- 1College of Medicine and Health Science, Woldia University, Woldia, Ethiopia
- 2Department of Clinical Pharmacy, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 3College of Medicine and Health Sciences, Samara University, Samara, Ethiopia
- 4Curtin School of Population Health, Curtin University, Perth, WA, Australia
Introduction: Resilience is the dynamic adaptive process of maintaining or recovering mental health from stressors, such as trauma, challenging life circumstances, critical transitions, or physical illnesses. Resilience after adversity can be fostered through protective factors and the implementation of interventions that promote resilience. Hence, it is essential to investigate both protective and vulnerable factors to reduce the negative effects of unfavorable life events and increase resilience through positive risk-response interventions.
Objective: To assess the effect of previous adversity, protecting factors, and resilience-promoting interventions to possess resilience after adversity in a global context.
Methods: The study included English language articles sourced from PubMed, Embase, Scopus, Web of Sciences, the Cochrane Database of Systematic Reviews, Scopus, and Google Scholar published before 15 April 2024. These articles reported the effect of adversity, protecting factors, and/or resilience-promoting interventions to possess resilience after adversity in a global context without a population age limitation. The quality of the included studies was assessed using the Assessment of Multiple Systematic Reviews. A weighted inverse-variance random-effects model was applied to find the pooled estimates. The subgroup analysis, heterogeneity, publication bias, and sensitivity analysis were also assessed.
Results: A total of 44 articles (n = 556,920 participants) were included in this umbrella review. From the random-effects model analysis, the pooled effect of adversity on the development of resilience was 0.25 (p < 0.001). The pooled effects of adversity-protective factors and resilience-promoting interventions after adversity were 0.31 (p < 0.001) and 0.42 (p < 0.001), respectively. The pooled effects of specific adversity protective factors were 0.26, 0.09, 0.05, 0.34, 0.23, and 0.43 for the availability of support, cognitive ability, community cohesion, positive self-perception, religious involvement, and self-regulation, respectively. The pooled effects of specific resilience-promoting interventions were 0.30, 0.21, 0.51, and 0.52 for cognitive behavior therapy (CBT) interventions, mindfulness-based interventions, mixed interventions, and resilience-promoting interventions, respectively.
Conclusion: The findings of this umbrella review revealed that people who experienced early adversity can develop resilience later in life. The study highlights the need to consider adversity protective factors, such as availability of support (family, friends, and school), cognitive ability, community cohesion, positive self-perception, religious involvement, and self-regulation, and resilience-promoting interventions, including CBT interventions, mindfulness-based interventions, and mixed interventions, to enhance resilience promotion programs.
Introduction
Adverse childhood experiences (ACEs) are potentially traumatic events that can be categorized as abuse (physical, emotional, and sexual), neglect (physical and emotional), and household challenges (mental illness, parent treated violently, divorce, incarcerated relative, and substance abuse) (1–3). Exposure to ACEs can raise the risk of various health and social problems, including harm, sexually transmitted diseases, maternity and pediatric health issues (teen pregnancy, pregnancy complications, and fetal death), human trafficking, suicide, and chronic diseases such as diabetes, heart disease, and cancer (3).
Researchers and practitioners increasingly recognize ACEs as powerful determinants of health and well-being. Originating from various sources, ACEs can have long-term detrimental effects on physical and mental health. These experiences are associated with an increased risk of developmental delays, learning difficulties, depression, diabetes, heart disease, substance abuse, and other chronic illnesses (3). Victims of Adverse Childhood Experience (ACE) might be subjected to additional harmful stress as a result of past and present traumas, and a graded association was observed between the number of ACE categories and the incidence of adult disorders such as liver disease, cancer, ischemic heart disease, chronic lung disease, and skeletal fractures (4).
The prevalence and impact of ACEs is a global concern, although the extent of the problem varies significantly across different regions and populations. Although data collection methodologies and definitions of ACEs can contribute to inconsistencies in prevalence rates, the available evidence suggests that ACEs are widespread. For instance, studies have reported ACE prevalence rates ranging from 31% to 93.5% in China (5, 6), 46.2% in young Europeans (7), and a substantial 72% to 82% in Sub-Saharan Africa (8).
The primary goal of the investigation into the “Effect of ACEs on Resilience Later in Life” is to clarify the complex connection between early adversity and people’s capacity to overcome, adapt, and thrive. Research suggests that protective factors within the home, school, and community are acknowledged, nurtured, and understood (9–11). Individual resilience is defined as the ability to tolerate, adjust to, and overcome stress and adversity (12). This capacity is fostered by the development of adaptive skills, positive experiences, and supportive relationships (13). Resilience acts as a buffer against the detrimental effects of stress, promoting positive emotional and cognitive development in children (13).
Several factors influence the development of resilience. The duration of adversity, the presence of supportive relationships, and previous experiences with challenges all contribute to a child’s resilience (14). The Centers for Disease Control and Prevention has outlined strategies to mitigate the immediate and long-term consequences of ACEs. These include strengthening economic support for families, promoting violence prevention, ensuring early childhood well-being, enhancing parenting and youth coping skills, fostering supportive relationships, and providing timely interventions (15).
The central objective of resilience researchers is to identify vulnerability and protective factors that influence how individuals respond to adversity. By understanding the psychological, emotional, and social mechanisms underlying resilience, researchers aim to develop targeted interventions. Resilience-promotive or adversity-protective factors include supportive relationships and effective coping strategies (16, 17). Understanding the underlying mechanisms of resilience is crucial for identifying pressing issues such as maternal depression, often linked to factors like family conflict, ineffective coping strategies, and negative parenting practices (18). Although research suggests that adversity-protective factors and resilience-promoting interventions can increase resilience, the findings are inconsistent. This gap emphasizes the need for comprehensive research to inform effective interventions and improve practices for promoting resilience. Therefore, this umbrella review aimed to (I) synthesize the pooled effects of childhood adversity; (II) determine the pooled effect of adversity-protective factors, and (III) examine the pooled effect of resilience-promoting interventions on the development of resilience following childhood adversity.
