- 1Epidemiology, Faculty of Medicine, University of Augsburg, Augsburg, Germany
- 2Department of Cardiology, Respiratory Medicine and Intensive Care, University Hospital Augsburg, Augsburg, Germany
- 3Institute for Medical Information Processing, Biometry and Epidemiology - IBE, Ludwig-Maximilians Universität (LMU) Munich, Munich, Germany
Introduction: This study aimed to explore mental health literacy (MHL) and its related factors in a cross-sectional, registry-based sample of patients after acute myocardial infarction (AMI).
Methods: All survivors of AMI between 2017 and 2019 from the Myocardial Infarction Registry Augsburg (n=1.712) received a postal questionnaire on MHL (Mental Health Literacy Scale (MHLS-GER)) and single questions on experiences with and information on mental disorders in 2023. The response rate was 49.9%. Logistic and linear regression models were used to investigate the associations between these variables and sociodemographic factors.
Results: In the sample of 855 patients (77.5% male, mean age 71.4 ± 10.9 years), 30.0% had experienced mental problems about 5 years after AMI. Among these, 17.4% received psychotherapy and 26.1% psychotropic drugs. Information about possible mental problems after their AMI was obtained from a physician by 30.8% of the patients and in a rehabilitation setting by 46.4%, respectively. Of the patients, 26.2% wished to receive more information on mental problems after AMI. MHLS-GER subscale scores ranged between and 54 (“Social distance”) and 76 (“Information seeking”) (best score 100). Age was the most important factor that was significantly associated with the report of mental health problems, a perceived lack of information, help seeking behavior and treatment, and MHL.
Discussion: Elderly and poorly educated patients were at risk of poor MHL. Further studies are required to specify the role of MHL in post-AMI life and health care.
1 Introduction
The concept of mental health literacy (MHL) was first introduced in 1997 by Jorm et al. who described it as “knowledge and beliefs about mental disorders which aid their recognition, management or prevention” (1). More current definitions include a number of additional components such as understanding how to obtain and maintain good mental health and prevent mental disorders, recognition of when a disorder is developing, knowledge of help-seeking options and treatments available, knowledge of effective self-help strategies for milder problems and first aid skills to support others who are developing a mental disorder or are in a mental health crisis (2).
Acute myocardial infarction (AMI) is one of the leading causes of mortality worldwide (3) with a declining short-term mortality in industrialized countries due to advances in treatment and prevention procedures (4). Hence, in ageing societies the lifespan after an AMI is extending and a closer examination of factors affecting post-AMI quality of life and clinical outcomes of AMI survivors is needed. Mental disorders are major influencing factors and there is convincing scientific evidence of a strong association between AMI and depression and anxiety disorders (5–9). Recent meta-analyses consistently reported a pooled prevalence of depression of about 28% among persons with AMI (8, 9). The pooled prevalence of moderate to severe anxiety symptoms was 38.08% in another recent meta-analysis (10). Compared with the rates of depression and anxiety symptoms in the general population, the rates in people post-AMI are considerably higher (11–13). For instance, in the German population aged 60 to 69 years, the prevalence of depressive symptoms (PHQ-9 > 9) was 7.2% (11). Depression and anxiety were shown to have a considerable negative effect on a variety of outcomes in AMI survivors including health-related quality of life (14, 15), work-resumption (16), recurrent AMI events, and mortality (17–20). Also, a number of factors were shown to contribute to post-AMI mental health problems, such as history of depression, stressors, e.g. financial strain, poor self-rated health, low socioeconomic status, and type-D personality (21–23).
Despite the high prevalence of depression and anxiety in AMI patients and the availability of effective treatment approaches, many of these patients remain undiagnosed and untreated (24–26). A meta-analysis of 15 cohort studies in patients with AMI showed that of 2381 depressed individuals 14% used antidepressant medication (27). Compared with depression treatment rates around 30% in the general population, undertreatment seems to be more common in post AMI patients (28, 29). The specific reasons for the persisting underdiagnosis and undertreatment of mental health problems in AMI patients remain unclear (30). Besides barriers located in the health care system and – providers, and sociodemographic factors, e.g. age or education, a lack of MHL among patients with AMI may also contribute substantially to these findings (see Figure 1).
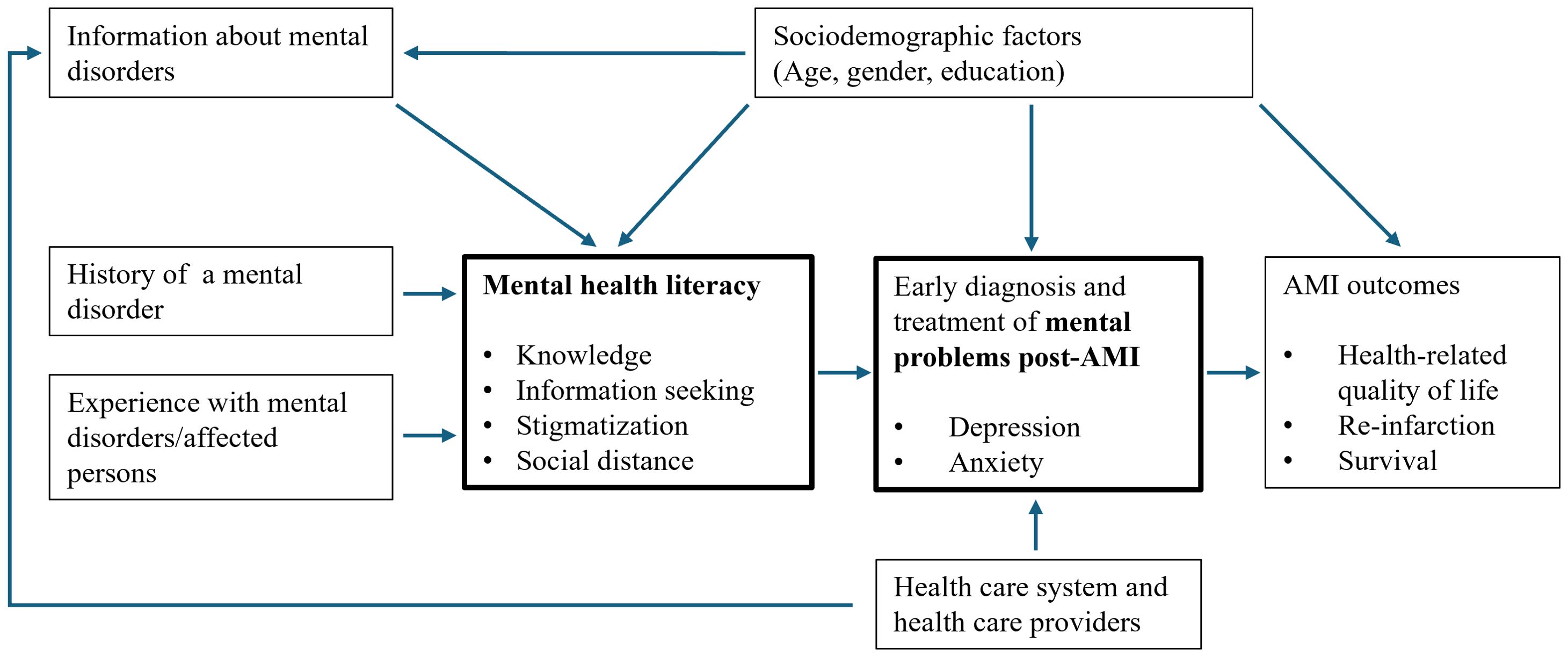
Figure 1. Conceptual model of the associations with mental health literacy in patients with acute myocardial infarction.
Figure 1 shows the conceptual framework of the present study which proposes an effect of MHL on the timely diagnosis and treatment of mental health problems in patients with AMI which may subsequently improve AMI outcomes such as health-related quality of life, re-infarction and survival. The present study will focus on factors being associated with MHL such as sociodemographic factors, history of a mental disease, experience with mental disorders or affected persons, and provision of information on mental disorders and will explore MHL in a cross-sectional, registry-based sample of patients after AMI.
2 Methods
2.1 Design and study population
The present study used data from a postal follow-up survey on participants of the Augsburg Myocardial Infarction Registry, which was established as a part of the MONICA-project (Monitoring Trends and Determinants in Cardiovascular disease) in 1984. The study area covers the city of Augsburg, Germany, and the two adjacent counties, including a total of approximately 680,000 inhabitants. The registry continuously registers all cases of coronary death and non-fatal AMI of the study population older than 24 years. Methods of case finding, diagnostic classification of AMI as well as data quality control were detailed elsewhere (31).
