- Changde Hospital, Xiangya School of Medicine, Central South University (The First People’s Hospital of Changde City), Changde, Hunan, China
Background: Studies on post-stroke anxiety (PSA) following the lifting of COVID-19 restriction measures are currently lacking. We investigated the factors affecting PSA after full release of COVID-19 epidemic in China.
Methods: Patients with stroke admitted to the First People’s Hospital of Changde City from March 2023 to September 2023 participated in a questionnaire survey comprising a general demographic questionnaire, the Generalized Anxiety Scale-7. Additionally, data on the National Institutes of Health Stroke Scale, modified Rankin Scale, C-reactive protein (CRP), thyroid-stimulating hormone (TSH), homocysteine, TOAST classification, and the stroke site were collected, and the correlations between these indices and the mental health conditions of the patients were evaluated.
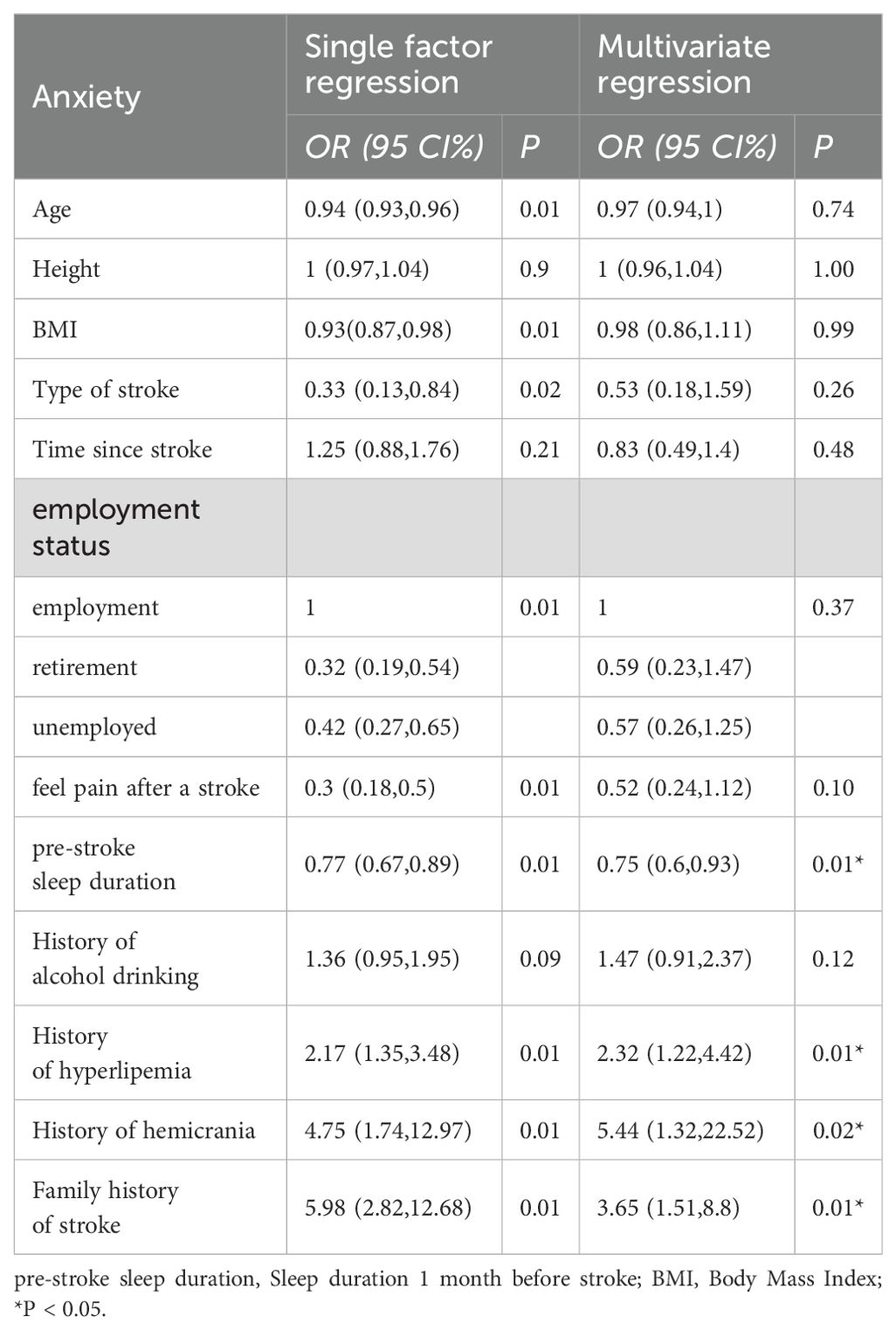
Results: Among 947 patients, the incidence of PSA was 14.57%.PSA was not linked to prior COVID-19 infection. This study found that Sleep duration (P=0.01), hyperlipidemia (P=0.01), migraine (P=0.02), and family history of stroke (P=0.01) were associated with PSA.
