- 1Operating Room, Henan Provincial People’s Hospital, Zhengzhou, China
- 2School of Medicine, Zhengzhou University of Industrial Technology, Zhengzhou, China
- 3Department of Oncology, Zhongda Hospital, Southeast University, Nanjing, China
- 4School of Nursing, Xinxiang Medical University, Xinxiang, China
- 5The First Affiliated Hospital of Zhengzhou University, Zhengzhou University, Zhengzhou, China
- 6Department of Rehabilitation, Henan Vocational College of Tuina, Zhengzhou, China
- 7Traditional Chinese Medicine Department, The Third People’s Hospital of Henan Province, Zhengzhou, China
- 8Nursing Department, The Third People’s Hospital of Henan Province, Zhengzhou, China
- 9Ultrasound Department, Sanmenxia Central Hospital, Sanmenxia, China
- 10Department of Nursing, Shenzhen Hospital of Integrated Traditional Chinese and Western Medicine, Shenzhen, China
Objective: The present study aims to investigate the levels of illness uncertainty in patients with moyamoya disease and to determine the association of socio-demographic characteristics, perceived social support and resilience with illness uncertainty in patients with moyamoya disease.
Method: A cross-sectional survey using convenience sampling was conducted in two hospitals in China from August to December 2023. A socio-demographic characteristics questionnaire, the Chinese versions of Mishel’s Unsurety in Disease Scale (MUIS), the Chinese version of Connor-Davidson Resilience Scale (CD-RISC), and the Chinese version of Multidimensional Scale of Perceived Social Support (MSPSS) were used to perform this research. The collected data were analyzed using SPSS 24.0 statistical software. The t-test, one-way analysis of variance (ANOVA), pearson correlation analysis and hierarchical regression analysis were used to identify associated factors.
Result: A total of 263 patients with moyamoya disease were recruited in this survey. The score of illness uncertainty was at a moderate level of (100.03 ± 18.59). The present study identified a negative correlation between illness uncertainty with resilience perceived social support. Hierarchical regression analysis showed that gender, occupation, education level, resilience and perceived social support were the related factors of illness uncertainty.
Conclusion: Patients with moyamoya disease experienced moderate disease uncertainty on average, which was related to gender, occupation, education level, resilience and perceived social support. Future research is needed to better explore the complex relationships between illness uncertainty, resilience, and perceived social support with different types of moyamoya disease using longitudinal research.
1 Introduction
Moyamoya disease (MMD) is a specific chronic cerebrovascular occlusive disease first reported by Japanese surgeons in 1957 (1). It is named for the smoke-like cerebrovascular morphology observed during cerebral angiography in the skull base (2). There are regional differences in the incidence of moyamoya disease worldwide. Studies have shown that the MMD is more prevalent in Japan and East Asia, while it is less common in European and North American populations. For example, the annual incidence in East Asian countries ranges from 0.5 to 1.5 per 100,000 people, compared to as low as 0.1 per 100,000 people in North America (3). In East Asia, the incidence rates also varies among countries. Japan and South Korea specifically have reported incidence rates of 0.94/100,000 and 2.3/100,000, respectively (4). In China, several epidemiological studies have also been conducted. A study conducted in Taiwan reported that the average incidence rate of MMD was 0.15/100000 (5). In the epidemiological study of Nanjing, the incidence rate from 2000 to 2007 was 3.92/100000 (6), lower than that of South Korea and Japan in general. However, national epidemiological studies of MMD in mainland China seem to have not yet been carried out.
MMD may present a series of clinical symptoms, including transient ischemic attack, ischemic stroke, hemorrhagic stroke, epilepsy, headache and cognitive impairment (7). The severity and progression of the disease may vary depending on the age of onset of symptoms and the type of first attack. MMD in children is mostly manifested as progressive cerebral ischemia, while adults with MMD is mostly manifested as cerebral ischemia and hemorrhage (8). It has also been found that even asymptomatic MMD patients may have cognitive impairments, particularly in areas such as intelligence, spatial ability, verbal working memory, and numerical operations (9). MMD and its complications bring not only physical damage to patients, but also great psychological challenges (10). A study showed that 46.7% of MMD patients were diagnosed with depression, 50% with anxiety, and 47.5% with post-traumatic stress disorder (11). The psychological problems caused by these diseases undoubtedly greatly affect the quality of life of patients (12). Therefore, for patients with MMD, it is not enough to only receive medical treatment for physiological diseases. It is necessary to conduct relevant researches on the mental health problems of MMD patients.
Illness uncertainty refers to the ambiguity and anxiety individuals experience due to unpredictable aspects of their health condition, commonly observed in cancer and chronic disease cohorts. It is also associated with depression and reduced quality of life in individuals with chronic illnesses (13). This uncertainty, stemming from the unpredictable trajectory and treatment outcomes of chronic and life-threatening diseases, also leads to reduced compliance with treatment regimens. Consequently, this not only undermines the effectiveness of therapeutic interventions but also adversely affects the overall prognosis of such conditions (14). Exploring the associated factors of illness uncertainty is therefore critical in improving patient outcomes and ensuring a more holistic approach to the management of chronic diseases like MMD.
Resilience is an individual’s ability to adapt and cope with adversity while maintaining well-being (15). It involves the development of skills and support systems for effective management and recovery, as well as the capacity to recover from traumatic experiences. Resilience serves as a buffer against stress and enhances one’s ability to manage stress, confront challenges, develop coping strategies, and adapt to changing circumstances (16, 17). Initially introduced by Block, the concept of resilience includes traits such as intelligence, strength, and adaptability that individuals display in response to ever-changing needs (18). These traits are considered protective factors. Patients with MMD require focused attention due to their unique psychological needs. However, research on resilience and its correlation with uncertainty in illness in patients with MMD seems to be rare. Fortunately, some related studies (19) have been conducted on stroke, which belongs to the same cerebrovascular disease as MMD, and their findings have certain reference value for us.
