- 1Case Room, Medical Department, Hunan Prevention and Treatment Institute for Occupational Diseases, Affiliated Prevention and Treatment Institute for Occupational Diseases of University of South China, Changsha, Hunan, China
- 2Department of Epidemiology and Health Statistics, Xiangya School of Public Health, Central South University, Changsha, Hunan, China
- 3Department of Nephrology, Xiangya Hospital, Central South University, Changsha, Hunan, China
- 4Department of Preventive Medicine, Changzhi Medical College, Changzhi, Shanxi, China
- 5Nursing Department, Hunan Prevention and Treatment Institute for Occupational Diseases, Affiliated Prevention and Treatment Institute for Occupational Diseases of University of South China, Changsha, Hunan, China
Background: Individuals with both type 2 diabetes mellitus (T2DM) and hypertension have an increased risk of cognitive impairment (CI) compared to those with either T2DM or hypertension. Therefore, this study aims to identify the prevalence of CI and its associated factors in T2DM patients with hypertension in Hunan, China.
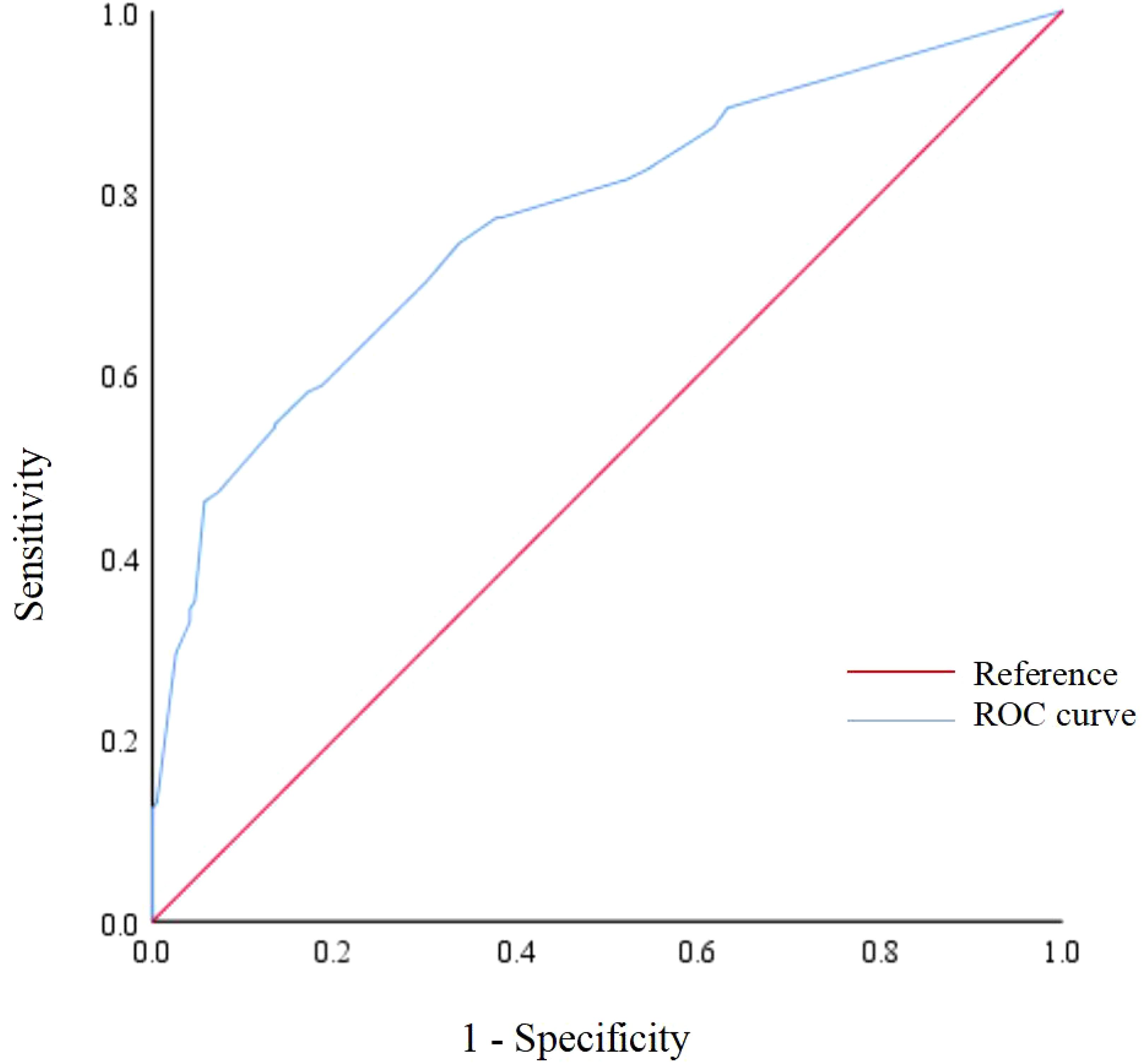
Methods: This cross-sectional study included T2DM patients with hypertension admitted to the Department of Endocrinology of Yuanjiang People’s Hospital in Hunan Province from July 2022 to February 2023. Data on sociodemographic, lifestyle, disease-related characteristics, and cognitive function were collected through face-to-face interviews. Cognitive function was assessed using the Mini-Mental State Examination. Backward stepwise multivariable logistic regression analysis was used to identify factors associated with CI. The predictive power was examined using the receiver operating characteristic (ROC) curve.