Conclusions: Our study found that the prevalence of PSA was 14.57%. In addition, sleep duration, hyperlipidemia, migraine and family history of stroke were independent risk factors for PSA following the lifting of COVID-19 restrictions.
1 Introduction
Novel coronavirus pneumonia, also known as coronavirus disease 2019 (COVID-19), is a widespread infectious disease posing a serious global threat to human health. As of March 2022, more than 445 million infections and 6 million fatalities were reported worldwide (1). After the initial outbreak in December 2019, China has diligently adhered to strict defense measures and a dynamic zero-COVID policy. Considering the gradual decrease in pathogenicity in Considering the decrease in pathogenicity towards the end of 2022,The Joint Prevention and Control Mechanism Comprehensive Team of The State Council issued the “New Ten Measures” on December 7, 2022 (2). Subsequently, the number of positive cases decreased after peaking on December 22,2022 (6.94 million cases) (3).
Stroke is the second highest cause of mortality globally and among the primary contributors to disability (4). Post-stroke anxiety (PSA) is a frequent and debilitating consequence experienced by a significant proportion of stroke survivors. It is the result of motor dysfunction and severe decline in quality of life, which can lead to a continuous and stable decline in quality of life. However, compared with other post-stroke psychological disorders, PSA is currently relatively neglected as a serious psychological and physical problem (5). PSA frequently presents as an exaggerated emphasis on individual outcomes, encompassing stroke recurrence, resumption of occupational activities, falls prevention, and the preservation of autonomy (6). Studies have demonstrated that COVID-19 infection or suspected infection can trigger intense emotional and behavioral responses, including fear, boredom, loneliness, anxiety, insomnia, or anger (7). The prevalence and burden of depression and anxiety have increased significantly during the COVID-19 pandemic (8). However, studies conducted during the COVID-19 pandemic period have indicated a comparable prevalence of post-stroke anxiety and depression to that observed in non-pandemic periods (9).
However, there are currently no studies on PSA after the full release of COVID-19. Therefore, further studies are needed to investigate whether COVID-19 infection is associated with PSA, and the related risk factors of PSA after full release of COVID-19 epidemic.
In order to clarify the above issues, the cross-sectional study investigated the factors associated with the development and persistence of anxiety following stroke after COVID-19 opening, which will provide a basis for early screening and intervention of PSA.
2 Methods
2.1 Study design and patient selection
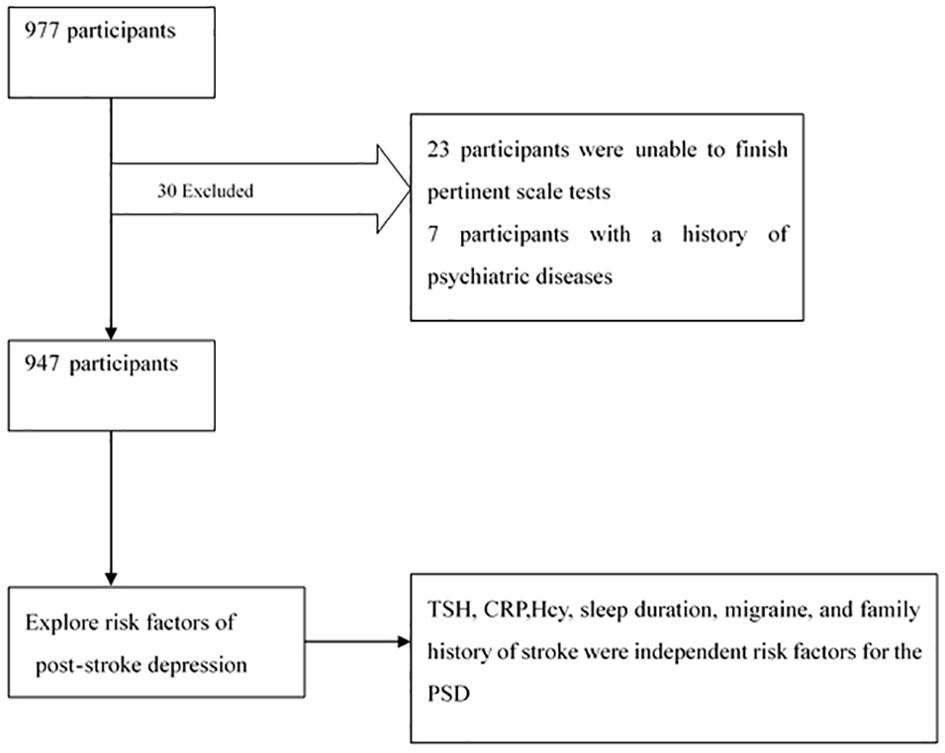
This study adopted a cross-sectional research design. We calculated the sample size by sample size = (Z value * standard deviation/error) ^2.All patients with stroke (including cerebral hemorrhage and infarction) admitted to the neurology department of the First People’s Hospital of Changde City from March 2023 to September 2023 were included in this study (Figure 1).