Perceived social support is a complex, multidimensional concept characterized by reciprocity, encompassing social, psychological, and material assistance an individual receipted from social networks (20). In other words, it refers to the help provided by family, friends, and significant others, playing a crucial role in directly and indirectly reducing illness uncertainty. The social support needs of patients are diverse and largely depend on the tasks they are facing at the time (21). Social support is closely related to the prognosis of patients with MMD. A study have found that illness uncertainty among patients with MMD decreases their quality of life, while a higher level of social support can improve their quality of life (22). In addition, it has been suggested that higher social support level is associated with lower illness uncertainty (23). This finding has been replicated in other populations of patients with chronic diseases (24, 25).
Therefore, although the study of illness uncertainty is very important for MMD patients, and relevant studies have also confirmed that resilience and perceived social support are related to illness uncertainty. However, there seems to be a lack of relevant research on the status quo of illness uncertainty in MMD patients. The relationship between resilience, perceived social support and illness uncertainty in MMD patients is not clear. Further research is needed to fill this gap. So, the present study aims to investigate the levels of illness uncertainty in MMD patients and to determine the association of socio-demographic characteristics, perceived social support and resilience with illness uncertainty in MMD patients. This would be of great benefit in understanding the mental state of MMD patients and provide valuable insights into future intervention strategies for MMD patients.
2 Methods
2.1 Study design
A cross-sectional (26) exploratory survey method was used in this study, because this research method has been widely used to investigate the current status of psychological indicators such as illness uncertainty (27), perceived social support (28) and resilience (29) of patients. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline was followed for this study.
2.2 Participants
The sample size of this study was calculated according to the sample size calculation principle used in Kendall’s cross-sectional investigation (30), n = independent variable × (5~10). Four scales with 17 independent variables were used in this study. The 17 independent variables were derived from the socio-demographic characteristics questionnaire (including age, gender, marriage status, religious faith, average monthly income, occupation and education level), the Chinese Version of Mishel Uncertainty in Illness Scale (including 3 dimensions), the Chinese Version of Connor–Davidson Resilience Scale (including 4 dimensions) and the Chinese Version of Multidimensional Scale of Perceived Social Support (including 3 dimensions). Considering the 20% invalid questionnaires, the minimum sample size required for this study was 107to 213.
Participants were recruited using convenience sampling from two tertiary hospitals in Zhengzhou, Henan province, China. The inclusion criteria for participants were as follows: (1) older than 18 years old; (2) moyamoya disease or unilateral moyamoya disease diagnosed by a clinician according to the criteria set by the Neuroradiology Committee (31); (3) patients had no history of psychiatry illness; (4) patients have the ability to understand the questionnaire content and complete the questionnaire independently; and (5) participating in this study voluntarily. On the other hand, the exclusion criteria for participants were: (1) patients with cerebral hemorrhage, stroke, hemangioma and other cerebrovascular diseases; (2) patients have history of intracranial surgery or trauma; (3) patients have basic diseases such as hypertension, diabetes or infection, and the condition has not been effectively controlled; and (4) patients have serious cognitive dysfunction.
2.3 Instruments
2.3.1 Socio-demographic characteristics questionnaire
We used a self-designed questionnaire to collect participants’ socio-demographic characteristics. All of the information gathered for this section was objective. The socio-demographic characteristics questionnaire included 7 questions. The 7 questions were gender, age, marriage status, religious faith, average monthly income, occupation and education level.
2.3.2 The Chinese Version of Mishel Uncertainty in Illness Scale
This scale developed by American nursing expert Mishel (32)based on the theory of disease uncertainty. The Chinese Version of uncertainty in illness scale translated by Zengjie Ye (33) et al. It is often used to measure illness uncertainty in patients with chronic diseases (e.g., breast cancer, stroke, etc.) in previous studies (34). This scale consists of 33 items, which fit into four different dimensions: uncertainty, lack of information, complexity and unpredictability. All the items in this study were scored by the Likert 5 method (1= strongly disagree, 5 = strongly agree). The total scores ranged from 32 to 160. In one previous study, the degree of illness uncertainty of patients was graded according to the score, respectively 32.0~74.7 being low, 74.8~117.4 being moderate and 117.5~160.0 being high (32). The higher the score was, the higher the uncertainty in illness was. In the present study, the Cronbach’s α of this scale is 0.85.
2.3.3 The Chinese Version of Connor-Davidson Resilience Scale
This scale was developed by Wagnild (35) et al. and used to examine the resilience of the participants. The Chinese Version of Connor-Davidson Resilience Scale was translated by Xiaonan Yu (36) et al. And it’s reliability and validity were verified, which showed that were acceptable. There are 25 items included in this scale. The scale is self-rated on a 5-point Likert scale with 0 = almost never and 4 = always. The final score of the scale is the sum of the item scores, with a higher total score indicating a higher level of resilience among the participants. In the present study, the Cronbach’s α of this scale was 0.97.
2.3.4 The Chinese version multidimensional scale of perceived social support
The Chinese version multidimensional scale of perceived social support developed to assess perceived social support from different sources in a Chinese population (37). The scale was developed by Zimet (38) et al. in 1988 and contains 12 items and three dimensions, namely family support, friends support, and significant others, with four items in each dimension. The scale uses a 7-point Likert scale (1= strongly disagree, 7= strongly agree). The scale’s total scores range from 12 to 84, where higher numbers correspond to higher perceptions of social support. The English version was first administered to American college students before being used in related studies on perceived social support in various nations and communities. Research has demonstrated the scale’s strong validity and reliability (39–41). In this study, the Chinese Version Multidimensional Perceived Social Support Scale translated by Qianjin Jiang (42) et al. was used. Multiple studies (43, 44) have confirmed that the Chinese version scale has good reliability and validity. In the present study, the Cronbach’s α of this scale was 0.97.
