- 1Department of Community Medicine, Government Medical College, Jammu, Jammu and Kashmir, India
- 2Department of Community Medicine, Acharya Shri Chander College of Medical Sciences and Hospital, Jammu, Jammu and Kashmir, India
- 3Institute of Human Genetics, University of Jammu, Jammu, Jammu and Kashmir, India
- 4Department of Human Genetics, Sri Pratap College, Cluster University Srinagar, Kashmir, Jammu and Kashmir, India
- 5Department of Psychology, Govt., Degree College, Billawar, Kathua, Jammu and Kashmir, India
- 6Department of Psychology, University of Jammu, Jammu, Jammu and Kashmir, India
- 7Department of Zoology, University of Jammu, Jammu, Jammu and Kashmir, India
- 8Department of Psychiatry, Government Medical College, Jammu, Jammu and Kashmir, India
- 9Department of Neurology, Super Specialty Hospital, Government Medical College, Jammu, Jammu and Kashmir, India
- 10Department of Community Medicine, All India Institute of Medical Science, Jammu, Jammu and Kashmir, India
Background: Mental health is crucial for overall well-being, but rural areas often face difficulties in accessing mental health services and understanding psychiatric disorders.
Aim: This study aimed to address these issues by assessing the prevalence of psychiatric disorders among adults in rural Jammu and examining how socio-cultural and demographic factors are related to these disorders.
Methods: A sample of 1,016 adults from rural Jammu was surveyed using the Mini International Neuropsychiatric Interview (MINI). Data were collected through house-to-house visits conducted by trained investigators. Descriptive and inferential statistics, including frequency distribution and odds ratio, were employed to analyze the data respectively.
Results: Overall, 20.67% of the participants had a psychiatric disorder. Alcohol dependence was the most common condition, affecting 12.30% of the individuals, followed by generalized anxiety disorder at 3.14%. The study found significant associations between psychiatric disorders and several factors. Specifically, older people were more likely to have psychiatric disorders, with an odds ratio of 3.7 [2.07-6.59]. Married individuals also had a higher likelihood of experiencing psychiatric disorders (OR: 2.3 [1.55-3.54]). Those with less schooling were at an increased risk, with an odds ratio of 7.77 [2.31-26.09], and people from lower socioeconomic backgrounds were more likely to have these disorders as well (OR: 5.1 [2.4-10.5]).
Discussion and conclusion: The findings underscore the complex association between socio-demographic factors and mental health outcomes in rural areas of Jammu region. Addressing these disparities requires targeted interventions and policies that account for the unique socio-cultural contexts of rural populations. By understanding the specific challenges faced by these communities, policymakers and healthcare providers can develop more effective strategies to enhance mental health services and promote well-being.
Introduction
Health is considered the most valuable asset, encompassing physical, mental, and social well-being, and not merely the absence of disease or infirmity, as defined by the World Health Organization (WHO) (1). An important implication of this definition is that mental health is more than just the absence of mental disorders or disabilities; it also includes resilience, social functioning, and overall quality of life. Recent advancements in psychiatry have significantly deepened our understanding of mental illnesses and their complexities. This growing knowledge has led to new perspectives on the causes of these conditions and the development of more effective treatment strategies (2). In light of this, there is increasing acknowledgment of the necessity to comprehend the prevalence and factors influencing psychiatric disorders, especially in rural and underserved communities (3) such as rural areas of Jammu (R.S. Pura). Numerous neurological diseases affecting the Jammu area have been the subject of notable research, including headaches (4), epilepsy (5, 6), and others (7, 8). Likewise, the Kashmir region of Jammu and Kashmir, India (UT) has been the site of many studies about different types of mental diseases such as depression, post-traumatic stress disorders (PTSD), and generalized anxiety disorders (9–12).
However, mental health research specifically in rural Jammu, such as R.S. Pura, is noticeably lacking. This may be due to the region’s unique socio-political challenges, as it is located near the international border between India and Pakistan. The limited research in this area underscores its status as an underserved community, warranting a focused investigation into mental health challenges. Therefore, this study primarily aims to determine the frequency of psychiatric disorders among people residing in rural Jammu. Additionally, we hope to shed light on this crucial aspect of mental health in the area by exploring the link between demographics, culture, socioeconomic status, and mental illness.
Method
Ethical consideration
Ethical clearance was secured from the Institutional Ethical Committee (IEC) of Government Medical College, Jammu, Jammu and Kashmir. All participants were asked to provide their informed consent before they were involved. They understood that their participation in the study would remain anonymous and confidential.
Sample size
A sample size of 1016 participants was determined to estimate mental disorder prevalence with a 10% baseline within a 20% margin of error. This estimation was conducted at a significance level of 5% (95% confidence level) and a power of 80%. Accounting for a 10% non-response rate ensures robust analysis and meaningful interpretation of the study findings.