Methods
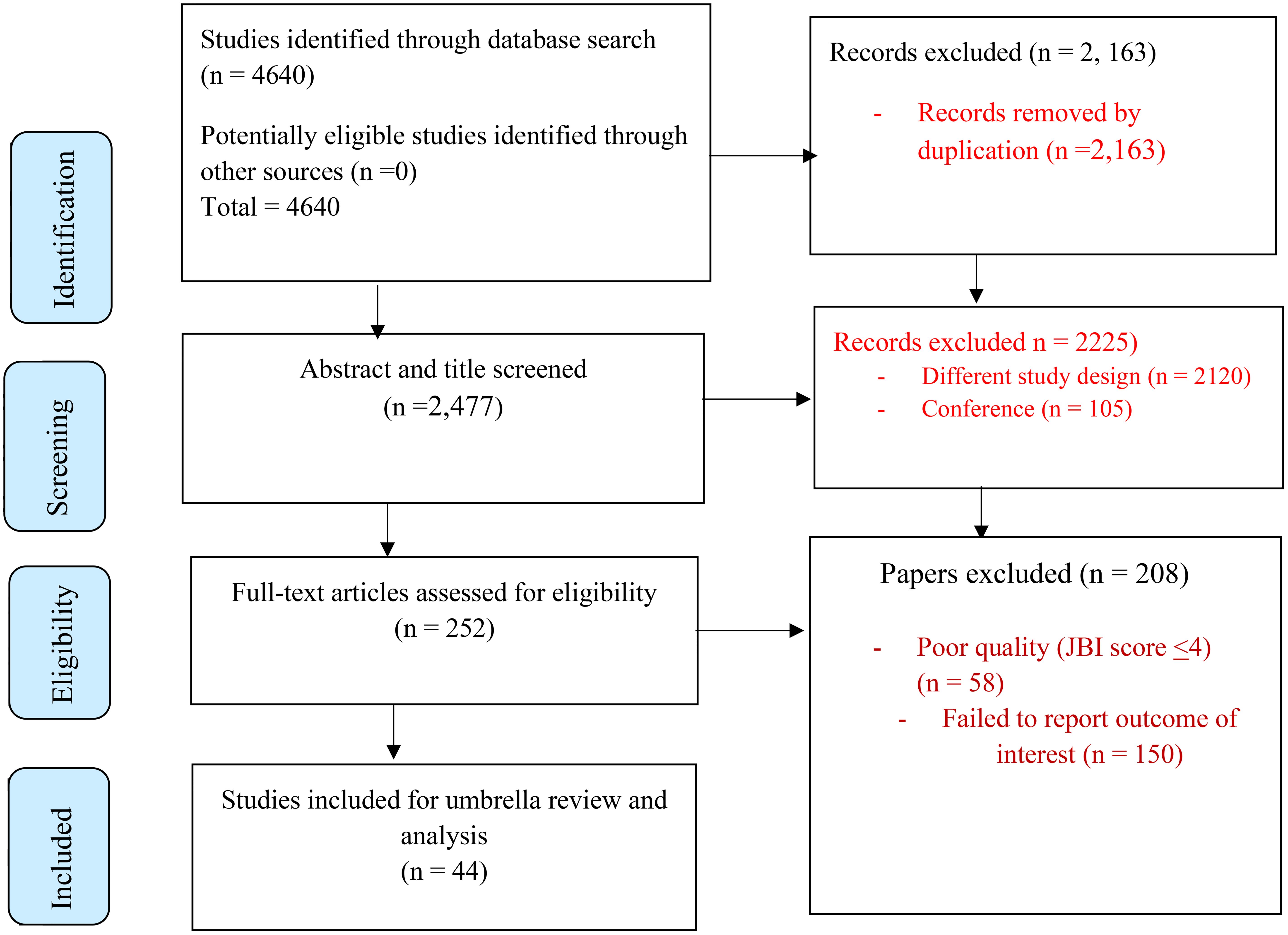
This umbrella review systematically synthesized eligible systematic review and meta-analysis (SRM) reports following established umbrella review methodology (19). Although not pre-registered in PROSPERO, the review protocol has been submitted and is available upon request from the corresponding author. The study adhered to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines and used excluding criteria based on an earlier study (20).
Searching strategy and information sources
A comprehensive search was conducted in PubMed, Embase, Web of Sciences, the Cochrane Database of Systematic Reviews, Scopus, and Google Scholar for studies published before 15 April 2024. These studies examined the impact of protective factors and resilience-promoting interventions on resilience development in a global context. No restrictions were placed on the study start year or participant age. Only English language articles were included. The search employed medical subject heading (MeSH) terms, keywords, and their combinations. Additionally, reference lists of retrieved articles were manually searched for potential studies. Five key concepts were identified for each search term, forming the basis of the search strategies.
Concept 1 (adversity): adverse childhood experience, life challenges, unpleasant, misfortune, hardship, distress, suffering, and sorrow. Concept 2 (resilience): resilience, resilien*, recovery, over-coming, resiliency, and adaptive function. Concept 3 (protective factors): religion, spirituality, support, self-esteem, and coping. Concept 4 (interventions): training, CBT, education, mindfulness, counseling, promotion, intervention, and meditation. Concept 5 (SRM): meta-analysis’, ‘systematic review’, and ‘review’.
The literature search was carried out by two reviewers independently, with discrepancies resolved by consensus. Articles with incomplete reported data were handled by contacting corresponding authors. We used the search terms independently and/or in combination using “OR” or “AND” [(“adversity” OR “adverse childhood experience” OR “life challenges” OR “unpleasant” OR “misfortune” OR “hardship” OR “distress” OR “suffering” OR “sorrow”) AND (“resilience” OR “resilien*” OR “recovery” OR “over-coming” OR “resiliency” OR “adaptive function”) AND (“religious” OR “spirituality” OR “support” OR “self-esteem,” OR “coping”) AND (“training” OR”CBT” OR “education” OR “mindfulness” OR “counseling” OR “promotion” OR “intervention” OR “meditate”)]. A sample of the literature search strategy, the PubMed search strategy, developed using a combination of MeSH terms and free texts is presented as a Supplementary Data Sheet 1 (Supplementary Table 1). In addition to the systematic database search, an article search was carried out using the reference list of the included studies and the ‘cited by’ and ‘related articles’ functions of PubMed.
Study selection/eligibility criteria
Retrieved articles were imported into Endnote v8 for duplicate removal. The screening and selection of studies were conducted in two stages. Two reviewers (BBA and MAB) independently screened titles and abstracts, followed by a full-text assessment using pre-specified inclusion criteria. To be included, SRMs had to report the effects of protective factors and resilience-promoting interventions on resilience development in a global context and be published in English. Additionally, studies were required to (a) present a defined literature search strategy, (b) appraise included studies using a relevant tool, and (c) employ a standardized approach to pooling studies and reporting summary estimates. Studies were excluded for the following reasons: (a) a lack of reporting on the measures of interest, (b) a language other than English, and (c) study type (narrative reviews, editorials, correspondence, abstracts, and methodological studies). Disagreements regarding study inclusion were resolved through consensus among reviewers.
Quality assessment
The methodological quality of included systematic reviews was assessed independently by two reviewers (AKS and AMK) using the AMSTAR tool (21). AMSTAR evaluates the quality of systematic reviews based on 11 items assessing the rigor of methods used for pooling and summarizing studies. Given its reliability and widespread use, AMSTAR was selected for this review. Studies were categorized as high (8–11), medium (4–7), or low (≤3) quality based on their total AMSTAR score. Only reviews with a medium- or high-quality rating (score ≥4) were included in this study. A predetermined quality threshold was established and agreed upon by all reviewers before the assessment process. Although the quality of the included systematic reviews was assessed, the quality of primary studies within these reviews was not explicitly evaluated for this umbrella review.
