
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Psychiatry , 10 January 2025
Sec. Psychological Therapy and Psychosomatics
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1422877
This article is part of the Research Topic Psychocardiology in Socially Disadvantaged Groups View all 4 articles
 Michael Friedman1*
Michael Friedman1* Ryan Chang2
Ryan Chang2 Zahir Malik Amin3
Zahir Malik Amin3 Tanuja Rajan4
Tanuja Rajan4 Rahul Singh5
Rahul Singh5 Samuel Yousefzai6
Samuel Yousefzai6 Izza Shahid7
Izza Shahid7 Khurram Nasir7
Khurram Nasir7 Zulqarnain Javed7
Zulqarnain Javed7While the physical health effects of obesity are well-characterized, an emerging branch of research has shown that obesity additionally plays a critical role in one’s mental health. Young adults, in a pivotal transition phase in their lives, may be particularly prone to the concurrent effects of obesity and adverse mental health outcomes. The purpose of this review is to comprehensively examine existing data regarding the connection between obesity and two widely validated measures of mental health: psychological distress and depression. The connection between mental health outcomes and obesity is mediated by a complex interplay between biological and sociocultural factors, which is explored in this review with particular focus on younger adults aged 20-39. Further, the impact of several demographic factors including race/ethnicity, gender, and immigration status are examined closely. To our knowledge, this review is one of the first efforts to integrate existing knowledge between obesity and mental health, with particular regard for young adults and the impact of other key sociodemographic characteristics. This review has important implications at the interface of two of the most pressing public health crises in the United States.
Obesity is an emerging public health crisis in the United States, and the rates of obesity have continued to rise substantially in recent decades. Obesity in adults aged 20 and over increased from 30.5% to 42.4% between 1999-2000 and 2017-2018, with the prevalence of severe obesity (BMI > 40.0) nearly doubling in this same time period (1). While the physical health risks associated with obesity—including cardiovascular disease (CVD), type 2 diabetes mellitus (T2DM), and cancer—are well characterized, the mental health effects of obesity remain less understood (2, 3).
Several studies have established that obesity is strongly associated with adverse mental health outcomes, including major depressive disorder (MDD) (4–9). Adolescents and young adults (AYAs), at a pivotal stage in their physical and neurological development, experience an increased risk of these mental health effects, as well as the concurrent effects of obesity. According to the CDC, 45.3% of adults aged 20-39 with depression also experience obesity, while just 30.0% of non-depressed individuals within this age group are obese (7).
The purpose of this review is to summarize emerging evidence regarding the intricate bidirectional association in AYAs between obesity and two widely validated measures of mental health: psychological distress (PD) and depression. To our knowledge, this review is one of the first efforts to integrate existing knowledge between obesity and mental health, with particular regard for younger populations and the impact of other key sociodemographic characteristics.
This review focuses on studies that have evaluated major depressive disorder (MDD) and psychological distress (PD) according to the following criteria:
MDD is formally defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria. According to the DSM-5, MDD is characterized by the presence of five or more characteristic depressive symptoms during the same 2-week period, representing a change from previous functioning, with at least one of the symptoms being either depressed mood or anhedonia (loss of interest or pleasure) (10).
PD encompasses symptoms of anxiety, depression, and other emotional suffering, which can significantly impact a person’s daily functioning and quality of life. Early evaluation and screening for distress are crucial for timely management and improved medical outcomes, which is typically performed through the Kessler Psychological Distress Scale (11, 12).
According to the CDC, an individual is classified as obese if their body mass index (BMI) is ≥ 30 kg/m2. Obesity is further divided into subcategories including Class 1 (BMI 30-34.99 kg/m2), Class 2 (BMI 35-39.99 kg/m2), and Class 3 (BMI >40 kg/m2).
Several population-based studies have established an association between mental health and obesity. In 2010, a meta-analysis of over 58,000 participants established a bi-directional association between depression and obesity that was statistically significant among adults aged 20-59 (8). The mixed aggregation of adults across all age categories limited the ability to make specific conclusions about younger adults, which was a consistent limitation seen across many of the studies that have been published in this area to date. Interestingly, the obesity/MDD association was not found to be statistically significant in individuals <20 years, further emphasizing the importance of age-related considerations in this area of research. An additional meta-analysis from De Wit et al. (13) and a cross-sectional study by Ul-Haq et al. again established a significant association between MDD and obesity – especially among females – but the age-related effects of this relationship were still unclear. Some studies indicate that this relationship may be especially potent in younger populations, though more of these studies have focused on adolescents rather than the impact on young adult populations (9, 14, 15).