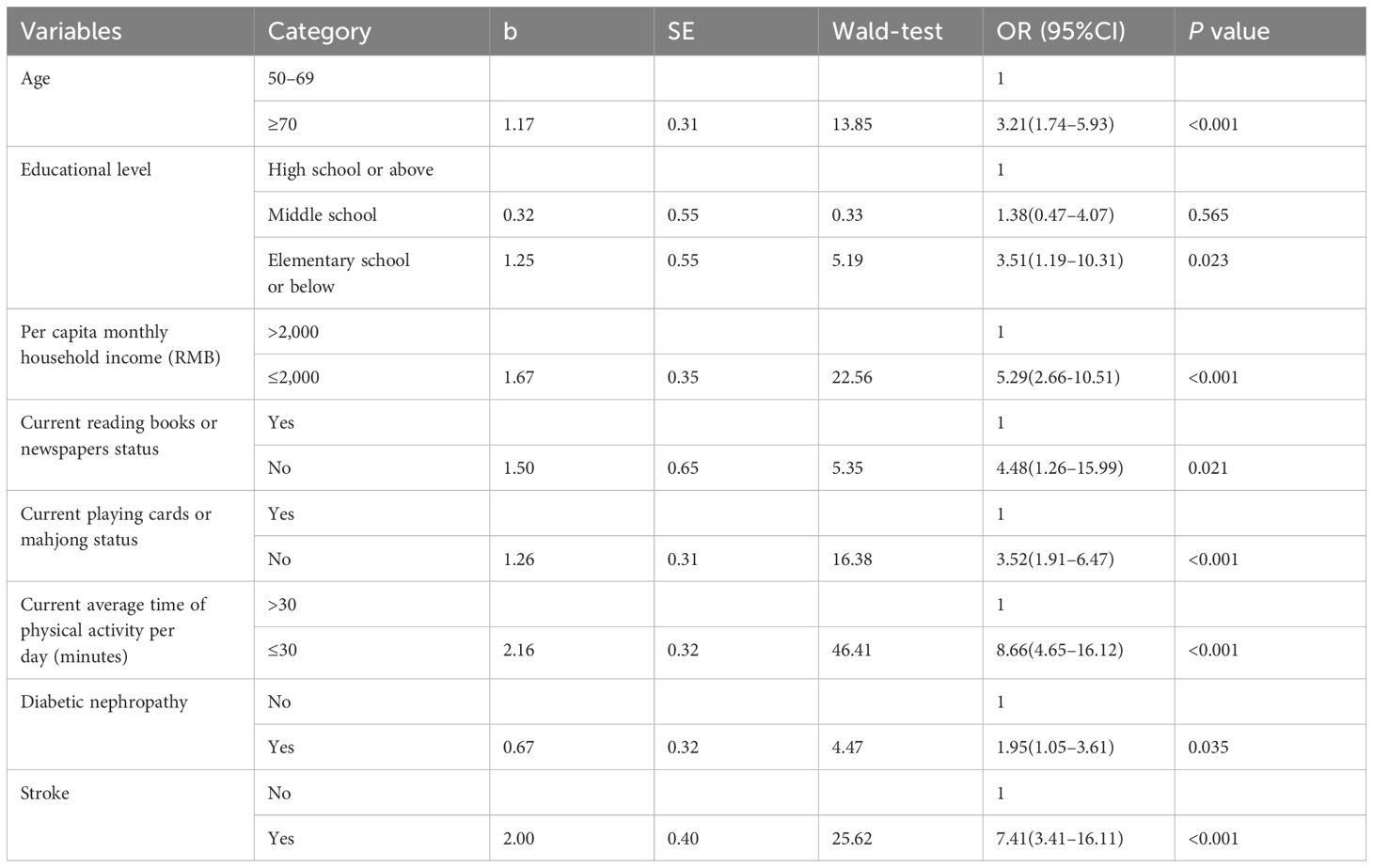
Results: A total of 475 participants were included. The prevalence of CI was 38.9% (95% confidence interval [95% CI]: 34.5%–43.3%). Multivariable logistic regression analysis showed that advanced age (odds ratio [OR]=3.21, 95% CI: 1.74–5.93), elementary school or below (OR=3.51, 95% CI: 1.19–10.31), per capita monthly household income ≤2000 RMB (OR=5.29, 95% CI: 2.66–10.51), not current reading books or newspapers (OR=4.48, 95% CI: 1.26–15.99), not current playing cards or mahjong (OR=3.52, 95% CI: 1.91–6.47), current average time of physical activity ≤30 minutes per day (OR=8.66, 95% CI: 4.65–16.12), diabetic nephropathy (OR=1.95, 95% CI: 1.05–3.61) and stroke (OR=7.41, 95% CI: 3.41–16.11) were associated with a higher risk of CI in T2DM patients with hypertension. The area under the ROC curve of this model was 0.925 (95% CI: 0.902–0.949).
Conclusions: The prevalence of CI was high in T2DM patients with hypertension in Hunan, China. Age, educational level, household income, current reading books or newspapers status, current playing cards or mahjong status, current average time of physical activity per day, diabetic nephropathy, and stroke were associated with CI in T2DM patients with hypertension.
1 Introduction
Type 2 diabetes mellitus (T2DM) and hypertension are commonly found to coexist due to similar risk factors such as endothelial dysfunction, vascular inflammation, and obesity (1). According to the latest Global Report on Hypertension released by the World Health Organization, the number of adults with hypertension doubled from 650 million in 1990 to 1.3 billion in 2019 (2). Furthermore, the total number of people with diabetes will rise to 643 million by 2030 and 783 million by 2045 (3). Previous meta-analyses showed that the pooled prevalence of hypertension among the diabetic population was approximately 50%, suggesting that there may be more than 322 million comorbidity cases worldwide in 2030 (4–6). Having one of these conditions increases the risk of developing the other by 1.5–2.0 times (7). Furthermore, such comorbidity confers a 2- to 4- fold increased risk of cardiovascular disease, end-stage kidney disease, and death (8–10).
Cognitive impairment (CI), characterized by the difficulty in processing thoughts, has become a major public health problem that reduces the quality of life of middle-aged and older adults (11–13). A growing body of evidence has suggested that the comorbidity of hypertension and diabetes can also accelerate cognitive decline (14, 15). A study in China reported that compared to those with hypertension only, individuals with both T2DM and hypertension had a higher risk of suffering from CI (odds ratio [OR]=1.44, 95% confidence interval [95% CI]: 1.14–1.80) (16), and Gorska-Ciebiada et al. (17) found that compared to those with T2DM only, individuals with both T2DM and hypertension had an increased risk of suffering from CI (OR=12.5, 95% CI: 2.92–54.0). The presence of CI in T2DM patients with hypertension may lead to poor self-management and medication adherence, ultimately contributing to increased mortality (18–20). Therefore, understanding the prevalence of CI in T2DM patients with hypertension and its associated factors is crucial, given that it cannot only facilitate the clinical management of such cases, but also help identify the high-risk group of CI among this population, as well as find intervention targets to reduce the incidence of CI.
Previous studies on this research topic have mainly focused on the general elderly populations, and those with either T2DM or hypertension (16, 21–24). These studies indicated that the prevalence of CI may differ by the sociodemographic, lifestyle and disease-related characteristics (16, 21–25). Specifically, sociodemographic characteristics included age, sex, and educational level (21, 24); lifestyle characteristics included smoking status, physical exercise, and reading status (16, 26); and disease-related characteristics included diabetes course, hypertension course, diabetic retinopathy, and cardiovascular disease (21, 24, 27). However, there is still a lack of research specifically addressing the prevalence of CI and its associated factors in T2DM patients with hypertension exclusively. Therefore, this study aimed to identify the prevalence of CI and its associated factors in T2DM patients with hypertension by comprehensively assessing the potential role of sociodemographic, lifestyle and disease-related characteristics.