Participants, sampling method, and data collection
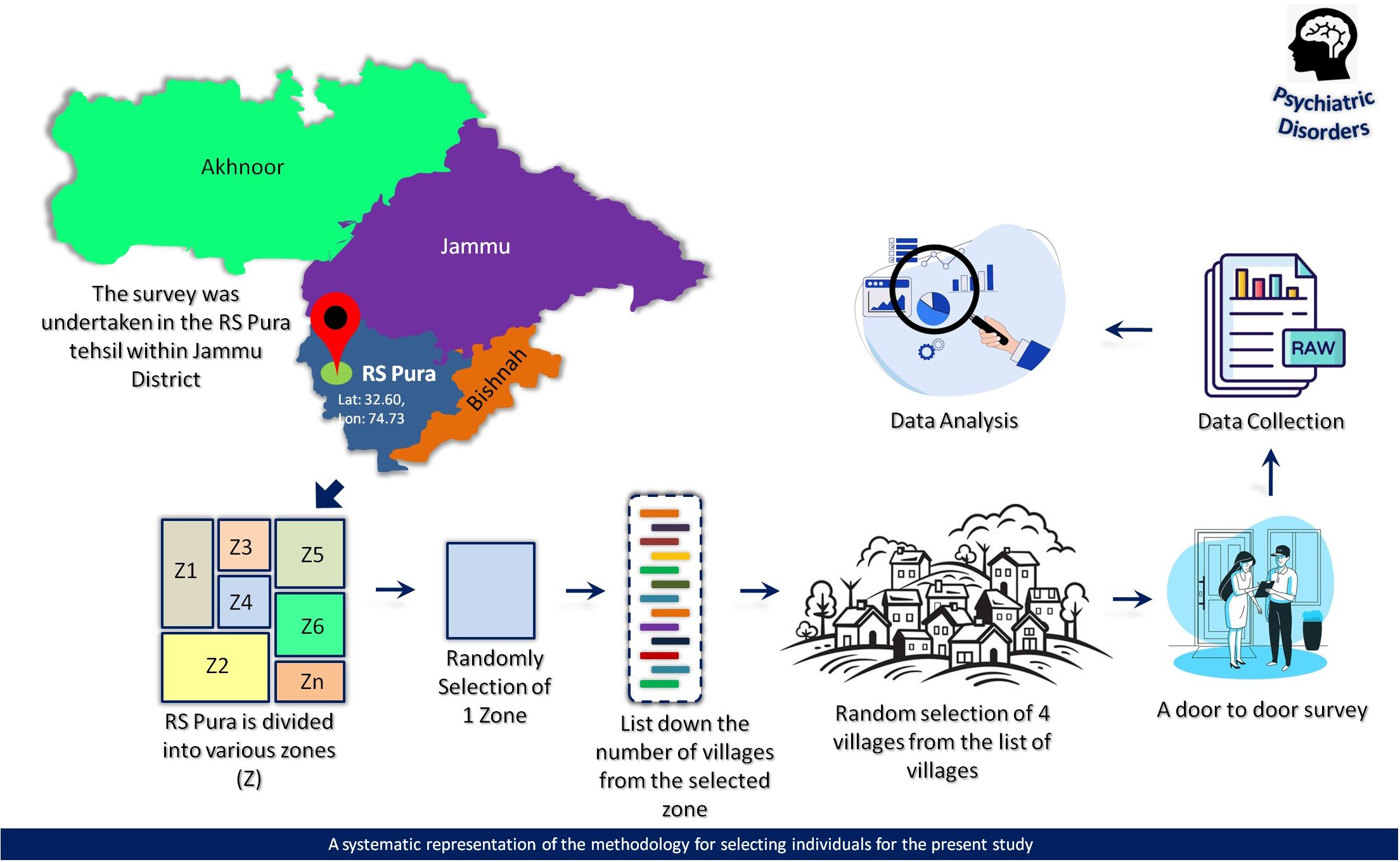
The area under study, named R.S. Pura, is located in the Jammu district at 32.6049° N, 74.7315° E, close to the international border between India and Pakistan. It covers a total area of 245 km², with 238.48 km² being rural and 6.78 km² being urban. Employing a simple random sampling method, 43 villages within the Miran Sahib block of R.S. Pura (rural area) were initially divided into 4 different zones (excluding urban areas) based on the criteria of “geographical proximity.” One zone was then randomly selected using simple random sampling. Within the chosen zone, a list of villages was compiled, and four villages—Benagarh, Ullawalchak, Ghazia, and Kotlimianfateh—were randomly selected for inclusion in the study. To ensure the representativeness of the sample, we excluded villages where the population had resided for less than 5 years and those with predominantly urban features. These features included characteristics such as significant infrastructure (e.g., large commercial centers, extensive transportation networks) and a predominance of non-agricultural occupations. These criteria were evaluated through preliminary surveys and local knowledge to ensure that only rural villages, which align with the study’s focus, were included. These criteria were evaluated through preliminary surveys and local knowledge to ensure that only rural villages, which align with the study’s focus, were included1.
After selecting the villages, we contacted opinion leaders, including the Sarpanch (the elected head of the village) and other key individuals, to brief them about the study’s purpose. They were asked to disseminate information about the upcoming study during village meetings to foster cooperation.
Before data collection began, the investigators underwent two weeks of training led by a consultant psychiatrist (M.A.). With this preparation complete, house-to-house visits commenced, during which trained investigators obtained consent from eligible participants before collecting data. All individuals in a given household who met the inclusion and exclusion criteria were invited to participate in the study. Participants were briefed about the study before data collection. Over the course of one year, relevant demographic information was recorded. All adult participants (aged 18 to 60 years) were personally interviewed by the investigators (S.B., M.A., D.K., and team) using the MINI tool (13) and a custom sociodemographic form. The demographic information included age group, socio-economic status, social caste, marital status, and educational status.
For cases where initial screening results were ambiguous or unclear, final diagnoses were determined by psychiatrists (M.A.). During the screening process, individuals who initially reported symptoms of psychiatric disorders, referred to as ‘positive respondents,’ were further assessed using the MINI to evaluate and diagnose potential conditions. Throughout the recruitment process, the inclusion and exclusion criteria were consistently applied. Inclusion criteria include years of age equal to or higher than 18, and less than or equal to 60 years, residing in the region for at least 5 years. Exclusion criteria: severe cognitive impairment or inability to communicate effectively. Additionally, it is important to note that if a household was locked during the initial door-to-door visit and remained locked on a second visit, that household was excluded from the sample. Confidentiality and privacy were ensured during data collection. A detailed flow diagram illustrating the recruitment of samples from the population is provided in Figure 1.
Statistical analysis
The data was first entered into Microsoft Excel to organize and analyze the information. We began by providing a clear summary of the participant’s demographic characteristics and the prevalence of psychiatric disorders. To achieve this, we used descriptive statistics, specifically frequency distribution, to present the discrete variables in an easily understandable format i.e., percentage (%). For the inferential statistics, we applied a logistic regression model, which allowed us to calculate the odds ratios (2 x 2 table). This helped us explore the association between socio-cultural and demographic factors and the prevalence of psychiatric disorders. We set a significance level of p < 0.05, meaning that any results with a p-value less than 0.05 were considered statistically significant. Data analysis was done in Medcalc (MedCalc Statistical Software version 19.2.6 (MedCalc Software bv, Ostend, Belgium; https://www.medcalc.org; 2020), and SPSS version 17(IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.).