2.4 Data collection
A cross-sectional survey using convenience sampling was conducted in China. Data collection conducted from August to December 2023 at two tertiary hospitals in Henan province, China. Researchers personally distributed questionnaires to the participants, who answered it in private in a quiet conference room. This questionnaire consisted of four scales, including socio-demographic characteristics questionnaire, Chinese Version of Mishel’s Unsurety in Disease Scale (MUIS-A), the Chinese Version of 10-item Connor-Davidson Resilience Scale (CD-RISC-10), and the Chinese Version Multidimensional Scale of Perceived Social Support (MSPSS). The questionnaire was filled out anonymously, and the disclosure of participants’ identity (name, address, etc.) was not involved in the questionnaire. After participants completed the answer, the person in charge verified the integrity of the answer. Two researchers independently collected paper questionnaires and input them into a computer; the causes of the differences were identified and resolved in a timely manner. Participants were recruited from outpatient clinics and inpatient wards at both hospitals. Eligible participants were briefed about the study objectives and provided with information regarding their rights as participants. Participants were assured of the confidentiality and anonymity of their responses, and data were securely stored and accessible only to the research team. Ethical approval for the study was obtained from the institutional review board before investigation, and written informed consent was obtained from each participant.
2.5 Data analysis
Descriptive statistics (i.e., frequencies, percentages, means, SD) were calculated to describe MMD demographics, illness uncertainty, resilience and perceived social support. Two-sided t-test and one-way analysis of variance (ANOVA) were used to examine difference of illness uncertainty scores among multiple variables. Pearson correlation analysis was calculated to examine associations between illness uncertainty, resilience and perceived social support. First, categorical variables were set as dummy variables. Then a hierarchical multiple regression with 3 consecutive steps was used to detect factors associated with illness uncertainty. Step 1 includes socio-demographic variables. In step 2, we examined the association of illness uncertainty with resilience, after controlling for socio-demographic variables. In steps 3, the association between perceived social support and illness uncertainty was tested after controlling for socio-demographic variables and resilience. At each step, each variable was entered into the hierarchical regression model using the enter method. Before conducting the regression analysis, collinearity tests was incorporated. All analyses were performed using SPSS 24.0 (SPSS/IBM, Armonk, NY, United States), and a P <0.05 was considered statistically significant.
2.6 Ethical considerations
Ethical approval for this study was obtained from the third People’s Hospital of Henan Province in Zhengzhou, China (Ethical Review NO.: 2024-SZSYKY-002). Prior to data collection, informed consent was obtained from all participants, who were provided with both oral and written explanations of the purpose and procedures of the study. Participants were fully informed that their participation was voluntary and that they could withdraw from the study at any length.