2 Methods
2.1 Ethical approval
The study protocol was approved by the Ethics Committee of Xiangya School of Public Health, Central South University (No: XYGW–2021–27), and all participants provided informed consent.
2.2 Study design and populations
This cross-sectional study was performed at the Department of Endocrinology of the First People’s Hospital of Yuanjiang City, Hunan Province, China, from July 2022 to February 2023. The hospital is a secondary hospital located in Yiyang City, Hunan Province, China. A total of 475 consecutive T2DM patients with hypertension were included. The inclusion criteria were as follows: (1) diagnosed with T2DM according to the Guidelines for the Prevention and Treatment of Type 2 Diabetes Mellitus in China (2020 edition) (28); (2) diagnosed with hypertension according to the Guidelines for the Prevention and Control of High Blood Pressure in China (2018 Revision) (29); (3) aged ≧50 years; and (4) volunteered to participate in this study and signed an informed consent form. Patients with clinical dementia were excluded.
2.3 Data collection
Data on sociodemographic and lifestyle characteristics were collected via face-to-face survey by trained investigators who received uniformly standardized training prior to the interview. Diabetes- and hypertension- related information was extracted from medical records, and cognitive function were assessed by experienced physicians.
2.4 Outcome variable
The outcome of this study was CI, assessed using the Mini-Mental State Examination (MMSE) scale by experienced physicians. The MMSE was developed by Folstein et al. (30) and comprises 30 items and five cognitive domains including orientation, immediate memory, attention and calculation, recall ability, and language ability with a total score of 30 points. The cutoff values for detecting CI vary based on the educational level, and those with a score of ≤19, ≤22, and ≤26 for an educational level of illiterates, primary school, and junior high school or above were considered as CI cases (31).
2.5 Independent variables
The independent variables in this study included sociodemographic, lifestyle and disease-related characteristics.
2.5.1 Sociodemographic and lifestyle characteristics
Sociodemographic characteristics included sex, age, marital status, educational level, per capita monthly household income, location of residence, residency status, work status, and body mass index (BMI). Lifestyle characteristics included smoking history, drinking history, current tea drinking status, current reading books or newspapers status, current computer users, current playing cards or mahjong status, and current average time of physical activity per day. Specifically, those who smoked continuously or cumulatively for more than 6 months or at least one cigarette per day were defined as having a smoking history; those who drank alcohol at least once a month for more than one year were defined as having a drinking history; those who drank tea ≥1 times/week in the past month were defined as current tea drinking; those who read ≥1 time/week in the past month were defined as current reading books or newspapers; those who used computers ≥1 time/week in the past month were defined as current computer users; and those who played cards or mahjong at least once in the past month were defined as current playing mahjong or cards.
2.5.2 Disease-related characteristics
Diabetes-related characteristics included duration of diabetes, family history of diabetes, type of medication used for diabetes, and complications of diabetes (including diabetic nephropathy, diabetic retinopathy, diabetic foot, diabetic peripheral neuropathy, diabetic peripheral vascular disease, and diabetic ketoacidosis). Hypertension-related characteristics included duration of hypertension, family history of hypertension, and type of medication used for hypertension. Information on diabetes or hypertension comorbidities such as hyperlipidaemia, coronary heart disease, chronic kidney disease, fatty liver, and stroke was also extracted.
2.6 Statistical analysis
The data were analyzed with SPSS version 25.0 software. Mean ± standard deviation (SD) was used to describe normally distributed continuous variables, while median (inter-quartile range, IQR) was used to describe non-normally distributed continuous variables. Frequency (n) and proportion (%) were used to describe categorical variables. The χ2 test or Fisher’s precision probability test was used to determine the univariable correlations between the independent variables and CI. Multicollinearity between the independent variables were assessed, and a variance inflation factor (VIF) value of less than 5 was considered as no multicollinearity problem. Backward stepwise multivariable logistic regression analysis was used to identify factors associated with CI by including the independent variables differed significantly in the univariable analyses. The goodness of fit of the model was evaluated using the Hosmer-Lemeshow goodness-of-fit test, with a P value of >0.05 indicated a good fit. In addition, the predictive value of the multivariable regression model was tested by the receiver operating characteristic (ROC) curve. All statistical tests were two-sided, and a P value of <0.05 was considered statistically significant.
3 Results
3.1 Participant characteristics
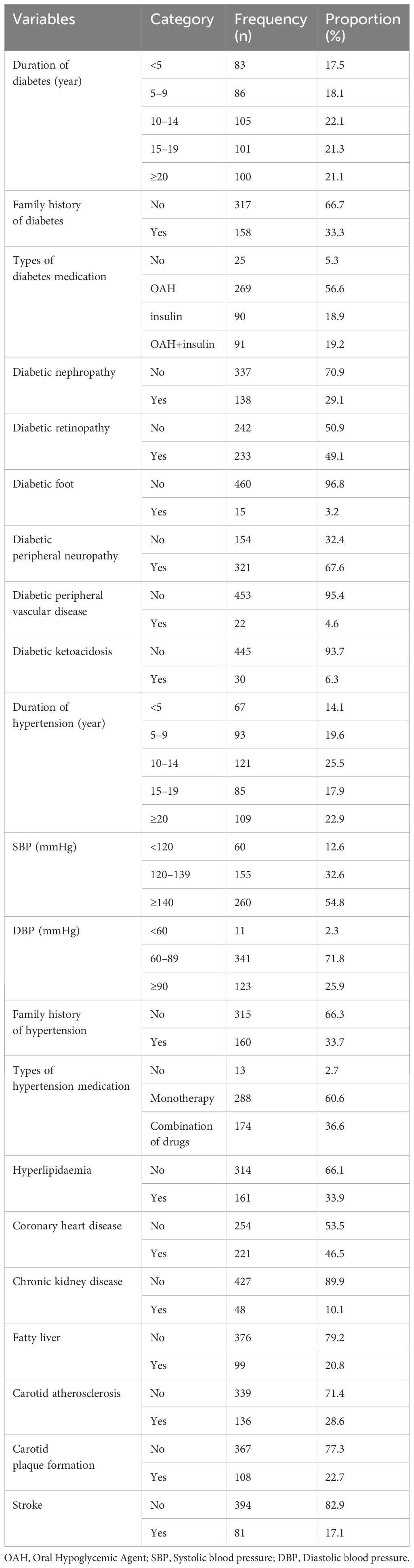
A total of 475 patients with complete data were included in this study, of which 198 (41.7%) were males and 277 (58.3%) were females. The age range of the study population was 50 to 95 years with a mean age of 69.80 ± 9.10 years. The mean duration of diabetes and hypertension was 13.36 ± 8.42 years, and 13.64 ± 8.63 years, respectively. The mean levels of fasting blood glucose (FBG), two-hour postprandial blood glucose (2hPG), and HemoglobinA1c (HbA1c, %) were 7.93 ± 2.42 mmol/L, 13.58 ± 3.30 mmol/L, and 8.12 ± 3.20, respectively. In addition, 82 (17.3%) attended high school and above; 199 (41.9%) had a BMI value of ≥24 kg/m2; 171 (36.0%) had a smoking history; 149 (31.4%) had a drinking history; 138 (29.1%) and 233 (49.1%) exhibited diabetic nephropathy and diabetic retinopathy, respectively; and 81 (17.1%) had a history of stroke. The characteristics of the study population are shown in Tables 1, 2.