Data extraction
Data from the included SRMs were extracted using a standardized Excel-based data abstraction form. For each SRM, the following information was collected: (a) study identification (first author, publication year), (b) review aim and type, (c) estimate of resilience among adversity-exposed populations, (d) effects of adversity protective factors, (e) effects of resilience-promoting interventions, (f) included primary studies (design type and sample size), (g) sample size of included studies, (h) publication bias assessment methods and results, (i) quality assessment methods and scores, (j) data synthesis method (random or fixed-effects), and (k) authors’ main conclusions (Table 1).
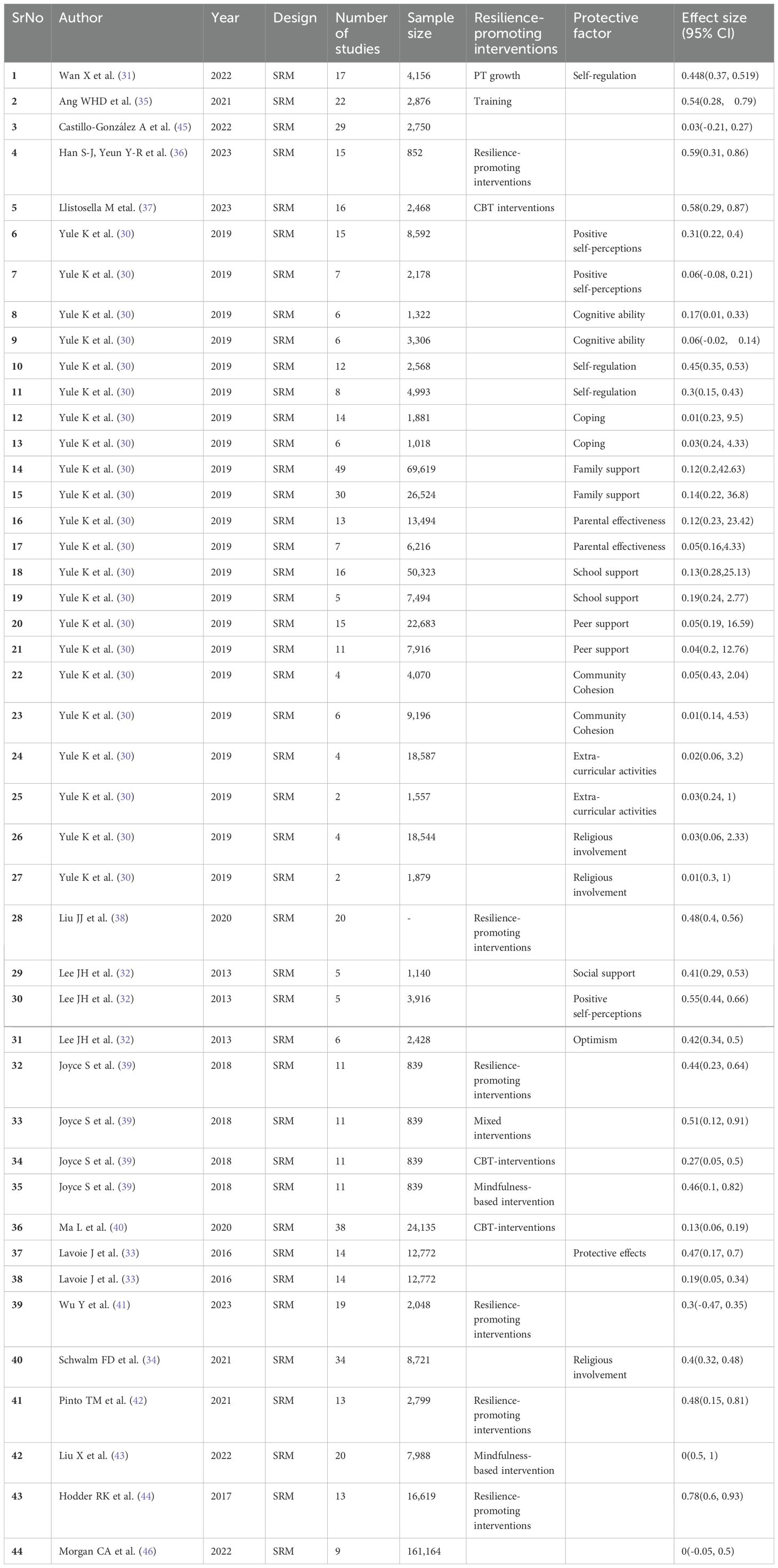
Table 1. Distribution of the included studies on resilience after adversity: the effect of protecting factors and resilience-promoting interventions, 2024.
Statistical analysis
Data extracted from the included SRMs using Microsoft Excel were imported into STATA v14.0 for analysis. A combined narrative and quantitative approach was used to summarize review estimates. When multiple estimates were available, a range of estimates and a pooled estimate were presented. Pooled estimates for the effects of adversity, protective factors, and resilience-promoting interventions on later-life resilience were calculated with 95% confidence intervals (CIs) and visualized using forest plots (22). The pooled estimates with 95% CIs were presented using forest plots.
Heterogeneity among the included SRMs was assessed using Galbraith plots, inverse variance (I² statistics), and Cochran’s Q statistic. I² values, ranging from 0 to 100%, quantify the proportion of total variance attributable to heterogeneity (23, 24). I2 of 25%, 50%, and 75% thresholds for low, moderate, and high heterogeneity, respectively, with a threshold of I² < 50%, is often considered indicative of low heterogeneity (25, 26). Additionally, τ² was calculated to estimate between-study variance, as I² can be influenced by study size (27). To further explore heterogeneity, 95% prediction intervals (PIs) for the standardized mean difference were calculated, providing a range for potential effect sizes in future studies (27). I², τ², and 95% PIs were computed for each SRM (28).
For heterogeneous data, a DerSimonian–Laird random-effects model was applied. Subgroup analyses were conducted based on protective factors and resilience-promoting intervention types. Sensitivity analysis was performed to evaluate the impact of individual studies on overall estimates. Publication bias was assessed using funnel plots and Egger’s regression test (29).
Results
A total of 4,640 studies were identified from different databases. After removing duplicates (2,163), 2,477 records remained. Subsequent title and abstract screening resulted in 252 full-text articles being selected for detailed evaluation, 208 of which were subsequently excluded due to poor quality (JBI score <4) (n=58) and a failure to report an outcome of interest (n=150). Finally, 44 articles encompassing 556,920 participants met the inclusion criteria and were included in the final analysis (Figure 1).
Characteristics of the included studies
The number of studies included in each SRM ranged from 2 (30) to 49 (30). The minimum and maximum sample sizes were 1,557 and 69,619, respectively. Out of 44 included SRMs, 27 investigated adversity protective factors for resilience development (Wan X et al. (31), Yule K et al. (30), Lee JH et al. (32), Lavoie J et al. (33) and Schwalm FD et al. (34)). Fourteen SRMs examined the effects of resilience-promoting interventions on resilience development (Wan X et al. (31), Ang WHD et al. (35), Han S-J, Yeun Y-R et al. (36), Llistosella M et al. (37), Liu JJ et al. (38), Joyce S et al. (39), Joyce S et al. (39), Ma L et al. (40), Wu Y et al. (41), Pinto TM et al. (42), Liu X et al. (43), Hodder RK et al. (44)). Five SRMs reported the association between adversity and resilience (Wan X et al. (31), Ang WHD et al. (35), Castillo‐González A et al. (45), Lavoie J et al. (33), Morgan CA et al. (46)) (Table 1).