To ensure confidentiality and anonymity, no identifying information, such as names, was collected. At the same time, each questionnaire was numbered, and participants were provided with a corresponding number on a debriefing sheet. This allowed for the maintenance of confidentiality throughout the study. Additionally, participants were informed that they could choose to withdraw their data prior to data analysis by contacting the researcher. Furthermore, all collected data were stored securely. Paper questionnaires were kept in a locked cupboard, while electronic data were stored on a password-protected computer. These measures were implemented to ensure the privacy and security of participants’ information.
3 Results
3.1 Socio-demographic characteristics of the participants
A total of 400 participants were invited to participate in this study, and only 271 of them agreed to participate in this study, but six of them had incomplete questionnaires, and two of them did not fill in the questionnaires. Finally, only 263 valid questionnaires were collected, and the effective recovery rate was 87.7%. Of the 263 participants, the majority were female, with 135 participants being female, accounting for 51.3% of the total participants. Regarding age distribution, participants aged 40 to 49 years constituted the largest group, comprising 42.5%. In terms of occupation, the largest group was composed of workers, with 102 individuals, accounting for 38.78% of the total. Among the participants in this study, 218 were married, accounting for 82.8% of the total number. There were 207 people without religious faith, accounting for 78.7% of the total. The average monthly income of most participants ranged from 3,000 yuan to 5,000 yuan (56.2%). As for profession, the largest group is workers, with 102 people, accounting for 38.78% of the total. Among the participants in this study, the highest number of junior high school students was 98, accounting for 37.26% of the total. After t-test and ANOVA analysis, the outcomes showed that the patient’s uncertainty score had statistically significant differences in gender, age, occupation and education level (P<0.05). In contrast, there were no statistically significant differences in marriage, religious faith, and average monthly income (P>0.05). See Table 1 for details.
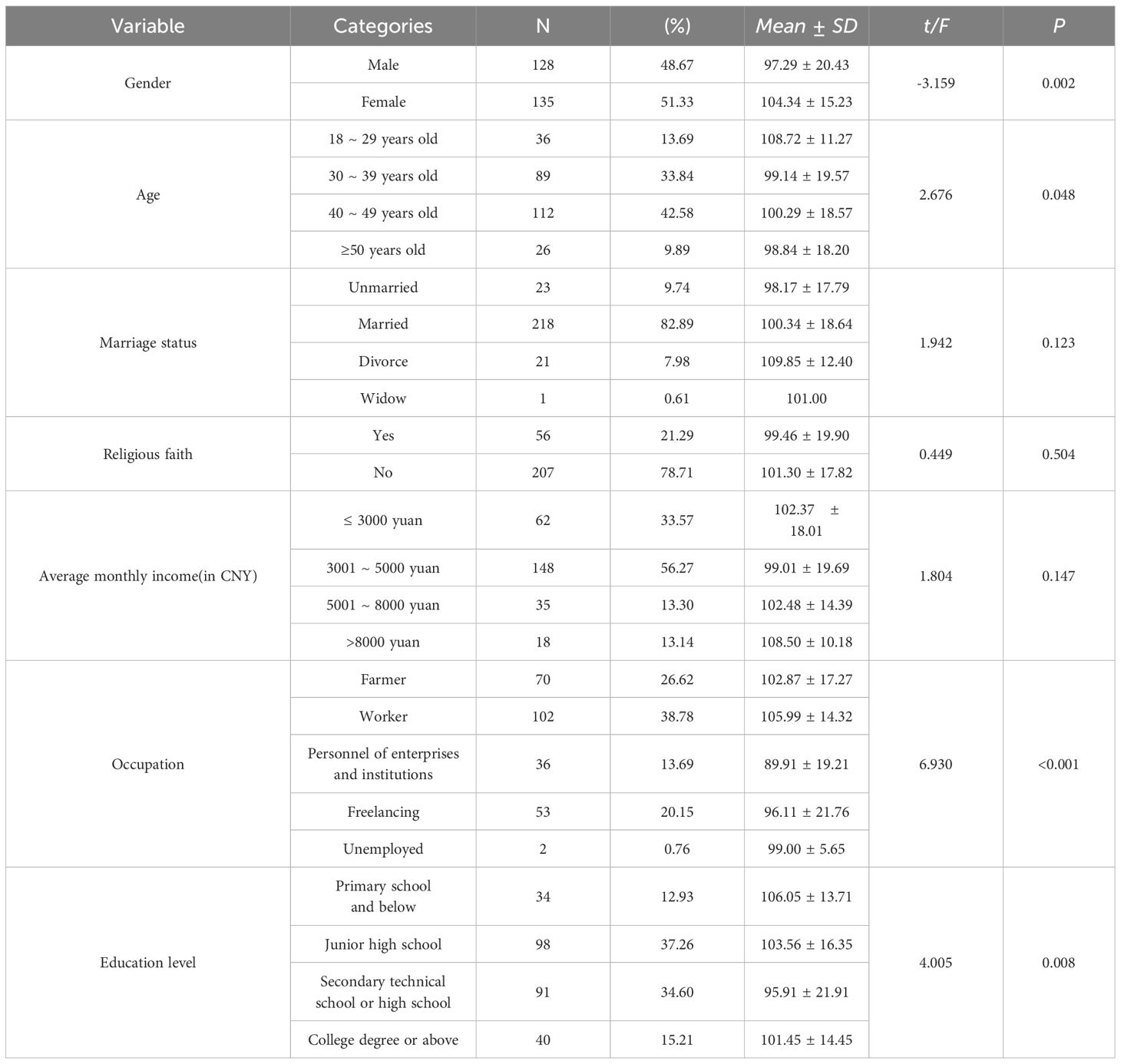
Table 1 Social-demographic characteristics of participants and comparison of different variables on illness uncertainty (N = 263).
3.2 Correlation between the status of illness uncertainty, resilience, and perceived social support in patients with MMD
According to pearson correlation analysis, illness uncertainty was significantly negatively correlated with resilience (r = -0.593, P = 0.000) and perceived social support (r =-0.599, P = 0.000). Further details can be found in Table 2.
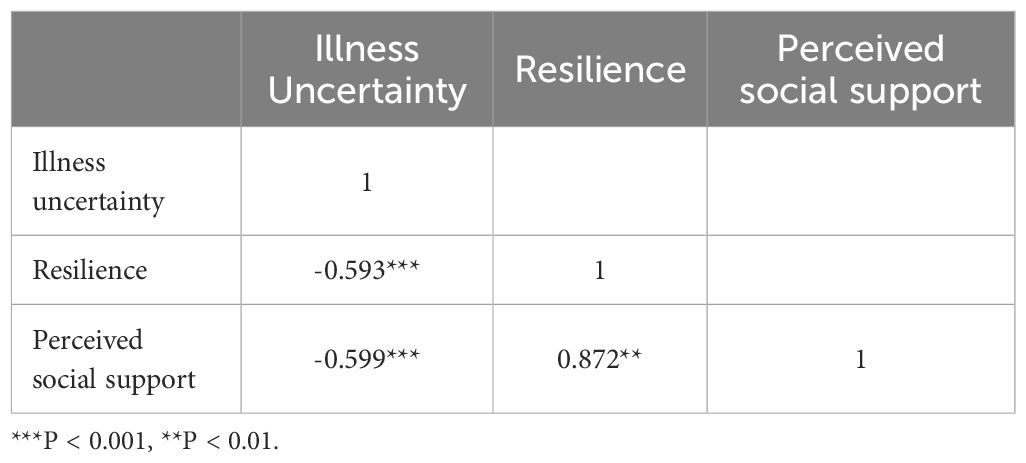
Table 2 Correlation between the illness uncertainty, resilience and perceived social support in MMD patients.
3.3 Multivariate hierarchical regression analysis of illness uncertainty
The results of the collinearity test showed that the tolerance of all variables was greater than 0.1, and the variance inflation factor (VIF) was less than 10, indicating that there was no multicollinearity between variables. As shown in Table 3, In step 1, the results showed that gender (β=0.200, P<0.001), age (β=0.156, P<0.001), occupation (β=3.276, P<0.01, β=5.678, P<0.001), and education level (β=2.538, P<0.05, β=2.367, P<0.05, β=2.500, P<0.05) were significantly correlated with the level of illness uncertainty. In step 2, after controlling for socio-demographic variables, the resilience score (β=-0.589, P<0.001) showed a negative correlation with disease uncertainty. In step 3, after controlling for demographic variables and resilience, the score of social support (β=-0.353, P<0.001) showed a significant negative correlation with disease uncertainty.