3.2 Prevalence of CI in T2DM patients with hypertension
The mean score of MMSE was 25.89 ± 3.73, with scores ranging from 17 to 30. Based on the established cutoff values, 187 were considered as CI cases and 288 were considered as non-CI cases with normal cognitive function. The prevalence of CI in T2DM patients with hypertension was 38.9% (95% CI: 34.5%–43.3%).
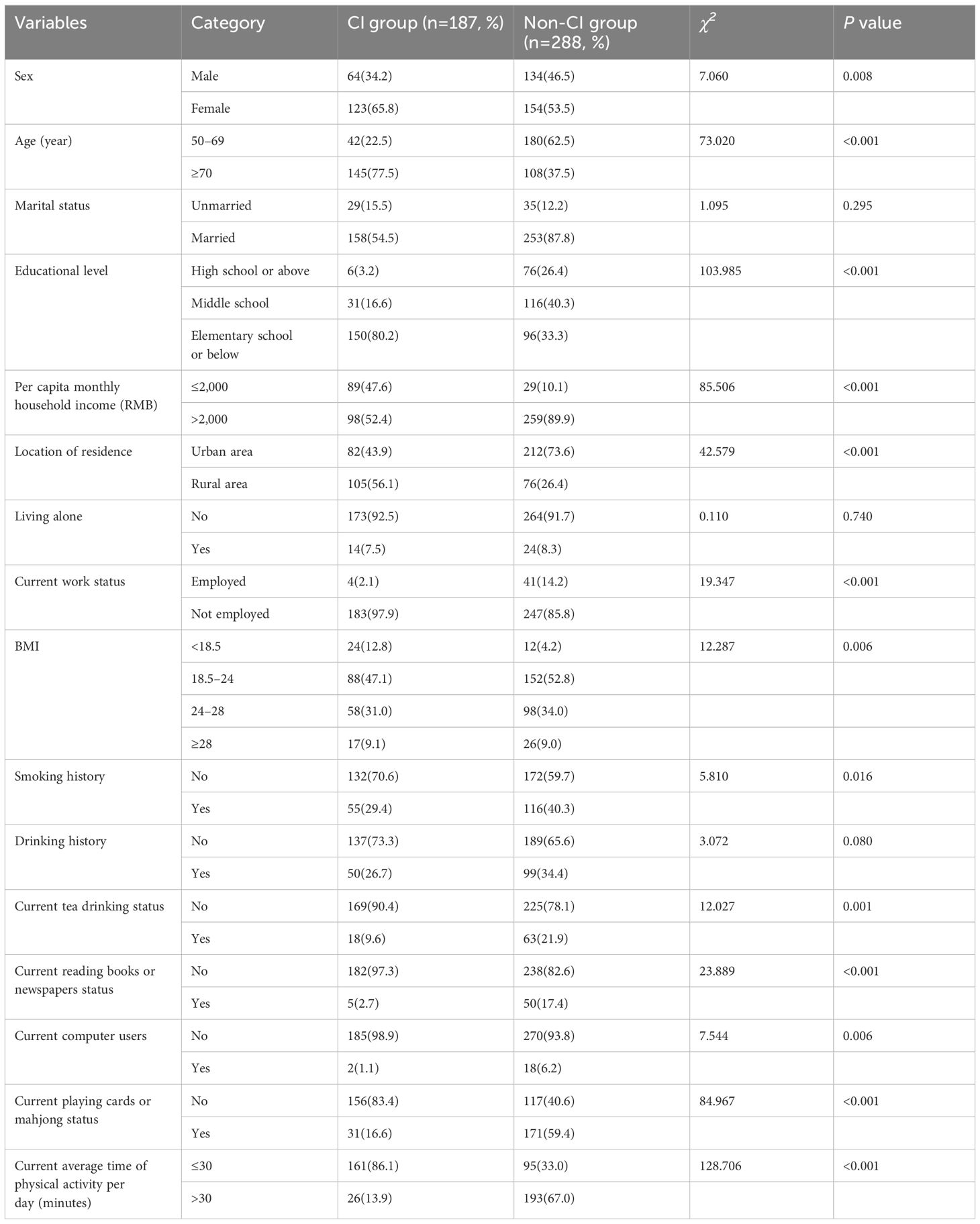
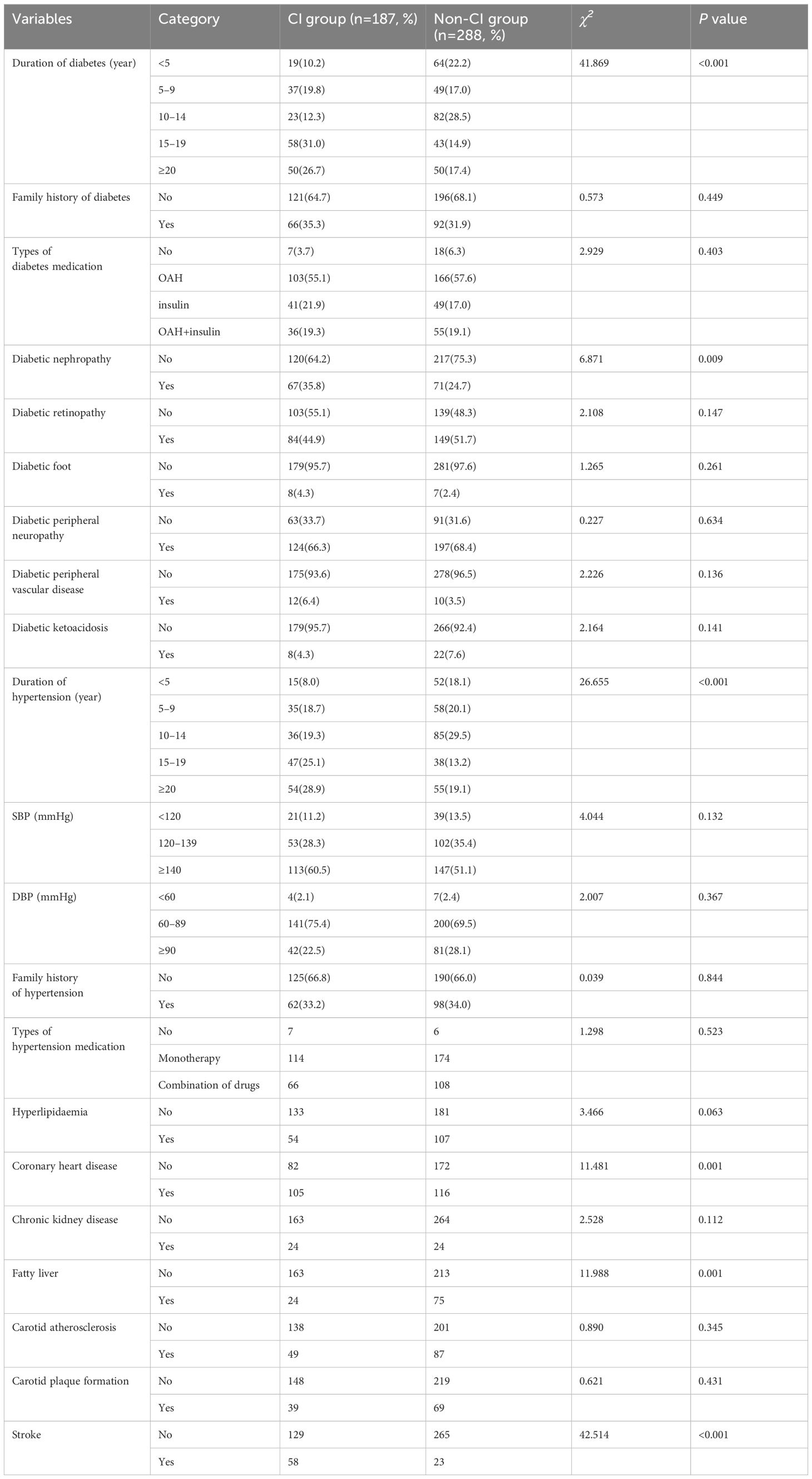
3.3 Univariable analyses of factors associated with CI
The results of univariable analyses are shown in Tables 3, 4. Sex, age, educational level, per capita monthly household income, location of residence, current work status, BMI, smoking history, current tea drinking status, current reading books or newspapers status, current computer users, current playing cards or mahjong status, and current average time of physical activity per day, duration of diabetes, diabetic nephropathy, duration of hypertension, coronary heart disease, fatty liver, and stroke differed significantly between the CI group and the non-CI group (P<0.05).
3.4 Multivariable analyses of factors associated with CI
The results of multivariable logistic regression analysis are presented in Table 5. Age, educational level, per capita monthly household income, current reading books or newspapers status, current playing cards or mahjong status, current average time of physical activity per day, diabetic nephropathy, and stroke were independently associated with CI in T2DM patients with hypertension. Aged ≥70 (OR=3.21, 95% CI: 1.74–5.93), elementary school or below (OR=3.51, 95% CI: 1.19–10.31), per capita monthly household income of ≤2000 RMB (OR=5.29, 95% CI: 2.66–10.51), not current reading books or newspapers (OR=4.48, 95% CI: 1.26–15.99), not current playing cards or mahjong (OR=3.52, 95% CI: 1.91–6.47), current average time of physical activity ≤30 minutes per day (OR=8.66, 95% CI: 4.65–16.12), diabetic nephropathy (OR=1.95, 95% CI: 1.05–3.61), and stroke (OR=7.41, 95% CI: 3.41–16.11) were associated with a higher risk of CI. The Hosmer-Lemeshow test indicated a good model fit (P=0.739). Figure 1 shows the ROC curve of the multivariable model. The area under the ROC curve was 0.925 (95% CI: 0.902–0.949) with a P value of <0.001, indicating a good model fit.
4 Discussion
