- 1Department of Experimental Medicine, University of Campania, “Luigi Vanvitelli”, Naples, Italy
- 2Department of Health Sciences, University of Catanzaro “Magna Gracia”, Catanzaro, Italy
- 3Department of Pharmacy, Health and Nutritional Sciences, University of Calabria, Cosenza, Italy
Introduction: This study investigated the quality of sleep in a sample of individuals from Southern Italy after the major waves of the COVID-19 pandemic, with the aim of evaluating how sleep patterns changed.
Methods: A cross-sectional study was conducted between March 2022 and January 2023 and involved adults who had a COVID-19 infection, who were invited to complete a self-administered online questionnaire.
Results: A total of 408 individuals participated in the survey. Overall, 66.4% had a reduction in social relations; 72.1% had an increase in the use of social media; and 86%, 77.2%, and 71.1% reported an extremely severe level of anxiety, stress, and depression, respectively. Almost all of the respondents had a Pittsburgh Sleep Quality Index score (PSQI) ≥5, indicating poor sleep quality. Subjects with a severe or extremely severe depression score, a severe or extremely severe stress score, who had a job, and who had someone close who died because of a COVID-19 infection were more likely to have a high PSQI global score. The use of sleep medication in the past months was significantly higher in those who were older, who had a job, who had a COVID-19 infection in the first and second waves, who had someone close who died from COVID-19, and who did not have changes in social relationships during the pandemic. Moreover, participants with severe or extremely severe depression scores, with severe or extremely severe stress scores, who were women, and who were older had troubles staying awake while engaging in social activities during the past month.
Conclusion: The results bring to light the high prevalence of poor sleep quality among individuals who were infected with SARS-CoV-2. Future research is needed to understand whether these disturbances are still present in the endemic period and whether it is necessary to investigate further determinants that have affected and/or are affecting sleep quality.
1 Introduction
The onset of the coronavirus disease 2019 (COVID-19) led to a catastrophic global pandemic (1). Managing the disease became increasingly difficult, prompting measures for containment such as track and trace, self-isolation, quarantine, social distancing, and nationwide lockdowns to curb the spread of infection (2, 3). These measures raised concerns about livelihoods and strained relationships, impacting the overall mental and physical health and well-being of individuals and their families (4). Research studies revealed a link between COVID-19 infection outbreaks and sleep dysfunction (5–8). Jaharmi et al. described sleep changes as a common symptom among COVID-19–infected individuals (9). A meta-analysis reported a global prevalence of about 40% for COVID-19–related sleep disturbances (10), yet it remains a relatively underexplored aspect in COVID-19 research (11). Sleep plays a recognized role in influencing the immune response, and there is evidence indicating that sleep disruptions may lead to immunosuppression (12, 13). Sleep, crucial for optimal organ and mental functioning, became a focal point during the pandemic. Poor sleep, associated with adverse clinical outcomes, posed an additional challenge during this emergency (9).
While the psychological and psychiatric repercussions of pandemic-related measures have been extensively studied, understanding their effects on sleep has been hindered by inconsistent study results (14–16).
Sleep-related manifestations, such as insomnia, can pose persistent challenges. If left untreated, insomnia can become chronic, aggravate pain syndromes and gastrointestinal disorders, and elevate the risk of hypertension, heart disease, and neuroinflammation (17, 18).
Italy has been one of the most affected nations worldwide during the pandemic; however, few studies have been conducted on sleep quality in the Italian population after this particular period. Therefore, we investigated the quality of sleep on a sample of individuals from Southern Italy after the major waves of the COVID-19 pandemic, with the aim of evaluating whether and how sleep patterns changed.
2 Materials and methods
2.1 Study population, sampling procedure, and data collection
This survey is part of larger research activities that investigated sleep quality among different populations in the Southern Italy (19). A cross-sectional study was conducted between March 2022 and January 2023. All individuals ≥18 years of age, who tested positive for COVID-19, were Italian speakers, and attended several health services (outpatient, clinic, vaccination center, etc.) of the Magna Graecia University of Catanzaro were included in the study. Those younger than 18 years old, those who did not give their consent to participate in the study, and those who had not been infected at least once with SARS-CoV-2 were excluded from the study. Part of the sample had already been involved in a previous study that explored the quality of sleep in a specific population-university students-who were or were not infected with SARS-CoV-2 (19).