The registry was approved by the ethics committee of the Bavarian Medical Association (Bayerische Landesärztekammer) and the study was performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
In April 2023, all survivors with incident or recurrent AMI admitted between 2017 and 2019 (n = 1.712) were sent a questionnaire via post and were asked to complete questions on diabetes, HRQOL, depression, fatigue, and mental health literacy. A total of 855 (49.9%) patients returned the questionnaire. From the 857 non-responders, 67 patients had died, 104 had moved with unknown address, and 42 indicated that they are not willing or able to answer the questions. The remaining 644 persons received a postal reminder, but they did not respond. No significant differences between responders and non-responders in terms of age and gender were found.
2.2 Survey data
Self-developed single items requested information on previous diagnosis of mental health conditions, experiences with mental disorders in the private environment or due to a professional activity, information on AMI-related mental problems by an attending physician or during a rehabilitation program, satisfaction with the amount of information and willingness to use digital information tools (see Supplementary Table 1). The participants were also asked whether they had any mental problems after the AMI and, if so, which problems they had, whether they sought help from there private environment or from professionals, and whether they received psychotherapy or pharmacotherapy.
MHL was assessed using the German version of the ‘Mental Health Literacy Scale’ (MHLS) (32). The 35 items of the MHLS address the ability to recognize specific mental disorders, the attitudes that promote recognition and appropriate help-seeking, as well as the knowledge of how to seek mental health information, of risk factors and causes, of self-treatments, and of professional help available. The MHLS has demonstrated sufficient reliability and validity in different languages (33–38). The psychometric evaluation of the German version of the MHLS (MHLS-GER) in different samples of the German population suggests the scoring of four subscales, namely “Knowledge” (11 items), “Information seeking” (4 items), “Stigmatization” (9 items), and “Social distance” (7 items) (39). Since 4- and 5-point Likert scales were used as response scales for the different subscales, all subscale scores were transformed to a 0 to 100-point scale [(sum of item scores - minimum sum score)/(maximum sum score – minimum sum score) * 100] with higher scores indicating better MHL.
Depressive symptoms were assessed with the depression module of the Patient Health Questionnaire (PHQ) (40–42). The PHQ-9 consists of 9 items with response options from 0 to 3 (never to nearly every day), resulting in a score ranging from 0 to 27. A score less than five can be interpreted as the absence of depressiveness. Values between five and ten constitute a mild degree of depressiveness. Values of ten and higher can be subdivided into moderate (ten to 14), moderately severe (15 to 19), and severe (20 to 27) depressiveness (27). The German version of the PHQ-9 showed good psychometric properties (43).
2.3 Data analysis
Continuous variables were described as means ± standard deviations (SD) and categorical variables as absolute and relative frequencies. Subgroup differences in MHLS-GER scores were tested using Mann-Whitney U-Test or Kruskal-Wallis test. Logistic regression models were performed to estimate the relation between binary outcome variables and the independent variables age, gender, and educational attainment. Multivariable linear regression models were performed to investigate the associations between the four subscales of the MHLS-GER (dependent variables) and sociodemographic or health-related variables (independent variables). The independent variables were selected based on results from available publications. The assumptions of multivariable linear regression were ensured. Effect size was determined using Cohen’s F2. For statistical tests an alpha level of 0.05 was defined. Due to the explorative study approach no adjustment for multiple testing was applied. Statistical analyses were performed using SAS Version 9.4.
3 Results
3.1 Sample characteristics
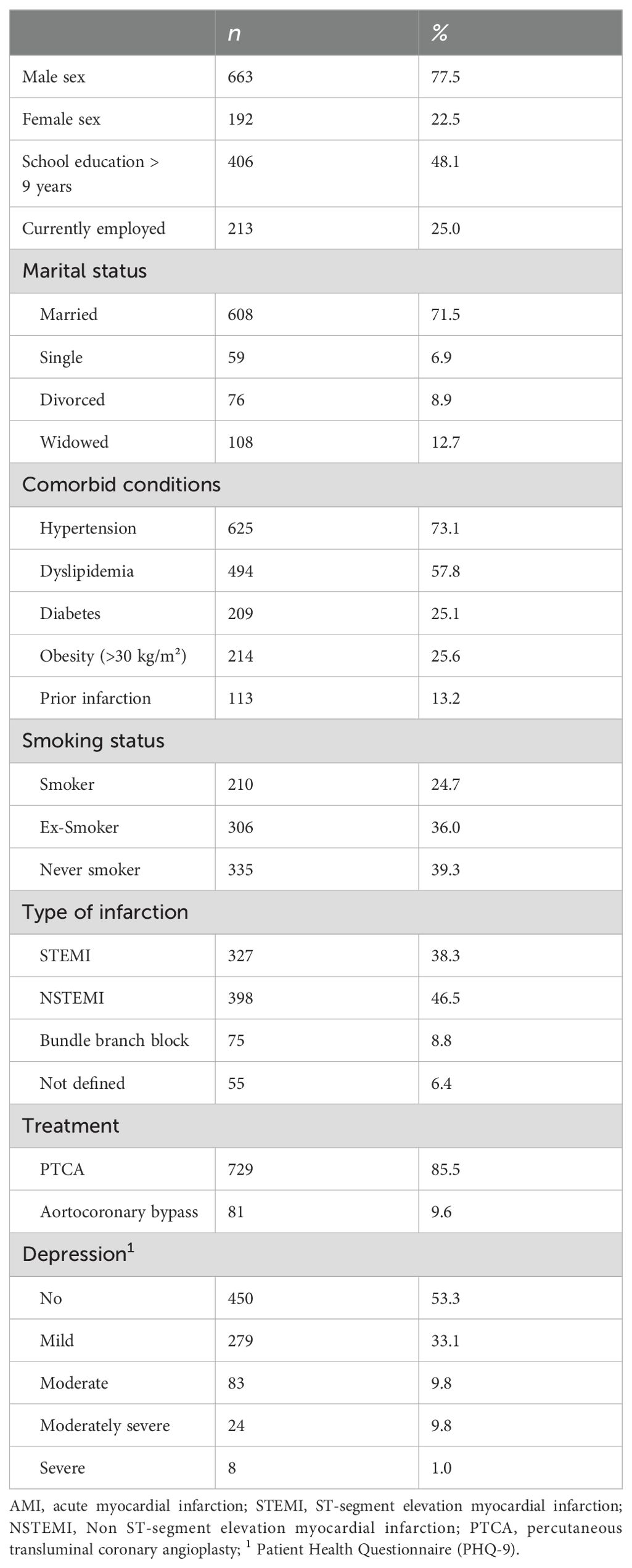
The demographic and clinical characteristics of the participants are shown in Table 1. The mean age of the enrolled participants at the time of the follow-up survey was 71.4 ± 10.9 years (Range 38 to 95 years) with 77.5% men (mean age 70.9 ± 10.8 years) and 22.5% women (mean age 73.3 ± 11.0 years). The mean time between AMI and survey was 4.8 ± 0.9 years.
3.2 Experiences with mental disorders and information about mental problems after AMI
The results stratified by gender, age and education are shown in Tables 2, 3. In brief, 10.6% of the study participants have ever been diagnosed of a mental disorder. Information about possible mental problems after their AMI were provided by a physician for 30.8% of the patients and during rehabilitation information was provided for 46.4% of the patients who received in-hospital or out-hospital rehabilitation (80.4%) A perceived lack of information was reported by 26.2% of the patients. About 31% of the patients would be willing to use digital tools for being informed about mental health problems after AMI. Mental problems after AMI were reported by 30.0% of the study participants, with 34.3% who sought help from the private environment and 32.6% from health professionals. Of those with mental problems after AMI, 17.4% received psychotherapy and 26.1% were treated with psychotropic drugs. Age emerged as the most important independent factor that was significantly associated with the responses (see Figure 2; Supplementary Table 2). Younger aged patients were significantly more likely to have a history of mental disorder, to experience mental problems after AMI, and to receive information about possible mental problems after AMI on the one hand, but to perceive an information lack on the other hand. Furthermore, younger patients were more likely to be willing to use digital tools to obtain more information, to seek help from the private environment and from health professionals and to be treated with psychotherapy or psychotropic drugs. Higher level of school education was significantly associated with mental disorders in the private environment, experiences with mental disorders due to professional activity, willingness to use digital tools for information about mental problems after AMI, and the use of psychotherapy. Women were significantly more likely than men to have a prior diagnosis of a mental disorder, to experience mental problems after AMI, to have experiences with mental disorders due to professional activity, and to prefer getting more information about mental problems after AMI.