Table 1 summarizes existing research in this area and the limitations of current data. Our findings point to a need for continued age-related considerations in this area of research for several reasons. First, studies indicate several key distinctions in the PD/MDD-obesity relationship across age groups. AYA populations are typically not as physically active and experience increased levels of psychosocial stress compared to pre-adolescents (16, 17). Weight changes and differences in appetite are more common in adolescent MDD than adult MDD (18), contributing to elevated risk of obesity among depressed AYAs. Other studies have indicated that early childhood traumatic events contribute to elevated risk of CVD and obesity in adulthood (14, 15, 19). There are additional neurological differences between AYA and adult depression, including differences in cortisol levels. While hypercortisolemia is commonly identified in adult patients with MDD, this same finding does not hold in AYA’s with MDD (20). Incidence of concurrent obesity and depression further varies depending on the subtype of depression. Individuals with atypical MDD– a form of depression characterized by mood improvements following positive experiences– are more likely to experience obesity than those with typical MDD (21). These findings indicate that the mental health/obesity association may be particularly potent in AYA populations, signifying a need for more age-specific considerations in this area of research.
Numerous studies have indicated that nutritious diets reduce inflammatory processes in the brain (22–24). Calorie-rich diets with high levels of saturated fats and sugar have been shown to stimulate immune activation and negatively affect hippocampal function and other cognitive processes (25, 26). Diets high in refined carbohydrates and saturated fat have additionally been shown to reduce brain-derived neurotrophic factor (BDNF) in the hippocampus, resulting in impaired spatial memory and increased risk of depression (22, 27, 28). Adipocytes initiate the release of pro-inflammatory cytokines including interleukin-6, interleukin-2, and C-reactive protein, which have an established role in inducing psychological distress (29). Longitudinal studies have further indicated that individuals scoring lower on their Dietary Inflammatory Index experience lower incidence of depression (30), and that anti-inflammatory drugs may alleviate some depressive symptoms (31, 32). These findings point to a marked relationship between diet quality, chronic inflammation, and concurrent obesity/mental health outcomes.
The association between obesity and depression appears to involve hypothalamic-pituitary-adrenal (HPA) axis dysregulation. Individuals with MDD commonly experience chronically elevated levels of cortisol, increasing the likelihood of HPA axis dysfunction (33, 34). Overstimulation of the HPA axis ultimately causes glucocorticoid receptors to become less sensitive (29), and subsequent inadequate negative feedback mechanisms result in continued production of stress hormones that contribute to increased obesity risk (29). The HPA-axis hypothesis may be especially critical in younger populations, as past research has established that cortisol levels vary depending on age and correspondingly may influence depression susceptibility (23, 35).
A “self-medication” hypothesis may also play a role in connecting MDD and obesity (19, 22). According to this theory, unhealthy foods provide temporary relief from stress, increasing the likelihood of “subtle addiction” (19). This can result in poor eating habits and increase the likelihood of concurrent depression and obesity, as revealed by the systemic inflammation hypothesis (See section 3.2) (22). Obese AYAs additionally experience increased risk of substance abuse as a coping mechanism for negative emotions (36).
Psychosocial stressors may contribute to additional maladaptive coping mechanisms, including suboptimal sleep patterns (37–39). Poor sleep quality has been linked to both increased risk of depression and obesity (40), and these stress-related disruptions to sleeping patterns seemingly play an especially important role in the mental well-being of younger populations (41–45).
Across all age groups, both PD and MDD are more common in females than males (46–48). This disparity is believed to be most pronounced during adolescence (49), and approximately one in six females aged 12-20 have experienced at least one episode of MDD (50). While obesity rates among males and females are similar between different age groups (1), females are more likely to experience effects of obesity-related diseases (16). Females may further experience higher levels of weight-related stigma compared to males, increasing the likelihood of adverse mental health outcomes (47). As such, females additionally are more likely to resort to extreme dieting practices that negatively impact bodily health and psychological well-being (47, 51). Adolescent females are also more likely to resort to negative coping mechanisms for weight concerns, including smoking (52).
Across all age groups, females with MDD are more likely to experience obesity than females without depression, yet this trend does not hold in males (7). A study of adults with MDD found that depression in females was positively linked to BMI, total body fat, and visceral fat, but these associations were not found to be statistically significant in males (53). Additionally, adolescent obese females have displayed a nearly four-times higher risk of MDD (HR=3.9) compared to normal weight individuals, significantly stronger than the association seen in males (HR=1.5) (54, 55).
Males have been found to be less likely to report weight dissatisfaction than females (56), though male experiences of stigma also contribute to substantially increased likelihood of psychological distress and depression (57, 58). Experiencing weight-related stigma is more common in younger populations, irrespective of gender (49, 57, 59). These experiences of stigmatization contribute to elevated risk of PD and lower levels of self-esteem in young populations (59).
The burden of obesity is increasing in younger populations across all racial groups in the U.S., but non-Hispanic Black (NHB) and Hispanic American adults experience particularly high rates of obesity (60).