The required sample size was calculated before the beginning of the study, considering a 95% confidence interval (CI), an alpha error of 5%, and assuming that 40% of individuals had sleep disturbances (10). Therefore, the minimum sample size was estimated to be 369 participants.
The data were collected by an anonymous, self-administered online questionnaire created with the Google Forms® online application. The questionnaire link, sent via email when the subject arrived at the health services, was accompanied by a brief of the study's purposes so that participants could choose to be involved or not, providing informed consent to take part in the survey. Only those who completed the questionnaire in all its parts were included, as the online form could be transmitted only by completing all answers. Furthermore, the online link could only be sent once to avoid repeated responses from the same participant.
The study protocol was approved by the Ethics Committee of the Magna Graecia University of Catanzaro (Protocol no. 107, 21 April 2022) and was conducted according to the Declaration of Helsinki. Participants did not receive any form of fee or incentive for contributing to this survey.
2.2 Survey instrument
The questions were grouped into four sections: (1) sociodemographic characteristics of the participants; (2) information on the contagion of COVID-19; (3) assessment of sleep quality; and (4) assessment of the level of anxiety, stress, and depression.
The variables examined in the sociodemographic section included gender, age, marital status, level of education, occupation, and collection of data on participants regarding the contagion by COVID-19, having been forced or not to mandatory quarantine, having had close individuals who had tested positive or not, having lost someone close due to COVID-19, and effects of the pandemic emergency on their social relationships (decrease/improvement of social contacts and use of social media).
Sleep quality was evaluated by the 19-item Pittsburgh Sleep Quality Index (PSQI) (20, 21). The PSQI is a self-administered questionnaire that appraises the quality of sleep with questions regarding the previous month. The scale is made up of the following seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunctions. By combining the records of each component, we obtained a final score between 0 and 21, where a score ≥5 indicates lower sleep quality, while a score <5 indicates higher sleep quality.
The short version of the Depression Anxiety Stress Scales (DASS-21) was employed to investigate anxiety, stress, and depression (22). DASS-21 is a self-rating scale to describe the frequency and severity of negative effects, in particular, depression is investigated by evaluating dysphoria, anhedonia, lack of incentives, and low self-esteem; anxiety by somatic symptoms of physiological over-arousal and fear response; and stress by irritability, impatience, tension, and arousal levels. Subscale scores are calculated as the sum of the answers to the seven items of all subscales and multiplied by 2 to meet the 42 items of the original instrument. The cutoffs of ≥14 defined moderate levels of depression, ≥10 of moderate anxiety, and ≥19 of moderate stress (23).
2.3 Statistical analysis
Results were examined using descriptive (frequencies, means, and standard deviations) and inferential (bivariate and multivariate analyses) statistics with the Stata software version 17 (24).
First, descriptive statistics were performed to summarize the main characteristics of the sample. Second, a univariate analysis was performed using the chi-square test, Student’s t-test, and Fisher’s exact test to evaluate the association between several potential determinants and having poor or good sleep (poor sleep = 0; good sleep = 1). All independent variables considered as potential determinants of the global score (PSQI) (continuous) (Model 1), of having used sleeping medicines in the past month (Model 2), and of having had trouble staying awake while engaging in social activities during the past month the questionnaire (Model 3) were included in the multivariate linear and logistic regression models with the purpose of identifying those predicting these outcomes of interest.