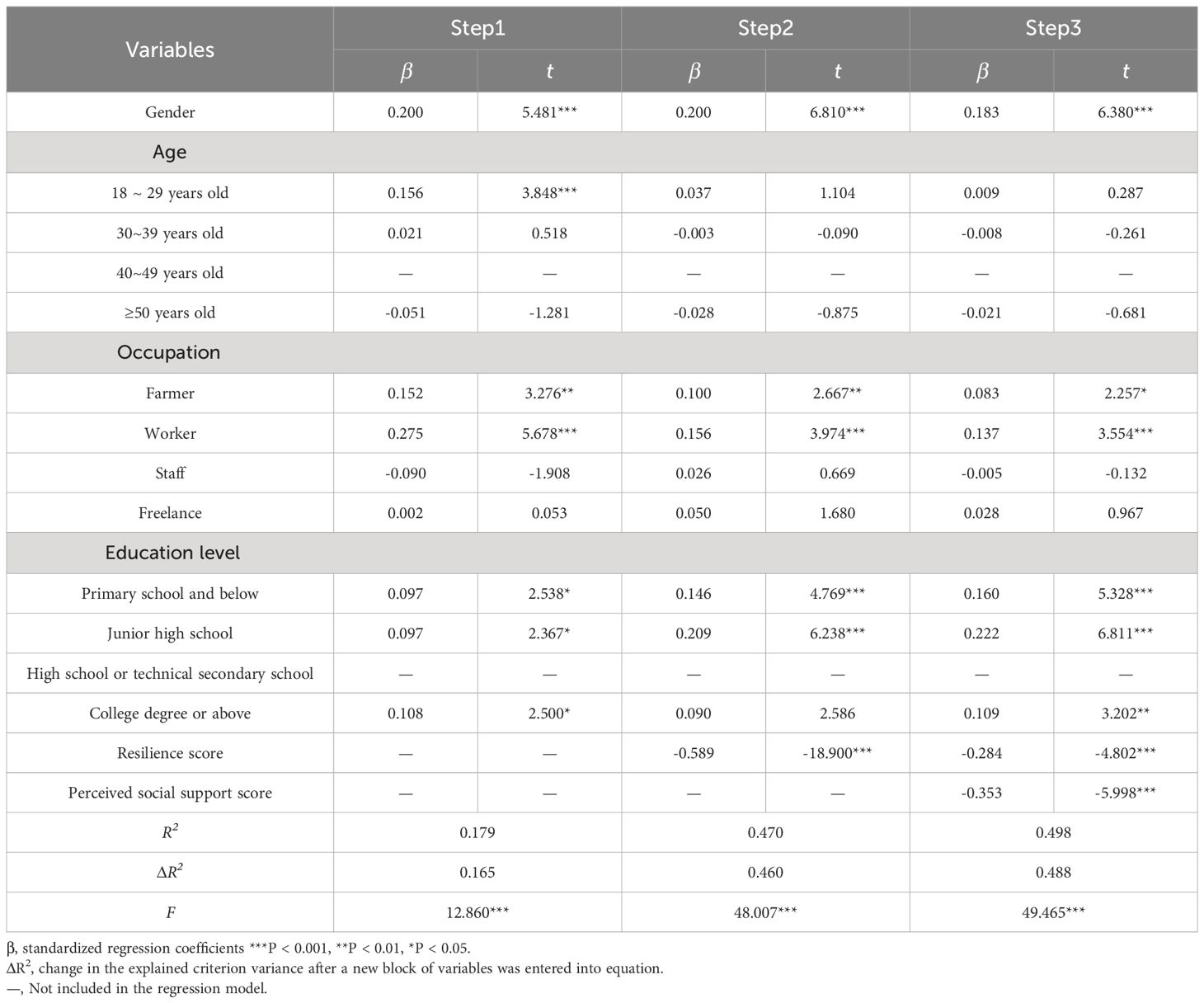
Table 3 Hierarchical regression analysis for factors associated with the illness uncertainty (N = 263).
4 Discussion
The present study aims to investigate the levels of illness uncertainty in MMD patients and to determine the association of socio-demographic characteristics, perceived social support and resilience with illness uncertainty in MMD patients. Therefore, we will follow the discussion in this order.
At present, there seems to be little relevant research in MMD patients. Most previous studies tend to focus on mental characters of cerebrovascular diseases patients in general, such as brain bleeds, stroke (45). Considering that MMD is also a kind of cerebrovascular disease, these research results focusing on cerebrovascular disease may have a certain reference for the current research.
The average score of illness uncertainty in MMD patients was (100.03 1008.59), which was at a moderate level. This result was similar to acute stroke patients (46). The reason for this may be that the high disability and mortality rates may increase the uncertainty of patients (47). McIntosh (48) has pointed out the ambiguity of patients regarding the occurrence, development, and prognosis of the disease greatly affects their uncertainty. What’s worse, as time goes by, patients’ concerns increase, thus increasing their sense of uncertainty, which may affect their psychological adjustment, treatment compliance and outlook on life.
The current study found that illness uncertainty of MMD patients was associated with gender. Specifically, female patients generally had higher disease uncertainty scores than male patients, which was consistent with the results of previous studies observed in other patients with chronic diseases (49, 50). This may be attributed to various factors, such as men’s psychological quality, coping strategies and social roles in dealing with diseases. In current Chinese society, many workers from the countryside. Also, the level of illness uncertainty was also related to the occupation of patients. In general, the illness uncertainty score of the workers was higher than that of the farmers, which was similar to another study results (51). The reason for this situation may be related to the social situation in China. These people no longer work as farmers and choose to work in the city itself may be due to the huge life pressure and economic burden they face, which leads to farming is no longer enough to support their daily expenses. Illness means the loss of main labor force of the family and the aggravation of economic burden. These factors make patients have more anxiety, and then produce a higher level of illness uncertainty (52).
What’s more, patients’ illness uncertainty scores were also observed to differ according to their education level, which was similar to previous studies (53, 54). According to the results of ANOVA analysis and the multiple hierarchical regression, scores of illness uncertainty of patients with different education levels showed that except for patients with secondary technical school or high school education levels, the patient ‘s education level was negatively correlated with the score of disease uncertainty, indicating that the higher the patient ‘s education level, the lower the score of disease uncertainty. The reason for this phenomenon may be that the higher the patient ‘s overall education level, the greater the ability and access to information may be (55).
The study found that MMD patients exhibited a moderate level of resilience, with an average score of (78.75 78.8.92), which was higher than a previous study conduct in elderly ischemic stroke patients. The reason for this difference may be due to the different types of diseases and the age of the study population. In addition, the results of this study exhibited a negative correlation between resilience and illness uncertainty, which indicating that the higher the resilience level of MMD patients, the lower the level of disease uncertainty. The results has been confirmed in other previous studies (56, 57). In addition, one study showed that resilience and disease uncertainty jointly affect sleep quality in female systemic lupus erythematosus patients (56). Another study revealed the elastic in emergency surgery patients disease play a mediating role between uncertainty and anxiety (58). Thus, resilience may play a protective role for patients in avoiding the negative effects arising from illness uncertainty. Future research may focus on cultivating tenacity to reduce the uncertainty in illness in patients with a negative influence on the patients.
We also found that the present study identified a negative correlation between illness uncertainty and perceived social support, which was a discovery that aligns with previous studies (59, 60). This suggests that higher levels of social support from family, friends, and healthcare professionals are associated with reduced illness uncertainty. Medical staff should work closely with patients’ families to provide support and information. Group activities and communication can also help address challenges and improve well-being for MMD patients. Healthcare professionals can make a significant impact on patients’ psychological well-being and overall quality of life.