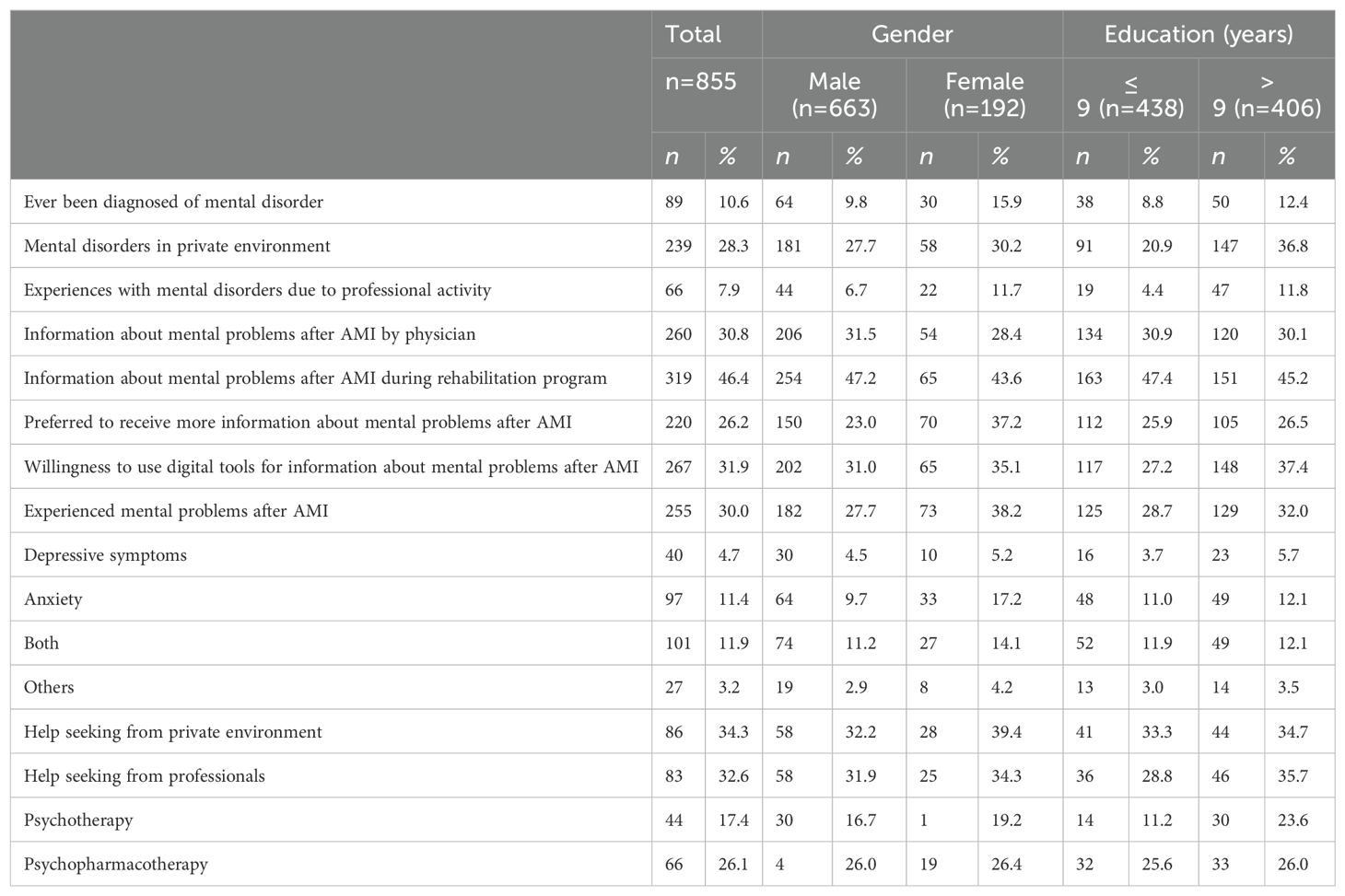
Table 2. Experiences with mental disorders and information about mental problems after acute myocardial infarction (AMI) stratified by gender, and education.
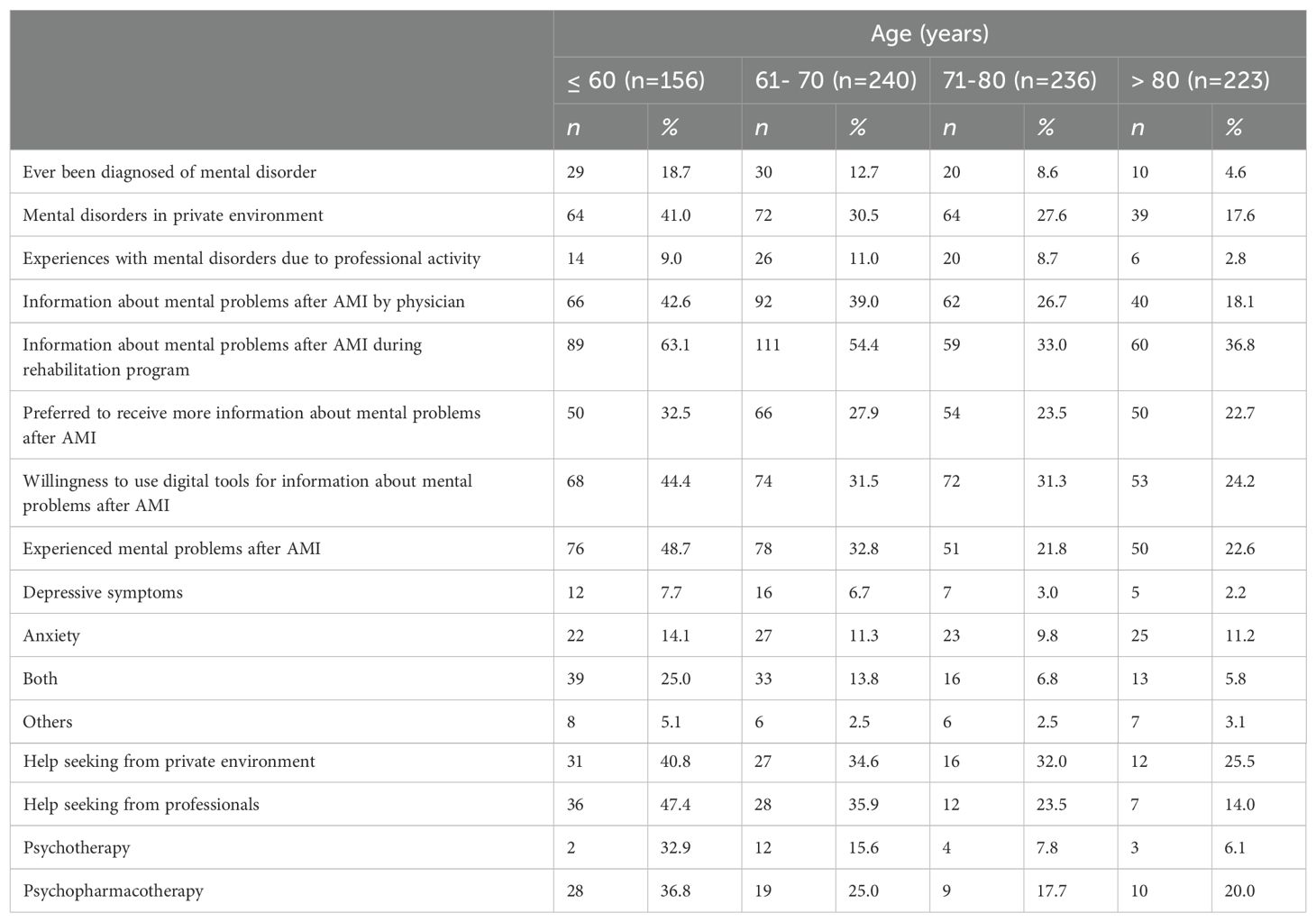
Table 3. Experiences with mental disorders and information about mental problems after acute myocardial infarction (AMI) stratified by age.