In the multivariate linear model, the following independent variables, which were judged to potentially have influenced the above mentioned outcome (Model 1), were included: gender (male = 0; female = 1); age in years (continuous); marital status (unmarried/widowed/divorced = 0; married/cohabitant = 1); education level (high school = 0; university degree/master = 1); occupation; time of COVID-19 infection (first and second waves = 0; subsequent waves = 1); someone close positive for COVID-19; someone close died from COVID-19; forced quarantine; changes in the social relationship during the pandemic (decreased = 0; stable/improved = 1); change in social media use during the pandemic (stable/decreased = 0; improved = 1); anxiety score (normal/mild/moderate = 0; severe/extremely severe = 1); depression score (normal/mild/moderate = 0; severe/extremely severe = 1); and stress score (normal/mild/moderate = 0; severe/extremely severe = 1). In the multivariate logistic models (Models 2 and 3), the following independent variables were selected for both models: gender (male = 0; female = 1); age in years (continuous); marital status (unmarried/widowed/divorced = 0; married/cohabitant = 1); education level (high school = 0; university degree/master = 1); occupation; time of COVID-19 infection (first and second waves = 0; subsequent waves = 1); someone close who tested positive for COVID-19, someone close who died from COVID-19; forced quarantine; changes in social relationship during the pandemic (decreased = 0; stable/improved = 1); change in social media use during the pandemic (stable/decreased = 0; improved = 1); anxiety score (normal/mild/moderate = 0; severe/extremely severe = 1); depression score (normal/mild/moderate = 0; severe/extremely severe = 1); and stress score (normal/mild/moderate = 0; severe/extremely severe = 1).
Backward stepwise procedures were applied, including in the final models only the characteristics that provided a significant explanation of the outcomes. Adjusted odds ratios (ORs) and 95% CIs were presented in the logistic regression models and standardized regression coefficients (β) and p-values in the linear regression model. All statistical tests were two-sided, and a p-value equal to or less than 0.05 was considered statistically significant.
3 Results
All 408 invited individuals agreed to participate in the survey. The main characteristics of the examined sample are reported in Table 1. A large majority of participants were women (75.5%), with a mean age of 31.7 (range = 19–64 ± 12.1), and 46.6% were unmarried, widowed, or divorced. Approximately half (46.8%) already had a university degree or master’s, and 41% were employed. Moreover, according to the COVID-19–related data, 61.5% of the participants declared to have had the infection in the third or subsequent waves, while quarantine was imposed on 98.1% of them; in addition, 92.4% declared to have had someone close who tested positive for COVID-19, and 10% had experienced someone close who died from COVID-19 infection. None reported to have been infected more than once. After the third wave, the majority of them (66.4%) had a reduction in social relationships, and 72.1% had an increase in the use of social media. Regarding mental health scores, individuals reported an extremely severe level of anxiety (86%), stress (77.2%), and depression (71.1%). Moreover, when exploring sleep quality, 95.3% of respondents had a PSQI score ≥5 (poor sleep quality). Regarding the single components of the PSQI score, 47.3% of participants reported a very bad subjective sleep quality; approximately half (49.8%) declared a sleep duration of 6 to 7 h per night; more than half (59.1%) reported having used sleep medications in the past month; and almost all subjects in the sample (93.2%) experienced daytime dysfunction in the past month, such as having trouble staying awake while driving, eating meals, or engaging in social activity (Supplementary Materials).
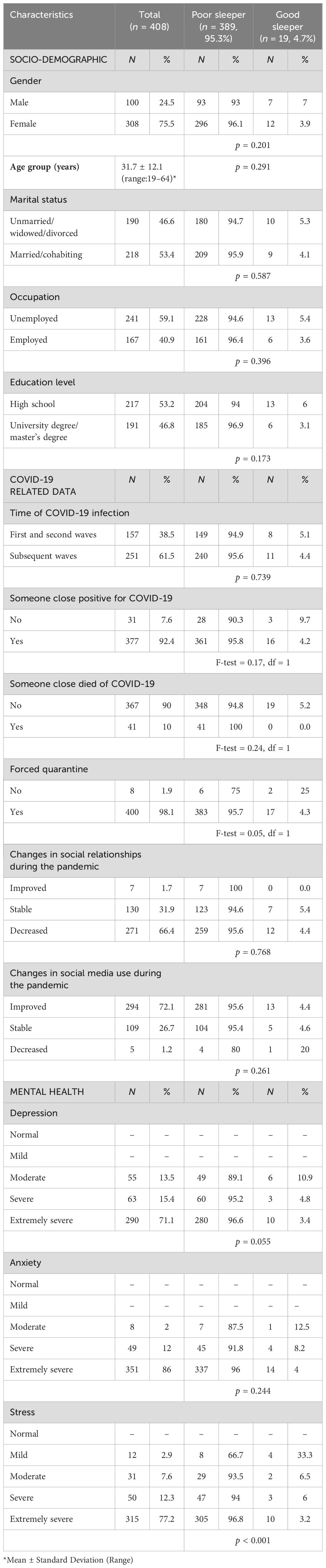
Table 1. Sociodemographic characteristics, COVID-19, and mental health data of the study population.