Evidence additionally suggests that NHB and Hispanic individuals tend to have higher levels of PD than non-Hispanic White (NHW) individuals, as well as higher rates of MDD (61, 62). Studies indicate that variation in socioeconomic status (SES), psychosocial stressors, limited access to healthcare resources, and experiences of racial discrimination may contribute to increased likelihood of concurrent MDD/PD and obesity among minority groups (62–64). In addition, barriers to treatment and diagnosis—including structural factors, lack of accessibility, and stigmatization—may contribute to significant underdiagnosis among racial/ethnic minorities (61, 63, 65).
More research is needed to identify racial/ethnic disparities in the progression of the MDD/obesity relationship. While these studies establish the current racial disparities in both obesity and mental health outcomes, there is limited evidence regarding the specific association between obesity and mental health outcomes in young adults. Future research should focus in particular on young adult minority populations, where current evidence is scarce.
The association between MDD and obesity varies depending on both immigration status and length of U.S. residency. Studies have further indicated that the MDD/obesity relationship in immigrant populations may differ from that seen in other socio-demographic groups (38). Surprisingly, a study of Brazilian, Haitian, and Latina immigrants found that females with higher levels of occupational physical activity had a higher likelihood of depression, despite experiencing lower rates of obesity (66). This result may suggest that other variables contribute to higher levels of depression among immigrants in physically active workplaces, such as physical strain, workplace demand, or employer discrimination (66).
Other studies have described an “immigrant paradox,” in which immigrant youth are less likely to experience mental health complications than US-born youth despite the elevated psychosocial risk factors associated with immigration (67, 68). However, this paradox does not appear to hold for obesity, as studies have indicated that children of immigrant mothers are more likely to be obese than the offspring of US-born mothers (69). These results, however, may vary by generational status of the immigrant population. In particular, obesity is less common in first-generation immigrant adolescents than second- or third-generation adolescents (70), indicating that more acculturated immigrants may be at higher risk of becoming obese. Additional studies have determined that relative obesity risk may be associated with the length of residency in the U.S (71–73).
As shown in Figure 1, the association between obesity and mental health outcomes is mediated by a complex interplay between biological and sociocultural factors, as well as upstream social determinants of health (SDOH). Evidence suggests that SDOH such as socioeconomic status, food insecurity, experiences of discrimination, social support, and housing conditions are strongly associated with both physical and mental health outcomes. Over 15% of individuals living in poverty also experience depression, compared to just 3.5% for those over 400% above the poverty line (74). Studies have proposed a “social mobility hypothesis” in which increased SES mitigates the mental health risk that one faces while in a lower SES bracket (75). According to this hypothesis, younger populations are at higher risk of mental health disorders due to less mobility in their SES (75), emphasizing the importance of age-specific considerations when analyzing depression risk.
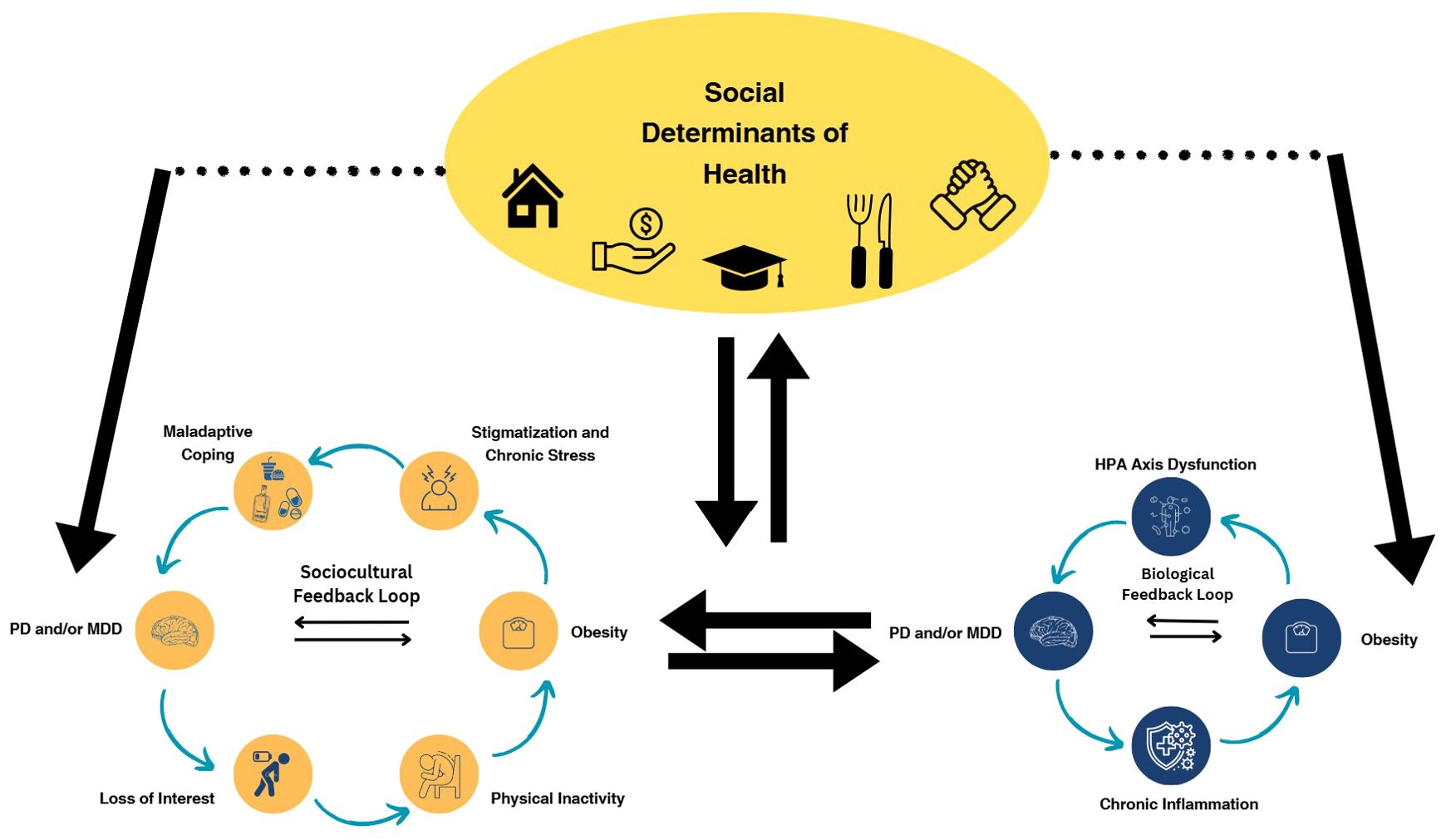
Figure 1. The PD/obesity association is upheld by several feedback loops, creating a vicious cycle where the two conditions reinforce one another. At play are both a sociocultural feedback loop involving several key dynamics including stigmatization, chronic stress, and maladaptive coping mechanisms such as substance abuse and binge eating. The biological association between PD and obesity is characterized by HPA axis dysfunction, excessive cortisol release, and systemic inflammation. Both of these feedback loops may be initiated by broader social determinants of health such as food insecurity, social support, and socioeconomic status.