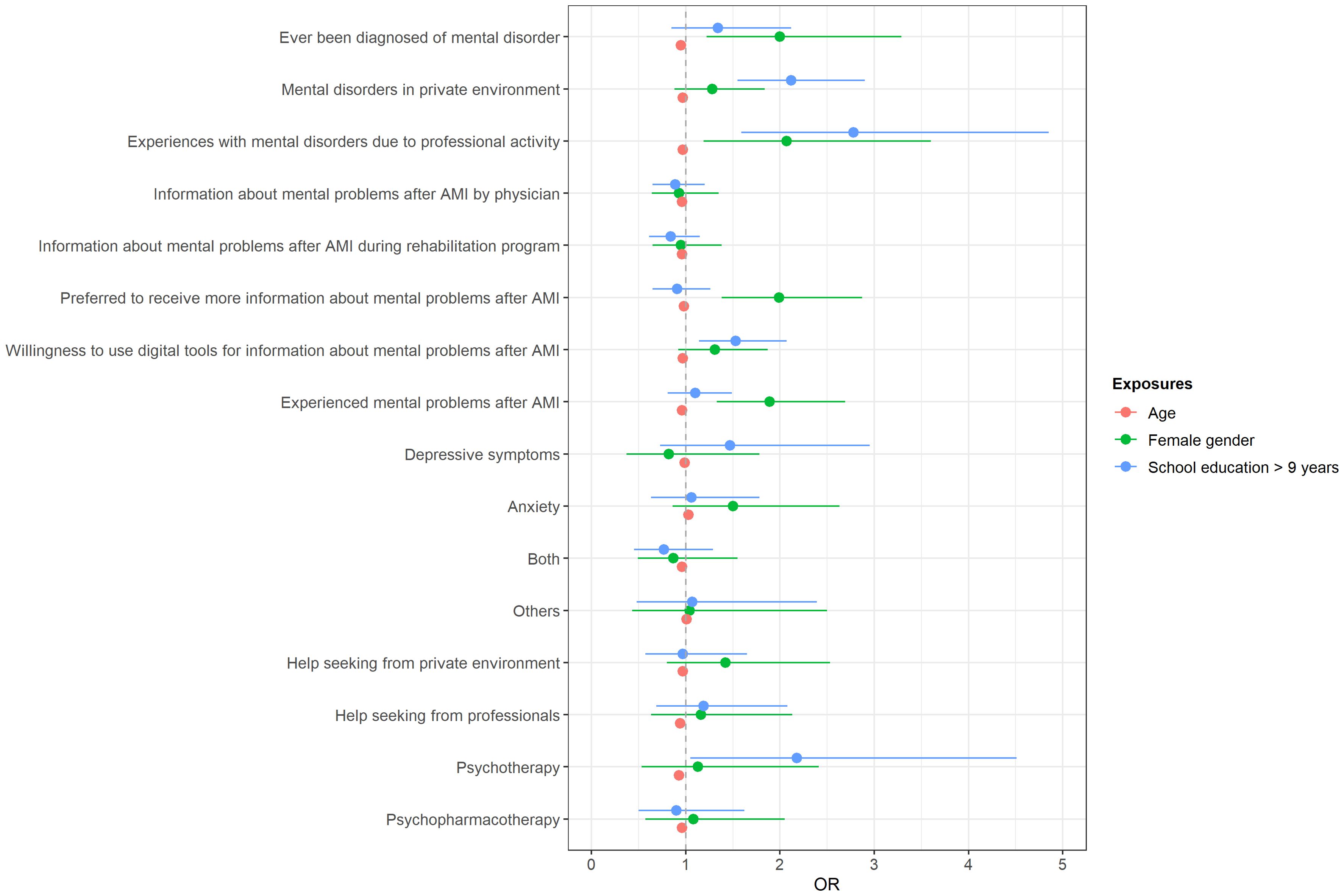
Figure 2. Multivariable logistic regression models. Outcomes: Experiences with mental disorders and information about mental problems after acute myocardial infarction, exposers: age, gender and education (OR, Odds ratio).
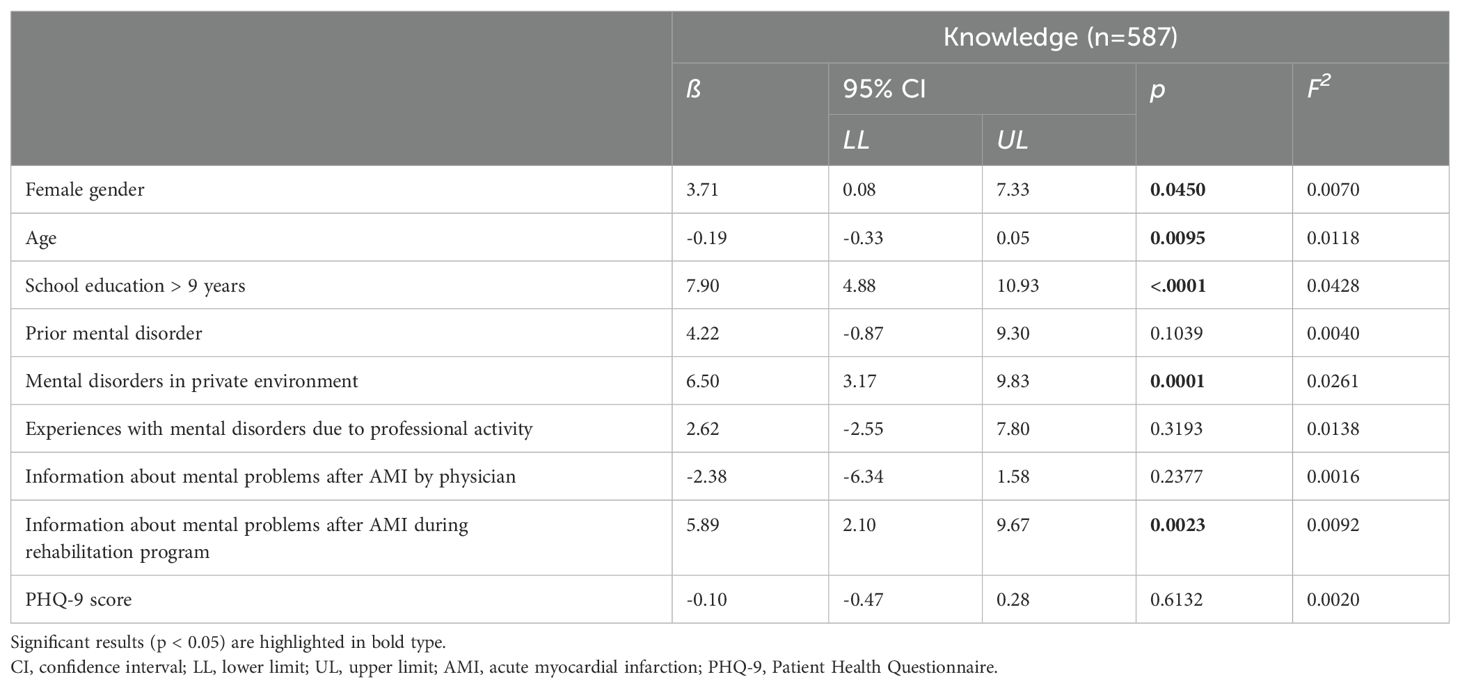
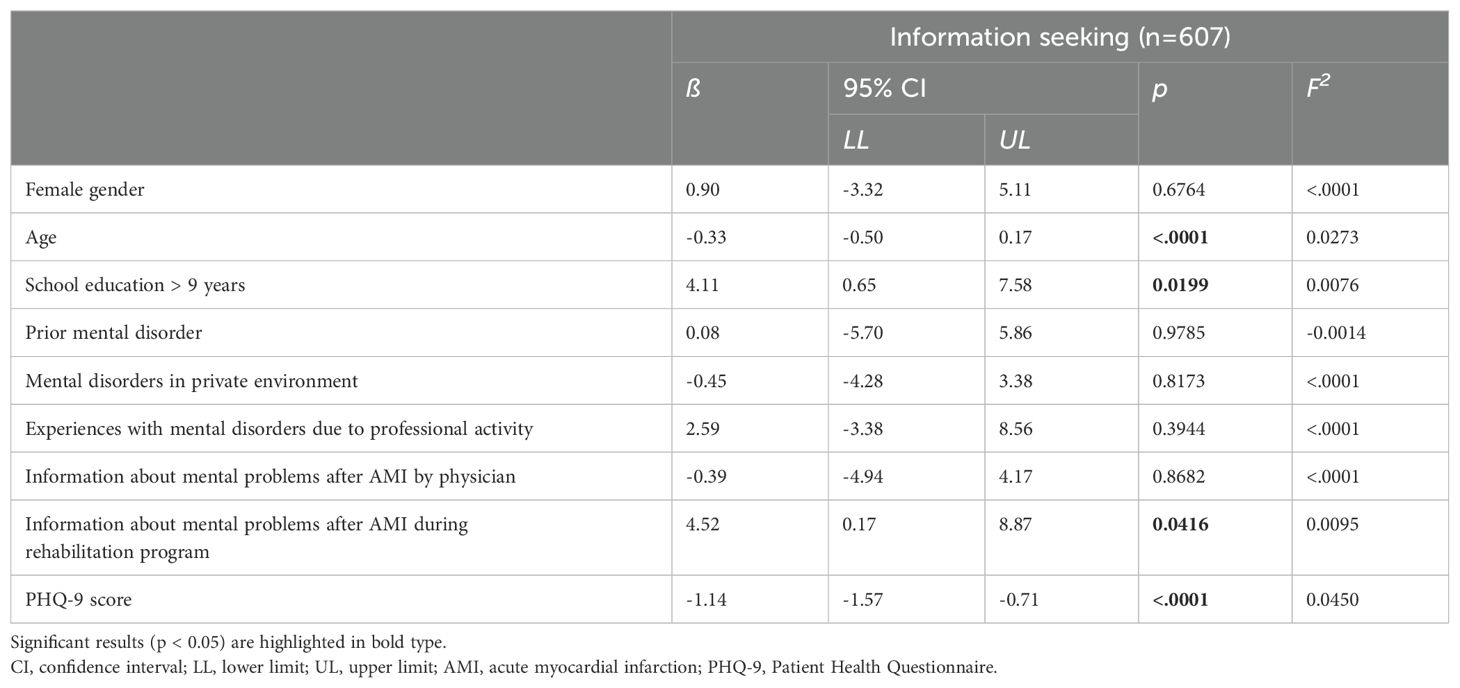
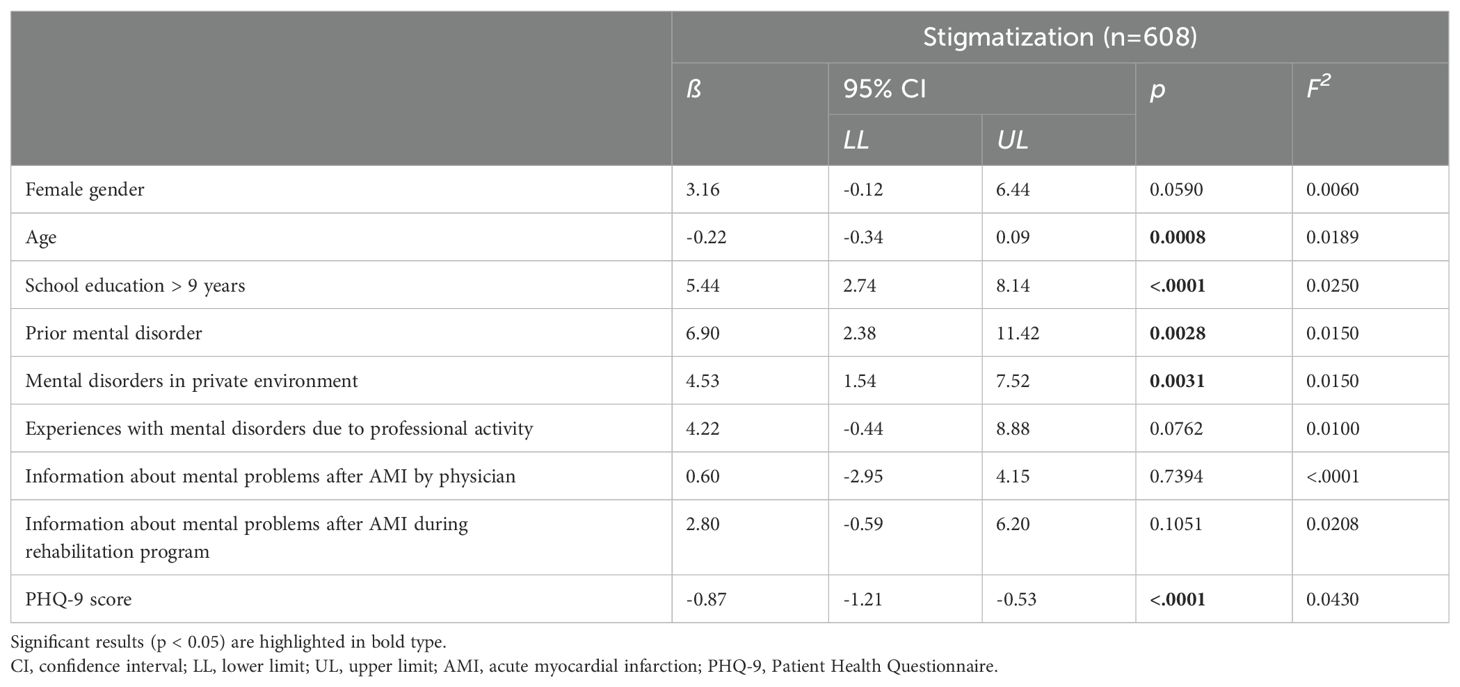
3.3 Factors associated with MHL
From the 855 respondents, 139 (16.3%) had missing scores in at least one MHLS-GER subscale. The subscale “Knowledge” was not completed by 11.5% of the participants. Participants with missing scores in at least one MHLS-GER subscale significantly differed from those who completed the questionnaire. They were significantly older (mean age 74.9 vs. 70.8 years, p<0.0001), had less often experienced mental problems after AMI (20.7% vs. 31.8%, p=0.0102), and had less experiences with mental disorders in the private environment (18.7% vs. 30.0%, p=0.0072).
Mean scores for the MHLS-GER subscales in the total sample were 64.03 ± 19.61 for “Knowledge”, 76.35 ± 22.37 for “Information seeking”, 74.17 ± 17.83 for “Stigmatization”, and 54.16 ± 21.91 for “Social distance”. Significantly higher MHLS-GER scores (indicating better MHL) in all four subscales were found in younger patients compared with older ones, and in patients who were educated about mental problems after AMI during a rehabilitation program compared with those who received no information (see Supplementary Table 3).
Furthermore, school education, prior diagnosis of a mental disorder, experiences with mental disorders in private environment, information about mental problems after AMI by a physician, perceived lack of information about mental problems after AMI, and PHQ-9 scores were significantly associated with three out of four MHLS-GER subscale scores. Experiences with mental disorders due to professional activity were significantly associated with better scores in two MHLS-GER subscale scores.