The results of the multivariate linear and logistic regression are shown in Table 2. The results of the multivariate linear analysis showed that subjects with severe or extremely severe depression scores, with severe or extremely severe stress scores, who had experienced someone close who died because of COVID-19 infection, and who had a job were more likely to have a high PSQI global score indicating poor sleep (Model 1 in Table 2).

Table 2. Results of multivariate linear and logistic regression analyses examining the determinants of the outcomes of interest.
When exploring behaviors, the use of sleep medication in the past months was significantly higher in those who were older (OR = 1.06; 95% CI 1.01–1.12), who had a job (OR = 11.19; 95% CI 3.89–32.16), who had COVID-19 infection in the first and second waves (OR = 0.29; 95% CI 0.16–0.52), who had someone close who died from COVID-19 (OR = 2.96; 95% CI 1.17–7.51), and who did not have changes in their social relationship during the pandemic (OR = 0.35; 95% CI 0.19–0.64) (Model 2 in Table 2). Moreover, the participants with severe or extremely severe depression scores (OR = 2.59; 95% CI 1.21–5.52) or stress scores (OR = 4.93; 95% CI 1.89–12.80), who were women (OR = 2.24; 95% CI 1.32–3.81), and were older (OR = 1.04; 95% CI 1.00–1.08) had significantly higher troubles staying awake while engaging in social activities during the past month (Model 3 in Table 2).
4 Discussion
Much of the literature emphasizes how behaviors relative to sleep in this historical period have changed and have had an impact, especially on mental disorders (25). The major factors influencing this association are physical illness, separation from loved ones, environmental stresses, social isolation, and pre-existing poor mental health (26–30). This study explored the determinants of sleep quality in individuals who had COVID-19 after major pandemic waves and suggested interesting implications for public health interventions aimed at improving sleep quality.
First, it is very interesting that 95.3% of respondents reported poor sleep quality; these data are higher than those reported in Europe before the COVID-19 pandemic, ranging from 35% to 47% (21, 31, 32). Compared with the quality of sleep in other countries, the results are worse than those reported in Romania (51%), Greece (52.4%), Pakistan (61.5%), and England (68.9%) (33–36).
Therefore, these data are very alarming; indeed, a meta-analysis that investigated the changes in the quality of sleep during the pandemic showed that 57% of the general population suffered a clear worsening in the quality of sleep (37). It is important to underline that disruption of bioelectrical brain activity and neurological symptoms have already been described in patients with COVID-19 infection at the beginning of the pandemic (38). Nevertheless, our results describe a very worrying situation that is in line with the data reported by this research group on university students in Italy during the pandemic, describing a relevant percentage of students (92.8%) as poor sleepers (19). Results suggest that this topic requires the insights that have been given in this paper in order to better understand, in a larger population, including university students who contract COVID-19, what the determinants of poor sleep quality are.
Second, regarding mental health scores, individuals reported extremely severe levels of anxiety (86%), stress (77.2%), and depression (71.1%). These data are more alarming, according to the DASS-21 than those reported in other countries. For example, in Vietnam, the proportion of extremely severe levels of depression, anxiety, and stress was reported to be 3%, 3.6%, and 0.8%, respectively (39), and in the Philippines, 4.2% reported severe to extremely severe depressive symptoms, 11.1% reported severe to extremely severe anxiety symptoms, and 3.9% reported severe to extremely severe stress signals (40). Moreover, results from the general population in Spain also described lower extreme values (2.8% for depression, 4.1% for anxiety, and 3.3% for stress) (41). A significant increase in depression and anxiety has been described from 6 months to 2–3 years after COVID-19 infection in the UK (42). Moreover, a study conducted in six countries described that COVID-19 patients had a higher prevalence of depressive symptoms (43). The lockdown and the prevailing epidemic situation in the Italian region had an impact on people's daily lives and their relationships with others (44), and presumably, this contributed to the variations in mental health problems observed during the COVID-19 pandemic. Indeed, Italy was one of the first and most affected countries worldwide during the pandemic; therefore, uncertainty and social restrictions may have adversely affected mental health. Further investigations are needed to better understand these associations.