The patient inclusion criteria were as follows:
1. cerebral infarction or hemorrhage diagnosed according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) and
2. site of hemorrhage or infarction identified by computed tomography (CT) or magnetic resonance imaging (MRI).
The patient exclusion criteria were as follows:
1. medical history of a psychiatric disorder,
2. unable to complete the questionnaire survey, or
3. opted out of the study.
Each patient underwent the below evaluations.
1. Laboratory examination: Standard blood tests, including the measurement of serum thyroid-stimulating hormone (TSH), homocysteine (Hcy), and C-reactive protein (CRP) levels, were conducted during admission.
2. Stroke-related assessments: The assessments included the patients’ scores on the National Institutes of Health Stroke Scale (NIHSS) and modified Rankin Scale (mRS), estimation of the bleeding volume and stroke location, and the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) subtype staging using various imaging and clinical data.
3. Web-based questionnaire survey: We administered face-to-face questionnaires to the patients. The web-based questionnaire survey on the Questionnaire Star platform collected information such as sex, age, height, weight, employment status, marital status, education level, presence of post-stroke pain, smoking and alcohol habits, neocoronary infections, past medical history, and family history of psychiatric disorders and stroke, as well as included assessments using the Generalized Anxiety Scale-7 (GAD-7).
2.1.1 Standard blood tests
2.1.1.1 TSH estimation
Fasting blood samples were collected at 6 a.m. on the day after admission. Samples were collected into standardized tubes containing an anticoagulant (EDTA), and stored at −80°C. The TSH levels were measured using a standardized radioimmunoassay kit. The normal range of TSH was 0.35–4.94 μIU/mL.
2.1.1.2 Hcy estimation
Serum Hcy levels were measured via an enzyme cycling method with a normal range of 0–15 μmol/L.
2.1.1.3 CRP estimation
Serum CRP levels were quantitatively determined via immunoturbidimetry within a detection range of 0–10 mg/L.
2.1.2 Stroke-related assessments
2.1.2.1 NIHSS
The NIHSS score is used to assess stroke severity (10). The total NIHSS score ranges from 0 to 42, wherein 0 indicates normal function and higher scores imply increasing impairment.
2.1.2.2 mRS
The mRS is used to examine residual disability in patients with stroke. The mRS is scored on a 5-point scale, with 0 representing no symptoms and 5 suggesting severe disability. The validity as well as interobserver and intraobserver reliability of the mRS in scoring the residual disability of patients with stroke in terms of the amount of assistance required to achieve various degrees of autonomy have been well documented (10).