Result
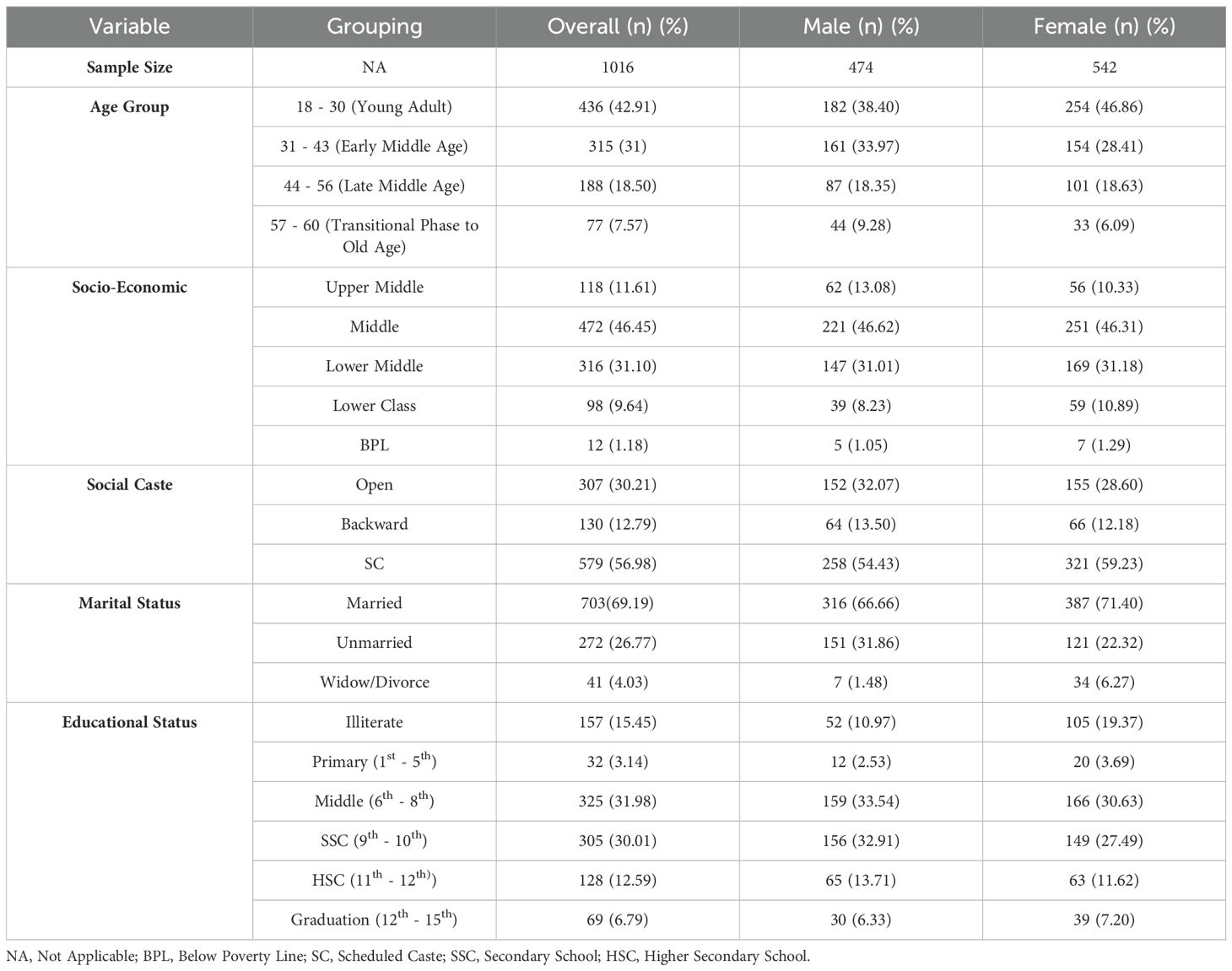
In the present study, a total of 1,016 individuals were included, with females constituting the majority (n=542, 53.35%) and males making up the rest (n=474, 46.65%). As detailed in Table 1, the age distribution shows that the largest group is young adults aged 18-30 (42.91%) (Figure 2A), with a higher proportion of females (46.86%) compared to males (38.40%). The middle-income group is the most represented socioeconomic status (46.45%) (Figure 2B), and the Scheduled Caste (SC) group constitutes the majority in terms of social caste (56.98%) (Figure 2E). It is important to note that in the Indian context, the caste system includes a range of categories with varying social and economic statuses. SC are historically marginalized and positioned at the lower end of the social hierarchy. Conversely, there are higher caste groups, such as the Brahmins and Kshatriyas, who traditionally occupy higher social and economic positions (14). The high representation of SC individuals in our sample underscores the prevalence of socioeconomically disadvantaged populations in the study area and provides insight into the broader context of caste-based disparities. Marital status analysis reveals that 69.19% of individuals are married (Figure 2C), with a slightly higher percentage among females (71.40%). Educational status indicates that a significant portion of the population has a middle-level education (31.98%) (Figure 2D), with females showing a higher frequency of illiteracy (19.37%) compared to males (10.97%).
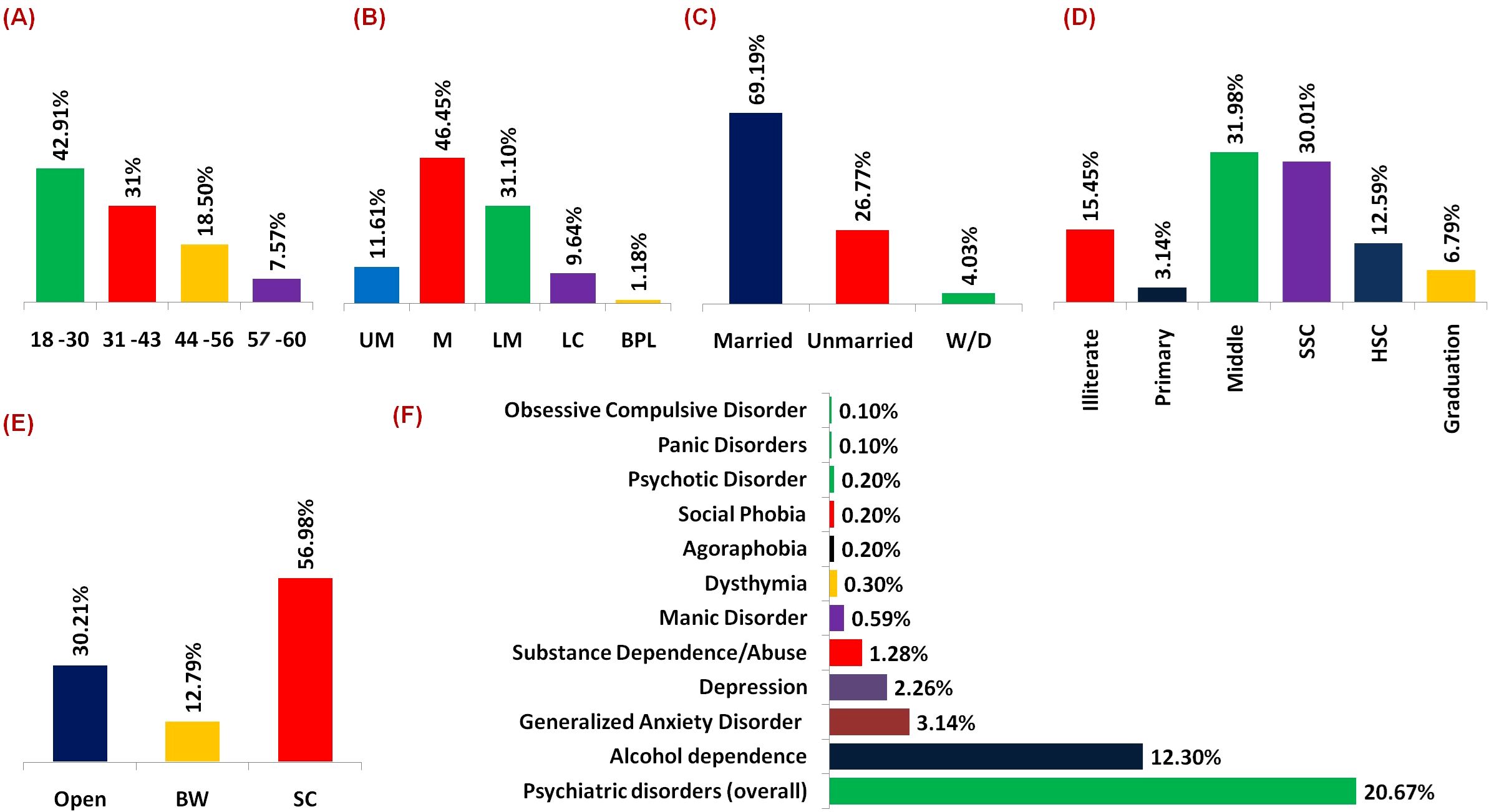