5 Limitations
Although every effort has been made to better the design of this study, some limitations are unavoidable. First, the use of a convenience sampling method, while practical, may limit the representativeness of the sample. Second, the cross-sectional study design can only represent the psychological status of patients at the time of the study, but it cannot reflect the full and dynamic psychological changes of patients with the diagnosis of MMD. Future research could employ longitudinal designs for causal exploration. Third, reliance on self-reported data may introduce subjective and recall biases, potentially impacting assessment accuracy. The study’s sample was drawn exclusively from two hospitals in China, possibly limiting the generalizability of findings to other regions within the country. Further investigation in diverse organizational and cultural settings is warranted.
6 Conclusion
In this survey involving 263 MMD patients, illness uncertainty levels were found to be at a moderate level. Additionally, illness uncertainty exhibited negative correlations with resilience and perceived social support. Multiple linear regression analysis revealed that gender, working status, education level, smoking history, current residential status, diagnosis duration of MMD, total score of perceived social support, and total score of resilience were independent factors associated with illness uncertainty, collectively explaining a significant portion of its variance. These findings highlight the importance of greater attention and intervention for patients with underlying poor psychological status, while we observe that fostering resilience and giving patients adequate social support may have a positive effect on reducing the uncertainty of their illness and improving their overall well-being.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Author contributions
WZ: Conceptualization, Writing – original draft. ZP: Data curation, Writing – original draft. YZ: Data curation, Writing – original draft. DL: Conceptualization, Investigation, Validation, Writing – original draft. HZ: Investigation, Writing – original draft, Methodology, Validation. SL: Methodology, Writing – original draft. CL: Methodology, Writing – original draft. XX: Methodology, Writing – original draft. QL: Methodology, Writing – original draft. GY: Methodology, Writing – original draft. SHY: Methodology, Writing – original draft. RS: Methodology, Writing – original draft. SY: Writing – original draft, Supervision. DW: Supervision, Writing – original draft. ML: Investigation, Methodology, Writing – review & editing. HL: Data curation, Methodology, Supervision, Conceptualization, Formal analysis, Project administration, Validation, Investigation, Resources, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
Thanks to all participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Oka K, Yamashita M, Sadoshima S, Tanaka K. Cerebral haemorrhage in Moyamoya disease at autopsy. Virchows Archiv A. (1981) 392:247–61. doi: 10.1007/BF02155663
2. Pop NO, Zaha DC, Pantiş C, Mekeres F. Clinicopathological evaluation of Moyamoya disease. Case Rep Rev Literature Rom J Mil Med. (2020) 123:102–5. doi: 10.1007/BF00270611
3. Bang OY, Ryoo S, Kim SJ, Yoon CH, Cha J, Yeon JY, et al. Adult moyamoya disease: a burden of intracranial stenosis in East Asians? PloS One. (2015) 10:e0130663. doi: 10.1371/journal.pone.0130663
4. Patel SD, Desai N, Rane S, Patel N, Desai R, Mehta T, et al. Trends in hospitalizations and epidemiological characteristics of adults Moyamoya disorder in the United States. J Neurological Sci. (2020) 419:117165. doi: 10.1016/j.jns.2020.117165
5. Chen PC, Yang SH, Chien KL, Tsai IJ, Kuo MF. Epidemiology of moyamoya disease in Taiwan: a nationwide population-based study. Stroke. (2014) 45:1258–63. doi: 10.1161/STROKEAHA.113.004160
6. Miao W, Zhao PL, Zhang YS, Liu HY, Chang Y, Ma J, et al. Epidemiological and clinical features of Moyamoya disease in Nanjing, China. Clin Neurol Neurosurg. (2010) 112:199–203. doi: 10.1016/j.clineuro.2009.11.009
7. Hirano Y, Miyawaki S, Imai H, Hongo H, Ohara K, Dofuku S, et al. Association between the onset pattern of adult moyamoya disease and risk factors for stroke. Stroke. (2020) 51:3124–8. doi: 10.1161/STROKEAHA.120.030653
8. Fox BM, Dorschel KB, Lawton MT, Wanebo JE. Pathophysiology of vascular stenosis and remodeling in moyamoya disease. Front Neurol. (2021) 12:661578. doi: 10.3389/fneur.2021.661578
9. Hirano Y, Miyawaki S, Imai H, Hongo H, Teranishi Y, Dofuku S, et al. Differences in clinical features among different onset patterns in moyamoya disease. J Clin Med. (2021) 10:2815. doi: 10.3390/jcm10132815
10. Das S, Dubey S, Das S, Hazra A, Pandit A, Ghosh R, et al. Epidemiology of moyamoya angiopathy in Eastern India. Front Neurol. (2022) 13:837704. doi: 10.3389/fneur.2022.837704
11. Liu C, Yi X, Li T, Xu L, Hu M, Zhang S, et al. Associations of depression, anxiety and PTSD with neurological disability and cognitive impairment in survivors of moyamoya disease. Psychology Health Med. (2019) 24:43–50. doi: 10.1080/13548506.2018.1467024