This study investigated the prevalence of CI and its associated factors in T2DM patients with hypertension in Hunan Province, China. To our knowledge, this is the first study to identify the prevalence of CI and its associated factors in T2DM patients with hypertension exclusively. This study found that the prevalence of CI was 39.37% (95 CI%: 34.98%–34.98%), which was much higher than the estimates reported by previous studies focused on either T2DM patients or hypertension patients (32–34). This difference may be explained by the fact that the comorbidity of diabetes and hypertension can cause damage to the central nervous system, which can subsequently accelerate cognitive decline (35). Given the high prevalence of CI in T2DM patients with hypertension found in this study and the fact that CI is associated with poor medical compliance (36, 37), early identification of those at high-risk group of CI is needed.
Advanced age is a common risk factor for CI in the general population (38, 39). Consistently, this study found that advanced age increased the risk of CI in T2DM patients with hypertension, which may be attributed to aging-related decline in synaptic density and function in the brain (40–42). The current study also found that lower educational levels were associated with a higher risk of CI, which is consistent with the findings of several previous studies conducted in T2DM populations (43, 44). Education enhances brain reserve capacity to prevent brain damage by promoting synaptic density and maintaining adequate and stable cerebral blood flow (45). Furthermore, the study showed that low income was associated with a higher risk of CI (OR=5.29, 95% CI: 2.66–10.51), which is consistent with several studies conducted among older populations (46, 47). For example, a study conducted among older adults in Saudi Arabia found that low income was associated with cognitive decline (adjusted OR [aOR]=1.825, 95% CI: 1.17–2.86) (47). This may be explained by the fact that individuals with higher income may have greater social support, more medical resources, and higher health literacy (48). Therefore, those with advanced age, low educational level, and low income should be given special concern for the management of T2DM patients with hypertension in the clinical practice.