2.1.2.3 TOAST classification system
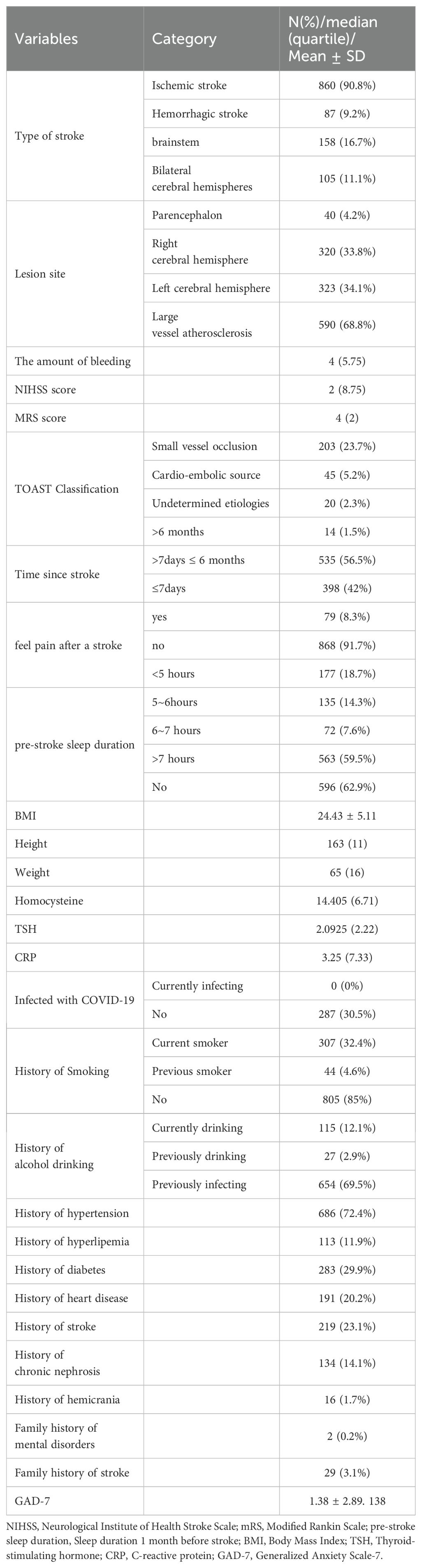
The TOAST classification system includes five categories: 1) large-artery atherosclerosis, 2) cardioembolism, 3) small-artery occlusion (lacune), 4) stroke of other determined etiology, and 5) stroke of undetermined etiology (Table 1). Diagnoses are based on clinical features and data collected via tests such as brain imaging (CT/MRI), cardiac imaging (including echocardiography), duplex sonography of the extracranial arteries, arteriography, and laboratory assessments for a prothrombotic state (11).
2.1.3 Questionnaire
2.1.2.1 GAD-7
The Chinese version of the GAD-7 scale was employed to evaluate the anxiety levels of the patients. The GAD-7 is a 7-item scale that determines the severity of anxiety symptoms on a scale of 0 (none at all) to 3 (almost every day). The total GAD-7 score ranges from 0–21, with higher scores implying severe anxiety. In line with prior studies, a total score of ≥5 was suggestive of a state of anxiety. Finally, the degree of anxiety based on the total score was categorized as follows: mild (5–9 points), moderate (10–14 points), and severe anxiety (≥15 points) (12–14).
2.2 Statistical analysis
All data analyses were performed using IBM SPSS software package version 20.0. Continuous numerical variables with normal distribution were presented as mean ± standard deviation, whereas quantitative and rank data with non-normal distribution were expressed as median (interquartile spacing). An independent sample t-test was utilized to compare normally distributed data, while the rank sum test was employed to compare non-normally distributed quantitative data. Count data were reported as quantity (%). The chi-square test was used to compare differences, and binary logistic regression was applied to explore the independent risk factors for anxiety. A P-value of <0.05 was considered statistically significant.