The effect of protective factors
The effects of protective factors were determined from 27 SRMs (Wan X et al. (31), Yule K et al. (30), Lee JH et al. (32), Lavoie J et al. (33), and Schwalm FD et al. (34)). The effects of protective factors ranged from 0.01 (95% CI: 0.14, 4.53) (30) to 0.45 (95% CI: 0.37, 0.519) (31). Random-effects model analysis of these studies revealed a pooled effect of protective factors on resilience development following adversity of 0.31 (95% CI: 0.22, 0.40) (I² = 78.46%; p < 0.001) (Figure 2)
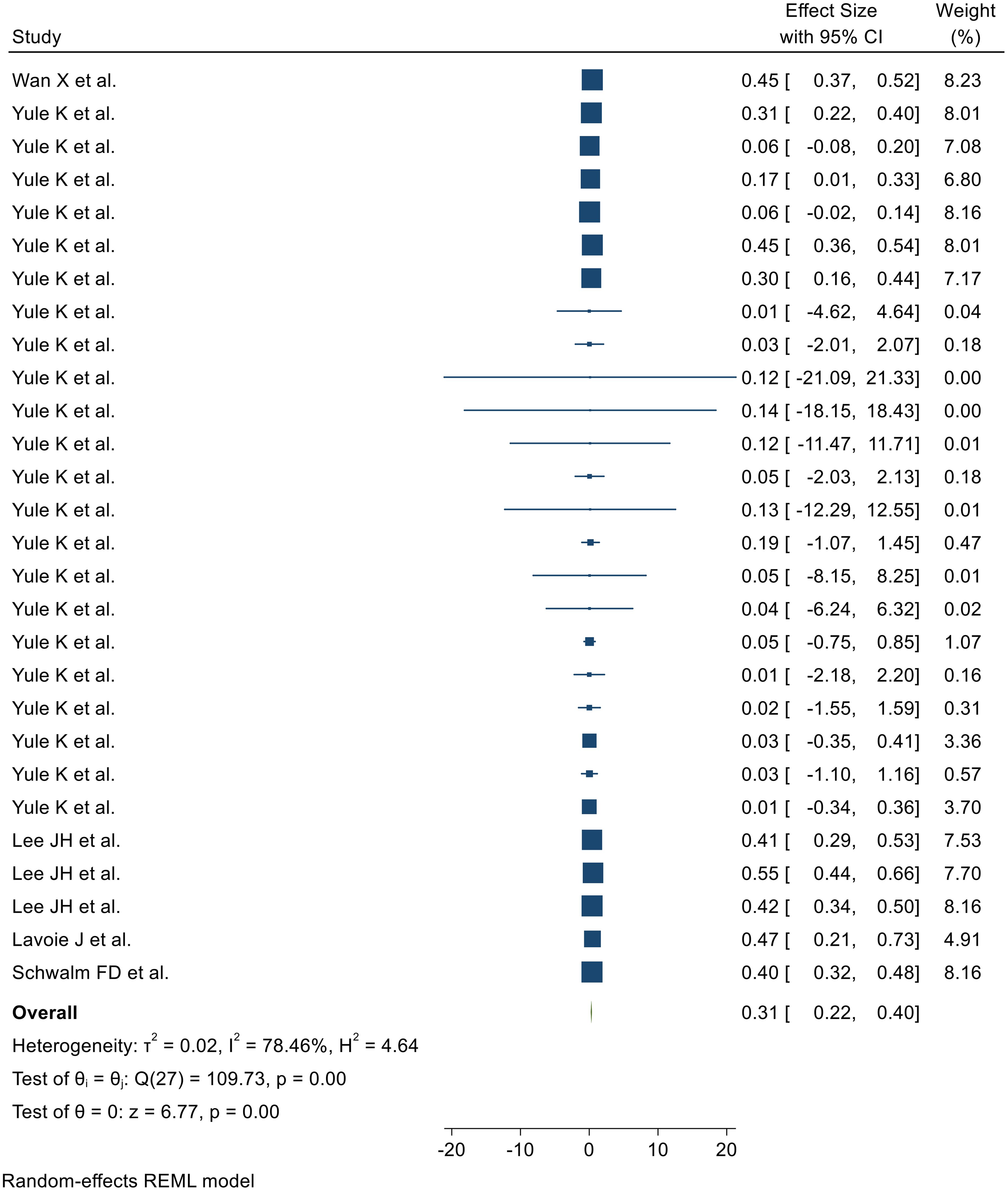
Figure 2. Forest plot showing the pooled effect of these protective factors for the development of resilience after adversity.
Heterogeneity outcome
Heterogeneity among the 27 included SRMs was assessed using Galbraith plots and I² statistics. Random-effects meta-analysis revealed a pooled effect of adversity protective factors on resilience development of 0.31 (95% CI: 0.22, 0.40) with substantial heterogeneity (I² = 78.46%, p < 0.001), as visualized in the Galbraith plot (Supplementary Figure 1).
Subgroup analysis
Subgroup analysis was conducted based on the protective factor type. Pooled effects for resilience development were 0.26 (95% CI: −0.04, 0.55) for availability of support, 0.09 (95% CI: −0.01, 0.19) for cognitive ability, 0.05 (95% CI: −0.71, 0.80) for community cohesion, 0.34 (95% CI: 0.14, 0.54) for positive self-perception, 0.23 (95% CI: −0.10, 0.57) for religious involvement, and 0.43 (95% CI: 0.37, 0.48) for self-regulation (Supplementary Figure 2).
Publication bias
A funnel plot exhibited a symmetrical distribution (Supplementary Figure 3). The Egger’s regression test yielded a value of 0.278, indicating no evidence of publication bias (Supplementary Figure 4). Consequently, a trim and fill analysis was not conducted (Supplementary Figure 5).
Sensitivity analysis
A leave-one-out sensitivity analysis was conducted to assess the influence of individual studies on the pooled estimate of protective factors for resilience development. Results indicated that the pooled findings were robust to the exclusion of any single study. The pooled estimate ranged from 0.297 (0.20–0.38) to 0.34 (0.28–0.41) after removing a single study (Supplementary Figure 6).
The effect of resilience-promoting interventions
Fourteen of the 44 included SRMs reported the effects of resilience-promoting interventions on resilience development following adversity (Wan X et al. (31), Ang WHD et al. (35), Han S-J, Yeun Y-R et al. (36), Llistosella M etal. (37), Liu JJ et al. (38), Joyce S et al. (39), Joyce S et al. (39), Ma L et al. (40), Wu Y et al. (41), Pinto TM et al. (42), Liu X et al. (43), Hodder RK et al. (44)). Random-effects model analysis of these studies revealed a pooled effect of resilience-promoting interventions on resilience development of 0.42 (95% CI: 0.30, 0.55), with substantial heterogeneity (I² = 78.46%; p < 0.001) (Figure 3).