This study showed that current reading books or newspapers and current playing cards or mahjong were associated with a lower risk of CI in T2DM patients with hypertension, which is consistent with the finding of previous studies conducted among older populations (49, 50). For example, a cohort study of 10,318 older Australians found that reading books, newspapers, or magazines and playing games, cards, or chess were associated with a reduced risk of dementia over 10 years (49), and a study among Chinese older adults found that compared to those who “never” engaged in reading books or newspapers and playing cards or mahjong, those who engaged in such activities “almost every day” were at a decreased risk of CI, the fully-adjusted hazard ratios were 0.64 (95% CI: 0.53–0.78) and 0.70 (95% CI: 0.56–0.86), respectively (50). Intellectual activities such as reading books and playing games may lower the risk of dementia by improving cognitive reserve and increasing stress tolerance (49, 51). In addition, this study showed that the current average time of physical activity per day less than 30 minutes was associated with an increased risk of CI in T2DM patients with hypertension. The cognitive benefits of physical exercise are associated with increased plasticity and reduced inflammation within the hippocampus (52). A randomized controlled trial in the community showed that physical activity, particularly moderate-intensity aerobic exercise, enhanced cognitive function and health-related quality of life in older adults with CI (53). Therefore, the cognitive function of T2DM patients with hypertension could be maintained or improved by reading books or newspapers, playing cards or mahjong, and taking regular exercise.
This study showed that diabetic nephropathy, a microvascular complication of diabetes (54), was associated with a higher risk of CI. One possible mechanism is that brain and kidney damage are characterized by similar microvascular lesions, and that when renal function is impaired, it affects the cerebral microcirculation and the blood-brain barrier, which increases the risk of CI (55). This finding was also consistent with a previous study in T2DM patients (55). Our study adds significantly to the existing body of knowledge by showing that diabetic nephropathy could lead to decreased cognitive function in those with both T2DM and hypertension. Moreover, stroke is a major health problem worldwide and a leading cause of long-term disability and death (56). This study found that a history of stroke was associated with a higher risk of CI in T2DM patients with hypertension, which may be explained by the mechanisms related to inadequate cerebral perfusion, white matter damage, and neuroinflammation (57). Therefore, comprehensive management and treatment of T2DM complications and comorbidities are of great importance for maintaining the cognitive function of those with both T2DM and hypertension.
This study has several limitations. First, the cross-sectional study design did not allow for any causal relationships between the variables of interest. Secondly, this was a hospital-based study with a single center, which may limit the generalizability of the findings. Thirdly, recall bias remained an issue when collecting data. In addition, this study used only the MMSE to assess CI, which could result in misclassification compared to the gold standard. Therefore, future longitudinal studies with gold standard are needed.
5 Conclusions
The prevalence of CI in T2DM patients with hypertension was high in Hunan, China. Age, educational level, household income, current reading books or newspapers status, current playing cards or mahjong status, current average time of physical activity per day, diabetic nephropathy, and stroke were associated with CI in T2DM patients with hypertension. Therefore, regular reading, intellectual activity and physical activity should be considered as intervention targets for the prevention and management of CI, and those with advanced age, low educational level, and low household income should be given special concern. In addition, it is suggested to maintain or improve the cognitive function of those with both T2DM and hypertension via strengthening the management of diabetic complications and comorbidities including diabetic nephropathy and stroke.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Xiangya School of Public Health, Central South University (No: XYGW–2021–27). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HL: Investigation, Methodology, Writing – original draft, Writing – review & editing. ZF: Data curation, Software, Writing – original draft, Writing – review & editing. WZ: Data curation, Investigation, Writing – review & editing. YL: Data curation, Investigation, Writing – review & editing. NX: Data curation, Investigation, Writing – review & editing. WC: Conceptualization, Methodology, Writing – review & editing. JY: Conceptualization, Methodology, Writing – review & editing. XYW: Conceptualization, Funding acquisition, Methodology, Writing – review & editing. ZS: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing. WD: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Major Scientific Research Project of Hunan Health high-level Talents in 2023 (grant number R2023072), the National Natural Science Foundation of China under (grant number 82103939), the National Natural Science Foundation of Hunan Province under (grant number 2023JJ30734), the Start-up Research Fund of Central South University under (grant number 202044003), and the National Key R&D Program of China under (grant number 2020YFC2008600).
Acknowledgments
The authors would like to thank all the participants for their participation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. (2018) 34:575–84. doi: 10.1016/j.cjca.2017.12.005
2. World Health Organization. Global report on hypertension: the race against a silent killer. Geneva: World Health Organization (2023).
3. Federation ID. IDF diabetes atlas, 10th edn. Brussels, Belgium: International Diabetes Federation (2021).
4. Zhang X, Yang XL, Liu S, Ye YS, Yang QT, Xia LN. Prevalence of hypertension among type 2 diabetes mellitus patients in China: a systematic review and meta-analysis. Int Health. (2024) 16:144–51. doi: 10.1093/inthealth/ihad047
5. Haile TG, Mariye T, Tadesse DB, Gebremeskel GG, Asefa GG, Getachew T. Prevalence of hypertension among type 2 diabetes mellitus patients in Ethiopia: a systematic review and meta-analysis. Int Health. (2023) 15:235–41. doi: 10.1093/inthealth/ihac060
6. Hinneh T, Akyirem S, Bossman IF, Lambongang V, Ofori-Aning P, Ogungbe O, et al. Regional prevalence of hypertension among people diagnosed with diabetes in Africa, a systematic review and meta-analysis. PloS Glob Public Health. (2023) 3:e0001931. doi: 10.1371/journal.pgph.0001931
7. Tatsumi Y, Ohkubo T. Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese. Hypertens Res. (2017) 40:795–806. doi: 10.1038/hr.2017.67
8. Strain WD, Paldánius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol. (2018) 17:57. doi: 10.1186/s12933-018-0703-2
9. Cai S, Cheng B, Li K, Li Y, Zhang A, Sun J, et al. Association of cognitive impairment and diabetes on survival in Chinese older people with hypertension: a 10-year prospective study. BMC Geriatr. (2023) 23:582. doi: 10.1186/s12877-023-04214-4
10. Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. (9841) 2012:601–10:380. doi: 10.1016/S0140-6736(12)60987-8
11. Murman DL. The impact of age on cognition. Semin Hear. (2015) 36:111–21. doi: 10.1055/s-0035-1555115
12. Glisky EL. Frontiers in neuroscience changes in cognitive function in human aging. In: Riddle DR, editor. Brain aging: models, methods, and mechanisms. CRC Press/Taylor & Francis Copyright © 2007, Taylor & Francis Group, LLC, Boca Raton (FL (2007).