The results of the multivariate linear and logistic regression analyses showed that several characteristics were independently associated with the different outcomes of interest. In particular, a higher PSQI global score was associated with depression and stress; indeed, it has been described that the overlapping prevalence rates between mental health symptoms and poor quality of sleep problems point to the likely bidirectional relationships between sleep and psychiatric diseases, particularly when more symptoms are present (such as depression and stress) (9). Moreover, those who had experienced someone close who died from COVID-19 infection were more likely to have a high PSQI global score; in fact, it has been described that poor sleep quality may be associated with trauma or post-traumatic stress disease symptoms (45, 46). Those who had a job were more likely to have a high PSQI global score; these data are inconsistent with other results reporting non-employees to have worse sleep quality during the COVID-19 pandemic (47). However, pre-pandemic results found evidence for reversed relations between work-related stress and sleep quality; in particular, low sleep quality was associated with a worsening in work-related stress over time (48). The use of sleep medication in the past months was significantly higher in those who were older, in those who had a job, in those who had COVID-19 infection in the first and second waves, in those who had someone close who died from COVID-19, and in those who did not change their social relationships during the pandemic. Our results, reporting higher use of sleep medications among the elderly, were confirmed by previous literature describing the elderly as being at higher risk for sleep disturbances (49). The higher risk of sleep problems in those who contracted COVID-19 has been attributed to physical pain and the side effects of medications administered for the treatment of the infection (50). Moreover, participants with severe or extremely severe depression or stress scores, who were women, and who were older, had more troubles staying awake while engaging in social activities during the past month. Evidence of an association between poor sleep quality and poorer physical performance in older adults, in particular women, has been described (51). It has been reported that bedtime and wake time were generally much later in women than in men and that women had significantly shorter sleep duration than men, particularly in individuals aged 30–40 (52).
This study presents some possible limitations that need to be explained when interpreting the results. First, the analysis was based on cross-sectional data, so absolute causal assumptions about the detected relationships between determinants and outcomes are limited. Second, participants may have been influenced to answer in a more “desirable” way, and this may have led to an overestimation of sleep quality and its components. Third, there were potential biases related to the use of self-report questionnaires, such as recall bias, because participants’ responses about sleep quality or mental health status might not be accurate. Fourth, the sample was collected in Southern Italy from a single center and might not be completely representative and may limit generalizability to the Italian population. Fifth, potential confounding factors have not been explored, such as drug use, previous sleep, and mental or psychiatric diseases diagnosed before or after the COVID-19 infection, for which participants were being treated by a psychiatrist or a neurologist. Last, the quality of sleep has also not been assessed with an objective procedure, such as the polysomnographic test; it was only measured with a subjective tool, and this might not indicate the participants’ real quality of sleep.
Despite these limitations, the results have delivered new knowledge on a relevant issue not yet completely explored.