Figure 2. (A) Bar graph illustrating the distribution of individuals across various age groups, highlighting a predominant presence within the 18-30 years cohort. (B) Bar graph delineating the distribution of individuals across distinct socio-economic strata, with a notable concentration within the middle-class segment [UM, Upper Middle; M, Middle; LM, Lower Middle; LC, Lower Class; BPL, Below Poverty Line]. (C) Bar graph portraying the distribution of individuals based on marital status [Widow/Divorce]. (D) Bar graph depicting the educational attainment levels of the surveyed populace [SSC, Secondary School; HSC, Higher Secondary School]. (E) Bar graph depicts the frequency distribution of social caste. [BW, Backward; SC, Scheduled Caste] (F) Bar graphs elucidating the prevalence rates of different psychiatric disorders, notably emphasizing a heightened occurrence of alcohol dependence.
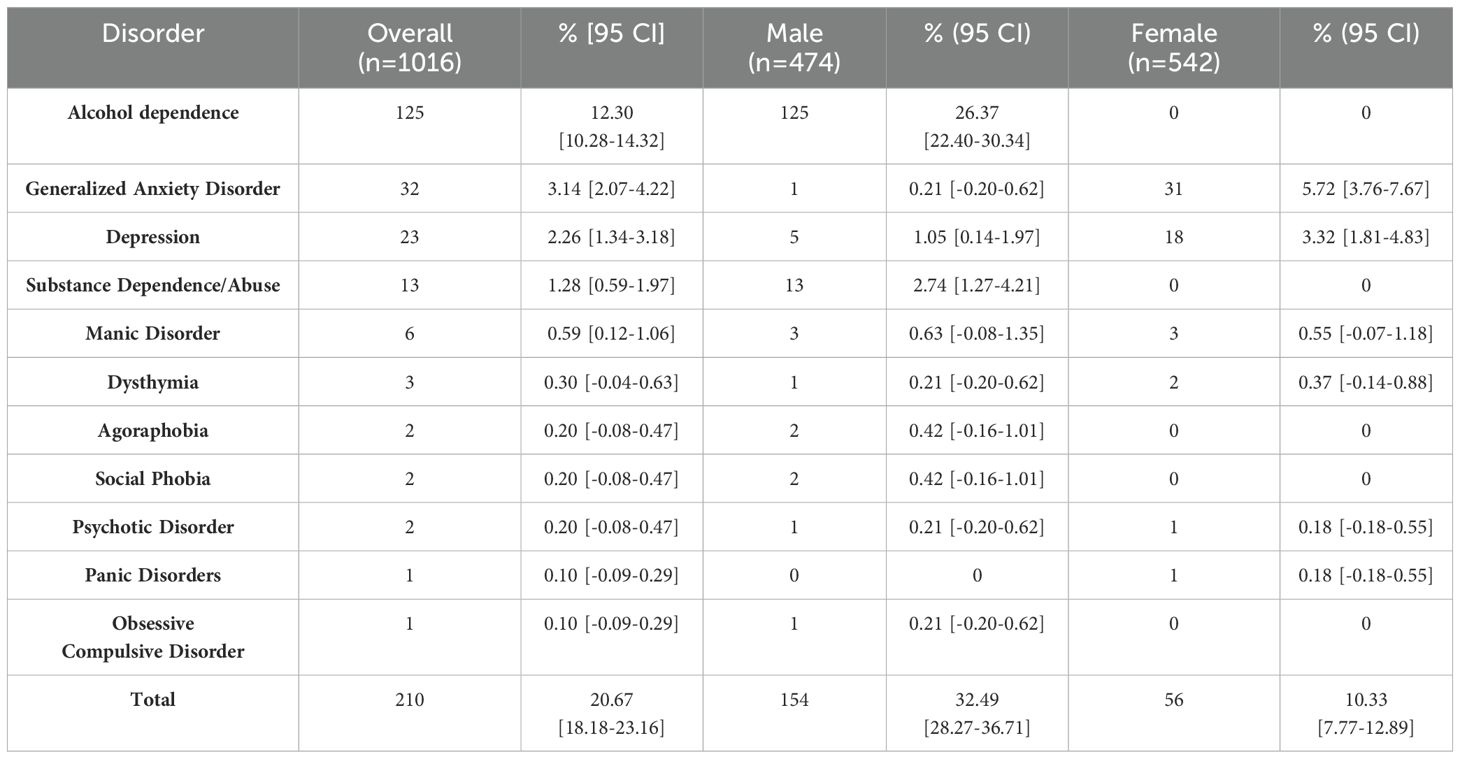
It was found that alcohol dependence emerges as the most prevalent overall, affecting 12.30% of the sample. Interestingly, there are notable gender differences in the prevalence of certain disorders (Table 2). Generalized Anxiety Disorder (GAD) and depression appear to be more prevalent among females, with rates of 5.72% and 3.32%, respectively, compared to much lower rates among males (0.21% and 1.05%) (Table 3). Conversely, Substance Dependence/Abuse shows a higher prevalence among males (2.74%) compared to females (0%). Other disorders, such as Manic Disorder, Dysthymia, Agoraphobia, Social Phobia, Psychotic Disorder, Panic Disorders, and obsessive-compulsive disorder, exhibit lower prevalence rates overall (Figure 2F), with some variations between genders (Table 2).