Additional SDOH associated with depression and obesity include social support, housing conditions, food insecurity, and experiences of discrimination (76, 77). Studies have indicated that there is a three-fold increase in depression incidence among individuals who reported being distant from family members (77), as well as a graded increase in obesity risk by relative SDOH burden (78). Strikingly, 12.8% of U.S. households still reported being food insecure at times in 2022 (79), which is strongly associated with obesity risk, malnutrition, and higher SDOH burden (80–82). Experiences of childhood food insecurity have additionally been shown to increase the likelihood of both obesity and adverse mental health outcomes later in life (83).
To date, there is still limited evidence regarding the specific impacts of these SDOH on AYAs. Future research should more thoroughly establish how the impacts of these SDOH vary depending on age group, and how they differentially contribute to obesity and mental health outcomes.
The change from adolescence to adulthood is a dynamic and complex developmental stage, during which the relationship between PD/MDD-obesity must be studied in detail. Our research establishes that this stage of life is a period of unique vulnerability to the concurrent effects of obesity and mental health outcomes, and that this association appears to be further exacerbated by key demographic characteristics including racial/ethnic, gender, and immigration status. While the association between MDD and obesity is well-characterized, our work indicates that the AYA population is often not well-represented in this area of research.
To effectively address the public health crises of obesity and mental illness, policies should emphasize the intertwined nature of these conditions, and the additional heightened vulnerability of AYAs to these effects. Health systems should partner with community stakeholders to confront challenges faced by AYAs with obesity, especially those from underserved backgrounds, and design evidence-based interventions to enhance access to preventive health services while addressing social and structural barriers in obesity and psychiatric care. These include obesity and psychiatric illness screening, nutritional counseling, social support, transportation, access to medical and psychological therapies, addressing cost barriers, and implementing strategies to address medication non-adherence in the AYA population.
Among AYAs, MDD and PD have an intricate interplay with obesity which may be distinct from their mutual association in the adult population. To date, research specifically examining this association in AYA populations is limited, pointing to a need for more research specifically considering the obesity/mental health association in young populations. SDOH such as housing, food insecurity, socioeconomic status, and discrimination have been shown to increase the risk of MDD and PD, although their potency in AYA is less clear. Factors involved in this include a dysregulated HPA axis, systemic inflammation, and the “self-medication” hypothesis. There is further nuanced variation based on gender, race/ethnicity and immigration/citizenship status, but age-related association remains somewhat unclear. These findings have important implications at the interface of two of the most pressing emerging public health crises in the U.S.
MF: Conceptualization, Investigation, Visualization, Writing – original draft, Writing – review & editing. RC: Conceptualization, Visualization, Writing – review & editing. ZA: Conceptualization, Writing – review & editing. TR: Visualization, Writing – review & editing. RS: Writing – original draft, Writing – review & editing. SY: Writing – review & editing. IS: Writing – review & editing. KN: Supervision, Writing – review & editing. ZJ: Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hales C, Carroll M, Fryar C. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief. (2020) 360:1–8.