13. Shang H, Xu C, Lu H, Zhang J. The early stage of abnormal aging: cognitive impairment. Adv Exp Med Biol. (2023) 1419:149–55. doi: 10.1007/978-981-99-1627-6_11
14. Newby D, Garfield V. Understanding the inter-relationships of type 2 diabetes and hypertension with brain and cognitive health: A UK Biobank study. Diabetes Obes Metab. (2022) 24:938–47. doi: 10.1111/dom.14658
15. Borshchev YY, Uspensky YP, Galagudza MM. Pathogenetic pathways of cognitive dysfunction and dementia in metabolic syndrome. Life Sci. (2019) 237:116932. doi: 10.1016/j.lfs.2019.116932
16. Xie C, Zhong D, Zhang Y, Liu X, Zhang L, Luo X, et al. Prevalence and risk factors of cognitive impairment in Chinese patients with hypertension: a systematic review and meta-analysis. Front Neurol. (2023) 14:1271437. doi: 10.3389/fneur.2023.1271437
17. Gorska-Ciebiada M, Ciebiada M. Association of hsCRP and vitamin D levels with mild cognitive impairment in elderly type 2 diabetic patients. Exp Gerontol. (2020) 135:110926. doi: 10.1016/j.exger.2020.110926
18. Moon Y, Lim JS, Lee CN, Choi H. Vulnerable strata to non-adherence and overuse in treatment for patients with cognitive impairment. Dement Neurocogn Disord. (2020) 19:152–60. doi: 10.12779/dnd.2020.19.4.152
19. Smith D, Lovell J, Weller C, Kennedy B, Winbolt M, Young C, et al. A systematic review of medication non-adherence in persons with dementia or cognitive impairment. PloS One. (2017) 12:e0170651. doi: 10.1371/journal.pone.0170651
20. Lv X, Li W, Ma Y, Chen H, Zeng Y, Yu X, et al. Cognitive decline and mortality among community-dwelling Chinese older people. BMC Med. (2019) 17:63. doi: 10.1186/s12916-019-1295-8
21. Wang ZQ, Fei L, Xu YM, Deng F, Zhong BL. Prevalence and correlates of suspected dementia in older adults receiving primary healthcare in Wuhan, China: A multicenter cross-sectional survey. Front Public Health. (2022) 10:1032118. doi: 10.3389/fpubh.2022.1032118
22. Zhong BL, Chen SL, Tu X, Conwell Y. Loneliness and cognitive function in older adults: findings from the chinese longitudinal healthy longevity survey. J Gerontol B Psychol Sci Soc Sci. (2017) 72:120–8. doi: 10.1093/geronb/gbw037
23. Zhong BL, Chen SL, Conwell Y. Effects of transient versus chronic loneliness on cognitive function in older adults: findings from the chinese longitudinal healthy longevity survey. Am J Geriatr Psychiatry. (2016) 24:389–98. doi: 10.1016/j.jagp.2015.12.009
24. Li YS, Li JB, Wang JJ, Wang XH, Jiang WR, Qiu HN, et al. Risk factors for cognitive impairment in middle-aged type 2 diabetic patients: a cross-sectional study. BMJ Open. (2024) 14:e074753. doi: 10.1136/bmjopen-2023-074753
25. Zhang HG, Fan F, Zhong BL, Chiu HF. Relationship between left-behind status and cognitive function in older Chinese adults: a prospective 3-year cohort study. Gen Psychiatr. (2023) 36:e101054. doi: 10.1136/gpsych-2023-101054
26. Jingyu L, Wen D, Liping Z, Xiaoling L. A nomogram for predicting mild cognitive impairment in older adults with hypertension. BMC Neurol. (2023) 23:363. doi: 10.1186/s12883-023-03408-y
27. Maimaitituerxun R, Chen W, Xiang J, Xie Y, Kaminga AC, Wu XY, et al. The use of nomogram for detecting mild cognitive impairment in patients with type 2 diabetes mellitus. J Diabetes. (2023) 15:448–58. doi: 10.1111/1753-0407.13384
28. Society CD. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes. (2021) 13:315–409. doi: 10.3760/cma.j.cn115791-20210221-00095
29. Hypertension, W.G.o.C.G.f.t.M.o. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. (2019) 24:24–56. doi: 10.3969/j.issn.1007-5410.2019.01.002
30. Folstein MF, Folstein SE, McHugh PR. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
31. Li H, Jia J, Yang Z. Mini-mental state examination in elderly chinese: A population-based normative study. J Alzheimers Dis. (2016) 53:487–96. doi: 10.3233/JAD-160119
32. Bozanic A, Toro P, Bello-Lepe S, Hurtado-Oliva J, Beyle C, Valdés C, et al. Cognitive impairment with Type 2 Diabetes Mellitus among community-dwelling older adults in Chile: Prevalence, risk factors and cognitive characteristics. Front Hum Neurosci. (2022) 16:1070611. doi: 10.3389/fnhum.2022.1070611
33. Liu S, Lu Y, Cai X, Cong R, Li J, Jiang H, et al. Glycemic control is related to cognitive dysfunction in elderly people with type 2 diabetes mellitus in a rural chinese population. Curr Alzheimer Res. (2019) 16:950–62. doi: 10.2174/1567205016666191023110712
34. Lazo-Porras M, Ortiz-Soriano V, Moscoso-Porras M, Runzer-Colmenares FM, Málaga G, Jaime Miranda J. Cognitive impairment and hypertension in older adults living in extreme poverty: a cross-sectional study in Peru. BMC Geriatr. (2017) 17:250. doi: 10.1186/s12877-017-0628-8
35. Zachara R, Właszczuk A, Gorzkowska A, Jędrzejowska-Szypułka H. The influence of hypertension, diabetes, lipid disorders and the presence of the APOE4 allele on the cognitive functions of patients over 65 years of age. Pol Merkur Lekarski. (2022) 50:391–4.