3 Results
3.1 Sociodemographic and clinical characteristics
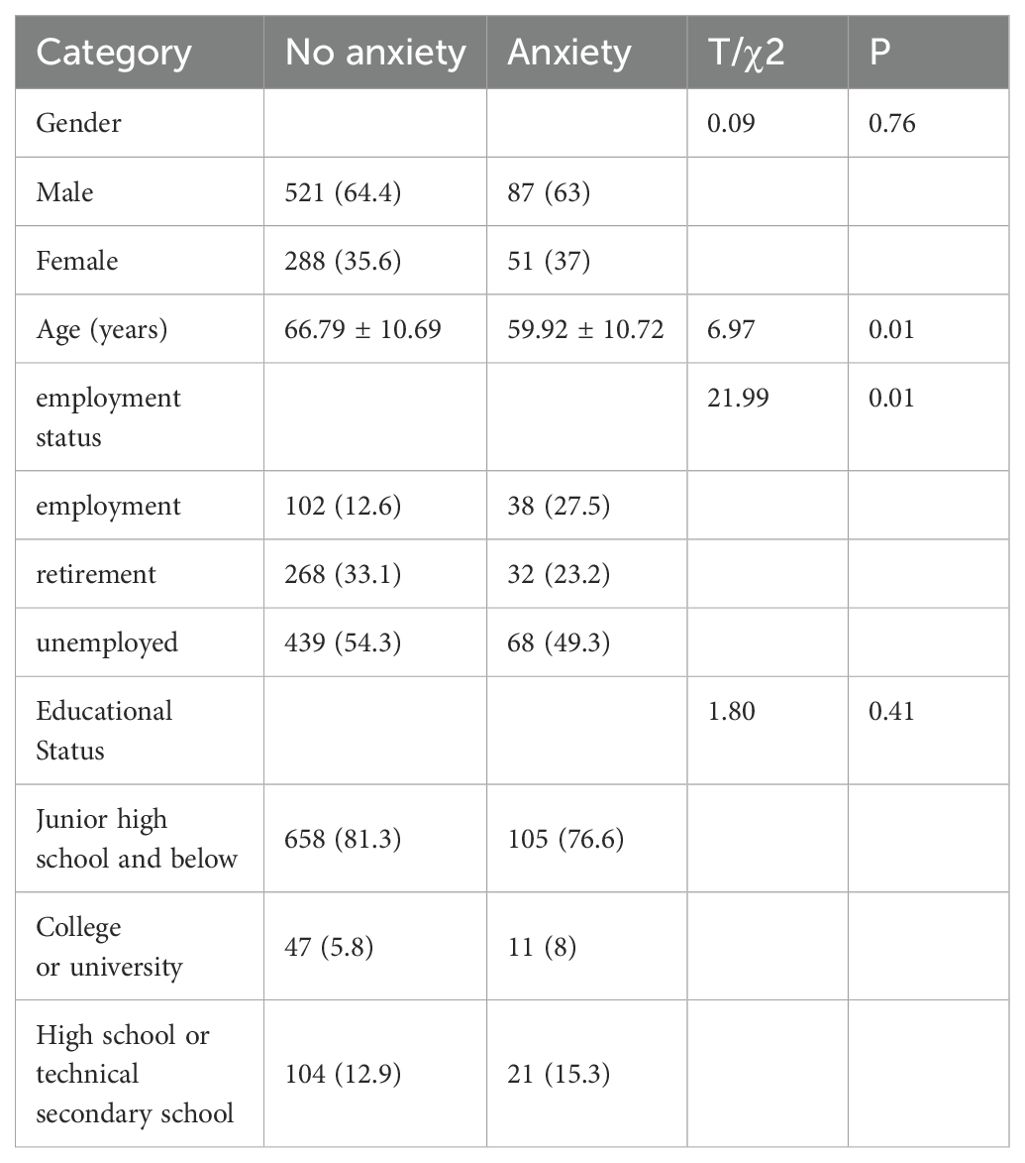
A total of 947 participants, including men and women, were enrolled for six months during the study. The participants’ demographic, clinical, GAD-7 scores were in Tables 1, 2. Our study found that the prevalence of anxiety was 14.57%, the mean GAD-7 scores was 1.38 ± 2.89. 138. Among them, 112 cases (11.83%) had mild anxiety, 20 cases (2.11%) had moderate anxiety, and 6 cases (0.63%) had severe anxiety.
3.2 Factors related to patient anxiety
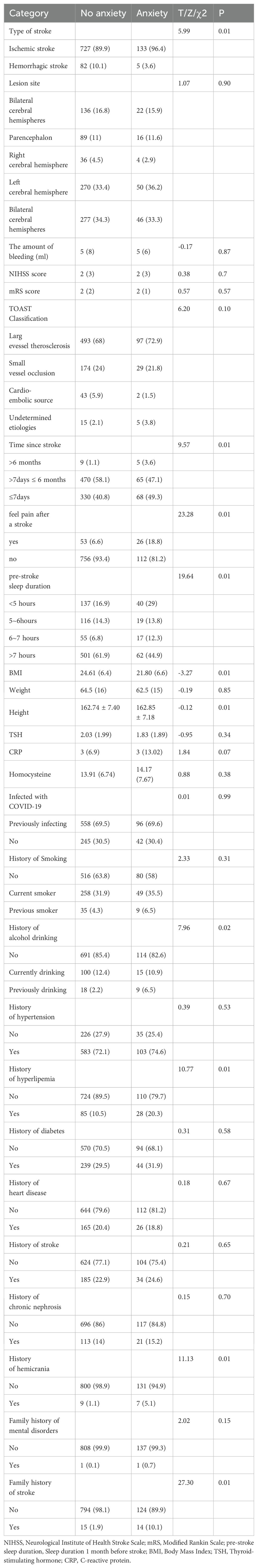
In order to explore the related factors of anxiety in stroke patients, patients were divided into groups according to the score of GAD-7, GAD-7 < 5 points were no anxiety and GAD-7 ≥ 5 points were anxiety group. The different parameters of anxiety group in no anxiety group are shown in Tables 3, 4. As shown in Tables 3, 4, compared with the non-anxiety group, the anxiety group was younger (59.92 ± 10.72, P=0.01), taller (162.85 ± 7.18, P=0.01), higher BMI (21.80(6.6), P=0.01), and higher proportion of cerebral infarction (P=0.01). More patients with stroke duration ≤7 days (P=0.01), more patients with employment (P=0.01), more patients with post-stroke pain (P=0.01), more patients with sleep duration < 5 hours (P=0.01), and more patients with sleep duration > 7 hours (P=0.01) than those without anxiety. The proportion of previous alcohol use was higher in the anxiety group (P=0.02), whereas the proportion of non-alcohol use and current alcohol use was higher in the non-anxiety group. The proportion of family history of hyperlipidemia, migraine and stroke was higher in the anxiety group (P=0.01).