2. García-Montero C, Ortega MA, Alvarez-Mon MA, Fraile-Martinez O, Romero-Bazán A, Lahera G, et al. The problem of malnutrition associated with major depressive disorder from a sex-gender perspective. Nutrients. (2022) 14:1107. doi: 10.3390/nu14051107
3. Kobylińska M, Antosik K, Decyk A, Kurowska K. Malnutrition in obesity: is it possible? Obes Facts. (2022) 15:19–25. doi: 10.1159/000519503
4. Milaneschi Y, Simmons WK, Van Rossum EFC, Penninx BW. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. (2019) 24:18–33. doi: 10.1038/s41380-018-0017-5
5. Lee JI, Busler JN, Millett CE, Principe JL, Levin LL, Corrigan A, et al. Association between visceral adipose tissue and major depressive disorder across the lifespan: A scoping review. Bipolar Disord. (2022) 24:375–91. doi: 10.1111/bdi.13130
6. Coryell WH, Butcher BD, Burns TL, Dindo LN, Schlechte JA, Calarge CA. Fat distribution and major depressive disorder in late adolescence. J Clin Psychiatry. (2016) 77:84–9. doi: 10.4088/JCP.14m09169
7. Pratt L, Brody D. Depression and obesity in the U.S. Adult household population, 2005–2010. NCHS Data Brief (2014) 303:1–8.
8. Luppino FS, De Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. (2010) 67:220. doi: 10.1001/archgenpsychiatry.2010.2
9. Kubzansky LD, Gilthorpe MS, Goodman E. A prospective study of psychological distress and weight status in adolescents/young adults. Ann Behav Med Publ Soc Behav Med. (2012) 43:219–28. doi: 10.1007/s12160-011-9323-8
10. Marx W, Penninx BWJH, Solmi M, Furukawa TA, Firth J, Carvalho AF, et al. Major depressive disorder. Nat Rev Dis Primer. (2023) 9:44. doi: 10.1038/s41572-023-00454-1
11. Tomitaka S, Kawasaki Y, Ide K, Akutagawa M, Ono Y, Furukawa TA. Distribution of psychological distress is stable in recent decades and follows an exponential pattern in the US population. Sci Rep. (2019) 9:11982. doi: 10.1038/s41598-019-47322-1
12. Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. (2003) 60:184. doi: 10.1001/archpsyc.60.2.184
13. De Wit L, Luppino F, Van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Research. (2010) 178:230–5. 10.1016/j.psychres.2009.04.015
14. Mundi MS, Hurt RT, Phelan SM, Bradley D, Haller IV, Bauer KW, et al. Associations between experience of early childhood trauma and impact on obesity status, health, as well as perceptions of obesity-related health care. Mayo Clin Proc. (2021) 96:408–19. doi: 10.1016/j.mayocp.2020.05.049
15. Gunstad J, Paul RH, Spitznagel MB, Cohen RA, Williams LM, Kohn M, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Res. (2006) 142:31–7. doi: 10.1016/j.psychres.2005.11.007
16. Muennig P, Lubetkin E, Jia H, Franks P. Gender and the burden of disease attributable to obesity. Am J Public Health. (2006) 96:1662–8. doi: 10.2105/AJPH.2005.068874
17. Matud MP, Díaz A, Bethencourt JM, Ibáñez I. Stress and psychological distress in emerging adulthood: A gender analysis. J Clin Med. (2020) 9:2859. doi: 10.3390/jcm9092859
18. Rice F, Riglin L, Lomax T, Souter E, Potter R, Smith DJ, et al. Adolescent and adult differences in major depression symptom profiles. J Affect Disord. (2019) 243:175–81. doi: 10.1016/j.jad.2018.09.015
19. Hemmingsson E. Early childhood obesity risk factors: socioeconomic adversity, family dysfunction, offspring distress, and junk food self-medication. Curr Obes Rep. (2018) 7:204–9. doi: 10.1007/s13679-018-0310-2
20. Kaufman J, Martin A, King RA, Charney D. Are child-, adolescent-, and adult-onset depression one and the same disorder? Biol Psychiatry. (2001) 49:980–1001. doi: 10.1016/s0006-3223(01)01127-1
21. Polanka BM, Vrany EA, Patel J, Stewart JC. Depressive disorder subtypes as predictors of incident obesity in US adults: moderation by race/ethnicity. Am J Epidemiol. (2017) 185:734–42. doi: 10.1093/aje/kwx030
22. O’Neil A, Quirk SE, Housden S, Brennan SL, Williams LJ, Pasco JA, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health. (2014) 104:e31–42. doi: 10.2105/AJPH.2014.302110
23. Firth J, Gangwisch JE, Borisini A, Wootton RE, Mayer EA. Food and mood: how do diet and nutrition affect mental wellbeing? BMJ. (2020) 369:m2382. doi: 10.1136/bmj.m2382
24. Wärnberg J, Gomez-Martinez S, Romeo J, Díaz L, Marcos A. Nutrition, inflammation, and cognitive function. Ann N Y Acad Sci. (2009) 1153:164–75. doi: 10.1111/j.1749-6632.2008.03985.x
25. Kanoski SE, Davidson TL. Western diet consumption and cognitive impairment: links to hippocampal dysfunction and obesity. Physiol Behav. (2011) 103:59–68. doi: 10.1016/j.physbeh.2010.12.003