Figure 3. Forest plot showing the pooled effect of resilience-promoting interventions for the development of resilience after adversity.
Heterogeneity outcome
Heterogeneity among the 14 included SRMs was assessed using Galbraith plots and I² statistics (Supplementary Figure 7). Random-effects meta-analysis revealed a pooled effect of resilience-promoting interventions on resilience development of 0.42 (95% CI: 0.30, 0.55), with substantial heterogeneity (I² = 78.46%, p < 0.001).
Subgroup analysis
Subgroup analysis was conducted based on the types of resilience-promoting interventions. Pooled effects for resilience development were 0.30 (95% CI: 0.05, 0.55) for CBT interventions, 0.21 (−0.24, 0.66) for mindfulness-based interventions, 0.51 (95% CI: 0.12, 0.90) for mixed interventions, and 0.52 (95% CI: 0.42, 0.62) for resilience-promoting interventions (Supplementary Figure 8).
Publication bias
A funnel plot showed a symmetrical distribution (Supplementary Figure 9). The Egger’s regression test value was 0.647, which indicated the absence of publication bias (Supplementary Figure 10). Owing to the absence of publication bias, we did not employ a trim and fill analysis (Supplementary Figure 11).
Effects of previous adversity on resilience later in life
Five SRMs reported the association between previous adversity and later-life resilience (Wan X et al. (31), Ang WHD et al. (35), Castillo‐González A et al. (45), Lavoie J et al. (33), Morgan CA et al. (46)). The random-effects model analysis from those studies revealed that the pooled effect of adversity for the development of resilience after previous adversity was 0.25 (95% CI: 0.05, 0.46) (I2 = 85.82%; p < 0.001) (Figure 4).

Figure 4. Forest plot showing the pooled effect of adversity for the development of later resilience.
Heterogeneity outcome
The Galbraith plot and I² were used to assess heterogeneity among the five included SRMs (Supplementary Figure 12). Random-effects meta-analysis revealed a pooled effect of adversity on resilience of 0.25 (95% CI: 0.05, 0.46), with substantial heterogeneity (I² = 85.82%; p < 0.001). The Galbraith plot also indicated heterogeneity.
Publication bias
A funnel plot exhibited a symmetrical distribution (Supplementary Figure 13). The Egger’s regression test yielded a value of 0.39, indicating no evidence of publication bias (Supplementary Figure 14). Consequently, a trim and fill analysis was not conducted.
Sensitivity analysis
A leave-one-out sensitivity analysis was conducted to assess the influence of individual studies on the pooled estimate of adversity on resilience development. Results indicated that the pooled findings were robust to the exclusion of any single study. The pooled estimate ranged from 0.18 (0.04–0.42) to 0.30 (0.10–0.50) after removing individual studies (Supplementary Figure 15).
Discussion
This umbrella review aimed to assess the effects of adversity, adversity protective factors, and resilience-promoting interventions on resilience development in a global context. Results indicated a significant pooled effect of resilience-promoting interventions on post-adversity resilience. According to Morgan CA et al.’s SRM, a substantial negative correlation exists between ACEs and resilience (46). Children worldwide face various adversities, with some developing resilience and others experience long-term psychological and social challenges. Individuals with ACEs were 63% less likely to exhibit high resilience compared with those without ACEs, emphasizing the importance of identifying factors contributing to resilience development.
The current study found a pooled effect of 0.31 for adversity protective factors on resilience development. These protective factors, including the availability of support, cognitive ability, community cohesion, positive self-perception, religious involvement, and self-regulation, significantly influenced resilience. This finding aligns with the work of Yule K et al. in 2019 (30).
Accordingly, 26% of individuals experiencing childhood hardship developed resilience due to supportive relationships with family, friends, or their school, aligning with Afifi TO and MacMillan HL’s 2011 analysis, “Resilience After Child Abuse: An Examination of Protective Elements” (47). Religious participation also contributed to resilience, with 23% of trauma-exposed individuals reporting increased resilience following religious involvement. These findings support previous studies on the protective effects of parental involvement and religion against behavioral problems in violence-exposed adolescents (48, 49).
To build resilience and mitigate the harmful effects of childhood adversity, future studies should prioritize the development and evaluation of interventions. Universal resilience-focused interventions, particularly CBT, have demonstrated efficacy in reducing ACE-related depressive and anxiety symptoms (50). Early community resilience assets, such as fair treatment, supportive friendships, opportunities for skill development, trusted adult relationships, and positive role models, have been independently linked to positive outcomes (51).
Research indicates that positive early relationships with compassionate adults can mitigate or prevent the harmful effects of ACEs, a form of toxic stress (3). Although ACEs pose significant challenges, some individuals demonstrate resilience by overcoming adversity and achieving personal growth. Emerging research highlights the role of protective factors and resilience in mitigating the negative impacts of ACEs. Resilience theories emphasize individuals’ strengths, including coping strategies (internal) and family and community support (external), in navigating stressful experiences, rather than focusing solely on vulnerabilities (52–54). Positive individual, family, and community characteristics, such as strong family functioning and parental engagement, are linked to better outcomes for children and adolescents exposed to ACEs (55, 56). Strong family functioning can serve as a protective factor against teenage mental health issues, poverty, neighborhood violence, and dysfunctional parental relationships (9–11).
This umbrella review indicates that interventions incorporating mindfulness or CBT techniques can enhance resilience measures. Although our analysis revealed significant pooled effects of resilience-promoting interventions across various subtypes, including CBT, mindfulness-based, and mixed interventions, further research is needed to optimize these approaches.
Previous studies have demonstrated the positive impact of resilience training on psychological well-being (57). Additionally, research suggests that CBT can influence resilience through its impact on life stories (58). A combination of CBT and mindfulness techniques within resilience interventions shows promise, building upon the established efficacy of these approaches in treating mental health conditions such as depression and anxiety (39, 59–61). Moreover, these interventions have been linked to improved overall psychological and physical health (62).
Implications for research
Protective factors, such as caregiver support, can increase resilience without necessarily directly impacting psychological symptoms, although their relationship to maladjustment warrants further investigation (63). To accurately measure resilience in children exposed to violence, studies should consider both indicators of healthy development and protective factors (63).
Research emphasizes the importance of strong relationships and understanding broader cultural contexts in fostering children’s resilience, calling for improved prevention strategies (64, 65). Effective prevention and health promotion across diverse cultural groups requires understanding how sociocultural factors influence protective factors within families, schools, and peer groups (66). The Resilience Portfolio Model offers a structured framework for examining factors influencing children’s adjustment processes (67, 68).