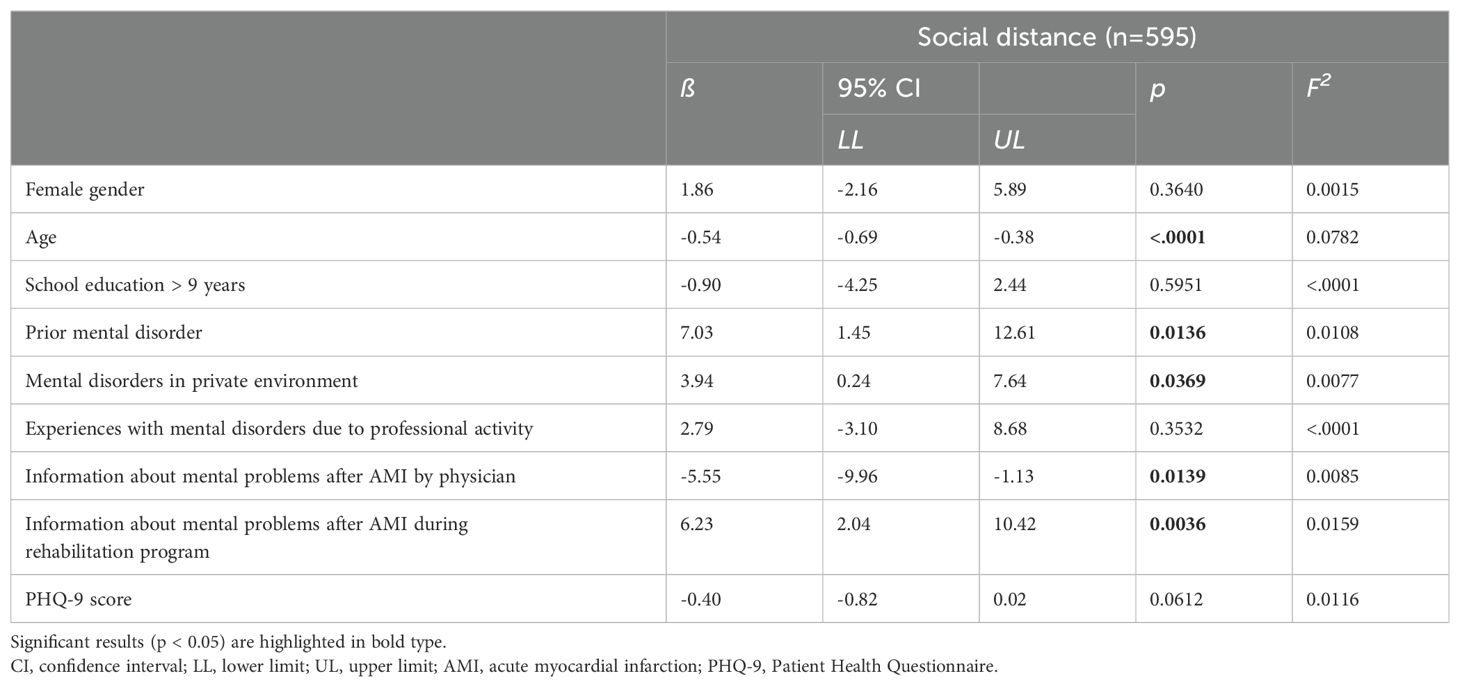
The multivariable linear regression models confirmed most of the univariable associations (see Tables 4–7). Younger age was significantly associated with better MHL in all four subscales. Higher school education, information about mental problems after AMI during a rehabilitation program, and experiences with mental disorders in private environment were significantly associated with better scores in three subscales. Patients with a prior diagnosis of a mental disorder and patients with lower PHQ-9 score had significantly better scores in two subscales compared with their counterparts. Information about mental problems after AMI by a physician was significantly associated with better scores in the subscale “Social distance”.
4 Discussion
Among the factors which are supposed to be associated with MHL according to the conceptual model displayed in Figure 1, age was the most relevant variable associated both with MHL and with other variables expected to be associated with MHL, such as information about mental disorders. Older persons were less likely to report mental problems after AMI than younger ones. However, older persons also were less likely to receive information about AMI by a doctor or in a rehabilitation setting and they had less often personal experiences with mental disorders than younger patients. Knowledge of mental health problems and proximity to individuals with mental health problems have been identified as major aspects of MHL which may also facilitate an early diagnosis and treatment of mental disorders (44). Indeed, the older patients who reported mental problems after AMI showed reduced help seeking behavior and were less often treated with psychotherapy or pharmacological treatment compared with younger patients. These findings may be to some extent caused by the overall lower MHL reflected by poorer scores in all MHLS-GER subscales compared with younger individuals. The association of age and MHL has been only rarely investigated in older aged populations so far and showed conflicting results (45, 46). The results from the present study, however, support that older age is also associated with poorer MHL in a sample of persons with AMI aged 71 years in average.
Besides age, poor education was identified as a relevant variable shown to be significantly related with poor MHL reflected by low scores in the MHLS-GER subscales “Knowledge”, “Information seeking”, and “Stigmatization” in the present study. Comparable results were found in a number of prior studies with different age groups, nationalities and health states (46–51). Furthermore, the results from the present study confirmed other studies that found associations between MHL and gender (47, 48, 52, 53), and MHL and proximity to persons with mental disorders in the private environment (54, 55).
Information about mental health problems after AMI provided by health carers is another important factor shown to be related with MHL in the present study. More than one fourth of all study participants reported that they would have preferred to receive more information about possible mental problems after AMI. Interestingly, these patients were younger, more often women and had more often private contacts with persons with mental disorders. Those persons seem to be already sensitized for mental health issues and thus open for further information regarding their own situation.
Of interest, patients who received information about possible mental problems after AMI in the post-AMI rehabilitation setting, showed significantly better MHL than patients without being informed. This finding may point to in-hospital or out-patient rehabilitation as a meaningful setting for interventions aiming to improve MHL in patients with AMI. However, it must be considered that in Germany about 20% of the patients with AMI do not utilize rehabilitation and thus interventions on MHL should also be offered in other settings. Education and provision of information are common interventions to improve MHL and digital provision of information, e.g. by internet websites or Apps, is increasingly applied in health care (56, 57). However, the results from this study also point to possible limitations of such an approach in older-aged target groups since in the study population of AMI patients only about one third reported to be willing to receive digital information on mental health problems after AMI. Thus, it seems essential that interventions on MHL in patients with AMI consider the personal and environmental characteristics of this group and chose a suitable communication medium and setting.
The present study also demonstrated that poor MHLS-GER scores of the subscales “Information seeking” and “Stigmatization” are associated with more depressive symptomatology according to PHQ-9 scores. This finding is consistent with Ding et al. (58) who found significant independent associations between PHQ-9 scores and MHL in a sample of the Chinese population with a mean age of 70 years. Further in-depth investigations of the relationships between the different variables and MHL are needed in order to increase knowledge about mediating, moderating or causal effects (45).
The present study also points to important aspects of MHL assessment in an elderly sample of patients with a somatic disorder. First, we assume that the questions on mental health and MHL have reduced the overall response rate, which was 49% and considerably lower than in previous follow-up surveys conducted at the Myocardial Infarction Registry with response rates of e.g. 67% (59). Some comments from non-responding patients indicated that it made no sense for them to complete questions on mental health issues since they have a somatic disease. This points to the missing awareness of mental comorbidities in somatic disorders.
To our knowledge, the present study is the first which investigated MHL in patients with AMI. Strengths of this study are the large number of well-characterized consecutive AMI-patients from a population-based registry. However, we cannot exclude a selection bias towards patients with better MHL as they were more likely to complete the questionnaire. Furthermore, patients with missing scores in the MHLS-GER significantly differed from those who completed the scale. Symptoms of depression were assessed using the PHQ-9, however, a clinical diagnosis of depression was not available. Since a comparison group is missing, the MHLS-GER scores of persons with AMI cannot be compared with persons without AMI. It cannot be excluded that other relevant covariables which may be associated with MHL, e.g. nationality, migration background or others, were not considered. Furthermore, due to the cross-sectional study design, causal relationships between the variables investigated cannot be deduced. Finally, the results may not be generalizable to other age-groups, ethnic groups and non-European nationalities.
In conclusion, the present study found a considerable burden of mental health problems in patients about 5 years after their AMI. Specifically elderly and poorly educated patients were identified as a risk group of poor MHL, subsequent undertreatment and persisting impaired mental health. Further studies are required to specify the role of MHL in post-AMI life and mental health care. Based on these results, interventions aimed at improving MHL in this patient group may be developed, which should be tailored to subgroups of patients with highest risk of poor MHL such as elderly and poorly educated, should apply a suitable communication medium and setting, and should be evaluated in randomized controlled studies.
Data availability statement
The data that support the findings of this study are available from the Chair of Epidemiology, Medical Faculty, University of Augsburg but restrictions apply to the availability of these data, which are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the Chair of Epidemiology. Requests to access the datasets should be directed to SW5nZS5LaXJjaGJlcmdlckBtZWQudW5pLWF1Z3NidXJnLmRl.
Ethics statement
The studies involving humans were approved by Ethical committee of the Bavarian Medical Association. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
IK: Conceptualization, Formal analysis, Methodology, Writing – original draft. SF: Formal analysis, Methodology, Writing – review & editing. PR: Resources, Supervision, Writing – review & editing. JL: Funding acquisition, Resources, Supervision, Writing – review & editing. CM: Funding acquisition, Methodology, Resources, Supervision, Writing – review & editing. TS: Conceptualization, Funding acquisition, Investigation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research received support from the Faculty of Medicine, University of Augsburg, and the University Hospital of Augsburg, Germany. Since the year 2000, the collection of AMI data has been co-financed by the German Federal Ministry of Health to provide population-based AMI morbidity data for the official German Health Report (see http://www.gbe-bund.de).