Further univariate and multivariate logistic regression analysis showed that Sleep duration before stroke, hyperlipidemia, migraine, family history of stroke, and anxiety were independent risk factors for the occurrence of stroke (Table 5).
4 Discussion
A total of 947 patients were enrolled in this cross-sectional study to explore the influencing factors of PSA after full release of COVID-19 epidemic. The present study revealed the prevalence of post-stroke anxiety was 14.57%. Sleep duration, hyperlipidemia, migraine and family history of stroke were independent risk factors for PSA.
Several studies have shown that during the COVID-19 pandemic, the prevalence rate of PSA is as high as 30.1% -32% (15, 16), which is significantly higher than our research results. The reason for the significant difference in results may be due to differences in research subjects, stroke onset time, and diagnostic tools used. The more important reason is that our investigation was conducted in the post pandemic era. The public was not so panicked about COVID-19 at this time.
This study suggests that pre-stroke sleep duration is associated with PSA, which is consistent with previous findings (17, 18), Improving sleep had a significant effect on anxiety (19). In sufficient sleep duration can impede the functioning of the prefrontal cortex, anterior cingulate cortex, amygdala, and striatum, thereby impacting emotion regulation. Additionally, it can disrupt the brain’s reward system through elevated levels of tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and CRP, increased cortisol levels, hypothalamic-pituitary-adrenal axis imbalance, and exacerbation of inflammatory response. All these alterations are secondary to sleep insufficiency and contribute to heightened anxiety levels (20). Another mechanism involves sleep deprivation-induced reduction in the availability of dopamine D2/D3 receptors in the striatum, as dopamine, a monoamine neurotransmitter, plays a pivotal role in modulating the reward system and facilitating pleasurable experiences (21).Therefore, we need to pay attention to the sleep condition of stroke patients and intervene in time to reduce the occurrence of PSA.
Next, the current investigation revealed a significant association between hyperlipidemia and post-stroke anxiety, which is consistent with the findings of prior research studies (22, 23). Some studies have identified a positive correlation between anxiety and elevated triglyceride levels (24). Another study demonstrated the effectiveness of interventions targeting triglyceride levels in alleviating symptoms of anxiety (25). A recently published experimental animal study also revealed that an 8-week high-fat diet effectively induced metabolic disorders, including obesity and hyperlipidemia, leading to anxiety-like behavior in mice (26). The aforementioned studies suggest that dyslipidemia may contribute to anxiety, possibly due to the promotion of brain-derived neurotrophic factor (BDNF) production in salivary glands by hypertriglyceridemia, thereby increasing plasma BDNF content. Salivary BDNF influences the hippocampus and enhances anxiety-like behavior (27). Although a Mendelian randomization analysis conducted in 2023 found no causal relationship between lipids and anxiety (28), lipids are likely predictors of post-stroke depression PSA, and lipid-lowering therapy may improve PSA outcomes.
This study also observed an association between migraine history and PSA, which is consistent with the results of previous studies (29). Due to the impact on daily life, work, and interpersonal relationships, individuals with migraines often experience negative emotions such as anxiety and depression (30).In addition, depression and migraine share many pathological mechanisms, including: central nervous system morphology and dysfunction, neurotransmitter and receptor systems, hormonal regulation, neuroinflammation, environmental factors, genetic predisposition, personality and temperament (31).Therefore, we need to pay attention to stroke patients with a history of migraine, who may be more likely to develop PSD.
Lastly, our study has revealed that a family history of stroke is associated with anxiety, which may be attributed to the high incidence, mortality and recurrence rate of stroke. These factors impose a significant burden on caregivers of stroke patients, leading to increased rates of anxiety and depression among them (32), Consequently, individuals with a family history of stroke are more likely to face greater economic and life pressures, thereby increasing their susceptibility to anxiety.
4.1 Limitations
This study has a few limitations that should be considered. First, establishing a causal relationship between pertinent factors and PSA was challenging, owing to the cross-sectional nature of our study. Second, the long-term influence of COVID-19 infection on PSA must be evaluated using a longitudinal cohort investigation. Third, the incidence of cerebral hemorrhage was limited in our study sample. Finally, this study only utilized scale scores as the diagnostic criteria for PSA, potentially leading to some bias. Therefore, further investigation is warranted to examine the correlation between PSA and COVID-19, identify predictors for PSD, and explore the related pathogenic factors.