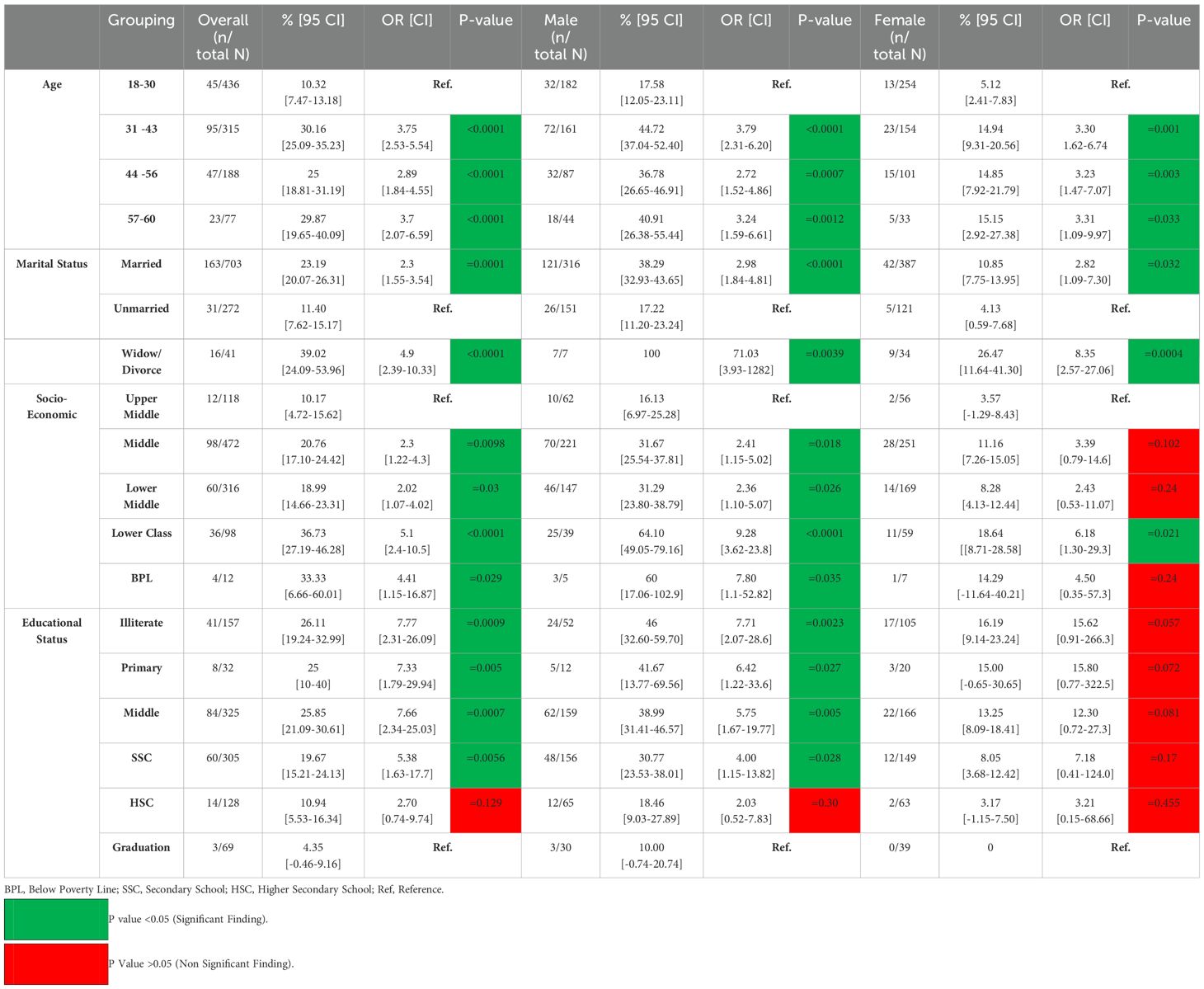
Table 3. Association Values (Odds Ratio with 95% Confidence Interval) of Demographic Variables and Overall Psychiatric Disorders.
In our analysis, we also examined the association between various socio-demographic variables and the likelihood of overall psychiatric disorders (Figure 3). Firstly, concerning age groups, we noted significant disparities in the odds of psychiatric disorders across different age brackets. For males, compared to the reference group aged 18-30, the odds of experiencing psychiatric disorder were 3.79 times higher in the age group 31-43 (OR: 3.79 [2.31-6.20]), 2.8 times higher in the age group 44-56, and 3.7 times higher in the age group 56-60 (OR: 3.7 [2.07-6.59]) (Figure 4A). Similarly, for females, the odds ratios for these age groups compared to the reference were 3.25, 3.23, and 3.31, respectively (Figure 4B), indicating a noteworthy association between age and the likelihood of psychiatric disorders (Table 3). Married individuals showed 2.3 times higher odds of experiencing psychiatric disorder compared to unmarried counterparts, while the odds of experiencing psychiatric disorder were notably higher at 4.9 times (Figure 3) among those who were widowed or divorced compared to the unmarried group (Table 3). Thirdly, socio-economic status revealed a gradient effect, with lower socio-economic such as lower class OR: 5.1 [2.4-10.5] and Below Poverty Line (BPL) OR: 4.41 [1.15-16.87] classes showed progressively higher odds ratios (Figure 3) for psychiatric disorders compared to the upper middle class (Table 3). This suggests a clear association between socio-economic status and the likelihood of psychiatric disorders. Lastly, educational status displayed a similar trend, with decreasing educational attainment associated with higher odds of experiencing psychiatric disorders compared to the reference group with graduation-level education (Figure 3). Specifically, the odds ratios ranged from 5.38 to 7.77 across different educational categories, highlighting the significance of education in shaping susceptibility to psychiatric disorders (Table 3). However, we found several non-significant associations in the female group (Figure 4B).

Figure 3. Forest plot delineating the association between various socio-demographic variables and the overall prevalence of psychiatric disorders [BPL, Below Poverty Line; SSC, Secondary School; HSC, Higher Secondary School].