Acknowledgments
We would like to thank all members of the Chair of Epidemiology, Medical Faculty, University of Augsburg, who were involved in the planning and conduct of the study. Many thanks for their support go to the local health departments, the office-based physicians and the clinicians of the hospitals within the study area. Finally, we express our appreciation to all study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1444381/full#supplementary-material
References
1. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. (1997) 166:182–6. doi: 10.5694/j.1326-5377.1997.tb140071.x
2. Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. (2012) 67:231–43. doi: 10.1037/a0025957
3. WHO. The top 10 causes of death. Available online at: https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death (Accessed 08/02/2023).
4. Dégano IR, Salomaa V, Veronesi G, Ferriéres J, Kirchberger I, Laks T, et al. Twenty-five-year trends in myocardial infarction attack and mortality rates, and case-fatality, in six European populations. Heart. (2015) 101:1413–21. doi: 10.1136/heartjnl-2014-307310
5. Headrick JP, Peart JN, Budiono BP, Shum DHK, Neumann DL, Stapelberg NJC. The heartbreak of depression: ‘Psycho-cardiac’ coupling in myocardial infarction. J Mol Cell Cardiol. (2017) 106:14–28. doi: 10.1016/j.yjmcc.2017.03.007
6. Lu Y, Wang Z, Georgakis MK, Lin H, Zheng L. Genetic liability to depression and risk of coronary artery disease, myocardial infarction, and other cardiovascular outcomes. J Am Heart Assoc. (2021) 10:e017986. doi: 10.1161/JAHA.120.017986
7. Li GH, Cheung CL, Chung AK, Cheung BM, Wong IC, Fok MLY, et al. Evaluation of bi-directional causal association between depression and cardiovascular disases: a Mendelian randomization study. Psychol Med. (2022) 52:1765–76. doi: 10.1017/S0033291720003566
8. Feng L, Li L, Liu W, Yang J, Wang Q, Shi L, et al. Prevalence of depression in myocardial infarction: A PRISMA-compliant meta-analysis. Med (Baltimore). (2019) 98:e14596. doi: 10.1097/MD.0000000000014596
9. Dong Z, Yang Q, Chen H. Estimating the prevalence of depression in people with acute coronary syndromes: A systematic review and meta-analysis. Med (Baltimore). (2024) 103:e37906. doi: 10.1097/MD.0000000000037906
10. Lian Y, Xiang J, Wang X, Kaminga AC, Chen W, Lai Z, et al. Prevalence of moderate to severe anxiety symptoms among patients with myocardial infarction: a meta-analysis. Psychiatr Q. (2022) 93:161–80. doi: 10.1007/s11126-021-09921-y
11. Busch MA, Maske UE, Ryl L, Schlack R, Hapke U. Prävalenz von depressiver Symptomatik und diagnostizierter Depression bei Erwachsenen in Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) [Prevalence of depressive symptoms and diagnosed depression among adults in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2013) 56:733–9. doi: 10.1007/s00103-013-1688-3
12. Hajek A, König HH. Prevalence and correlates of individuals screening positive for depression and anxiety on the PHQ-4 in the German general population: findings from the nationally representative German socio-economic panel (GSOEP). Int J Environ Res Public Health. (2020) 17:7865. doi: 10.3390/ijerph17217865
13. Kocalevent RD, Hinz A, Brähler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2013) 35:551–5. doi: 10.1016/j.genhosppsych.2013.04.006
14. Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Effects of depression and anxiety on mortality and quality-of-life 4 months after myocardial infarction. J Psychosom Res. (2000) 49:229–38. doi: 10.1016/S0022-3999(00)00170-7
15. Dickens CM, McGowan L, Percival C, Tomenson B, Cotter L, Heagerty A, et al. Contribution of depression and anxiety to impaired health-related quality of life following first myocardial infarction. Br J Psychiatry. (2006) 189:367–72. doi: 10.1192/bjp.bp.105.018234
16. O’Neil A, Sanderson K, Oldenburg B. Depression as a predictor of work resumption following myocardial infarction (MI): a review of recent research evidence. Health Qual Life Outcomes. (2010) :8:95. doi: 10.1186/1477-7525-8-95
17. Meijer A, Conradi HJ, Bos EH, Anselmino M, Carney RM, Denollet J, et al. Adjusted prognostic association of depression following myocardial infarction with mortality and cardiovascular events: individual patient data meta-analysis. Br J Psychiatry. (2013) 203:90–102. doi: 10.1192/bjp.bp.112.111195
18. Wu Q, Kling JM. Depression and the risk of myocardial infarction and coronary death: A meta-analysis of prospective cohort studies. Med (Baltimore). (2016) 95:e2815. doi: 10.1097/MD.0000000000002815
19. Roest AM, Martens EJ, Denollet J, de Jonge P. Prognostic association of anxiety post myocardial infarction with mortality and new cardiac events: a meta-analysis. Psychosom Med. (2010) 72:563–9. doi: 10.1097/PSY.0b013e3181dbff97
20. Celano CM, Millstein RA, Bedoya CA, Healy BC, Roest AM, Huffman JC. Association between anxiety and mortality in patients with coronary artery disease: A meta-analysis. Am Heart J. (2015) 170:1105–15. doi: 10.1016/j.ahj.2015.09.013
21. Doi-Kanno M, Fukahori H. Predictors of Depression in Patients Diagnosed with Myocardial Infarction after Undergoing Percutaneous Coronary Intervention: A literature review. J Med Dent Sci. (2016) 63:37–43. doi: 10.11480/jmds.630301
22. Murphy B, Le Grande M, Alvarenga M, Worcester M, Jackson A. Anxiety and depression after a cardiac event: prevalence and predictors. Front Psychol. (2020) 10:3010. doi: 10.3389/fpsyg.2019.03010
23. Martens EJ, Smith ORF, Winter J, Denollet J, Pedersen SS. Cardiac history, prior depression and personality predict course of depressive symptoms after myocardial infarction. psychol Med. (2008) 38:257–64. doi: 10.1017/S0033291707001377
24. Huffman C, Smith FA, Blais MA, Beiser ME, Januzzi JL, Fricchione GL. Recognition and treatment of depression and anxiety in patients with acute myocardial infarction. Am J Cardiol. (2006) 98:319–24. doi: 10.1016/j.amjcard.2006.02.033
25. Amin AA, Jones AM, Nugent K, Rumsfeld JS, Spertus JA. The prevalence of unrecognized depression in patients with acute coronary syndrome. Am Heart J. (2006) 152:928–34. doi: 10.1016/j.ahj.2006.05.006
26. Pogosova N, Kotseva K, De Bacquer D, von Känel R, De Smedt D, Bruthans J, et al. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: Results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur J Prev Cardiol. (2017) 24:1371–80. doi: 10.1177/2047487317711334
27. Ladwig S, Zhou Z, Xu Y, Wang X, Chow CK, Werheid K, et al. Comparison of treatment rates of depression after stroke versus myocardial infarction: A systematic review and meta-analysis of observational data. Psychosom Med. (2018) 80:754–63. doi: 10.1097/PSY.0000000000000632
28. Mekonen T, Chan GCK, Connor JP, Hides L, Leung J. Estimating the global treatment rates for depression: A systematic review and meta-analysis. J Affect Disord. (2021) 295:1234–42. doi: 10.1016/j.jad.2021.09.038
29. Moitra M, Santomauro D, Collins PY, Vos T, Whiteford H, Saxena S, et al. The global gap in treatment coverage for major depressive disorder in 84 countries from 2000-2019: A systematic review and Bayesian meta-regression analysis. PloS Med. (2022) 19:e1003901. doi: 10.1371/journal.pmed.1003901
30. Peltzer S, Köstler U, Müller H, Scholten N, Schulz-Nieswandt F, Jessen F, et al. The psychological consequences of living with coronary heart disease: Are patients’ psychological needs served? A mixed-method study in Germany. Health Expect. (2022) 25:2746–61. doi: 10.1111/hex.13467
31. Meisinger C, Hoermann A, Heier M, Kuch B, Lowel H. Admission blood glucose and adverse outcomes in non-diabetic patients with myocardial infarction in reperfusion era. Int J Cardiol. (2006) 113:229–35. doi: 10.1016/j.ijcard.2005.11.018
32. O’Connor M, Casey L. The Mental Health Literacy Scale (MHLS): A new scale-based measure of mental health literacy. Psychiatry Res. (2015) 229:511–6. doi: 10.1016/j.psychres.2015.05.064
33. Montagni I, González Caballero JL. Validation of the mental health literacy scale in French university students. Behav Sci (Basel). (2022) 12:259. doi: 10.3390/bs12080259
34. Dias Neto D, Rocha I, Figueiras MJ, Nuenes da Silva A. Measuring health literacy. Adaptation and validation of the Portuguese version of the mental health literacy scale (MHLS). Eur J Ment Health. (2021) 16:64–77. doi: 10.5708/EJMH.16.2021.1.5
35. Heizomi H, Kouzekanani K, Asghari Jafarabadi M, Allahverdipour H. Psychometric properties of the Persian version of mental health literacy scale. Int J Womens Health. (2020) 12:513–20. doi: 10.2147/IJWH.S252348
36. Nejatian M, Tehrani H, Momeniyan V, Jafari A. A modified version of the mental health literacy scale (MHLS) in Iranian people. BMC Psychiatry. (2021) 21:53. doi: 10.1186/s12888-021-03050-3
37. Alshehri E, Alosaimi D, Rufaidi E, Alsomali N, Tumala R. Mental health literacy scale Arabic version: A validation study among Saudi university students. Front Psychiatry. (2021) :741146. doi: 10.3389/fpsyt.2021.741146
38. Chen S, Chen K, Wang S, Wang W, Li Y. Initial validation of a Chinese version of the mental health literacy scale among Chinese teachers in Henan province. Front Psychiatry. (2021) 12:661903. doi: 10.3389/fpsyt.2021.661903
39. Fischer S, Schmitz T, Meisinger C, Linseisen J, Kirchberger I. German translation and psychometric evaluation of the Mental Health Literacy Scale (MHLS-GER) in a general population sample and in patients with acute myocardial infarction. J Psychiatr Res. (2024) 178:201–9. doi: 10.1016/j.jpsychires.2024.08.008
40. Löwe B, Spitzer R, Zipfel S, Herzog W. PHQ-D Manual. Komplettversion und Kurzform. Autorisierte deutsche Version des “Prime MD Patient Health Questionnaire (PHQ)”. In: PLOS Blogs. Heidelberg (2002). Available at: https://www.klinikum.uni-heidelberg.de/fileadmin/Psychosomatische_Klinik/download/PHQ_Manual1.pdf.