5 Conclusions
Our study found that the prevalence of PSA was 14.57% and sleep duration, hyperlipidemia, migraine and family history of stroke were independent risk factors for PSA following the lifting of COVID-19 restrictions. These conclusions have guiding significance for early detection and diagnosis of post-stroke anxiety in our clinic. Further studies are needed to determine the causal relationship between these risk factors and PSA, so that some preventive measures can be taken against PSA.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the First People’s Hospital of Changde city. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SL: Writing – original draft. YH: Data curation, Writing – review & editing. JW: Project administration, Supervision, Writing – review & editing. XZ: Conceptualization, Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Scientific Research Project of Hunan Provincial Health Commission (w20242014), Changde Hospital, Xiangya School of Medicine, Central South University (The first people’s hospital of Changde city) (2022ZZ11), and The science and technology innovation program of Changde City (2022.51.1, 2020SK005).
Acknowledgments
The authors wish to thank all participants for their contributions to the study. We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Allan M, Lièvre M, Laurenson-Schafer H, de Barros S, Jinnai Y, Andrews S, et al. The World Health Organization COVID-19 surveillance database. Int J Equity Health. (2022) 21:167. doi: 10.1186/s12939-022-01767-5
2. Huang X, Wu A. Recommendations for the management of COVID-19 infection, home treatment, and return to work of medical staff after the “New Ten” measures. Chin J Infection Control. (2022) 21:1157–60.
3. Epidemic situation of 2019 novel coronavirus infection in China. Chin Center Dis Control Prev. (2023).
4. Campbell BCV, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Primers. (2019) 5:70. doi: 10.1038/s41572-019-0118-8
5. Zhou J, Fangma Y, Chen Z, Zheng Y. Post-stroke neuropsychiatric complications: types, pathogenesis, and therapeutic intervention. Aging Dis. (2023) 14:2127–52. doi: 10.14336/AD.2023.0310-2
6. Wang J, Zhao D, Lin M, Huang X, Shang X. Post-stroke anxiety analysis via machine learning methods. Front Aging Neurosci. (2021) 13:657937. doi: 10.3389/fnagi.2021.657937
7. Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci. (2020) 74:281–2. doi: 10.1111/pcn.12988
8. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
9. Elias S, Benevides ML, Martins ALP, Martins GL, Marcos ABSW, Nunes JC. Factors associated with post-stroke depression in the acute phase of ischemic stroke: A cross-sectional study. Clin Neurol Neurosurg. (2022) 223:107505. doi: 10.1016/j.clineuro.2022.107505
10. Siniscalchi A. Use of stroke scales in clinical practice: Current concepts. Turk J Emerg Med. (2022) 22:119–24. doi: 10.4103/2452-2473.348440
11. Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. (1993) 24:35–41. doi: 10.1161/01.str.24.1.35
12. Lin L-Y, Wang J, Ou-Yang X-Y, Miao Q, Chen R, Liang F-X, et al. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. (2021) 77:348–54. doi: 10.1016/j.sleep.2020.05.018
13. Seo J-G, Park S-P. Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain. (2015) 16:97. doi: 10.1186/s10194-015-0583-8
14. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
15. Ahmed ZM, Khalil MF, Kohail AM, Eldesouky IF, Elkady A, Shuaib A. The prevalence and predictors of post-stroke depression and anxiety during COVID-19 pandemic. J Stroke Cerebrovasc Dis. (2020) 29:105315. doi: 10.1016/j.jstrokecerebrovasdis.2020.105315
16. Yao M, Li H, Luo Y, Li L, Yu J. High prevalence of post-stroke anxiety in elderly patients following COVID-19 outbreak. Front Psychiatry. (2021) 12:699869. doi: 10.3389/fpsyt.2021.699869
17. Almhdawi KA, Alazrai A, Kanaan S, Shyyab AA, Oteir AO, Mansour ZM, et al. Post-stroke depression, anxiety, and stress symptoms and their associated factors: A cross-sectional study. Neuropsychol Rehabil. (2021) 31:1091–104. doi: 10.1080/09602011.2020.1760893