12. Haas P, Fudali M, Wang SS, Hurth H, Hauser TK, Ernemann U, et al. Quality of life impairment in adult Moyamoya patients-preoperative neuropsychological assessment and correlation to MRI and H(2)(15)O PET findings. Neurosurgical Rev. (2022) 45:1533–41. doi: 10.1007/s10143-021-01660-9
13. Young AM, Ashbury FD, Schapira L, Scotté F, Ripamonti CI, Olver IN. Uncertainty upon uncertainty: supportive care for cancer and COVID-19. Supportive Care Cancer. (2020) 28:4001–4. doi: 10.1007/s00520-020-05604-9
14. Brown A, Hayden S, Klingman K, Hussey LC. Managing uncertainty in chronic illness from patient perspectives. J Excellence Nurs Healthcare Pract. (2020) 2:1. doi: 10.5590/JENHP.2020.2.1.01
15. Denckla CA, Cicchetti D, Kubzansky LD, Seedat S, Teicher MH, Williams DR, et al. Psychological resilience: an update on definitions, a critical appraisal, and research recommendations. Eur J Psychotraumatol. (2020) 11:1822064. doi: 10.1080/20008198.2020.1822064
16. Taylor MG, Carr D. Psychological resilience and health among older adults: A comparison of personal resources. Journals Gerontology: Ser B. (2021) 76:1241–50. doi: 10.1093/geronb/gbaa116
17. Süss H, Ehlert U. Psychological resilience during the perimenopause. Maturitas. (2020) 131:48–56. doi: 10.1016/j.maturitas.2019.10.015
18. Darabos K, Renna ME, Wang AW, Zimmermann CF, Hoyt MA. Emotional approach coping among young adults with cancer: Relationships with psychological distress, posttraumatic growth, and resilience. Psycho-Oncology. (2021) 30:728–35. doi: 10.1002/pon.5621
19. Choi M, Lee J, Oh EG, Chu SH, Sohn YH, Park CG. Factors associated with uncertainty in illness among people with parkinson's disease. Clin Nurs Res. (2020) 29:469–78. doi: 10.1177/1054773818788492
20. Modde Epstein C, Rice MJ, French JA, Kupzyk KA, Houfek JF. Social support buffers the effects of prenatal depressed mood: A mixed-methods study. J Am Psychiatr Nurses Assoc. (2024) 30:95–107. doi: 10.1177/10783903211073793
21. Li H, Lyu M, Wang A, Yin Y, Zhang J, Li P. Social support and life satisfaction in women with cervical cancer: A serial multiple mediation model. Cancer Nurs. (2024) 47:64–71. doi: 10.1097/NCC.0000000000001146
22. Oh W-O, Heo Y-J, Han J, Lee E. Analyzing symptom experiences and pathways to enhancing quality of life in adolescents with Moyamoya disease. J Pediatr Nurs. (2024) 75:72–9. doi: 10.1016/j.pedn.2023.12.007
23. Guan T, Guo P, Judge Santacroce S, Chen DG, Song L. Illness uncertainty and its antecedents for patients with prostate cancer and their partners. Oncol Nurs Forum. (2020) 47:721–31. doi: 10.1188/20.ONF.721-731
24. Li X, He L, Wang J, Wang M. Illness uncertainty, social support, and coping mode in hospitalized patients with systemic lupus erythematosus in a hospital in Shaanxi, China. PloS One. (2019) 14:e0211313. doi: 10.1371/journal.pone.0211313
25. Wang T, Sun J, Gu D, Shen S, Zhou Y, Wang Z. Dyadic effects of social support, illness uncertainty on anxiety and depression among lung cancer patients and their caregivers: a cross-sectional study. Supportive Care cancer: Off J Multinational Assoc Supportive Care Cancer. (2023) 31:402. doi: 10.1007/s00520-023-07876-3
26. Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. (2020) 158:S65–71. doi: 10.1016/j.chest.2020.03.012
27. Massazza A, Kienzler H, Al-Mitwalli S, Tamimi N, Giacaman R. The association between uncertainty and mental health: a scoping review of the quantitative literature. J Ment Health. (2023) 32:480–91. doi: 10.1080/09638237.2021.2022620
28. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
29. Fung S-f. Validity of the brief resilience scale and brief resilient coping scale in a Chinese sample. Int J Environ Res Public Health. (2020) 17:1265. doi: 10.3390/ijerph17041265
30. Zeng L, Chen Q, Fan S, Yi Q, An W, Liu H, et al. Factors influencing the professional identity of nursing interns: a cross-sectional study. BMC Nurs. (2022) 21:200. doi: 10.1186/s12912-022-00983-2
31. Kuroda S, Fujimura M, Takahashi J, Kataoka H, Ogasawara K, Iwama T, et al. Diagnostic criteria for moyamoya disease-2021 revised version. Neurologia Medico-chirurgica. (2022) 62:307–12. doi: 10.2176/jns-nmc.2022-0072
32. Mishel MH. The measurement of uncertainty in illness. Nurs Res. (1981) 30:258–63. doi: 10.1097/00006199-198109000-00002
33. Ye Z, Ying S, Liang M, Tish K, Jane D, Hu Q, et al. Revised Chinese Version of Mishel Uncertainty in Illness Scale: development, reliability and validity. Chin Gen Pract. (2018) 21:1091–7. doi: 10.3969/j.issn.1007-9572.2018.00.068
34. Guan T, Santacroce SJ, Chen DG, Song L. Illness uncertainty, coping, and quality of life among patients with prostate cancer. Psychooncology. (2020) 29:1019–25. doi: 10.1002/pon.5372
35. Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Measurement. (1993) 1:165–78.
36. Yu X, Zhang J. A comparison between the chinese version of ego-resiliency scale and connor-davidson resilience scale. psychol Sci. (2007) 30:3.