The results of the current study bring to light the high prevalence of poor sleep quality among individuals who were infected by SARS-CoV-2 and add to the recent literature on sleep quality on how the pandemic had an impact on sleep health. Future research is needed to understand whether these disorders are still present in the endemic period and whether it is necessary to investigate further determinants that have affected and/or are affecting sleep quality.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Magna Graecia University of Catanzaro. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
VS: Formal analysis, Resources, Visualization, Writing – original draft. SA: Conceptualization, Data curation, Investigation, Writing – original draft. GP: Formal analysis, Resources, Writing – original draft. CP: Data curation, Writing – original draft. CN: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing – original draft. GD: Formal analysis, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
Preliminary results have been presented at the "XXXII Congresso Interregionale Siculo- Calabro" of the Italian Public Health Association (SItI), Enna, May 23-25, 2024.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1428423/full#supplementary-material
References
1. COVID-19 Cumulative Infection Collaborators. Estimating global, regional, and national daily and cumulative infections with SARS-CoV-2 through Nov 14, 2021: a statistical analysis. Lancet. (2022) 399:2351–80. doi: 10.1016/S0140-6736(22)00484-6
2. Hussain T, Jawed N, Mughal S, Shafique K. Public perception of isolation, quarantine, social distancing and community containment during COVID-19 pandemic. BMC Public Health. (2022) 22:528. doi: 10.1186/s12889-022-12970-y
3. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
4. Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, Holzinger B, et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. (2020) 29:e13052. doi: 10.1111/jsr.13052
5. Shaik L, Boike S, Ramar K, Subramanian S, Surani S. COVID-19 and sleep disturbances: a literature review of clinical evidence. Medicina (Kaunas). (2023) 59:818. doi: 10.3390/medicina59050818
6. Abel KM, Carr MJ, Ashcroft DM, Chalder T, Chew-Graham CA, Hope H, et al. Association of SARS-CoV-2 infection with psychological distress, psychotropic prescribing, fatigue, and sleep problems among UK primary care patients. JAMA Netw Open. (2021) 4:e2134803. doi: 10.1001/jamanetworkopen.2021.34803
7. Donzella SM, Kohler LN, Crane TE, Jacobs ET, Ernst KC, Bell ML, et al. COVID-19 infection, the COVID-19 pandemic, and changes in sleep. Front Public Health. (2022) 9:795320. doi: 10.3389/fpubh.2021.795320
8. Jiang Z, Zhu P, Wang L, Hu Y, Pang M, Ma S, et al. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. J Psychiatr Res. (2021) 136:595–602. doi: 10.1016/j.jpsychires.2020.10.034
9. Jahrami H, BaHammam AS, Bragazzi NL, Saif MZ, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. (2021) 17:299–313. doi: 10.5664/jcsm.8930
10. Jahrami HA, Alhaj OA, Humood AM, Alenezi AF, Fekih-Romdhane F, AlRasheed MM, et al. Sleep disturbances during the COVID-19 pandemic: a systematic review, meta-analysis, and meta-regression. Sleep Med Rev. (2022) 62:101591. doi: 10.1016/j.smrv.2022.101591
11. Choudhry AA, Shahzeen F, Choudhry SA, Batool N, Murtaza F, Dilip A, et al. Impact of COVID-19 infection on quality of sleep. Cureus. (2021) 13:e18182. doi: 10.7759/cureus.18182
12. Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. (2012) 463:121–37. doi: 10.1007/s00424-011-1044-0
13. Zambrelli E, Canevini M, Gambini O, D’Agostino A. Delirium and sleep disturbances in COVID–19: a possible role for melatonin in hospitalized patients? Sleep Med. (2020) 70:111. doi: 10.1016/j.sleep.2020.04.006
14. Jeong H, Yim HW, Song YJ, Ki M, Min JA, Cho J, et al. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health. (2016) 38:e2016048. doi: 10.4178/epih.e2016048
15. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
16. Su CT, Wang JD, Lin CY. Child-rated versus parent-rated quality of life of community-based obese children across gender and grade. Health Qual Life Outcomes. (2013) 11:206. doi: 10.1186/1477-7525-11-206
17. Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J Psychosom Res. (2021) 141:110343. doi: 10.1016/j.jpsychores.2020.110343
18. Becker PM. Overview of sleep management during COVID-19. Sleep Med. (2021) 91:211–8. doi: 10.1016/j.sleep.2021.04.024
19. Angelillo S, Sansone V, Paduano G, Lateano L, Di Giuseppe G, Nobile CGA. The quality of sleep: evaluation among university students. Front Public Health. (2024) 11:1270426. doi: 10.3389/fpubh.2023.1270426
20. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–364 213. doi: 10.1016/0165-1781(89)90047-4
21. Curcio G, Tempesta D, Scarlata S, Marzano C, Moroni F, Rossini PM, et al. Validity of the Italian version of the Pittsburgh sleep quality index (PSQI). Neurol Sci. (2013) 34:511–9. doi: 10.1007/s10072-012-1085-y
22. Bottesi G, Ghisi M, Altoè G, Conforti E, Melli G, Sica C. The Italian version of the Depression Anxiety Stress Scales-21: factor structure and psychometric properties on community and clinical samples. Compr Psychiatry. (2015) 60:170–81. doi: 10.1016/j.comppsych.2015.04.005