26. Noble EE, Hsu TM, Kanoski SE. Gut to brain dysbiosis: mechanisms linking western diet consumption, the microbiome, and cognitive impairment. Front Behav Neurosci. (2017) 11:9. doi: 10.3389/fnbeh.2017.00009
27. Bocchio-Chiavetto L, Bagnardi V, Zanardini R, Molteni R, Nielsen MG, Placentino A, et al. Serum and plasma BDNF levels in major depression: a replication study and meta-analyses. World J Biol Psychiatry Off J World Fed Soc Biol Psychiatry. (2010) 11:763–73. doi: 10.3109/15622971003611319
28. Molteni R, Barnard RJ, Ying Z, Roberts CK, Gómez-Pinilla F. A high-fat, refined sugar diet reduces hippocampal brain-derived neurotrophic factor, neuronal plasticity, and learning. Neuroscience. (2002) 112:803–14. doi: 10.1016/S0306-4522(02)00123-9
29. Steptoe A, Frank P. Obesity and psychological distress. Philos Trans R Soc Lond B Biol Sci. (2023) 378:20220225. doi: 10.1098/rstb.2022.0225
30. Lassale C, Batty GD, Baghdadli A, Jacka F, Sánchez-Villegas A, Kivimäki M, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry. (2019) 24:965–86. doi: 10.1038/s41380-018-0237-8
31. Kohler O, Krogh J, Mors O, Benros ME. Inflammation in depression and the potential for anti-inflammatory treatment. Curr Neuropharmacol. (2016) 14:732–42. doi: 10.2174/1570159X14666151208113700
32. KopsChina Feltes P, Doorduin J, Klein HC, Juárez-Orozco LE, Dierckx RA, Moriguchi-Jeckel CM, et al. Anti-inflammatory treatment for major depressive disorder: implications for patients with an elevated immune profile and non-responders to standard antidepressant therapy. J Psychopharmacol Oxf Engl. (2017) 31:1149–65. doi: 10.1177/0269881117711708
33. Bentley T, Widom CS. A 30-year follow-up of the effects of child abuse and neglect on obesity in adulthood. Obes Silver Spring Md. (2009) 17:1900–5. doi: 10.1038/oby.2009.160
34. Fu X, Wang Y, Zhao F, Cui R, Xie W, Liu Q, et al. Shared biological mechanisms of depression and obesity: focus on adipokines and lipokines. Aging. (2023) 15:5917–50. doi: 10.18632/aging.204847
35. Zajkowska Z, Gullett N, Walsh A, Zonca V, Pedersen GA, Souza L, et al. Cortisol and development of depression in adolescence and young adulthood - a systematic review and meta-analysis. Psychoneuroendocrinology. (2022) 136:105625. doi: 10.1016/j.psyneuen.2021.105625
36. Lanza HI, Grella CE, Chung PJ. Adolescent obesity and future substance use: Incorporating the psychosocial context. J Adolesc. (2015) 45:20–30. doi: 10.1016/j.adolescence.2015.08.014
37. Fatima Y, Doi SAR, Mamun AA. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. (2016) 17:1154–66. doi: 10.1111/obr.v17.11
38. Jackson CL. Determinants of racial/ethnic disparities in disordered sleep and obesity. Sleep Health. (2017) 3:401–15. doi: 10.1016/j.sleh.2017.08.001
39. Araghi MH, Jagielski A, Neira I, Brown A, Higgs S, Thomas GN, et al. The complex associations among sleep quality, anxiety-depression, and quality of life in patients with extreme obesity. Sleep. (2013) 36:1859–65. doi: 10.5665/sleep.3216
40. O’Leary K, Bylsma LM, Rottenberg J. Why might poor sleep quality lead to depression? A role for emotion regulation. Cognit Emot. (2017) 31:1698–706. doi: 10.1080/02699931.2016.1247035
41. Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: A longitudinal epidemiological study of young Adults. Biol Psychiatry. (1996) 39:411–8. doi: 10.1016/0006-3223(95)00188-3
42. Bruce ES, Lunt L, McDonagh JE. Sleep in adolescents and young adults. Clin Med Lond Engl. (2017) 17:424–8. doi: 10.7861/clinmedicine.17-5-424
43. Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. (2004) 27:661–6. doi: 10.1093/sleep/27.4.661
44. Meyer KA, Wall MM, Larson NI, Laska MN, Neumark-Sztainer D. Sleep duration and BMI in a sample of young adults. Obesity. (2012) 20:1279–87. doi: 10.1038/oby.2011.381
45. Steptoe A. Sleep duration and health in young adults. Arch Intern Med. (2006) 166:1689. doi: 10.1001/archinte.166.16.1689
46. Abate KH. Gender disparity in prevalence of depression among patient population: a systematic review. Ethiop J Health Sci. (2013) 23:283–8. doi: 10.4314/ejhs.v23i3.11
47. Sattler KM, Deane FP, Tapsell L, Kelly PJ. Gender differences in the relationship of weight-based stigmatisation with motivation to exercise and physical activity in overweight individuals. Health Psychol Open. (2018) 5:2055102918759691. doi: 10.1177/2055102918759691
48. Weismann J, Pratt L, Miller E, Parker J. Serious Psychological Distress Among Adults: United States, 2009-2013. NCHS Data Brief (2015) 203:1–8. Available online at: https://stateofchildhoodobesity.org/demographic-data/ages-10-17/:~:text=In%202021%2D2022%2C%20Non%2D,Alaska%20Native%20(21.4%25)%20children.
49. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
50. Rohde P, Beevers CG, Stice E, O’Neil K. Major and minor depression in female adolescents: onset, course, symptom presentation, and demographic associations. J Clin Psychol. (2009) 65:1339–49. doi: 10.1002/jclp.v65:12
51. Daee A, Robinson P, Lawson M, Turpin JA, Gregory B, Tobias JD. Psychologic and physiologic effects of dieting in adolescents. South Med J. (2002) 95:1032–41. doi: 10.1097/00007611-200295090-00016
52. Potter B, Pederson L, Chan S, Aubut JA, Koval J. Does a relationship exist between body weight, concerns about weight, and smoking among adolescents? An integration of the literature with an emphasis on gender. Nicotine Tob Res. (2004) 6:397–425. doi: 10.1080/14622200410001696529
53. Li L, Gower BA, Shelton RC, Wu X. Gender-specific relationship between obesity and major depression. Front Endocrinol. (2017) 8:292. doi: 10.3389/fendo.2017.00292
54. Anderson SE, Cohen P, Naumova EN, Jacques PF, Must A. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosom Med. (2007) 69:740–7. doi: 10.1097/PSY.0b013e31815580b4
55. Blasco BV, García-Jiménez J, Bodoano I, Gutiérrez-Rojas L. Obesity and depression: its prevalence and influence as a prognostic factor: A systematic review. Psychiatry Investig. (2020) 17:715–24. doi: 10.30773/pi.2020.0099
56. Tsai SA, Lv N, Xiao L, Ma J. Gender differences in weight-related attitudes and behaviors among overweight and obese adults in the United States. Am J Mens Health. (2016) 10:389–98. doi: 10.1177/1557988314567223
57. Himmelstein MS, Puhl RM, Quinn DM. Weight stigma and health: The mediating role of coping responses. Health Psychol Off J Div Health Psychol Am Psychol Assoc. (2018) 37:139–47. doi: 10.1037/hea0000575
58. Himmelstein MS, Puhl RM, Quinn DM. Overlooked and understudied: health consequences of weight stigma in men. Obesity. (2019) 27:1598–605. doi: 10.1002/oby.v27.10
59. Hand WB, Robinson JC, Stewart MW, Zhang L, Hand SC. The identity threat of weight stigma in adolescents. West J Nurs Res. (2017) 39:991–1007. doi: 10.1177/0193945917704201
60. Cossrow N, Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J Clin Endocrinol Metab. (2004) 89:2590–4. doi: 10.1210/jc.2004-0339