37. Chou K-L. Assessing Chinese adolescents’ social support: the multidimensional scale of perceived social support. Pers Individ Dif. (2000) 28:299–307. doi: 10.1016/S0191-8869(99)00098-7
38. Zimet GD, Dahlem NW, Zimet SG. The multidimensional scale of perceived social support: journal of personality assessment: vol 52, no 1. J Pers Assess. (1988) 52. doi: 10.1207/s15327752jpa5201_2
39. Pérez-Villalobos C, Briede-Westermeyer JC, Schilling-Norman MJ, Contreras-Espinoza S. Multidimensional scale of perceived social support: evidence of validity and reliability in a Chilean adaptation for older adults. BMC Geriatrics. (2021) 21:461. doi: 10.1186/s12877-021-02404-6
40. Kieu PT, Vuong NL, Dung DV. Validation of multidimensional scale of perceived social support (MSPSS) in Vietnamese among people living with HIV/AIDS. AIDS Behav. (2023) 27:2488–96. doi: 10.1007/s10461-022-03974-1
41. Boggatz T. Psychometric properties of the German version of the multidimensional perceived social support scale. Int J Older People Nurs. (2023) 18:e12540. doi: 10.1111/opn.12540
43. Mo Q, Tan C, Wang X, Soondrum T, Zhang J. Optimism and symptoms of anxiety and depression among Chinese women with breast cancer: the serial mediating effect of perceived social support and benefit finding. BMC Psychiatry. (2022) 22:635. doi: 10.1186/s12888-022-04261-y
44. Ng SSM, Liu TW, Ho LYW, Chan NH, Wong TWL, Tsoh J. Assessing the level of perceived social support among community-dwelling stroke survivors using the Multidimensional Scale of Perceived Social Support. Sci Rep. (2022) 12:19318. doi: 10.1038/s41598-022-23840-3
45. Zhang Y, Yu H, Ke C, Sun Q. Systematic review and meta-analysis of various risk factors of death from emergency cerebrovascular diseases in the department of neurology. Ann Palliat Med. (2021) 10:10661–73. doi: 10.21037/apm
46. Liu J, Wang H, Lin B, Ning L, Liu D, Li J. Mediating role of resourcefulness in the relationship between illness uncertainty and poststroke depression. Front Psychol. (2022) 13:852739. doi: 10.3389/fpsyg.2022.852739
47. Ni C, Peng J, Wei Y, Hua Y, Ren X, Su X, et al. Uncertainty of acute stroke patients: A cross-sectional descriptive and correlational study. J Neurosci nursing: J Am Assoc Neurosci Nurses. (2018) 50:238–43. doi: 10.1097/JNN.0000000000000373
48. Mackintosh NJ, Davis RE, Easter A, Rayment-Jones H, Sevdalis N, Wilson S, et al. Interventions to increase patient and family involvement in escalation of care for acute life-threatening illness in community health and hospital settings. Cochrane Database Systematic Rev. (2020) 12. doi: 10.1002/14651858.CD012829.pub2
49. Obispo B, Cruz-Castellanos P, Fernández-Montes A, Coca-Membribes S, Rogado J, Antoñanzas M, et al. Coping strategies as mediators of uncertainty and psychological distress in patients with advanced cancer. Psychooncology. (2023) 32:1694–701. doi: 10.1002/pon.6219
50. Bailey DE Jr., Yao J, Yang Q. Illness uncertainty in patients awaiting liver transplant. Western J Nurs Res. (2021) 43:509–16. doi: 10.1177/0193945920952059
51. Qin X, Ding S, Cui L, Chen Z. Status and influencing factors of uncertainty on illness among patients with type 2 diabetes. J Nurs Administration. (2017) 17:341–3. doi: 10.3969/j.issn.1671-315X.2017.05.014
52. Zhang D, Fan Z, Gao X, Huang W, Yang Q, Li Z, et al. Illness uncertainty, anxiety and depression in Chinese patients with glaucoma or cataract. Sci Rep. (2018) 8:11671. doi: 10.1038/s41598-018-29489-1
53. Jeon HO, Kim BH, Kim O. Illness uncertainty and complementary and alternative medicine use in patients undergoing hemodialysis. Nurs Health Sci. (2019) 21:375–81. doi: 10.1111/nhs.12609
54. Blake A, Asnani V, Leger RR, Harris J, Odesina V, Hemmings DL, et al. Stigma and illness uncertainty: adding to the burden of sickle cell disease. Hematol (Amsterdam Netherlands). (2018) 23:122–30. doi: 10.1080/10245332.2017.1359898
55. Qi W, Li H, Lian Q, Zuo X, Yu C, Lou C, et al. Knowledge level and access barriers related to sexual and reproductive health information among youth with disabilities in China: a cross-sectional study. Reprod Health. (2023) 20:84. doi: 10.1186/s12978-023-01625-9
56. Li T, Cui C, Li Y, Wang L. The impacts of resilience on the association between illness uncertainty and sleep quality among Chinese women with systemic lupus erythematosus. Clin Rheumatol. (2020) 39:1609–16. doi: 10.1007/s10067-019-04898-3
57. Friedman D, Kaskas MM, Quittner AL, Smith BA, Georgiopoulos AM. Patient engagement in the development of CF-CBT: A cystic fibrosis-specific cognitive-behavioral intervention for adults. Front Psychol. (2022) 13:937189. doi: 10.3389/fpsyg.2022.937189
58. Wu M, Dai S, Wang R, Yang S. The relationship between uncertainty and acute procedure anxiety among surgical patients in Chinese mainland: the mediating role of resilience. BMC Psychiatry. (2023) 23:796. doi: 10.1186/s12888-023-05315-5
59. Chen LW, Chou HH, Wang SY, Shih WM. Unmet care needs and uncertainty in patients newly diagnosed with breast cancer. Healthcare (Basel Switzerland). (2022) 10:341–3. doi: 10.3390/healthcare10112148
Keywords: illness uncertainty, resilience, perceived social support, MMD, moyamoya disease
Citation: Zhang W, Pan Z, Zhu Y, Lv D, Zhang H, Li S, Liu C, Xiong X, Li Q, Yao G, Yang S, Song R, Yan S, Wang D, Li M and Liu H (2024) Illness uncertainty, resilience, and perceived social support among patients with moyamoya disease: a cross-sectional study. Front. Psychiatry 15:1405594. doi: 10.3389/fpsyt.2024.1405594
Received: 23 March 2024; Accepted: 28 June 2024;
Published: 23 July 2024.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
André Luiz Monezi Andrade, Pontifical Catholic University of Campinas, BrazilXiaoXiao Mei, Hong Kong Polytechnic University, Hong Kong SAR, China
Siqing Chen, Zhejiang University, China
Zhihui Zhao, Wuhan University, China
Copyright © 2024 Zhang, Pan, Zhu, Lv, Zhang, Li, Liu, Xiong, Li, Yao, Yang, Song, Yan, Wang, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hanjiao Liu, liuhanjiao000@163.com; Meng Li, 1697912083@qq.com; Dongyang Wang, wangdongyang1994@gmail.com
†These authors have contributed equally to this work
 Wenling Zhang1†
Wenling Zhang1† Shen Li
Shen Li Qiong Li
Qiong Li Sumei Yan
Sumei Yan Dongyang Wang
Dongyang Wang Meng Li
Meng Li