Implications for prevention and intervention
This study emphasizes the importance of universal prevention, sensitive caregiving, supportive family relationships, and parental intervention programs in fostering children’s resilience (69). Caregiver programs promoting self-regulation, including emotion socialization strategies, have demonstrated improvements in socio-emotional competencies and reduced behavioral issues among preschoolers (70).
Schools are transitioning from punitive discipline toward promoting healthy development through social emotional learning (SEL) principles, cultivating supportive relationships and individual strengths among students and teachers (71–73). SEL programs, encompassing self-regulation, teacher-student relationships, positive self-perception, and symptom reduction, can be integrated into school-based initiatives (74). Mindfulness-based interventions (75), such as compassion and attention in schools, which teach attention focus and mental/physical self-control (76, 77), have shown benefits for self-perception, well-being, self-regulation, coping, and mental health in children and adolescents (78, 79).
Trauma-sensitive schools adopt a comprehensive approach, including SEL curricula, support services, and targeted interventions, to address the impact of trauma on children’s behavior (80–82). Research affirms the potential of trauma-sensitive schools to enhance children’s functioning, regardless of trauma exposure (82). Although this meta-analysis highlights the significance of protective factors in parenting and school-based programs, their effectiveness in enhancing children’s functioning is often underestimated (83). Program evaluations investigating the impact of self-regulation and supportive teacher-student relationships on children’s health and well-being contribute to resilience research by examining their additive and buffering effects.
The findings of this study should be interpreted with caution due to several limitations. First, the included studies exhibited substantial heterogeneity, indicating variability in the methodologies, populations, and outcomes reported. Although a random-effects model and subgroup analysis were employed to account for this heterogeneity, it is important to acknowledge that the pooled estimate may not accurately represent the true effect size in all contexts. Second, the geographical distribution of the included studies was uneven, with a potential overrepresentation of certain regions. This limitation may restrict the generalizability of the findings to populations from underrepresented geographical areas. Finally, the inclusion of only English language studies might have led to the exclusion of relevant research conducted in other languages. This language bias could potentially limit the comprehensiveness of the evidence base.
Conclusion and recommendation
This umbrella review demonstrates that individuals exposed to early adversity can develop resilience. Protective factors, including support from family, friends, and school, cognitive abilities, community cohesion, positive self-perception, religious involvement, and self-regulation, are associated with an increased likelihood of developing resilience following adversity. Resilience-promoting interventions, such as CBT and mindfulness-based approaches, can also enhance resilience outcomes. To foster resilience among at-risk youth and their caregivers, concerted efforts to strengthen positive relationships within families, schools, and communities are essential.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
BA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AS: Writing – review & editing, Data curation, Methodology, Supervision, Conceptualization, Formal analysis, Project administration, Validation, Investigation, Funding acquisition, Resources, Visualization, Software. AT: Writing – review & editing, Data curation, Methodology, Supervision, Conceptualization, Formal analysis, Project administration, Validation, Investigation, Funding acquisition, Resources, Visualization, Software. TE: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AA: Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation. GA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1391312/full#supplementary-material
References
1. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
2. Felitti VJ, Anda RF. The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders, and sexual behavior: Implications for healthcare. In: The impact of early life trauma on health and disease: The hidden epidemic. United States (2010). p. 77–87.
3. Control C.f.D and Prevention. Adverse Childhood Experiences Prevention Strategy. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (2021).
4. Austin A. Association of adverse childhood experiences with life course health and development. NC Med J. (2018) 79:99–103. doi: 10.18043/ncm.79.2.99
5. Wei W, Xiaoming Yu M. Adverse childhood experience as a risk factor for adolescent pregnancy in China. Int J Child Adolesc Health. (2013) 6:323.
6. Lee S, Guo WJ, Tsang A, He YL, Huang YQ, Zhang MY, et al. The prevalence of family childhood adversities and their association with first onset of DSM-IV disorders in metropolitan China. psychol Med. (2011) 41:85–96. doi: 10.1017/S0033291710000450
7. Hughes K, Bellis MA, Sethi D, Andrew R, Yon Y, Wood S, et al. Adverse childhood experiences, childhood relationships and associated substance use and mental health in young Europeans. Eur J Public Health. (2019) 29:741–7. doi: 10.1093/eurpub/ckz037
8. Amene EW, Annor FB, Gilbert LK, McOwen J, Augusto A, Manuel P, et al. Prevalence of adverse childhood experiences in sub-saharan Africa: a multicountry analysis of the Violence against Children and Youth Surveys (VACS). Child Abuse Negl. (2024) 150:106353. doi: 10.1016/j.chiabu.2023.106353
9. Mistry RS, Vandewater EA, Huston AC, McLoyd VC. Economic well-being and children’s social adjustment: The role of family process in an ethnically diverse low-income sample. Child Dev. (2002) 73:935–51. doi: 10.1111/1467-8624.00448
10. Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: A meta-analysis. J Adolesc Health. (2013) 53:S32–8. doi: 10.1016/j.jadohealth.2013.05.004
11. Fan Y, Chen Q. Family functioning as a mediator between neighborhood conditions and children’s health: Evidence from a national survey in the United States. Soc Sci Med. (2012) 74:1939–47. doi: 10.1016/j.socscimed.2012.01.039
12. Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol. (2014) 5:25338. doi: 10.3402/ejpt.v5.25338
13. Rutter M. Resilience as a dynamic concept. Dev Psychopathol. (2012) 24:335–44. doi: 10.1017/S0954579412000028
14. Masten AS, Barnes AJ. Resilience in children: Developmental perspectives. Children. (2018) 5:98. doi: 10.3390/children5070098
15. Control C.f.D and Prevention. Adverse childhood experiences (ACEs) prevention resource for action: A compilation of the best available evidence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (2019).