23. Lovibond SH, Lovibond PF. Depression anxiety stress scales. Sydney: Psychol Foundation Aust Inc. (1996).
24. Stata Corporation. Stata Reference Manual Release 17. College Station, TX, USA: Stata Corporation (2017).
25. Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. (2021) 8:130–40. doi: 10.1016/S2215-0366(20)30462-4
26. Pang JCY, Chan ELS, Lau HMC, Reeves KKL, Chung THY, Hui HWL, et al. The impacts of physical activity on psychological and behavioral problems, and changes in physical activity, sleep and quality of life during the COVID-19 pandemic in preschoolers, children, and adolescents: a systematic review and meta-analysis. Front Pediatr. (2023) 11:1015943. doi: 10.3389/fped.2023.1015943
27. Xin J, Zhang Y, Tang Y, Yang Y. Brain differences between men and women: evidence from deep learning. Front Neurosci. (2019) 13:185. doi: 10.3389/fnins.2019.00185
28. Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. (2021) 51:1052–3. doi: 10.1017/S0033291720000999
29. Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. (2020) 87:49–50. doi: 10.1016/j.bbi.2020.04.031
30. Lin CY, Li YP, Lin SI, Chen C. Measurement equivalence across gender and education in the WHOQOL-BREF for community-dwelling elderly Taiwanese. Int Psychogeriatrics. (2016) 28:1375–82. doi: 10.1017/S1041610216000594
31. Pileggi C, Lotito F, Bianco A, Nobile CG, Pavia M. Relationship between chronic short sleep duration and childhood body mass index: a school-based cross-sectional study. PloS One. (2013) 8:e66680. doi: 10.1371/journal.pone.0066680
32. Sañudo B, Fennell C, Sánchez-Oliver AJ. Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns pre- and during-COVID-19 quarantine in young adults from Spain. Sustainability (Basel Switzerland). (2020) 12:5890. doi: 10.3390/su12155890
33. Munteanu I, Marc M, Gheorghevici C, Diaconu GA, Feraru N, Sion D, et al. Sleep quality aspects in post-COVID-19 patients. J Pers Med. (2023) 13:1125. doi: 10.3390/jpm13071125
34. Eleftheriou A, Rokou A, Arvaniti A, Nena E, Steiropoulos P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front Public Health. (2021) 9:775374. doi: 10.3389/fpubh.2021.775374
35. Malik M, Atiq A, Tahir MJ, Akhtar FK, Malik MI, Hassan W, et al. Comparison of sleep quality among COVID-19 patients and non-COVID-19 population in Pakistan: a cross sectional study during the COVID-19 pandemic. Ann Med Surg (Lond). (2022) 78:103894. doi: 10.1016/j.amsu.2022.103894
36. Kantor J, Kantor BN, Fortgang RG, Pace-Schott EF. Sleep quality impairment is associated with pandemic attitudes during the Coronavirus Disease 2019 (COVID-19) circuit breaker lockdown in England: a cross-sectional study. Front Public Health. (2022) 10:819231. doi: 10.3389/fpubh.2022.819231
37. Limongi F, Siviero P, Trevisan C, Noale M, Catalani F, Ceolin C, et al. Changes in sleep quality and sleep disturbances in the general population from before to during the COVID-19 lockdown: a systematic review and meta-analysis. Front Psychiatry. (2023) 14:1166815. doi: 10.3389/fpsyt.2023.1166815
38. Waliszewska-Prosół M, Budrewicz S. The unusual course of a migraine attack during COVID-19 infection - Case studies of three patients. J Infect Public Health. (2021) . 14:903–5. doi: 10.1016/j.jiph.2021.04.013
39. Nguyen Thanh H, Cap Minh D, Hoang Thu H, Nguyen Quang D. Symptoms, mental health, and quality of life among patients after COVID-19 infection: a cross-sectional study in Vietnam. J Prev Med Public Health. (2024) 57:128–37. doi: 10.3961/jpmph.23.511
40. Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. (2020) 277:379–91. doi: 10.1016/j.jad.2020.08.043
41. Reno-Chanca S, Van Hoey J, Santolaya-Prego de Oliver JA, Blasko-Ochoa I, Sanfeliu Aguilar P, Moret-Tatay C. Differences between the psychological symptoms of health workers and general community after the first wave of the COVID-19 outbreak in Spain. Front Psychol. (2021) 12:644212. doi: 10.3389/fpsyg.2021.644212
42. Taquet M, Skorniewska Z, De Deyn T, Hampshire A, Trender WR, Hellyer PJ, et al. Cognitive and psychiatric symptom trajectories 2-3 years after hospital admission for COVID-19: a longitudinal, prospective cohort study in the UK. Lancet Psychiatry. (2024) 12:644212. doi: 10.1016/S2215-0366(24)00214-1
43. Taquet M, Sillett R, Zhu L, Mendel J, Camplisson I, Dercon Q, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. (2022) 9:815–27. doi: 10.1016/S2215-0366(22)00260-7
44. Romano V, Ancillotti M, Mascalzoni D, Biasiotto R. Italians locked down: people's responses to early COVID-19 pandemic public health measures. Humanit Soc Sci Commun. (2022) 9:342. doi: 10.1057/s41599-022-01358-3
45. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
46. Gibson CJ, Richards A, Villanueva C, Barrientos M, Neylan TC, Inslicht SS. Subjective sleep related to post traumatic stress disorder symptoms among trauma-exposed men and women. Behav Sleep Med. (2019) . 17:492–501. doi: 10.1080/15402002.2017.1409223
47. Alharbi AS, Alshahrani SM, Alsaadi MM, Al-Jahdali HH, Wali SO, BaHammam AS. Sleep quality and insomnia during the COVID-19 lockdown among the Saudi public: a cross-sectional study. Saudi Med J. (2021) 42:384–90. doi: 10.15537/smj.2021.42.4.20200735
48. Van Laethem M, Beckers DG, Kompier MA, Kecklund G, van den Bossche SN, Geurts SA. Bidirectional relations between work-related stress, sleep quality and perseverative cognition. J Psyc Res. (2015) 79:391–8. doi: 10.1016/j.jpsychores.2015.08.011
49. Hasan F, Tu YK, Lin CM, Chuang LP, Jeng C, Yuliana LT, et al. Comparative efficacy of exercise regimens on sleep quality in older adults: a systematic review and network meta-analysis. Sleep Med Rev. (2022) 65:101673. doi: 10.1016/j.smrv.2022.101673
50. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
51. Denison HJ, Jameson KA, Sayer AA, Patel HP, Edwards MH, Arora T, et al. Poor sleep quality and physical performance in older adults. Sleep Health. (2021) 7:205–11. doi: 10.1016/j.sleh.2020.10.002
Keywords: COVID-19, mental health, sleep quality, social activities, survey
Citation: Sansone V, Angelillo S, Paduano G, Pileggi C, Nobile CGA and Di Giuseppe G (2024) Quality of sleep after COVID-19 infection: a cross-sectional study in the Southern Italy. Front. Psychiatry 15:1428423. doi: 10.3389/fpsyt.2024.1428423
Received: 16 May 2024; Accepted: 21 August 2024;
Published: 24 September 2024.
Edited by:
Carolina Marzuillo, Sapienza University of Rome, ItalyReviewed by:
Marta Waliszewska-Prosół, Wroclaw Medical University, PolandAnnalisa Rosso, Local Health Authority Rome 2, Italy
Erika Renzi, Sapienza University of Rome, Italy
Copyright © 2024 Sansone, Angelillo, Paduano, Pileggi, Nobile and Di Giuseppe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Silvia Angelillo, c2lsdmlhLmFuZ2VsaWxsb0BzdHVkZW50aS51bmljei5pdA==
 Vincenza Sansone
Vincenza Sansone Silvia Angelillo
Silvia Angelillo Giovanna Paduano
Giovanna Paduano Claudia Pileggi
Claudia Pileggi Carmelo Giuseppe Angelo Nobile3
Carmelo Giuseppe Angelo Nobile3 Gabriella Di Giuseppe
Gabriella Di Giuseppe