Risk Assessment. In: Abed R, St John-Smith P, editors. Evolutionary Psychiatry: Evolutionary Perspectives on Mental Health., vol. . p . Cambridge University Press, Cambridge (2022). p. 134–52.
58. Galasinski D, Ziółkowska J. The end of ambivalence. A narrative perspective on ambivalence in the suicidal process. Suicide Life- Threatening Behav. (2024) 54:888–99. doi: 10.1111/sltb.13101
59. Dempsey CL, Benedek DM, Zuromski KL, Riggs-Donovan C, Ng THH, Nock MK, et al. Association of firearm ownership, use, accessibility, and storage practices with suicide risk among us army soldiers. JAMA network Open. (2019) 2:e195383–e. doi: 10.1001/jamanetworkopen.2019.5383
60. Rogers ML, Gai AR, Joiner TE. Fluctuations in and associations between physical and psychological distance to suicide methods, fearlessness about death, and suicidal intent. J Psychopathol Clin Sci. (2022) 131:868. doi: 10.1037/abn0000783
62. Kuehn KS, King KM, Linehan MM, Harned MS. Modeling the suicidal behavior cycle: understanding repeated suicide attempts among individuals with borderline personality disorder and a history of attempting suicide. J consulting Clin Psychol. (2020) 88:570–81. doi: 10.1037/ccp0000496
63. Stanley B, Brown GK. Safety planning intervention: A brief intervention to mitigate suicide risk. Cogn Behav Pract. (2012) 19:256–64. doi: 10.1016/j.cbpra.2011.01.001
64. Wenzel A, Brown G, Beck AT. Cognitive Therapy for Suicidal Patient. Washington, D.C: APA (2009).
66. Orbach I. Dissociation, physical pain, and suicide: A hypothesis. Suicide Life-Threatening Behav. (1994) 24:68–79. doi: 10.1111/j.1943-278X.1994.tb00664.x
68. Owens C, Derges J, Abraham C. Intervening to prevent a suicide in a public place: A qualitative study of effective interventions by lay people. BMJ Open. (2019) 9:e032319. doi: 10.1136/bmjopen-2019-032319
69. Joiner TE, Hom MA, Rogers ML, Chu C, Stanley IH, Wynn GH, et al. Staring down death. Crisis. (2016) 73:212–7. doi: 10.1027/0227-5910/a000367
70. Simon TR, Swann AC, Powell KE, Potter LB, Kresnow M-J, O’Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life-Threatening Behav. (2001) 32:49–59. doi: 10.1521/suli.32.1.5.49.24212
71. Millner AJ, Lee MD, Nock MK. Describing and measuring the pathway to suicide attempts: A preliminary study. Suicide Life-Threatening Behav. (2017) 47:353–69. doi: 10.1111/sltb.12284
74. Bhaskaran J, Wang Y, Roos L, Sareen J, Skakum K, Bolton JM. Method of suicide attempt and reaction to survival as predictors of repeat suicide attempts: A longitudinal analysis. J Clin Psychiatry. (2014) 75:11887. doi: 10.4088/JCP.13m08879
75. Bahlmann L, Lübbert MB, Sobanski T, Kastner UW, Walter M, Smesny S, et al. Relapse Prevention Intervention after Suicidal Event (Rise): Feasibility Study of a Psychotherapeutic Short-Term Program for Inpatients after a Recent Suicide Attempt. Front Psychiatry. (2022) 13:937527. doi: 10.3389/fpsyt.2022.937527
77. Stanley IH, Hom MA, Boffa JW, Stage DRL, Joiner TE. Ptsd from a suicide attempt: an empirical investigation among suicide attempt survivors. J Clin Psychol. (2019) 75:1879–95. doi: 10.1002/jclp.22833
78. Hom MA, Stanley IH, Joiner TE Jr. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: A review of the literature. Clin Psychol Rev. (2015) 40:28–39. doi: 10.1016/j.cpr.2015.05.006
79. Kivelä L, van der Does WA, Riese H, Antypa N. Don’t miss the moment: A systematic review of ecological momentary assessment in suicide research. Front Digital Health. (2022) 4:876595. doi: 10.3389/fdgth.2022.876595
80. Trull TJ, Ebner-Priemer UW. Using experience sampling methods/ecological momentary assessment (ESM/EMA) in clinical assessment and clinical research: introduction to the special section. psychol Assess. (2009) 21:457–62. doi: 10.1037/a0017653
Keywords: suicidality, ambivalence, risk assessment, case conceptualization, psychotherapy
Citation: Teismann T, Britton PC and Forkmann T (2024) Ambivalence model of suicidality [ABS-model]: an orientation model for the treatment of suicidal individuals. Front. Psychiatry 15:1449565. doi: 10.3389/fpsyt.2024.1449565
Received: 15 June 2024; Accepted: 18 November 2024;
Published: 29 November 2024.
Edited by:
Karin Meissner, Hochschule Coburg, GermanyReviewed by:
Fengchun Wu, The Affiliated Brain Hospital of Guangzhou Medical University, ChinaIvo Dönnhoff, Heidelberg University Hospital, Germany
Copyright © 2024 Teismann, Britton and Forkmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas Forkmann, dGhvbWFzLmZvcmttYW5uQHVuaS1kdWUuZGU=
 Tobias Teismann
Tobias Teismann Peter C. Britton
Peter C. Britton Thomas Forkmann
Thomas Forkmann