16. Zimmerman MA, Stoddard SA, Eisman AB, Caldwell CH, Aiyer SM, Miller A. Adolescent resilience: resources and assets for informing prevention. Child Dev Perspect. (2013) 7:215–20. doi: 10.1111/cdep.12042
17. Buchanan M, Walker G, Boden JM, Mansoor Z, Newton-Howes G. Protective factors for psychosocial outcomes following cumulative childhood adversity: systematic review. BJPsych Open. (2023) 9:e197. doi: 10.1192/bjo.2023.561
18. Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, Curtis LJ. Mutual influences on maternal depression and child adjustment problems. Clin Psychol Rev. (2004) 24:441–59. doi: 10.1016/j.cpr.2004.02.002
19. Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evidence Implementation. (2015) 13:132–40. doi: 10.1097/XEB.0000000000000055
20. Komasi S, Rezaei F, Hemmati A, Rahmani K, Amianto F, Miettunen J, et al. Comprehensive meta-analysis of associations between temperament and character traits in Cloninger’s psychobiological theory and mental disorders. J Int Med Res. (2022) 50:03000605211070766. doi: 10.1177/03000605211070766
21. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Method. (2007) 7:1–7. doi: 10.1186/1471-2288-7-10
22. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res synthesis Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
23. Abate BB, Tilahun BD, Yayeh BM. Global COVID-19 vaccine acceptance level and its determinants: an umbrella review. BMC Public Health. (2024) 24:5. doi: 10.1186/s12889-023-17497-4
24. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
25. Ioannidis JP. Interpretation of tests of heterogeneity and bias in meta-analysis. J Eval Clin Pract. (2008) 14:951–7. doi: 10.1111/j.1365-2753.2008.00986.x
26. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
27. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. Bmj. (2011) 342:302–49. doi: 10.1136/bmj.d549
28. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. BMJ Ment Health. (2019) 35:45–77. doi: 10.1136/ebmental-2019-300117
29. Egger M, Smith DG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. bmj. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
30. Yule K, Houston J, Grych J. Resilience in children exposed to violence: A meta-analysis of protective factors across ecological contexts. Clin Child Family Psychol Rev. (2019) 22:406–31. doi: 10.1007/s10567-019-00293-1
31. Wan X, Huang H, Peng Q, Yu NX, Zhang Y, Ding Y. A meta-analysis on the relationship between posttraumatic growth and resilience in people with breast cancer. Nurs Open. (2023) 10:2734–45. doi: 10.1002/nop2.1540
32. Lee JH, Nam SK, Kim A-R, Kim B, Lee MY, Lee SM. Resilience: a meta-analytic approach. J Couns Dev. (2013) 91:269–79. doi: 10.1002/j.1556-6676.2013.00095.x
33. Lavoie J, Pereira LC, Talwar V. Children’s physical resilience outcomes: Meta-analysis of vulnerability and protective factors. J Pediatr Nurs. (2016) 31:701–11. doi: 10.1016/j.pedn.2016.07.011
34. Schwalm FD, Zandavalli RB, de Castro Filho ED, Lucchetti G. Is there a relationship between spirituality/religiosity and resilience? A systematic review and meta-analysis of observational studies. J Health Psychol. (2022) 27:1218–32. doi: 10.1177/1359105320984537
35. Ang WHD, Chew HSJ, Dong J, Yi H, Mahendren R, Lau Y. Digital training for building resilience: Systematic review, meta-analysis, and meta-regression. Stress Health. (2022) 38:848–69. doi: 10.1002/smi.3154
36. Han S-J, Yeun Y-R. Psychological intervention to promote resilience in nurses: A systematic review and meta-analysis. Healthcare. (2023) 10:102–45. doi: 10.3390/healthcare12010073
37. Llistosella M, Martín-Delgado L, Miranda-Mendizabal A, Franch Martinez B, Pérez-Ventana C. Effectiveness of resilience-based interventions in schools for adolescents: A systematic review and meta-analysis. Front Psychol. (2023) 14. doi: 10.3389/fpsyg.2023.1211113
38. Liu JJ, Ein N, Gervasio J, Battaion M, Reed M, Vickers K. Comprehensive meta-analysis of resilience interventions. Clin Psychol Rev. (2020) 82:101919. doi: 10.1016/j.cpr.2020.101919
39. Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. (2018) 8:54–87. doi: 10.1136/bmjopen-2017-017858
40. Ma L, Zhang Y, Huang C, Cui Z. Resilience-oriented cognitive behavioral interventions for depressive symptoms in children and adolescents: A meta-analytic review. J Affect Disord. (2020) 270:150–64. doi: 10.1016/j.jad.2020.03.051
41. Wu Y, Zhang Y-Y, Zhang Y-T, Zhang H-J, Long T-X, Zhang Q, et al. Effectiveness of resilience-promoting interventions in adolescents with diabetes mellitus: a systematic review and meta-analysis. World J Pediatr. (2023) 19:323–39. doi: 10.1007/s12519-022-00666-7
42. Pinto TM, Laurence PG, Macedo CR, Macedo EC. Resilience programs for children and adolescents: a systematic review and meta-analysis. Front Psychol. (2021) 12:754115. doi: 10.3389/fpsyg.2021.754115
43. Liu X, Wang Q, Zhou Z. The association between mindfulness and resilience among university students: a meta-analysis. Sustainability. (2022) 14:10405. doi: 10.3390/su141610405
44. Hodder RK, Freund M, Wolfenden L, Bowman J, Nepal S, Dray J. Systematic review of universal school-based ‘resilience’interventions targeting adolescent tobacco, alcohol or illicit substance use: A meta-analysis. Prev Med. (2017) 100:248–68. doi: 10.1016/j.ypmed.2017.04.003
45. Castillo-González A, Velando-Soriano A, De La Fuente-Solana EI, Martos-Cabrera BM, Membrive-Jiménez MJ. Relation and effect of resilience on burnout in nurses: A literature review and meta-analysis. Int Nurs Rev. (2023) 5:39–80. doi: 10.1111/inr.12838
46. Morgan CA, Chang Y-H, Choy O, Tsai M-C, Hsieh S. Adverse childhood experiences are associated with reduced psychological resilience in youth: A systematic review and meta-analysis. Children. (2021) 9:27. doi: 10.3390/children9010027
47. Afifi TO, MacMillan HL. Resilience following child maltreatment: A review of protective factors. Can J Psychiatry. (2011) 56:266–72. doi: 10.1177/070674371105600505
48. Pearce MJ, Jones SM, Schwab-Stone ME, Ruchkin V. The protective effects of religiousness and parent involvement on the development of conduct problems among youth exposed to violence. Child Dev. (2003) 74:1682–96. doi: 10.1046/j.1467-8624.2003.00631.x
49. Paranjape A, Kaslow N. Family violence exposure and health outcomes among older African American women: Do spirituality and social support play protective roles? J women’s Health. (2010) 19:1899–904. doi: 10.1089/jwh.2009.1845
50. Fritz J, de Graaff AM, Caisley H, van Harmelen A-L, Wilkinson PO. A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Front Psychiatry. (2018) 9:230. doi: 10.3389/fpsyt.2018.00230
51. Bellis MA, Hughes K, Ford K, Hardcastle KA, Sharp CA, Wood S. Adverse childhood experiences and sources of childhood resilience: a retrospective study of their combined relationships with child health and educational attendance. BMC Public Health. (2018) 18:1–12. doi: 10.1186/s12889-018-5699-8