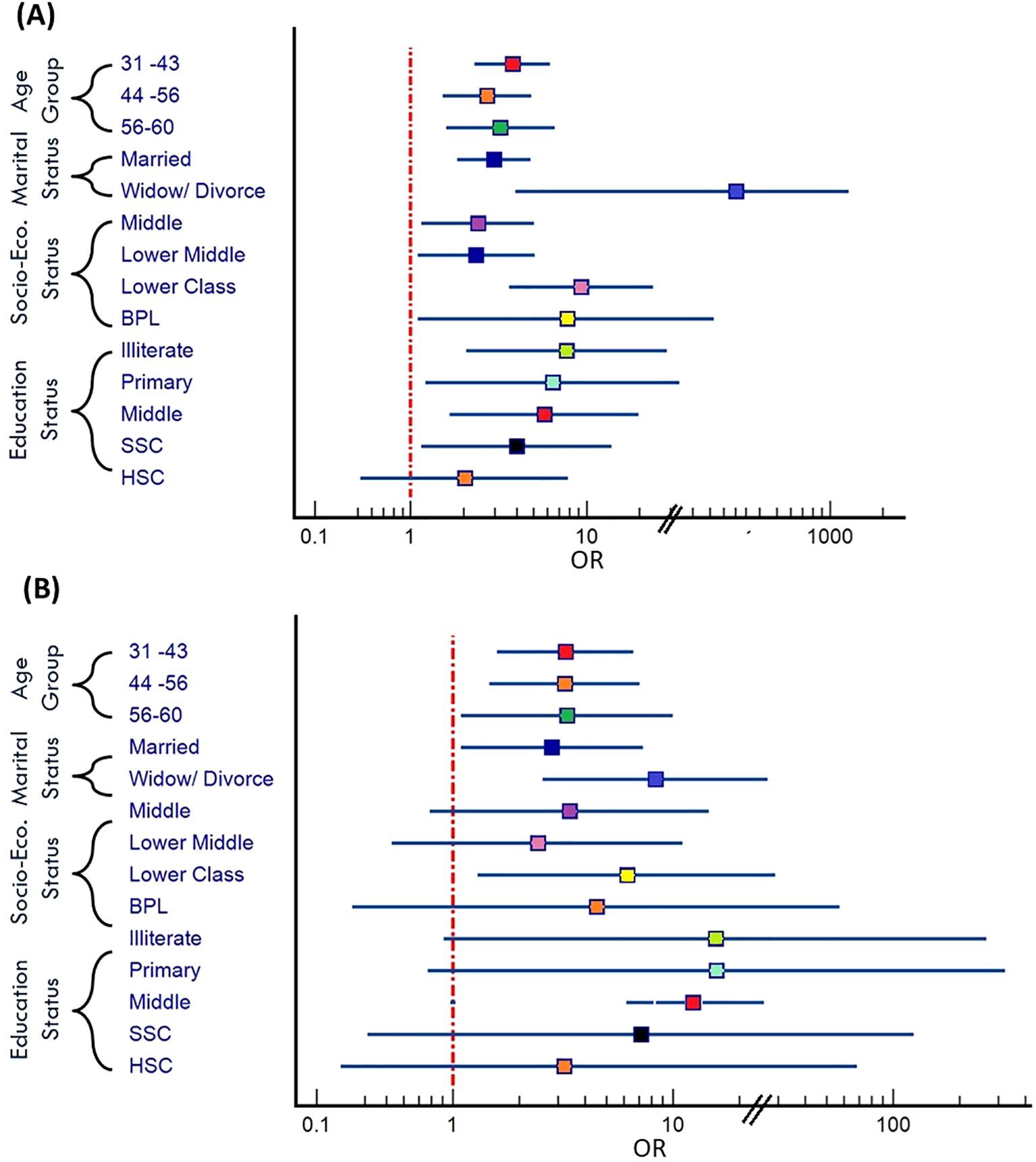
Figure 4. (A) Forest plot depicts the association between various factors and likelihood of psychiatric disorder in male (B) Forest plot depicts the association between various factors and likelihood of psychiatric disorder in female [BPL, Below Poverty Line; SSC, Secondary School; HSC, Higher Secondary School].
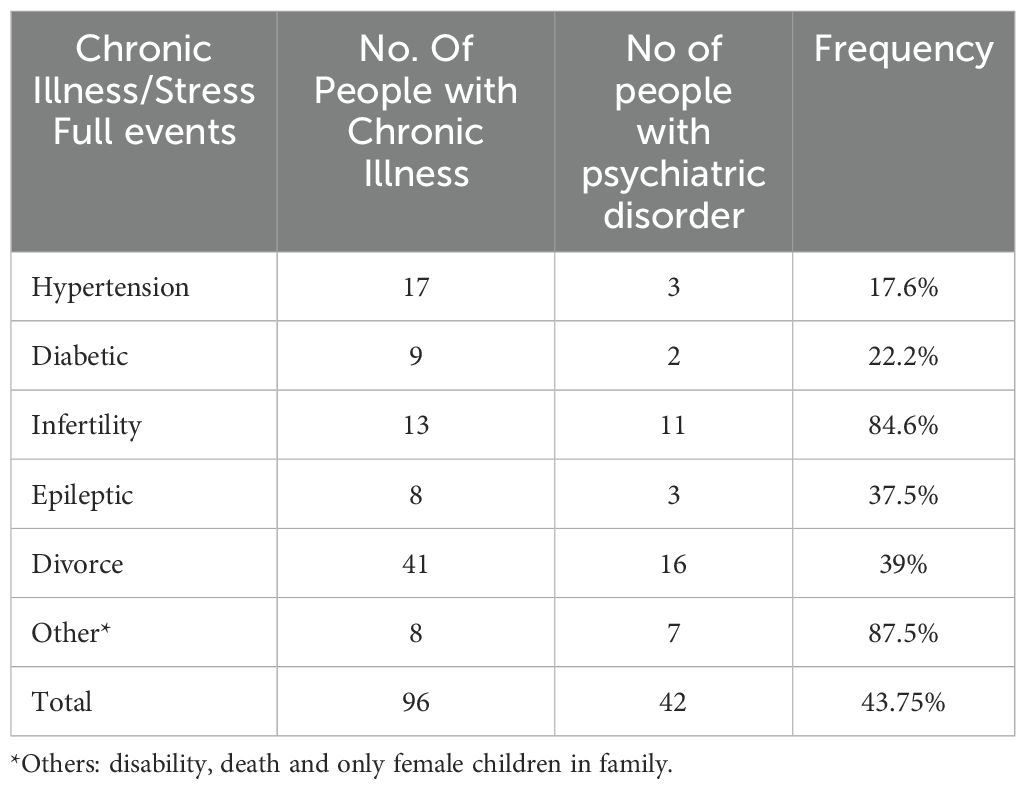
In addition to socio-demographic variables, the study identified a significant number of individuals with psychiatric disorders who also showed chronic illnesses. These include hypertension (17.6%), diabetes (22.2%), infertility (84.6%), epilepsy (37.5%), and other factors such as disability and bereavement, as well as situations specific to families, such as having only female children (87.5%) (Table 4). It is important to note that the data related to disability, death, and only female children were relatively sparse. As a result, these events were grouped together and presented under the ‘Other’ category to ensure meaningful representation and avoid potential issues with statistical reliability due to small sample sizes.