61. Brody D, Pratt L, Hughes J. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief. (2018) 303:1–8.
62. Williams DR. Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav. (2018) 59:466–85. doi: 10.1177/0022146518814251
63. Wallace AE, Young-Xu Y, Hartley D, Weeks WB. Racial, socioeconomic, and rural–urban disparities in obesity-related bariatric surgery. Obes Surg. (2010) 20:1354–60. doi: 10.1007/s11695-009-0054-x
64. Lu W. Adolescent depression: national trends, risk factors, and healthcare disparities. Am J Health Behav. (2019) 43:181–94. doi: 10.5993/AJHB.43.1.15
65. Eberly LA, Yang L, Essien UR, Eneanya ND, Julien HM, Luo J, et al. Racial, ethnic, and socioeconomic inequities in glucagon-like peptide-1 receptor agonist use among patients with diabetes in the US. JAMA Health Forum. (2021) 2:e214182. doi: 10.1001/jamahealthforum.2021.4182
66. Sliwa SA, Must A, Peréa FC, Boulos RJ, Economos CD. Occupational physical activity and weight-related outcomes in immigrant mothers. Am J Prev Med. (2016) 51:637–46. doi: 10.1016/j.amepre.2016.04.017
67. Lee M, Bhimla A, Ma GX. Depressive symptom severity and immigration-related characteristics in Asian American immigrants. J Immigr Minor Health. (2020) 22:935–45. doi: 10.1007/s10903-020-01004-7
68. Zhang L, Bo A, Lu W. To unfold the immigrant paradox: maltreatment risk and mental health of racial-ethnic minority children. Front Public Health. (2021) 9:619164. doi: 10.3389/fpubh.2021.619164
69. Baker EH, Rendall MS, Weden MM. Epidemiological paradox or immigrant vulnerability? Obesity among young children of immigrants. Demography. (2015) 52:1295–320. doi: 10.1007/s13524-015-0404-3
70. McCullough MB, Marks AK. The immigrant paradox and adolescent obesity: examining health behaviors as potential mediators (DO NOT HAVE ACCESS). J Dev Behav Pediatr. (2014) 35:138–43. doi: 10.1097/DBP.0000000000000027
71. Afable A, Ursua R, Wyatt LC, Aguilar D, Kwon SC, Islam NS, et al. Duration of US residence is associated with overweight risk in Filipino immigrants living in New York Metro Area. Fam Community Health. (2016) 39:13–23. doi: 10.1097/FCH.0000000000000086
72. Lindsay AC, Greaney ML, Wallington SF, Wright JA, Hunt AT. Depressive symptoms and length of U.S. Residency are associated with obesity among low-income latina mothers: A cross-sectional analysis. Int J Environ Res Public Health. (2017) 14:869. doi: 10.3390/ijerph14080869
73. Commodore-Mensah Y, Ukonu N, Obisesan O, Aboagye JK, Agyemang C, Reilly CM, et al. Length of residence in the United States is associated with a higher prevalence of cardiometabolic risk factors in immigrants: A contemporary analysis of the national health interview survey. J Am Heart Assoc. (2016) 5:e004059. doi: 10.1161/JAHA.116.004059
74. Zare H, Meyerson NS, Nwankwo CA, Thorpe RJ. How income and income inequality drive depressive symptoms in U.S. Adults, does sex matter: 2005-2016. Int J Environ Res Public Health. (2022) 19:6227. doi: 10.3390/ijerph19106227
75. Jalla R, Baral D, Pithadia D. Social determinants of mental health in adolescents and young adults in western nations – a literature review. Int J Ment Health Psychiatry (2020) 6:3. doi: 10.37532/ijmhp.2020.6(3).181
76. Alegría M, NeMoyer A, Falgàs Bagué I, Wang Y, Alvarez K. Social determinants of mental health: where we are and where we need to go. Curr Psychiatry Rep. (2018) 20:95. doi: 10.1007/s11920-018-0969-9
77. Shim RS, Ye J, Baltrus P, Fry-Johnson Y, Daniels E, Rust G. Racial/ethnic disparities, social support, and depression: examining a social determinant of mental health. Ethn Dis. (2012) 22:15–20.
78. Javed Z, Valero-Elizondo J, Maqsood MH, Mahajan S, Taha MB, Patel KV, et al. Social determinants of health and obesity: Findings from a national study of US adults. Obesity. (2022) 30:491–502. doi: 10.1002/oby.23336
79. Rabbitt MP, Hales LJ, Burke MP, Coleman-Jensen A. Household Food Security in the United States in 2022 (Report No. ERR-325), U.S. Department of Agriculture. Economic Research Service (2023).
80. Ferris WF, Crowther NJ. Once fat was fat and that was that: our changing perspectives on adipose tissue. Cardiovasc J Afr. (2011) 22:147–54. doi: 10.5830/CVJA-2010-083
81. Sumińska M, Podgórski R, Bogusz-Górna K, Skowrońska B, Mazur A, Fichna M. Historical and cultural aspects of obesity: From a symbol of wealth and prosperity to the epidemic of the 21st century. Obes Rev. (2022) 23:e13440. doi: 10.1111/obr.13440
82. Carvajal-Aldaz D, Cucalon G, Ordonez C. Food insecurity as a risk factor for obesity: A review. Front Nutr. (2022) 9:1012734. doi: 10.3389/fnut.2022.1012734
Keywords: obesity, depression, psychological distress (PD), young adults, cardiovascular health, social determinants of health (SDOH), mental health
Citation: Friedman M, Chang R, Amin ZM, Rajan T, Singh R, Yousefzai S, Shahid I, Nasir K and Javed Z (2025) Understanding the bidirectional association between obesity and risk of psychological distress and depression in young adults in the US: available evidence, knowledge gaps, and future directions. Front. Psychiatry 15:1422877. doi: 10.3389/fpsyt.2024.1422877
Received: 05 June 2024; Accepted: 16 December 2024;
Published: 10 January 2025.
Edited by:
Don Byrne, Australian National University, AustraliaReviewed by:
Britta Stapel, Hannover Medical School, GermanyCopyright © 2025 Friedman, Chang, Amin, Rajan, Singh, Yousefzai, Shahid, Nasir and Javed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael Friedman, bWljaGFlbGZAd3VzdGwuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.