52. Cairns RB, Cairns BD. Lifelines and risks: Pathways of youth in our time. Cambridge University Press (1994).
53. Rutter M. Resilience in the face of adversity: Protective factors and resistance to psychiatric disorder. Br J Psychiatry. (1985) 147:598–611. doi: 10.1192/bjp.147.6.598
54. Masten AS. Ordinary magic: Resilience processes in development. Am Psychol. (2001) 56:227. doi: 10.1037/0003-066X.56.3.227
55. Balistreri KS, Alvira-Hammond M. Adverse childhood experiences, family functioning and adolescent health and emotional well-being. Public Health. (2016) 132:72–8. doi: 10.1016/j.puhe.2015.10.034
56. Bethell C, Gombojav N, Solloway M, Wissow L. Adverse childhood experiences, resilience and mindfulness-based approaches: common denominator issues for children with emotional, mental, or behavioral problems. Child Adolesc Psychiatr Clinics. (2016) 25:139–56. doi: 10.1016/j.chc.2015.12.001
57. Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Systematic Rev. (2020) 7:102–37. doi: 10.1002/14651858.CD012527.pub2
58. Hutnik N, Smith P, Koch T. Using cognitive behaviour therapy to explore resilience in the life-stories of 16 UK centenarians. Nurs Open. (2016) 3:110–8. doi: 10.1002/nop2.44
59. Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J consulting Clin Psychol. (2010) 78:169. doi: 10.1037/a0018555
60. Keng S-L, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: A review of empirical studies. Clin Psychol Rev. (2011) 31:1041–56. doi: 10.1016/j.cpr.2011.04.006
61. Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. (2013) 33:763–71. doi: 10.1016/j.cpr.2013.05.005
62. Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J psychosomatic Res. (2010) 68:539–44. doi: 10.1016/j.jpsychores.2009.10.005
63. Masten AS. Pathways to integrated resilience science. psychol Inq. (2015) 26:187–96. doi: 10.1080/1047840X.2015.1012041
64. Ungar M. The social ecology of resilience: addressing contextual and cultural ambiguity of a nascent construct. Am J orthopsychiatry. (2011) 81:1. doi: 10.1111/j.1939-0025.2010.01067.x
65. Bronfenbrenner U. Making human beings human: Bioecological perspectives on human development. sage (2005).
66. Khan A, Khanlou N, Stol J, Tran V. Immigrant and refugee youth mental health in Canada: A scoping review of empirical literature. In: Today’s youth and mental health: Hope, power, and resilience. United Kingdom (2018). p. 3–20.
67. Grych J, Hamby S, Banyard V. The resilience portfolio model: Understanding healthy adaptation in victims of violence. Psychol violence. (2015) 5:343. doi: 10.1037/a0039671
68. Hamby S, Grych J, Banyard V. Resilience portfolios and poly-strengths: Identifying protective factors associated with thriving after adversity. Psychol violence. (2018) 8:172. doi: 10.1037/vio0000135
69. Yates TM, Egeland B, Sroufe LA. Rethinking resilience: A developmental process perspective. In: Resilience and vulnerability: Adaptation in the context of childhood adversities. United Kingdom, vol. 243. (2003). p. 266.
70. Havighurst SS, Wilson KR, Harley AE, Prior MR, Kehoe C. Tuning in to Kids: improving emotion socialization practices in parents of preschool children–findings from a community trial. J Child Psychol Psychiatry. (2010) 51:1342–50. doi: 10.1111/j.1469-7610.2010.02303.x
71. Anderson M, Werner-Seidler A, King C, Gayed A, Harvey SB, O’Dea B. Mental health training programs for secondary school teachers: A systematic review. School Ment Health. (2019) 11:489–508. doi: 10.1007/s12310-018-9291-2
72. Hymel S, Low A, Starosta L, Gill R, Schonert-Reich K. Promoting mental well-being through social-emotional learning in schools: Examples from British Columbia. Can J Community Ment Health. (2018) 36:97–107. doi: 10.7870/cjcmh-2017-029
73. Whitley J, Smith JD, Vaillancourt T. Promoting mental health literacy among educators: A critical aspect of school-based prevention and intervention. In: Handbook of school-based mental health promotion: An evidence-informed framework for implementation. Canada (2018). p. 143–65.
74. Stallard P, et al. The FRIENDS emotional health programme: Initial findings from a school-based project. Child Adolesc Ment Health. (2007) 12:32–7. doi: 10.1111/j.1475-3588.2006.00421.x
75. Broderick PC, Kabat-Zinn M, Kabat-Zinn J. Learning to Breathe: A Mindfulness Curriculum for Adolescents to Cultivate Emotion Regulation. Attention, and Performance. New Harbinger Publications (2013).
76. Terjestam Y, Bengtsson H, Jansson A. Cultivating awareness at school. Effects on effortful control, peer relations and well-being at school in grades 5, 7, and 8. School Psychol Int. (2016) 37:456–69. doi: 10.1177/0143034316658321
77. Greenberg MT, Domitrovich CE, Weissberg RP, Durlak JA. Social and emotional learning as a public health approach to education. Future Children. (2017) 5:13–32. doi: 10.1353/foc.2017.0001
78. Carsley D, Khoury B, Heath NL. Effectiveness of mindfulness interventions for mental health in schools: A comprehensive meta-analysis. Mindfulness. (2018) 9:693–707. doi: 10.1007/s12671-017-0839-2
79. Zoogman S, Goldberg SB, Hoyt WT, Miller L. Mindfulness interventions with youth: A meta-analysis. Mindfulness. (2015) 6:290–302. doi: 10.1007/s12671-013-0260-4
80. Kataoka SH, Vona P, Acuna A, Jaycox L, Escudero P, Rojas C. Applying a trauma informed school systems approach: Examples from school community-academic partnerships. Ethnicity Dis. (2018) 28:417. doi: 10.18865/ed.28.S2.417
81. Plumb JL, Bush KA, Kersevich SE. Trauma-sensitive schools: An evidence-based approach. School Soc Work J. (2016) 40:37–60.
82. Dorado JS, Martinez M, McArthur LE, Leibovitz T. Healthy Environments and Response to Trauma in Schools (HEARTS): A whole-school, multi-level, prevention and intervention program for creating trauma-informed, safe and supportive schools. School Ment Health. (2016) 8:163–76. doi: 10.1007/s12310-016-9177-0
Keywords: adversity, resilient, protecting factors, interventions, umbrella review
Citation: Abate BB, Sendekie AK, Tadesse AW, Engdaw T, Mengesha A, Zemariam AB, Alamaw AW, Abebe G and Azmeraw M (2024) Resilience after adversity: an umbrella review of adversity protective factors and resilience-promoting interventions. Front. Psychiatry 15:1391312. doi: 10.3389/fpsyt.2024.1391312
Received: 25 February 2024; Accepted: 20 August 2024;
Published: 04 October 2024.
Edited by:
Ali Nawaz Khan, Hubei Engineering University, ChinaReviewed by:
Saeid Komasi, Mind GPS Institute, IranNicholas Collins, University of Delaware, United States
Copyright © 2024 Abate, Sendekie, Tadesse, Engdaw, Mengesha, Zemariam, Alamaw, Abebe and Azmeraw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Biruk Beletew Abate, YmlydWtrZWxlbWJAZ21haWwuY29t
 Biruk Beletew Abate
Biruk Beletew Abate Ashenafi Kibret Sendekie2
Ashenafi Kibret Sendekie2 Ayelign Mengesha
Ayelign Mengesha Alemu Birara Zemariam
Alemu Birara Zemariam Addis Wondmagegn Alamaw
Addis Wondmagegn Alamaw Gebremeskel Abebe
Gebremeskel Abebe Molla Azmeraw
Molla Azmeraw