Discussion
The present study sheds light on the prevalence of psychiatric disorders among adults in rural Jammu and how socio-cultural and demographic factors might be linked to these disorders. By conducting a comprehensive survey involving 1016 individuals, the findings observed that psychiatric disorders affected a significant portion of the population, with an overall frequency of 20.67%. Notably, the prevalence rates were higher for males (32.49%), than for females (10.33%). Moreover, the survey highlights the widespread nature of alcohol dependence (Figure 2F). Furthermore, the investigation delineates varying rates of anxiety and depression across genders (Table 2).
In India, multiple studies have shown a high prevalence of psychiatric disorders. Sathyanarayana Rao and group reported a 24.40% prevalence in Karnataka, with significant issues such as depression, anxiety, and alcohol dependence (15). Similarly, Nair and group found a 33.9% prevalence of mental illness among people over 60 years old in rural Karnataka. It’s important to note that Nair et al.’s study specifically focused on this older age group, which differs from the age range in our study (16). In another study from the Kashmir region, Amin and Khan explored depression characteristics amid prolonged conflict, finding a high prevalence (55.72%), notably among 15 to 35-year-olds, with rural areas showing higher rates. Their research underscores the importance of culturally sensitive mental health initiatives to mitigate the conflict’s impact and improve overall well-being (9). A study conducted by Hussain and group found a point prevalence of mental illness in the Kashmir valley at 11.3% among the adult population, with a higher prevalence among females (12.9%) compared to males (8.4%). Depressive disorders were identified as the most common psychiatric condition (8.4%), followed by anxiety disorders (5.1%) (17). These studies not only reinforce the significance of our findings but also emphasize the urgent necessity for enhanced mental health services in rural areas. This underscores the critical importance of addressing mental health challenges in underserved communities and highlights the imperative for targeted interventions to ensure equitable access to care.
Our study focuses on the prevalence of psychiatric disorders in the RS Pura tehsil of the Jammu region, examining factors such as age, marital status, socio-economic status, and education level (Figure 3). We also identified significant stressors contributing to psychiatric disorders, including chronic illnesses like hypertension, diabetes, and epilepsy, as well as life stressors such as divorce and family-specific issues like having only female children (Table 4). Although our findings are specific to the RS Pura tehsil, similar patterns have been observed in other studies from different regions, which lends support to the relevance of these factors in rural settings (18–23). However, to avoid overgeneralization, we acknowledge that our results may not fully represent all rural areas. We suggest that further research is needed to explore whether the factors identified in RS Pura are applicable to other rural populations.
The findings from our study underscore the urgent need for enhanced mental health services in the rural area of Jammu region. There is a need to increase the availability of trained mental health professionals and to integrate mental health services into primary healthcare facilities. Community-based mental health centers, telemedicine, and mobile health clinics could significantly improve accessibility. Additionally, public education campaigns are essential to reduce stigma and encourage help-seeking behavior. Special attention should be given to supporting individuals with psychiatric disorders linked to chronic illnesses and significant life stressors. By working together with researchers, healthcare providers, policymakers, and community members we can make sure everyone has fair access to mental health care, no matter where they live.
Strength, limitation, & future perspective
This study benefits from a well-defined sampling approach, utilizing a simple random sampling in the RS Pura region to ensure representative coverage of the rural Jammu region. The use of the MINI tool for psychiatric assessments provides a reliable and standardized diagnostic process, contributing to the robustness of the findings. Additionally, the study’s large sample size of 1016 participants allows for a detailed analysis of various socio-demographic factors and their associations with psychiatric disorders.
The study faces several limitations. The geographical focus on a specific rural area may limit the generalizability of the findings to other regions or urban settings. Additionally, the cross-sectional design restricts the ability to establish causal relationships between socio-demographic factors and psychiatric disorders. We also observed several non-significant associations within the female group, which may be attributed to the small sample size and variability within educational categories. To obtain more accurate and generalizable results, larger samples and more diverse data are needed.
Future research could benefit from broader sampling that includes diverse geographic locations and urban areas to improve generalizability. Longitudinal studies are valuable for understanding the progression and tracking changes in psychiatric disorders over time. Additionally, exploring other influencing factors such as cultural practices, healthcare access, and specific regional stressors could provide more comprehensive insights into mental health in the rural Jammu region.
Conclusion
Mental health is vital to well-being, yet rural communities sometimes lack access to therapies and knowledge about psychiatric diseases. The present study sought to determine the prevalence of demographic characteristics linked with psychiatric diseases. Our investigation shows a complex link between socio-demographic factors and psychiatric problems. These findings help identify socio-economic gaps and demographic patterns in mental health outcomes, which is essential for establishing targeted interventions and policies to improve mental health.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Ethical Committee (IEC) of Government Medical College, Jammu, Jammu and Kashmir. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SB: Conceptualization, Methodology, Validation, Writing – original draft, Writing – review & editing. AS: Software, Visualization, Writing – original draft, Writing – review & editing. S: Conceptualization, Methodology, Investigation, Validation, Writing – review & editing. MY: Investigation, Software, Writing – review & editing. MA: Conceptualization, Investigation, Methodology, Resources, Supervision, Validation, Writing – review & editing. HK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – review & editing. PK: Validation, Writing – review & editing. DK: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to use this opportunity to extend their appreciation to the Government Medical College in Jammu for the assistance and facilities that they gave throughout this research. We would like to express our sincere gratitude to the individuals who willingly gave their valuable data to this investigation. Without their assistance, this research would not have been feasible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviation
WHO, World Health Organization; MINI, Mini International Neuropsychiatric Interview; MINI-S, Mini International Neuropsychiatric Interview-Screen; CI, Confidence Interval; SD, Standard Deviation; SC, Socio-Cultural; SPSS, Statistical Package for the Social Sciences; IRB, Institutional Review Board; GHQ-12, General Health Questionnaire-12; BPL, Below Poverty Line; UM, Upper Middle; M, Middle; LM, Lower Middle; LC, Lower Class; SC, Scheduled Caste.
Footnotes
- ^ [The random selection of villages was performed using the Excel function =RAND(), which generates random numbers to ensure an unbiased sampling process].
References
1. World Health Organization. Health and well-being, the global health observatory (2024). Available online at: https://www.who.int/data/gho/data/major-themes/healthand-well-being (Accessed 23 August 2024).