18. Liu F, Yang Y, Wang S, Zhang X-L, Wang A-X, Liao X-L, et al. Impact of sleep duration on depression and anxiety after acute ischemic stroke. Front Neurol. (2021) 12:630638. doi: 10.3389/fneur.2021.630638
19. Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med Rev. (2021) 60:101556. doi: 10.1016/j.smrv.2021.101556
20. Blake MJ, Trinder JA, Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: Implications for behavioral sleep interventions. Clin Psychol Rev. (2018) 63:25–40. doi: 10.1016/j.cpr.2018.05.006
21. Volkow ND, Tomasi D, Wang G-J, Telang F, Fowler JS, Logan J, et al. Evidence that sleep deprivation downregulates dopamine D2R in ventral striatum in the human brain. J Neurosci. (2012) 32:6711–7. doi: 10.1523/JNEUROSCI.0045-12.2012
22. Chang WH, Chen WT, Lee IH, Chen PS, Yang YK, Chen KC. Coexisting anxiety disorders alter associations with physical disorders in the elderly: A Taiwan cross-sectional nationwide study. Psychiatry Clin Neurosci. (2016) 70:211–7. doi: 10.1111/pcn.12381
23. Ho C-H, Hsieh K-Y, Liang F-W, Li C-J, Wang J-J, Chio C-C, et al. Pre-existing hyperlipidaemia increased the risk of new-onset anxiety disorders after traumatic brain injury: a 14-year population-based study. BMJ Open. (2014) 4:e005269. doi: 10.1136/bmjopen-2014-005269
24. Hildrum B, Mykletun A, Midthjell K, Ismail K, Dahl AA. No association of depression and anxiety with the metabolic syndrome: the Norwegian HUNT study. Acta Psychiatr Scand. (2009) 120:14–22. doi: 10.1111/j.1600-0447.2008.01315.x
25. Yin MXC, Du LB, Zou XN, Fung YL, Sun YY, Chan CHY, et al. Can psychosocial intervention suppress testosterone and triglycerides among women with polycystic ovary syndrome? A feasibility trial. Front Psychol. (2021) 12:690539. doi: 10.3389/fpsyg.2021.690539
26. Li Y, Cheng Y, Zhou Y, Du H, Zhang C, Zhao Z, et al. High fat diet-induced obesity leads to depressive and anxiety-like behaviors in mice via AMPK/mTOR-mediated autophagy. Exp Neurol. (2022) 348:113949. doi: 10.1016/j.expneurol.2021.113949
27. Kikuchi T, Sakaguchi W, Saruta J, Yamamoto Y, To M, Kurimoto Y, et al. Hypertriglyceridemia-induced brain-derived neurotrophic factor in rat submandibular glands. J Oral Biosci. (2020) 62:327–35. doi: 10.1016/j.job.2020.08.003
28. Li B, Qu Y, Fan Z, Gong X, Xu H, Wu L, et al. Causal relationships between blood lipids and major psychiatric disorders: Univariable and multivariable mendelian randomization analysis. BMC Med Genomics. (2023) 16:250. doi: 10.1186/s12920-023-01692-8
29. Chu H-T, Liang C-S, Lee J-T, Yeh T-C, Lee M-S, Sung Y-F, et al. Associations between depression/anxiety and headache frequency in migraineurs: A cross-sectional study. Headache. (2018) 58:407–15. doi: 10.1111/head.13215
30. Battista S, Lazzaretti A, Coppola I, Falsiroli Maistrello L, Rania N, Testa M. Living with migraine: A meta-synthesis of qualitative studies. Front Psychol. (2023) 14:1129926. doi: 10.3389/fpsyg.2023.1129926
31. Wachowska K, Bliźniewska-Kowalska K, Sławek J, Adamczyk-Sowa M, Szulc A, Maes M, et al. Common pathomechanism of migraine and depression. Psychiatr Pol. (2023) 57:405–19. doi: 10.12740/PP/OnlineFirst/143982
Keywords: COVID-19, stroke, anxiety, hyperlipidemia, migraine
Citation: Luo S, Hong Y, Wen J and Zhang X (2024) Prevalence and correlates of post-stroke anxiety in Changde, China during 2023 following the lifting of COVID-19 restrictions. Front. Psychiatry 15:1430034. doi: 10.3389/fpsyt.2024.1430034
Received: 20 May 2024; Accepted: 20 September 2024;
Published: 30 September 2024.
Edited by:
Faris Lami, University of Baghdad, IraqReviewed by:
Riyadh Al-Rudaini, Ministry of Health, IraqDr. Naseem Akhtar Qureshi, Al-Falah University, India
Copyright © 2024 Luo, Hong, Wen and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Wen, Y2R3ZW5qdW4xOTczQDE2My5jb20=; Xiaobo Zhang, Mjg1MDU4MDQxQHFxLmNvbQ==
 Shangyu Luo
Shangyu Luo Yunjun Hong
Yunjun Hong Jun Wen
Jun Wen Xiaobo Zhang
Xiaobo Zhang