41. Kroenke K, Spitzer RL, Williams JBW, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. (2010) 32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006
42. Manea L, Gilbody S, McMillan D. A diagnostic meta-analysis of the Patient Health Questionnaire-9v(PHQ-9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry. (2015) 37:67–75. doi: 10.1016/j.genhosppsych.2014.09.009
43. Löwe B, Gräfe K, Quenter A, Zipfel S, Herzog W. Screening psychischer Störung mit dem Gesundheitsfragebogen für Patienten (PHQD) Ergebnisse der deutschen Validierungsstudie. Diagnostica. (2004) 50:171–81. doi: 10.1026/0012-1924.50.4.171
44. Bartels SM, Cardenas P, Uribe-Restrepo JM, Cubillos L, Torrey WC, Castro SM, et al. Barriers and facilitators to the diagnosis and treatment of depression in primary care in Colombia: Perspectives of providers, healthcare administrators, patients and community representatives. Rev Colomb Psiquiatr (Engl Ed). (2021) 50 Suppl 1:64–72. doi: 10.1016/j.rcpeng.2021.01.001
45. Root EZ, Caskie GIL. The associations between eMental health literacy, barriers to mental health services, and psychological distress in older adults. J Appl Gerontol. (2023) 42:951–61. doi: 10.1177/07334648221146775
46. Piper SE, Bailey PE, Lam LT, Kneebone II. Predictors of mental health literacy in older people. Arch Gerontol Geriatr. (2018) 79:52–6. doi: 10.1016/j.archger.2018.07.010
47. Kim YS, Lee HY, Lee MH, Simms T, Park BH. Mental health literacy in korean older adults: A cross-sectional survey. J Psychiatr Ment Health Nurs. (2017) 24:523–33. doi: 10.1111/jpm.12395
48. Simões de Almeida R, Trigueiro MJ, Portugal P, de Sousa S, Simões-Silva V, Campos F, et al. Mental health literacy and stigma in a municipality in the north of Portugal: A cross-sectional study. Int J Environ Res Public Health. (2023) 20:3318. doi: 10.3390/ijerph20043318
49. Jafari A, Nejatian M, Momeniyan V, Barsalani FR, Tehrani H. Mental health literacy and quality of life in Iran: a cross-sectional study. BMC Psychiatry. (2021) 21:499. doi: 10.1186/s12888-021-03507-5
50. Adu P, Jurcik T, Dmitry G. Mental health literacy in Ghana: Implications for religiosity, education and stigmatization. Transcult Psychiatry. (2021) 58:516–31. doi: 10.1177/13634615211022177
51. Lopez V, Sanchez K, Killian MO, Eghaneyan BH. Depression screening and education: an examination of mental health literacy and stigma in a sample of Hispanic women. BMC Public Health. (2018) 18:646. doi: 10.1186/s12889-018-5516-4
52. Tesfaye Y, Agenagnew L, Anand S, Tucho GT, Birhanu Z, Ahmed G, et al. Knowledge of the community regarding mental health problems: a cross-sectional study. BMC Psychol. (2021) 9:106. doi: 10.1186/s40359-021-00607-5
53. Tariku Seboka B, Hailegebreal S, Negash M, Mamo TT, Ali Ewune H, Gilano G, et al. Predictors of mental health literacy and information seeking behavior toward mental health among university students in resource-limited settings. Int J Gen Med. (2022) 15:8159–72. doi: 10.2147/IJGM.S377791
54. Singh S, Zaki RA, Farid NDN, Kaur K. The determinants of mental health literacy among young adolescents in Malaysia. Int J Environ Res Public Health. (2022) 19:3242. doi: 10.3390/ijerph19063242
55. Phoa PKA, Ab Razak A, Kuay HS, Ghazali AK, Ab Rahman A, Husain M, et al. Predictors of mental health literacy among parents, guardians, and teachers of adolescents in west Malaysia. Int J Environ Res Public Health. (2023) 20:825. doi: 10.3390/ijerph20010825
56. Ren Z, Zhao C, Tian F, Yan Y, Li D, Zhao Z, et al. Meta-analysis of the effect of mental health literacy intervention in Chinese people. Acta Psychologica Sin. (2020) (4):497–521. doi: 10.3724/SP.J.1041.2019.00497
57. Jorm AF. Mental health literacy interventions in adults. In: Okan O, Bauer U, Levin-Zamir D, Pinheiro P, Sorensen K, editors. International handbook of health literacy. Research, practice and policy across the lifespan. Policy Press, Bristol (2019). p. 359–70.
58. Ding KR, Wang SB, Xu WQ, Lin LH, Liao DD, Chen HB, et al. Low mental health literacy and its association with depression, anxiety and poor sleep quality in Chinese elderly. Asia Pac Psychiatry. (2022) 14:e12520. doi: 10.1111/appy.12520
Keywords: mental health literacy, myocardial infarction, depression feldfunktion geändert, help seeking behavior, education
Citation: Kirchberger I, Fischer S, Raake P, Linseisen J, Meisinger C and Schmitz T (2024) Mental health literacy in patients with acute myocardial infarction: a cross-sectional registry-based study. Front. Psychiatry 15:1444381. doi: 10.3389/fpsyt.2024.1444381
Received: 05 June 2024; Accepted: 21 October 2024;
Published: 13 November 2024.
Edited by:
Marlies Elizabeth Alvarenga, Institute of Health and Wellbeing, AustraliaReviewed by:
Ervin Toci, University of Medicine, AlbaniaDon Byrne, Australian National University, Australia
Copyright © 2024 Kirchberger, Fischer, Raake, Linseisen, Meisinger and Schmitz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Inge Kirchberger, SW5nZS5LaXJjaGJlcmdlckBtZWQudW5pLWF1Z3NidXJnLmRl
 Inge Kirchberger
Inge Kirchberger Simone Fischer
Simone Fischer Philip Raake2
Philip Raake2 Jakob Linseisen
Jakob Linseisen Timo Schmitz
Timo Schmitz