2. Stein DJ, Shoptaw SJ, Vigo DV, Lund C, Cuijpers P, Bantjes J, et al. Psychiatric diagnosis and treatment in the 21st century: paradigm shifts versus incremental integration. World Psychiatry. (2022) 21:393–414. doi: 10.1002/wps.20998
3. Svalastog AL, Donev D, Jahren Kristoffersen N, Gajović S. Concepts and definitions of health and health-related values in the knowledge landscapes of the digital society. Croatian Med J. (2017) 58:431–5. doi: 10.3325/cmj.2017.58.431
4. Sudershan A, Pushap AC, Younis M, Sudershan S, Bhagat S, Kumar H, et al. Neuroepidemiology study of headache in the region of Jammu of north Indian population: A cross-sectional study. Front Neurol. (2023) 13:1030940. doi: 10.3389/fneur.2022.1030940
5. Koul R, Razdan S, Motta A. Prevalence and pattern of epilepsy (Lath/Mirgi/Laran) in rural Kashmir, India. Epilepsia. (1988) 29:116–22. doi: 10.1111/j.1528-1157.1988.tb04406.x
6. Raina SK, Razdan S, Nanda R. Prevalence of neurological disorders in children less than 10 years of age in RS Pura town of Jammu and Kashmir. J Pediatr Neurosci. (2011) 6:103–5. doi: 10.4103/1817-1745.92815
7. Raina SK, Razdan S, Pandita KK. Prevalence of dementia in ethnic Dogra population of Jammu district, North India: a comparison survey. Neurol Asia. (2010) 15.
8. Maqbool M, Dugassa D, Fekadu G. Adverse drug reactions of antiepileptic drugs in the neurology department of a tertiary care hospital, Srinagar, Jammu and Kashmir, India. Arch Neurosci. (2021) 8. doi: 10.5812/ans
9. Amin S, Khan AW. Life in conflict: characteristics of depression in kashmir. Int J Health Sci. (2009) 3:213–23.
10. Banal R, Thappa J, Shah HU, Hussain A, Chowhan A, Kaur H, et al. Psychiatric morbidity in adult Kashmiri migrants living in a migrant camp at Jammu. Indian J Psychiatry. (2010) 52:154–8. doi: 10.4103/0019-5545.64597
11. Housen T, Lenglet A, Ariti C, Shah S, Shah H, Ara S, et al. Prevalence of anxiety, depression and post-traumatic stress disorder in the Kashmir Valley. BMJ Global Health. (2017) 2:e000419. doi: 10.1136/bmjgh-2017-000419
12. Pandey S, Saxena S, Joshi PC, Mahajan C. Perceived stress, anxiety and depression: Living along the border in Jammu and Kashmir. Int J Soc Psychiatry. (2023) 69:1532–40. doi: 10.1177/00207640231168032
13. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59 Suppl 20:22–57.
14. Goghari VM, Kusi M. An introduction to the basic elements of the caste system of India. Front Psychol. (2023) 14:1210577. doi: 10.3389/fpsyg.2023.1210577
15. Sathyanarayana Rao TS, Darshan MS, Tandon A, Raman R, Karthik KN, Saraswathi N, et al. Suttur study: An epidemiological study of psychiatric disorders in south Indian rural population. Indian J Psychiatry. (2014) 56:238–45. doi: 10.4103/0019-5545.140618
16. Nair SS, Raghunath P, Nair SS. Prevalence of psychiatric disorders among the rural geriatric population: A pilot study in karnataka, India. Cent Asian J Global Health. (2015) 4:138. doi: 10.5195/cajgh.2015.138
17. Hussain A, Dar MA, Shah MS, Roub F. An epidemiological study of psychiatric disorders in Kashmir. J Family Med Primary Care. (2024) 13:845–50. doi: 10.4103/jfmpc.jfmpc_593_21
18. Turner RJ, Lloyd DA, Taylor J. Physical disability and mental health: An epidemiology of psychiatric and substance disorders. Rehabil Psychol. (2006) 51:214. doi: 10.1037/0090-5550.51.3.214
19. Maia AC, Braga AA, Brouwers A, Nardi AE, Oliveira e Silva AC. Prevalence of psychiatric disorders in patients with diabetes types 1 and 2. Compr Psychiatry. (2012) 53:1169–73. doi: 10.1016/j.comppsych.2012.03.011
20. Hesdorffer DC, Ishihara L, MyNepalli L, Webb DJ, Weil J, Hauser WA. Epilepsy, suicidality, and psychiatric disorders: a bidirectional association. Ann Neurol. (2012) 72:184–91. doi: 10.1002/ana.23601
21. Stein DJ, Aguilar-Gaxiola S, Alonso J, Bruffaerts R, de Jonge P, Liu Z, et al. Associations between mental disorders and subsequent onset of hypertension. Gen Hosp Psychiatry. (2014) 36:142–9. doi: 10.1016/j.genhosppsych.2013.11.002
22. Gupta C, Arora M, Gupta RK, Akhtar N, Langer B, Kumari R, et al. Prevalence and correlates of depression in a rural adult population in Northwest India. J Family Med primary Care. (2020) 9:151–5. doi: 10.4103/jfmpc.jfmpc_656_19
Keywords: psychiatric disorders, rural areas, Jammu, socio-demographic factors, mental health disparities
Citation: Bailam S, Sudershan A, Sheetal, Younis M, Arora M, Kumar H, Kumar P and Kumar D (2024) Prevalence of psychiatric disorders among the adult population in a rural community of Jammu, India: a cross-sectional study. Front. Psychiatry 15:1433948. doi: 10.3389/fpsyt.2024.1433948
Received: 16 May 2024; Accepted: 28 August 2024;
Published: 25 October 2024.
Edited by:
Elisa Harumi Kozasa, Hospital Israelita Albert Einstein, BrazilReviewed by:
Danilo Forghieri Santaella, University of São Paulo, BrazilPhoutdavone Phimphasone-Brady, University of Colorado Anschutz Medical Campus, United States
Mateus Torres-Cruz, Albert Einstein Israelite Hospital, Brazil
Copyright © 2024 Bailam, Sudershan, Sheetal, Younis, Arora, Kumar, Kumar and Kumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Parvinder Kumar, cGFydmluZGVya2IyMDAzQGdtYWlsLmNvbQ==; Dinesh Kumar, ZGluZXNoZ21jamFtQHJlZGlmZm1haWwuY29t
 Sandeepa Bailam
Sandeepa Bailam Amrit Sudershan
Amrit Sudershan Sheetal5,6
Sheetal5,6 Mohd Younis
Mohd Younis Hardeep Kumar
Hardeep Kumar