36. Ma LY, He F, Liu S, Wang XD, Gao Y, Shi Z, et al. The association between the prevalence, medication adherence and control of hypertension and the prevalence of mild cognitive impairment in rural northern China: A cross-sectional study. Patient Prefer Adherence. (2022) 16:493–502. doi: 10.2147/PPA.S351588
37. He X, Wang X, Wang B, Zhu A. The association between mild cognitive impairment and medication non-adherence among elderly patients with chronic diseases. Cureus. (2023) 15:e47756. doi: 10.7759/cureus.47756
38. Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. (2020) 5:e661–71. doi: 10.1016/S2468-2667(20)30185-7
39. Deng Y, Zhao S, Cheng G, Yang J, Li B, Xu K, et al. The prevalence of mild cognitive impairment among chinese people: A meta-analysis. Neuroepidemiology. (2021) 55:79–91. doi: 10.1159/000512597
40. Bettio LEB, Rajendran L, Gil-Mohapel J. The effects of aging in the hippocampus and cognitive decline. Neurosci Biobehav Rev. (2017) 79:66–86. doi: 10.1016/j.neubiorev.2017.04.030
41. Cho K. Neutrophil-mediated progression of mild cognitive impairment to dementia. Int J Mol Sci. (2023) 24(19):14795. doi: 10.3390/ijms241914795
42. Satoh A, Imai SI, Guarente L. The brain, sirtuins, and ageing. Nat Rev Neurosci. (2017) 18:362–74. doi: 10.1038/nrn.2017.42
43. Panyawattanakit C, Wongpradit W, Kanhasing R, Kulalert P. Cognitive impairment and associated factors among older adults with diabetes in a suburban primary health center in Thailand. Dement Geriatr Cognit Disord. (2022) 51:175–81. doi: 10.1159/000524132
44. Ma ZY, Wu YY, Cui HY, Yao GY, Bian H. Factors influencing post-stroke cognitive impairment in patients with type 2 diabetes mellitus. Clin Interv Aging. (2022) 17:653–64. doi: 10.2147/CIA.S355242
45. Zhang W, Tang F, Chen Y, Silverstein M, Liu S, Dong X. Education, activity engagement, and cognitive function in US chinese older adults. J Am Geriatr Soc. (2019) 67:S525–s531. doi: 10.1111/jgs.v67.S3
46. Petersen JD, Wehberg S, Packness A, Svensson NH, Hyldig N, Raunsgaard S, et al. Association of socioeconomic status with dementia diagnosis among older adults in Denmark. JAMA Netw Open. (2021) 4:e2110432. doi: 10.1001/jamanetworkopen.2021.10432
47. Alshammari SA, Alhamdan AA, Bindawas SM, Al-Amoud MM, Al-Orf SM, Al-Muammar MN, et al. Assessing the cognitive status of older adults attending primary healthcare centers in Saudi Arabia using the Mini-Mental State Examination. Saudi Med J. (2020) 41:1315–23. doi: 10.15537/smj.2020.12.25576
48. Lu Y, Liu C, Fawkes S, Ma J, Liu Y, Yu D. Inequality in social support associated with mild cognitive impairment: A cross-sectional study of older (≥60 years) residents in shanghai, China. Front Public Health. (2021) 9:706322. doi: 10.3389/fpubh.2021.706322
49. Wu Z, Pandigama DH, Wrigglesworth J, Owen A, Woods RL, Chong TT, et al. Lifestyle enrichment in later life and its association with dementia risk. JAMA Netw Open. (2023) 6:e2323690. doi: 10.1001/jamanetworkopen.2023.23690
50. Mao C, Li ZH, Lv YB, Gao X, Kraus VB, Zhou JH, et al. Specific leisure activities and cognitive functions among the oldest-old: the chinese longitudinal healthy longevity survey. J Gerontol A Biol Sci Med Sci. (2020) 75:739–46. doi: 10.1093/gerona/glz086
51. Wang J, Liu N, Zhao X. Association of playing cards or mahjong with cognitive function in chinese older adults. Int J Environ Res Public Health. (2022) 19(15):9249. doi: 10.3390/ijerph19159249
52. De Miguel Z, Khoury N, Betley MJ, Lehallier B, Willoughby D, Olsson N, et al. Exercise plasma boosts memory and dampens brain inflammation via clusterin. Nature. (2021) 600:494–9. doi: 10.1038/s41586-021-04183-x
53. Song D, Yu DSF. Effects of a moderate-intensity aerobic exercise programme on the cognitive function and quality of life of community-dwelling elderly people with mild cognitive impairment: A randomised controlled trial. Int J Nurs Stud. (2019) 93:97–105. doi: 10.1016/j.ijnurstu.2019.02.019
54. Yang J, Liu Z. Mechanistic pathogenesis of endothelial dysfunction in diabetic nephropathy and retinopathy. Front Endocrinol (Lausanne). (2022) 13:816400. doi: 10.3389/fendo.2022.816400
55. Li J, Pan J, Li B, Tian H, Zhu Y, Liao Z, et al. Positive correlation between cognitive impairment and renal microangiopathy in patients with type 2 diabetic nephropathy: a multicenter retrospective study. J Int Med Res. (2018) 46:5040–51. doi: 10.1177/0300060518789299
56. Feigin VL, Krishnamurthi RV, Parmar P, Norrving B, Mensah GA, Bennett DA, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990-2013: the GBD 2013 study. Neuroepidemiology. (2015) 45:161–76. doi: 10.1159/000441085
Keywords: type 2 diabetes mellitus, hypertension, cognitive impairment, prevalence, associated factors
Citation: Liu H, Feng Z, Zhang W, Liu Y, Xiong N, Chen W, Yang J, Wu XY, Shi Z and Dai W (2024) Prevalence of cognitive impairment and its associated factors in type 2 diabetes mellitus patients with hypertension in Hunan, China: a cross-sectional study. Front. Psychiatry 15:1445323. doi: 10.3389/fpsyt.2024.1445323
Received: 07 June 2024; Accepted: 02 December 2024;
Published: 19 December 2024.
Edited by:
Yan Xi, Shanghai University of Traditional Chinese Medicine, ChinaReviewed by:
Dinesh Upadhya, Manipal Academy of Higher Education, IndiaXiu-Jun Liu, Wuhan Mental Health Center, China
Copyright © 2024 Liu, Feng, Zhang, Liu, Xiong, Chen, Yang, Wu, Shi and Dai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zeya Shi, c3RvbmUyMDAxMDMyNkBzaW5hLmNvbQ==; Wenjie Dai, bTE4NjczOTY1NzkxQDE2My5jb20=
 Hongying Liu
Hongying Liu Ziling Feng2
Ziling Feng2 Jianzhou Yang
Jianzhou Yang Xin Yin Wu
Xin Yin Wu Wenjie Dai
Wenjie Dai